Abstract
Objective:
The present study examined young adults’ completion of the web-based intervention content in a randomized trial that tested two Personalized Feedback Interventions (PFIs) for alcohol use and risky sex behavior (RSB).
Method:
Data are from a study that evaluated efficacy of two web-delivered PFIs (combined PFI and integrated PFI) among 269 sexually active young adults between the ages of 18 and 25. We described the view patterns of the web-based intervention and examined if baseline sociodemographic and alcohol- and sex-related behavioral factors were associated with the completion of PFI.
Results:
Many participants viewed the intervention more than one time, and the majority finished all intervention pages in at least one session. Older participants and participants who drink more frequently prior to or during sex were more likely to complete.
Conclusions:
Most participants, especially the young adults who were at higher risk, utilized the intervention contents as intended.
Keywords: Web-based intervention, PFI, young adults, alcohol-related sexual behavior
Introduction
Young adulthood is associated with increased alcohol use compared to other developmental periods, and national estimates show that 62.6% of U.S. young adults have been drunk in the past year.1 Acute alcohol-related negative consequences occur in personal, interpersonal, social, and health domains, including academic and/or occupational impairment, blackouts, injury, and death.2-4 Moreover, an estimated 29.2% of 18-29-year-olds with past-year alcohol use have an alcohol use disorder.5 As such, young adult alcohol use continues to be a public health concern in the U.S. and needs further prevention efforts.
In addition, both observational and experimental studies have demonstrated a connection between alcohol use and risky sexual behavior (e.g., Howells and Orcutt,6 Rehm et al,7 and Scott-Sheldon et al8). Alcohol use may contribute to risky sexual behavior through its effects on temporary cognitive impairment. According to alcohol myopia theory,9 acute alcohol intoxication creates cognitive impairment that results in an inability to attend fully to situational cues. For risky sexual behavior, acutely intoxicated individuals may be less likely to attend to less salient and more distal cues (i.e., risk for sexually transmitted infections) and more likely to attend to more salient and proximal cues (i.e., sexual arousal in the moment), resulting in a greater likelihood of risky sexual behavior.7, 10, 11 It has been argued that reducing heavy episodic drinking (4/5 or more drinks in a sitting for women/men) is a promising approach to preventing risky sexual behavior.6
Although most of the effects are modest and short-term, brief motivational interventions (BMIs), especially those with personalized feedback components, have been shown to be efficacious in reducing heavy drinking and alcohol-related problems,12, 13 including alcohol-related sexual behavior, among young adults.14-16 Moreover, web-delivered personalized feedback interventions (PFIs) have been widely used and can easily reach key populations outside of educational settings to reduce risky alcohol use and alcohol-related risky sexual behavior.16 Web-based interventions have pragmatic advantages over traditional in-person interventions, due to their brevity and cost-effectiveness. Moreover, research has shown that adults, particularly younger, female, and more educated adults, prefer web-based alcohol intervention among various intervention options.17, 18
Although more convenient than in-person interventions, participant engagement in web-delivered interventions has been lower than expected. Some factors, such as hazardous alcohol consumption, have been found to explain the lack of engagement or compliance in a web-based alcohol intervention study.19 Participants with higher alcohol consumption may experience a defensive reaction to the content provided or cognitive dissonance when viewing intervention contents, which may lead to their early termination from intervention participation. Thus, it is important to examine young adults’ engagement with web-delivered intervention content to help identify ways in which web-delivered interventions can be improved to keep young adults engaged with the feedback provided for them. Research to date has focused primarily on investigating the general efficacy of web-based alcohol interventions in reducing alcohol outcomes, with very little evidence on user experience and viewing patterns of the web-based intervention content.
This present study evaluated young adults’ engagement with the content of two web-based personalized feedback interventions aimed to reduce alcohol-related risky sexual behavior in a three-arm randomized controlled trial among sexually active, high-risk young adult drinkers.16 The two feedback interventions were the integrated PFI and the combined PFI. The Integrated PFI included integrated feedback on alcohol use and RSB components to address alcohol consumption as a factor in sexual behavior and highlight how these behaviors relate to each other, whereas the combined PFI separately addressed alcohol use and RSB among young adults. Although there was an overall significant effect of intervention compared to control, no significant differences were detected between the two PFIs in reducing young adult alcohol-related risky sexual behavior (RSB).
Assessment of young adults’ engagement with the two types of PFI consisted of automatic tracking of the number of times participants accessed the intervention, the number of page views of each intervention component, and the duration of time that participants spent on each page at every viewing session. This study aimed to: (1) examine the extent to which young adults engaged with the PFI content by describing their viewing patterns, and (2) test whether baseline sociodemographic and alcohol- and sex-related behavioral factors were associated with their completion of viewing all pages of the PFI.
Methods
Participants and Procedures
Participants were drawn from a study that examined web-based personalized feedback interventions (PFIs) among young adult drinkers aged 18-25.16 Through various national recruiting methods, this study enrolled 402 sexually active, high-risk drinkers who were not in a monogamous relationship (i.e., single, not dating; dating, not serious); had not used a condom during vaginal or anal sex after drinking in the past month; had an alcoholic drink at least once a week on average over the past 3 months; and had at least one episode of heavy episodic drinking (HED; 4+/5+ drinks for women/men in one sitting) in the past month. See Lewis et al16 for additional procedural details and inclusion criteria.
Participants were randomly assigned to three conditions: a combined PFI, an integrated PFI, or attention control. Webpages sent to the control group have general health-related information without any personalization or peer comparisons. Webpages sent to the two PFI groups included the intervention components such as descriptive norm (e.g., perceived alcohol use of peers compared with typical average alcohol use among peers), blood alcohol content (BAC) knowledge (e.g., knowledge with peer comparison and general knowledge), expectancies (i.e., beliefs about the effects of alcohol), biphasic effects of alcohol, perceived vulnerability (i.e., alcohol and perceived risk), alcohol myopia (i.e., why does alcohol affect "in the moment" decision making), consequences after drinking, willingness (e.g., summary about what a participant would be willing to do in a drinking scenario), and protective behavioral strategies.
The current study focused on data from the 269 participants who were assigned to two PFI groups (See Table 1). The mean age of participants was 22.34 years (SD = 1.83) at baseline. About half of the sample were female (53.2%) and current students (46.5%), 58.4% were non-Hispanic White, and 44.6% had at least some same-sex sexual experience. Of those who were current students, 67.2% attended a 4-year college, 20.8% attended a 2-year college, 8.0% attended graduate or professional school, 3.2% attended a vocational, technical, or trade school, and 0.8% were in high school. For the highest level of education completed, 35.7% of the sample had a bachelor’s degree, 26.4% had some college education, 21.9% had a high school diploma, 8.6% had an associate’s degree, 4.8% had a GED, 1.5% had a graduate or professional degree, 0.7% had a vocational degree, and 0.4% had less than a high school diploma. All assessment and intervention deliveries were completed entirely via the internet. The amount of time participants spent viewing each page of the web-based intervention was automatically recorded in 5-second intervals.
Table 1.
Descriptive statistics for baseline variables by intervention groups (N = 269).
| Variable | Range | Combined n = 134 |
Integrated n = 135 |
Overall N = 269 |
|---|---|---|---|---|
| Demographic | ||||
| Age, Mean (SD) | 18-25 | 22.6 (1.73) | 22.1 (1.90) | 22.3 (1.83) |
| % Female | - | 53.0 | 53.3 | 53.2 |
| % Non-Hispanic White | - | 57.1 | 60.0 | 58.6 |
| % Hispanic | - | 12.8 | 16.3 | 14.6 |
| % Black | - | 13.5 | 8.1 | 10.8 |
| % student | - | 44.3 | 50.0 | 47.2 |
| % of not entirely heterosexual | - | 50.0 | 39.3 | 44.6 |
| Baseline Risk Behaviors, Mean (SD) | ||||
| # of casual sexual partners | 0-15 | 1.4 (1.15) | 1.5 (1.76) | 1.5 (1.49) |
| # of times drinking before/during sex | 0-20 | 3.2 (3.40) | 3.1 (3.10) | 3.1 (3.25) |
| Alcohol-related sexual consequences | 0-22 | 4.7 (4.27) | 5.0 (4.89) | 4.8 (4.58) |
| Typical drinks per week | 0-84 | 20.7 (15.15) | 19.7 (12.79) | 20.2 (14.00) |
Note. The number of missing cases ranges from 0-3. There were no statistically significant differences between the two intervention groups, except that the Integrated PFI group tended to be younger (t = 2.2, p = .029).
Intervention Groups
Integrated PFI
The integrated PFI consisted of synthesized alcohol use and RSB components to address alcohol consumption as a factor in sexual behavior and highlight how these behaviors relate to each other (e.g., normative comparisons for the number of drinks consumed prior to sex, condom-related protective behavioral strategies when drinking). See Lewis et al16 for additional detail on integrated intervention content. The components of the integrated PFI included 15 pages of feedback (See Table 2 for details). Integrated alcohol and RSB components were presented to highlight how these behaviors relate to each other. Most of the integrated PFI pages contained personalized feedback and feedback in comparison with peers.
Table 2.
The information type, intervention component, and amount of time spent in seconds viewing each web-delivered intervention page.
| Combined |
Integrated |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pg | Mean | SD | Md | IQR | Max | * | PF | CM | Mean | SD | Md | IQR | Max | * | PF | CM |
| 1 | 22.5 | 55.85 | 10 | 15 | 560 | I | 0 | 0 | 27.3 | 66.42 | 10 | 15 | 455 | I | 0 | 0 |
| 2 | 30.8 | 46.13 | 20 | 16 | 350 | N | 1 | 1 | 30.4 | 40.14 | 20 | 20 | 280 | N | 1 | 1 |
| 3 | 11.4 | 17.65 | 5 | 10 | 130 | N | 1 | 1 | 10.5 | 28.55 | 5 | 5 | 300 | N | 1 | 1 |
| 4 | 10.7 | 26.56 | 5 | 10 | 285 | N | 1 | 1 | 7.1 | 10.25 | 5 | 10 | 55 | N | 1 | 1 |
| 5 | 9.1 | 47.54 | 5 | 10 | 550 | N | 1 | 1 | 6.6 | 16.46 | 5 | 5 | 150 | N | 1 | 1 |
| 6 | 7.0 | 11.99 | 5 | 10 | 100 | N | 1 | 1 | 45.3 | 63.23 | 30 | 40 | 435 | K | 1 | 1 |
| 7 | 7.1 | 27.05 | 0 | 5 | 290 | N | 1 | 1 | 18.5 | 30.52 | 5 | 25 | 175 | K | 1 | 0 |
| 8 | 42 | 41.69 | 30 | 40 | 220 | K | 1 | 1 | 16.5 | 31.18 | 10 | 15 | 300 | E | 1 | 1 |
| 9 | 17.6 | 25.35 | 5 | 25 | 145 | K | 1 | 0 | 7.7 | 8.54 | 5 | 15 | 40 | V | 1 | 0 |
| 10 | 8.5 | 17.92 | 5 | 10 | 180 | E | 1 | 0 | 4.3 | 8.45 | 0 | 5 | 70 | V | 1 | 0 |
| 11 | 14.9 | 31.58 | 5 | 15 | 215 | B | 0 | 0 | 4.3 | 10.33 | 0 | 5 | 85 | C | 1 | 0 |
| 12 | 10.0 | 24.61 | 5 | 11 | 265 | V | 1 | 0 | 8.3 | 19.01 | 5 | 5 | 160 | M | 0 | 0 |
| 13 | 3.4 | 7.00 | 0 | 5 | 55 | V | 1 | 0 | 4.9 | 11.43 | 0 | 5 | 85 | W | 1 | 0 |
| 14 | 7.9 | 15.17 | 5 | 10 | 125 | M | 0 | 0 | 47 | 48.66 | 35 | 50 | 305 | P | 1 | 0 |
| 15 | 4.5 | 13.38 | 0 | 5 | 135 | C | 1 | 0 | 57.7 | 119 | 33 | 45 | 900 | P | 1 | 0 |
| 16 | 4.5 | 13.52 | 0 | 5 | 140 | W | 1 | 0 | - | - | - | - | - | - | - | - |
| 17 | 3.6 | 8.43 | 0 | 5 | 65 | W | 1 | 0 | - | - | - | - | - | - | - | - |
| 18 | 43.0 | 47.37 | 35 | 55 | 275 | P | 1 | 0 | - | - | - | - | - | - | - | - |
| 19 | 37.3 | 61.51 | 20 | 45 | 460 | P | 1 | 0 | - | - | - | - | - | - | - | - |
Note. Pg = page. Md = median. IQR = interquartile range. PF = personalize feedback, CM = feedback with peer comparison.
Component of each intervention page. I=Introduction, N=Descriptive Norm, K=Knowledge, E=Expectancies, B=Biphasic Effect of Alcohol, V=Perceived Vulnerability, M=Alcohol Myopia, C=Alcohol-related Consequences, W=Willingness, P= Protective behavioral strategies; 0=Yes. 1=No.
Combined PFI
The combined PFI consisted of intervention components (i.e., normative comparison, alcohol expectancies, alcohol myopia, protective behavioral strategies) drawn from previous efficacious web-based interventions addressing both alcohol use and RSB among young adults. Components were presented independently without any discussion of the influence of alcohol on RSB (see Lewis et al16). There were 19 pages of feedback (Table 2). Information on alcohol was not integrated into the feedback on sexual behavior and vice versa. Most of the combined PFI pages contained personalized feedback and feedback in comparison to peers.
Measures
Baseline Demographics
Demographic variables examined in this study include age, biological sex (0 = female, 1 = male), race, ethnicity, student status, and sexual experience. Participants self-identified their ethnicity (0 = non-Hispanic/Latino, 1 = Hispanic/Latino) and their race from the following seven options: (1) Asian/Asian American, (2) Black/African, (3) Caucasian/White, (4) American Indian/Alaska Native, (5) Native Hawaiian/Pacific Islander, (6) more than one race, and (7) other. Racial and ethnic groups were dichotomized into 0 = others and 1 = non-Hispanic White (See Table 1). To assess student status, participants reported whether or not they were currently a student (0 = no, 1 = yes). To assess sexual experience, one item asked, “what statement best describes your sexual experience?” using response options 1 = entirely heterosexual experience, 2 = largely heterosexual experience, 3 = largely heterosexual but considerable homosexual experience, 4 = equally heterosexual and homosexual experience, 5 = largely homosexual but considerable heterosexual experience, 6 = largely homosexual but some heterosexual experience, and 7 = entirely homosexual experience. Sexual experience was dichotomized into entirely heterosexual experience (coded 1, if response was 1 for this sexual experience item) and not exclusively heterosexual experience (coded 0, if otherwise).
Baseline Risk Behaviors and Consequences
We defined each behavior before asking the questions to participants. The number of casual sexual partners was assessed by asking participants how many casual partners they had oral, vaginal, or anal sex with during the past month 15, 20. A casual partner was defined as a sexual partner with whom they did not have a monogamous relationship (i.e., sex only with each other) or someone they had known for less than 24 hours. The number of times participants drank prior to or during sex was assessed by asking participants how many times they had consumed alcohol before or during oral, vaginal, or anal sex in the past month 15, 20.
Alcohol-related sexual consequences were assessed using the 41-item Alcohol-related Sexual Consequences Scale.16, 21 Participants reported whether or not each consequence had occurred in the past month as a result of drinking alcohol (0 = no, 1 = yes). Items assessed digital, oral, vaginal, and anal sex with definitions of each sexual behavior. Sample items are: “In the past month, as a result of drinking alcohol… I had digital sex that I later regretted", “I had vaginal sex that I later regretted,” “I had oral sex without a condom,” and “I had vaginal sex with someone I wouldn't have had sex with when I was sober.” Items were summed to create a total number of alcohol-related sexual consequences experienced in the past month.
Typical drinks per week were assessed using the 7-item Daily Drinking Questionnaire (DDQ; Collins et al22). Participants were asked to consider a typical week during the past month and reported how much alcohol, on average, they drank on each day of a typical week (e.g., Monday, Tuesday). A standard drink was defined as 12 oz. beer (10 oz. Microbrew; 8 oz Malt Liquor, Canadian beer or Ice beer; 6 oz. ice malt liquor); 5 oz. of wine; 10 oz. wine cooler; or 1 Cocktail with 1 oz. of 100 proof liquor or 1½ oz. (single jigger) of 80 proof liquor. The seven items were summed to indicate the total number of drinks participants consumed in a typical week during the past month.
Time Spent Viewing Online Personalized Feedback
For all conditions, the online intervention feedback was programmed to automatically record how long participants viewed each page of the feedback. Because participants’ engagement with the profile feedback was recorded every five seconds, it was required for participants to see a page for at least five seconds to register a viewing time. When participants viewed the feedback more than once (in whole or part), viewing times were recorded separately for each viewing session. We coded the time spent using all valid viewing sessions and reported the following values separately: time spent on each page (in seconds), time spent per intervention component (in seconds), and the average duration of time spent per viewing session (in minutes).
Analysis Plan
Data Screening and Checking
Data were first examined for extreme values (outliers) in the number of casual partners in the past month (one case greater than 40 partners), the number of times consumed alcohol before or during a sexual encounter when had any sex in the past month (two cases greater than 35 times), alcohol-related sexual consequences (one case scored greater than 37), typical drinks per week (one case greater than 175 drinks), and time spent on the viewing session that may compromise the accuracy of conclusions drawn from the analysis. We also examined the length of viewing each page by session and identified 21 records where the length was extremely long. After calculating the average time duration participants spent on each page across all sessions and the duration of each viewing session, we identified extreme values and treated them as missing values. Decisions to treat them as missing values and consequently exclude them from subsequent analyses were based on the degree to which an individual observation was separated from the rest of the distribution, which can happen, for example, if someone started a page but got distracted by a phone call and left. This procedure resulted in missing data from 2% or fewer cases for the analysis of each variable.
Descriptive and Regression Analysis
Aim 1 was evaluated using descriptive analyses to examine the record of views of the web-based intervention. For Aim 2, logistic regression was conducted to examine if baseline sociodemographic and alcohol- and sex-related behavioral factors were associated with the completion of looking at all pages of the PFI. Statistical analyses were performed using the SPSS (IBM Inc., Version 26, Armonk, New York) statistical software program. Statistical significance was defined as a two-sided test at p <.05.
Results
Aim 1: Descriptive Analyses on Young Adults’ Engagement with The PFI Content
We examined the viewing process of participants who were randomized into the two intervention groups (N = 269). Across both intervention conditions, almost all (97%) participants viewed at least part of the online feedback, and about two-fifths (42.0%) viewed it more than once (i.e., some returned to see the web-delivered information after their first viewing session). Of those who accessed their feedback (n = 262), the number of viewing sessions ranged from 1 to 8 times (M = 1.7, SD = 1.05). Most (79.9%) of the participants in the two PFI groups looked at all pages one or more times, with approximately half of the participants (53.5%) completing their feedback at the first viewing session (See Table 3 for more details).
Table 3.
Viewing patterns of web-based contents by intervention groups (N=269).
| Indicator | Combined n = 134 |
Integrated n = 135 |
|---|---|---|
| Total number of viewing sessions, Mean (SD) | 1.7 (1.13) | 1.7 (0.95) |
| Ave. duration per session (in minutes), Mean (SD) | 3.5 (3.56) | 3.5 (3.33) |
| Ave. progress at the 1st session (%) | 72.9 | 68.0 |
| Completed at the 1st session (%) | 53.7 | 53.3 |
| Return to view after the 1st session (%) | 43.2 | 43.1 |
| Completed at least one session (%) | 79.1 | 80.7 |
Note. The number of missing cases ranged from 0-7.
The average time spent on each intervention page was 12.5 seconds (SD = 12.4, range 0-76 sec). In general, participants spent more time on pages that included both personalized feedback and peer comparison, followed by personalized feedback only and general educational information. For intervention components, participants spent more time on pages about knowledge with peer comparison and protective behavioral strategies (See Table 2 and Table 4). These pages contained hands-on or interactive components such as calculating BAC and answering questions about their intention to use a list of protective behavioral strategies in the next month. The majority (75%) of participants (79.3% in the Integrated PFI group and 70.9% in the Combined PFI group) chose at least one protective behavioral strategy from the list. The most frequently selected strategy was “plan safe transportation” both intervention groups, and the least frequently selected strategy was “avoid drinking games.” Among participants who received the combined PFI, two (1.5%) participants did not view any page, 106 (79.1%) looked at all pages at least once, and 57 (42.5%) returned to the feedback for a subsequent viewing session; among participants who received the integrated PFI, the numbers were five (3.7%), 109 (80.7%), and 56 (41.5%), respectively (See Figure 1).
Table 4.
Average time (in seconds) per page spent on each web-delivered intervention component and each information type.
| Combined |
Integrated |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention Component | Mean | SD | Md | IQR | Max | Mean | SD | Md | IQR | Max |
| Descriptive norm | 12.7 | 16.4 | 7.5 | 9.2 | 144.2 | 13.7 | 17.7 | 8.8 | 7.5 | 130.0 |
| Knowledge with comparison | 42.0 | 41.7 | 30.0 | 40.0 | 220.0 | 45.3 | 63.2 | 30.0 | 40.0 | 435.0 |
| General knowledge | 17.6 | 25.4 | 5.0 | 25.0 | 145.0 | 18.5 | 30.5 | 5.0 | 25.0 | 175.0 |
| Expectancies | 8.5 | 17.9 | 5.0 | 10.0 | 180.0 | 16.5 | 31.2 | 10.0 | 15.0 | 300.0 |
| Biphasic effect of alcohol | 14.9 | 31.6 | 5.0 | 15.0 | 215.0 | - | - | - | - | - |
| Perceived vulnerability | 6.7 | 13.2 | 2.5 | 7.5 | 132.5 | 6.0 | 6.8 | 5.0 | 10.0 | 37.5 |
| Alcohol myopia | 7.9 | 15.2 | 5.0 | 10.0 | 125.0 | 8.3 | 19.0 | 5.0 | 5.0 | 160.0 |
| Consequences | 4.5 | 13.4 | 0.0 | 5.0 | 135.0 | 4.3 | 10.3 | 0.0 | 5.0 | 85.0 |
| Willingness | 8.1 | 19.4 | 0.0 | 10.0 | 185.0 | 8.3 | 19.0 | 5.0 | 5.0 | 160.0 |
| Protective behavioral strategies | 40.2 | 50.7 | 27.5 | 48.1 | 337.5 | 52.3 | 71.4 | 35.0 | 47.5 | 485.0 |
| Overall Information Type* | ||||||||||
| Feedback with peer comparison | 16.8 | 16.9 | 12.9 | 15.4 | 130.0 | 23.3 | 24.5 | 16.5 | 16.0 | 136.0 |
| Feedback only | 14.7 | 15.9 | 10.0 | 16.4 | 80.0 | 20.6 | 23.3 | 14.3 | 16.4 | 144.3 |
| General information | 11.4 | 19.2 | 5.0 | 12.5 | 127.5 | 8.3 | 19.0 | 5.0 | 5.0 | 160.0 |
Note. Md = median. IQR = interquartile range. See Table 2 for detailed information about the intervention component and information type on each intervention page.
If a page had both personalized feedback (PF) and peer comparison (CM) content (PF = 1 and CM = 1), overall information type was coded as feedback with peer comparison; if a page had only feedback but no peer comparison (PF = 1 and CM = 0), the page was categorized as feedback only; and if a page did not have any feedback or peer comparison content (PF = 0 and CM = 0), the page type was coded as general information.
Figure 1. Viewing process of combined PFI (top) and integrated PFI (bottom).
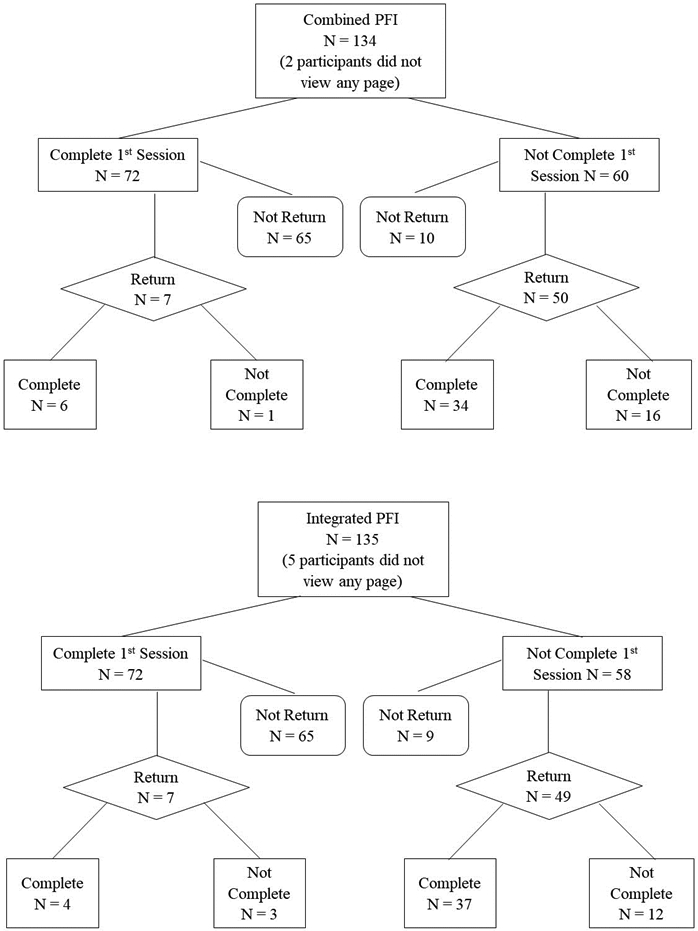
Note. The number of one-time completions is 106 (79%) for combined PFI and 109 (81%) for integrated PFI. The total number of one-time completions is 215 (80%) for two groups.
Aim 2: Logistic Regression Analyses Testing Predictors of Viewing All PFI Content
Logistic regression results for participant-reported baseline demographic characteristics and behavioral factors as predictors of whether or not participants viewed the entire contents of the web-based PFI at least once are presented in Table 5. The model tested was statistically better than the null model (Likelihood-ratio X2 = 19.48, df = 10, p = 0.03, Nagelkerke R2 = 0.12).
Table 5.
Logistic regression of intervention completion on baseline demographics and behavior factors among participants who received combined or integrated PFI (N = 269).
| Predictor | OR | 95% CI Lower |
95% CI Upper |
|---|---|---|---|
| Male vs. Female | 0.61 | 0.30 | 1.23 |
| Age | 1.31 | 1.07 | 1.60 |
| Non-Hispanic White vs. Others | 0.60 | 0.30 | 1.20 |
| Entirely heterosexual vs. Not entirely heterosexual experience | 1.73 | 0.84 | 3.60 |
| Student vs. Non-student | 1.93 | 0.93 | 4.04 |
| Integrated PFI vs. Combined PFI | 1.29 | 0.67 | 2.51 |
| # of casual sexual partners | 1.01 | 0.72 | 1.42 |
| # of times drinking prior to or during sex | 1.18 | 1.01 | 1.38 |
| Alcohol-related sexual consequences | 0.94 | 0.87 | 1.02 |
| Typical drinks per week | 1.00 | 0.97 | 1.02 |
Note. Intervention completion (0 = Did not finish reading all the pages of the intervention across all viewing sessions; 1 = Finished all intervention pages at least once across all viewing sessions). Reference groups were female, non-white others, not entirely heterosexual experience, non-student, and combined PFI. Missing cases = 11. Statistically significant estimates are in bold.
Each year in age was associated with a 31% increase in the odds of completing the entire contents of the web-based PFI (Adjusted Odds Ratio = 1.31, 95% confidence interval [CI] = [1.07, 1.60]). For each added alcohol-related sexual behavior (i.e., an episode of drinking prior to or during sex), the odds of completing the entire PFI increased by 18% (Adjusted Odds Ratio = 1.18, 95% CI = [1.01, 1.38]). We did not find sex or race differences in terms of completing the web-delivered PFI content. Furthermore, there was no evidence that the completion of reviewing all pages of web-based PFI was related to student status, intervention group membership (integrated vs. combined), sexual orientation, the number of casual sexual partners, the typical number of drinks per week, and alcohol-related sexual consequences.
Discussion
The present findings contribute novel knowledge about young adults’ willingness to engage with and acceptance of personalized feedback and their interactions with an online alcohol-related sexual behavior PFI. Specifically, we found that most participants completed the entire online PFI and that almost 40% of the participants viewed the PFI more than once. Research has shown participants have multiple distractions when viewing online interventions;23 thus, participants may need multiple sessions to view feedback in its entirety and return to the feedback for a more detailed and careful review for all or specific pages. Consistent with previous studies, our findings indicated that web-delivered PFI programs should allow long-term and sustained access so that participants can return to the intervention materials when needed. The findings also suggest that future studies collect more user experience data to examine if increased time or undisrupted and focused time on intervention pages will reduce risk behaviors to a greater extent.
In addition to demonstrating that many participants viewed their online feedback more than once, this study revealed which components of the intervention young adults spent the most time viewing in the online PFI. Overall, participants spent more time on feedback pages in which their behavior was compared to peers of their age and sex, such as descriptive normative comparisons, or pages in which participants were asked to indicate future intentions, such as willingness to use protective behavioral strategies in the next month. Of importance, pages on which very little time was spent included those providing only general knowledge without personalized feedback or normative comparisons. Notably, participants spent the least time on the page that listed the specific negative consequences that the participant had reported experiencing. This finding suggests that the intervention content on negative consequences needs to be modified to hold young adults’ attention and engage them in the material. These findings are similar to Ray et al24, in which levels of personalization were associated with intervention outcomes when many intervention content topics were discussed.
This study also examined if there were demographic and baseline behaviors that predicted who was likely to view the PFI in its entirety. Across both interventions (combined or integrated), findings indicated that per each additional year of age, the odds of completion increased by 31%, and for each additional number of times drinking prior to or during sex, the odds of completion increased by 18%. There were no other significant predictors. These findings were in line with prior research suggesting that it is difficult to determine who is likely to finish a video PFI.25 Compared to other treatment options, web-based PFI is a more preferred intervention delivery method among young adults. However, our results indicated that once assigned to the intervention, older young adults who engaged more frequently in alcohol-related risky sexual behavior at baseline were more likely to complete web-based intervention. Additional research is needed to help understand who is more likely to complete intervention content and why, regardless of intervention content is delivered (e.g., online or video-conferencing).
Overall, these findings suggest that future research should consider ways to increase quality time spent on individual pages of feedback by increasing personalized information or normative comparison information. If participants are willing to come back to view feedback information more than once, this suggests that interventions could include “real-time” drinking behavior or sexual risk behavior profiles to reflect the ongoing experience of behavior over time as well as provide content specific to risk-prone events, such as holidays or weekends. Of the emerging research in this area, findings suggest that personalized interventions are most effective in reducing alcohol use among young adults who reported greater perceived attention to the web-based content.23 Moreover, research has also shown that gamified interventions or interventions with an expressive writing component hold promise as potential ways for increasing attention.26-28 Although boosters are common in PFI studies, they often repeat the original intervention material rather than provide updated or new content. Future research should consider PFIs that build attractive, interactive, dynamic profiles of behavior that update over time.
Limitations
Several limitations of this study should be noted. First, we focused on time spent on the online intervention pages, which cannot account for the possibility that participants may have stopped looking at the intervention content on their computer screen while engaging in another activity. Here we assume that the time spent on the feedback page is a proxy for time spent actually viewing and engaging in that content (i.e., reading and processing). Future work should explore other indicators or interactive components to show that young adults actively engage and process online intervention content. Second, we cannot determine whether participants spent more time on the intervention page because the content was engaging and interesting or because it was confusing. Third, we could not assume that longer time spent on web-based PFI is related to better intervention outcomes because we do not know how participants interact with the intervention content in a real-world environment. More studies are warranted to explore the associations among viewing behavior, engagement with intervention content, and the effectiveness of web-based intervention in reducing alcohol-related risky sexual behavior among young adults. Fourth, findings may not generalize to interventions targeting other behaviors (e.g., marijuana use) or to other populations (e.g., adolescents).
Conclusions
Findings from the current study unequivocally suggest it is important to afford young adults the ability to return to online PFI content. Young adults may not be able to review all the content in a single session and may want to revisit the intervention content. In order for online PFIs to optimize their potential impact on reducing risky behaviors (and maximize intervention effect sizes) among young adults, it may be optimal to allow for multiple viewing sessions of online intervention content. In addition, we found that young adults did spend time on pages with personalized and interactive components with peer comparison but relatively less time on general educational information. Our findings suggest that it is important for researchers and providers to develop more engaging online activities when designing web-delivered interventions, especially those targeting young adults.
Funding Details
Data collection was supported by NIAAA Grant R21 AA021767 awarded to M. A. Lewis. Manuscript preparation was supported in part by NIAAA Grant R01 AA019511 awarded to E.-Y. Mun.
Footnotes
Conflict of Interest
The authors have no conflicts of interest to declare. The content of this manuscript is solely the responsibility of the author(s) and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health.
References
- 1.Schulenberg JE, Johnston LD, O'Malley PM, Bachman JG, Miech RA, Patrick ME. Monitoring the Future national survey results on drug use, 1975-2018. Volume II, college students & adults ages 19-60. 2019. http://monitoringthefuture.org/pubs.html#monographs [Google Scholar]
- 2.Cleveland MJ, Mallett KA, White HR, Turrisi R, Favero S. Patterns of alcohol use and related consequences in non-college-attending emerging adults. J Stud Alcohol Drugs. 2013;74(1):84–93. doi: 10.15288/jsad.2013.74.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hingson R, White A. New research findings since the 2007 Surgeon General's Call to Action to Prevent and Reduce Underage Drinking: A review. J Stud Alcohol Drugs. 2014;75(1):158–69. doi: 10.15288/jsad.2014.75.158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.White A, Hingson R. The burden of alcohol use excessive alcohol consumption and related consequences among college students. Alcohol Res Curr Rev. 2013;35(2):201–218. [PMC free article] [PubMed] [Google Scholar]
- 5.Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911–923. doi: 10.1001/jamapsychiatry.2017.2161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howells NL, Orcutt HK. Diary study of sexual risk taking, alcohol use, and strategies for reducing negative affect in female college students. J Stud Alcohol Drugs. 2014;75(3):399–403. doi: 10.15288/jsad.2014.75.399 [DOI] [PubMed] [Google Scholar]
- 7.Rehm J, Shield KD, Joharchi N, Shuper PA. Alcohol consumption and the intention to engage in unprotected sex: Systematic review and meta-analysis of experimental studies. Addiction. 2012;107(1):51–9. doi: 10.1111/j.1360-0443.2011.03621.x [DOI] [PubMed] [Google Scholar]
- 8.Scott-Sheldon LA, Carey KB, Cunningham K, Johnson BT, Carey MP, Team MR. Alcohol use predicts sexual decision-making: A systematic review and meta-analysis of the experimental literature. AIDS Behav. 2016;20 Suppl 1:S19–39. doi: 10.1007/s10461-015-1108-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steele CM, Josephs RA. Alcohol myopia. Its prized and dangerous effects. Am Psychol. 1990;45(8):921–33. doi: 10.1037//0003-066x.45.8.921 [DOI] [PubMed] [Google Scholar]
- 10.Davis KC, Hendershot CS, George WH, Norris J, Heiman JR. Alcohol's effects on sexual decision making: An integration of alcohol myopia and individual differences. J Stud Alcohol Drugs. 2007;68(6):843–51. doi: 10.15288/jsad.2007.68.843 [DOI] [PubMed] [Google Scholar]
- 11.Scott-Sheldon LA, Carey KB, Cunningham K, Johnson BT, Carey MP, Mash Research Team. Alcohol use predicts sexual decision-making: A systematic review and meta-analysis of the experimental literature. AIDS Behav. 2016;20 Suppl 1:S19–39. doi: 10.1007/s10461-015-1108-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huh D, Mun EY, Larimer ME, et al. Brief motivational interventions for college student drinking may not be as powerful as we think: An individual participant-level data meta-analysis. Alcohol Clin Exp Res. 2015;39(5):919–931. doi: 10.1111/acer.12714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carey KB, Henson JM, Carey MP, Maisto SA. Which heavy drinking college students benefit from a brief motivational intervention? J Consult Clin Psychol. 2007;75(4):663–669. doi: 10.1037/0022-006X.75.4.663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dermen KH, Thomas SN. Randomized controlled trial of brief interventions to reduce college students' drinking and risky sex. Psychol Addict Behav. 2011;25(4):583–594. doi: 10.1037/a0025472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewis MA, Patrick ME, Litt DM, et al. Randomized controlled trial of a web-delivered personalized normative feedback intervention to reduce alcohol-related risky sexual behavior among college students. J Consult Clin Psychol. 2014;82(3):429–440. doi: 10.1037/a0035550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lewis MA, Rhew IC, Fairlie AM, Swanson A, Anderson J, Kaysen D. Evaluating personalized feedback intervention framing with a randomized controlled trial to reduce young adult alcohol-related sexual risk taking. Prev Sci. 2019;20(3):310–320. doi: 10.1007/s11121-018-0879-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Epler AJ, Sher KJ, Loomis TB, O'Malley SS. College student receptiveness to various alcohol treatment options. J Am Coll Health. 2009;58(1):26–32. doi: 10.3200/JACH.58.1.26-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Batterham PJ, Calear AL. Preferences for internet-based mental health interventions in an adult online sample: Findings from an online community survey. JMIR Ment Health. 2017;4(2):e26. doi: 10.2196/mental.7722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Radtke T, Ostergaard M, Cooke R, Scholz U. Web-based alcohol intervention: Study of systematic attrition of heavy drinkers. J Med Internet Res. 2017;19(6):131–142. doi: 10.2196/jmir.6780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lewis MA, Lee CM, Patrick ME, Fossos N. Gender-specific normative misperceptions of risky sexual behavior and alcohol-related risky sexual behavior. Sex Roles. 2007;57(1-2):81–90. [Google Scholar]
- 21.Fairlie AM, Jaffe AE, Davis KC, et al. Establishing a new measure of alcohol-related sexual consequences and examining its association to alcohol consequences among at-risk young adults. J Stud Alcohol Drugs. 2021;82(4):493–502. doi: 10.15288/jsad.2021.82.493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. J Consult Clin Psychol. 1985;53(2):189–200. doi: 10.1037/0022-006X.53.2.189 [DOI] [PubMed] [Google Scholar]
- 23.Lewis MA, Neighbors C. An examination of college student activities and attentiveness during a web-delivered personalized normative feedback intervention. Psychol Addict Behav. 2015;29(1):162–167. doi: 10.1037/adb0000003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ray AE, Kim SY, White HR, et al. When less is more and more is less in brief motivational interventions: Characteristics of bmi content and their associations with drinking outcomes. Psychol Addict Behav. 2014;28(4):1026–1040. doi: 10.1037/a0036593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee CM, Cadigan J, Kilmer J, et al. Brief Alcohol Screening and Intervention for Community Collee Students (BASICCS): Feasibility and preliminary efficacy of web-conferencing BASICCS and supporting automated text-messages. Psychol Addict Behav. 2021;35(7):840–851. doi: 10.1037/adb0000745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boyle SC, Earle AM, LaBrie JW, Smith DJ. PNF 2.0? Initial evidence that gamification can increase the efficacy of brief, web-based personalized normative feedback alcohol interventions. Addict Behav. 2017;67:8–17. doi: 10.1016/j.addbeh.2016.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Earle AM, LaBrie JW, Boyle SC, Smith D. In pursuit of a self-sustaining college alcohol intervention: Deploying gamified PNF in the real world. Addict Behav. 2018;80:71–81. doi: 10.1016/j.addbeh.2018.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Young CM, Neighbors C. Incorporating writing into a personalized normative feedback intervention to reduce problem drinking among college students. Alcohol Clin Exp Res. 2019;43(5):916–926. doi: 10.1111/acer.13995 [DOI] [PMC free article] [PubMed] [Google Scholar]


