ABSTRACT
Background
Research is needed to identify pathways by which household food insecurity (FI) contributes to parental controlling feeding styles and infant food responsiveness, 2 factors that play a role in shaping obesity risk across infancy and early childhood.
Objectives
This longitudinal study tested the hypothesis that prenatal FI would be positively associated with higher infant food responsiveness via greater parental mental health symptomatology and controlling feeding styles (pressuring, restrictive).
Methods
Participants included a community sample of 170 birth parents and their infants participating in an ongoing longitudinal study. Parents self-reported household FI and mental health symptoms (depression and anxiety) during pregnancy. Postnatally, parents reported their mental health symptoms, their use of controlling feeding styles, and infant food responsiveness. Path analyses with bias-corrected 95% bootstrapped CIs tested direct and indirect associations between prenatal FI and infant food responsiveness.
Results
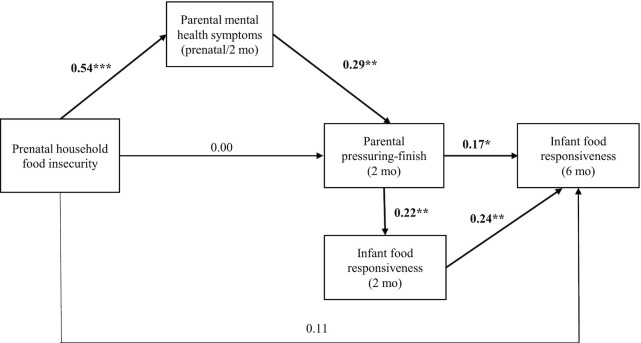
Prenatal FI was indirectly associated with higher infant food responsiveness via greater parental mental health symptomatology and pressuring to finish (b = 0.01; 95% CI: 0.001, 0.025). Prenatal FI was associated with greater parental mental health symptomatology across the peripartum period (β = 0.54; P < 0.001), which in turn was associated with more pressuring to finish at 2 months pospartum (β = 0.29; P = 0.01) and higher infant food responsiveness at 6 months (β = 0.17; P = 0.04). There were no direct effects of prenatal FI on controlling feedings styles or infant food responsiveness.
Conclusions
Our findings point to parental mental health as a potential pathway by which FI may be associated with obesity-promoting parental feeding styles and infant appetitive behaviors. In addition to ensuring reliable access to enough quality food during pregnancy, multipronged assistance that promotes emotional well-being during the peripartum period and clinical guidance on noncontrolling feeding styles could benefit parent and infant health and well-being.
Keywords: food insecurity, controlling feeding styles, appetitive behaviors, food responsiveness, mental health symptoms, infancy
Household food insecurity (FI), defined as limited or uncertain access to nutritionally adequate foods for an active and healthy life (1), is associated with poor pregnancy outcomes (e.g., low birth weight, higher gestational weight gain) (2, 3) and has negative consequences for child health and development (4, 5). A large body of literature has examined associations between household FI and child weight outcomes, but results from these studies are inconsistent (4, 6–8). To date, very few studies have targeted the prenatal and early postnatal periods, times of increased vulnerability due to developmental programming of obesity in utero and the importance of infancy for establishing healthy growth patterns (9). Furthermore, the pathways by which FI may contribute to adverse weight outcomes in infancy and early childhood, which are likely multifactorial and cascading, are largely unknown (10, 11).
Individual variation in infant appetitive behaviors is evident within the first few weeks of life (12). Higher levels of food responsiveness, characterized by feeding demandingness, excessive hunger, and responsiveness to external food cues (12), have been associated with higher BMIs and greater weight gain across infancy (13–15). Although FI has been associated with higher food responsiveness among low-income preschool-age children (16, 17), this association has not been tested in infants to date. Additionally, both household FI (18–20) and child food responsiveness (21, 22) have been associated with parental controlling feeding styles, such as pressuring (e.g., encouraging intake despite child fullness) and restriction (e.g., limiting intake even if the child is still hungry). Thus, controlling feeding may function as an indirect path by which prenatal FI affects an infant's food responsiveness.
Household FI is a significant stressor for families (23, 24), and the experience of FI may influence parenting behaviors, such as feeding, through its effects on mental health (25). For example, a depressed mood may interfere with a parent's ability to appropriately respond to infant hunger and fullness cues, and increased anxiety may exacerbate concern over the amount an infant is eating (26, 27). In studies with infants, parental depression and anxiety have been associated with forceful and uninvolved feeding styles (28), and anxiety symptoms assessed prenatally and at 6 months postnatally predicted greater restrictive feeding at 1 year (27). Prior studies with preschool- and school-aged children have shown that depressive symptoms may be associated with greater pressuring to eat, assessed via parent reports (29, 30) and video-recorded observations (31). Evidence also suggests that FI and its associated mental health symptomatology may contribute to controlling feeding and child food responsiveness. In a sample of preschool-aged children, Eagleton and colleagues (17) found higher child food responsiveness among food insecure compared to food secure children in the context of high perceived stress. Another study found that higher parental stress and a depressed mood earlier in the day predicted greater restrictive feeding among food insecure families with children aged 5–7 years (32). To date, no studies, to our knowledge, have explicitly examined parental mental health (depression and anxiety in particular) as a factor that may help explain previously reported associations between FI, parental feeding styles, and child appetitive behaviors.
Therefore, the purpose of the current study is to examine the association between prenatal household FI and infant food responsiveness, an appetitive behavior that plays a role in shaping obesity risk in early childhood, and to assess whether parental depressive or anxious symptomatology and controlling feeding styles are indirect pathways by which prenatal FI influences infant food responsiveness. Using longitudinal data from a community-based sample of birth parents and their infants, we tested the following hypotheses: 1) prenatal FI is directly associated with greater parental mental health symptomatology, greater endorsement of controlling feeding styles, and higher infant food responsiveness; and 2) prenatal FI is indirectly associated with higher infant food responsiveness at 6 months through greater parental mental health symptomatology and controlling feeding styles, while controlling for stability in food responsiveness from 2 to 6 months and any possible concurrent association between controlling feeding and food responsiveness at 2 months.
Methods
Participants
Participants included mother-infant dyads from cohort 1 (n = 176) of the Infant Growth and Development Study (iGrow), a longitudinal study examining prenatal and early postnatal predictors of childhood obesity risk (33). Participants were recruited during pregnancy in Guilford County, North Carolina, from childbirth education classes at hospitals and the public health department; Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) breastfeeding classes; and flyers advertised in obstetric and gynecological clinics and on social media. Recruitment for cohort 1 began in January 2019 and ended in March 2020 due to coronavirus disease 2019 (COVID-19). The eligibility criteria included a birth parent age of at least 18 years, expecting a singleton birth, written English comprehension, and plans to remain in the region for at least 3 years. Data collection for the prenatal through the 6-month waves for cohort 1 spanned February 2019 to October 2020. This study was approved by the university's Institutional Review Board (protocol #18–0198). For the current study, infants born at <35 weeks of gestation (n = 3) and with parent-reported medical conditions that could affect feeding or growth (n = 3) were excluded, resulting in an analytic sample of 170. Of the analytical sample, 168 provided data on FI at the prenatal wave, 143 provided controlling feeding style data at 2 months, and 142 provided food responsiveness data at 6 months.
Procedures
Participating birth parents provided written consent and completed online questionnaires prior to a prenatal laboratory visit during their third trimester of pregnancy. Approximately 1 week after infants’ due dates, phone interviews were conducted with birth parents to obtain infant birth details, and online questionnaires were completed prior to laboratory visits when their infants were approximately 2 months (mean = 2.23; SD = 0.55) and 6 months (mean = 7.09; SD = 1.36) old. Following laboratory visits, participants received  50 at the prenatal wave,
50 at the prenatal wave,  80 at the 2-month wave, and
80 at the 2-month wave, and  80 at the 6-month wave. If travel to laboratory visits was greater than 25 miles, compensation was provided, if requested. Additionally, participants received small gifts throughout the study.
80 at the 6-month wave. If travel to laboratory visits was greater than 25 miles, compensation was provided, if requested. Additionally, participants received small gifts throughout the study.
Measures
Household FI
Household FI was assessed using the Short-Form Household Food Security Module from the USDA (34), a validated 6-item subset of the 18-item version of the module. The survey was completed at the prenatal wave to assess FI specifically experienced during the current pregnancy, rather than asking about the last year (e.g., “during this pregnancy, did you ever cut the size of your meals or skip meals because there wasn't enough food?”). Each response was dichotomized as either affirmative or nonaffirmative, and affirmative responses were summed. The continuous sum score was used in primary analyses, with higher scores reflecting more severe FI (α = 0.87) (35–37). For descriptive purposes, households were classified as food insecure if 2 or more of the 6 items were answered affirmatively and food secure if fewer than 2 of the 6 items were answered affirmatively (34).
Parental mental health symptomatology
At the prenatal and 2-month waves, mental health symptoms related to depression and anxiety were assessed. Depressive symptoms over the past week were assessed using the 20-item Center for Epidemiological Studies Depression scale (38). The State-Trait Anxiety Inventory was used to assess trait anxiety at the prenatal wave and state anxiety at the 2-month wave (39). The 20-item trait anxiety scale asks participants to indicate how they generally feel (e.g., “I feel pleasant,” “I feel nervous and restless”), and the state anxiety scale asks participants to indicate how they feel right now, at this moment (e.g., “I am worried,” “I feel tense”). For each scale, items were reverse scored as needed, and a mean score was calculated such that higher scores reflected a greater number of symptoms (α = 0.89–0.93). Due to the high correlation between depressive and anxiety symptoms at the 2 time points [prenatal r = 0.74 (P < 0.001); 2-month r = 0.76 (P < 0.001)], the mean scores for depressive and anxiety symptoms at the prenatal and 2-month waves were standardized and averaged within wave. Total symptomatology was highly correlated across the 2 waves (r = 0.50; P < 0.001). Thus, they were averaged to create 1 score reflecting mental health symptomatology across the peripartum period.
Controlling feeding styles
Controlling feeding styles were assessed at the 2-month wave using the Infant Feeding Styles Questionnaire (IFSQ) (40). The IFSQ was validated in a sample of low-income, black parent-infant dyads and has been successfully used in racially and ethnically and socioeconomically diverse samples (41, 42) and with infants <6 months old (43, 44). The IFSQ assesses 5 feeding style domains that reflect a range of parental behaviors and beliefs surrounding infant and toddler feeding. The current study focused on pressuring and restrictive feeding styles, the 2 controlling feeding domains that the IFSQ measures. Pressuring feeding was measured using 3 subscales: pressuring-finish (6 items; α = 0.78; “I try to get my baby to eat even if he/she seems not hungry”), pressuring-cereal (5 items; α = 0.78; “an infant less than 6 months needs more than formula or breastmilk to be full”), and pressuring-soothing (4 items; α = 0.59; “when my baby cries, I immediately feed him/her”). Restrictive feeding was measured using 2 subscales: restrictive-amount (4 items; α = 0.71; “I am very careful not to feed my baby too much”) and restrictive-diet quality (5 items; α = 0.74; “an infant should never eat fast food”). Behaviors (coded as 1 for “never” to 5 for “always”) and beliefs (coded as 1 for “disagree” to 5 for “agree”) were scored, and a mean score was calculated for each subscale, such that higher scores reflect greater endorsement of that feeding belief or practice. These 5 subscales were considered separately in analyses rather than being aggregated into the broader pressuring and restrictive feeding styles.
Infant food responsiveness
Infant food responsiveness was assessed at the 2-month (as a covariate) and the 6-month (primary outcome) waves using the 6-item food responsiveness subscale from the Baby Eating Behavior Questionnaire (BEBQ) (12). Participants rated the frequency (coded as 1 for “never” to 5 for “always”) of their infant's responsiveness to milk and feeding cues (“my baby frequently wants more milk than I have given him/her”). Within each wave, items were averaged to calculate a mean score, with higher scores reflecting higher infant food responsiveness (α values = 0.79 and 0.80 at 2 and 6 months, respectively). The BEBQ has been used previously, both with the sample from the current study (45) and in other studies with a broad range of sociodemographic characteristics (46–48).
Demographic characteristics
Participants reported their age, race, ethnicity, educational attainment, marital status, household members, income, and pre-pregnancy weight at the prenatal wave. We calculated an income-to-needs ratio by dividing the total annual household income by its corresponding poverty threshold, determined by the year in which the income was earned and the total number of household members. The poverty thresholds for 2018 and 2019, published in US Census Reports, were used to determine a household's poverty threshold (49). Participant height was measured in duplicate at the prenatal laboratory visit, and pre-pregnancy BMI (kg/m2) was calculated. Participants reported their infant's sex, health status, and birth date (used to calculate gestational age) over the phone approximately 1 week after their infant's due date. At the 2-month wave, participants reported participation in WIC, which is a federal assistance program that serves low-income pregnant, postpartum, and breastfeeding women and their infants and children up to 5 years of age by providing supplemental foods, nutrition education, and health-care referrals. Participants also provided detailed feeding information using a modified version of the Infant Feeding Practices Study II Questionnaire (50). The percentage of total milk feedings (breastmilk and formula) that were breastmilk (either at the breast or by bottle) were estimated, and breastfeeding intensity was defined as the proportion of milk feedings per day that were breastmilk (51). Because data collection occurred during the COVID-19 pandemic, we created a variable reflecting the number of days the participant had been exposed to the pandemic by the dates of their 2-month and 6-month visits (beginning from 11 March 2020). This variable is intended to reflect accumulated change and distress due to the pandemic, which was an unexpected potential confound.
Statistical analysis
Preliminary data analysis was conducted in SPSS Version 27 (IBM). Descriptive statistics were calculated to describe the sample. We examined differences in participant characteristics and primary study variables by household food security status using t-tests for continuous variables and χ2 tests for categorical variables. Primary analyses were conducted in Mplus, version 8.1 (Muthen & Muthen). Participants who did not provide data at either the 2-month or 6-month waves were younger [mean = 27.22 (SD = 4.91) compared with 29.56 (SD = 6.11), respectively; t(164) = 2.14; P = 0.04] and had lower educational attainment [mean = 3.73 (SD = 1.71) compared with 4.42 (SD = 1.91), respectively; t(164) = 1.98; P = 0.05] than the rest of the sample. There were no differences by race or ethnicity, having an intimate partner in the home, the income-to-needs ratio, or food security status. Thus, analyses were conducted with the entire analytic sample ( N = 170) using full information maximum likelihood, which takes all available data into account and minimizes the estimation bias (52). Indirect effects were estimated using bias-corrected 95% bootstrapped CIs (1000 draws) (53).
We used path analysis to test the direct and indirect associations among prenatal household FI (measured continuously), parental mental health symptomatology across the peripartum period, controlling feeding styles at 2 months, and infant food responsiveness at 6 months, while controlling for stability in food responsiveness from 2 to 6 months and any possible concurrent association between controlling feeding and food responsiveness at 2 months. Multiple fit indices were used to evaluate the model fit: the χ2 goodness-of-fit statistic, the comparative fit index (CFI), the root mean square error of approximation (RMSEA), and the standardized root mean residual (SRMR). A model has acceptable fit when the χ2 statistic is nonsignificant (P value > 0.05), CFI > 0.95, RMSEA < 0.06, and SRMR < 0.08 (54).
Based on prior research (55–60) and/or preliminary analyses, we identified covariates to include in the path analysis models. Bivariate correlations and t-tests were conducted to examine associations with or mean differences in our outcome variables (i.e., mental health symptoms, controlling feeding styles, and infant food responsiveness) by participant characteristics. Participant characteristics that were associated with an outcome variable at a P value < 0.10 were entered as covariates and specified from household FI to each outcome in the model, which included birth parent age, race and ethnicity (coded as 0 for non-Hispanic white and 1 for all others), educational attainment (a continuous measure ranging from 1 to 7), income-to-needs ratio, residing with an intimate partner (coded as 0 for no partner in home and 1 for partner in home), WIC participation (coded as 0 for WIC nonparticipant and 1 for WIC participant), and breastfeeding intensity. Infant age and exposure to the COVID-19 pandemic were not associated with our outcomes (data not shown) and, thus, were not entered as covariates.
Results
Table 1 summarizes sample characteristics and descriptive statistics for key study variables, presented for the total sample and by household food security status. Overall, the sample was relatively diverse in terms of race and ethnicity and socioeconomic status. Over half of the participating birth parents identified as members of a racial or ethnic minoritized group, 22% of participants had a high school education or less, 23% did not reside with an intimate partner, and 55% of participants reported being enrolled in WIC and receiving the program's benefits at the 2-month visit. Most infants were full term, and approximately half were female. Approximately 28% of participants reported household FI during pregnancy.
TABLE 1.
Participant demographic characteristics and descriptive statistics for primary study variables by prenatal household food security status1
| Total sample, N = 170 | Household food security status2 | P value | |||||
|---|---|---|---|---|---|---|---|
| Food insecure, n = 48 | Food secure, n = 120 | ||||||
| N | Mean ± SD or % | n | Mean ± SD or % | n | Mean ± SD or % | ||
| Parental and household characteristics | |||||||
| Age, y | 166 | 29.04 ± 5.93 | 47 | 27.15 ± 4.66 | 119 | 29.78 ± 6.23 | 0.004 |
| Parental race3,4 | <0.001 | ||||||
| White | 82 | 51.2% | 11 | 23.9% | 71 | 62.3% | |
| Black | 55 | 34.4% | 27 | 58.7% | 28 | 24.6% | |
| Other, biracial, and multiracial | 23 | 14.3% | 8 | 17.4% | 15 | 13.2% | |
| Parental ethnicity4 | 0.223 | ||||||
| Hispanic | 14 | 8.4% | 2 | 4.3% | 12 | 10.1% | |
| Non-Hispanic | 152 | 91.6% | 45 | 95.7% | 107 | 89.9% | |
| Parental education4 | 0.017 | ||||||
| ≤High school diploma or GED | 36 | 21.7% | 17 | 36.2% | 19 | 16.0% | |
| Some college | 36 | 21.7% | 12 | 25.5% | 24 | 20.2% | |
| 2-year college degree | 17 | 10.2% | 5 | 10.6% | 12 | 10.1% | |
| 4-year college degree | 35 | 21.1% | 7 | 14.9% | 28 | 23.5% | |
| Postgraduate work or degree | 42 | 25.3% | 6 | 12.8% | 36 | 30.3% | |
| Income-to-needs ratio | 161 | 3.15 ± 3.01 | 46 | 1.36 ± 1.75 | 115 | 3.86 ± 3.12 | <0.001 |
| Intimate partner in home4 | <0.001 | ||||||
| Yes | 128 | 77.1% | 27 | 57.4% | 101 | 84.9% | |
| No | 38 | 22.9% | 20 | 42.6% | 18 | 15.1% | |
| Pre-pregnancy BMI, kg/m2 | 157 | 28.35 ± 7.56 | 44 | 28.99 ± 7.82 | 112 | 27.99 ± 7.41 | 0.454 |
| WIC participation at 2 mo4 | <0.001 | ||||||
| WIC participant | 80 | 55.2% | 34 | 87.2% | 44 | 42.3% | |
| WIC nonparticipant | 65 | 44.8% | 5 | 12.8% | 60 | 57.7% | |
| Days in COVID-19 at 2 mo | 131 | 13.34 ± 42.00 | 36 | 4.14 ± 24.83 | 93 | 15.49 ± 44.65 | 0.070 |
| Days in COVID-19 at 6 mo | 142 | 86.65 ± 87.82 | 40 | 77.15 ± 83.39 | 100 | 90.07 ± 89.25 | 0.432 |
| Parental mental health5 | |||||||
| Depressive symptoms | 165 | 0.58 ± 0.39 | 47 | 0.81 ± 0.46 | 117 | 0.49 ± 0.32 | <0.001 |
| Anxiety symptoms | 168 | 1.80 ± 0.41 | 48 | 2.04 ± 0.51 | 119 | 1.71 ± 0.32 | <0.001 |
| Controlling feeding styles at 2 mo | |||||||
| Pressuring-finish | 143 | 2.14 ± 0.77 | 37 | 2.35 ± 0.76 | 105 | 2.06 ± 0.76 | 0.047 |
| Pressuring-cereal | 144 | 1.75 ± 0.83 | 37 | 1.95 ± 0.96 | 106 | 1.68 ± 0.78 | 0.089 |
| Pressuring-soothe | 144 | 2.70 ± 0.72 | 37 | 2.72 ± 0.73 | 106 | 2.69 ± 0.71 | 0.834 |
| Restrictive-amount | 144 | 2.91 ± 0.99 | 37 | 3.17 ± 0.9) | 106 | 2.81 ± 0.99 | 0.058 |
| Restrictive-diet quality | 142 | 3.41 ± 0.84 | 37 | 3.29 ± 0.82 | 104 | 3.45 ± 0.85 | 0.317 |
| Infant characteristics | |||||||
| Infant sex | 0.960 | ||||||
| Male | 82 | 50.3% | 23 | 50.0% | 58 | 50.4% | |
| Female | 81 | 49.7% | 23 | 50.0% | 57 | 49.6% | |
| Infant gestational age, wk | 163 | 39.37 ± 1.23 | 46 | 39.25 ± 1.25 | 115 | 39.42 ± 1.24 | 0.419 |
| Infant birth weight, kg | 163 | 3.35 ± 0.48 | 46 | 3.34 ± 0.46 | 115 | 3.35 ± 0.49 | 0.954 |
| Breastfeeding intensity at 2 mo | 145 | 0.63 ± 0.42 | 39 | 0.56 ± 0.40 | 104 | 0.68 ± 0.43 | 0.181 |
| Infant food responsiveness at 2 mo | 146 | 2.72 ± 0.77 | 37 | 2.90 ± 0.77 | 108 | 2.65 ± 0.75 | 0.080 |
| Infant food responsiveness at 6 mo | 142 | 2.35 ± 0.73 | 43 | 2.58 ± 0.65 | 98 | 2.25 ± 0.74 | 0.012 |
Values are means ± SDs for continuous variables and percentages of participants for categorical variables. P values were obtained from t-tests to compare differences by food security status for continuous variables and from χ2 tests for categorical variables. Abbreviation: COVID-19, coronavirus disease 2019; GED, general education diploma; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Households were classified as food insecure if 2 or more of the 6 items from the Household Food Security Short Form were answered affirmatively and food secure if fewer than 2 of the 6 items were answered affirmatively.
The biracial, multiracial, and other group was comprised of participants that identified as biracial (n = 12), multiracial (n = 4), Asian (n = 1), American Indian or Alaskan Native (n = 1), and other (n = 5).
Race and ethnicity (coded as 0 for non-Hispanic white and 1 for all others), residing with an intimate partner (coded as 0 for no partner in home and 1 for partner in home), and WIC participation (coded as 0 for WIC nonparticipant and 1 for WIC participant) were dichotomized; educational attainment (ranging from 1 for some high school to 7 for graduate degree) and food insecurity (ranging from 1 to 6) were measured continuously.
Depressive and anxiety symptoms assessed at the prenatal and 2-month waves were averaged to create a composite of parental mental health symptomatology across the peripartum period.
Bivariate correlations among covariates and primary study variables are presented in Table 2. Household FI was associated with greater parental mental health symptoms and higher infant food responsiveness and was marginally positively associated with both pressuring-finish and pressuring-cereal scores. Greater parental mental health symptoms were associated with higher pressuring-finish, pressuring-cereal, and restrictive-amount scores, and were marginally associated with pressuring-soothe scores. Pressuring-finish, pressuring-cereal, and restrictive-amount scores were all associated with infant food responsiveness. Given pressuring-finish, pressuring-cereal, and restrictive-amount scores were associated with both parental mental health symptoms and infant food responsiveness, we conducted a separate path analysis for each controlling feeding subscale that examined the indirect effect of household FI on infant food responsiveness through parental mental health and subsequent controlling feeding. In the covariate-adjusted path analysis models, pressuring-finish was the only controlling feeding subscale associated with food responsiveness; thus, the results from the models with pressuring-cereal, pressuring-soothe, and restrictive-amount subscales are not presented.
TABLE 2.
Zero-order correlations among participant demographic characteristics and primary study variables1
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Parental age | 1.00 | — | — | — | — | — | — | — | — | — | — | — | — | — | — |
| 2. Race and ethnicity | −0.252 | 1.00 | — | — | — | — | — | — | — | — | — | — | — | — | — |
| 3. Educational attainment | 0.482 | −0.442 | 1.00 | — | — | — | — | — | — | — | — | — | — | — | — |
| 4. Income-to-needs ratio | 0.322 | −0.442 | 0.612 | 1.00 | — | — | — | — | — | — | — | — | — | — | — |
| 5. Residing with an intimate partner | 0.302 | −0.382 | 0.312 | 0.322 | 1.00 | — | — | — | — | — | — | — | — | — | — |
| 6. Breastfeeding intensity at 2 mo | 0.153 | −0.282 | 0.362 | 0.292 | 0.182 | 1.00 | — | — | — | — | — | — | — | — | — |
| 7. WIC participation at 2 mo | −0.392 | 0.622 | −0.642 | −0.672 | −0.402 | −0.352 | 1.00 | — | — | — | — | — | — | — | — |
| 8. Prenatal food insecurity | −0.222 | 0.232 | −0.282 | −0.352 | −0.222 | −0.11 | 0.452 | 1.00 | — | — | — | — | — | — | — |
| 9. Parental mental health symptoms | −0.162 | 0.162 | −0.212 | −0.242 | −0.02 | −0.153 | 0.143 | 0.492 | 1.00 | — | — | — | — | — | — |
| 10. Pressuring-finish | −0.09 | 0.212 | −0.143 | −0.09 | −0.163 | −0.202 | 0.10 | 0.153 | 0.312 | 1.00 | — | — | — | — | — |
| 11. Pressuring-cereal | −0.182 | 0.432 | −0.25 | −0.252 | −0.272 | −0.292 | 0.252 | 0.163 | 0.222 | 0.332 | 1.00 | — | — | — | — |
| 12. Pressuring-soothe | 0.06 | −0.12 | 0.06 | 0.03 | −0.05 | −0.00 | 0.00 | 0.05 | 0.153 | 0.172 | 0.09 | 1.00 | — | — | — |
| 13. Restrictive-amount | −0.222 | 0.442 | −0.242 | −0.252 | −0.222 | −0.412 | 0.302 | 0.06 | 0.202 | 0.452 | 0.372 | 0.01 | 1.00 | — | — |
| 14. Restrictive-diet quality | 0.07 | −0.12 | 0.06 | 0.143 | 0.05 | 0.10 | −0.01 | −0.07 | −0.07 | −0.02 | −0.202 | 0.10 | −0.06 | 1.00 | — |
| 15. Food responsiveness at 2 mo | −0.14 | 0.12 | −0.13 | −0.143 | −0.02 | −0.05 | 0.153 | 0.242 | 0.272 | 0.212 | 0.172 | 0.192 | 0.172 | −0.02 | 1.00 |
| 16. Food responsiveness at 6 mo | −0.252 | 0.272 | −0.312 | −0.312 | −0.222 | −0.10 | 0.252 | 0.262 | 0.162 | 0.282 | 0.222 | 0.00 | 0.182 | −0.00 | 0.342 |
Race and ethnicity (coded as 0 for non-Hispanic white and 1 for all others), residing with an intimate partner (coded as 0 for no partner in home and 1 for partner in home), and WIC participation (coded as 0 for WIC nonparticipant and 1 for WIC participant) were dichotomized. Educational attainment (ranging from 1 for some high school to 7 for graduate degree) and food insecurity (ranging from 1 to 6) were measured continuously. Depressive and anxiety symptoms assessed at the prenatal and 2-month waves were averaged to create a composite of parental mental health symptomatology across the peripartum period. Abbreviation: WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
P < 0.05.
P < 0.10.
Results for the path analysis testing the indirect effects of prenatal FI on infant food responsiveness via parental mental health symptoms and pressuring-finish scores are shown in Figure 1. The path model fit the data well [χ2 (10) = 12.67; P = 0.24; CFI = 0.98; RMSEA = 0.04; SRMR = 0.04]. Adjusting for covariates, 3 statistically significant indirect effects of prenatal household FI were observed. First, there was an indirect effect from prenatal household FI to pressuring-finish scores at 2 months that operated through parental mental health symptoms (b = 0.07; 95% CI: 0.02, 0.13). Second, household FI was indirectly associated with infant food responsiveness at 6 months through parental mental health symptoms and pressuring-finish scores (b = 0.01; 95% CI: 0.001, 0.025). Specifically, prenatal household FI was associated with greater mental health symptoms during the peripartum period (β = 0.54; P < 0.001), which in turn was positively associated with higher pressuring-finish scores at 2 months (β = 0.29; P = 0.01) and higher infant food responsiveness at 6 months (β = 0.17; P = 0.04). Third, household FI was indirectly associated with infant food responsiveness at 6 months through parental mental health symptoms, pressuring-finish scores at 2 months, and infant food responsiveness at 2 months (b = 0.003; 95% CI: 0.000, 0.010). Household FI was not directly associated with 2-month pressuring-finish scores or 6-month infant food responsiveness. The final model predicted 33% of the variability in mental health symptoms (95% CI: 0.186, 0.468), 16% of the variability in pressuring-finish scores at 2 months (95% CI: 0.044, 0.268), and 25% of the variability in infant food responsiveness at 6 months (95% CI: 0.115, 0.377).
FIGURE 1.
Path analysis with bootstrapped CIs showing the roles of parental mental health symptomatology during the peripartum period and pressuring-finish at 2 months as pathways linking prenatal household FI and infant food responsiveness at 6 months (n = 170), while controlling for stability in food responsiveness from 2 to 6 months and any possible concurrent association between controlling feeding and food responsiveness at 2 months. FI was measured continuously (ranging from 1 to 6), such that higher scores reflect more severe FI. Covariates specified from household FI to all 3 outcomes (i.e., parental mental health symptomatology, pressuring-finish, infant food responsiveness) included birth parent age, race and ethnicity (coded as 0 for non-Hispanic white and 1 for all others), educational attainment (ranging from 1 for some high school to 7 for graduate degree), income-to-needs ratio, residing with an intimate partner (coded as 0 for no partner in home and 1 for partner in home), WIC participation (coded as 0 for WIC nonparticipant and 1 for WIC participant), and breastfeeding intensity. The final model predicted 33% of the variability in mental health symptoms (95% CI: 0.186, 0.468), 16% of the variability in pressuring-finish at 2 months (95% CI: 0.044, 0.268), and 25% of the variability in infant food responsiveness at 6 months (95% CI: 0.115, 0.377). *P < 0.05; **P < 0.01; ***P < 0.001. Abbreviations: FI, food insecurity; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Discussion
This longitudinal study tested direct and indirect associations among prenatal FI, parental controlling feeding styles, and infant food responsiveness in a community-based sample of birth parents and their infants. Our findings indicate that FI during pregnancy was indirectly associated with higher infant food responsiveness at the infant age of 6 months through greater parental mental health symptomatology across the peripartum period and higher pressuring to finish at the infant age of 2 months, a period of exclusive milk feeding. Pressuring to finish is considered a parent-centered feeding style that is intended to increase the amount of milk an infant consumes, regardless of infant hunger and fullness (40). Our study extends prior research related to the influence of FI on children's appetitive behaviors in 2 significant ways. First, the current study provides findings from a community sample of infants that is relatively diverse in terms of race and ethnicity and socioeconomic status, thus extending previous research that has focused on homogeneous samples that are predominantly low-income (16–18, 20), non-Hispanic white (17), or Hispanic (16, 18, 19). Second, the results provide evidence for potential pathways by which FI may contribute to increased infant appetitive drive during a key developmental period when adaptive self-regulatory mechanisms related to food intake and infant growth begin to develop (9).
As hypothesized, household prenatal FI was indirectly associated with higher infant food responsiveness at 6 months, controlling for relevant parental and family sociodemographic characteristics. Specifically, more severe prenatal FI was associated with higher infant food responsiveness via greater parental mental health symptomatology and subsequent higher use of pressure to finish. The hypothesized direct effect of prenatal FI on controlling feeding and infant food responsiveness was not supported. In contrast, 2 prior cross-sectional studies with low-income preschool-age children showed a direct link between food security status and child food responsiveness (16, 17). One study reported higher ratings of food responsiveness among children in food insecure compared to food secure households, whereas another study observed differences in food responsiveness by child food security status (i.e., higher food responsiveness among children directly impacted by FI). Differences in study design could explain why we did not detect a direct association between prenatal FI and food responsiveness at the infant age of 6 months. We did not assess FI postnatally; thus, it is unclear whether FI is concurrently associated with food responsiveness during infancy. It is also possible that we did not observe a unique direct effect of FI on infant food responsiveness given our analyses included indirect pathways, such as parental mental health and controlling feeding, which is another key difference from prior research. Further, prenatal FI may only be associated with pressuring feeding styles when FI is a chronic issue and experienced both prenatally and during infancy. For example, Gross and colleagues (19) showed that prolonged food insecurity (assessed prenatally and postnatally at 10 months), but not prenatal FI alone, was associated with greater pressuring feeding at the infant age of 10 months. Our findings suggest that in utero exposure to household FI may not contribute directly to the developmental programming of infant food responsiveness. Instead, it appears that environmental factors in the early caregiving environment (i.e., parental mental health and pressuring feeding) that result from FI during pregnancy may help shape individual differences in infant food responsiveness. Importantly, further studies are needed to confirm our findings.
Inconsistent with our hypotheses, prenatal household FI was not directly associated with pressuring or restrictive feeding styles. The null associations are contrary to prior research demonstrating positive associations between FI and controlling feeding among infants and children (18–20, 61), but are in line with other studies in preschool and school-aged children (16, 62, 63). A study by Gross and colleagues (18) demonstrated that food insecure mothers reported higher pressuring and restrictive feeding style scores compared to food secure mothers when infants were 2 weeks to 6 months old. As compared to the current study, which examined feeding style subscales available in the IFSQ (e.g., pressuring-finish), Gross and colleagues (18) assessed more global feeding styles that asked about the mother's perceived need to ensure their infant does not eat too much (i.e., restrictive) or too little (i.e., pressuring). Gross and colleagues (18) also showed that a mother's concern over their infant becoming overweight mediated the associations between FI and global pressuring and restrictive feeding. It is possible that FI during infancy may have predicted concern or anxiety over an infant eating an appropriate amount, rather than predicting restriction and pressure per se.
Another study conducted by Gross and colleagues (19) reported an association between prenatal FI and 2 pressuring feeding style subscales: pressuring to soothe and pressuring with cereal. However, in their analyses that adjusted for prenatal depression, the association between prenatal FI and pressuring was no longer statistically significant. This finding may suggest that parental depressive and anxiety symptoms have indirect paths in this relationship, which is what we observed in our sample: prenatal FI was associated with pressuring to finish through heightened parental mental health symptomatology (i.e., depressive and anxiety symptoms). This finding extends previous research during infancy demonstrating an effect of FI on child outcomes via parental depression and parenting practices (64). To our knowledge, this is the first study to explicitly test mental health symptomatology as a pathway linking prenatal FI and controlling feeding styles, which fills an important gap in the literature (26).
In contrast to a study that assessed feeding styles when infants were 18 months old (19), results from the current study did not demonstrate an association between prenatal FI and pressuring to soothe or pressuring with cereal in early infancy. Pressuring to soothe and pressuring with cereal may be more salient in later infancy. For example, parental use of food to soothe infant distress has been shown to increase across infancy (65), and pressuring with cereal likely becomes more prevalent as breastfeeding rates decline, bottle feeding increases, and infants begin to consume solid foods on a regular basis. Pressuring to finish specifically focuses on encouraging infants to consume or finish milk or food, regardless of infant hunger and satiety cues. The period of exclusive milk feeding in early infancy presents a developmental period in which parents may be particularly susceptible to adopting a feeding style marked by pressuring to finish. Within the first few months of life, infant hunger and satiety cues tend to be less clear (66), and parents are able to exert more control over the feeding interaction. Parents that experienced FI during pregnancy may also be particularly concerned about whether their infant is getting enough to eat (67). Although pressuring is more commonly reported among mothers who perceive their infant as underweight (68, 69), parents' perceptions of their child's weight status are often inaccurate (70) and parents of infants are typically more concerned about underweight than overweight (68, 71). Heightened mental health symptomatology associated with FI may amplify both the motivation to not waste energetic resources when food is available (18) and concern for infant growth and development, thus manifesting as pressuring to eat beyond infant fullness.
Study findings should be interpreted with caution given several noteworthy limitations. First, FI was only measured once during the prenatal period, and the measure of FI used in this study does not distinguish between household compared with child FI or account for potential fluctuations in household FI, both of which could have limited our ability to detect statistically significant, direct effects of FI. Second, we did not measure parental perceptions of infant weight status (e.g., over- or underweight), which could be impacted by prenatal FI and could have an influence on parental feeding styles. Additionally, this study utilized parent report measures that are subject to social desirability biases and other perceptions that can be shaped by a variety of cognitions and emotions. However, the measures of feeding styles and infant food responsiveness utilized in the current study are well validated, are commonly used (12, 40), and provide an assessment of typical behavior across various situations, as opposed to observations that mark a single context at 1 point in time (72).
Strengths of the study include our measure of FI, which asked participants to report on their experience of FI during pregnancy as opposed to the preceding 12 months more generally. Further, FI was measured on a continuous linear scale, which allows for a better understanding of the increasing severity of FI and may be a more sensitive measure in diverse samples that, on average, are not high risk. Additionally, we adjusted for multiple covariates, including indicators of socioeconomic status (i.e., income-to-needs ratio, educational attainment), which have been shown to inversely predict infant food responsiveness from 16 months to 5 years (57). Finally, the study findings related to indirect effects add to the existing literature that lacks longitudinal research examining potential explanatory pathways by which FI influences parenting and child outcomes (10, 26).
Our findings highlight several directions for future research. First, observational data on parent feeding and infant appetitive behaviors is needed to clarify and expand upon the present findings. Given the current study did not assess parent perceptions of infant weight, future work should examine whether FI contributes to parental misperceptions of infant weight status and whether such perceptions contribute to controlling feeding styles. Future studies that include perceived infant weight status could include this potentially important factor as a covariate or another possible explanatory pathway. Further, there are likely additional pathways by which prenatal FI influences infant food responsiveness; thus, research is warranted to test other mechanisms, including biological factors that could have a developmental programming effect on later food responsiveness, such as hormonal risk during pregnancy. In addition to the need for research that examines how changes in FI across the prenatal and postpartum periods impact later infant food responsiveness, future studies might also collect repeated measures (e.g., ecological momentary assessments) of FI to capture temporal fluctuations in the severity of FI that may coincide with the distribution of federal assistance program benefits and/or employer payments. Following this cohort longitudinally through the child's first 2 years will help to determine how the pathways elucidated in the current study contribute to child weight outcomes.
The current study examined direct and indirect associations among prenatal FI, parental mental health symptomatology during the peripartum period, controlling feeding styles (restrictive and pressuring) at the infant age of 2 months, and food responsiveness at the infant age of 6 months. Results showed that prenatal FI was indirectly associated with greater pressuring to finish through increased mental health symptomatology and that greater use of pressuring to finish, in turn, predicted higher infant food responsiveness. Using longitudinal data from a community-based sample, we address several gaps in the literature on negative outcomes related to the experience of FI during pregnancy, a vulnerable time for both parent and child health. Interventions that target parent feeding should 1) work to move beyond individual behavior change strategies that often focus solely on the parent (73); and 2) consider the context of food insecurity and the broader sociopolitical environment, especially when working with socially and economically disadvantaged populations most impacted by FI (74). In addition to policy initiatives that ensure adequate, reliable access to nutritious food during pregnancy, screening and referrals for elevated depressive and anxiety symptoms in the peripartum period are warranted. Given the frequency of well-child visits during infancy, pediatricians are also well positioned to support child-centered, noncontrolling feeding by discussing healthy infant growth and having an open, culturally competent dialogue with parents around feeding concerns that is sensitive to the needs and health beliefs of the family (75).
Acknowledgements
We thank the participating families for their time and our research team, led by Megan Chandler, for their dedication to data collection efforts. The authors’ responsibilities were as follows – EML, CB, LHS, LW: contributed to the design and measurement approaches used in the Infant Growth and Development Study (iGrow) study; SGE: conducted the primary analyses and drafted the manuscript; and all authors: contributed to the conceptualization of the manuscript and read and approved the final manuscript.
Notes
This study was supported by R01HD093662 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. SGE was supported by postdoctoral fellowship (T32-HD07376) through the Frank Porter Graham Child Development Institute, University of North Carolina at Chapel Hill.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development or the National Institutes of Health. All authors report no conflicts of interest.
Abbreviations used: BEBQ, Baby Eating Behavior Questionnaire; CFI, comparative fit index; COVID-19, coronavirus disease 2019; FI, food insecurity; IFSQ, Infant Feeding Styles Questionnaire; RMSEA, root mean square error of approximation; SRMR, standardized root mean residual; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Contributor Information
Sally G Eagleton, Human Development and Family Studies, University of North Carolina Greensboro, Greensboro, NC, USA.
Lenka H Shriver, Department of Nutrition, University of North Carolina Greensboro, Greensboro, NC, USA.
Cheryl Buehler, Human Development and Family Studies, University of North Carolina Greensboro, Greensboro, NC, USA.
Laurie Wideman, Department of Kinesiology, University of North Carolina Greensboro, Greensboro, NC, USA.
Esther M Leerkes, Human Development and Family Studies, University of North Carolina Greensboro, Greensboro, NC, USA.
Data Availability
Data described in the article, code book, and analytic code will be made available upon request.
References
- 1. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food insecurity in the United States in 2019. US Department of Agriculture, Economic Research Service; 2020. [Google Scholar]
- 2. Borders AEB, Grobman WA, Amsden LB, Holl JL. Chronic stress and low birth weight neonates in a low-income population of women. Obstet Gynecol. 2007;109(2, Part 1):331–8. [DOI] [PubMed] [Google Scholar]
- 3. Laraia BA, Siega-Riz AM, Gundersen C. Household food insecurity is associated with self-reported pregravid weight status, gestational weight gain, and pregnancy complications. J Am Diet Assoc. 2010;110(5):692–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Drennen CR, Coleman SM, Ettinger de Cuba S, Frank DA, Chilton M, Cook JTet al. Food insecurity, health, and development in children under age four years. Pediatrics. 2019;144(4):e20190824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Johnson AD, Markowitz AJ. Associations between household food insecurity in early childhood and children's kindergarten skills. Child Dev. 2018;89(2):e1–e17. [DOI] [PubMed] [Google Scholar]
- 6. Eisenmann JC, Gundersen C, Lohman BJ, Garasky S, Stewart SD. Is food insecurity related to overweight and obesity in children and adolescents? A summary of studies, 1995–2009. Obes Rev. 2011;12(5):e73–83. [DOI] [PubMed] [Google Scholar]
- 7. Larson NI, Story MT. Food insecurity and weight status among U.S. children and families: A review of the literature. Am J Prev Med. 2011;40(2):166–73. [DOI] [PubMed] [Google Scholar]
- 8. Benjamin-Neelon SE, Allen C, Neelon B. Household food security and infant adiposity. Pediatrics. 2020;146(3):e20193725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lillycrop KA, Burdge GC. Epigenetic changes in early life and future risk of obesity. Int J Obes. 2011;35(1):72–83. [DOI] [PubMed] [Google Scholar]
- 10. Brown AGM, Esposito LE, Fisher RA, Nicastro HL, Tabor DC, Walker JR. Food insecurity and obesity: Research gaps, opportunities, and challenges. Transl Behav Med. 2019;9(5):980–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gross RS, Mendelsohn AL. Food insecurity during early childhood: Marker for disparities in healthy growth and development. Pediatrics. 2019;144(4):e20192430. [DOI] [PubMed] [Google Scholar]
- 12. Llewellyn CH, van Jaarsveld CH, Johnson L, Carnell S, Wardle J. Development and factor structure of the Baby Eating Behaviour Questionnaire in the Gemini birth cohort. Appetite. 2011;57(2):388–96. [DOI] [PubMed] [Google Scholar]
- 13. van Jaarsveld CH, Llewellyn CH, Johnson L, Wardle J. Prospective associations between appetitive traits and weight gain in infancy. Am J Clin Nutr. 2011;94(6):1562–7. [DOI] [PubMed] [Google Scholar]
- 14. van Jaarsveld CH, Boniface D, Llewellyn CH, Wardle J. Appetite and growth: A longitudinal sibling analysis. JAMA Pediatrics. 2014;168(4):345–50. [DOI] [PubMed] [Google Scholar]
- 15. Quah PL, Chan YH, Aris IM, Pang WW, Toh JY, Tint MTet al. Prospective associations of appetitive traits at 3 and 12 months of age with body mass index and weight gain in the first 2 years of life. BMC Pediatr. 2015;15(1):153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McCurdy K, Gans KM, Risica PM, Fox K, Tovar A. Food insecurity, food parenting practices, and child eating behaviors among low-income Hispanic families of young children. Appetite. 2022;169:105857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Eagleton SG, Na M, Savage JS. Food insecurity is associated with higher food responsiveness in low-income children: The moderating role of parent stress and family functioning. Pediatr Obes. 2022;17(1):e12837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gross RS, Mendelsohn AL, Fierman AH, Racine AD, Messito MJ. Food insecurity and obesogenic maternal infant feeding styles and practices in low-income families. Pediatrics. 2012;130(2):254–61. [DOI] [PubMed] [Google Scholar]
- 19. Gross RS, Mendelsohn AL, Messito MJ. Additive effects of household food insecurity during pregnancy and infancy on maternal infant feeding styles and practices. Appetite. 2018;130:20–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Orr CJ, Ben-Davies M, Ravanbakht SN, Yin HS, Sanders LM, Rothman RLet al. Parental feeding beliefs and practices and household food insecurity in infancy. Acad Pediatr. 2019;19(1):80–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Steinsbekk S, Belsky J, Wichstrom L. Parental feeding and child eating: An investigation of reciprocal effects. Child Dev. 2016;87(5):1538–49. [DOI] [PubMed] [Google Scholar]
- 22. Jansen PW, Roza SJ, Jaddoe VWV, Mackenbach JD, Raat H, Hofman Aet al. Children's eating behavior, feeding practices of parents and weight problems in early childhood: Results from the population-based Generation R Study. Int J Behav Nutr Phys Act. 2012;9:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Leung CW, Epel ES, Willett WC, Rimm EB, Laraia BA. Household food insecurity is positively associated with depression among low-income supplemental nutrition assistance program participants and income-eligible nonparticipants. J Nutr. 2015;145(3):622–7. [DOI] [PubMed] [Google Scholar]
- 24. Laraia B, Vinikoor-Imler LC, Siega-Riz AM. Food insecurity during pregnancy leads to stress, disordered eating, and greater postpartum weight among overweight women. Obesity (Silver Spring). 2015;23(6):1303–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. McCurdy K, Gorman KS, Metallinos-Katsaras E. From poverty to food insecurity and child overweight: A family stress approach. Child Dev Perspect. 2010;4(2):144–51. [Google Scholar]
- 26. Arlinghaus KR, Laska MN. Parent feeding practices in the context of food insecurity. Int J Environ Res Public Health. 2021;18(2):366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Farrow CV, Blissett J. Is maternal psychopathology related to obesogenic feeding practices at 1 year?. Obes Res. 2005;13(11):1999–2005. [DOI] [PubMed] [Google Scholar]
- 28. Hurley KM, Black MM, Papas MA, Caufield LE. Maternal symptoms of stress, depression, and anxiety are related to nonresponsive feeding styles in a statewide sample of WIC participants. J Nutr. 2008;138(4):799–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Goulding AN, Rosenblum KL, Miller AL, Peterson KE, Chen Y-P, Kaciroti Net al. Associations between maternal depressive symptoms and child feeding practices in a cross-sectional study of low-income mothers and their children. Int J Behav Nutr Phys Act. 2014;11(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Francis LA, Hofer SM, Birch LL. Predictors of maternal child-feeding style: Maternal and child characteristics. Appetite. 2001;37(3):231–43. [DOI] [PubMed] [Google Scholar]
- 31. Haycraft E, Farrow C, Blissett J. Maternal symptoms of depression are related to observations of controlling feeding practices in mothers of young children. J Fam Psychol. 2013;27(1):159. [DOI] [PubMed] [Google Scholar]
- 32. Berge JM, Fertig AR, Trofholz A, Neumark-Sztainer D, Rogers E, Loth K. Associations between parental stress, parent feeding practices, and child eating behaviors within the context of food insecurity. Prev Med Rep. 2020;19:101146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Leerkes EM, Buehler C, Calkins SD, Shriver LH, Wideman L. Protocol for iGrow (Infant Growth and Development Study): Biopsychosocial predictors of childhood obesity risk at 2 years. BMC Public Health. 2020;20(1):1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Blumberg SJ, Bialostosky K, Hamilton WL, Briefel RR. The effectiveness of a short form of the Household Food Security Scale. Am J Public Health. 1999;89(8):1231–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to measuring household food security, revised 2000. Alexandria, VA: US Department of Agriculture, Food and Nutrition Service; 2000. [Google Scholar]
- 36. Armstrong B, Hepworth AD, Black MM. Hunger in the household: Food insecurity and associations with maternal eating and toddler feeding. Pediatr Obes. 2020;15(10):e12637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Loopstra R, Tarasuk V. What does increasing severity of food insecurity indicate for food insecure families? Relationships between severity of food insecurity and indicators of material hardship and constrained food purchasing. J Hunger Environ Nutr. 2013;8(3):337–49. [Google Scholar]
- 38. Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 39. Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 40. Thompson AL, Mendez MA, Borja JB, Adair LS, Zimmer CR, Bentley ME. Development and validation of the Infant Feeding Style Questionnaire. Appetite. 2009;53(2):210–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. DiSantis KI, Hodges EA, Fisher JO. The association of breastfeeding duration with later maternal feeding styles in infancy and toddlerhood: A cross-sectional analysis. Int J Behav Nutr Phys Act. 2013;10:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Benjamin-Neelon SE, Neelon B. Associations between maternal and paternal feeding styles of infants in a racially diverse US birth cohort. Pediatr Obes. 2020;15(10):e12712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ventura AK, Pollack Golen R. A pilot study comparing opaque, weighted bottles with conventional, clear bottles for infant feeding. Appetite. 2015;85:178–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hupp MK, Papathakis PC, Phelan S, Ventura AK. Associations between mothers' use of food to soothe, feeding mode, and infant weight during early infancy. Appetite. 2022;168:105736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Shriver LH, Eagleton SG, Lawless MC, Buehler C, Wideman L, Leerkes EM. Infant appetite and weight gain in early infancy: Moderating effects of controlling feeding styles. Appetite. 2022;176:106139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Shepard DN, Chandler-Laney PC. Prospective associations of eating behaviors with weight gain in infants. Obesity (Silver Spring). 2015;23(9):1881–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Patel N, Godfrey KM, Pasupathy D, Levin J, Flynn AC, Hayes Let al. Infant adiposity following a randomised controlled trial of a behavioural intervention in obese pregnancy. Int J Obes. 2017;41(7):1018–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Harris HA, Moore AM, Ruggiero CF, Bailey-Davis L, Savage JS. Infant food responsiveness in the context of temperament and mothers' use of food to soothe. Front Nutr. 2022;8:1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. US Census Bureau . Poverty thresholds [Internet]. Washington, DC: US Census Bureau; 2022. Available from: https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html [Google Scholar]
- 50. Fein SB, Labiner-Wolfe J, Shealy KR, Li R, Chen J, Grummer-Strawn LM. Infant feeding practices study II: Study methods. Pediatrics. 2008;122(Suppl 2):S28–35. [DOI] [PubMed] [Google Scholar]
- 51. Li R, Fein SB, Grummer-Strawn LM. Association of breastfeeding intensity and bottle-emptying behaviors at early infancy with infants' risk for excess weight at late infancy. Pediatrics. 2008;122(Suppl 2):S77–84. [DOI] [PubMed] [Google Scholar]
- 52. Acock AC. Working with missing values. J Marriage Fam. 2005;67(4):1012–28. [Google Scholar]
- 53. Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–31. [DOI] [PubMed] [Google Scholar]
- 54. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55. [Google Scholar]
- 55. Ventura AK, Teitelbaum S. Maternal distraction during breast- and bottle feeding among WIC and non-WIC mothers. J Nutr Educ Behav. 2017;49(7):S169–76..e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Barrett KJ, Thompson AL, Bentley ME. The influence of maternal psychosocial characteristics on infant feeding styles. Appetite. 2016;103:396–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kininmonth AR, Smith AD, Llewellyn CH, Fildes A. Socioeconomic status and changes in appetite from toddlerhood to early childhood. Appetite. 2020;146:104517. [DOI] [PubMed] [Google Scholar]
- 58. Wehrly SE, Bonilla C, Perez M, Liew J. Controlling parental feeding practices and child body composition in ethnically and economically diverse preschool children. Appetite. 2014;73:163–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Taveras EM, Scanlon KS, Birch L, Rifas-Shiman SL, Rich-Edwards JW, Gillman MW. Association of breastfeeding with maternal control of infant feeding at age 1 year. Pediatrics. 2004;114(5):e577–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kolko RP, Salk RH, Sweeny GM, Marcus MD, Levine MD. Mothers' loss of control over eating during pregnancy in relation to their infants' appetitive traits. Appetite. 2018;120:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Adams EL, Caccavale LJ, Smith D, Bean MK. Food insecurity, the home food environment, and parent feeding practices in the era of COVID-19. Obesity (Silver Spring). 2020;28(11):2056–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Feinberg E, Kavanagh PL, Young RL, Prudent N. Food insecurity and compensatory feeding practices among urban black families. Pediatrics. 2008;122(4):e854–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Matheson DM, Varady J, Varady A, Killen JD. Household food security and nutritional status of Hispanic children in the fifth grade. Am J Clin Nutr. 2002;76(1):210–17. [DOI] [PubMed] [Google Scholar]
- 64. Bronte-Tinkew J, Zaslow M, Capps R, Horowitz A, McNamara M. Food insecurity works through depression, parenting, and infant feeding to influence overweight and health in toddlers. J Nutr. 2007;137(9):2160–5. [DOI] [PubMed] [Google Scholar]
- 65. Stifter CA, Moding KJ. Understanding and measuring parent use of food to soothe infant and toddler distress: A longitudinal study from 6 to 18 months of age. Appetite. 2015;95:188–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. DiSantis KI, Hodges EA, Johnson SL, Fisher JO. The role of responsive feeding in overweight during infancy and toddlerhood: A systematic review. Int J Obes. 2011;35(4):480–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Gross RS, Mendelsohn AL, Gross MB, Scheinmann R, Messito MJ. Material hardship and internal locus of control over the prevention of child obesity in low-income Hispanic pregnant women. Acad Pediatr. 2016;16(5):468–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Harrison M, Brodribb W, Davies PSW, Hepworth J. Impact of maternal infant weight perception on infant feeding and dietary intake. Matern Child Health J. 2018;22(8):1135–45. [DOI] [PubMed] [Google Scholar]
- 69. Gross RS, Mendelsohn AL, Fierman AH, Messito MJ. Maternal controlling feeding styles during early infancy. Clin Pediatr (Phila). 2011;50(12):1125–33. [DOI] [PubMed] [Google Scholar]
- 70. Lundahl A, Kidwell KM, Nelson TD. Parental underestimates of child weight: A meta-analysis. Pediatrics. 2014;133(3):e689–703. [DOI] [PubMed] [Google Scholar]
- 71. Laraway KA, Birch LL, Shaffer ML, Paul IM. Parent perception of healthy infant and toddler growth. Clin Pediatr (Phila). 2010;49(4):343–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Gardner F. Methodological issues in the direct observation of parent-child interaction: Do observational findings reflect the natural behavior of participants?. Clin Child Fam Psychol Rev. 2000;3(3):185–98. [DOI] [PubMed] [Google Scholar]
- 73. Baxter KA, Nambiar S, So THJ, Gallegos D, Byrne R. Parental feeding practices in families experiencing food insecurity: A scoping review. Int J Environ Res Public Health. 2022;19(9):5604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Kumanyika S. Nutrition and chronic disease prevention: Priorities for US minority groups. Nutr Rev. 2006;64(2):9–14. [DOI] [PubMed] [Google Scholar]
- 75. Cheng TL, Emmanuel MA, Levy DJ, Jenkins RR. Child health disparities: What can a clinician do?. Pediatrics. 2015;136(5):961–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data described in the article, code book, and analytic code will be made available upon request.