Abstract
Food insecurity is associated with poor clinical outcomes among adults with diabetes; however, associations with non-clinical outcomes, such as missed work, have not been well-characterized. Our objective was to assess the association between food insecurity, health-related missed workdays, and overnight hospitalizations. We pooled National Health Interview Survey data from 2011 through 2018 to analyze food insecurity among 13,116 adults aged 18–65 years with diabetes. Food insecurity was associated with increased odds of reporting any health-related missed workdays, more than twice the rate of health-related missed workdays, and increased odds of overnight hospitalization within the prior 12 months. There was no significant association between food insecurity and the number of nights spent hospitalized. These findings underscore the broad impacts food insecurity on health and wellness for working-age adults with diabetes. When weighing the costs and benefits of proposed interventions to address food insecurity, policymakers should consider potential benefits related to productivity in addition to implications for health care utilization.
Keywords: diabetes, food insecurity, absenteeism, hospitalization
Introduction
The United States Department of Agriculture (USDA) defines household food insecurity as “the limited or uncertain availability of nutritionally adequate and safe foods or limited or uncertain ability to acquire acceptable foods in socially acceptable ways.”(1) The USDA Economic Research Service estimates that 10.5 percent of households in the United States (13.8 million) were food insecure in 2020.(2) Food insecurity is more common among individuals with diabetes, and both the prevalence and incidence of type 2 diabetes is higher among individuals in food-insecure households.(3),(4),(5) Food insecurity can affect diabetes management in several ways. First, food insecurity is associated with poor diet quality.(6) Second, food insecurity may force individuals to make trade-offs among food, medications, and medical supplies. Food-insecure adults with diabetes are more likely to report cost-related medication underuse, in addition to less frequent blood glucose monitoring, than food secure adults with diabetes.(7–9) Finally, food insecurity has been shown to exacerbate stress and worsen mental health.(7)
Perhaps for these reasons, prior studies have found that food insecurity among individuals with diabetes is associated with poor clinical outcomes, including an increased risk for episodes of severe hypoglycemia(9), high HbA1c levels, and elevated LDL cholesterol levels.(5,10) Food insecurity has also been associated with high levels of utilization of and spending on health services.(5,7,11–14)
However, the association between food insecurity and outcomes within the health care system is likely only part of the burden of food insecurity on patients with chronic illness. A key concern is that the experience of food insecurity may create a vicious cycle whereby food insecurity can worsen health, resulting in hospitalizations and missed work, and the resulting missed work can lower income, thereby increasing the risk and extent of food insecurity.
There have been few studies of the relationship between food insecurity and work absenteeism among working-age adults with diabetes. Our study used nationally representative data to evaluate the association between food insecurity, health-related missed workdays, and overnight hospitalizations among this population. We hypothesized that food insecurity would be associated with greater odds of having a health-related missed workday and an overnight hospitalization. We also hypothesized that among working-age adults with diabetes, food insecurity would be associated with more health-related missed workdays and more nights hospitalized.
Methods
Data Source
This study used data from the National Health Interview Survey (NHIS) accessed through the Integrated Public Use Microdata Series, known as IPUMS.(15) The NHIS is conducted annually by the National Center for Health Statistics at the Centers for Disease Control and Prevention (CDC)(16,17) through interviews with a nationally representative sample of households in the civilian, non-institutionalized population.(17) Our analytic sample consisted of adults who reported a diabetes diagnosis and were aged 18 to 65 years old, which we considered working age as this age range has been used in prior research regarding workplace absenteeism and chronic illness(18). The sample years were 2011 – 2018, which we pooled into a single dataset for cross-sectional analysis to increase the sample size. These years were chosen due to the consistent availability of the necessary variables across the time period.
Measures
Exposure:
The primary exposure was food security status. Food security status is determined by the NHIS through the Family Food Security Supplement, a 10-item household questionnaire focusing on experiences with food security in the previous 30-day period. The raw scores on these questionnaires are used to categorize households as either food secure (0–2 affirmative responses) or food insecure (≥3 affirmative responses).
Outcomes:
The primary outcome was work missed due to injury or illness, which we refer to as health-related missed workdays. NHIS respondents were asked to report the number of days they missed work because of illness or injury in the previous 12 months, excluding maternity or paternity leave. The secondary outcome was overnight hospitalizations. All respondents were asked if they had any overnight hospitalizations in the prior 12 months and if so, they were asked to report the number of nights spent in the hospital within this time frame. The sample in the overnight hospitalization analysis included all working age-adults with diabetes, both those inside and outside the workforce. Only respondents who reported working for wages or at a family business were asked about missed work; therefore, the sample of individuals with health-related missed workdays was smaller than the sample of individuals with overnight hospitalizations. We top-coded the number of health-related missed workdays at 120, which is the 99th percentile of health-related missed workdays and is larger than the numbers among adults with diabetes that have been reported in previous research.(19,20) Similarly, we top-coded the number of nights spent hospitalized at 120, which was likewise above the 99th percentile.
Covariates:
To account for potential confounding of the relationship between food insecurity and study outcomes, we included respondent age; sex; race/ethnicity (categorized as Hispanic, non-Hispanic American Indian/Alaskan Native, non-Hispanic Asian, non-Hispanic Black/African-American, non-Hispanic White, and non-Hispanic other race and/or multiple races); income; education; and health insurance as covariates in the analysis. Race and ethnicity variables were included to help account for effects of interpersonal and structural racism, as more specific measures of racism were not available.(21) Income categories were defined relative to the United States Census Bureau’s poverty thresholds, which account for household size and inflation across survey years.
Statistical Analyses
Entropy Balance Weighting
We used entropy balancing weights to balance the covariates that we believe are likely to confound the relationship between food insecurity and study outcomes. This method is becoming increasingly popular in health services research for estimating effects in observational studies.(22–26) Similar to propensity score methods, entropy balancing allows researchers to create samples that are balanced on their covariates for the estimation of treatment effects.(27) A key advantage of using entropy balance weighting over traditional propensity score approaches is that entropy balancing directly searches for weights that meet a pre-determined level of covariate balance, thus eliminating the need to iteratively fit propensity score models and continually check balance until the optimal balance is reached.(27,28) For comparison, we provide the same analyses using a propensity score-based method (inverse probability weighting) in Appendix Exhibit 5.(29) We present the entropy balanced models as our main specifications, as entropy balance weighting achieved better covariate balance than the propensity score approach.
We used entropy balancing weights to balance the food secure and food insecure groups on income category, age, sex, race/ethnicity, education level, and health insurance status. We also included the NHIS survey weight as a covariate for entropy balancing as recommended by DuGoff, Schuler, and Stuart (2014) for the estimation of population average treatment effects.(30) We then multiplied the balancing weights by the NHIS survey weights for the outcome modeling. This approach yields results that are nationally representative. As there are fewer respondents included in the sample for the health-related missed workdays outcome, we separately calculated two sets of weights, one for use in modeling health-related missed workdays and one for modeling overnight hospitalizations. Covariate balance prior to and after entropy balancing is shown in Appendix Exhibits 1a and 1b.(29) We also conducted sensitivity analyses in which we removed income and insurance from both weighting and outcome modeling to address concerns of potential endogeneity.
Outcome modeling
To model the outcomes of hospitalizations and health-related missed workdays, we implemented two hurdle models. The first part of a hurdle model estimates the probability of any occurence of the outcome (such as whether an individual had any hospitalization in a given year), while the second part of the model estimates the expected level of the outcome conditional on an individual having any occurence of the outcome(such as how many nights an individual would be expected to be hospitalized if they were hospitalized).(31) Using hurdle models allowed us to estimate the association between food insecurity and having any missed workdays or hospitalizations, along with the association between food insecurity and the number of health-related missed workdays and the number of nights spent in the hospital. Further, it allows for a population-averaged estimate of the overall association between food insecurity and study outcomes (combining both parts of the model).
We specified the first part of our hurdle models as a logistic regression and, to address overdispersion, we specified the second part as zero-truncated negative binomial regressions. We report the results of the first part of the hurdle models in relative terms as odds ratios (ORs) and the results of the second part of the hurdle models as incidence rate ratios (IRRs). We used predictive margins (also known as recycled predictions) to express results in absolute terms.(32) We use a 2-tailed p-value < 0.05 to indicate statistical significance. Because our data had less than 10% of observations with missingness across any of the included items (>90% complete cases), we did not pursue imputation of missing data. In the event of a single sampling unit, we scaled our variance using the average of variances of the strata with multiple sampling units. We included all of the predictors used in the entropy balancing in our outcome models to produce doubly-robust estimates.(33–35) All data cleaning and entropy balance weighting was conducted using R(36) and RStudio(37), primarily using the WeightIt(38) and cobalt(39) packages, and outcome modeling was conducted with Stata 16.(40)
The study has several key strengths. We provide nationally representative estimates using rigorous statistical methods to account for potential confounders of the relationship between food insecurity and study outcomes. We also characterize the association between food insecurity and absenteeism, which complements traditional clinical and health care utilization outcomes, to assess the holistic effects of food insecurity on overall wellbeing of individuals with diabetes.
Limitations
There are several limitations to our analysis. First, the analysis is cross-sectional, thus we cannot establish the time ordering between food insecurity and study outcomes. Next, NHIS data are self-reported. As such, study variables may have been measured with error. Additionally, though we adjusted for a robust set of covariates, we cannot exclude the possibility of unmeasured confounding. Furthermore, NHIS assesses food insecurity during the previous 30-day period and study outcomes during the previous 12-month period. While reverse causation is a potential problem for any cross-sectional study, it may be of particular concern here. Specifically, missed work and/or hospitalizations may lead to food insecurity, rather than the other way around. However, even if missed work or a hospitalization is what initially led to food insecurity, ongoing food insecurity could lead to further missed work or hospitalizations. Thus, it is important to consider the possible occurrence of a ‘vicious cycle’—whereby food insecurity contributes to worsened health and the consequences of worsened health contribute to food insecurity—when assessing the relationship between these two factors.
Finally, our analyses of missed work yielded estimates that are conditional on an individual having a form of employment. If food insecurity had prevented an individual from pursuing or maintaining employment prior to the study period, the true effects of food insecurity on health-related missed work could be underestimated in our analyses. An important direction for future work would be to examine the role, if any, of food insecurity in determining whether individuals participate in the labor force at all, particularly those with chronic conditions.
Results
Results presented in this section reflect the application of the weights previously described, unless otherwise noted. The analytic sample for the health-related missed workdays outcome included 7,308 (unweighted) respondents aged 18 – 65 years old, with diagnosed diabetes from years 2011 through 2018. They represented 2.91 million individuals. The mean age among those included in this sample was 50.33 years (SD: 10.69), and 15.07% were food insecure. This analytic sample consisted of 52.77% males and 47.23% females. Descriptive statistics, based on the weighted sample sizes, can be found in Exhibit 1. The study sample for the hospitalization outcome consisted of 13,116 (unweighted) respondents, representing 5.14 million adults in the United States. Of the respondents, 24.42% were food insecure and the mean age was 52.35 years (SD: 10.48). This analytic sample consisted of 50.83% females and 49.17% males.
Exhibit 1:
Characteristics of sample to analyze impact of food insecurity on health-related missed workdays and hospitalizations, weighted, 2011 – 2018
| Characteristic | Health-Related Missed Workdays | Hospitalizations | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Total N = 2,910,104 | Food Insecure N = 438,803 | Food Secure N = 2,471,301 | Total N = 5,135,950 | Food Insecure N = 1,254,208 | Food Secure N = 3,881,742 | |
|
| ||||||
| Age (mean) | 50.33 | 50.36 | 50.32 | 52.35 | 52.40 | 52.34 |
| Sex (%) | ||||||
| Female | 47.23 | 45.09 | 47.61 | 50.83 | 50.32 | 51.00 |
| Male | 52.77 | 54.91 | 52.39 | 49.17 | 49.68 | 49.00 |
| Race/Ethnicity (%) | ||||||
| Hispanic | 15.74 | 16.12 | 15.67 | 15.99 | 16.54 | 15.81 |
| American Indian/Alaskan Native |
0.93 |
0.77 |
0.96 |
1.14 |
1.01 |
1.18 |
| Asian | 4.46 | 3.81 | 4.57 | 3.59 | 3.18 | 3.73 |
| Black/African American |
16.23 |
17.41 |
16.03 |
18.06 |
18.72 |
17.84 |
| Other Race and/or Multiple Races |
1.45 |
1.69 |
1.40 |
1.81 |
1.91 |
1.78 |
| White | 61.19 | 60.21 | 61.37 | 59.42 | 58.65 | 59.66 |
| Education (%) | ||||||
| Some college or higher | 62.58 | 63.25 | 62.46 | 53.26 | 53.04 | 53.34 |
| High school diploma, GED, or equivalent | 26.33 | 25.83 | 26.42 | 28.33 | 27.98 | 28.44 |
| Less than high school diploma | 11.09 | 10.92 | 11.12 | 18.41 | 18.98 | 18.22 |
| Income level (%) | ||||||
| Percent of poverty | ||||||
| Less than 100% | 10.93 | 10.54 | 11.00 | 24.41 | 25.01 | 24.21 |
| 100 – 199% | 16.32 | 17.22 | 16.16 | 20.94 | 21.25 | 20.84 |
| 200 – 299% | 16.42 | 16.64 | 16.39 | 14.82 | 14.75 | 14.85 |
| 300 – 399% | 14.82 | 13.56 | 15.05 | 11.53 | 10.96 | 11.72 |
| 400 – 499% | 12.29 | 13.42 | 12.09 | 9.01 | 9.74 | 8.77 |
| 500% and above | 29.21 | 28.62 | 29.32 | 19.30 | 18.30 | 19.62 |
| Insurance (%) | ||||||
| Private | 70.9 | 69.72 | 71.16 | 51.03 | 50.07 | 51.35 |
| Military Health Plan | 0.99 | 1.22 | 0.95 | 1.66 | 1.85 | 1.60 |
| Medicare | 2.19 | 2.19 | 2.19 | 10.55 | 10.77 | 10.48 |
| Medicaid | 6.32 | 7.22 | 6.15 | 12.47 | 13.03 | 12.29 |
| Medicare & Medicaid | 0.80 | 0.80 | 0.80 | 6.32 | 6.39 | 6.30 |
| Other health insurance | 6.03 | 5.44 | 6.13 | 6.37 | 6.08 | 6.46 |
| Uninsured | 12.73 | 13.40 | 12.61 | 11.58 | 11.80 | 11.51 |
SOURCE: Authors’ analysis of National Health Interview Survey (NHIS) data, including the NHIS Survey Family Food Security Supplement, 2011–2018. NOTES: Households responding affirmatively to 3 or more of the 10 questions on the Supplement about food security over the previous 30 days were categorized as food insecure and otherwise as food secure. The main NHIS questionnaire asked respondents about health-related missed workdays and overnight hospitalizations over the previous 12 months. N’s, means, and percentages are weighted using a combination of NHIS survey weights and entropy balancing weights. Only respondents who reported employment were asked about missed work; therefore, the sample of individuals included in the health-related missed workdays analysis was smaller than the sample of individuals included in the overnight hospitalizations analysis. Racial groups are non-Hispanic. Poverty level represents the US Census Bureau’s poverty threshold, which accounts for household size and inflation across survey years. Private health insurance includes all comprehensive private health plans, including employer-sponsored commercial insurance and insurance purchased in the individual insurance market.
Unadjusted outcomes are presented in Exhibit 2. Approximately half (50.57%) of working-age adults with diabetes had a health-related missed workday in the previous 12 months, with an average of 13.32 (SD: 28.04) missed workdays among food-insecure individuals and 6.02 (SD: 17.80) missed workdays among food-secure individuals. Approximately 19% of working-age adults with diabetes had an overnight hospitalization in the previous 12 months. Food-insecure individuals spent an average of 2.77 (SD: 11.12) nights hospitalized, and food-secure individuals had an average of 1.41 (SD: 6.25) nights in the hospital.
Exhibit 2:
Unadjusted missed workdays and hospitalizations among working-age adults with diabetes by food security status, 2011 – 2018
| Any health-related missed workdays (%) | Number of health-related missed workdays (mean) | Any overnight hospitalizations (%) | Number of nights spent hospitalized (mean) | |
|---|---|---|---|---|
|
| ||||
| Total | 50.57 | 7.12 | 19.03 | 1.74 |
| Food Insecure | 58.37 | 13.32 | 25.37 | 2.77 |
| Food Secure | 49.18 | 6.02 | 16.97 | 1.41 |
SOURCE: Authors’ analysis of National Health Interview Survey (NHIS) data, including the NHIS Survey Family Food Security Supplement, 2011–2018. NOTES: Households responding affirmatively to 3 or more of the 10 questions on the Supplement about food security over the previous 30 days were categorized as food insecure and otherwise as food secure. The main NHIS questionnaire asked respondents about health-related missed workdays and overnight hospitalizations over the previous 12 months. 1,471,640 (weighted) individuals in the health-related missed workdays analysis had a health-related missed workday and 976,765(weighted) individuals in the hospitalizations analysis had an overnight hospitalization. Means and percentages are weighted using a combination of NHIS survey weights and entropy balancing weights.
Food insecurity was associated with greater odds of having any missed workdays (OR: 1.47, 95% CI: 1.06, 2.04) in the past 12 months (Appendix Exhibit 2, Appendix Exhibit 3). (29) The mean predicted probability of a health-related missed workday was 58.34% (95% CI: 50.83%, 65.84%) for food insecure adults with diabetes compared to 49.19% (95% CI: 47.74%, 50.64%) for food secure adults with diabetes (Exhibit 3). Among those who missed any workdays, food insecurity was also associated with more than twice as many workdays missed due to injury or illness (IRR: 2.24, 95% CI: 1.56, 3.22), (Appendix Exhibit 2, Appendix Exhibit 3). (29) The mean predicted number of health-related missed workdays was 4.36 (95% CI: 4.23, 4.49) for food insecure adults with diabetes compared to 1.41 (95% CI: 1.39, 1.43) for food secure adults with diabetes (distribution in Appendix Exhibit 6a).(29)
EXHIBIT 3.
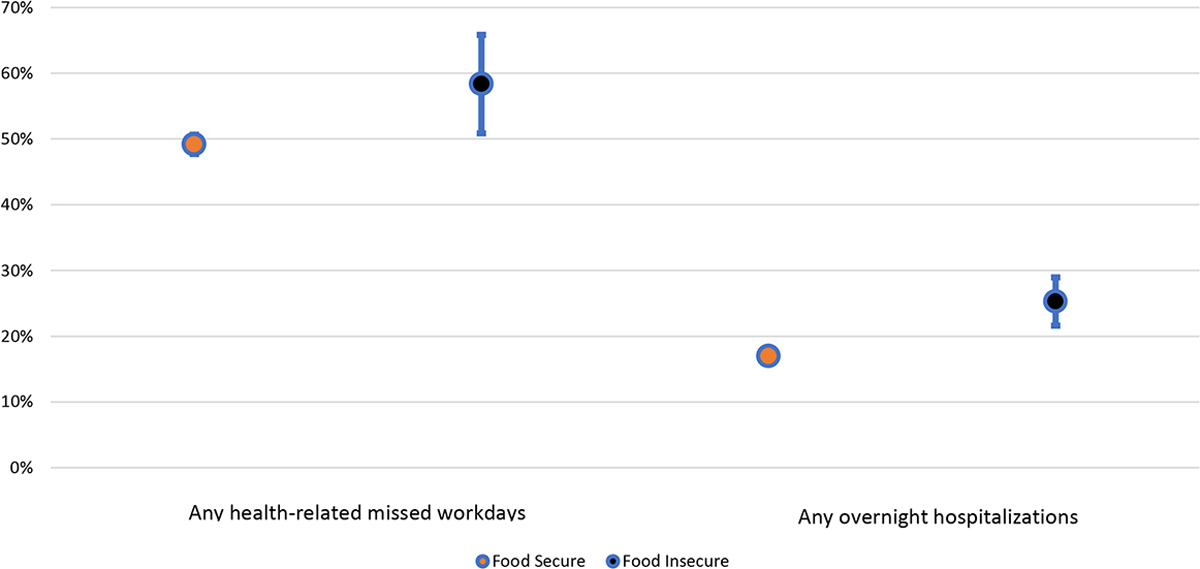
Predicted probability of health-related missed workdays and overnight hospitalizations among working-age adults with diabetes by food security status, 2011 – 2018
SOURCE: Authors’ analysis of National Health Interview Survey (NHIS) data, including the NHIS Survey Family Food Security Supplement, 2011 – 2018.
NOTES: Households responding affirmatively to 3 or more of the 10 questions on the Supplement about food security over the previous 30 days were categorized as food insecure and otherwise as food secure. The main NHIS questionnaire asked respondents about health-related missed workdays and overnight hospitalizations over the previous 12 months. Predicted probabilities were calculated via predictive margins (i.e. recycled predictions), a method to calculate the marginal effects in non-linear models by varying the characteristic of interest across all observations in the data and averaging the predictions.(52)
Food insecurity was associated with greater odds of any overnight hospitalization (OR: 1.68, 95% CI: 1.36, 2.07) in the past 12 months (Appendix Exhibit 2, Appendix Exhibit 3).(29) The mean predicted probability of an overnight hospitalization was 25.27% (95% CI: 21.61%, 28.93%) for food insecure adults with diabetes, compared to 17.00% (95% CI: 16.14%, 17.86%) for food secure adults with diabetes (Exhibit 3). Of those who had any overnight hospitalizations, there was no statistically significant association between food insecurity and the number of nights spent in the hospital (IRR: 1.050, 95% CI: 0.79, 1.40) (Appendix Exhibit 2, Appendix Exhibit 3).(29) The mean predicted number of nights spent hospitalized was 1.70 (95% CI: 1.66, 1.74) for food-insecure adults with diabetes and 0.77 (95% CI: 0.76, 0.78) for food-secure adults with diabetes (distribution in Appendix Exhibit 6b).(29)
Results of the sensitivity analysis are presented in Appendix Exhibit 4.(29) Compared to estimates from the main models, estimates from models that did not adjust for health insurance and income category were similar with regard to health-related missed workdays, but found both a higher odds ratio for any overnight hospitalizations (OR: 2.039, 95% CI: 1.80, 2.31) and a significantly higher incidence rate for nights spent hospitalized (IRR: 1.50, 95% CI: 1.22, 1.83).
Discussion
In a nationally representative study, and accounting for several relevant confounders, we found that food insecurity was associated with a greater risk of missing work, a greater number of missed workdays, and a greater risk of hospitalizations in working-age adults with diabetes. The magnitude of the association is notable; food insecurity was associated with more than twice the incidence rate of health-related missed workdays among adults with diabetes compared to being food secure. Food insecurity was associated with nearly a full 5-day (predicted 4.36 days) work week of health-related missed workdays in the past 12 months; it is reasonable to posit that this degree of absenteeism may worsen subsequent food insecurity and have broader economic impacts for the individuals affected, such as inability to afford medication and/or other necessities. Absenteeism is an important, patient-oriented measure of health status, and is an indicator of day-to-day impacts of chronic illness that complements more standard indicators such as clinical outcomes and healthcare utilization. Therefore, absenteeism should be examined when evaluating the health and economic impact of chronic illness.
Food insecurity is a consequence of insufficient financial means, primarily household income.(41) There is a well-documented relationship between income and health status,(42–46) especially among individuals with diabetes.(47–50) For hourly workers, missed workdays often represent lost wages, and, thus, lower incomes than they would have received had they not missed work. Bishu et al. (2015) found that the mean cost of missed workdays for those with diabetes was $277 in 2011 (equivalent to $354 in 2022,(51) suggesting that multiple days of missed work per year associated with food insecurity may have a substantial economic impact. For this reason, it is plausible that policies to address lost wages, such as paid sick leave, could help prevent a reinforcing feedback loop whereby food insecurity leads to poor health, resulting in missed work, which could lead to lower income that contributes to food insecurity.
Our findings on the association between food insecurity and hospitalization generally align with prior studies.(7,8,12,14) Above all, these data underscore the complex and far-reaching ways in which food security may impact multiple aspects of health and wellness for working-age adults with diabetes. Food insecurity may be a key focus for interventions seeking to improve health for individuals experiencing material disadvantage. Further, our findings serve as a reminder that food insecurity may have significant effects on day-to-day management of and experiences of living with diabetes that are not entirely ‘seen’ within the health care system, and thus, these effects may not be entirely captured by measures of healthcare utilization.
Future research should continue to prioritize patient-oriented and holistic metrics for diabetes outcomes stemming from food insecurity. Outcomes such as health-related missed workdays should be incorporated into the evaluation of food assistance programs to ensure that they are successful not only from clinical perspective, but also with regard to functional and financial impacts.
Future research could build on this study through designs to more precisely determine causality. For example, such studies could collect longitudinal data to assess changes in hospitalization and health-related workplace absenteeism among those experiencing varying degrees of food security, especially since food security status may be transitory and undergo changes during an individual’s lifetime. Randomized trials of food insecurity interventions will be important tools for understanding health effects of efforts to alleviate food insecurity, including effects on health outcomes traditionally measured in health services research, as well as on economic outcomes such as missed work.
Conclusion
Food insecurity is all too common in the United States, especially for individuals with diabetes. Evidence from this study and others contribute to a growing body of literature suggesting that food insecurity may lead to a vicious cycle whereby it worsens health, resulting in hospitalizations and missed work, thus potentially lowering income and increasing the risk and extent of food insecurity. New and creative approaches to address food insecurity may help break this cycle. Because medical and social factors are intertwined, policy approaches to improve health for people with diabetes should address not only health care but also social circumstances, such as food insecurity, that affect health. When weighing the costs and benefits of proposed interventions, policymakers should consider potential benefits related to productivity in addition to implications for health care utilization.
Supplementary Material
Acknowledgements:
JMW, SAB, ARK conceptualized the study design and analyses. JMW ran analyses and drafted the initial version of the manuscript. JMW, SAB, ARK critically revised the manuscript.
Endnotes
- 1.Coleman-Jensen A, Rabbitt MP, Hales L, Gregory CA. Food Insecurity in the U.S.: Measurement [Internet]. Washington, DC: United States Department of Agriculture Economic Research Service; 2021. [cited 2021 Oct 4]. Available from: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/measurement.aspx [Google Scholar]
- 2.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2020. Washington, D.C.: United States Department of Agriculture Economic Research Service; 2021. [cited 2021 Oct 4] Sep. Report No.: ERR-298. Available at: https://www.ers.usda.gov/publications/pub-details/?pubid=102075 [Google Scholar]
- 3.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med. 2007. Jul;22(7):1018–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tait CA, L’Abbé MR, Smith PM, Rosella LC. The association between food insecurity and incident type 2 diabetes in Canada: A population-based cohort study. PLoS ONE. 2018. May 23;13(5):e0195962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berkowitz SA, Meigs JB, DeWalt D, Seligman HK, Barnard LS, Bright O-JM, et al. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med. 2015. Feb;175(2):257–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Orr CJ, Keyserling TC, Ammerman AS, Berkowitz SA. Diet quality trends among adults with diabetes by socioeconomic status in the U.S.: 1999–2014. BMC Endocr Disord. 2019. May 31;19(1):54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gucciardi E, Vahabi M, Norris N, Del Monte JP, Farnum C. The Intersection between Food Insecurity and Diabetes: A Review. Curr Nutr Rep. 2014;3(4):324–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marjerrison S, Cummings EA, Glanville NT, Kirk SFL, Ledwell M. Prevalance and associations of food insecurity in children with diabetes mellitus. J Pediatr. 2011. Apr;158(4):607–11. [DOI] [PubMed] [Google Scholar]
- 9.Seligman HK, Jacobs EA, Lopez A, Sarkar U, Tschann J, Fernandez A. Food insecurity and hypoglycemia among safety net patients with diabetes. Arch Intern Med. 2011. Jul 11;171(13):1204–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care. 2013. Oct;36(10):3093–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berkowitz SA, Basu S, Meigs JB, Seligman HK. Food Insecurity and Health Care Expenditures in the United States, 2011–2013. Health Serv Res. 2018. Jun;53(3):1600–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mendoza JA, Haaland W, D’Agostino RB, Martini L, Pihoker C, Frongillo EA, et al. Food insecurity is associated with high risk glycemic control and higher health care utilization among youth and young adults with type 1 diabetes. Diabetes Res Clin Pract. 2018. Apr;138:128–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nelson K, Cunningham W, Andersen R, Harrison G, Gelberg L. Is food insufficiency associated with health status and health care utilization among adults with diabetes? J Gen Intern Med. 2001. Jun;16(6):404–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seligman HK, Davis TC, Schillinger D, Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved. 2010. Nov;21(4):1227–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blewett LA, Rivera Drew JA, King ML, Williams KCW. IPUMS Health Surveys: National Health Interview Survey, Version 6.4 [Internet]. Minneapolis, MN: IPUMS; 2019. [cited 2021 Dec 30]. Available from: https://nhis.ipums.org/nhis/ [Google Scholar]
- 16.Centers for Medicare & Medicaid Services. National Health Interview Survey (NHIS) [Internet]. Woodlawn, MD: Centers for Medicare & Medicaid Services; 2021. [cited 2021 Oct 4]. Available from: https://www.cms.gov/About-CMS/Agency-Information/OMH/resource-center/hcps-and-researchers/data-tools/sgm-clearinghouse/nhis [Google Scholar]
- 17.Center for Disease Control and Prevention, National Center for Health Statistics. National Health Interview Survey 2018 Data Release [Internet]. Hyattsville, MD: Centers for Disease Control and Prevention, National Center for Health Statistics; 2020. [cited 2021 Oct 3]. Available from: https://www.cdc.gov/nchs/nhis/nhis_2018_data_release.htm [Google Scholar]
- 18.Salter A, Thomas N, Tyry T, Cutter G, Marrie RA. Employment and absenteeism in working-age persons with multiple sclerosis. J Med Econ. 2017. May;20(5):493–502. [DOI] [PubMed] [Google Scholar]
- 19.Testa MA, Simonson DC. Health economic benefits and quality of life during improved glycemic control in patients with type 2 diabetes mellitus: a randomized, controlled, double-blind trial. JAMA. 1998. Nov 4;280(17):1490–6. [DOI] [PubMed] [Google Scholar]
- 20.Tunceli K, Bradley CJ, Lafata JE, Pladevall M, Divine GW, Goodman AC, et al. Glycemic control and absenteeism among individuals with diabetes. Diabetes Care. 2007. May;30(5):1283–5. [DOI] [PubMed] [Google Scholar]
- 21.Hill-Briggs F, Adler NE, Berkowitz SA, Chin MH, Gary-Webb TL, Navas-Acien A, et al. Social determinants of health and diabetes: A scientific review. Diabetes Care. 2020. Nov 2; 44(1):258–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mattke S, Han D, Wilks A, Sloss E. Medicare home visit program associated with fewer hospital and nursing home admissions, increased office visits. Health Aff (Millwood). 2015. Dec;34(12):2138–46. [DOI] [PubMed] [Google Scholar]
- 23.Ko H, Glied SA. Associations between a new york city paid sick leave mandate and health care utilization among medicaid beneficiaries in new york city and new york state. JAMA Health Forum. 2021. May 6;2(5):e210342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marty R, Dolan CB, Leu M, Runfola D. Taking the health aid debate to the subnational level: the impact and allocation of foreign health aid in Malawi. BMJ Glob Health. 2017. Jan 11;2(1):e000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trombley M Investigating Applications of Prognostic Scores to Balancing Weights: Evidence from an Evaluation of Accountable Care Organizations. Health Serv Res. 2021. Sep;56(S2):68–68. [Google Scholar]
- 26.Gottschalk S, König H-H, Brettschneider C. The association between informal caregiving and behavioral risk factors: a cross-sectional study. Int J Public Health. 2020. Jul;65(6):911–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hainmueller J Entropy balancing for causal effects: A multivariate reweighting method to produce balanced samples in observational studies. Political Analysis. 2012;20(01):25–46. [Google Scholar]
- 28.Parish WJ, Keyes V, Beadles C, Kandilov A. Using entropy balancing to strengthen an observational cohort study design: lessons learned from an evaluation of a complex multi-state federal demonstration. Health Serv Outcomes Res Method. 2018. Mar;18(1):17–46. [Google Scholar]
- 29.To access the appendix, click on the Details tab of the article online.
- 30.Dugoff EH, Schuler M, Stuart EA. Generalizing observational study results: applying propensity score methods to complex surveys. Health Serv Res. 2014. Feb;49(1):284–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deb P, Norton EC. Modeling health care expenditures and use. Annu Rev Public Health. 2018. Apr 1;39:489–505. [DOI] [PubMed] [Google Scholar]
- 32.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999. Jun;55(2):652–9. [DOI] [PubMed] [Google Scholar]
- 33.Zhao Q, Percival D. Entropy balancing is doubly robust. J Causal Inference. 2017. Sep 26;5(1):20160010. [Google Scholar]
- 34.Josey KP, Berkowitz SA, Ghosh D, Raghavan S. Transporting experimental results with entropy balancing. Stat Med. 2021. Aug 30;40(19):4310–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Funk MJ, Westreich D, Wiesen C, Stürmer T, Brookhart MA, Davidian M. Doubly robust estimation of causal effects. Am J Epidemiol. 2011. Apr 1;173(7):761–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.R Core Team. R: A language and environment for statistical computing [Internet]. Vienna, Austria: R Foundation for Statistical Computing; 2021. [cited 2021 Oct 15]. Available from: https://www.R-project.org/. [Google Scholar]
- 37.RStudio Team. RStudio: Integrated Development Environment for R [Internet]. Boston, MA: RStudio, PBC; 2021. [cited 2021 Oct 15]. Available from: http://www.rstudio.com/. [Google Scholar]
- 38.Greifer N WeightIt: Weighting for Covariate Balance in Observational Studies [Internet]. Vienna, Austria: R Foundation for Statistical Computing Comprehensive R Archive Network (CRAN); 2021. [cited 2021 Oct 15]. Available from: https://CRAN.R-project.org/package=WeightIt [Google Scholar]
- 39.Greifer N Cobalt: Covariate Balance Tables and Plots [Internet]. Vienna, Austria: R Foundation for Statistical Computing Comprehensive R Archive Network (CRAN); 2021. [cited 2021 Oct 15]. Available from: https://CRAN.R-project.org/package=cobalt [Google Scholar]
- 40.StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC. [Google Scholar]
- 41.Furness BW, Simon PA, Wold CM, Asarian-Anderson J. Prevalence and predictors of food insecurity among low-income households in Los Angeles County. Public Health Nutr. 2004. Sep;7(6):791–4. [DOI] [PubMed] [Google Scholar]
- 42.Pickett KE, Wilkinson RG. Income inequality and health: a causal review. Soc Sci Med. 2015. Mar;128:316–26. [DOI] [PubMed] [Google Scholar]
- 43.Marmot M The influence of income on health: views of an epidemiologist. Health Aff (Millwood). 2002. Apr;21(2):31–46. [DOI] [PubMed] [Google Scholar]
- 44.Emerson E, Graham H, Hatton C. Household income and health status in children and adolescents in Britain. Eur J Public Health 2006. Aug;16(4):354–60. [DOI] [PubMed] [Google Scholar]
- 45.McLeod CB, Lavis JN, Mustard CA, Stoddart GL. Income inequality, household income, and health status in Canada: a prospective cohort study. Am J Public Health. 2003. Aug;93(8):1287–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Odutayo A, Gill P, Shepherd S, Akingbade A, Hopewell S, Tennankore K, et al. Income Disparities in Absolute Cardiovascular Risk and Cardiovascular Risk Factors in the United States, 1999–2014. JAMA Cardiol. 2017. Jul 1;2(7):782–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cengiz E, Xing D, Wong JC, Wolfsdorf JI, Haymond MW, Rewers A, et al. Severe hypoglycemia and diabetic ketoacidosis among youth with type 1 diabetes in the T1D Exchange clinic registry. Pediatr Diabetes. 2013. Sep;14(6):447–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Minges KE, Whittemore R, Weinzimer SA, Irwin ML, Redeker NS, Grey M. Correlates of overweight and obesity in 5529 adolescents with type 1 diabetes: The T1D Exchange Clinic Registry. Diabetes Res Clin Pract. 2017. Apr;126:68–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lipman TH, Hawkes CP. Racial and socioeconomic disparities in pediatric type 1 diabetes: time for a paradigm shift in approach. Diabetes Care. 2021. Jan;44(1):14–6. [DOI] [PubMed] [Google Scholar]
- 50.Gallegos-Macias AR, Macias SR, Kaufman E, Skipper B, Kalishman N. Relationship between glycemic control, ethnicity and socioeconomic status in Hispanic and white non-Hispanic youths with type 1 diabetes mellitus. Pediatr Diabetes. 2003. Mar;4(1):19–23. [DOI] [PubMed] [Google Scholar]
- 51.Bishu KG, Gebregziabher M, Dismuke CE, Egede LE. Quantifying the Incremental and Aggregate Cost of Missed Workdays in Adults with Diabetes. J Gen Intern Med. 2015. Dec;30(12):1773–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.StataCorp. Stata 17 Base Reference Manual. College Station, TX: Stata Press; 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


