Abstract
Background
In contrast to adults, the situation for pediatric trauma care from an international point of view and the global management of severely injured children remain rather unclear. The current study investigates structural management of pediatric trauma in centers of different trauma levels as well as experiences with pediatric trauma management around the world.
Methods
A web-survey had been distributed to the global mailing list of the World Society of Emergency Surgery from 10/2021–03/2022, investigating characteristics of respondents and affiliated hospitals, case-load of pediatric trauma patients, capacities and infrastructure for critical care in children, trauma team composition, clinical work-up and individual experiences with pediatric trauma management in response to patients´ age. The collaboration group was subdivided regarding sizes of affiliated hospitals to allow comparisons concerning hospital volumes. Comparable results were conducted to statistical analysis.
Results
A total of 133 participants from 34 countries, i.e. 5 continents responded to the survey. They were most commonly affiliated with larger hospitals (> 500 beds in 72.9%) and with level I or II trauma centers (82.0%), respectively. 74.4% of hospitals offer unrestricted pediatric medical care, but only 63.2% and 42.9% of the participants had sufficient experiences with trauma care in children ≤ 10 and ≤ 5 years of age (p = 0.0014). This situation is aggravated in participants from smaller hospitals (p < 0.01). With regard to hospital size (≤ 500 versus > 500 in-hospital beds), larger hospitals were more likely affiliated with advanced trauma centers, more elaborated pediatric intensive care infrastructure (p < 0.0001), treated children at all ages more frequently (p = 0.0938) and have higher case-loads of severely injured children < 12 years of age (p = 0.0009). Therefore, the majority of larger hospitals reserve either pediatric surgery departments or board-certified pediatric surgeons (p < 0.0001) and in-hospital trauma management is conducted more multi-disciplinarily. However, the majority of respondents does not feel prepared for treatment of severe pediatric trauma and call for special educational and practical training courses (overall: 80.2% and 64.3%, respectively).
Conclusions
Multi-professional management of pediatric trauma and individual experiences with severely injured children depend on volumes, level of trauma centers and infrastructure of the hospital. However, respondents from hospitals at all levels of trauma care complain about an alarming lack of knowledge on pediatric trauma management.
Supplementary information
The online version contains supplementary material available at 10.1186/s13017-022-00473-5.
Keywords: Emergency surgery, Trauma surgery, Emergency, Appendicitis, WSES, Pediatric surgery, Children, Injury, Pediatric trauma
Background
Pre-clinical classification, in-hospital survey, management and treatment of trauma patients is basically a well-organized and choreographed continuum, whose principles are fixed in evidence-based national guidelines [1, 2], recommendations from diverse medical societies [3–18, www.aast.org], as well as educational programs [19]. Driven by current evidences, various recommendations give important implications on the classification and emergency management of severely injured trauma patients. Furthermore, they provide a concrete evidence-based guide for either non-operative, interventional or operative treatment options for multiple and complex injuries [1–19, www.aast.org]. Management and therapeutic decision-making in diverse trauma situations had been well described with high levels of evidence and are clinical routine in emergency departments around the world—for adult patients. In contrast, the incidence of severe trauma in children is certainly lower [2, 19–21], but, “injury remains the most common cause of death and disability in childhood” and “injury morbidity and mortality […] making trauma the most serious public health and health care problem in this population” [19]. These two introducing statements from the Advanced Trauma Life Support ® (ATLS ®) manual (tenth edition) [19] underline the importance of adequate reaction and therapeutic decisions in pediatric trauma, which vice versa improves short-term mortality and long-term outcome [22–24]. However, children are not small adults [2, 19, 25]. Trauma classification systems, diagnostic and therapeutic options as well as surgical techniques or intra-operative considerations in the emergency trauma setting majorly differ between children and adults [2, 6, 9, 19, 26–28]. Despite adequate pre-hospital patient selection and consecutive allocation of severely injured pediatric patients to more experienced trauma centers by rescue services [2, 29], members from trauma centers at any level should be aware of treatment principles and early resuscitation for special cases of pediatric trauma. Knowledge on the principles of pediatric trauma care or inclusion of specialized pediatric surgeons into multi-professional treatment considerations of severely injured children consecutively leads not only to decreased mortality but also to decreased rates of (unnecessary) surgery, for example reduced rates of splenectomies and higher rates of organ-preserving therapy [2, 23, 24, 29–33]. Thereby, recommendations from adult trauma guidelines cannot simply applied to pediatric trauma situations. However, pediatric trauma is insufficiently covered by general trauma guidelines and consecutively high evidence-based recommendations for pediatric trauma management are widely lacking [1, 2, 6, 19]. Furthermore, studies including especially pediatric patients are also rare on sustaining evidence-based trauma protocols in relation to outcome. In consequence, the situation of pediatric trauma care from an international point of view remains rather unclear. Situations of severe pediatric trauma induce stress, have psychological and emotional effects on trauma team members. The current study investigates structural management of pediatric trauma in hospitals of different volumes and consecutively centers of different trauma levels, experiences with and necessity of educational programs for pediatric trauma management. The responses are set in relation to sizes of hospitals and ages of the severely injured children. This follows the aim to enhance preparedness for treatment of severely injured children, to reduce concerns and fears against pediatric trauma and to improve quality of trauma care in children, patient morbidity and mortality. By this survey, the World Society of Emergency Surgery (WSES) claims to gain global information on pediatric trauma care. The results could lead to the initiation of educational programs for pediatric trauma management and to underline the necessity for a WSES-driven guideline program.
Methods
As described previously [34, 35], an online survey was designed by a core group of investigators of the study group. Google Forms (Google LLC, Mountain View, California, USA) was used as the platform for the survey. After the survey was approved by the WSES project steering committee, this cross-sectional survey study was distributed in October 2021 to the global mailing list of WSES members. The survey was closed in March 2022.
The survey was designed, the survey study was conducted, and the results were analyzed and reported following the CHERRIES statement [36].
The survey consists of single-choice items as well as one open-answer question. The items of the present questionnaire are organized in five sections: (1) recording the characteristics of respondents and their affiliated hospitals, (2) volume of pediatric trauma patients, (3) individual capacities and infrastructure for pediatric trauma and surgical emergency care in children, (4) in-hospital trauma team composition, clinical work-up and team training for pediatric trauma and pediatric surgical emergency care and (5) individual experiences with pediatric trauma care and emergency surgery in children in response to patients´ age.
After closing the survey, the results were checked for duplicates. Results of the total study cohort are presented descriptively within the Figures of the manuscript.
Results of items, that were comparable, were conducted to statistical analyses. Furthermore, the collaboration group was subdivided with regard to sizes of affiliated hospitals. ≤ 500 in-hospital beds indicated the smaller hospitals, > 500 in-hospital beds indicated the larger hospitals. Comparisons of survey results allow to interpret the current situation in pediatric traumatology and emergency surgery concerning individual hospital volumes. Results of subgroup analyses are presented in Tables.
Statistical analyses were performed using GraphPad Prism (Version 9 for Windows, GraphPad Software, San Diego, CA, USA, www.graphpad.com). For descriptive statistics, categorical data were analyzed using Fishers exact test or Pearson’s X2 test. p values ≤ 0.05 were considered to indicate statistical significance. Because of the exploratory character of the study, no adjustments of p values were performed. Data are given as n respondents and / or percentages of the participants.
Results
Characteristics of participants and their affiliated hospitals
A total of 133 health care specialists in emergency medicine and emergency surgical patient care from several 34 countries (5 continents, approximately two-thirds from Europe and 21% from Asia) around the world completed the survey (Additional file 1). Most of the participants work in larger hospitals with more than 500 beds (72.9%). They were affiliated with level one or level two trauma centers (82.0%), defined by the American College of Surgeons (ACS) and the American Trauma Society (ATS) as a most experienced trauma team in the emergency room, which is constantly available and able to initiate treatment of every aspect of injury [www.amtrauma.org/page/TraumaLevels, accessed May 2nd, 2022 and 37]. The vast majority of the respondents came from general and abdominal surgery (80.5%) and were well-experienced personnel, including at least board-certified surgeons in 77.4% (Fig. 1).
Fig. 1.
Characteristics of the participants and their affiliated hospitals. The current position (a) and the medical profession (b) of the respondents. The volume of the affiliated hospitals (c) and the level of the trauma centers from I to III (d). The level of the trauma centers was defined in accordance with the current definition from the American College of Surgeons and American Trauma Society [www.amtrauma.org/page/TraumaLevels, accessed May 2nd, 2022 and 37]
Individual infrastructure for pediatric trauma and surgical emergency care
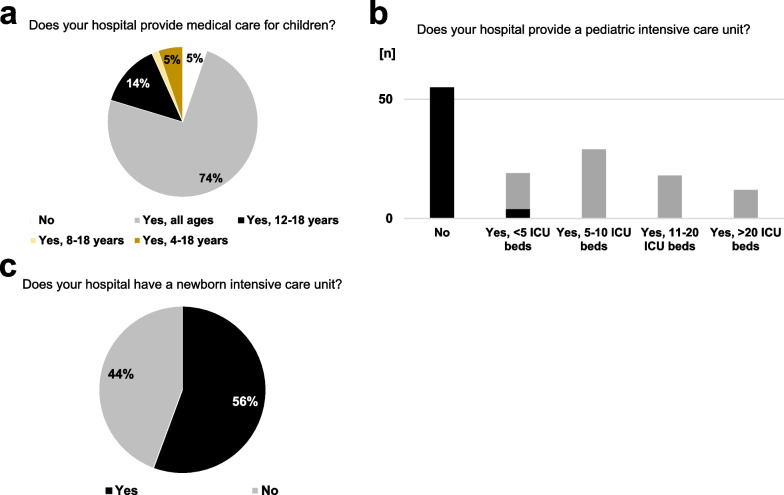
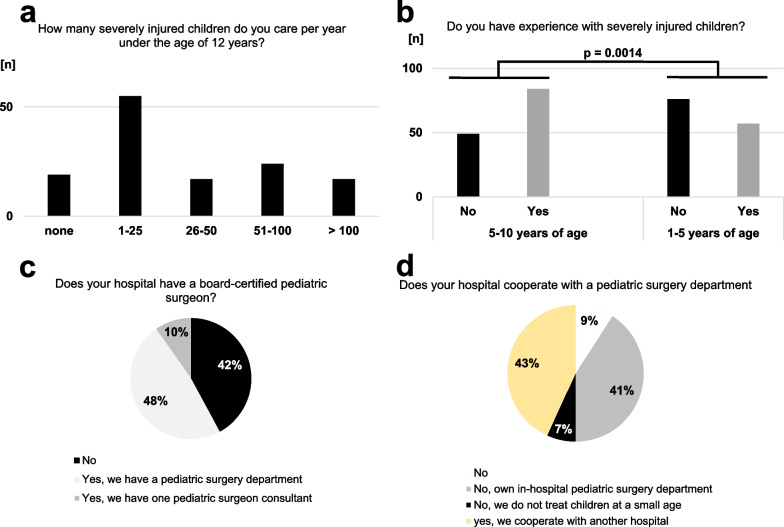
Medical care for children at any age was provided by 74.4% of the affiliated hospitals. However, pediatric patient care was not offered in 5.3% of the affiliated hospitals. In most other cases, the ability to treat pediatric patients was stratified by patient age. In this line, 41.4% or 44.4% of the affiliated hospitals were not equipped with general pediatric intensive care units (ICU) or units for intensive care of newborns, respectively. Vice versa, if a pediatric ICU was available, intensive care of newborns was also possible in most cases. Nevertheless, high-volume pediatric ICUs with more than 10 beds had rarely been reported in the affiliated hospitals of the participants of the survey (Fig. 2). In this line, the vast majority reported a rather low case load (n = 1–25 per year) of severely injured children below the age of 12 years. Experiences of the study group with severely injured children declined dramatically by patient age: while 63.2% of the participants had any experiences with surgical trauma care in children with an age of 5–10 years, this rate decreased to 42.9% in children below the age of 5 (p = 0.0014). Facing this situation, some 57.9% or 42.9% of the participants work together with specialized pediatric surgeons either from their affiliated hospital or by cooperation with pediatric surgeons from other hospitals in cases of severely injured children, respectively (Fig. 3).
Fig. 2.
Infrastructure for the care of critically-ill pediatric patients. Most of the affiliated hospitals provide medical care for children (a), but approximately half of the hospitals lack a pediatric (b) or newborn intensive care unit (c). Figure 2b: gray bars indicate hospitals, which also treat newborns; black bars indicate hospitals, which do not treat newborns
Fig. 3.
Individual and institutional experiences with pediatric trauma care of participants and their affiliated hospitals. The trauma center volume with regard to the treatment of severely injured children under 12 years of age (a). Significantly less participants were experienced with treatment of severely injured children below the age of 5 years (b, p = 0.0014 versus 5–10 years of age). In-hospital availability of specialized pediatric surgeons (c) or a department of pediatric surgery (d)
Team building and team training for pediatric surgical emergency care
The structure of in-hospital trauma teams in their affiliated hospitals varied strongly between the respondents. One-third of the participants reported that both pediatricians and pediatric surgeons are the regular team members during the in-hospital trauma survey for severely injured children regardless of patient age. Otherwise, adjustments of the standard trauma team were possible upon results of the primary trauma survey and in relation to day or night time (Fig. 4).
Fig. 4.
Team considerations in pediatric emergency situations. Emergency room (ER) and surgical team compositions in cases of injured children (a and b, respectively). Scenarios: trauma surgery versus appendicitis in children at different ages (c). * indicates p = 0.0210. # indicates p = 0.0485
Similar differences in initial trauma teams were recorded for the consecutive question "Who performs emergency surgery for pediatric trauma in patients younger than 10 or 5 years of age?". While approximately one fourth of the respondents stated that emergency surgery in pediatric trauma patients is routinely performed either by emergency surgeons or by specialized pediatric surgeons, in half of the affiliated hospitals complex severely injured children undergo surgery by a multidisciplinary team, which includes specialized pediatric surgeons (Fig. 4). In the opposite to surgical care of younger patients with acute appendicitis, the patients´ age has no strong statistic effect on team considerations in emergency surgery for trauma.
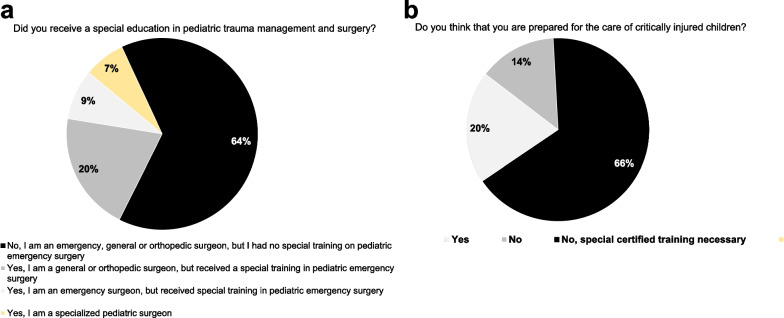
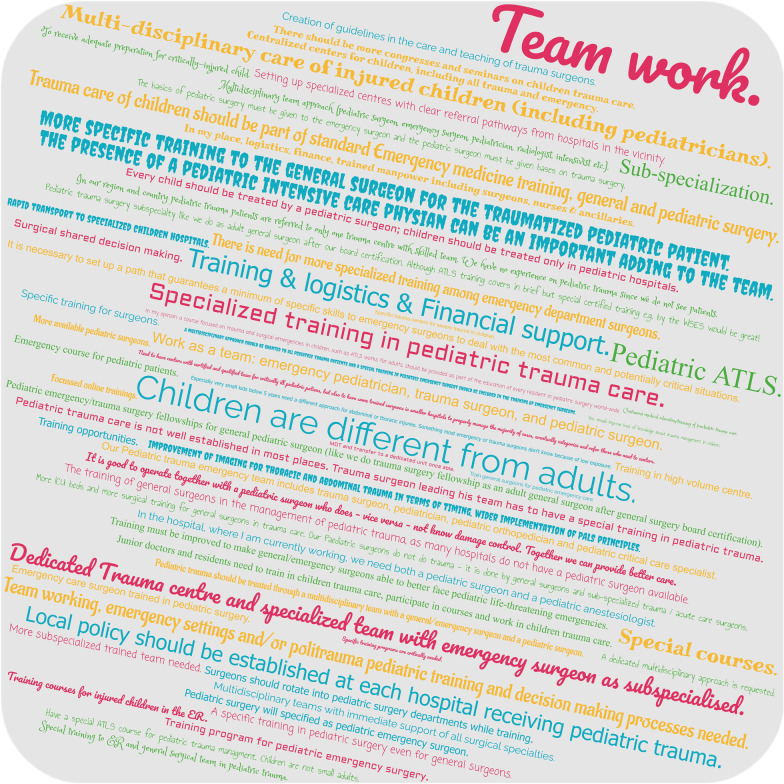
Last and most relevant, the majority of participants of the present survey (80.2%) do not feel sufficiently prepared for the (surgical) treatment of severely injured children and 64.3% stated the urgent need for special training in pediatric trauma care and emergency surgery in children (Fig. 5). The word cloud in Fig. 6 collects the answers on the question, what might enhance preparedness of trauma teams for severely injured children and consequently quality of pediatric trauma care in the future.
Fig. 5.
Preparedness for care of severely injured pediatric patients. The majority of emergency surgeons worldwide received neither a special education in pediatric trauma management or surgery (a) nor feel sufficiently prepared for the management and surgical treatment of critically injured pediatric trauma patients (b)
Fig. 6.
What might enhance preparedness of trauma teams for severely injured children and quality of pediatric trauma care in the future? Answers from the respondents collected in a word cloud
Hospital size effects on pediatric emergency and trauma care
The hospital size was stratified by numbers of in-hospital beds. A bed count of more than 500 was decided to separate larger from smaller hospitals. 36 (27.1%) participants work in smaller hospitals (≤ 500 in-hospital beds), vice versa, 97 (72.9%) respondents work in larger hospitals (> 500 in-hospital beds). Larger hospitals were more likely being affiliated with more advanced trauma centers including full trauma care being continuously available with well-experienced staff (level 1: 33.3% versus 77.3%, p < 0.0001) as well as with more elaborated pediatric intensive care infrastructure (p < 0.0001). Although not significant, treatment of children of all ages was more frequently feasible in larger hospitals by tendency (58.3% versus 80.4%, p = 0.0938); the estimated case load of more severely injured children below the age of 12 was considerably higher in larger hospitals (p = 0.0009). Therefore, the majority of larger hospitals reserve either an independent department for pediatric surgery or at least one board-certified pediatric surgeon consultant (22.2% versus 71.1%, p < 0.0001, Table 1). Nevertheless, a significant proportion of the respondents, who are themselves specialists in surgical emergency and trauma care, stated that they have no sufficient experiences with severely injured children. This situation is dramatically aggravated by lower patient age and is more evident in participants from smaller hospitals (Table 1 and 2). Interestingly, in-hospital trauma teams as well as surgical teams involved in the treatment of pediatric trauma are composed primarily more multidisciplinary including pediatricians and specialized pediatric surgeons in larger hospitals, whereas a specific age effect of injured children (1–5 years versus 5–10 years of age) was not observed herein (Tables 3 and 4).
Table 1.
Spectrum and expertise with regard to the size and volume of affiliated hospitals
| Items (question & answer) | ≤ 500 in-hospital beds n = 36 (27.1%) | > 500 in-hospital beds n = 97 (72.9%) | p value | ||
|---|---|---|---|---|---|
| (n) | n.a | (n) | n.a | ||
| Trauma center# | 0 | 0 | p < 0.0001 | ||
| Level 1 | 12 | 75 | |||
| Level 2 | 13 | 9 | |||
| Level 3 | 11 | 13 | |||
| Does your hospital regularly provide medical care for children? | 0 | 0 | p = 0.0938 | ||
| No | 2 | 5 | |||
| Yes, all ages (0–18 years) | 21 | 78 | |||
| Yes, at an age of 4–18 years | 3 | 4 | |||
| Yes, at an age of 8–18 years | 1 | 1 | |||
| Yes, at an age of 12–18 years | 9 | 9 | |||
| Does your hospital provide a pediatric ICU? | 0 | 0 | p < 0.0001 | ||
| No | 26 | 29 | |||
| Yes, < 5 ICU beds | 8 | 11 | |||
| Yes, 5–10 ICU beds | 1 | 28 | |||
| Yes, 11–20 ICU beds | 1 | 17 | |||
| Yes, > 20 ICU beds | 0 | 12 | |||
| How many severely injured children do you care per year at an age < 12 years? | 0 | 1 | p = 0.0009 | ||
| None | 7 | 12 | |||
| 1–25 | 24 | 31 | |||
| 26–50 | 1 | 16 | |||
| 51–100 | 2 | 22 | |||
| > 100 | 2 | 15 | |||
| Does your hospital have a board-certified pediatric surgeon? | 0 | 0 | p < 0.0001 | ||
| No | 28 | 28 | |||
| Yes, own department | 3 | 61 | |||
| Yes, one pediatric surgeon consultant | 5 | 8 | |||
| Do you have experiences with injured children? | 0 | 0 | |||
| 5–10 years of age | p = 0.0086 | ||||
| No | 20 * | 29* | |||
| Yes | 16 | 68 | |||
| 1–5 years of age | p = 0.0002 | ||||
| No | 30* | 46* | |||
| Yes | 6 | 51 | |||
#Regarding the American College of Surgeons and American Trauma Society. n.a. = no answer. ICU = Intensive care unit. *Significant difference (p ≤ 0.05) by patient age (1–5 years versus 5–10 years of age)
Table 2.
Preparedness for pediatric trauma of the collaborators with regard to the size and volume of affiliated hospitals
| Items (question & answer) | ≤ 500 in-hospital beds n = 36 (27.1%) | > 500 in-hospital beds n = 97 (72.9%) | p value | ||
|---|---|---|---|---|---|
| (n) | n.a | (n) | n.a | ||
| Did you receive a special training in pediatric emergency management and surgery? | 1 | 3 | p = 0.0075 | ||
| No | 29 | 54 | |||
| Yes | 6 | 40 | |||
| Do you feel prepared for management, surgery and treatment of an severely injured child? | 1 | 1 | p = 0.0024 | ||
| No | 34 | 71 | |||
| Yes | 1 | 25 | |||
n.a. = no answer
Table 3.
Trauma team considerations with regard to the size and volume of the affiliated hospitals
| Items (question & answer) | ≤ 500 in-hospital beds n = 36 (27.1%) | > 500 in-hospital beds n = 97 (72.9%) | p value | ||
|---|---|---|---|---|---|
| (n) | n.a | (n) | n.a | ||
| Trauma team in cases of injured children? | |||||
| 5–10 years of age | 0 | 2 | p = 0.0043 | ||
| Routine team | 5ø | 16ø | |||
| Pediatrician additionally | 12 | 11 | |||
| Pediatric surgeon additionally | 4 | 13 | |||
| Pediatrician AND pediatric surgeon additionally | 6 | 36 | |||
| Depend on day/night time | 0 | 8 | |||
| Additional team members on-call, depend on results of trauma survey | 9 | 11 | |||
| 1–5 years of age | 1 | 1 | p = 0.0147 | ||
| Routine team | 5ø | 19ø | |||
| Pediatrician additionally | 10 | 12 | |||
| Pediatric surgeon additionally | 3 | 11 | |||
| Pediatrician AND pediatric surgeon additionally | 8 | 38 | |||
| Depend on day/night time | 0 | 7 | |||
| Additional team members on-call, depend on results of trauma survey | 9 | 9 | |||
| Who performs emergency surgery in cases of injured children? | |||||
| 5–10 years of age | 0 | 1 | p < 0.0001 | ||
| Emergency surgeon | 18ø | 13ø | |||
| Emergency surgeon together with the pediatric surgeon | 4 | 10 | |||
| Pediatric surgeon | 6 | 25 | |||
| Depend on injury, multidisciplinary surgical team | 6 | 14 | |||
| Depend on injury, multidisciplinary surgical team including pediatric surgeons | 2 | 34 | |||
| 1–5 years of age | 1 | 1 | p = 0.0053 | ||
| Emergency surgeon | 16ø | 17ø | |||
| Emergency surgeon together with the pediatric surgeon | 2 | 8 | |||
| Pediatric surgeon | 8 | 30 | |||
| Depend on injury, multidisciplinary surgical team | 6 | 11 | |||
| Depend on injury, multidisciplinary surgical team including pediatric surgeons | 3 | 30 | |||
n.a. = no answer. ICU = Intensive care unit. Ø no difference (p > 0.05) by patient age (1–5 years versus 5–10 years of age)
Table 4.
Surgical team considerations for pediatric surgical emergency scenarios with regard to the size and volume of affiliated hospitals
| Items (Question & answer) | ≤ 500 in-hospital beds n = 36 (27.1%) | > 500 in-hospital beds n = 97 (72.9%) | p value | ||
|---|---|---|---|---|---|
| (n) | n.a | (n) | n.a | ||
| Who performs trauma surgery? | |||||
| Scenario 1: car accident, free abdominal fluid in a 8 year old child? | 1 | 0 | p = 0.0004 | ||
| Emergency surgeon | 10ø | 23ø | |||
| General surgeon | 15 | 13 | |||
| Pediatric surgeon | 5 | 46 | |||
| General OR pediatric surgeon | 5 | 15 | |||
| Scenario 2: car accident, free abdominal fluid in a 4 year old child? | 3 | 1 | p = 0.0002 | ||
| Emergency surgeon | 9ø | 21ø | |||
| General surgeon | 14 | 10 | |||
| Pediatric surgeon | 8 | 50 | |||
| General OR pediatric surgeon | 2 | 15 | |||
| Who performs emergency surgery? | |||||
| Scenario 3: acute appendicitis in a 8 year old child? | 5 | 5 | p = 0.0025 | ||
| Emergency surgeon | 5ø | 10ø | |||
| General surgeon | 15 | 17 | |||
| Pediatric surgeon | 7 | 53 | |||
| General OR pediatric surgeon | 4 | 12 | |||
| Scenario 4: acute appendicitis in a 4 year old child? | 2 | 2 | p = 0.0046 | ||
| Emergency surgeon | 5ø | 8ø | |||
| General surgeon | 14 | 14 | |||
| Pediatric surgeon | 13 | 62 | |||
| General OR pediatric surgeon | 2 | 11 | |||
n.a. = no answer. Ø no difference (p > 0.05) by patient age (1–5 years versus 5–10 years of age)
Discussion
Basically, the present study dramatically confirms the expected conclusion: Everyone is involved in some way in the treatment of injured children, but the minority is really sufficiently prepared for pediatric trauma management. As expected, the sizes of trauma centers have an influence on the experience level of the emergency surgeon in pediatric trauma management: Although even 29.9% and 47.4% of the respondents from larger hospitals have no experiences with trauma management of children below the age of 10 years and below the age of 5 years, respectively, significantly more emergency surgeons from smaller hospitals were vice versa inexperienced with pediatric trauma management at all. Pediatric trauma management in larger hospitals is performed more multi-professionally according to the trauma level definition from the ACS and ATS [www.amtrauma.org/page/TraumaLevels, accessed May 2nd, 2022 and 37]. Participants from larger hospitals were more commonly trained in pediatric trauma management and, furthermore, pediatricians as well as specialized pediatric surgeons play a major role in the treatment of severely injured children in these larger, even more experienced centers.
Nevertheless, through the global perspective centralization of pediatric trauma care is difficult. The treatment of critically injured children is typically covered worldwide by both smaller and larger trauma centers. In many countries, a comprehensive trauma care for children with highly experienced and specialized pediatric surgeons is not well organized even for the early resuscitation phase of trauma care. This is particularly the critical situation in rural areas, where also hospitals without dedicated pediatric trauma services are confronted with these special pediatric trauma cases [37]. Our study reflects this problem, as also trauma teams from smaller hospitals with even inexperienced trauma centers are involved in the initial treatment or urgent resuscitation of pediatric trauma patients with nonsignificant numbers per year (1–25 severely injured children in 66.7% of these cases, see Table 1).
Although the response rate with 133 participants from the global mailing list of the international WSES was rather low and reflects a major limitation of our study, the results of the survey give important implications on the question: How experienced are emergency surgeons worldwide in pediatric trauma care. Though the vast majority of participants from smaller hospitals (97.1%) do not feel enough and sufficiently prepared for the treatment of severely injured children. Nevertheless, even 74.0% of the respondents from larger hospitals do not feel prepared adequately for appropriate management of severely injured children, but they can fall back and have access to sufficient back-up consisting of specialized pediatric surgeons, pediatricians and high-volume pediatric ICU in their affiliated trauma centers providing total care of every aspect of injury [www.amtrauma.org/page/TraumaLevels, accessed May 2nd, 2022 and 37].
Highly evidence-based and universal recommendations on pediatric trauma management from local or international medical societies analogous to adult trauma are widely lacking at present. To face this dilemma in pediatric emergency trauma care, the Committee on Trauma from the American College of Surgeons gives advices for defining pediatric trauma centers and pediatric trauma teams, which might facilitate referral considerations of the involved pre-hospital rescue service [22, 23, 37, 38]. Whether this closes the gap between the lack of evidence, the low experience especially in small hospitals and the clinical outcome of pediatric trauma patients remains to be determined in the future. However, our data show impressively that there are situations, when even smaller hospitals affiliated with lower level (adult) trauma centers without broad experience in emergency care of pediatric patients have to provide primary care of severely injured children, especially in areas where pediatric emergency and trauma services are scarce [37]. It is alarming that our study shows a dramatic lack of education, practical training as well as tactical and organizational deficiencies for these pediatric cases. Consequently, surgeons from smaller hospitals with less experienced trauma centers should also increase their knowledge of principles and treatment considerations in pediatric trauma management. Vice versa, this will not only reduce concerns and fears against situations with severely injured children, but also might improve outcomes of pediatric trauma patients. The worldwide recognized educational ALTS ® course has now implemented a specific section about pediatric trauma [19]. Guidelines, which are available for traumatic injuries in adults, should be revised and edited for pediatric trauma patients by respective national as well as international medical societies, like the World Society for Emergency Surgeons had done for various situations of severe trauma (e.g., spleen trauma, liver trauma, duodeno-pancreatic and biliary tree trauma or kidney and uro- trauma) [5, 6, 9–11, 39]. This might improve theoretical education and knowledge of trauma team members, especially trauma surgeons involved in pediatric trauma management. On a more local basis trans-regional level I or II trauma centers from larger hospitals should provide practical courses, consultations or fellowships for trauma team members and trauma surgeons from more unexperienced trauma centers or smaller hospitals to enhance and exercise their theoretical knowledge in “real life”. Both might increase and strengthen the preparedness for management of trauma and severe injuries in pediatric patients even of trauma teams, who are not regularly confronted with severely injured children.
Despite these important aspects in the care of pediatric trauma from the global perspective, our study has some other limitations that must be listed besides the low response rate mentioned above. Precise conclusions about differences between individual countries or specific regions cannot be drawn due to the low return rate. Furthermore, the responses are based on subjective opinions and feelings of the participants and, for example, the answers to the infrastructural questions were not officially verified. For these reasons, it was decided to use hospital size (≤ versus > 500 beds) rather than trauma center level regarding the ATS to stratify hospitals, even though the parameter is certainly somewhat less accurate in capturing the quality of care for trauma patients. Although the number (≤ versus > 500 beds) was chosen arbitrarily, it can be anticipated and it is shown by results presented here that rather the larger hospitals are associated with more advanced trauma centers. Finally, the lack of external validation of the survey should certainly be seen as a minor limitation of the work. To take this into account, the survey was designed and internally validated by core investigators of this work and then, revised and validated for the international professional society members by the WSES steering committee representatives.
Conclusions
In conclusion, our study shows that emergency surgeons from both high and low level trauma centers report an alarming lack of knowledge on pediatric trauma care. Multi-professional management of pediatric trauma patients and the individual experience with severely injured children is strongly dependent on the volume, the level of the trauma center and infrastructure of the specific hospital. However, smaller hospitals with less experienced trauma centers are also confronted with pediatric trauma patients. This underlines the importance of theoretical education and practical training programs for appropriate management of pediatric trauma and primary survey or resuscitation as well as early induction of adequate therapy of severely injured children. Recommendation, guidance of appropriate therapy, teaching and training might be the future mission of national and international medical societies as well as trans-regional well-experienced pediatric trauma centers in the perspective of global improvements in pediatric trauma care.
Supplementary information
Additional file 1. The WSES pediatric emergency surgery collaboration group (only those who agree are listed as collaborators).
Acknowledgements
The authors sincerely thank all respondents and collaborators of the study for participation in the survey.
WSES project steering committee representative
Federico Coccolini and Fausto Catena.
The WSES pediatric emergency surgery collaboration group (only those who agree are listed as collaborators).
Agron Dogjani, University of Medicine of Tirana, Tirana, Albania; Akira Kuriyama, Emergency and Critical Care Center, Kurashiki Central Hospital, Japan; Alberto Porcu, Università degli Studi di Sassari, Italy; Aleix Martínez-Pérez, Department of General and Digestive Surgery, Hospital Universitario Doctor Peset, Valencia, Spain; Alessandro Coppola, General Surgery, Fondazione Policlinico Universitario Campus Bio-Medico, Rome, Italy; Alessandro Spolini, UOC Chirurgia Generale Sondrio ASST Valtellina-Alto Lario, Italy; Alessio Giordano, General Surgery unit, Nuovo Ospedale S. Stefano, Prato, Italy; Alexandros Kyriakidis, General Hospital of Amfissa, Greece; Ali Yasen Y Mohamedahmed, Sandwell and West Birmingham NHS trust, United Kingdome; Anastasia Vasilopoulou, Trauma and Orthopedic Department, Korgialenio-Benakio- Hellenic Red Cross Hospital, Athens, Greece; Andee Dzulkarnaen Zakaria, Department of Surgery, School of Medical Sciences & Hospital USM, Universiti Sains Malaysia, Malaysia; Andrea Balla, UOC of General and Minimally Invasive Surgery, Hospital “San Paolo”, Largo Donatori del Sangue 1, Civitavecchia, Rome, Italy; Andreas Fette, PS_SS, Weissach im Tal, Germany; Andrey Litvin, Department of Surgical Disciplines, Immanuel Kant Baltic Federal University, Regional Clinical Hospital, Kaliningrad, Russia; Anna Guariniello, Santa Maria delle Croci Hospital, Ravenna, Italy; Arda Isik, Istanbul medeniyet university, Turkey; Aristotelis Kechagias, Department of General Surgery, Kanta-Häme Central Hospital, Finland; Ashrarur Rahman Mitul, Bangladesh Shishu Hospital & Institute, Bangladesh; Belinda De Simone, Department of Emergency, digestive and metabolic minimally invasive surgery, Poissy and Saint Germain en Laye Hospitals, Ile de France, France; Biagio Zampogna, Department of Orthopaedic and Trauma Surgery, Campus Bio-Medico University of Rome, Rome, Italy; Bruno Sensi, Policlinico tor vergata, Rome, Italy; Carlo Gazia, Istituto Nazionale Tumori Regina Elena, Italy; Charalampos Seretis, General University Hospital of Patras, Greece; Cristine Brooke; Davide Luppi, General And Emergency Surgery, ASMN IRCCS Reggio Emilia, Italy; Diego Coletta, AO Ospedali Riuniti Marche Nord, Department of General Surgery, Italy; Diego Sasia, General and Oncological Surgery Unit, Santa Croce and Carle Hospital, Cuneo, Italy; Diletta Corallino, Policlinico Umberto I Rome, Italy; Dimitrios Chatzipetris, Department of Surgery, Metaxa Cancer Hospital, Piraeus, Greece; Dimitrios Schizas, First Department of Surgery, Laikon General Hospital, University of Athens, Athens, Greece; Eftychios Lostoridis, Kavala General Hospital, Kavala, Greece; Elmuiz A. Hsabo, Manchester University NHS Foundation Trust, United Kingdom; Emmanouil Kaouras, Department of Surgery, Metaxa Cancer Hospital, Piraeus, Greece; Emmanuel Schneck, Department of Anesthesiology, Operative Intensive Care Medicine and Pain Therapy, University Hospital of Giessen, Rudolf-Buchheim-Strasse 7, Giessen, Germany; Enrico Pinotti, Policlinico San Pietro, Italy; Evgeni Dimitrov, Department of Surgical Diseases, University Hospital "Prof. Dr. Stoyan Kirkovich" Stara Zagora, Bulgaria; Fabrizio D’Acapito, Chirurgia Generale e Terapie ocnologiche Avanzate, Morgagni-Pierantoni Hospital, Forlì, AUSL Romagna, Italy; Federica Saraceno, UOC of General and Minimally Invasive Surgery, Hospital „San Paolo“, Largo Donatori del Sangue 1, Civitavecchia, Rome, Italy; Fikri Abu-Zidan, Department of Surgery, College of Medicine, UAE University, Al-Ain, United Arab Emirates; Francesca Maria Silvestri; Francesco Favi, U.O.C. Chirurgia Gerenale e d’Urgenza, Dipartimento Chirurgico e Grandi Traumi—Ospedale “M. Bufalini” Cesena AUSL della Romagna, Italy; Francesco Fleres, General Surgery Unit—ASST Valtellina e Alto Lario, Sondrio Hospital, Sondrio, Italy; Francesk Mulita, Department of Surgery, General University Hospital of Patras, Greece; Gabriela Nita, Sant'Anna Hospital, AUSL Reggio Emilia, Italy; Gennaro Martines, Azienda Ospedaliero Universitaria Policlinico Bari, Italy; Gennaro Mazzarella, Department of Emergency Surgery, Sapienza University of Rome, Rome, Italy; Gennaro Perrone, Department of emergency surgery, Parma Maggiore Hospital, Parma, Italy; Giorgio Giraudo, Department of Surgery ASO Santa Croce e Carle Cuneo, Italy; Giulia Bacchiocchi, Tor Vergata University, Rome, Italy; Giulio Argenio, UOC Chirurgia d'Urgenza, AOU San Giovanni di Dio e Ruggi d'Aragona, Salerno, Italy; Giuseppe Brisinda, Department of Surgery, Fondazione Policlinico Universitario A Gemelli, IRCCS and Università Cattolica S. Cuore, Rome, Italy; Giuseppe Currò, AOU Mater Domini Catanzaro—Magna Graecia University of Catanzaro, Italy; Giuseppe Palomba, Università Federico II di Napoli, Italy; Gustavo P. Fraga, Division of Trauma Surgery, School of Medical Sciences, University of Campinas (Unicamp), Brazil; Hytham K. S. Hamid, Kuwaiti Specialized Hospital, Khartoum, Sudan; Ioannis Katsaros, Department of Surgery, Metaxa Cancer Hospital, Pireaus, Greece; Ionut Negoi, General Surgery Department, Carol Davila University of Medicine and Pharmacy Bucharest, Emergency Hospital of Bucharest, Romania; Joel Noutakdie Tochie, Department of Emergency Medicine, Anaesthesiology, Critical Care Medicine, Laquintinie Hospital of Douala, Douala, Cameroon; Justin Davies, Addenbrooke’s Hospital, Cambridge University Hospitals NHS Foundation Trust, United Kingdom; Kenneth Y. Y. Kok, Pengiran Anak Puteri Rashidah Sa´adatul Bolkiah Institue of Health Sciences, Universiti Brunei darussalam, Brunei; Konstantinos G. Apostolou, Department of General and Endocrine Surgery, Athens Medical Center, Palaio Faliro, Athens, Greece; Konstantinos Lasithiotakis, Department of Surgery, University Hospital of Heraklion, Crete, Greece; Konstantinos Tsekouras, Sismanogleio General Hospital, Athens, Greece; Larysa Sydorchuk, Bukovinian State Medical University, Ukraine; Leandro Siragusa, Department of Surgery, Università degli studi di Roma „Tor Vergata“, Italy; Leonardo Solaini, Department of Medical and Surgical Sciences, University of Bologna, Morgagni Pierantoni Hospital, Forlì, Italy; Luca Ferrario, General Surgery Trauma Team ASST-GOM Niguarda, Milan, Italy; Luis Buonomo, Hospital Zonal de Agudos "Dr. Alberto Balestrini", Argentina; Maciej Walędziak, Military Institute of Medicine, Department of General Surgery, Poland; Mahir Gachabayov, Vladimir City Emergency Hospital, Russia; Maloni Bulanauca, Department of Surgery, Labasa Hospital, Fiji; Manish Kumar Agrawal, King George’s Medical University Lucknow, India; Marco Ceresoli, University of Milano-Bicocca, Italy; Maria Chiara Ranucci, Azienda ospedaliera Santa Maria di Terni, Italy; Maria Petridou, Department of Pediatric Surgery, Ippokration General Hospital of Thessaloniki, Thessaloniki, Greece; Mario D’Oria, Division of Vascular and Endovascular Surgery, Cardiovascular Department, University Hospital of Trieste, Italy; Massimiliano Veroux, General Surgery, University Hospital of Catania, Department of Medical and Surgical Sciences and Advanced Technologies, University of Catania, Italy; Maximos Frountzas, First Propaedeutic Department of Surgery, National and Kapodistrian University of Athens, Medical School, Hippocration General Hospital of Athens, Greece; Michel Paul Johan Teuben, Cantonal Hospital Frauenfeld, Switzerland; Miklosh Bala, Department of General Surgery, Hadassah Medical Center and Faculty of Medicine, Hebrew University of Jerusalem, Israel; Mirja Amadea Minger, Department of Pediatric Surgery, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland; Miroslava Gonçalves, Centro Hospitalar Universitário Lisboa Norte—Hospital de Santa Maria, Lisboa, Portugal; Natasha Sharma; Nicolò Tamini, ASST Monza—Ospedale San Gerardo, Italy; Noushif Medappil, Aster Malabar Institute of Medical Sciences (Aster MIMS—Calicut), India; Orestis Ioannidis, 4th Department of Surgery, Medical School, Aristotle University of Thessaloniki, General Hospital “George Papanikolaou”, Thessaloniki, Greece; Pietro Bisagni, Department of Surgery, ASST di Lodi, Lodi, Italy; Razrim Rahim, Universiti Sains Islam Malaysia, Malaysia; Ricardo Alessandro Teixeira Gonsaga, Centro Universitário Padre Albino, Catanduva (SP), Brazil; Roberta Ragozzino, General surgery and Trauma Team, ASST Niguarda, Milano, Piazza Ospedale Maggiore 3, Milan, Italy; Roberto Bini, ASST Niguarda Hospital, Italy; Roberto Cammarata, Campus Biomedico University of Rome, Italy; Ruslan Sydorchuk, General Surgery Department, Regional Acute and Emergency Hospital Chernivtsi, Ukraine; Salomone Di Saverio, Ospedale Madonna del Soccorso San benedetto del Tronto, Italy; Selmy S. Awad, Mansoura university hospitals, Mansoura University, Egypt; Semra Demirli Atici, University of Health Sciences Tepecik Training and Research Hospital, Turkey; Serhat Meric, General surgery department, Bağcılar training and research hospital, Istanbul, Turkey; Sharfuddin Chowdhury, King Saud Medical City, Riyadh, Saudi Arabia; Sofia Xenaki, Department of General Surgery, University Hospital of Heraklion Crete, Greece; Tadeja Pintar, Surgery Department, UMC Ljubljana, Ljubljana, Sloviena; Teresa Perra, Università degli Studi di Sassari, Italy; Timothy C. Hardcastle, IALCH Trauma and UKZN Department of Surgery, Durban and University of KwaZulu-Natal, South Africa; Valerio Voglino, Ospedale Pediatrico Bambino Gesù, Roma, Italy; Varut Lohsiriwat, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand; Victor Kong, Department of Surgery, University of KwaZulu Natal, Durban, South Africa; Voskidis Christos, Pediatric Surgery, Greece; Wietse Zuidema, Amsterdam University Medical Center, Amsterdam, Netherlands.
Abbreviations
- ACS
American College of Surgeons
- ATS
American Trauma Society
- CHERRIES
The checklist for reporting results of Internet E-Surveys
- ICU
Intensive care unit
- WSES
World Society of Emergency Surgery
Author contributions
Each author had made substantial contributions to the present manuscript. Conception and design were contributed by MR, MS, IHA, MAW, FCo, FCa, WP, JGR, AH. Acquisition and analysis of data were contributed by MR, JB, AH. Interpretation of data was contributed by MR, MH, AH. Writing first draft was contributed by MR, MH, AH. Critical revision of the manuscript was contributed by MS, IHA, MAW, VA, FCo, FCa, WP, JGR. All authors read the final version of the manuscript and gave final approval for the submission.
Funding
Open Access funding enabled and organized by Projekt DEAL. Martin Reichert was supported by the Justus-Liebig-University Giessen Clinician Scientist Program in Biomedical Research (JLU-CAREER) funded by the German Research Foundation (DFG No. GU405/14–1).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
None declared.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shared last authorship: Jens G. Riedel and Andreas Hecker
Core investigator: Martin Reichert, Massimo Sartelli, Ingolf H. Askevold, Markus A. Weigand, Winfried Padberg, Andreas Hecker
Contributor Information
Andreas Hecker, Email: andreas.hecker@chiru.med.uni-giessen.de.
The WSES pediatric emergency surgery collaboration group:
Agron Dogjani, Akira Kuriyama, Alberto Porcu, Aleix Martínez-Pérez, Alessandro Coppola, Alessandro Spolini, Alessio Giordano, Alexandros Kyriakidis, Ali Yasen Y. Mohamedahmed, Anastasia Vasilopoulou, Andee Dzulkarnaen Zakaria, Andrea Balla, Andreas Fette, Andrey Litvin, Anna Guariniello, Arda Isik, Aristotelis Kechagias, Ashrarur Rahman Mitul, Belinda De Simone, Biagio Zampogna, Bruno Sensi, Carlo Gazia, Charalampos Seretis, Cristine Brooke, Davide Luppi, Diego Coletta, Diego Sasia, Diletta Corallino, Dimitrios Chatzipetris, Dimitrios Schizas, Eftychios Lostoridis, Elmuiz A. Hsabo, Emmanouil Kaouras, Emmanuel Schneck, Enrico Pinotti, Evgeni Dimitrov, Fabrizio D’Acapito, Federica Saraceno, Fikri Abu-Zidan, Francesca Maria Silvestri, Francesco Favi, Francesco Fleres, Francesk Mulita, Gabriela Nita, Gennaro Martines, Gennaro Mazzarella, Gennaro Perrone, Giorgio Giraudo, Giulia Bacchiocchi, Giulio Argenio, Giuseppe Brisinda, Giuseppe Currò, Giuseppe Palomba, Gustavo P. Fraga, Hytham K. S. Hamid, Ioannis Katsaros, Ionut Negoi, Joel Noutakdie Tochie, Justin Davies, Kenneth Y. Y. Kok, Konstantinos G. Apostolou, Konstantinos Lasithiotakis, Konstantinos Tsekouras, Larysa Sydorchuk, Leandro Siragusa, Leonardo Solaini, Luca Ferrario, Luis Buonomo, Maciej Walędziak, Mahir Gachabayov, Maloni Bulanauca, Manish Kumar Agrawal, Marco Ceresoli, Maria Chiara Ranucci, Maria Petridou, Mario D’Oria, Massimiliano Veroux, Maximos Frountzas, Michel Paul Johan Teuben, Miklosh Bala, Mirja Amadea Minger, Miroslava Gonçalves, Natasha Sharma, Nicolò Tamini, Noushif Medappil, Orestis Ioannidis, Pietro Bisagni, Razrim Rahim, Ricardo Alessandro Teixeira Gonsaga, Roberta Ragozzino, Roberto Bini, Roberto Cammarata, Ruslan Sydorchuk, Salomone Di Saverio, Selmy S. Awad, Semra Demirli Atici, Serhat Meric, Sharfuddin Chowdhury, Sofia Xenaki, Tadeja Pintar, Teresa Perra, Timothy C. Hardcastle, Valerio Voglino, Varut Lohsiriwat, Victor Kong, Voskidis Christos, and Wietse Zuidema
References
- 1.Bouillon B. S3 – Leitlinie Polytrauma/Schwerverletztenbehandlung, AWMF Register-Nr. 012/019. 2016;
- 2.Schmittenbecher PP. S2k - Leitlinie Polytraumaversorgung im Kindesalter, AWMF Register-Nr. 006–120. 2020;
- 3.Kozar RA, Crandall M, Shanmuganathan K, Zarzaur BL, Coburn M, Cribari C, et al. Organ injury scaling 2018 update: Spleen, liver, and kidney. J Trauma Acute Care Surg, United States. 2018;85:1119–22. doi: 10.1097/TA.0000000000002058. [DOI] [PubMed] [Google Scholar]
- 4.Coccolini F, Montori G, Catena F, Di Saverio S, Biffl W, Moore EE, et al. Liver trauma: WSES position paper. World J Emerg Surg; 2015;10: 39 [DOI] [PMC free article] [PubMed]
- 5.Coccolini F, Catena F, Moore EE, Ivatury R, Biffl W, Peitzman A, et al. WSES classification and guidelines for liver trauma. World J Emerg Surg. England; 2016;11:50. [DOI] [PMC free article] [PubMed]
- 6.Coccolini F, Montori G, Catena F, Kluger Y, Biffl W, Moore EE, et al. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg. England; 2017;12:40. [DOI] [PMC free article] [PubMed]
- 7.Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, et al. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. England; 2017;12:5. [DOI] [PMC free article] [PubMed]
- 8.Coccolini F, Catena F, Kluger Y, Sartelli M, Baiocchi G, Ansaloni L, et al. Abdominopelvic trauma: from anatomical to anatomo-physiological classification. World J Emerg Surg. England; 2018;13:50. [DOI] [PMC free article] [PubMed]
- 9.Coccolini F, Fugazzola P, Morganti L, Ceresoli M, Magnone S, Montori G, et al. The World Society of Emergency Surgery (WSES) spleen trauma classification: a useful tool in the management of splenic trauma. World J Emerg Surg. England; 2019;14:30. [DOI] [PMC free article] [PubMed]
- 10.Coccolini F, Kobayashi L, Kluger Y, Moore EE, Ansaloni L, Biffl W, et al. Duodeno-pancreatic and extrahepatic biliary tree trauma: WSES-AAST guidelines. World J Emerg Surg. England; 2019;14:56. [DOI] [PMC free article] [PubMed]
- 11.Coccolini F, Moore EE, Kluger Y, Biffl W, Leppaniemi A, Matsumura Y, et al. Kidney and uro-trauma: WSES-AAST guidelines. World J Emerg Surg. England; 2019;14:54. [DOI] [PMC free article] [PubMed]
- 12.Pereira BMT, Chiara O, Ramponi F, Weber DG, Cimbanassi S, De Simone B, et al. WSES position paper on vascular emergency surgery. World J Emerg Surg. England; 2015;10:49. [DOI] [PMC free article] [PubMed]
- 13.Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision) J Trauma United States. 1995;38:323–324. doi: 10.1097/00005373-199503000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Moore EE, Cogbill TH, Jurkovich GJ, McAninch JW, Champion HR, Gennarelli TA, et al. Organ injury scaling. III: Chest wall, abdominal vascular, ureter, bladder, and urethra. J Trauma. United States. 1992;33:337–9. doi: 10.1097/00005373-199209000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Moore EE, Jurkovich GJ, Knudson MM, Cogbill TH, Malangoni MA, Champion HR, et al. Organ injury scaling. VI: Extrahepatic biliary, esophagus, stomach, vulva, vagina, uterus (nonpregnant), uterus (pregnant), fallopian tube, and ovary. J Trauma. United States. 1995;39:1069–70. doi: 10.1097/00005373-199512000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Moore EE, Cogbill TH, Malangoni MA, Jurkovich GJ, Champion HR, Gennarelli TA, et al. Organ injury scaling, II: Pancreas, duodenum, small bowel, colon, and rectum. J Trauma United States. 1990;30:1427–1429. doi: 10.1097/00005373-199011000-00035. [DOI] [PubMed] [Google Scholar]
- 17.Moore EE, Malangoni MA, Cogbill TH, Shackford SR, Champion HR, Jurkovich GJ, et al. Organ injury scaling. IV: Thoracic vascular, lung, cardiac, and diaphragm. J Trauma. United States. 1994;36:299–300. doi: 10.1097/00005373-199403000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Coccolini F, Sartelli M, Kluger Y, Pikoulis E, Karamagioli E, Moore EE, et al. COVID-19 the showdown for mass casualty preparedness and management: the Cassandra Syndrome. World J Emerg Surg. 2020;15:26. doi: 10.1186/s13017-020-00304-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Advanced Trauma Life Support ® (ATLS ®), 10th Edition, 2018, American College of Surgeons, The Committee on Trauma.
- 20.Debus F, Lefering R, Frink M, Kühne CA, Mand C, Bücking B, et al. Numbers of Severely Injured Patients in Germany. A Retrospective Analysis From the DGU (German Society for Trauma Surgery) Trauma Registry. Dtsch Arztebl Int. 2015;112:823–9. [DOI] [PMC free article] [PubMed]
- 21.Lutz N, Vandermensbrugghe NG, Dolci M, Amiet V, Racine L, Carron P-N. Pediatric emergencies admitted in the resuscitation room of a Swiss university hospital. Pediatr Emerg Care United States. 2014;30:699–704. doi: 10.1097/PEC.0000000000000231. [DOI] [PubMed] [Google Scholar]
- 22.Wesson DE. Pediatric trauma centers: coming of age. Texas Hear Inst J. 2012;39:871–873. [PMC free article] [PubMed] [Google Scholar]
- 23.Osler TM, Vane DW, Tepas JJ, Rogers FB, Shackford SR, Badger GJ. Do pediatric trauma centers have better survival rates than adult trauma centers? An examination of the National Pediatric Trauma Registry. J Trauma United States. 2001;50:96–101. doi: 10.1097/00005373-200101000-00017. [DOI] [PubMed] [Google Scholar]
- 24.Choi PM, Hong C, Woods S, Warner BW, Keller MS. Early impact of American College of Surgeons-verification at a level-1 pediatric trauma center. J Pediatr Surg United States. 2016;51:1026–1029. doi: 10.1016/j.jpedsurg.2016.02.081. [DOI] [PubMed] [Google Scholar]
- 25.Livingston DH, Lavery RF, Passannante MR, Skurnick JH, Baker S, Fabian TC, et al. Free fluid on abdominal computed tomography without solid organ injury after blunt abdominal injury does not mandate celiotomy. Am J Surg United States. 2001;182:6–9. doi: 10.1016/S0002-9610(01)00665-1. [DOI] [PubMed] [Google Scholar]
- 26.Mehall JR, Ennis JS, Saltzman DA, Chandler JC, Grewal H, Wagner CW, et al. Prospective results of a standardized algorithm based on hemodynamic status for managing pediatric solid organ injury. J Am Coll Surg United States. 2001;193:347–353. doi: 10.1016/S1072-7515(01)01027-4. [DOI] [PubMed] [Google Scholar]
- 27.Notrica DM, Eubanks JW, 3rd, Tuggle DW, Maxson RT, Letton RW, Garcia NM, et al. Nonoperative management of blunt liver and spleen injury in children: Evaluation of the ATOMAC guideline using GRADE. J Trauma Acute Care Surg United States. 2015;79:683–93. doi: 10.1097/TA.0000000000000808. [DOI] [PubMed] [Google Scholar]
- 28.St Peter SD, Sharp SW, Snyder CL, Sharp RJ, Andrews WS, Murphy JP, et al. Prospective validation of an abbreviated bedrest protocol in the management of blunt spleen and liver injury in children. J Pediatr Surg United States. 2011;46:173–177. doi: 10.1016/j.jpedsurg.2010.09.079. [DOI] [PubMed] [Google Scholar]
- 29.Strohm PC, Zwingmann J, Bayer J, Neumann MV, Lefering R, Schmal H, et al. Differences in the outcome of seriously injured children depending on treatment level. Unfallchirurg Germany. 2018;121:306–312. doi: 10.1007/s00113-017-0346-x. [DOI] [PubMed] [Google Scholar]
- 30.Hall JR, Reyes HM, Meller JL, Loeff DS, Dembek R. The outcome for children with blunt trauma is best at a pediatric trauma center. J Pediatr Surg United States. 1996;31:72–77. doi: 10.1016/S0022-3468(96)90322-X. [DOI] [PubMed] [Google Scholar]
- 31.Potoka DA, Schall LC, Gardner MJ, Stafford PW, Peitzman AB, Ford HR. Impact of pediatric trauma centers on mortality in a statewide system. J Trauma United States. 2000;49:237–245. doi: 10.1097/00005373-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Ingram M-CE, Siddharthan R V, Morris AD, Hill SJ, Travers CD, McKracken CE, et al. Hepatic and splenic blush on computed tomography in children following blunt abdominal trauma: Is intervention necessary? J Trauma Acute Care Surg. United States; 2016;81:266–70. [DOI] [PubMed]
- 33.Stylianos S. Outcomes from pediatric solid organ injury: role of standardized care guidelines. Curr Opin Pediatr United States. 2005;17:402–406. doi: 10.1097/01.mop.0000163693.96101.84. [DOI] [PubMed] [Google Scholar]
- 34.Reichert M, Sartelli M, Weigand MA, Doppstadt C, Hecker M, Reinisch-Liese A, et al. Impact of the SARS-CoV-2 pandemic on emergency surgery services-a multi-national survey among WSES members. World J Emerg Surg. 2020;15:64. doi: 10.1186/s13017-020-00341-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reichert M, Sartelli M, Weigand MA, Hecker M, Oppelt PU, Noll J, et al. Two years later: Is the SARS-CoV-2 pandemic still having an impact on emergency surgery? An international cross-sectional survey among WSES members. World J Emerg Surg. 2022;17:34. doi: 10.1186/s13017-022-00424-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004. p. e34. [DOI] [PMC free article] [PubMed]
- 37.American College of Surgeons. Resources for Optimal Care of the Injured Patient, 2014 Standards. 2014. https://www.facs.org.
- 38.American College of Surgeons. Resources for Optimal Care of the Injured Patient, 2022 Standards. 2022. https://www.facs.org.
- 39.Coccolini F, Coimbra R, Ordonez C, Kluger Y, Vega F, Moore EE, et al. Liver trauma: WSES 2020 guidelines. World J Emerg Surg. 2020;15:24. doi: 10.1186/s13017-020-00302-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. The WSES pediatric emergency surgery collaboration group (only those who agree are listed as collaborators).
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.