Abstract
Background
Prompt, effective CPR greatly increases the chances of survival in out-of-hospital c ardiac arrest. However, it is often not provided, even by people who have previously undertaken training. Psychological and behavioural factors are likely to be important in relation to CPR initiation by lay-people but have not yet been systematically identified.
Methods
Aim: to identify the psychological and behavioural factors associated with CPR initiation amongst lay-people.
Design: Systematic review
Data sources: Cochrane Library, MEDLINE, EMBASE, CINAHL, PsycInfo and Google Scholar.
Study eligibility criteria: Primary studies reporting psychological or behavioural factors and data on CPR initiation involving lay-people published (inception to 31 Dec 2021).
Study appraisal and synthesis methods: Potential studies were screened independently by two reviewers. Study characteristics, psychological and behavioural factors associated with CPR initiation were extracted from included studies, categorised by study type and synthesised narratively.
Results
One hundred and five studies (150,820 participants) comprising various designs, populations and of mostly weak quality were identified. The strongest and most ecologically valid studies identified factors associated with CPR initiation: the overwhelming emotion of the situation, perceptions of capability, uncertainty about when CPR is appropriate, feeling unprepared and fear of doing harm. Current evidence comprises mainly atheoretical cross-sectional surveys using unvalidated measures with relatively little formal testing of relationships between proposed variables and CPR initiation.
Conclusions
Preparing people to manage strong emotions and increasing their perceptions of capability are likely important foci for interventions aiming to increase CPR initiation. The literature in this area would benefit from more robust study designs.
Systematic review registration
PROSPERO: CRD42018117438.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12872-022-02904-2.
Keywords: CPR, Bystander, Laypeople, Systematic review, Psychological, Behavioural, Out-of-hospital cardiac arrest
Introduction
Out of hospital cardiac arrest (OHCA) has a devastatingly high mortality rate [1]. Survival to hospital discharge ranges between countries from < 1% [2] to 25% in the best European centres [3], reflecting differences in case identification, demography, geography and emergency service provision [4]. Reducing the mortality associated with OHCA is a strategic priority of many countries [5–10].
Prompt, effective bystander cardiopulmonary resuscitation (CPR) is the most important factor determining survival from OHCA, increasing survival almost 4-fold [11, 12]. Registry data show most OHCA occur at home [2, 13, 14]. Even the most prompt emergency medical response will take at least a few minutes (median 6 mins.) [15], and so the response of others in the home is critical.
Governments and charities invest significantly in training lay-people in CPR [16–18]. Despite this, those in OHCA often do not receive CPR prior to the arrival of emergency services [19]. Even amongst those who are trained, less than half attempt CPR when required [20]. Increasing the proportion of lay-people trained in CPR who actually apply their skills in a real emergency situation is essential [21] as otherwise much of the effort expended in training lay-people will not improve outcomes for patients.
Research relating to CPR training of lay-people has largely been concerned with increasing knowledge and achieving competence in the skill of CPR. Questions of how best to teach CPR tend to be answered by studies using skills performance (e.g. compression depth) and assessment of knowledge as outcome measures [22, 23]. However the International Liaison Committee on Resuscitation [24] and behavioural science [25] would suggest that psychological factors (e.g. people’s attitudes about CPR) are likely to be critical in explaining whether or not people initiate CPR. To date there has not been a systematic synthesis of this literature.
The aim of this review was to synthesise evidence relating to lay-people initiating CPR and to identify the psychological and behavioural factors that facilitate or inhibit people’s willingness to perform CPR.
Method
Protocol and registration
In line with best practice, a review protocol was published (2018) and registered with the PROSPERO International Prospective Register of systematic reviews (protocol number 117438): https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=117438.
Eligibility criteria
Inclusion
Types of study
All primary study designs.
Types of participants
Lay members of the public (i.e. not healthcare professionals or others who receive CPR training as a part of their job, e.g. lifeguards) of any age.
Types of outcome measure
Studies which contained psychological/behavioural data (not CPR knowledge or training status) related to 1) why the participants did or did not perform CPR in real emergencies or 2) would or would not perform CPR in a hypothetical or simulated situation. CPR was defined as performing chest compressions (CC), mouth-to-mouth ventilations, applying an Automated External Defibrillator (AED) or any combination of these.
Exclusion
Papers which did not report a primary empirical study (e.g. reviews, editorials, opinion pieces) were excluded.
Information sources and search strategy
Six electronic databases - Cochrane Library, MEDLINE, EMBASE, CINAHL, PsycInfo and Google Scholar- were searched for publications from inception of each database to 13th December 2019 (search strategy is supplied in supplementary materials Additional file 1). Supplementary searches included: a) reference lists of included studies, b) citations of included studies (Science Citation Index (SCI), Social Sciences Citation Index (SSCI) and Arts and Humanities Citation Index (A&HCI), c) hand-searches of titles (Jan 2005 – Jan 2020) of Resuscitation and a further update database search performed 01/06/21.
Study selection
Screening of titles was undertaken independently by two reviewers (BF and DD) to exclude titles that were obviously irrelevant. The inclusion/exclusion criteria were applied to abstracts of studies and irrelevant abstracts were excluded. Inter-rater agreement kappa was 0.85, pabak kappa = 0.85. Full texts considered potentially relevant by either reviewer were screened independently (BF and DD). At full-text stage, any disagreements between the reviewers were resolved by discussion.
Assessment of methodological quality and risk of bias
The methodological quality of studies was assessed using the Effective Public Health Practice Project (EPHPP) Quality Assessment Tool for quantitative studies [26] and the Joanna Briggs Institute’s Quality Assessment and Review Instrument (QARI) for qualitative studies [27]. Included studies were independently assessed by two reviewers (BF and CT) for methodological quality, with discrepancies being resolved through discussion.
Data extraction
Guided by the CONSORT guidelines [28] and the published protocol, the following data were extracted for each study: study details (author & date, location, study duration, objectives), study methods (design, setting, target population, sample size estimation, actual sample size, sampling and recruitment method, behavioural and psychological data, analysis, dates of recruitment) and study results.
BF and SM independently performed data extraction on 20% of the included studies (n = 20) to assess reliability. No discrepancies in independently extracted data were found and the remainder were extracted by a single researcher (BF or SM).
Synthesis and analysis
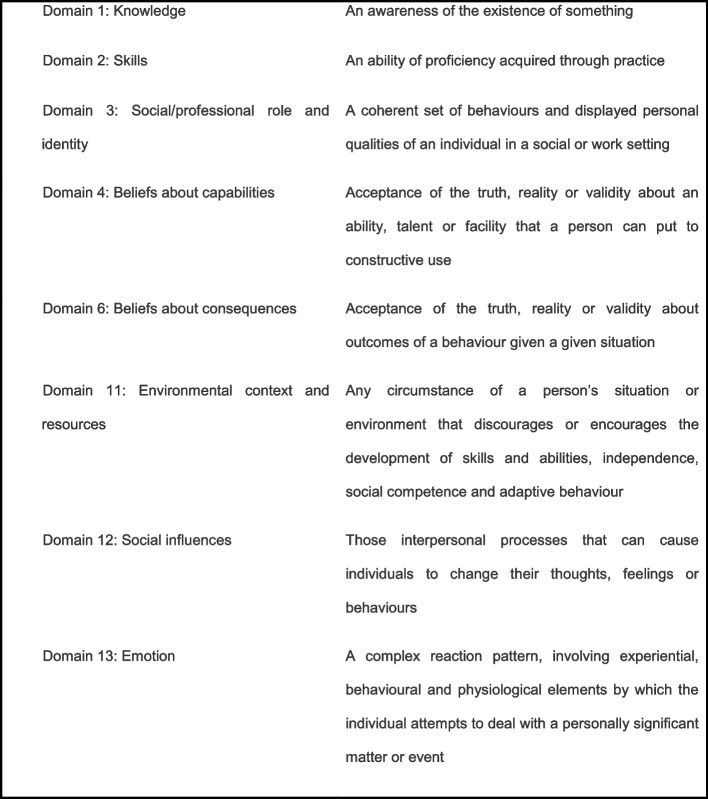
Behavioural and psychological factors identified during extraction were grouped into conceptually similar ‘factors’ by BF: 51 individual factors were identified. To facilitate interpretation, this large number of factors were grouped using categorisations or domains from the Theoretical Domains Framework Version 2 [29] (a validated, comprehensive, theory-informed approach to identifying determinants of behaviour). Definition of domains referred to in this paper are provided in Box 1. Domain categorisations were confirmed by a second reviewer (DD).
Included studies were differentiated according to the study population, study design and whether factors were identified by participants in response to an open question or endorsed from a list of factors presented by researchers. In order to facilitate comparisons studies were grouped according to the summary statistics used and p-values and Odds Ratios compared where possible. We prioritised 1) the most ecologically valid data [30, 31] (i.e. real-life OHCA calls and accounts of people who had actually witnessed OHCA), 2) studies which formally assessed posited relationships and 3) methodologically strong studies (i.e. assessed as low risk of bias) in the findings section.
Results
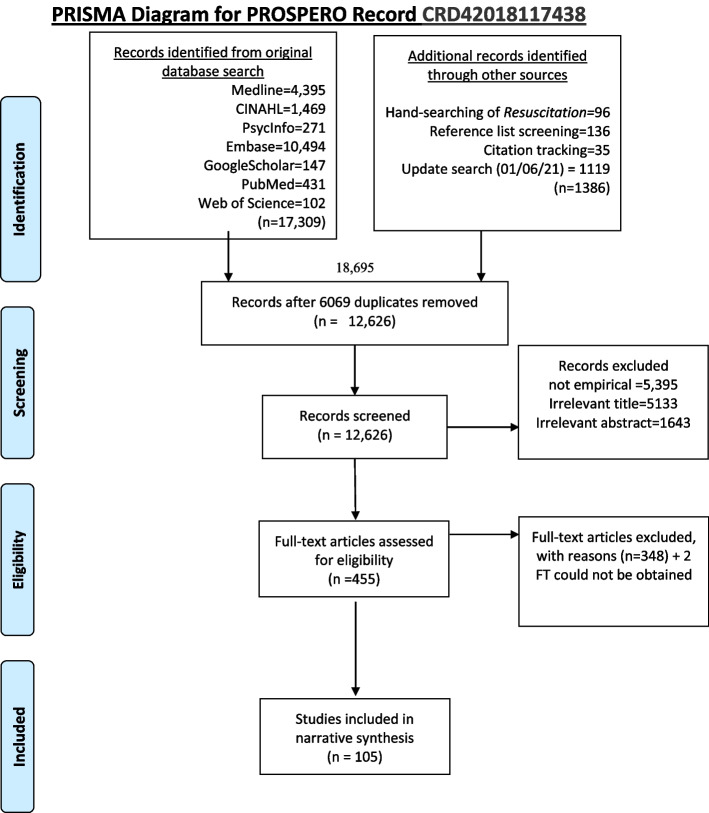
Original database searches conducted on 13th Dec 2018 (see PRISMA diagram, Fig. 1) identified 17,309 citations with 87 studies included after screening for eligibility. An update search conducted 01/06/21 identified 1119 additional titles, 15 of which were assessed as eligible. Hand-searching of Resuscitation (Jan 2005-Dec 2021) identified 96 potentially relevant titles, seven of which had not already been identified by database screening, none met the inclusion criteria. Reference lists of included studies identified an additional 136 papers, 26 of which had not been previously identified, two studies were eligible and included. Finally, citation tracking identified 35 potentially relevant titles, seven not previously screened and one study included. Therefore, a total of 105 studies were included in the narrative synthesis.
Fig. 1.
PRISMA diagram
Description of included studies
Table 1 summarises the main characteristics of the 105 included studies comprising a total of 150,820 participants. The studies were published between 1989 and 2021 and conducted across 30 countries. The studies were heterogenous in design and included: randomised controlled trials (n = 6); non-randomised trials (n = 1); a quasi-experimental deign (n = 1), prospective cohort study (n = 1); before and after studies (n = 15); cross sectional studies (n = 67), qualitative studies (n = 9) and studies examining actual OHCA calls to Emergency Medical Services (n = 5).
Table 1.
List of included studies
| Author(s) | Country | Study Type | Participants | (n=) |
|---|---|---|---|---|
| Aaberg et al. 2014 [32] | Denmark | Before and after study | High School students | 399 |
| Alhussein et al. 2021 [33] | Saudi Arabia | Cross-sectional survey | Adults (≥18 years) | 856 |
| Alshudukhi et al. 2018 [34] | Saudi Arabia | Cross-sectional survey | Adults (≥18 years) | 310 |
| Anto-Ocra et al. 2020 [35] | Ghana | Cross-sectional survey | Adults (≥18 years) | 277 |
| Axelsson et al. 1996 [36] | Sweden | Cross-sectional survey | People who reported making a CPR attempt between 1990 and 1994 | 742 |
| Axelsson et al. 2000 [37] | Sweden | Cross-sectional survey | Adults (≥18 years) who had received training in basic CPR in January 1997 | 1012 |
| Babic et al. 2020 [38] | Slovenia | Cross-sectional survey | Adults (≥18 years) | 198 |
| Becker et al. 2019 [39] | USA | Cross-sectional survey | Adults (≥18 years) who attended CPR training event | 677 |
| Bin et al. 2013 [40] | Saudi Arabia | Cross-sectional survey | High school students | 575 |
| Birkun & Kosova 2018 [41] | Crimea | Cross-sectional survey | Adult (≥18 yrs) | 384 |
| Bohn et al. 2012 [42] | Germany | Prospective cohort | Grammar school pupils (age 10 and age 13) | 280 |
| Bouland et al. 2017 [43] | USA | Before and after study | Laypeople (≥14 years) | 238 |
| Bray et al. 2017 [44] | Australia | Cross-sectional survey | Adult (≥18 yrs) | 404 |
| Breckwoldt, Scholesser & Arntz 2009 [45] | Germany | Cross-sectional survey | Witnesses of an OHCA | 138 |
| Brinkrolf et al. 2018 [46] | Germany | Cross-sectional survey | Witnesses of an OHCA | 101 |
| Case et al. 2018 [47] | Australia | Retrospective analysis of emergency calls for OHCA | Calls to Dispatch Centre with OHCA | 120 |
| Chen et al. 2017 [48] | China | Cross-sectional survey | Adult laypersons (≥18 yrs) + 3 < 18 years | 1841 |
| Cheng et al. 1997 [49] | Taiwan | Cross-sectional survey | Families of cardiac patients and general public | 856 |
| Cheng-Yu et al. 2016 [50] | Taiwan | Before and after study | Adults (≥20 years) | 401 |
| Cheskes et al. 2016 [51] | Canada | Cross-sectional survey | Adult (≥18 yrs) | 428 |
| Chew et al. 2009 [52] | Malaysia | Cross-sectional survey | School teachers | 73 |
| Chew et al. 2019 [53] | Malaysia | Cross-sectional survey | Adult (min age NR) participants at a mass CPR training event | 6248 |
| Cho et al. 2010 [54] | Korea | Before and after study | Lay people aged 11 years and over | 890 |
| Compton et al. 2003 [55] | USA | Cross-sectional survey | School teachers | 201 |
| Coons & Guy 2009 [56] | USA | Cross-sectional survey | Adult (≥18 years) | 755 |
| Cu, Phan & O’Leary 2009 [57] | Australia | Cross-sectional survey | Caregivers of children presenting to the Emergency Department (≥18 years) | 348 |
| Dami et al. 2010 [58] | Switzerland | Retrospective analysis of emergency calls for OHCA | Call to Dispatch Centre with OHCA | 738 |
| De Smedt et al. 2018 [59] | Belgium | Cross-sectional survey | Schoolchildren aged 10–18, teachers and principals | 929 |
| Dobbie et al. 2018 [60] | Scotland | Cross-sectional survey | Adults (≥16 years) | 1027 |
| Donohoe, Haefeli & Moore 2006 [61] | England | Qualitative: focus groups | Adults (≥16 years) | NR |
| Dracup et al. 1994 [62] | USA | Randomised Controlled Trial | Family members of patients at risk of cardiac arrest | 172 |
| Dwyer 2008 [63] | Australia | Cross-sectional survey | Adults (≥18 years) | 1208 |
| Enami et al. 2010 [64] | Japan | Before and after study | Adults (≥17 years). New driver licence applicants | 8890 |
| Fratta et al. 2020 [65] | USA | Cross-sectional survey | Attendees at large public gatherings (aged ≥14) | 516 |
| Han et al. 2018 [66] | Korea | Before and after study | Family members (≥18 years) of patients at risk of cardiac arrest | 203 |
| Hauff et al. 2003 [67] | USA | Retrospective analysis of emergency calls for OHCA | Call to Dispatch Centre with OHCA | 404 |
| Hawkes et al. 2019 [68] | UK | Cross-sectional survey | Adults (≥18 years) | 2084 |
| Hollenberg et al. 2019 [69] | Sweden | Randomised Controlled Trial | School students (13 years) | 641 |
| Huang, Hu & Mao 2016 [70] | China | Cross-sectional survey | School and University students (13–21 years) | 1407 |
| Hubble et al. 2003 [71] | USA | Cross-sectional survey | High school students | 683 |
| Hung et al. 2017 [72] | Hong Kong | Cross-sectional survey | College and University students (≥15 years) | 351 |
| Iserbyt 2016 [73] | Belgium | Before and after study | Secondary school pupils | 313 |
| Jelinek et al. 2001 [74] | Australia | Cross-sectional survey | General public (age not recorded) | 803 |
| Johnston et al. 2003 [75] | Australia | Cross-sectional survey | Adults (≥18 years) | 4490 |
| Kandakai & King 1999 [76] | USA | Before and after study | College students | 214 |
| Kanstad, Nilsen & Fredriksen 2011 [77] | Norway | Cross-sectional survey | Secondary school students (16–19 years) | 376 |
| Karuthan et al. 2019 [78] | Malaysia | Cross-sectional survey | College students | 393 |
| Kua et al. 2018 [79] | Singapore | Before and after study | School students (11–17 years) | 966 |
| Kuramoto et al. 2008 [80] | Japan | Cross-sectional survey | Adults (≥15 years) | 1132 |
| Lam et al. 2007 [81] | Hong Kong | Cross-sectional survey | Laypersons who attended the CPR course (aged ≥7 years) | 305 |
| Lee et al. 2013 [82] | South Korea | Before and after study | College students | 2029 |
| Lerner et al. 2008 [83] | USA | Retrospective analysis of emergency calls for OHCA | Call to Dispatch Centre with OHCA | 168 |
| Lester, Donnelly & Weston 1997 [84] | Wales | Cross-sectional survey | First year high school pupils | 233 |
| Lester, Donnelly & Assar 1997 [85] | Wales | Cross-sectional survey | General public | 241 |
| Lester, Donnelly & Assar 2000 [86] | UK | Cross-sectional survey | Participants who had attended a CPR course | 416 |
| Liaw et al. 2020 [87] | Malaysia | Before and after study | University employees (non-medical) | 184 |
| Locke et al. 1995 [88] | USA | Cross-sectional survey | Lay people (minimum age not reported) & health care providers | 975 |
| Lu et al. 2017 [89] | China | Cross-sectional survey | College students | 609 |
| Lynch & Einspruch 2010 [90] | USA | Randomised Controlled Trial | Adults (≥18 years) | 1065 |
| Maes et al. 2015 [91] | Belgium | Before and after study | Hospital visitors (≥13 years) | 85 |
| Magid et al. 2019 [92] | USA | Cross-sectional survey | College students | 588 |
| Mathiesen et al. 2017 [93] | Norway | Qualitative: interviews | Witnesses of an OHCA | 10 |
| Mausz, Snobelen & Tavares 2018 [94] | Canada | Qualitative: interviews/focus groups | Witnesses of an OHCA | 15 |
| McCormack, Damon & Einsenberg 1989 [95] | USA | Cross-sectional survey | Witnesses of an OHCA | 34 |
| Mecrow et al. 2015 [96] | Bangladesh | Cross-sectional survey | Lay people (≥10 years) | 721 |
| Meischke et al. 2002 [97] | USA | Cross-sectional survey | Older adults (minimum age not reported) | 159 |
| Moller et al. 2014 [98] | Denmark | Qualitative: interviews | Witnesses of an OHCA | 33 |
| Nielsen et al. 2013 [99] | Denmark | Before and after study | Adults (≥15 years) | 1639 |
| Nishiyama et al. 2019 [100] | Japan | Cross-sectional survey | University students | 5549 |
| Nolan et al. 1999 [101] | Canada | Cross-sectional survey | Adults (≥45 years) | 786 |
| Nord et al. 2016 [102] | Sweden | Cluster randomised trial | Schoolchildren | 1124 |
| Nord et al. 2017 [103] | Sweden | Cluster randomised trial | Schoolchildren | 587 |
| Omi et al. 2008 [104] | Japan | Cross-sectional survey | High school students | 3316 |
| Onan et al. 2018 [105] | Turkey | Quasi-experimental study | High school students (aged 17–18) | 77 |
| Parnell et al. 2006 [106] | New Zealand | Cross-sectional survey | High school students | 494 |
| Pei-Chuan Huang et al. 2019 [107] | Taiwan | Cross-sectional survey | Adults (≥20 years) | 1073 |
| Platz et al. 2000 [108] | USA | Cross-sectional survey | Family members of patients at risk of cardiac arrest | 100 |
| Rankin et al. 2020 [109] | Australia | Cross-sectional survey | Adults (18–21 years) | 178 |
| Riou et al., 2020 [110] | Australia | Retrospective analysis of emergency calls for OHCA | Call to Ambulance service with OHCA where caller initially did not agree to perform CPR | 65 |
| Ro et al. 2016 [111] | Korea | Cross-sectional survey | Adults (≥19 years) | 62,425 |
| Rowe et al. 1998 [112] | Canada | Cross-sectional survey | Adults (≥44 years) | 811 |
| Sasaki et al. 2015 [113] | Japan | Cross-sectional survey | Adults (≥15 years) | 4853 |
| Sasson et al. 2013 [114] | USA | Qualitative: focus groups | Laypeople (minimum age not stated) | 42 |
| Sasson et al. 2015 [115] | USA | Qualitative: focus groups | Laypeople (≥13 years) | 64 |
| Schmid et al. 2016 [116] | Costa Rica | Cross-sectional survey | Laypeople (minimum age not stated) | 370 |
| Schmitz et al. 2015 [117] | Netherlands | Randomised Controlled Trial | High school students | 201 |
| Schneider et al. 2004 [118] | Austria | Before and after study | Survivors of OHCA and people who know them | 112 |
| Shams et al. 2016 [119] | Lebanon | Cross-sectional survey | University students | 948 |
| Shibata et al. 2000 [120] | Japan | Cross-sectional survey | High school students and teachers | 626 |
| Sipsma, Stubbs & Plorde 2011 [121] | USA | Cross-sectional survey | Adults (≥18 years) | 1001 |
| Skora & Riegel 2001 [122] | USA | Cross-sectional survey (qualitative analysis) | Laypersons who had provided out-of-hospital CPR to strangers | 12 |
| Smith et al. 2003 [123] | Australia | Cross-sectional survey | Householders (age not reported) | 1489 |
| Sneath & Lacey 2009 [124] | USA | Cross-sectional survey | Adults (≥18 years) | 78 |
| So et al. 2020 [125] | Hong Kong | Before and after study | High school students (12–15 years) | 128 |
| Swor et al. 2006 [20] | USA | Cross-sectional survey | Witnesses of an OHCA | 684 |
| Swor et al. 2013 [126] | USA | Cross-sectional survey | Witnesses of an OHCA | 30 |
| Tang et al. 2020 [127] | China | Cross-sectional survey | High school students (senior, age NR) | 397 |
| Taniguchi, Omi & Inaba 2007 [128] | Japan | Cross-sectional survey | High school students and teachers | 3444 |
| Taniguchi et al. 2012 [129] | Japan | Cross-sectional survey | High school students and teachers | 1946 |
| Thorén et al. 2010 [130] | Sweden | Qualitative: interviews | Partners of people who experienced OHCA | 15 |
| Vaillancourt et al. 2013 [131] | Canada | Cross-sectional survey | Adults (≥55 years) | 192 |
| Vetter et al. 2016 [132] | USA | Non-randomised trial | High school students | 412 |
| Wilks et al. 2015 [133] | Hong Kong | Cross-sectional survey | Secondary school students (15–16 years) | 383 |
| Winkelman et al. 2009 [134] | USA | Cross-sectional survey | Teacher candidates | 582 |
| Zinckernagel et al. 2016 [135] | Denmark | Qualitative: interviews and focus groups | Secondary school leaders and teachers | 25 |
Methodological quality
Of the quantitative studies, four [58, 69, 103, 110] were identified as strong, six as moderate [83, 90, 102, 117, 125, 131] with the remaining 87 quantitative studies rated ‘weak’ (see Table 2). There was a predominance of non-randomised designs, uncontrolled confounders, and use of unvalidated data collection methods. All qualitative studies were assessed as of sufficient quality for inclusion but also varied in quality (n = 8).
Table 2.
EPHPP Quality Assessment of included studies
| Selection Bias | Study Design | Confounders | Blinding | Data Collection Method | Withdrawals & Drop outs | Global rating | |
|---|---|---|---|---|---|---|---|
| Aaberg et al. 2014 [32] | Moderate | Moderate | Strong | Weak | Weak | Moderate | Weak |
| Alhussein et al. 2021 [33] | Moderate | Weak | Strong | Weak | Strong | Moderate | Weak |
| Alshudukhi et al. 2018 [34] | Weak | Weak | Weak | Weak | Weak | Moderate | Weak |
| Anto-Ocra et al. [35] | Moderate | Weak | Strong | Weak | Moderate | Moderate | Weak |
| Axelsson et al. 1996 [36] | Moderate | Weak | Weak | Weak | Weak | Moderate | Weak |
| Axelsson et al. 2000 [37] | Moderate | Weak | Weak | Weak | Moderate | Moderate | Weak |
| Babic et al. 2020 [38] | Weak | Weak | Weak | Weak | Weak | Moderate | Weak |
| Becker et al. 2019 [39] | Moderate | Weak | Weak | Weak | Weak | Moderate | Weak |
| Bin et al. 2013 [40] | Weak | Weak | Weak | Weak | Weak | Moderate | Weak |
| Birkun & Kosova 2018 [41] | Moderate | Weak | Weak | Weak | Strong | Moderate | Weak |
| Bohn et al. 2012 [42] | Moderate | Moderate | Weak | Weak | Weak | Weak | Weak |
| Bouland et al. 2017 [43] | Moderate | Weak | Weak | Weak | Moderate | Strong | Weak |
| Bray et al. 2017 [44] | Moderate | Weak | Weak | Weak | Weak | Moderate | Weak |
| Breckwoldt, Scholesser & Arntz 2009 [45] | Moderate | Weak | Weak | Weak | Weak | Moderate | Weak |
| Brinkrolf et al. 2018 [46] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Case et al. 2018 [47] | Moderate | Weak | Weak | Moderate | Strong | Moderate | Weak |
| Chen et al. 2017 [48] | Weak | Weak | Weak | Weak | Weak | Strong | Weak |
| Cheng et al. 1997 [49] | Weak | Weak | Moderate | Weak | Weak | Strong | Weak |
| Cheng-Yu et al. 2016 [50] | Moderate | Weak | Weak | Weak | Weak | Weak | Weak |
| Cheskes et al. 2016 [51] | Moderate | Weak | Weak | Weak | Strong | Moderate | Weak |
| Chew et al. 2009 [52] | Weak | Weak | Weak | Weak | Weak | Moderate | Weak |
| Chew et al. 2019 [53] | Weak | Weak | Moderate | Weak | Strong | Weak | Weak |
| Cho et al. 2010 [54] | Moderate | Moderate | Weak | Weak | Weak | Moderate | Weak |
| Compton et al. 2003 [55] | Strong | Weak | Weak | Weak | Weak | Moderate | Weak |
| Coons & Guy 2009 [56] | Moderate | Weak | Weak | Moderate | Strong | Weak | Weak |
| Cu, Phan & O’Leary 2009 [57] | Moderate | Weak | Weak | Weak | Strong | Weak | Weak |
| Dami et al. 2010 [58] | Strong | Moderate | Moderate | Moderate | Strong | Moderate | Strong |
| De Smedt et al. 2018 [59] | Weak | Weak | Weak | Weak | Moderate | Moderate | Weak |
| Dobbie et al. 2018 [60] | Moderate | Weak | Weak | Weak | Strong | Weak | Weak |
| Dracup et al. 1994 [62] | Moderate | Moderate | Weak | Moderate | Weak | Moderate | Weak |
| Dwyer 2008 [63] | Moderate | Weak | Weak | Weak | Moderate | Weak | Weak |
| Enami et al. 2010 [64] | Weak | Weak | Weak | Moderate | Weak | Weak | Weak |
| Fratta et al. 2020 [65] | Moderate | Weak | Moderate | Weak | Weak | Moderate | Weak |
| Han et al. 2018 [66] | Moderate | Weak | Weak | Weak | Weak | Weak | Weak |
| Hauff et al. 2003 [67] | Weak | Weak | Weak | Moderate | Strong | Moderate | Weak |
| Hawkes et al. 2019 [68] | Moderate | Weak | Weak | Weak | Weak | Moderate | Weak |
| Hollenberg et al. 2019 [69] | Moderate | Strong | Strong | Moderate | Strong | Strong | Strong |
| Huang, Hu & Mao 2016 [70] | Weak | Weak | Weak | Weak | Moderate | Moderate | Weak |
| Hubble et al. 2003 [71] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Hung et al. 2017 [72] | Weak | Weak | Weak | Weak | Strong | Strong | Weak |
| Iserbyt 2016 [73] | Weak | Weak | Weak | Weak | Moderate | Strong | Weak |
| Jelinek et al. 2001 [74] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Johnston et al. 2003 [75] | Moderate | Weak | Weak | Moderate | Strong | Weak | Weak |
| Kandakai & King 1999 [76] | Weak | Weak | Weak | Weak | Strong | Weak | Weak |
| Kanstad, Nilsen & Fredriksen 2011 [77] | Weak | Weak | Weak | Moderate | Weak | Weak | Weak |
| Karuthan et al. 2019 [78] | Moderate | Weak | Moderate | Weak | Weak | Moderate | Weak |
| Kua et al. 2018 [79] | Weak | Weak | Weak | Moderate | Weak | Moderate | Weak |
| Kuramoto et al. 2008 [80] | Weak | Weak | Weak | Weak | Moderate | Weak | Weak |
| Lam et al. 2007 [81] | Weak | Weak | Weak | Weak | Weak | Moderate | Weak |
| Lee et al. 2013 [82] | Moderate | Weak | Weak | Weak | Moderate | Weak | Weak |
| Lerner et al. 2008 [83] | Strong | Moderate | Moderate | Moderate | Weak | Moderate | Moderate |
| Lester, Donnelly & Weston 1997 [84] | Weak | Weak | Weak | Weak | Weak | Strong | Weak |
| Lester, Donnelly & Assar 1997 [85] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Lester, Donnelly & Assar 2000 [86] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Liaw et al. 2020 [87] | Weak | Weak | Moderate | Weak | Weak | Moderate | Weak |
| Locke et al. 1995 [88] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Lu et al. 2016 [89] | Weak | Weak | Weak | Weak | Moderate | Strong | Weak |
| Lynch & Einspruch 2010 [90] | Moderate | Moderate | Weak | Moderate | Moderate | Moderate | Moderate |
| Maes et al. 2015 [91] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Magid et al. 2019 [92] | Weak | Weak | Weak | Weak | Moderate | Strong | Weak |
| Mecrow et al. 2015 [96] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Meischke et al. 2002 [97] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Nielsen et al. 2013 [99] | Moderate | Weak | Moderate | Moderate | Weak | Moderate | Weak |
| Nishiyama et al. 2019 [100] | Moderate | Weak | Moderate | Weak | Weak | Moderate | Weak |
| Nolan et al. 1999 [101] | Moderate | Strong | Weak | Moderate | Weak | Weak | Weak |
| Nord et al. 2016 [102] | Strong | Strong | Weak | Strong | Strong | Moderate | Moderate |
| Nord et al. 2017 [103] | Moderate | Moderate | Moderate | Moderate | Moderate | Strong | Strong |
| Omi et al. 2008 [104] | Moderate | Weak | Weak | Weak | Weak | Strong | Weak |
| Onan et al. 2018 [105] | Weak | Weak | Weak | Weak | Weak | Strong | Weak |
| Parnell et al. 2006 [106] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Pei-Chuan Huang et al. 2019 [107] | Moderate | Moderate | Weak | Weak | Strong | Weak | Weak |
| Platz et al. 2000 [108] | Weak | Weak | Weak | Weak | Moderate | Strong | Weak |
| Rankin et al. 2020 [109] | Weak | Weak | Moderate | Weak | Weak | Moderate | Weak |
| Riou et al. 2020 [110] | Strong | Moderate | Moderate | Moderate | Strong | Strong | Strong |
| Ro et al. 2016 [111] | Moderate | Weak | Weak | Weak | Strong | Weak | Weak |
| Rowe et al. 1998 [112] | Moderate | Weak | Weak | Weak | Moderate | Weak | Weak |
| Sasaki et al. 2015 [113] | Moderate | Weak | Weak | Moderate | Weak | Weak | Weak |
| Schmid et al. 2016 [116] | Weak | Weak | Weak | Weak | Moderate | Strong | Weak |
| Schmitz et al. 2015 [117] | Moderate | Strong | Weak | Moderate | Moderate | Moderate | Moderate |
| Schneider et al. 2004 [118] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Shams et al. 2016 [119] | Moderate | Weak | Weak | Weak | Weak | Moderate | Weak |
| Shibata et al. 2000 [120] | Weak | Weak | Weak | Weak | Weak | Moderate | Weak |
| Sipsma, Stubbs & Plorde 2011 [121] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Skora & Riegel 2001 [122] | Weak | Weak | Weak | Moderate | Weak | Moderate | Weak |
| Smith et al. 2003 [123] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Sneath & Lacey 2009 [124] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| So et al. 2020 [125] | Moderate | Moderate | Moderate | Weak | Moderate | Strong | Moderate |
| Swor et al. 2006 [20] | Moderate | Moderate | Weak | Weak | Weak | Moderate | Weak |
| Swor et al. 2013 [126] | Weak | Weak | Weak | Moderate | Weak | Moderate | Weak |
| Tang et al. 2020 [127] | Moderate | Weak | Moderate | Weak | Weak | Moderate | Weak |
| Taniguchi, Omi & Inaba 2007 [128] | Weak | Weak | Weak | Weak | Weak | Moderate | Weak |
| Taniguchi et al. 2012 [129] | Weak | Weak | Weak | Weak | Weak | Moderate | Weak |
| Vaillancourt et al. 2013 [131] | Moderate | Moderate | Weak | Strong | Moderate | Moderate | Moderate |
| Vetter et al. 2016 [132] | Weak | Weak | Weak | Weak | Weak | Weak | Weak |
| Wilks et al. 2015 [133] | Moderate | Weak | Moderate | Weak | Moderate | Moderate | Weak |
| Winkelman et al. 2009 [134] | Weak | Weak | Weak | Weak | Moderate | Moderate | Weak |
| Zinckernagel et al. 2016 [135] | Weak | Weak | Weak | Weak | Moderate | Strong | Weak |
The psychological and behavioural factors identified from the included studies are reported below and summarised in Tables 3, 4, 5, 6, 7, 8, 9 and 10 below. Studies were divided into subgroups according to the study population (i.e. results from those with direct experience versus general samples responding to a ‘hypothetical’ OHCA); study design and statistics used. Data were further categorised depending on whether the ‘predictor’ was identified by participants in response to an open question or whether it was presented as a possible factor and subsequently endorsed. Factors are presented in relation to the domains of the Theoretical Domains Framework so that theoretically similar factors are grouped together and can be compared across study designs (Fig. 2).
Table 3.
Psychological and behavioural factors associated with LOWER actual/intended CPR initiation (grouped using Theoretical Domains Framework V.2 [29])
| Factor related to reluctance | Participants | Number (total) | Number in analysis for each factor | Unprompted identification of each factor (% of whole sample and % of unwilling subsample) | Endorsement of each factor when prompted (% of whole sample and % of unwilling subsample) | |
|---|---|---|---|---|---|---|
| 6. Beliefs about Consequences | ||||||
| Concerns about doing something wrong | ||||||
| Aaberg et al. 2014 [32] | High School students | 399 | 399 responding as to their worst fear | NR (1 of 3 qualitative themes identified) | ||
| Compton et al. 2003 [55] | School teachers | 201 | 180 | 71% of untrained | ||
| 42% of trained | ||||||
| Coons & Guy 2009 [56] | Adults (≥18) | 755 | 435 (who endorsed reasons) | 20% (stranger) | ||
| 22.5% (family) | ||||||
| Dwyer 2008 [56] | Adults (≥18) | 1208 | 379 (not confident) | 55% | ||
| Iserbyt 2016 [63] | Secondary school pupils | 313 | 313 | 38% (girls) | ||
| 26% (boys) | ||||||
| Nolan et al. 1999 [101] | Adults (≥45) | 786 | 203 (not ready to perform CPR) | 53% | ||
| Onan et al. 2018 [105] | High School students | 83 | 83 | NR (concern identified) | ||
| Sasson et al. 2013 [114] | Lay-people (min age not stated) | 42 | 42 | NR (1 of 10 qualitative barriers) | ||
| Swor 2006 [20] | Witnesses of OHCA | 684 | 279 (did not perform CPR) | 11% | ||
| Tang et al. 2020 [127] | High school students (senior, age NR) | 397 | 397 | 78% (fail to meet professional standards) | ||
| Zinckernagel et al. 2016 [135] | Secondary school leaders and teachers | 25 | 25 | NR (a qualitative theme identified) | ||
| Concerns about doing harm | ||||||
| Aaberg et al. 2014 [32] | High School students | 399 | 399 responding as to their worst fear | NR (1 of 3 qualitative themes identified) | ||
| Alhussein 2021 [33] | Adults (≥18) | 856 | Those whose source of knowledge was media sources (largest group) (n = 331) | Break rib 22% (family/friend) | ||
| Break rib 21% (stranger) | ||||||
| Organ damage 14% (family/friend) | ||||||
| Organ damage 12% (stranger) | ||||||
| Stopping heart 8% (family/friend) | ||||||
| Stopping heart 5% (stranger) | ||||||
| Anto-Ocra et al. 2020 [35] | Adults (≥18 years) | 277 | 277 | 35% | ||
| Babic et al. 2020 [38] | Adults (≥18 years) | 198 | 198 | 15% (MMV) | ||
| 23% (compressions) | ||||||
| Becker et al. 2019 [39] | Adults (≥18 years) who attended CPR training event | 677 | 306 resp. concerns elderly patient | 63% | ||
| 249 resp. concerns for woman | 21% | |||||
| 291 resp. concerns for child | 51% | |||||
| Cheng-Yu et al. 2016 [50] | Adults (≥20) | 401 | 144 (unwilling to perform on stranger) | 11% | ||
| Compton et al. 2003 [55] | School teachers | 201 | 180 | 64% of untrained | ||
| 41% of trained | ||||||
| Coons & Guy 2009 [56] | Adults (≥18) | 755 | 435 (who endorsed reasons) | 19.4% stranger | ||
| 26.4% (family) | ||||||
| Cu 2009 [50] | Caregivers of children presenting to the Emergency Department (≥18 years) | 348 | 125 (unwilling to perform CPR on adult) | 38% | ||
| Dami 2010 [51] | Call to Dispatch Centre with OHCA | 738 | 73 medically appropriate who refused | 3% | ||
| Dobbie 2018 [53] | Adults (≥16 years) | 1027 | 1027 | 22% | ||
| Donohoe 2006 [54] | Adults (≥16 years) | NR | Focus groups (NR) | NR (Qualitative theme identified) | ||
| Dwyer 2008 [56] | Adults (≥18) | 1208 | 379 (not confident) | 10% | ||
| Han 2018 [58] | Family members (≥18 years) of patients at risk of cardiac arrest | 203 | 88 | 7% | ||
| Huang 2016 [60] | School and University students (13–21 years) | 1407 | 546 (unwilling to perform on stranger) | 68% | ||
| Hubble 2003 [61] | High school students | 683 | 683 | 25% (MMV) | ||
| 31% (AED) | ||||||
| 25% (CC) | ||||||
| Hung 2017 [62] | College and University students (≥15 years) | 351 | 351 | 26% | ||
| Kandakai & King 1999 [76] | College students | 214 | 214 | 65% | ||
| Kanstad, Nilsen & Fredriksen 2011 [77] | Secondary school students (16–19 years) | 376 | 376 | 17% | ||
| Karuthan et al. 2019 [78] | College students | 393 | 393 | 5% (HO stranger) | ||
| 3% (HO family-member) | ||||||
| Kua et al. 2018 [79] | School students (11–17 years) | 1196 | 966 | 58% | ||
| Liaw et al. 2020 [87] | University employees (non-medical) | 184 | NR | Fear and concern identified as significantly reduced by training in 54% | ||
| Maes et al. 2015 [91]a | Hospital visitors (≥13 years) | 85 | 51 who did not feel able to use AED | 2% | ||
| Omi 2008 [91] | High school students | 3316 | 2203 unwilling to perform CPR | 23% | ||
| Onan et al. 2018 [105] | High School students | 83 | 83 | NR (concern identified) | ||
| Magid et al. 2019 [92] | College students | 588 | 300 (who identified barriers) | 52% | ||
| Pei-Chuan Huang et al. 2019 [107] | Adults (≥20) | 1073 | 141 (who provided reasons why not) | 36.5% | ||
| Platz et al. 2000 [108] | Family members of patients at risk of cardiac arrest | 100 | 100 | 49% | ||
| Rankin et al. 2020 [109] | Adults (18–21 years) | 178 | Not CPR trained, for family 76% | |||
| CPR trained, for family 67% | ||||||
| Not CPR trained, for stranger 69% | ||||||
| CPR trained, for stranger 57% | ||||||
| Sasson et al. 2013 [114] | Lay-people (min age not stated) | 42 | 42 | NR (1 of 10 qualitative barriers) | ||
| Schmid et al. 2016 [116] | Laypeople (minimum age not stated) | 370 | 370 | 17.30% | ||
| Shams et al. 2016 [119] | University students | 948 | 948 | 53% | ||
| So et al. 2020 [125] | High school students (12–15 years) | 128 | NR | 94% | ||
| Swor 2006 [20] | Witnesses of OHCA | 684 | 279 (did not perform CPR) | 2% | ||
| Taniguchi 2012 [112] | High school students and teachers | 1946 | 1708 (students on a stranger) | 14% | ||
| Thoren 2010 [113] | Partners of people who experienced OHCA | 15 | 15 | NR (Qualitative theme identified) | ||
| Wilks et al. 2015 [133] | Secondary school students (15–16 years) | 383 | NR | 28% | ||
| Concern about being the cause of the person’s death | ||||||
| Aaberg et al. 2014 [32] | High School students | 399 | 399 responding as to their worst fear | NR (1 of 3 qualitative themes identified) | ||
| Becker et al. 2019 [39] | Adults (≥18 years) who attended CPR training event | 677 | 306 resp. concerns elderly patient | 6% | ||
| 249 resp. concerns for woman | 2% | |||||
| 291 resp. concerns for child | 4% | |||||
| Nolan et al. 1999 [101] | Adults (≥45) | 786 | 203 (not ready to perform CPR) | 40% | ||
| Onan et al. 2018 [105] | High School students | 83 | 83 | NR (concern identified) | ||
| Tang et al. 2020 [127] | High school students (senior, age NR) | 397 | 397 | 9% (fear of treating dying person) | ||
| Belief CPR futile | ||||||
| Axelsson et al. 1996 [36] | People who reported making a CPR attempt between 1990 and 1994 | 742 | 51 bystanders described hesitation | NR | ||
| Case et al. 2018 [47] | OHCA Calls | 120 | 120 calls where no CPR given | 28% | ||
| Hauff 2003 [59] | Call to Dispatch Centre with OHCA | 404 | 52 who did not accept CPR instructions | 23% | ||
| Nolan et al. 1999 [101] | Adults (≥45) | 786 | 203 (not ready to perform CPR) | 34% | ||
| Riou et al. 2020 [110] | Retrospective analysis of emergency calls for OHCA | 65 | 57 (where caller responded with an account) | 50% expressed an ‘epistemic’ account – i.e. too late or futile | ||
| Skora & Riegel 2001 [122] | Previously performed CPR | 12 | 12 participants | NR (Qualitative theme identified) | ||
| Swor 2006 [20] | Witnesses of OHCA | 684 | 279 (did not perform CPR) | 4% | ||
| Belief CPR does not work | ||||||
| Babic et al. 2020 [38] | Adults (≥18 years) | 198 | 198 | 0.5% (MMV) | ||
| 1% (compressions) | ||||||
| Schmid et al. 2016 [116] | Laypeople (minimum age not stated) | 370 | 370 | 10% | ||
| Shams et al. 2016 [119] | University students | 948 | 948 | 9% | ||
| Violates beliefs about death | ||||||
| Hubble 2003 [61] | High school students | 683 | 683 | 4% (MMV) | ||
| 4% (AED) | ||||||
| 4% (CC) | ||||||
| Schmid et al. 2016 [116] | Laypeople (minimum age not stated) | 370 | 370 | 5% | ||
| Concerns about MMV | ||||||
| Anto-Ocra et al. 2020 [35] | Adults (≥18 years) | 277 | 277 | 5% | ||
| Axelsson et al. 1996 [36] | People who reported making a CPR attempt between 1990 and 1994 | 742 | 51 bystanders described hesitation | NR | ||
| Cheng-Yu et al. 2016 [50] | Adults (≥20) | 401 | 144 (unwilling to perform on stranger) | 46% | ||
| Cho et al. 2010 [54] | Lay people aged 11 years and over | 890 | 539 (unwilling to perform CPR) | 17% | ||
| Coons & Guy 2009 [56] | Adults (≥18) | 755 | 435 (who endorsed reasons) | 19% (stranger) | ||
| 16.5% (family) | ||||||
| Dobbie 2018 [53] | Adults (≥16 years) | 1027 | 1027 | 7% | ||
| Donohoe 2006 [54] | Adults (≥16 years) | NR | Focus groups (NR) | NR (Qualitative theme identified) | ||
| Iserbyt 2016 [63] | Secondary school pupils | 313 | 313 | 19% (girls) | ||
| 10% (boys) | ||||||
| Pei-Chuan Huang et al. 2019 [107] | Adults (≥20) | 1073 | 141 (who provided reasons why not) | 13% | ||
| Sasson et al. 2013 [114] | Lay-people (min age not stated) | 42 | 42 | NR (1 of 10 qualitative barriers identified) | ||
| Schmid et al. 2016 [116] | Laypeople (minimum age not stated) | 370 | 370 | 18% | ||
| Shams et al. 2016 [119] | University students | 948 | 948 | 19% | ||
| Swor 2006 [20] | Witnesses of OHCA | 684 | 279 (did not perform CPR) | 1% | ||
| Concern about legal ramifications | ||||||
| Alhussein 2021 [33] | Adults (≥18) | 856 | Those whose source of knowledge was media sources (largest group) (n = 331) | 5% (family/friend) | ||
| 22% (stranger) | ||||||
| Alshudukhi et al. 2018 [34] | Adults (≥18) | 310 | 168 unwilling to perform CPR | 2% | ||
| Anto-Ocra et al. 2020 [35] | Adults (≥18 years) | 277 | 277 | 8% | ||
| Chen et al. 2017 [48] | Adult laypersons (≥18 yrs) + 3 < 18 years | 1841 | 1841 | 53% | ||
| Cheng-Yu et al. 2016 [50] | Adults (≥20) | 401 | 144 (unwilling to perform on stranger) | 37% | ||
| Cho et al. 2010 [54] | Lay people aged 11 years and over | 890 | 539 (unwilling to perform CPR) | 55% | ||
| Compton et al. 2003 [55] | School teachers | 201 | 180 | 52% of untrained | ||
| 54% of trained | ||||||
| Coons & Guy 2009 [56] | Adults (≥18) | 755 | 435 (who endorsed reasons) | 20.9% (stranger) | ||
| 12.1% (family) | ||||||
| Dobbie 2018 [53] | Adults (≥16 years) | 1027 | 1027 | 8% | ||
| Donohoe 2006 [54] | Adults (≥16 years) | NR | Focus groups (NR) | NR (Qualitative theme identified) | ||
| Huang 2016 [60] | School and University students (13–21 years) | 1407 | 546 (unwilling to perform on stranger) | 91% | ||
| Hubble 2003 [61] | High school students | 683 | NR | 16% (MMV) | ||
| 17% (AED) | ||||||
| 13% (CC) | ||||||
| Hung 2017 [62] | College and University students (≥15 years) | 351 | 351 | 17% | ||
| Iserbyt 2016 [63] | Secondary school pupils | 313 | 313 | 4% (girls) | ||
| 6% (boys) | ||||||
| Jelinek 2001 [64] | General public (age not reported) | 803 | 84 unwilling to perform MMV | 4% | ||
| 26 unwilling to perform CC | 19% | |||||
| Johnston 2003 [65] | Adults (≥18 years) | 4490 | 4490 | 2% | ||
| Kandakai & King 1999 [76] | College students | 214 | 214 | 48% | ||
| Karuthan et al. 2019 [78] | College students | 393 | 393 | 1% (HO stranger) | ||
| 1% (HO family-member) | ||||||
| Lerner et al. 2008 [83] | Call to Dispatch Centre with OHCA | 168 | 145 who did not follow CPR instructions | 1% | ||
| Liaw et al. 2020 [87] | University employees (non-medical) | 184 | NR | Fear and concern identified as significantly reduced by training in 59% | ||
| Lu et al. 2016 [89] | College students | 609 | 609 (non-medical) | 7–21% (dep on subject) | ||
| Nolan et al. 1999 [101] | Adults (≥45) | 786 | 203 (not ready to perform CPR) | 38% | ||
| Pei-Chuan Huang et al. 2019 [107] | Adults (≥20) | 1073 | 141 (who provided reasons why not) | 44% | ||
| Rankin et al. 2020 [109] | Adults (18–21 years) | 178 | Not CPR trained, for family 32% | |||
| CPR trained, for family 26% | ||||||
| Not CPR trained, for stranger 60% | ||||||
| CPR trained, for stranger 75% | ||||||
| Sasson et al. 2013 [114] | Lay-people (min age not stated) | 42 | 42 | NR (1 of 10 qualitative barriers identified) | ||
| Sasson et al. 2015 [115] | Lay-people (≥13) | 64 | 64 | NR (qualitative barrier identified) | ||
| Schmid et al. 2016 [116] | Laypeople (minimum age not stated) | 370 | 370 | 30% | ||
| Shams et al. 2016 [119] | University students | 948 | 948 | 25% | ||
| So et al. 2020 [125] | High school students (12–15 years) | 128 | NR | 52% | ||
| Tang et al. 2020 [127] | High school students (senior, age NR) | 397 | 397 | 67% | ||
| Wilks et al. 2015 [133] | Secondary school students (15–16 years) | 383 | NR | 14% | ||
| Winkelman et al. 2009 [134] | Teacher candidates | 582 | 47 | 17% | ||
| Concerns about risk to self | ||||||
| Becker et al. 2019 [39] | Adults (≥18 years) who attended CPR training event | 677 | 306 resp. concerns elderly patient | 2% | ||
| 249 resp. concerns for woman | 2% | |||||
| 291 resp. concerns for child | 1% | |||||
| Cu 2009 [50] | Caregivers of children presenting to the Emergency Department (≥18 years) | 348 | 125 (unwilling to perform CPR on adult) | 3% | ||
| Hubble 2003 [61] | High school students | 683 | NR | 7% (MMV) | ||
| 10% (AED) | ||||||
| 6% (CC) | ||||||
| Jelinek 2001 [64] | General public (age not reported) | 803 | 84 unwilling to perform MMV | 56% | ||
| Johnston 2003 [65] | Adults (≥18 years) | 4490 | 4490 | 4.50% | ||
| Lester, Donnelly & Weston 1997 [84] | First year high school pupils | 233 | 233 | 11% | ||
| Liaw et al. 2020 [87] | University employees (non-medical) | 184 | NR | Fear and concern identified as significantly reduced by training in 34% | ||
| Mathiesen et al. 2017 [93] | Witnesses of OHCA | 10 | 10 | NR (qualitative barrier identified) | ||
| Sasson et al. 2013 [114] | Lay-people (min age not stated) | 42 | 42 | NR (1 of 10 qualitative barriers) | ||
| Sasson et al. 2015 [115] | Lay-people (≥13) | 64 | 64 | NR (qualitative barrier identified) | ||
| Concerns about risk of infection | ||||||
| Alhussein 2021 [33] | Adults (≥18) | 856 | Those whose source of knowledge was media sources (largest group) (n = 331) | 2% (family/friend) | ||
| 5% (stranger) | ||||||
| Anto-Ocra et al. 2020 [35] | Adults (≥18 years) | 277 | 277 | 18% | ||
| Axelsson et al. 2000 [37] | Adults (≥18 years) who had received training in basic CPR in January 1997. | 1012 | 1012 | 8% | ||
| Babic et al. 2020 [38] | Adults (≥18 years) | 198 | 198 | 15% (MMV) | ||
| 0.5% (compressions) | ||||||
| Chen et al. 2017 [48] | Adult laypersons (≥18 yrs) + 3 < 18 years | 1841 | 1841 | 2% | ||
| Cheskes et al. 2016 [51] | Adult (≥18 yrs) | 428 | NR | 24% | ||
| Cho et al. 2010 [54] | Lay people aged 11 years and over | 890 | 539 (unwilling to perform CPR) | 10% | ||
| Compton et al. 2003 [55] | School teachers | 201 | 180 | 50% of untrained | ||
| 58% of trained | ||||||
| Dami 2010 [51] | Call to Dispatch Centre with OHCA | 738 | 73 medically appropriate who refused | 4% | ||
| Dobbie 2018 [53] | Adults (≥16 years) | 1027 | 1027 | 10% | ||
| Donohoe 2006 [54] | Adults (≥16 years) | NR | Focus groups (n NR) | NR (Qualitative theme identified) | ||
| Dwyer 2008 [56] | Adults (≥18) | 1208 | 379 (not confident) | 1% | ||
| Han 2018 [58] | Family members (≥18 years) of patients at risk of cardiac arrest | 203 | 88 | 1% | ||
| Huang 2016 [60] | School and University students (13–21 years) | 1407 | 546 (unwilling to perform on stranger) | 24% | ||
| Hubble 2003 [61] | High school students | 683 | NR | 35% (MMV) | ||
| 11% (AED) | ||||||
| 12% (CC) | ||||||
| Hung 2017 [62] | College and University students (≥15 years) | 351 | 351 | 8% | ||
| Iserbyt 2016 [63] | Secondary school pupils | 313 | 313 | 10% (girls) | ||
| 11% (boys) | ||||||
| Jelinek 2001 [64] | General public (age not reported) | 803 | 84 unwilling to perform MMV | 19% (MMV) | ||
| Johnston 2003 [65] | Adults (≥18 years) | 4490 | 4490 | 18% | ||
| Kanstad, Nilsen & Fredriksen 2011 [77] | Secondary school students (16–19 years) | 376 | 376 | 6% | ||
| Karuthan et al. 2019 [78] | College students | 393 | 393 | 3% (HO stranger) | ||
| 1% (HO family-member) | ||||||
| Lee et al. 2013 [82] | College students | 2029 | 242 (unwilling to perform CPR) | < 1% | ||
| Lester, Donnelly & Weston 1997 [84] | First year high school pupils | 233 | 233 | 12% (7% HIV, 5% other) | ||
| Lester, Donnelly & Assar 1997 [85] | General public | 241 | 241 | 8% (5% HIV, 3% other) | ||
| Liaw et al. 2020 [87] | University employees (non-medical) | 184 | NR | Fear and concern identified as significantly reduced by training in 34% | ||
| Lu et al. 2016 [89] | College students | 609 | 609 (non-medical) | 10–45% (dep on subject) | ||
| Nolan et al. 1999 [101] | Adults (≥45) | 786 | 203 (not ready to perform CPR) | 36% | ||
| Omi 2008 [91] | High school students | 3316 | 2203 unwilling to perform CPR | 11% (of 2203 who were unwilling) | ||
| Pei-Chuan Huang et al. 2019 [107] | Adults (≥20) | 1073 | 141 (who provided reasons why not) | 28% | ||
| Platz et al. 2000 [108] | Family members of patients at risk of cardiac arrest | 100 | 100 | 9% | ||
| Rankin et al. 2020 [109] | Adults (18–21 years) | 178 | Not CPR trained, for family 6% | |||
| CPR trained, for family 15% | ||||||
| Not CPR trained, for stranger 32% | ||||||
| CPR trained, for stranger 44% | ||||||
| Shams et al. 2016 [119] | University students | 948 | 948 | 33% | ||
| Shibata 2000 [105] | Schoolchildren and teachers | 626 | NR | 5% | ||
| So et al. 2020 [125] | High school students (12–15 years) | 128 | NR | 28% | ||
| Skora & Riegel 2001 [122] | Previously performed CPR | 12 | 12 participants | 8% | ||
| Tang et al. 2020 [127] | High school students (senior, age NR) | 397 | 397 | 23% | ||
| Taniguchi 2007 [111] | High school students and teachers | 3444 | 3444 | 10% | ||
| Taniguchi 2012 [112] | High school students and teachers | 1946 | 1708 students on a stranger | 7% | ||
| Wilks et al. 2015 [133] | Secondary school students (15–16 years) | 383 | NR | 6% | ||
| Winkelman et al. 2009 [134] | Teacher candidates | 582 | 47 | 30% | ||
| Delaying CPR won’t do harm | ||||||
| Magid et al. 2019 [92] | College students | 588 | 300 (who identified barriers) | 3.5% | ||
| Concerns about substance use | ||||||
| Drugs | ||||||
| Dobbie 2018 [53] | Adult (> 16) | 1027 | 1027 | 16% | ||
| Johnston 2003 [65] | Adults (≥18 years) | 4490 | 4490 | 2% | ||
| Alcohol | ||||||
| Dobbie 2018 [53] | Adults (≥16 years) | 1027 | 1027 | |||
| Johnston 2003 [65] | Adults (≥18 years) | 4490 | 4490 | 2% | 10% | |
| 4. Beliefs about capabilities | ||||||
| Concerns about capability (general) | ||||||
| Alhussein 2021 [33] | Adults (≥18) | 856 | Those whose source of knowledge was media sources (largest group) (n = 331) | 84% (family/friend) | ||
| 83% (stranger) | ||||||
| Alshudukhi et al. 2018 [34] | Adults (≥18) | 310 | 168 unwilling to perform CPR | 61% | ||
| Anto-Ocra et al. 2020 [35] | Adults (≥18 years) | 277 | 277 | 61% | ||
| Babic et al. 2020 [38] | Adults (≥18 years) | 198 | 198 | 37% (MMV) | ||
| 32% (compressions) | ||||||
| Becker et al. 2019 [39] | Adults (≥18 years) who attended CPR training event | 677 | 306 resp. concerns elderly patient | 13% | ||
| 249 resp. concerns for woman | 14% | |||||
| 291 resp. concerns for child | 23% | |||||
| Chen et al. 2017 [48] | Adult laypersons (≥18 yrs) + 3 < 18 years | 1841 | 1841 | 44% | ||
| Cheng-Yu et al. 2016 [50] | Adults (≥20) | 401 | 144 (unwilling to perform on stranger) | 6% | ||
| Cho et al. 2010 [54] | Lay people aged 11 years and over | 890 | 539 (unwilling to perform CPR) | 50% | ||
| Cu 2009 [50] | Caregivers of children presenting to the Emergency Department (≥18 years) | 348 | 125 (unwilling to perform CPR on adult) | 77% | ||
| Dobbie 2018 [53] | Adults (≥16 years) | 1027 | 1027 | 19% | ||
| Huang 2016 [60] | School and University students (13–21 years) | 1407 | 546 (unwilling to perform on stranger) | 53% | ||
| Iserbyt 2016 [63] | Secondary school pupils | 313 | 313 | 31% (girls) | ||
| 23% (boys) | ||||||
| Johnston 2003 [65] | Adults (≥18 years) | 4490 | 4490 | 2% | ||
| Karuthan et al. 2019 [78] | College students | 393 | 393 | 36% (HO stranger) | ||
| 27% (HO family-member) | ||||||
| Kanstad, Nilsen & Fredriksen 2011 [77] | Secondary school students (16–19 years) | 376 | 376 | 79% | ||
| Maes et al. 2015 [91]a | Hospital visitors (≥13 years) | 85 | 51 who did not feel able to use AED | 45% (Don’t know how AED works) | ||
| Nielsen et al. 2013 [99] | Adults (≥15 years) | 1639 | n = 114 (unwilling to provide CC, 2008) | 54% | ||
| n = 94 (unwilling to provide MMV, 2008) | 44% | |||||
| n = 89 (unwilling to provide CC, 2009) | 48% | |||||
| n = 90 (unwilling to provide MMV, 2009) | 35% | |||||
| Omi 2008 [91] | High school students | 3316 | 2203 unwilling to perform CPR | 55% (of 2203 who were unwilling) | ||
| Pei-Chuan Huang et al. 2019 [107] | Adults (≥20) | 1073 | 141 (who provided reasons why not) | 12% | ||
| Platz et al. 2000 [108] | Family members of patients at risk of cardiac arrest | 100 | 100 | 35% | ||
| Rankin et al. 2020 [109] | Adults (18–21 years) | 178 | Not CPR trained, for family 65% | |||
| CPR trained, for family 68% | ||||||
| Not CPR trained, for stranger 58% | ||||||
| CPR trained, for stranger 57% | ||||||
| Shams et al. 2016 [119] | University students | 948 | 948 | 56% | ||
| Shibata 2000 [105] | Schoolchildren and teachers | 626 | NR | 80% | ||
| Sipsma, Stubbs & Plorde 2011 [121] | Adults (≥18) | 1001 | 333 | 33% | ||
| Taniguchi 2007 [111] | High school students and teachers | 3444 | 3444 | 70% | ||
| Taniguchi 2012 [112] | High school students and teachers | 1946 | 1708 students on a stranger | 67% | ||
| Winkelman et al. 2009 [134] | Teacher candidates | 582 | 47 | 38% | ||
| Concerns about physical capability | ||||||
| Case et al. 2018 [47] | OHCA Calls | 120 | 120 calls where no CPR given | 15% | ||
| Coons & Guy 2009 [56] | Adults (≥18) | 755 | 435 (who endorsed reasons) | 21.5% (stranger) | ||
| 22.5% (family) | ||||||
| Dami 2010 [51] | High school students | 3316 | 2203 unwilling to perform CPR | 55% (of 2203 who were unwilling) | ||
| Hauff 2003 [59] | Call to Dispatch Centre with OHCA | 404 | 52 who did not accept CPR instructions | 11% | ||
| Jelinek 2001 [64] | General public (age not reported) | 803 | 26 unwilling to perform CC | 11% | ||
| Lerner et al. 2008 [83] | Call to Dispatch Centre with OHCA | 168 | 145 who did not follow CPR instructions | 8% | ||
| Lu et al. 2016 [89] | College students | 609 | 609 (non-medical) | 1–3% (dep on subject) | ||
| Pei-Chuan Huang et al. 2019 [107] | Adults (≥20) | 1073 | 141 (who provided reasons why not) | 1.3% | ||
| Platz et al. 2000 [108] | Family members of patients at risk of cardiac arrest | 100 | 100 | 14% | ||
| Riou et al. 2020 [110] | Retrospective analysis of emergency calls for OHCA | 65 | 57 (where caller responded with an account) | 35% | ||
| Schneider et al. 2004 [118]a | Survivors of OHCA and people who know them | 112 | 112 | 4–5% | ||
| Sipsma, Stubbs & Plorde 2011 [121] | Adults (≥18) | 1001 | 333 | 8% | ||
| Swor 2006 [20] | Witnesses of OHCA | 684 | 279 (did not perform CPR) | 4% | ||
| Winkelman et al. 2009 [134] | Teacher candidates | 582 | 47 | 2% | ||
| Lack of confidence | ||||||
| Anto-Ocra et al. 2020 [35] | Adults (≥18 years) | 277 | 277 | 16% | ||
| Case et al. 2018 [47] | OHCA Calls | 120 | 120 calls where no CPR given | “many” | ||
| Cheskes et al. 2016 [51] | Adult (≥18 yrs) | 428 | NR | 6–12% | ||
| Dobbie 2018 [53] | Adults (≥16 years) | 1027 | 1027 | 15% | ||
| Hung 2017 [62] | College and University students (≥15 years) | 351 | 351 | 48% | ||
| Jelinek 2001 [64] | General public (age not reported) | 803 | 26 unwilling to perform CC | 4% | ||
| Lu et al. 2016 [89] | College students | 609 | 609 (non-medical) | 12–40% (dep on subject) | ||
| Magid et al. 2019 [92] | College students | 588 | 300 (who identified barriers) | 61% | ||
| Teachers | 383 | NR | 49% | |||
| Sasson et al. 2013 [114] | Teachers | 383 | NR | 49% | ||
| Nishiyama et al. 2019 [100] | University students who had witnessed OHCA | 5549 | 94 (who did not perform CPR) | 10% | ||
| So et al. 2020 [125] | High school students (12–15 years) | 128 | NR | 91% | ||
| Wilks et al. 2015 [133] | Secondary school students (15–16 years) | 383 | NR | 27% | ||
| Uncertainty whether cardiac arrest | ||||||
| Axelsson et al. 1996 [36] | People who reported making a CPR attempt between 1990 and 1994 | 742 | 51 bystanders described hesitation | NR | ||
| Breckwoldt et al. 2009 [45] | Witnesses of OHCA | 138 | 39 where agonal breathing | 39% | ||
| Case et al. 2018 [47] | OHCA Calls | 120 | 120 calls where no CPR given | 28% | ||
| Dobbie 2018 [53] | Adults (≥16 years) | 1027 | 1027 | 14% | ||
| Hauff 2003 [59] | Call to Dispatch Centre with OHCA | 404 | 52 who did not accept CPR instructions | 6% | ||
| Han 2018 [58] | Family members (≥18 years) of patients at risk of cardiac arrest | 203 | 88 | 10% | ||
| Lee et al. 2013 [82] | College students | 2029 | 242 (unwilling to perform CPR) | 34% | ||
| Magid et al. 2019 [92] | College students | 588 | 300 (who identified barriers) | 40% | ||
| Mathiesen et al. 2017 [93] | Witnesses of OHCA | 10 | 10 | NR (qualitative barrier identified) | ||
| Mausz, Snobelen & Tavares 2018 [94] | Witnesses of OHCA | 14 | 15 | NR (qualitative barrier identified) | ||
| Nishiyama et al. 2019 [100] | University students who had witnessed OHCA | 5549 | 94 (who did not perform CPR) | 12% | ||
| Nolan et al. 1999 [101] | Adults (≥45) | 786 | 203 (not ready to perform CPR) | 34% | ||
| Platz et al. 2000 [108] | Family members of patients at risk of cardiac arrest | 100 | 100 | 34% | ||
| Sasson et al. 2013 [114] | Lay-people (min age not stated) | 42 | 42 | NR (1 of 10 qualitative barriers identified) | ||
| Sasson et al. 2015 [115] | Lay-people (≥13) | 64 | 64 | NR (qualitative barrier identified) | ||
| Swor et al. 2013 [126]a | Witnesses of OHCA | 30 | 30 | 10% (seizures/agonal breathing) | ||
| Feeling unprepared | ||||||
| Mausz, Snobelen & Tavares 2018 [94] | Witnesses of OHCA | 14 | 15 | NR (qualitative barrier identified) | ||
| Moller et al. 2014 [98] | Witnesses of OHCA | 33 | 33 | NR (qualitative barrier identified) | ||
| 13. Emotion | ||||||
| Strong emotions | ||||||
| Aaberg et al. 2014 [32] | High School students | 399 | 399 responding as to their worst fear | NR (1 of 3 qualitative themes identified) | ||
| Bohn et al. 2012 [42] | Grammar school pupils (age 10 and age 13) | 280 | 144 (training group) | 25% | ||
| Case et al. 2018 [47] | OHCA calls | 120 | 120 calls where no CPR given | 20% | ||
| Dami 2010 [51] | Call to Dispatch Centre with OHCA | 738 | 73 medically appropriate who refused | 42% | ||
| Hauff 2003 [59] | Call to Dispatch Centre with OHCA | 404 | 52 who did not accept CPR instructions | 11% | ||
| Iserbyt 2016 [63] | Secondary school pupils | 313 | 313 | 19% (girls) | ||
| 13% (boys) | ||||||
| Kandakai & King 1999 [76] | College students | 214 | 214 | 61% | ||
| Lerner et al. 2008 [83] | Call to Dispatch Centre with OHCA | 168 | 145 who did not follow CPR instructions | 14% | ||
| Maes et al. 2015 [91]a | Hospital visitors (≥13 years) | 85 | 51 who did not feel able to use AED | 4% | ||
| Mausz, Snobelen & Tavares 2018 [94] | Witnesses of OHCA | 14 | 15 | NR (qualitative barrier identified) | ||
| Nishiyama et al. 2019 [100] | University students who had witnessed OHCA | 5549 | 94 (who did not perform CPR) | 14% | ||
| Platz et al. 2000 [108] | Family members of patients at risk of cardiac arrest | 100 | 100 | 13% | ||
| Riou et al. 2020 [110] | Retrospective analysis of emergency calls for OHCA | 65 | 2 | NR (being ‘shaken’ and fear expressed in 2 example quotations) | ||
| Skora & Riegel 2001 [122] | Laypersons who had provided out-of-hospital CPR to strangers | 12 | 12 participants | NR (Qualitative theme identified) Fear and anxiety | ||
| Swor 2006 [20] | Witnesses of OHCA | 684 | 279 (did not perform CPR) | 39% | ||
| Thoren 2010 [113] | Partners of people who experienced OHCA | 15 | 15 | NR (Qualitative theme identified) | ||
| Winkelman et al. 2009 [134] | Teacher candidates | 582 | 47 | 13% | ||
| Embarrassed | ||||||
| Lu et al. 2016 [89] | College students | 609 | 609 (non-medical) | 4–32% (dep on subject) | ||
| 12. Social influences | ||||||
| Reluctance to take responsibility / get involved | ||||||
| Lu et al. 2016 [89] | College students | 609 | 609 (non-medical) | 3–64% (dep on subject) | ||
| Nishiyama et al. 2019 [100] | University students who had witnessed OHCA | 5549 | 94 (who did not perform CPR) | 6% | ||
| Sasson et al. 2013 [114] | Lay-people (min age not stated) | 42 | 42 | NR (1 of 10 qualitative barriers identified) | ||
| Wait for someone else to step forward | ||||||
| Johnston 2003 [65] | Adults (≥18 years) | 4490 | 4490 | 2% | ||
| Magid et al. 2019 [92] | College students | 588 | 300 (who identified barriers) | 20% | ||
| Believe should wait for health professional | ||||||
| Huang 2016 [60] | School and University students (13–21 years) | 1407 | 546 (unwilling to perform on stranger) | 7% | ||
| Kua et al. 2018 [79] | School students (11–17 years) | 1196 | 966 | 28% | ||
| Pei-Chuan Huang et al. 2019 [107] | Adults (≥20) | 1073 | 141 (who provided reasons why not) | 3.5% | ||
| Tang et al. 2020 [127] | High school students (senior, age NR) | 397 | 397 | 33% | ||
| Perceptions about what others would do? | ||||||
| Sasson et al. 2013 [114] | Lay-people (min age not stated) | 42 | 42 | NR (1 of 10 qualitative barriers identified) | ||
| Modesty concerns | ||||||
| Becker et al. 2019 [39] | Adults (≥18 years) who attended CPR training event | 677 | 249 resp. concerns for woman | 14% | ||
| Shams et al. 2016 [119] | College students | 948 | 948 | 18% chest exposure | ||
| 10% touching opposite gender | ||||||
| Reluctance to touch a stranger | ||||||
| Babic et al. 2020 [38] | Adults (≥18 years) | 198 | 198 | 10% (MMV) | ||
| 5% (compressions) | ||||||
| Becker et al. 2019 [39] | Adults (≥18 years) who attended CPR training event | 677 | 306 resp. concerns elderly patient | 2% (or blame) | ||
| 249 resp. concerns for woman | 6% (or be accused) | |||||
| 291 resp. concerns for child | 5% (blame) | |||||
| 11. Environmental context | ||||||
| Disagreeable characteristics | ||||||
| General | ||||||
| Axelsson et al. 1996 [36] | People who reported making a CPR attempt between 1990 and 1994 | 742 | 51 bystanders described hesitation | NR | ||
| Dobbie 2018 [53] | Adults (≥16 years) | 1027 | 1027 | 19% | ||
| Hauff 2003 [59] | Call to Dispatch Centre with OHCA | 404 | 52 who did not accept CPR instructions | 2% | ||
| Lerner et al. 2008 [83] | Call to Dispatch Centre with OHCA | 168 | 145 who did not follow CPR instructions | 3% | ||
| Shams et al. 2016 [119] | University students | 948 | 948 | 30% | ||
| Blood | ||||||
| Johnston 2003 [65] | Adults (≥18 years) | 4490 | 4490 | 12% | ||
| Lester, Donnelly & Weston 1997 [84] | First year high school pupils | 233 | 233 | 23% | ||
| Lester, Donnelly & Assar 1997 [85] | General public | 241 | 241 | 5% | ||
| Cu 2009 [50] | Caregivers of children presenting to the Emergency Department (≥18 years) | 348 | 125 (unwilling to perform CPR on adult) | 10% | ||
| Kandakai & King 1999 [76] | College students | 214 | 214 | 88% | ||
| Skora & Riegel 2001 [122] | Previously performed CPR | 12 | 12 participants | NR (Qualitative theme identified) | ||
| Dirty | ||||||
| Dobbie 2018 [53] | Adults (≥16 years) | 1027 | 1027 | 5% | ||
| Johnston 2003 [65] | Adults (≥18 years) | 4490 | 4490 | 11% | ||
| Vomit | ||||||
| Johnston 2003 [65] | Adults (≥18 years) | 4490 | 4490 | 3% | ||
| Kandakai & King 1999 [76] | College students | 214 | 214 | 81% | ||
| Nolan et al. 1999 [101] | Adults (≥45) | 786 | 203 (not ready to perform CPR) | 38% | ||
| Skora & Riegel 2001 [122] | Previously performed CPR | 12 | 12 participants | NR (Qualitative theme identified) momentary hesitation | ||
| Saliva | ||||||
| Kandakai & King 1999 [76] | College students | 214 | 214 | 54% | ||
Table 4.
Psychological and behavioural factors associated with GREATER actual/intended CPR initiation (grouped by Theoretical Domains Framework V.2 [29])
| Factors related to initiation of CPR | Participants | Number (total) | Number in analysis for this factor | Unprompted identification of each factor (% of whole sample and % of unwilling subsample) |
Endorsement of each factor when prompted (% of whole sample and % of unwilling subsample) |
|---|---|---|---|---|---|
| 3. Social role and identity | |||||
| Instinct for saving others | |||||
| Huang 2016 [70] | School and University students (13–21 years) | 1407 | 807 (willing to perform on stranger) | 89% | |
| Sense of personal responsibility/duty | |||||
| Huang 2016 [70] | School and University students (13–21 years) | 1407 | 807 (willing to perform on stranger) | 64% | |
| Kua et al. 2018 [79] | School students (11–17 years) | 1196 | 966 | 34% | |
| Mathiesen 2017 [93] | Witness of OHCA | 10 | 10 | NR (Qualitative theme identified - normative obligation) | |
| Skora 2001 [122] | Previously performed CPR | 12 | 12 | NR (Qualitative themes identified – Duty & Responsibility, Guilt and Social pressure, Altruism) | |
| Wilks 2015 [133] | Secondary school students (15–16 years) | 383 | NR | NR | |
| 6. Beliefs about Consequences | |||||
| Anticipate guilt if don’t act | |||||
| Mathiesen 2017 [93] | Witness of OHCA | 10 | 10 | NR (Qualitative theme identified) | |
| Believe more likely to help than harm | |||||
| Hung 2017 [72] | College and University students (≥15 years) | 351 | 351 | 79% | |
| Kua et al. 2018 [79] | School students (11–17 years) | 1196 | 966 | 12% | |
| Pei-Chuan Huang 2019 [107] | Adults (≥20 years) | 1073 | 1073 | 85% | |
| Person will die if I don’t | |||||
| Johnston 2003 [75] | Adults (≥18 years) | 4490 | 4490 | 6% | |
| Believe CPR increases survival | |||||
| Hung 2017 [72] | College and University students (≥15 years) | 351 | 351 | 79% | |
| Wilks 2015 [133] | Secondary school students (15–16 years) | 383 | NR | NR | |
| Know risk of permanent brain damage if don’t act | |||||
| Pei-Chuan Huang 2019 [107] | Adults (≥20 years) | 1073 | 1073 | 79% | |
| Johnston 2003 [75] | Adults (≥18 years) | 4490 | 4490 | 6% | |
| Kua 2018 [79] | School students (11–17 years) | 1196 | 966 | 37% | |
| Awareness of legal protection (e.g.Good Samaritan Law) | |||||
| Pei-Chuan Huang 2019 [107] | Adults (≥20 years) | 1073 | 1073 | 85% | |
| 12. Social influences | |||||
| Make every effort even if no hope | |||||
| Huang 2016 [70] | School and University students (13–21 years) | 1407 | 807 (willing to perform on stranger) | 13% | |
| Belief that life is precious | |||||
| Hung 2017 [72] | College and University students (≥15 years) | 351 | 351 | 49% | |
| Mathiesen 2017 [93] | Witness of OHCA | 10 | 10 | NR (Qualitative theme identified) | |
Table 5.
Studies which formally assess association of variables with measures of CPR initiation/intention (grouped by Theoretical Domains Framework V.2 [29])
| Factor associated with CPR initiation | Population (Number, Country, Age Group) | Measure of CPR intention | Variable associated with CPR initiation | Odds ratio (95% CI) (unless indicated otherwise) | |
| 1. Knowledge | |||||
| Knowing importance of CPR | |||||
| Kuramoto 2008 [80] | 1132 Japan Adults (≥15 years) | Willingness to attempt CPR | 1.9 (1.3–2.8) | ||
| 11. Environmental context | |||||
| Having friends with heart diseases | |||||
| Kuramoto 2008 [80] | 1132 Japan Adults (≥15 years) | Willingness to attempt CPR | 1.8 (1.1–3.0) | ||
| Self-rated health status | |||||
| Ro et al. 2016 [111] | 62,425 Korea ≥19 years | Provision of bystander CPR (CPR self-efficacy) | Good self-rated health status | 1.3 (1.2–1.4) | |
| 2. Skills | |||||
| Previous experience of CPR | |||||
| Chew et al. 2019 [53] | 6248 Malaysian Adults (min age NR) | Willingness to perform CPR | Previous experience of administering CPR | Mean rank =2877.42, U = 1,205,596, p < 0.001 | |
| Hawkes et al. 2019 [68] | 2084 UK Adults (≥18 years) | Likelihood of performing CPR | Having witnessed OHCA previously | 1.53 (1.17–2.10) | |
| Kuramoto 2008 [80] | 1132 Japan Adults (≥15 years) | Willingness to attempt CPR | Actual experience with CPR | 3.8 (1.7–8.) | |
| Sasaki et al. 2015 [113] | 4853 Japan adults (≥15 years) | Confidence in performing CPR | Previous experience performing CPR | CC: 4.8 (1.8–12.9) | |
| MMV: 3.7 (2.1–6.6) | |||||
| AED: 2.7 (1.3–5.7) | |||||
| Schmid et al. 2016 [116] | 371 Costa Rica age unknown | Willingness to perform CPR on a stranger | Prior witness OHCA | 2.5 (1.2–5.3) | |
| 6. Beliefs about Consequences | |||||
| Believe legal consequences if person dies | |||||
| Schmid et al. 2016 [116] | 371 Costa Rica age unknown | Willingness to perform CPR on a stranger | Belief that CPR has legal consequences | 0.4 (0.2–0.6) | |
| Hesitancy about mouth to mouth | |||||
| Schmid et al. 2016 [116] | 371 Costa Rica age unknown | Willingness to perform CPR on a stranger | Hesitancy to do MMV | 0.3 (0.2–0.6) | |
| Outcome expectancies | |||||
| Meischke et al. 2002 [97] | 159 USA older adults | Intentions to use an AED | Outcome expectancies | 4.65 (2.0–10.6) | |
| Attitudes | |||||
| Vaillancourt et al. 2013 [131] | 192 Canada Adults (≥55 years) | Intention to perform CPR | Attitude | 1.6 (1.3–2.0) | |
| Magid et al. 2019 [92] | 588 USA College students | Intention to perform CPR | Attitude | Beta (95%CI): 0.164 [0.131, 0.197] | |
| 4. Beliefs about capabilities | |||||
| Feeling confident in ability to perform CPR | |||||
| Shams et al. 2016 [119] | 948, Lebanon, university students | Willingness to perform CPR | Feeling confident in abilities | 1.9 (1.3–2.9) | |
| Feel lack expertise | 0.6 (0.4–0.8) | ||||
| Meischke et al. 2002 [97] | 159 USA older adults | Intentions to use an AED | Self-perceived ability | 11.5 (3.8–34.4) | |
| Vaillancourt et al. 2013 [131] | 192 Canada Adults (≥55 years) | Intention to perform CPR | Control | 1.4 (1.2–1.5) | |
| Magid et al. 2019 [92] | 588 USA College students | Intention to perform CPR | Perceived Behavioural Control | Beta (95%CI): 0.083 [0.047, 0.119] | |
| 12. Social influences | |||||
| Vaillancourt et al. 2013 [131] | 192 Canada Adults (≥55 years) | Intention to perform CPR | Normative | 1.2 (1.1–1.4) | |
| Magid et al. 2019 [92] | 588 USA College students | Intention to perform CPR | Subjective norm | Beta (95%CI): 0.176 [0.133, 0.219] | |
| Studies Reporting differences in beliefs between participants who were willing to perform CPR and those who were unwilling | |||||
| Group | Belief (measure) | Difference between the groups | |||
| willing | unwilling | ||||
| 4. Beliefs about Capabilities | |||||
| Nolan et al. 1999 [101] | 786 Canada Adults (≥45) | 62% | 47% | Self-efficacy (confidence to perform CPR) | P < 0.001 |
| Schmitz et al. 2015 [117] | 110 (experimental group) | 11.1 | 8.6 | Self-efficacy (capacity belief) (self-efficacy score (higher score = greater efficacy) | P = 0.009 |
| 6. Beliefs about Consequences | |||||
| Parnell 2006 [106] | 494 New Zealand High School Students | 70% positive attitude | 47% negative attitude | Attitudes (% positive or negative attitude) | P < 0.001 |
| Schmitz et al. 2015 [117] | 110 (experimental group) | 22.3 | 18.8 | Attitudes (attitude score (higher score = more positive attitude) | P = 0.04 |
| 13. Emotion | |||||
| Nolan et al. 1999 [101] | 786 Canada Adults (≥45) | 2.17 | 2.42 | Anticipate negative emotions with CPR (mean number of negative emotions)) | P < 0.02 |
Table 6.
Summary of studies exploring relationship to victim (Domain 11. Environmental context and resources [29])
| Author | Country | Participants | n | Relatives (%) | Neighbour/Friend (%) | Unknown person (%) | Drug addict (%) | Unkempt (%) | Difference (%) | Other statistics |
|---|---|---|---|---|---|---|---|---|---|---|
| Alhussein 2021 [33] | Saudi Arabia | Adults (≥18) | 413 (subsample aware of CPR) | 36 | 24 /22 | 16 | 20 | P < .001 | ||
| Anto-Ocra et al. 2020 [35] | Ghana | Adults (≥18) not medical | 277 | 78 | 60 | 46 | 32 | |||
| Axelsson 2000 [37] | Sweden | Adults (≥18 years) who had received training in basic CPR in January 1997. | 1012 | 97 | 91 | 70 | 17 | 7 | 27 | |
| Bin 2013 [40] | Saudi Arabia | High school students | 575 | 67 (male respondents) | 42 (male respondents) | 25 | ||||
| 67 (female respondents) | 24 (female respondents) | 43 | ||||||||
| Birkun 2018 [41] | Crimea | Adult (≥18 yrs) | 384 | 91 | 79 | 12 | ||||
| Bray 2017 [44] | Australia | Adult (≥18 yrs) | 404 | 91 (conventional CPR, low rate area) | 88 (conventional CPR, low rate area) | 3 | ||||
| Brinkrolf 2018 [46] | Germany | Witnesses of an OHCA | 101 | 70.20 | 60 | 59.40 | 11 | |||
| Chen 2017 [48] | China | Adult laypersons (≥18 yrs) + 3 < 18 years | 1841 | 98.7 | 76.3 | 22.4 | ||||
| Cheng 1997 [49] | Taiwan | Families of cardiac patients and general public | 856 | 92.40 | 88 | 75.10 | 17.3 | |||
| Cheng-Yu 2016 [50] | Taiwan | Adults (≥20 years) | 401 | 86.80 | 36.60 | 50 | ||||
| Chew 2009 [52] | Malaysia | School teachers. | 73 | 97.30 | 94.50 | 8.20 | ||||
| Cho 2010 [54] | Korea | Lay people aged 11 years and over | 890 | 55.80 | 19 | 36 | ||||
| Coons 2009 [56] | USA | Adult (≥18 years) | 370 (urban) | 84.5 (urban) | 51.3 (urban) | 33 | ||||
| 385 (rural) | 82.5 (rural) | 55 (rural) | 28 | |||||||
| Cu 2009 [57] | Australia | Caregivers of children presenting to the Emergency Department (≥18 years) | 348 | 81 | 64 | 17 | P < 0.001 | |||
| De Smedt 2018 [59] | Belgium | Schoolchildren aged 10–18, teachers and principals | 390 | 96 | 92 | 67 (woman) | 29 | |||
| Dracup 1994 [62] | USA | Family members of patients at risk of cardiac arrest | 172 | 86 | 82 | 4 | ||||
| Fratta et al. 2020 [65] | USA | Attendees at large public gatherings (aged ≥14) | 516 | 69 | 45 | P < 0.001 | ||||
| Han 2018 [66] | Korea | Family members (≥18 years) of patients at risk of cardiac arrest | 203 | 68 (CS group) | 64 (CS) | 4 | ||||
| 76 (CV group) | 65 (CV) | 5 | ||||||||
| 67 (no risk group) | 50 (no risk) | 17 | ||||||||
| Hollenberg et al. 2019 [69] | Sweden | School students (13 years) | 641 | 85 (directly after training native) | 38 (directly after training native) | 47 | NR | |||
| 84 (Directly after training other native) | 52 (Directly after training other native) | 32 | ||||||||
| 78 (at 6 mths native) | 31 (at 6 mths native) | 47 | ||||||||
| 80 (at 6 months other native | 42 (at 6 months other native | 38 | ||||||||
| Iserbyt 2016 [73] | Belgium | Secondary school pupils | 313 | 51 (F) | 49 (F) | 11 (F) | 40 (F) | All scores increased with training | ||
| 49 (M) | 48 (M) | 8 (M) | 41 (M) | |||||||
| Jelinek 2001 [74] | Australia | General public (age not recorded) | 803 | 96 (trained < 12 months) | 54.5 (trained < 12 months) | 42 | ||||
| 94.4 (trained 1–5 y) | 51.8 (trained 1-5y) | 43 | ||||||||
| 90 (trained ≥5y) | 45.2 (trained≥5 y) | 45 | ||||||||
| Karuthan et al. 2019 [78] | Malaysia | College students | 393 | 68 | 55 | 13 | ||||
| Kuramoto 2008 [80] | Japan | Adults (≥15 years) | 1132 | 13 | 7 | 6 | ||||
| Lam 2007 [81] | Hong Kong | Laypersons who attended the CPR course (aged ≥7 years) | 305 | 87 | 61 | 26 | ||||
| Lester 1997b [85] | Wales | General public | 241 | Adult 100 (definitely or probably) | 100 | 99 | 1 | |||
| Locke 1995 [88] | USA | Lay people (minimum age not reported) & health care providers | 975 | 94 | 55 | 39 | ||||
| Mecrow 2015 [96] | Bangladesh | Lay people (≥10 years) | 721 | Data extracted for mother | Data extracted for friend of same sex | |||||
| 88 (M) | 80.8 (M) | 50 (M) | 38 (M) | |||||||
| 96.4 (F) | 75.3 (F) | 47 (F) | 49 (F) | |||||||
| Nord 2016 [102] | Sweden | Schoolchildren | 1124 | 75 (App training grp) | 32 (App training grp) | 43 (App) | ||||
| 78 (DVD training gps) | 31 (DVD training gp) | 47 (DVD) | ||||||||
| Nord 2017 [103] | Sweden | Schoolchildren | 549 | 76 (O training grp) | 31 (O training grp) | 45 (O) | ||||
| 73 (T training grp) | 31 (T training grp) | 42 (T) | ||||||||
| 78 (RT grp) | 29 (RT training grp) | 49 (RT) | ||||||||
| Omi 2008 [104] | Japan | High school students | 3316 | 41 | 15 | 26 | ||||
| Parnell 2006 [106] | New Zealand | High school students | 494 | 84 | 63 | 21 | ||||
| Pei-Chuan Huang 2019 [107] | Taiwan | Adults (≥20 years) | 1073 | 92 | 86.7 (assuming skill) | |||||
| Rankin et al. 2020 [109] | Australia | Adults (18–21 years) | 178 | 82 | 64 | 18 | ||||
| Rowe 1998 [112] | Canada | Adults (≥44 years) | 811 | 58 | 41 | 17 | ||||
| Shibata 2000 [120] | Japan | High school students and teachers | 479 | 52.8 (students) CC + MMV | 12.9 (students) CC + MMV | 40 (students MMV) | ||||
| 147 | 63.9 (teachers) CC + MMV | 25.2 (teachers) CC + MMV | 29 (teachers MMV) | |||||||
| 479 | 84.8 (students) CC only | 73.1 (students) CC only | 12 (students CC-only) | |||||||
| 147 | 89.8 (teachers) CC only | 75.5 (teachers) CC only | 14 (teachers CC-only) | |||||||
| So et al. 2020 [125] | Hong Kong | High school students (12–15 years) | 128 | 25 | 24 | 18 | 7 | |||
| Taniguchi 2007 [128] | Japan | High school students and teachers | 3444 | 41.1 (students) | 14.8 (students) | 26 (students) | ||||
| 64.5 (teachers) | 28.5 (teachers) | 36 (teachers) | ||||||||
| Taniguchi 2012 [129] | Japan | High school students and teachers | 1946 | 42 (students MMV) | 16 (students MMV) | 26 (students) |
Table 7.
Studies exploring relationship with victim (Likert Scale) ((Domain 11. Environmental context and resources [29])
| Median (IQR) | Sig. level | ||||||
|---|---|---|---|---|---|---|---|
| Study | Country | Participants | Number of participants | Willingness measured on likert scale | Friend/family | Stranger | |
| Bouland 2017 [43] | USA | Laypeople (≥14 years) | 238 | 1–10 | 9 (5–10) | 5 (3–8) | p < 0.001 |
| Mean (SD) | |||||||
| Lynch 2010 [90] | USA | Adults (40–70 years) | 822 | 1–5 | 4.06 (1.18) | 3.68 (1.23) | NR |
| Sneath 2009 [124] | USA | Adults (≥18 years) | 78 | 1–5 | 4.01 (NR) | 2.74 (NR) | NR |
Table 8.
Studies exploring mouth-to-mouth ventilation as a deterrent (Domain 6. Beliefs about consequences [29])
| Study | Country | Participants | Sample (n) | CPR inc. ventilations | At least CC-only | % of sample more likely to do CC-only CPR | Significance (if stated) |
|---|---|---|---|---|---|---|---|
| Bray 2017 [44] | Australia | Adult (≥18 yrs) | 404 | 91% (close family) | 91% (close family) | 0 (family) | |
| (results from 223 in low-bystander region) | 88% (friend) | 91% (friend) | 3 (friend) | ||||
| 67% (stranger) | 88% (stranger) | 21 (stranger) | |||||
| Cheng-Yu 2016 [50] | Taiwan | Adults (≥20 years) | 401 | 86.8% (known) | 88.1% (known) | 1.3 (known) | |
| 36.6% (stranger) | 67.8% (stranger) | 31.2 (stranger) | |||||
| Cheskes 2016 [51] | Canada | Adult (≥18 yrs) | 428 | 39.7% (stranger) | 61.5% (stranger) | 21.8 (stranger) | (61.5% v. 39.7%, p < 0.001). |
| Cho 2010 [54] | Korea | Lay people aged 11 years and over | 890 | 55.8% (family) | 55.5% (family) | 0.3 (family) | |
| 19% (adult) | 30.1% (adult) | 11.1 (adult) | |||||
| Enami 2010 [64] | Japan | Adults (≥17 years). New driver licence applicants | 8890 | 72% | 86.3% | 14.3 | |
| Hubble 2003 [71] | USA | High school students | 683 | 43% | 55% | 12 | P < 0.001 |
| Jelinek 2001 [74] | Australia | General public (age not recorded) | 803 | 90.7% (friend/relative) | 91.4% (friend/relative) | 0.7 (friend/relative) | |
| 47.2% (stranger) | 78.1% (stranger) | 30.9 (stranger) | |||||
| Lam 2007 [81] | Hong Kong | Laypersons who attended the CPR course (aged ≥7 years) | 305 | 87% (family) | 93% (family) | 6 (family) | |
| 61% (stranger) | 84% (strangers) | 23 (stranger) | |||||
| Lester 2000 [86] | UK | Participants who had attended a CPR course | 416 | 82% | 94% | 12 | |
| Locke 1995 [88] | USA | Lay people (minimum age not reported) & health care providers | 975 | 74% (friend/relative) | 88% (friend/relative) | 14 (friend/relative) | |
| 15% (stranger) | 68% (stranger) | 53 (stranger) | |||||
| Nielsen 2013 [99] | Denmark | Adults (≥15 years) | 1639 | 59% (stranger) | 63% (stranger) | 4 | |
| Nord 2016 [102] | Sweden | Schoolchildren | 1124 | 75% (known-App grp) | 93% (known-App) | 18 (known) | |
| 78% (known DVD grp) | 94% (DVD grp) | 16 (known) | |||||
| 32% (stranger –app) | 87% (stranger-app) | 55 (stranger) | |||||
| 31% (stranger DVD) | 82% (stranger DVD) | 51 (stranger) | |||||
| Nord 2017 [103] | Sweden | Schoolchildren | 397 | 73% (friend-T grp) | 92% (friend T grp) | 19 (friend T grp) | |
| 78% (friend RT grp) | 98% (friend RT grp) | 20 (friend RT grp) | |||||
| 31% (stranger- T grp) | 83% (stranger –T grp) | 52 (stranger) | |||||
| 29% (stranger- RT grp) | 87% (stranger RT grp) | 58 (stranger) | |||||
| Omi 2008 [104] | Japan | High school students | 3316 | 41% (relative) | 69% (relative) | 28 (relative) | |
| 15% (stranger) | 53% (stranger) | 38 (stranger) | |||||
| Smith 2003 [123] | Australia | Householders (age not reported) | 1489 | 60.5% (stranger) | 79.7% (stranger) | 19.2 (stranger) | |
| Shibata 2000 [120] | Japan | High school students and teachers | 626 | Students (n = 479) | Students | Students | Students |
| 12.9% (strangers) | 73.1% (strangers) | 60.2 (stranger) | p < 0.001 | ||||
| 52.8% (relatives) | 84.8% (relatives) | 32.0 (relatives) | p < 0.001 | ||||
| Teachers (n = 147) | Teachers | Teachers | Teachers | ||||
| 25.2% (strangers) | 75.5% (strangers) | 50.3 (stranger) | p < 0.001 | ||||
| 63.9% (relatives) | 89.8% (relatives) | 25.9 (relatives) | p < 0.001 | ||||
| Taniguchi 2012 [129] | Japan | High school students and teachers | 1946 | Students (n=1708) | Students | Students | |
| 42% (relative) | 72% (relative) | 30 (relative) | |||||
| 16% (stranger) | 59% (stranger) | 43 (stranger) | |||||
| Teachers (n = 238) | Teachers | Teachers | |||||
| 60% (relative) | 84% (relative) | 24 (relative) | |||||
| 28% (stranger) | 73% (stranger) | 45 (stranger) |
Table 9.
Studies exploring mouth-to-mouth ventilation as a deterrent (Likert Scale) ((Domain 6. Beliefs about consequences [29])
| Study | Country | Participants | No of participants | Willingness (likert scale) | Type of CPR (median) | Sig. level | |
|---|---|---|---|---|---|---|---|
| CC & ventilation | CC only | ||||||
| Vetter 2016 [132] | USA | High school students | 412 | 1–5 (1 most likely) | 2 (relative) | 1.6 (relative) | P < 0.02 |
Table 10.
Studies exploring disagreeable characteristics (Domain 11. Environmental context and resources [29])
| Study | Country | Participants | Sample (n) | % willing to perform CPR in presence of disagreeable characteristic | Adult stranger | Difference |
|---|---|---|---|---|---|---|
| Vomit | ||||||
| Lester, Donnelly & Assar 1997 [85] | Wales | General public | 241 | 25% | 69% | 44% |
| Smith et al. 2003 [123] | Australia | Householders (age not reported) | 1489 | 73% (CC) | 80% (CC) | 7% (CC) |
| 41.5% (MMV) | 60.5% (MMV) | 19% (MMV) | ||||
| Not Clean | ||||||
| Lester, Donnelly & Assar 1997 [85] | Wales | General public | 241 | 30% | 69% | 39% |
| Smith et al. 2003 [123] | Australia | Householders (age not reported) | 1489 | 75% (CC) | 80% (CC) | 5% (CC) |
| 52% (MMV) | 60.5 (MMV) | 8.5% (MMV) | ||||
| Smells | ||||||
| Lester, Donnelly & Assar 1997 [85] | Wales | General public | 241 | 30% | 69% | 39% |
| Bleeding | ||||||
| Lester, Donnelly & Assar 2000 [86] | UK | Participants who had attended a CPR course | n = 365 (facial blood) | 68% (CC) | 94% (CC) | 26% (CC) |
| n = 367 (adult stranger) | 40% (MMV) | 82% (MMV) | 42% (MMV) | |||
| Smith et al. 2003 [123] | Australia | Householders (age not reported) | 1489 | 55% (CC) | 80% (CC) | 25% (CC) |
| 39% (MMV) | 60.5% (MMV) | 21.5% (MMV) |
Fig. 2.
Theoretical Domains Framework definitions [29]
Studies involving those with direct experience of OHCA
Sixteen studies involving people with direct experience of OHCA were identified. These included five studies which analysed recorded calls involving OHCA [47, 58, 67, 83, 110], four qualitative studies exploring the experiences of people who had witnessed an OHCA [93, 94, 98, 130] and seven cross-sectional surveys which asked open questions about people’s experiences of facilitators and barriers to them having performed CPR [20, 36, 46, 95, 122, 126, 136].
Real-life calls
TDF domain 4: beliefs about capabilities
Limitations in the physical capacity of the caller was also identified in all five studies. Physical capability was a barrier to CPR in 15% [47], 51% [58], 11% [67], 35% [110] and 8% [83] of calls. Difficulties moving the person who had collapsed to a flat position in order to perform CPR and the rescuer being frail or with a condition making CPR difficult were described. Uncertainty about whether cardiac arrest was happening (e.g. person still making some respiratory sounds) was reported in 28% of calls by Case (2018) [47] and in 6% by Hauff (2003) [67].
Case (2018) [47] reported that “many callers” reported a lack of confidence.
TDF domain 6: beliefs about consequences
Concerns that CPR was futile (e.g. that the person was already dead/beyond help) were reported in 50% of calls analysed by Riou et al. (2020) [110], in 28% of calls analysed by Case (2018) [47] and in 23% by Hauff (2003) [67]. Concern about infection (4%) [58], fear of doing harm (3%) and fear of legal consequences (1%) [83] were reported in a small minority of calls.
TDF domain 11: environmental context
Disagreeable characteristics associated with the victim was identified as a factor in 3% [83] and 2% [67] of calls.
TDF domain 13: emotion
All five studies of real-life calls analysed calls where the layperson hesitated or refused to provide CPR identified the strong emotion of the situation as a factor that prevented initiation of CPR. Elements of emotional distress, such as panic, upset and stress were identified in 20% [47], 42% [58], 11% [67] and 14% [83] of calls where callers expressed reluctance. ‘Being shaken’ and ‘fear’ were described in 2 example quotations by Riou et al. (2020) [110].
Qualitative studies of people who have witnessed OHCA
Four qualitative accounts of people’s experiences of encountering OHCA and CPR were identified [93, 94, 98, 130] comprising interviews with a total of 107 participants (aged 24 [93] to 87 [130]).
TDF domain 2: skills
Feeling unprepared as to what to expect in a cardiac arrest was a theme identified by Mausz (2018) [94] and Moller (2014) [98], in particular that reality was very different from training with a manikin [98].
TDF domain 3: social/professional role and identity
A sense of community or social responsibility were described as encouraging performance of CPR, some stating it was expected of any responsible citizen [93].
TDF domain 4: beliefs about capabilities
Problems identifying whether cardiac arrest had actually occurred (and thus whether CPR was indicated) were identified [93, 94].
TDF domain 6: beliefs about consequences
Fear of doing the patient harm was identified as a cause for hesitation [130]. Recognising the extreme seriousness of the situation led people to erroneously assume that the person was already dead and that CPR would be futile [130]. However, anticipating feeling guilty if they didn’t perform CPR and the person died as a result was a motivation for participants [93].
Concerns about personal safety [93] and liability in the context of a workplace [94] were also expressed.
TDF domain 11: emotion
Participants also described experiencing panic and extreme emotions which inhibited their ability to perform CPR actions [94, 130].
Cross-sectional surveys
Eight cross sectional surveys included analyses of barriers and facilitators of CPR identified by participants who had direct experience of OHCA [20, 46, 93, 95, 100, 122, 126, 136]. Issues identified were very similar to those already described above in the qualitative studies:
Studies of participants where direct experience of CPR was not required
Studies examining the relationship between psychological/behavioural variables and willingness/confidence/intention to perform CPR
Thirteen studies formally explored the relationship between behavioural and psychological predictor variables and willingness to initiate CPR (see Table 5).
TDF domain 1: knowledge
Knowing the importance of CPR (OR 1.9) was positively and significantly related to willingness to perform CPR [80].
TDF domain 2: skills
Having previous experience of CPR or OHCA was the strongest predictor of anticipated willingness to perform CPR [80, 113, 116]. Odds ratios across four studies ranged from 1.5 [68] to 4.8 [113].
TDF domain 4: beliefs about capabilities
Those with good self-rated health status (AOR, 1.26) were more likely to report that they could provide bystander CPR than those reporting poor health [111] and feeling confident (OR 1.9) [119] was positively and significantly related to willingness to perform CPR [97]. Perceiving a lack of expertise was negatively related to willingness (OR 0.6) [119]. Nolan et al. (1999) [101] also showed that confidence differed significantly between those willing and unwilling to initiate CPR. Those unwilling to act also perceived a greater number of psychosocial barriers than those willing (p ≤ .05).
Vaillancourt (2013) [131] and Magid (2019) [92] explored the ability of constructs from the Theory of Planned Behaviour, to predict intention to perform CPR in the event of a cardiac arrest. Attitudes (e.g. I could save someone’s life with CPR) were with the strongest predictor of respondents’ intentions to perform CPR (OR 1.63) identified by Vaillancourt (2013) and also found to be significant in predicting intention to perform CPR. Similarly, both Vaillancourt (2013) and Magid (2019) found higher control beliefs (I feel confident in my abilities to perform CPR) to be significantly related to increased intentions to perform CPR on a cardiac arrest victim (OR 1.16) [131].
Domain 12: social influences
Normative beliefs (derived from the Theory of Planned Behaviour (TPB)) (e.g. My friends and family expect me to do CPR) were found to be modestly but significantly related to people’s intentions to perform CPR on a cardiac arrest victim (OR: 1.07) [131]. Magid (2019) [92] also found subjective norms predictive of intention to perform CPR.
TDF domain 13: emotion
Nolan et al. (1990) [101] showed that confidence differed significantly between those willing and unwilling to initiate CPR. Those unwilling to act anticipated a higher number of negative emotions (afraid, sad, angry, anxious, confused) if they were to perform CPR compared to those who were willing to act (p ≤ .02).
Studies which have compared responses to scenarios -varying psychological/behavioural factors
Sixty-two studies explored a variety of other factors related to willingness to perform CPR (see Tables 6, 7, 8, 9 and 10). Respondents were more willing to perform CPR on their family and friends compared to strangers and in situations that did not involve disagreeable characteristics (TDF Domain 11: Environmental context and resources).
Respondents were more willing to perform compression-only CPR compared to mouth-to-mouth CPR and in situations where there was a perceived risk of transmissible infection willingness to perform CPR was reduced, e.g. after a SARS outbreak (TDF Domain 6: Beliefs about consequences).
Studies of people’s anticipated barriers and facilitators to CPR
Qualitative studies
Four studies provided qualitative accounts of people’s perceptions of CPR [61, 114, 115, 135]. Many of the barriers anticipated by participants in these studies were similar to those identified by people with direct experience of OHCA, as reported above. Additionally, issues around a general fear of ‘getting involved’ with possible consequences in relation to immigration status/law enforcement [115] were identified (TDF Domain 6: Beliefs about Consequences).
Cross-sectional data
Twelve studies [32, 39, 51, 60, 71, 73–75, 84, 85, 91, 104] explored the reasons people indicated a reluctance or unwillingness to perform CPR using open questions (rather than presenting possible reasons).
Unprompted reasons provided by those categorised as ‘unwilling’
-
TDF domain 4: beliefs about capability Concerns around capability were reported by 11% of unwilling high school students [104], and by 45% of those not willing to use an AED [91]. Concerns about physical capability in particular were reported by 11% of unwilling general public [74]. Low confidence was also reported (4%) [74] and 6–12% [51].
TDF domain 6: beliefs about consequences The reasons most commonly volunteered by those categorised as unwilling were concerns about to the risk to self: 56% of unwilling general public [74] with 24% [51], 35% [71] and 19% [74] concerned about the risk of infection in particular. Concerns about doing harm to the casualty were reported by 25% [71] and 23% [104]. Legal concerns were reported by 13% [71] and 19% [74] of people unwilling to provide CC and by 16% [71] and 4% [74] of those unwilling to provide mouth-to-mouth ventilation. CPR violating beliefs about death were also reported (4%) [71].
TDF domain 13: emotion Being too stressed (4%) [91] was also reported as a reason for unwillingness.
Prompted reasons
The reasons for not performing CPR most commonly proposed by researchers were: fear of doing harm (27 studies); concerns about infection (29 studies); legal concerns (24 studies); concerns about capability (26 studies) and concerns about mouth-to-mouth ventilation (10 studies). Averaging across the studies, the reasons endorsed by the largest proportion of unwilling participants were Lack of confidence (TDF Domain 4: Beliefs about capabilities), Fear of doing it wrong (TDF Domain 6: Beliefs about consequences) and Concerns about capability (TDF Domain 4: Beliefs about capabilities).
Discussion
We have conducted a comprehensive, high-quality, pre-registered systematic review of the psychological and behavioural factors relating to initiation of CPR. This provides a useful synthesis of the evidence to date and identifies promising avenues for intervention and further research. The prominence of two themes: the overwhelming emotion of the OHCA situation and concerns about physical capability in the more methodologically strong studies [58, 83] and evident across the various designs suggests these may be particularly important to address in order to increase CPR initiation.
Emotion of the situation
All five studies [47, 58, 67, 83] that analysed call-recordings involving actual CPR attempts identified the emotion of the situation as an important factor delaying initiation of CPR, as did studies of people who had witnessed OHCA [20, 94, 130].
In hypothetical studies, the expectation of high emotion was significantly associated with not being prepared to act [101] and identified as a likely barrier to CPR by high school students [32]. However, interestingly the potential impact of strong emotions was not frequently anticipated by those without experience of CPR (even when prompted) suggesting people may under-estimate the impact of emotion on their behaviour. Helping people to prepare for the unanticipated impact of strong emotions and providing strategies to perform CPR despite their emotional response might be helpful.
Concerns about capability
Concerns about physical capability were identified as a barrier to initiation in all five studies that analysed emergency call recordings [47, 58, 67, 83], identified in a survey of people who had witnesses an OHCA [20] and provided unprompted as an issue by 11% of the general public [74]. Further, those with good self-rated health were more likely to report being able to perform CPR than those with poor health [111]. Evidence also identified that feeling confident about one’s capability [119] and self-perceived capability [97, 117] are associated with increased willingness to perform CPR and conversely that a lack of confidence reduces willingness [101]. Concerns about capability were identified unprompted by 11% of students [104] and endorsed when prompted by up to 80% of participants. This triangulation of evidence from very different sources suggests concerns about capability as a key issue. Concerns may reflect actual physical limitations amongst potential rescuers but are also likely to reflect people’s beliefs about their capabilities; both are amenable to intervention but importantly will require very different approaches.
Predictors of CPR that have been formally tested
Studies which statistically tested the relationship between variables of interest and intention to perform CPR or actual behaviour were few, highlighting a need for more definitive studies to confirm posited relationships. Previous experience in performing [80, 113] or witnessing CPR [116] and self-perceived ability [97] were the variables most strongly associated with willingness suggesting interventions that improve perceptions of capability may be helpful.
Six studies found evidence to support predictors derived from behavioural theory such as the Theory of Planned Behaviour [137], highlighting the potential utility of an approach to intervention that is based on behavioural theory. Positive attitudes about CPR [92, 106, 131], perceived behavioural control [92, 131] and normative beliefs [92, 131] were significantly associated with intention to perform CPR and Magid (2019) [92] found the theory accounted for 51% of the variance in intention to perform CPR overall. These belief-based constructs are amenable to change and thus are promising targets for intervention. Resources such as the Behaviour Change Technique Taxonomy [138] and the Theory and Techniques resource (https://theoryandtechniquetool.humanbehaviourchange.org/) are available to help researchers and practitioners identify techniques to include in interventions based on their likely mode of action and their likely effectiveness to change the behaviour of interest (in this case initiation of CPR) in the required situation of OHCA.
Overall, it was notable how few papers explicitly discussed underlying theory and how multiple terms were used to refer to highly similar constructs (e.g. intention, willingness, readiness, prepared to act, capable in an emergency). Construct proliferation [139] and lack of precision in defining and labelling of constructs limits our collective ability to synthesise available evidence and to build a cumulative science [140]. This may lead to wasteful duplication of effort and hinder our ability to identify factors that increase initiation of CPR and, importantly, the factors that make initiation of CPR less likely. Greater attention to robust study design, explicit use of theory or at least consistent definitions of terms might bring us more quickly to our collective goal of increasing CPR initiation.
Limitations
This review is limited as we have only assessed published materials. There is thus the potential that publication bias has resulted in studies with negative findings being less likely to be identified [141]. We identified a preponderance of cross-sectional surveys using unvalidated measures with relatively little formal testing of posited ‘predictors’ meaning that it is difficult to draw robust and reliable conclusions from the literature.
Conclusion
Many psychological and behavioural factors associated with CPR initiation can be identified from the current literature with varying degrees of supporting evidence. Preparing people to manage strong emotions and increasing their perceptions of capability are likely important foci for interventions aiming to increase CPR initiation.
Greater use of theory and more robust study designs would strengthen knowledge in this area.
PROSPERO registration number: CRD42018117438.
Supplementary Information
Acknowledgements
We would like to acknowledge the following: Anna Temp who helped with registering the review, conducting the initial searches, and obtaining manuscripts. Sheena Moffat, Librarian at Edinburgh Napier University who provided invaluable advice on database searching. The Chief Scientist Office, Scottish Government who provided funding for the review (CGA/18/11).
An earlier draft of this review was presented at Euroheartcare conference 2021. Abstract published in European Journal of Cardiovascular Nursing [142].
Abbreviations
- CPR
Cardio-pulmonary resuscitation
- OHCA
Out of hospital cardiac arrest
- EPHPP
Effective public health practice project
- QARI
Qualitative assessment and review instrument
- PRISMA
Preferred reporting items for systematic review and meta-analysis
- TPB
Theory of planned behaviour
- TDF
Theoretical domains framework
Authors’ contributions
Barbara Farquharson (BF) created the original concept, methodology, obtained funding for the review, conducted searches, performed screening and data extraction, supervised others on the project and wrote the original draft manuscript. Diane Dixon (DD) created the original concept, methodology, obtained funding for the review, conducted searches, performed screening and data extraction, supervised others on the project and contributed to the final manuscript. Brian Williams (BW) created the original concept, methodology, obtained funding for the review and contributed to the final manuscript. Claire Torrens (CT) performed screening and data extraction and contributed to the final manuscript. Melanie Philpott (MP) contributed to the final manuscript. Henriette Laidlaw (HL) helped plan data extraction and contributed to the final manuscript. Siobhan McDermott (SM) performed data extraction and contributed to the final manuscript. The author(s) read and approved the final manuscript.
Funding
The Chief Scientist Office (Scotland) funded the study (CGA/18/11) but had no role in study design, in the collection, analysis and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable (Systematic Review).
Consent for publication
Not applicable (Systematic Review).
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Barbara Farquharson, Email: bf19@stir.ac.uk.
Diane Dixon, Email: diane.dixon@abdn.ac.uk.
Brian Williams, Email: brian.williams@uhi.ac.uk.
Claire Torrens, Email: c.e.torrens@stir.ac.uk.
Melanie Philpott, Email: mep00047@students.stir.ac.uk.
Henriette Laidlaw, Email: henriettelaidlaw@gmail.com.
Siobhan McDermott, Email: siobhanmmcdermott@gmail.com.
References
- 1.Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–1487. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Ong MEH, Do Shin S, De Souza NNA, Tanaka H, Nishiuchi T, Song KJ, et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: the Pan Asian Resuscitation Outcomes Study (PAROS) Resuscitation. 2015;96:100–108. doi: 10.1016/j.resuscitation.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 3.Lindner TW, Soreide E, Nilsen OB, Torunn MW, Lossius HM. Good outcome in every fourth resuscitation attempt is achievable--an Utstein template report from the Stavanger region. Resuscitation. 2011;82(12):1508–1513. doi: 10.1016/j.resuscitation.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 4.Perkins GD, Lockey AS, de Belder MA, Moore F, Weissberg P, Gray H. National initiatives to improve outcomes from out-of-hospital cardiac arrest in England. London: BMJ Publishing Group Ltd and the British Association for Accident & Emergency Medicine; 2015. [DOI] [PMC free article] [PubMed]
- 5.Gräsner J-T, Wnent J, Herlitz J, Perkins GD, Lefering R, Tjelmeland I, et al. Survival after out-of-hospital cardiac arrest in Europe-results of the EuReCa TWO study. Resuscitation. 2020;148:218–226. doi: 10.1016/j.resuscitation.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 6.Graham R, McCoy MA, Schultz AM. Strategies to improve cardiac arrest survival: a time to act. Washington: National Academies Press; 2015. [PubMed]
- 7.Beck B, Bray J, Cameron P, Smith K, Walker T, Grantham H, et al. Regional variation in the characteristics, incidence and outcomes of out-of-hospital cardiac arrest in Australia and New Zealand: results from the Aus-ROC Epistry. Resuscitation. 2018;126:49–57. doi: 10.1016/j.resuscitation.2018.02.029. [DOI] [PubMed] [Google Scholar]
- 8.Scottish Government. Out-of-hospital cardiac arrest: A strategy for Scotland. Edinburgh: Scottish Government; 2015.
- 9.British Heart Foundation . Consensus paper on out-of-hospital cardiac arrest in England. 2014. [Google Scholar]
- 10.Welsh Government . In: Out of hospital cardiac arrest plan in. Wales N, editor. 2017. [Google Scholar]
- 11.Hasselqvist-Ax I, Riva G, Herlitz J, Rosenqvist M, Hollenberg J, Nordberg P, et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372(24):2307–2315. doi: 10.1056/NEJMoa1405796. [DOI] [PubMed] [Google Scholar]
- 12.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63-81. [DOI] [PubMed]
- 13.Gräsner J-T, Lefering R, Koster RW, Masterson S, Böttiger BW, Herlitz J, et al. EuReCa ONE-27 nations, ONE Europe, ONE registry: A prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–195. doi: 10.1016/j.resuscitation.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 14.McNally B, Robb R, Mehta M, Vellano K, Valderrama AL, Yoon PW, et al. Out-of-hospital cardiac arrest surveillance—cardiac arrest registry to enhance survival (CARES), United States, October 1, 2005–December 31, 2010. Morb Mortal Wkly Rep Surveill Summ. 2011;60(8):1–19. [PubMed] [Google Scholar]
- 15.Barnard EBG, Sandbach DD, Nicholls TL, Wilson AW, Ercole A. Prehospital determinants of successful resuscitation after traumatic and non-traumatic out-of-hospital cardiac arrest. Emerg Med J. 2019;36(6):333–339. doi: 10.1136/emermed-2018-208165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Association AH. Our impact https://www.heart.org/en/impact-map2021 [cited 2021 26/02/21]. Available from: https://www.heart.org/en/impact-map.
- 17.Foundation BH. Government confirms plans to teach CPR in schools 2020 [Available from: https://www.bhf.org.uk/what-we-do/news-from-the-bhf/news-archive/2019/january/government-confirms-plans-to-teach-cpr-in-schools]. Accessed 30 Nov 2022.
- 18.Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF, et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. Jama. 2013;310(13):1377–1384. doi: 10.1001/jama.2013.278483. [DOI] [PubMed] [Google Scholar]
- 19.Government S . OHCA data linkage statistics. 2019. [Google Scholar]
- 20.Swor R, Khan I, Domeier R, Honeycutt L, Chu K, Compton S. CPR training and CPR performance: do CPR-trained bystanders perform CPR? Acad Emerg Med. 2006;13(6):596–601. doi: 10.1197/j.aem.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 21.Soar J, Maconochie I, Wyckoff MH, Olasveengen TM, Singletary EM, Greif R, et al. 2019 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task forces. Circulation. 2019;140(24):e826–ee80. doi: 10.1161/CIR.0000000000000734. [DOI] [PubMed] [Google Scholar]
- 22.Plant N, Taylor K. How best to teach CPR to schoolchildren: a systematic review. Resuscitation. 2013;84(4):415–421. doi: 10.1016/j.resuscitation.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 23.Yeung J, Meeks R, Edelson D, Gao F, Soar J, Perkins GD. The use of CPR feedback/prompt devices during training and CPR performance: A systematic review. Resuscitation. 2009;80(7):743–751. doi: 10.1016/j.resuscitation.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 24.Greif R, Bhanji F, Bigham BL, Bray J, Breckwoldt J, Cheng A, et al. Education, implementation, and teams: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2020;142(16_suppl_1):S222–SS83. doi: 10.1161/CIR.0000000000000896. [DOI] [PubMed] [Google Scholar]
- 25.Fishbein M, Ajzen I. Predicting and changing behavior: the reasoned action approach. New York: Taylor & Francis; 2011.
- 26.EPHPP. Effective Public Health Practice Project. (1998). Quality Assessment Tool For Quantitative Studies. http://www.ephpp.ca/tools.html. 2009 7/2015. Available from: http://www.ephpp.ca/tools.html. Accessed 30 Nov 2022.
- 27.Briggs J. Checklist for qualitative research. Adelaide: JoannBriggs Institute; 2017. [Available from: https://jbi.global/sites/default/files/2020-08/Checklist_for_Qualitative_Research.pdf].
- 28.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8(1):18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(1):1–18. doi: 10.1186/s13012-017-0605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Holleman GA, Hooge IT, Kemner C, Hessels RS. The ‘real-world approach’and its problems: A critique of the term ecological validity. Front Psychol. 2020;11:721. doi: 10.3389/fpsyg.2020.00721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513. doi: 10.1037/0003-066X.32.7.513. [DOI] [Google Scholar]
- 32.Aaberg AM, Larsen CE, Rasmussen BS, Hansen CM, Larsen JM. Basic life support knowledge, self-reported skills and fears in Danish high school students and effect of a single 45-min training session run by junior doctors; a prospective cohort study. Scand J Trauma Resusc Emerg Med. 2014;22:24. doi: 10.1186/1757-7241-22-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alhussein RM, Albarrak MM, Alrabiah AA, Aljerian NA, Bin Salleeh HM, Hersi AS, et al. Knowledge of non-healthcare individuals towards cardiopulmonary resuscitation: a cross-sectional study in Riyadh City, Saudi Arabia. Int J Emerg Med. 2021;14(1):1–9. doi: 10.1186/s12245-021-00335-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alshudukhi A, Alqahtani A, Alhumaid A, Alfakhri A, Aljerian NJIJCRLS. Knowledge, attitudes, and behavior of the general saudi population regarding cardiopulmonary resuscitation: a survey. Int J Curr Res Life Sci. 2018;7(04):1699–704.
- 35.Anto-Ocrah M, Maxwell N, Cushman J, Acheampong E, Kodam R-S, Homan C, et al. Public knowledge and attitudes towards bystander cardiopulmonary resuscitation (CPR) in Ghana, West Africa. Int J Emerg Med. 2020;13(1):1–12. doi: 10.1186/s12245-020-00286-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Axelsson A, Herlitz J, Ekström L, Holmberg S. Bystander-initiated cardiopulmonary resuscitation out-of-hospital. A first description of the bystanders and their experiences. Resuscitation. 1996;33(1):3–11. doi: 10.1016/S0300-9572(96)00993-8. [DOI] [PubMed] [Google Scholar]
- 37.Axelsson A, Thoren A, Holmberg S, Herlitz J. Attitudes of trained Swedish lay rescuers toward CPR performance in an emergency: a survey of 1012 recently trained CPR rescuers. Resuscitation. 2000;44:27-36. [DOI] [PubMed]
- 38.Babić SB, Gregor; Peršolja, Melita. Laypersons’ awareness of cardiac arrest resuscitation procedures: cross-sectional study. Ošetrovateľstvo:Tteória, Výskum, Vzdelávanie. 2020; 10(2):[55–62]. Available from: https://www.osetrovatelstvo.eu/archiv/2020-rocnik-10/cislo-2/laypersons-awareness-of-cardiac-arrest-resuscitation-procedures-cross-sectional-study.
- 39.Becker TK, Gul SS, Cohen SA, Maciel CB, Baron-Lee J, Murphy TW, et al. Public perception towards bystander cardiopulmonary resuscitation. Emerg Med J. 2019;36(11):660–665. doi: 10.1136/emermed-2018-208234. [DOI] [PubMed] [Google Scholar]
- 40.Bin H, M AL, H AL, Alanazi A, Al o, Saleh. Community awareness about cardiopulmonary resuscitation among secondary school students in Riyadh. World J Med Sci 2013;8(3):186–189.
- 41.Birkun A, Kosova Y. Social attitude and willingness to attend cardiopulmonary resuscitation training and perform resuscitation in the Crimea. World J Emerg Med. 2018;9(4):237–248. doi: 10.5847/wjem.j.1920-8642.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bohn A, Van Aken HK, Mollhoff T, Wienzek H, Kimmeyer P, Wild E, et al. Teaching resuscitation in schools: annual tuition by trained teachers is effective starting at age 10. A four-year prospective cohort study. Resuscitation. 2012;83(5):619–625. doi: 10.1016/j.resuscitation.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 43.Bouland AJ, Halliday MH, Comer AC, Levy MJ, Seaman KG, Lawner BJ. Evaluating barriers to bystander CPR among laypersons before and after compression-only CPR training. Prehosp Emerg Care. 2017;21(5):662–669. doi: 10.1080/10903127.2017.1308605. [DOI] [PubMed] [Google Scholar]
- 44.Bray JE, Straney L, Smith K, Cartledge S, Case R, Bernard S, et al. Regions with low rates of bystander cardiopulmonary resuscitation (CPR) have Lower rates of CPR training in Victoria, Australia. J Am Heart Assoc. 2017;6(6):05. doi: 10.1161/JAHA.117.005972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Breckwoldt J, Schloesser S, Arntz HR. Perceptions of collapse and assessment of cardiac arrest by bystanders of out-of-hospital cardiac arrest (OOHCA) Resuscitation. 2009;80(10):1108–1113. doi: 10.1016/j.resuscitation.2009.06.028. [DOI] [PubMed] [Google Scholar]
- 46.Brinkrolf P, Metelmann B, Scharte C, Zarbock A, Hahnenkamp K, Bohn A. Bystander-witnessed cardiac arrest is associated with reported agonal breathing and leads to less frequent bystander CPR. Resuscitation. 2018;127:114–118. doi: 10.1016/j.resuscitation.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 47.Case R, Cartledge S, Siedenburg J, Smith K, Straney L, Barger B, et al. Identifying barriers to the provision of bystander cardiopulmonary resuscitation (CPR) in high-risk regions: A qualitative review of emergency calls. Resuscitation. 2018;129:43–47. doi: 10.1016/j.resuscitation.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 48.Chen M, Wang Y, Li X, Hou L, Wang Y, Liu J, et al. Public knowledge and attitudes towards bystander cardiopulmonary resuscitation in China. Biomed Res Int. 2017;2017:3250485. doi: 10.1155/2017/3250485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cheng YC, Hu SC, Yen D, Kao WF, Lee CH. Targeted mass CPR training for families of cardiac patients - experience in Taipei city. Tzu Chi Med J. 1997;9(4):273–278. [Google Scholar]
- 50.Cheng-Yu C, Yi-Ming W, Shou-Chien H, Chan-Wei K, Chung-Hsien C. Effect of population-based training programs on bystander willingness to perform cardiopulmonary resuscitation. Signa Vitae. 2016;12(1):63–69. [Google Scholar]
- 51.Cheskes L, Morrison LJ, Beaton D, Parsons J, Dainty KN. Are Canadians more willing to provide chest-compression-only cardiopulmonary resuscitation (CPR)?—a nation-wide public survey. CJEM: Canadian. J Emerg Med. 2016;18(4):253–263. doi: 10.1017/cem.2015.113. [DOI] [PubMed] [Google Scholar]
- 52.Chew KS, Yazid MN, Kamarul BA, Rashidi A. Translating knowledge to attitude: a survey on the perception of bystander cardiopulmonary resuscitation among dental students in Universiti Sains Malaysia and school teachers in Kota Bharu. Kelantan Med J Malaysia. 2009;64(3):205–209. [PubMed] [Google Scholar]
- 53.Chew KS, Ahmad Razali S, Wong SSL, Azizul A, Ismail NF, Robert SJKCA, et al. The influence of past experiences on future willingness to perform bystander cardiopulmonary resuscitation. Int J Emerg Med. 2019;12(1):1–7. doi: 10.1186/s12245-019-0256-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cho GC, Sohn YD, Kang KH, Lee WW, Lim KS, Kim W, et al. The effect of basic life support education on laypersons' willingness in performing bystander hands only cardiopulmonary resuscitation. Resuscitation. 2010;81(6):691–694. doi: 10.1016/j.resuscitation.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 55.Compton S, Swor RA, Dunne R, Welch RD, Zalenski RJ. Urban public school teachers' attitudes and perceptions of the effectiveness of CPR and automated external defibrillators. Am J Health Educ. 2003;34(4):186–192. doi: 10.1080/19325037.2003.10761861. [DOI] [Google Scholar]
- 56.Coons SJ, Guy MC. Performing bystander CPR for sudden cardiac arrest: behavioral intentions among the general adult population in Arizona. Resuscitation. 2009;80:334-40. [DOI] [PubMed]
- 57.Cu J, Phan P, O'Leary FM. Knowledge and attitude towards paediatric cardiopulmonary resuscitation among the carers of patients attending the Emergency Department of the Children’s Hospital at Westmead. Emerg Med Australas. 2009;21(5):401–406. doi: 10.1111/j.1742-6723.2009.01217.x. [DOI] [PubMed] [Google Scholar]
- 58.Dami F, Carron PN, Praz L, Fuchs V, Yersin B. Why bystanders decline telephone cardiac resuscitation advice. Acad Emerg Med. 2010;17(9):1012–1015. doi: 10.1111/j.1553-2712.2010.00851.x. [DOI] [PubMed] [Google Scholar]
- 59.De Smedt L, Depuydt C, Vekeman E, De Paepe P, Monsieurs KG, Valcke M, et al. Awareness and willingness to perform CPR: a survey amongst Flemish schoolchildren, teachers and principals. Acta Clin Belgica: Int J Clin Lab Med. 2018;74(5):1–20. [DOI] [PubMed]
- 60.Dobbie F, MacKintosh AM, Clegg G, Stirzaker R, Bauld L. Attitudes towards bystander cardiopulmonary resuscitation: results from a cross-sectional general population survey. PLoS One. 2018;13(3):e0193391. doi: 10.1371/journal.pone.0193391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Donohoe RT, Haefeli K, Moore F. Public perceptions and experiences of myocardial infarction, cardiac arrest and CPR in London. Resuscitation. 2006;71(1):70–79. doi: 10.1016/j.resuscitation.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 62.Dracup K, Moser DK, Guzy PM, Taylor SE, Marsden C. Is cardiopulmonary resuscitation training deleterious for family members of cardiac patients? Am J Public Health. 1994;84(1):116–118. doi: 10.2105/AJPH.84.1.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dwyer T. Psychological factors inhibit family members' confidence to initiate CPR. Prehosp Emerg Care. 2008;12(2):157–161. doi: 10.1080/10903120801907216. [DOI] [PubMed] [Google Scholar]
- 64.Enami M, Takei Y, Goto Y, Ohta K, Inaba H. The effects of the new CPR guideline on attitude toward basic life support in Japan. Resuscitation. 2010;81(5):562–567. doi: 10.1016/j.resuscitation.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 65.Fratta KA, Bouland AJ, Vesselinov R, Levy MJ, Seaman KG, Lawner BJ, et al. Evaluating barriers to community CPR education. Am J Emerg Med. 2020;38(3):603–609. doi: 10.1016/j.ajem.2019.10.019. [DOI] [PubMed] [Google Scholar]
- 66.Han KS, Lee JS, Kim SJ, Lee SW. Targeted cardiopulmonary resuscitation training focused on the family members of high-risk patients at a regional medical center: A comparison between family members of high-risk and no-risk patients. Turk J Trauma Emerg Surg. 2018;24(3):224–233. doi: 10.5505/tjtes.2017.01493. [DOI] [PubMed] [Google Scholar]
- 67.Hauff SR, Rea TD, Culley LL, Kerry F, Becker L, Eisenberg MS. Factors impeding dispatcher-assisted telephone cardiopulmonary resuscitation. Ann Emerg Med. 2003;42(6):731–737. doi: 10.1016/S0196-0644(03)00423-2. [DOI] [PubMed] [Google Scholar]
- 68.Hawkes CA, Brown TP, Booth S, Fothergill RT, Siriwardena N, Zakaria S, et al. Attitudes to cardiopulmonary resuscitation and defibrillator use: a survey of UK adults in 2017. J Am Heart Assoc. 2019;8(7):e008267. doi: 10.1161/JAHA.117.008267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hollenberg J, Claesson A, Ringh M, Nordberg P, Hasselqvist-Ax I, Nord A. Effects of native language on CPR skills and willingness to intervene in out-of-hospital cardiac arrest after film-based basic life support training: a subgroup analysis of a randomised trial. BMJ Open. 2019;9(5):e025531. doi: 10.1136/bmjopen-2018-025531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Huang Q, Hu C, Mao J. Are Chinese students willing to learn and perform bystander cardiopulmonary resuscitation? J Emerg Med. 2016;51(6):712–720. doi: 10.1016/j.jemermed.2016.02.033. [DOI] [PubMed] [Google Scholar]
- 71.Hubble MW, Bachman M, Price R, Martin N, Huie D. Willingness of high school students to perform cardiopulmonary resuscitation and automated external defibrillation. Prehosp Emerg Care. 2003;7(2):219–224. doi: 10.1080/10903120390936815. [DOI] [PubMed] [Google Scholar]
- 72.Hung MSY, Chow MCM, Chu TTW, Wong PP, Nam WY, Chan VLK, et al. College students’ knowledge and attitudes toward bystander cardiopulmonary resuscitation: A cross-sectional survey. Cogent Medicine. 2017;4(1):1334408. doi: 10.1080/2331205X.2017.1334408. [DOI] [Google Scholar]
- 73.Iserbyt P. The effect of Basic Life Support (BLS) education on secondary school students’ willingness to and reasons not to perform BLS in real life. Acta Cardiol. 2016;71(5):519–526. doi: 10.1080/AC.71.5.3167494. [DOI] [PubMed] [Google Scholar]
- 74.Jelinek GA, Gennat H, Celenza T, O'Brien D, Jacobs I, Lynch D. Community attitudes towards performing cardiopulmonary resuscitation in Western Australia. Resuscitation. 2001;51(3):239–246. doi: 10.1016/S0300-9572(01)00411-7. [DOI] [PubMed] [Google Scholar]
- 75.Johnston TC, Clark MJ, Dingle GA, FitzGerald G. Factors influencing Queenslanders’ willingness to perform bystander cardiopulmonary resuscitation. Resuscitation. 2003;56:67-75. [DOI] [PubMed]
- 76.Kandakai TL, King KA. Perceived self-efficacy in performing lifesaving skills: an assessment of the American red Cross's responding to emergencies course. J Health Educ. 1999;30(4):235–241. doi: 10.1080/10556699.1999.10604645. [DOI] [Google Scholar]
- 77.Kanstad BK, Nilsen SA, Fredriksen K. CPR knowledge and attitude to performing bystander CPR among secondary school students in Norway. Resuscitation. 2011;82:1053-9. [DOI] [PubMed]
- 78.Karuthan SR, binti Firdaus PJF, Angampun AD-AG, Chai XJ, Sagan CD, Ramachandran M, et al. Knowledge of and willingness to perform hands-only cardiopulmonary resuscitation among college students in Malaysia. Medicine (Baltimore). 2019;98(51):e18466. [DOI] [PMC free article] [PubMed]
- 79.Kua PHJ, White AE, Ng WY, Fook-Chong S, Ng EKX, Ng YY, et al. Knowledge and attitudes of Singapore schoolchildren learning cardiopulmonary resuscitation and automated external defibrillator skills. Singapore Med J. 2018;59(9):487–499. doi: 10.11622/smedj.2018021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kuramoto N, Morimoto T, Kubota Y, Maeda Y, Seki S, Takada K, et al. Public perception of and willingness to perform bystander CPR in Japan. Resuscitation. 2008;79(3):475–481. doi: 10.1016/j.resuscitation.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 81.Lam K-K, Lau F-L, Chan W-K, Wong W-N. Effect of severe acute respiratory syndrome on bystander willingness to perform cardiopulmonary resuscitation (CPR)–is compression–only preferred to standard CPR? Prehosp Disaster Med. 2007;22(4):325–329. doi: 10.1017/S1049023X00004957. [DOI] [PubMed] [Google Scholar]
- 82.Lee MJ, Hwang SO, Cha KC, Cho GC, Yang HJ, Rho TH. Influence of nationwide policy on citizens' awareness and willingness to perform bystander cardiopulmonary resuscitation. Resuscitation. 2013;84(7):889–894. doi: 10.1016/j.resuscitation.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 83.Lerner EB, Sayre MR, Brice JH, White LJ, Santin AJ, Billittier AJ, et al. Cardiac arrest patients rarely receive chest compressions before ambulance arrival despite the availability of pre-arrival CPR instructions. Resuscitation. 2008;77(1):51–56. doi: 10.1016/j.resuscitation.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 84.Lester C, Donnelly P, Weston C. Is peer tutoring beneficial in the context of school resuscitation training? Health Educ Res. 1997;12(3):347–354. doi: 10.1093/her/12.3.347. [DOI] [PubMed] [Google Scholar]
- 85.Lester C, Donnelly P, Assar D. Community life support training: does it attract the right people? Public Health. 1997;111(5):293–296. doi: 10.1038/sj.ph.1900389. [DOI] [PubMed] [Google Scholar]
- 86.Lester C, Donnelly P, Assar D. Lay CPR trainees: retraining, confidence and willingness to attempt resuscitation 4 years after training. Resuscitation. 2000;45(2):77–82. doi: 10.1016/S0300-9572(00)00170-2. [DOI] [PubMed] [Google Scholar]
- 87.Liaw SY, Chew KS, Zulkarnain A, Wong SSL, Singmamae N, Kaushal DN, et al. Improving perception and confidence towards bystander cardiopulmonary resuscitation and public access automated external defibrillator program: how does training program help? Int J Emerg Med. 2020;13(1):1–7. doi: 10.1186/s12245-020-00271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Locke CJ, Berg RA, Sanders AB, Davis MF, Milander MM, Kern KB, et al. Bystander cardiopulmonary resuscitation. Concerns about mouth-to-mouth contact. Arch Intern Med. 1995;155(9):938–943. doi: 10.1001/archinte.1995.00430090077009. [DOI] [PubMed] [Google Scholar]
- 89.Lu C, Jin Y-h, Shi X-t, Ma W-j, Wang Y-y, Wang W, et al. Factors influencing Chinese university students’ willingness to performing bystander cardiopulmonary resuscitation. Int Emerg Nurs. 2017;32:3–8. doi: 10.1016/j.ienj.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 90.Lynch B, Einspruch EL. With or without an instructor, brief exposure to CPR training produces significant attitude change. Resuscitation. 2010;81(5):568–575. doi: 10.1016/j.resuscitation.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 91.Maes F, Marchandise S, Boileau L, Polain L, de Waroux JB, Scavee C. Evaluation of a new semiautomated external defibrillator technology: a live cases video recording study. Emerg Med J. 2015;32(6):481–485. doi: 10.1136/emermed-2013-202962. [DOI] [PubMed] [Google Scholar]
- 92.Magid KH, Heard D, Sasson C. Addressing gaps in cardiopulmonary resuscitation education: training middle school students in hands-only cardiopulmonary resuscitation. J Sch Health. 2018;88(7):524–530. doi: 10.1111/josh.12634. [DOI] [PubMed] [Google Scholar]
- 93.Mathiesen WT, Bjørshol CA, Høyland S, Braut GS, Søreide E. Exploring how lay rescuers overcome barriers to provide cardiopulmonary resuscitation: A qualitative study. Prehosp Disaster Med. 2017;32(1):27–32. doi: 10.1017/S1049023X16001278. [DOI] [PubMed] [Google Scholar]
- 94.Mausz J, Snobelen P, Tavares W. “Please. Don't. Die.”: A grounded theory study of bystander cardiopulmonary resuscitation. Circ Cardiovasc Qual Outcomes. 2018;11(2):e004035-e. doi: 10.1161/CIRCOUTCOMES.117.004035. [DOI] [PubMed] [Google Scholar]
- 95.McCormack AP, Damon SK, Eisenberg MS. Disagreeable physical characteristics affecting bystander CPR. Ann Emerg Med. 1989;18(3):283–285. doi: 10.1016/S0196-0644(89)80415-9. [DOI] [PubMed] [Google Scholar]
- 96.Mecrow TS, Rahman A, Mashreky SR, Rahman F, Nusrat N, Scarr J, et al. Willingness to administer mouth-to-mouth ventilation in a first response program in rural Bangladesh. BMC Int Health Hum Rights. 2015;15(1):1–5. doi: 10.1186/s12914-015-0057-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Meischke HW, Rea TD, Eisenberg MS, Rowe SM. Intentions to use an automated external defibrillator during a cardiac emergency among a group of seniors trained in its operation. Heart Lung. 2002;31(1):25–29. doi: 10.1067/mhl.2002.119833. [DOI] [PubMed] [Google Scholar]
- 98.Moller TP, Hansen CM, Fjordholt M, Pedersen BD, Ostergaard D, Lippert FK. Debriefing bystanders of out-of-hospital cardiac arrest is valuable. Resuscitation. 2014;85(11):1504–11. doi: 10.1016/j.resuscitation.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 99.Nielsen AM, Isbye DL, Lippert FK, Rasmussen LS. Can mass education and a television campaign change the attitudes towards cardiopulmonary resuscitation in a rural community? Scandinavian journal of trauma. Resuscit Emerg Med. 2013;21(1):39. doi: 10.1186/1757-7241-21-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nishiyama C, Sato R, Baba M, Kuroki H, Kawamura T, Kiguchi T, et al. Actual resuscitation actions after the training of chest compression-only CPR and AED use among new university students. Resuscitation. 2019;141:63–68. doi: 10.1016/j.resuscitation.2019.05.040. [DOI] [PubMed] [Google Scholar]
- 101.Nolan RP, Wilson E, Shuster M, Rowe BH, Stewart D, Zambon S. Readiness to perform cardiopulmonary resuscitation: an emerging strategy against sudden cardiac death. Psychosom Med. 1999;61(4):546–551. doi: 10.1097/00006842-199907000-00020. [DOI] [PubMed] [Google Scholar]
- 102.Nord A, Svensson L, Hult H, Kreitz-Sandberg S, Nilsson L. Effect of mobile application-based versus DVD-based CPR training on students’ practical CPR skills and willingness to act: a cluster randomised study. BMJ Open. 2016;6(4):e010717-e. doi: 10.1136/bmjopen-2015-010717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Nord A, Hult H, Kreitz-Sandberg S, Herlitz J, Svensson L, Nilsson L. Effect of two additional interventions, test and reflection, added to standard cardiopulmonary resuscitation training on seventh grade students' practical skills and willingness to act: a cluster randomised trial. BMJ Open. 2017;7(6):e014230-e. doi: 10.1136/bmjopen-2016-014230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Omi W, Taniguchi T, Kaburaki T, Okajima M, Takamura M, Noda T, et al. The attitudes of Japanese high school students toward cardiopulmonary resuscitation. Resuscitation. 2008;78:82-7. [DOI] [PubMed]
- 105.Onan A, Turan S, Elcin M, Erbil B, Bulut ŞÇ. The effectiveness of traditional basic life support training and alternative technology-enhanced methods in high schools. 2018. [Google Scholar]
- 106.Parnell M, Pearson J, Galletly D, Larsen P. Knowledge of and attitudes towards resuscitation in New Zealand high-school students. Emerg Med J. 2006;23(12):899–902. doi: 10.1136/emj.2006.041160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Pei-Chuan Huang E, Chiang WC, Hsieh MJ, Wang HC, Yang CW, Lu TC, et al. Public knowledge, attitudes and willingness regarding bystander cardiopulmonary resuscitation: A nationwide survey in Taiwan. J Formos Med Assoc. 2018;118(2):72-81. [DOI] [PubMed]
- 108.Platz E, Scheatzle MD, Pepe PE, Dearwater SR. Attitudes towards CPR training and performance in family members of patients with heart disease. Resuscitation. 2000;47(3):273–280. doi: 10.1016/S0300-9572(00)00245-8. [DOI] [PubMed] [Google Scholar]
- 109.Rankin T, Holmes L, Vance L, Crehan T, Mills B. Recent high school graduates support mandatory cardiopulmonary resuscitation education in Australian high schools. Aust N Z J Public Health. 2020;44(3):215–218. doi: 10.1111/1753-6405.12990. [DOI] [PubMed] [Google Scholar]
- 110.Riou M, Ball S, Whiteside A, Gallant S, Morgan A, Bailey P, et al. Caller resistance to perform cardio-pulmonary resuscitation in emergency calls for cardiac arrest. Soc Sci Med. 2020;256:113045. [DOI] [PubMed]
- 111.Ro YS, Shin SD, Song KJ, Hong SO, Kim YT, Cho S-I. Bystander cardiopulmonary resuscitation training experience and self-efficacy of age and gender group: a nationwide community survey. Am J Emerg Med. 2016;34(8):1331–1337. doi: 10.1016/j.ajem.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 112.Rowe BH, Shuster M, Zambon S, Wilson E, Stewart D, Nolan RP, et al. Preparation, attitudes and behaviour in nonhospital cardiac emergencies: evaluating a community's readiness to act. Can J Cardiol. 1998;14(3):371–377. [PubMed] [Google Scholar]
- 113.Sasaki M, Ishikawa H, Kiuchi T, Sakamoto T, Marukawa S. Factors affecting layperson confidence in performing resuscitation of out-of-hospital cardiac arrest patients in Japan. Acute Med Surg. 2015;2(3):183–189. doi: 10.1002/ams2.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sasson C, Haukoos JS, Bond C, Rabe M, Colbert SH, King R, et al. Barriers and facilitators to learning and performing cardiopulmonary resuscitation in neighborhoods with low bystander cardiopulmonary resuscitation prevalence and high rates of cardiac arrest in Columbus. OH Circ Cardiovasc Qual Outcomes. 2013;6(5):550–558. doi: 10.1161/CIRCOUTCOMES.111.000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sasson C, Haukoos JS, Ben-Youssef L, Ramirez L, Bull S, Eigel B, et al. Barriers to calling 911 and learning and performing cardiopulmonary resuscitation for residents of primarily Latino, high-risk neighborhoods in Denver, Colorado. Ann Emerg Med. 2015;65(5):545–52. e2. doi: 10.1016/j.annemergmed.2014.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Schmid KM, Mould-Millman NK, Hammes A, Kroehl M, Garcia RQ, McDermott MU, et al. Barriers and facilitators to community CPR education in San Jose, Costa Rica. Prehosp Disaster Med. 2016;31(5):509–515. doi: 10.1017/S1049023X16000777. [DOI] [PubMed] [Google Scholar]
- 117.Schmitz B, Schuffelen P, Kreijns K, Klemke R, Specht M. Putting yourself in someone else's shoes: the impact of a location-based, collaborative role-playing game on behaviour. Comput Educ. 2015;85:160–169. doi: 10.1016/j.compedu.2015.02.012. [DOI] [Google Scholar]
- 118.Schneider L, Sterz F, Haugk M, Eisenburger P, Scheinecker W, Kliegel A, et al. CPR courses and semi-automatic defibrillators - life saving in cardiac arrest? Resuscitation. 2004;63(3):295–303. doi: 10.1016/j.resuscitation.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 119.Shams A, Raad M, Chams N, Chams S, Bachir R, El Sayed MJ. Community involvement in out of hospital cardiac arrest: A cross-sectional study assessing cardiopulmonary resuscitation awareness and barriers among the Lebanese youth. Medicine (Baltimore). 2016;95(43):e5091. [DOI] [PMC free article] [PubMed]
- 120.Shibata K, Taniguchi T, Yoshida M, Yamamoto K. Obstacles to bystander cardiopulmonary resuscitation in Japan. Resuscitation. 2000;44:187-93. [DOI] [PubMed]
- 121.Sipsma K, Stubbs BA, Plorde M. Training rates and willingness to perform CPR in King County, Washington: a community survey. Resuscitation. 2011;82(5):564–567. doi: 10.1016/j.resuscitation.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 122.Skora J, Riegel B. Thoughts, feelings, and motivations of bystanders who attempt to resuscitate a stranger: A pilot study. Am J Crit Care. 2001;10(6):408–416. doi: 10.4037/ajcc2001.10.6.408. [DOI] [PubMed] [Google Scholar]
- 123.Smith KL, Cameron PA, Meyer AD, McNeil JJ. Is the public equipped to act in out of hospital cardiac emergencies? Emerg Med J. 2003;20(1):85–87. doi: 10.1136/emj.20.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Sneath JZ, Lacey R. Marketing defibrillation training programs and bystander intervention support. Health Mark Q. 2009;26(2):87–97. doi: 10.1080/07359680802619784. [DOI] [PubMed] [Google Scholar]
- 125.So KY, Ko HF, Tsui CSY, Yeung CY, Chu YC, Lai VKW, et al. Brief compression-only cardiopulmonary resuscitation and automated external defibrillator course for secondary school students: a multischool feasibility study. BMJ Open. 2020;10(10):e040469. doi: 10.1136/bmjopen-2020-040469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Swor R, Grace H, McGovern H, Weiner M, Walton E. Cardiac arrests in schools: assessing use of automated external defibrillators (AED) on school campuses. Resuscitation. 2013;84(4):426–429. doi: 10.1016/j.resuscitation.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 127.Tang H-m, Wu X, Jin Y, Jin Y-q, Wang Z-j, Luo J-y, et al. Shorter training intervals increase high school students’ awareness of cardiopulmonary resuscitation: a questionnaire study. J Int Med Res. 2020;48(1):0300060519897692. doi: 10.1177/0300060519897692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Taniguchi T, Omi W, Inaba H. Attitudes toward the performance of bystander cardiopulmonary resuscitation in Japan. Resuscitation. 2007;75(1):82–87. doi: 10.1016/j.resuscitation.2007.02.019. [DOI] [PubMed] [Google Scholar]
- 129.Taniguchi T, Sato K, Fujita T, Okajima M, Takamura M. Attitudes to bystander cardiopulmonary resuscitation in Japan in 2010. Circ J. 2012;76(5):1130–1135. doi: 10.1253/circj.CJ-11-0054. [DOI] [PubMed] [Google Scholar]
- 130.Thorén A-N, Danielson E, Herlitz J, Axelsson AB. Spouses' experiences of a cardiac arrest at home: an interview study. Eur J Cardiovasc Nurs. 2010;9(3):161–167. doi: 10.1016/j.ejcnurse.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 131.Vaillancourt C, Kasaboski A, Charette M, Islam R, Osmond M, Wells GA, et al. Barriers and facilitators to CPR training and performing CPR in an older population most likely to witness cardiac arrest: a national survey. Resuscitation. 2013;84(12):1747–1752. doi: 10.1016/j.resuscitation.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 132.Vetter VL, Haley DM, Dugan NP, Iyer VR, Shults J. Innovative cardiopulmonary resuscitation and automated external defibrillator programs in schools: results from the student program for olympic resuscitation training in schools (SPORTS) study. Resuscitation. 2016;104:46–52. doi: 10.1016/j.resuscitation.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 133.Wilks J, Ma AWW, Vyas L, Wong KL, Tou AYL. CPR knowledge and attitudes among high school students aged 15-16 in Hong Kong. Hong Kong J Emerg Med. 2015;22(1):3–13. doi: 10.1177/102490791502200101. [DOI] [Google Scholar]
- 134.Winkelman JL, Fischbach R, Spinello EF. Assessing CPR training: the willingness of teaching credential candidates to provide CPR in a school setting. Educ Health. 2009;22(3):81. [PubMed] [Google Scholar]
- 135.Zinckernagel L, Malta Hansen C, Rod MH, Folke F, Torp-Pedersen C, Tjornhoj-Thomsen T. What are the barriers to implementation of cardiopulmonary resuscitation training in secondary schools? A qualitative study. BMJ Open. 2016;6(4):e010481. doi: 10.1136/bmjopen-2015-010481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Breckwoldt J, Lingemann C, Wagner P. Resuscitation training for lay persons in first aid courses: transfer of knowledge, skills and attitude. [German] Anaesthesist. 2016;65(1):22–29. doi: 10.1007/s00101-015-0113-8. [DOI] [PubMed] [Google Scholar]
- 137.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 138.Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46:81-95. [DOI] [PubMed]
- 139.Shaffer JA, DeGeest D, Li A. Tackling the problem of construct proliferation: A guide to assessing the discriminant validity of conceptually related constructs. Organ Res Methods. 2016;19(1):80–110. doi: 10.1177/1094428115598239. [DOI] [Google Scholar]
- 140.Michie S, Johnston M. Theories and techniques of behaviour change: developing a cumulative science of behaviour change. Health Psychol Rev. 2012;6(1):1–6. doi: 10.1080/17437199.2012.654964. [DOI] [Google Scholar]
- 141.Sutton AJ, Duval SJ, Tweedie R, Abrams KR, Jones DR. Empirical assessment of effect of publication bias on meta-analyses. Bmj. 2000;320(7249):1574–1577. doi: 10.1136/bmj.320.7249.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Farquharson B, Dixon D, Williams B. The psychological and behavioural factors associated with laypeople initiating CPR for our-of-hospital cardiac arrest: a systematic review. Euro J Cardio Nurs. 2021;20(supp 1):zvab060-045. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.