Abstract
The concept of alliance reflects the collaborative relationship between a clinician and a patient, defined as consisting of three elements: a) the agreement on the goals of treatment; b) the agreement on a task or series of tasks; c) the development of a bond. Although much of the theory and research on the alliance comes from the domain of psychotherapy, the concept is applicable to any practice involving a person seeking help and a socially sanctioned healer. An extensive research evidence suggests that the alliance (typically measured at the third or fourth session) is a robust predictor of the outcomes of various forms of psychotherapy, even when prior symptom improvement and other factors are considered. Both the clinician and the patient bring to the therapy situation different capacities to form an alliance. Factors concerning the patient include, among others, the diagnosis, attachment history and style, motivation, and needs for affiliation. However, the benefits of the alliance have been found to be mostly due to the therapist's contribution, in particular his/her facilitative interpersonal skills, including verbal fluency, communication of hope and positive expectations, persuasiveness, emotional expression; warmth, acceptance and understanding; empathy, and alliance rupture‐repair responsiveness. Placebo studies have allowed to experimentally manipulate aspects of the relationship between a therapist and a patient in non‐psychotherapy contexts. In these settings, two components of the relationship have emerged: an emotional one (involving being cared for and understood by the clinician) and a cognitive one (including the belief in the competence of the therapist to select and administer an effective treatment). Here we propose a model that describes three pathways through which the alliance creates benefits, named CARE (caring, attentive, real and empathic), EXPECTANCY, and SPECIFIC. Although research and clinical attention have mostly focused on the alliance between a clinician and a patient in face‐to‐face interactions, there is preliminary evidence concerning the alliance between patients and other clinic staff, systems of care, or the program in Internet‐mediated services. These new research areas clearly require further development.
Keywords: Alliance, relationship, bond, expectations, treatment goals, competence, warmth, empathy, placebos, trust
In many instances, there is a propensity for humans to disregard phenomena that permeate everyday life. For example, we converse using language much of the day without paying it the least regard. Of course, we become acutely aware of language when confronted with an unusual situation, such as an interaction with a person with aphasia, when interacting with others who are using an unfamiliar language, or when having to pick our words carefully in a challenging situation. Yet language, when examined, is exceedingly complex and is studied and understood from a variety of perspectives, including linguistics, psychology, neuroscience, anthropology, sociology, and literature. Language is vital to human life – without it, humans could not exist.
The alliance is the “language” of mental health care. To varying degrees, it is present in all interactions between a clinician and a patient but, like language, it is typically ignored until it is disrupted or vanishes. Examining the alliance from multiple perspectives unveils its nature and highlights aspects of it that could lead to improved quality of care.
In this paper, we trace the historical roots of the alliance concept, and provide a definition of it. We then review the evidence related to the alliance, which demonstrates its importance for the outcomes of mental health treatments. These discussions lead to a presentation of the psychological mechanisms that explain how the alliance produces benefits, and of clinical applications, including some recent developments which involve systems of care.
HISTORICAL ROOTS AND DEFINITION OF THE ALLIANCE CONCEPT
The concept of the alliance is usually traced to E. Bordin's seminal 1979 paper entitled The Generalizability of the Psychoanalytic Concept of the Working Alliance 1 . Bordin intertwined two psychoanalytic threads. The first involved the relationship between the analyst and the patient's rational ego as well as the notion of a therapeutic contract2, 3. The second borrowed the psychoanalytic concept of the “real relationship”, which is the transference‐free relationship between the patient and the analyst4, 5.
Bordin's contribution was to weave the two threads together to define a concept that he labeled the working alliance, which applied to all forms of psychotherapy as well as to other relationships that involved a person seeking help and a person designated as a helper. He defined the alliance as containing three elements: a) the agreement on the goals of treatment; b) the assignment of a task or series of tasks; and c) the development of a bond. Several of the issues discussed by Bordin over a half century ago remain central to current discussions of the alliance.
The title of Bordin's paper mentioned generalizability to emphasize that the importance of the alliance was not limited to psychoanalysis. Indeed, he stated: “I propose that the working alliance between the person who seeks change and the one who offers to be a change agent is one of the keys, if not the key, to the change process… A working alliance between a person seeking change and a change agent can occur in many places besides the locale of psychotherapy. The working alliance can be defined and elaborated in terms which make it universally applicable” 1, p.252 . Accordingly, his model is often referred to as trans‐theoretical, although he did not use that label. However, he did emphasize that aspects of the alliance will depend on the nature of the treatment used to create change. That is, the nature of the alliance and how it leads to improved outcomes depends on the particular treatment.
The expression agreement on the goals of treatment suggests to many that the therapist and the patient explicitly discuss the goals of treatment, coming to an agreement, after which the treatment can begin. However, it rarely happens this way. It seems that experienced therapists in high‐alliance and successful cases rarely explicitly discuss the very specific goals of treatment, although they do induce a future orientation through various techniques6, 7. This raises the question of what is meant by goals of treatment, particularly the level of specificity of such goals.
As Bordin discussed, the choice of therapist and therapy determines much about the goals of treatment. Treatment by a psychoanalyst or a psychodynamically oriented therapist “rests on the mutual agreement that the patient's stresses, frustrations and dissatisfactions are to a significant extent a function of his own ways of thinking, feeling and acting” 1, p.253 , but this understanding may not be realized until therapy has progressed for some time. On the other hand, cognitive and behavior therapists direct attention toward more concrete and circumscribed goals related to behavior, cognitions, emotions and values. Some therapies emphasize character or personality change, while others are focused on symptoms or well‐being. The goals for a patient receiving psychopharmacological treatment will be typically focused on symptoms of the disorder.
Clearly, agreement on goals is not a simple matter. The use of the terms goals and agreement on goals suggest to many a degree of specificity; alternative language could refer to general aims of treatment and clarification of aims of treatment. Moreover, as any clinician knows, what the patient identifies as problematic in his/her life may change as therapy provides insight or understanding. Further complicating the situation, patients may report that they have come to an agreement on the goals of therapy in the absence of any discussion of goals 7 , suggesting that an implicit understanding might be sufficient. Anyway, the degree to which psychotherapy is focused on the patient's perceived problems is related to the efficacy of the treatment 8 .
The second element of the alliance, as formulated by Bordin, is therapist's assignment of tasks. Bordin was clear that the choice of therapeutic tasks is not unilaterally made by the therapist and presented to the patient, and noted that “collaboration between patient and therapist involves an agreed‐upon contract” 1, p.254 . However, he recognized that the choice of therapist determined the range of tasks that would be utilized in therapy.
The particular tasks assigned by therapists will be different across orientations. For example, a patient presenting to a biologically oriented psychiatrist will not be surprised to receive a prescription for psychotropic medication, and the patient's task will involve taking the medication as prescribed. Thus, the patient has expectations about the nature of the tasks that will be assigned, which predisposes to collaboration and creates expectations for the outcomes of the therapy, thereby increasing its effectiveness, as will be discussed later9, 10, 11.
Despite the frequent citation of Bordin when discussing the alliance, the assignment of tasks element of the alliance is commonly referred to as agreement on the tasks of treatment, although it is important to remember the asymmetric relationship in mental health care, where the clinician has a particular expertise and various therapeutic skills that influence the tasks of treatment. As will be discussed, the clinician's persuasiveness and verbal fluency increase collaboration between the clinician and the patient. That is, the manner in which the clinician explains the treatment influences the degree to which the patient believes that the treatment will be effective.
The bond between the clinician and the patient is the least well defined and understood of the three elements of the alliance, and is the most controversial. According to Bordin, goal setting and collaboration on the tasks of treatment “appear intimately linked to the nature of the human relationship between therapist and patient” 1, p.254 . Calling the third therapeutic element the bond conveys the idea that it is linked to the relationship, but there are two central ways that the bond has been discussed in the literature.
First, the bond has been conceptualized as the “real relationship”, which refers to the collaborative quality of a genuine, caring, unconditional and understanding stance of the clinician, something akin to C. Rogers's “core conditions” 12 . Such a collaborative relationship quality can be healing in and of itself, as discussed later. A second interpretation of the bond is one of trust: for example, does the patient sufficiently trust that the clinician has the expertise to be helpful, so that the patient is willing to engage in the difficult and sometimes distressing work involved in the treatment? The former is oriented toward the person of the clinician, and the latter toward the competence of the clinician. Both aspects are valuable, but the distinction is important.
Moreover, the nature of the bond might well depend on the nature of the treatment, the treatment stage, and the patient's characteristics, as noted by Bordin: “Some basic level of trust surely marks all varieties of therapeutic relationships, but when attention is directed toward the more protected recesses of inner experience, deeper bonds of trust and attachment are required and developed… One bond may not necessarily be stronger than the other, but they do differ in kind” 1, p.254 .
There is a characteristic of the alliance that separates it from all, or almost all, other healing concepts. The alliance is, by definition, a dyadic concept. The alliance is created by the work that the clinician and the patient do together. Other therapeutic concepts involve conditions created or actions taken by the clinicians, although patients will be affected by or react to such conditions and actions differently. Consider empathy: a therapist can offer an empathic response to a patient after the patient describes a difficult event in his/her life, and such a response can be seen as empathic regardless of how the patient receives, understands and is affected by the response. By definition there is no “alliant‐ic” therapist response, as alliance is created in the dyadic interaction and is a phenomenon that occurs as a consequence of the therapist and patient interaction.
As such, both participants contribute to the alliance. The therapist creates the conditions under which the alliance will develop, but importantly patients perceive this as having a collaborative quality. The ontological distinction between the alliance and other therapeutic factors has been highlighted most convincingly by R. Hatcher 13 , who emphasized that the alliance is a collaborative construct. The dyadic nature of the alliance is central to understanding its role in leading to effective treatment.
Although Bordin's discussion of the alliance was ground‐breaking and his ideas have persisted, there have been theoretical variations on his conceptualization, one of which offers particularly important insights. L. Luborsky and A.O. Horvath14, 15, 16 discussed the alliance from a variety of perspectives, including its psychodynamic origins, its Rogerian client‐centered relational aspects, the social influence concept, and the pan‐theoretical perspective.
From these multiple perspectives, two types of alliance were identified as well as a sequencing of these types over the course of treatment. Luborsky suggested that the alliance is a dynamic rather than a static entity, responsive to the changing demands of different phases of therapy. Type 1 alliance is “based on the patient's experiencing the therapist as supportive and helpful with himself as a recipient”; Type 2 alliance is “a sense of working together in a joint struggle against what is impeding the patient… on shared responsibility for working out treatment goals… a sense of 'we‐ness'” 14, p.563 . According to Luborsky, Type 1 alliance is more evident in the beginning of therapy, and Type 2 more typical of later phases of treatment.
Although much of the theory and research on the alliance comes from the psychotherapy domain, the concept is applicable, as Bordin emphasized, to any practice involving a person seeking help and a socially sanctioned healer. Accordingly, we will discuss alliance with a psychotherapist and then expand the concept by discussing other domains, including psychiatry, medicine and placebos, among others.
As the alliance became to be seen as central to mental health treatments, researchers needed to have a reliable and valid way to measure it. We now discuss several of the measures of the alliance. Because the alliance is a dyadic phenomenon, respondents using these instruments are giving their own sense of the alliance. Consequently, clinicians and patients typically assess identical items, but rate the alliance as they perceive it. The clinician and the patient may not perceive the alliance similarly, as each rates the alliance filtered through his/her own lens and interpretation of the interaction. There are some instruments in which an observer rates the alliance, providing an outsider's perspective, although observers are still rating on the basis of their perspective of a dyadic construct.
MEASUREMENT OF THE ALLIANCE
Measurement of interpersonal perceptions of individuals in a social context has been a lasting challenge in psychological sciencese.g., 17, 18. For example, a person may love his/her partner but, at the same time, his/her evaluation will also consider how much it feels that this kind of love is reciprocatede.g., 19, 20. Evaluating the alliance needs to consider the relationship of two persons as well as the two persons, as individuals, with individual characteristics. According to Kenny's social relations model 21 , the evaluation focuses on three components: perceiver, target and relationship.
Alliance scores are thus based on the two actors and their general rating tendencies as well as their perceptions of the other and the relationship 16 . More specifically, alliance is assessed by particular measures completed by raters (patient, therapist, or sometimes an observer) evaluating a relational phenomenon at a particular time in therapy. The majority of studies assessing the alliance refer to overall reports at the end of a session (item examples: “I feel that my therapist appreciates me”; “As a result of these sessions I am clearer as to how I might be able to change”; “I believe the way we are working with my problem is correct”). These items do provide a more general alliance evaluation across sessions, and they are not focused on a particular intervention or time during a session. There is some empirical indication that the alliance assessed at post‐session is rated somewhat higher than the alliance immediately before the next therapy session, even though no additional interaction occurred 22 .
Four post‐session alliance measures – the California Psychotherapy Alliance Scale (CALPAS) 23 , the Helping Alliance Questionnaire (HAQ) 24 , the Vanderbilt Psychotherapy Process Scale (VPPS) 25 , and the Working Alliance Inventory (WAI) 26 – are used in approximately two‐thirds of the alliance‐outcome studies. Over time, there has been a trend toward developing and using shorter versions of these measurement instruments. About 70% of the published papers in the past decade have used an inventory based on WAI items 18 . Separate versions for patient, therapist and observer ratings have been developed. Each of the above‐mentioned four core instruments has demonstrated acceptable internal consistency, in the range of .81 to .87 (Cronbach's alpha).
Various studies of the factor structure of the measures range from multiple factors to more coordinated perceptions across the alliance elements (e.g., coordinated view of tasks, goals and bonde.g., 27 ). The shared variance of alliance across measures and evaluators is low, indicating that there is much uniqueness in the alliance ratings of particular evaluators 28 .
Despite these issues of measurement, the evidence for the importance of the alliance converges across raters, measures and assessment times, and how the alliance is involved in producing therapeutic benefits is in many ways unambiguous.
EVIDENCE FOR THE BENEFITS OF THE ALLIANCE
A search for the term “alliance” in the titles of articles indexed in the PsycINFO database yields approximately 5,000 publications that deal with the alliance in the sense used here. Consistent with Bordin's observation that the alliance spans an array of healing settings, the concept is also referenced in medicine (>900 hits in PsycINFO), social work (>800 hits), nursing (>200 hits), school counseling (>600 hits), and pharmacotherapy (>100 hits). The emphasis on the alliance is also central in the emerging patient‐centered care movement 29 .
In this section, we review the evidence for the benefits of the alliance. It will be clear that making valid conclusions from the available research is challenging, because the alliance is complex and designing research to investigate it is difficult. There are threats to validity to each alliance study as well as to all studies using a particular design. To rule out various threats, the design of the studies has evolved. The evidence produced by the studies also reveals important aspects of the alliance, showing that research and theory development go hand‐in‐hand.
Due to the volume of the alliance research, various meta‐analyses have been conducted, the results of which will be cited to summarize the evidence. For various critical issues, particular studies will be discussed.
The association between the alliance and outcomes of treatment
At the most basic level, if the alliance is an important aspect of mental health care, then the alliance measured during the course of therapy should predict the final outcomes of treatment. Said another way, the stronger the alliance, the better the outcomes of treatment.
The first study that investigated the association of the alliance with outcomes was a doctoral dissertation by A.O. Horvath in 1981 30 , who studied 29 patients receiving various types of treatment. The alliance was measured by the WAI (rated by both patient and therapist) early in therapy, and outcomes were measured by the Psychotherapy Questionnaire (also rated by both patient and therapist). Across the various measures, the alliance‐outcome correlation was .49, suggesting a rather strong association.
By 1991, there was a sufficient number of studies (i.e., 24) to conduct a meta‐analysis of the alliance‐outcome association. The typical study measured the alliance early in treatment (at the third or fourth session) and then the correlation of the alliance score with outcomes as a criterion variable was calculated. The results of this meta‐analysis 31 are presented in Table 1. The 24 studies involved 1,148 patients and yielded an aggregate correlation of .26, which is generally considered of moderate size. When converted to standardized mean difference (SMD), the effect was .54, which would be regarded as sizable and clinically important. This effect size indicates that seven percent of the variability in outcomes (i.e., R 2 ) is due to the alliance. Although this may not appear impressively large, there is no variable measured early in therapy, except for initial severity of the patient's condition, that predicts the outcomes better than the alliance.
Table 1.
Summary of meta‐analyses of the correlation of alliance and outcome
| Population | N. studies | N. patients | Aggregate correlation (r) | Equivalent SMD | R2 | |
|---|---|---|---|---|---|---|
| Horvath & Symonds 31 | Adults | 24 | 1,148 | .26 | .54 | .07 |
| Martin et al 32 | Adults | 79 | 4,770 | .22 | .45 | .05 |
| Horvath & Bedi 33 | Adults | 100 | 5,741 | .21 | .43 | .04 |
| Horvath et al 34 | Adults | 190 | 17,422 | .28 | .58 | .08 |
| Flückiger et al 35 | Adults | 295 | >30,000 | .28 | .58 | .08 |
| Karver et al 36 | Children and adolescents | 43 | 3,447 | .20 | .40 | .04 |
| Friedlander et al 37 | Couples and families | 40 | 4,113 | .30 | .62 | .08 |
SMD – standardized mean difference
The number of studies examining the correlation between the alliance and outcomes has remarkably increased over the years. Four additional meta‐analyses have been conducted since 199132, 33, 34, 35, whose results are summarized in Table 1. Clearly, the range of the aggregate correlation of alliance with outcomes exceeds .20, and in the most recent and comprehensive meta‐analysis approaches .30. Due to the number of studies (almost 300) and number of patients (over 30,000) within the studies in the most recent meta‐analysis 35 , it is safe to conclude that there is a robust association between alliance and outcomes of psychotherapy. Indeed, the standard error of estimate for the aggregate correlation of .28 was approximately .011.
Importantly, the association of the alliance between the therapist and youth is also predictive of outcomes 36 . Furthermore, the alliance is associated with outcomes also in marital, family and group therapy, although in these cases there are multiple alliances to consider37, 38.
The adage that “correlation does not mean causation” provides a cautionary note to making claims about the alliance from these meta‐analyses, even if they are comprehensive and precise. However, research has burgeoned to address many of the threats to the validity of the conclusion that the alliance is a central therapeutic factor, and also provides clinical insight into how the alliance is therapeutic. We now briefly review this additional evidence.
Is the alliance an epiphenomenon of early symptom change?
The correlation between the alliance and outcomes discussed earlier involves a measurement of the alliance early in therapy, typically at the third or fourth session. The alliance, it is thought, cannot be validly assessed earlier, because it is a dyadic construct that needs sufficient clinician‐patient interaction to develop. However, by the time the alliance is measured, many patients will have experienced a significant decrease in distress39, 40, which has generated two conjectures about early treatment gains.
The first conjecture, put forth by DeRubeis et al 41 among others, is that the specific treatment actions create early change, and it may well be that the patients who have experienced significant benefits early in treatment will tend to rate all aspects of the treatment favorably, including the alliance, and will have better final outcomes. In this case, it could be said that the alliance is a consequence of the benefits of treatment. This epiphenomenon argument has been proposed as an explanation for the alliance‐outcome correlation and to suggest that the alliance may not be an important therapeutic factor 41 .
The second conjecture is that early treatment progress is due to remoralization, a tenet of the psychotherapy model proposed by J. Frank 10 . Remoralization is related to the patient taking action to solve his/her problems (i.e., partake in psychotherapy) as well as to the expectation that the treatment will be effective (which is intimately tied to the agreement about the goals of treatment and the acceptance of the therapeutic tasks, and to the unconditional acceptance by a clinician who shows understanding and caring). In the former epiphenomenon case, it is the specific treatment action itself that results in symptom change 42 as well as a strong alliance, whereas in the latter it is the engagement in the therapeutic process and feeling accepted by the clinician that is important 43 .
The evidence for these two conjectures partially clarifies their relative validity 44 . The first issue, which has been examined quite extensively, is whether the alliance is predictive of the outcome of therapy beyond the early progress of treatment observed before the alliance was measured. Indeed, there are other processes occurring in therapy prior to alliance measurement that might generate higher alliance ratings and better treatment outcomes, such as adherence to the treatment protocol and therapist competence at delivering the treatment. Moreover, there are several characteristics of patients that might present confounds, such as patient personality, demographics, and context (racial, ethnic or cultural variables), as well as the initial severity of the patient's condition.
Over the years, there have been several attempts to statistically control for patient characteristics and early processes. Recently, a meta‐analysis examined studies that partialled out factors occurring before measurement of the alliance and found that the alliance‐outcome correlation was not attenuated by these factors 45 . Thus, there is evidence that the alliance is not simply an epiphenomenon of factors occurring before it is measured. However, early symptom change also predicts the final outcomes of therapy 46 and mediates change47, 48, a result which beseeches further investigation of how symptom change and alliance are related over the course of treatment.
An advance in statistical methods has clarified to some extent the alliance‐symptom association. The evidence discussed up to now is known as a between‐patient effect. The alliance‐outcome correlation is a bivariate statistic indicating that, with patients for whom the rated alliance is larger than for other patients, the outcome is better than for other patients. Such statistics say nothing about the temporal aspects of the alliance. An important question is whether the level of the alliance for a particular patient at a particular session is followed subsequently by a reduction in symptoms for that patient. Conversely, is a reduction of symptoms followed by an increase in the rated alliance? Such questions are answered by a within‐patient analysis 49 . This analysis requires that the two variables are assessed at regular intervals over the course of therapy (i.e., a longitudinal design) 49 .
Increasingly, researchers have examined alliance and symptoms over the course of psychotherapy, providing a sufficient number of longitudinal studies to be meta‐analytically synthesized 50 . The meta‐analysis examined 17 primary studies of the alliance and symptoms over the course of the first phase of treatment, which was designated as the first seven sessions. A between‐ and within‐patient analysis was conducted with the data from each primary study, and the results from the 17 studies were then aggregated, yielding several informative findings.
First, early alliance was related to the level of symptoms at post‐treatment, consistent with the meta‐analyses reviewed earlier. Second, at the within‐patient level, the relative level of the alliance for a patient predicted the subsequent level of symptoms, but as well the relative level of symptoms for a patient predicted subsequent level of the alliance. That is, there is a reciprocal relationship between alliance and symptoms as treatment unfolds during the initial phase. The reciprocal relationship between alliance and symptoms was stronger for patients with stronger alliance relative to other patients, whereas it was stronger for patients with lower symptom level than for other patients. The results of this meta‐analysis demonstrate that the alliance is not simply a consequence of symptom improvement, but suggest that symptom improvement and alliance work synergistically.
Whose contribution (therapist or patient?) to the alliance mostly leads to change?
The alliance is a dyadic construct that reflects the interaction between a therapist and a patient. However, each of the participants brings to the therapy situation different capacities to form an alliance51, 52. Patients have, for example, varying attachment histories, attachment styles, motivation, and needs for affiliation – all these factors may affect the strength of the alliance. Similarly, therapists will differ in their ability to form alliances with patients51, 53. The correlation of the alliance with outcomes is what is called a total correlation 51 , in that it ignores that the phenomenon under investigation is due to two sources. When the total correlation is disaggregated, there are two possibilities.
First, it might be the patient contribution to the alliance that is more important for the outcomes of therapy. For example, a patient may have a secure attachment style, lack of stress in life (e.g., adequate economic resources and social support), no comorbid personality disorder, and be motivated to reduce his/her distress. This patient would likely form a good alliance with the therapist and would likely have relatively satisfactory outcomes. If this were the case over a sample of such patients, there would be a positive correlation of alliance with outcomes, and this correlation would be due primarily to the patient's capacity to form an alliance.
On the other hand, if some therapists are able to form better alliances than others, then it could well be that therapists who are able to form strong alliances across a range of patients also produce better outcomes. In this case, there would be a strong total correlation, but this would be mostly due to the therapist contribution to the alliance. Of course, the total correlation could be due to both the therapist and the patient contribution.
Disaggregating the total correlation into therapist and patient contributions is possible with multilevel modeling, that takes into consideration that the patients (level 1) are nested within therapists (level 2). For example, Baldwin et al 51 disaggregated the total alliance‐outcome correlation, which allowed identification of whose contribution to the alliance was mostly associated with outcomes. They examined the outcomes of 331 patients who were treated by 80 therapists. The outcomes of therapy were measured by the Outcome Questionnaire 45 (OQ‐45) at baseline and termination, and alliance was measured by the WAI early in therapy from the patients' perspective.
The total correlation of WAI and post‐treatment OQ‐45 was –.24 (negative because lower OQ scores indicate better outcomes). When the baseline OQ‐45 score was included in the model as a covariate, the total correlation was –.21. These total correlations were approximately equal to the values estimated in various meta‐analyses35, 45. Using multilevel models that disaggregated the patient and therapist contribution to the alliance, it was found that the therapist contribution to the alliance predicted outcomes (y02 = –0.33, p<0.01), but the patient contribution did not (y20 = –0.08, not significant).
The differential effectiveness of therapists has been labeled therapist effects 54 . A therapist who generally forms stronger alliances with his/her patients than other therapists also generally has better outcomes than other therapists. However, an apparently surprising result of Baldwin et al's study 51 was that patients with a stronger alliance with that particular therapist did not have better outcomes than the same therapist's other patients with a lower alliance.
To understand this result, consider a chronically depressed patient with a comorbid Cluster B personality disorder, who has a difficult attachment history, an insecure attachment style, and little social support. This patient's alliance with a therapist who generally forms strong alliances will likely be weak relative to the other patients of that therapist. However, this alliance will likely be stronger than it would have been had this patient been treated by another therapist. This patient is accustomed to having a chaotic relationship with everyone in his/her world and here is a therapist who is able to form with him/her a relatively stable relationship, albeit less strong than with other patients. This stronger alliance than usual for this patient will generate positive outcomes.
There have been several investigations that have disaggregated the patient and therapist contributions to the alliance, some of which have replicated Baldwin et al's findings and some others have not 54 . However, two meta‐analyses have examined the corpus of alliance‐outcome correlation by utilizing an innovative method. Del Re et al55, 56 examined several potential moderators of the alliance‐outcome correlation, and found that a significant moderator was the patient‐to‐therapist ratio (i.e., the number of patients in each study divided by the number of therapists). It was found that the lower that ratio, the higher the alliance‐outcome correlation. This result, which remained significant even when several potential covariates were controlled, confirms the significance of therapists' impact on the alliance‐outcome relationship.
That the benefits of the alliance are mostly due to the therapist contribution raises the fundamental question of what are the characteristics and actions of therapists who form strong alliances across a range of patients. Psychotherapy research has shown that the age, ethnicity, gender, profession of therapist, therapist's theoretical orientation, therapist's experience, size of therapist's caseload, self‐reported social skills on a valid inventory, and expert interviewer's rating of trainees' clinical skills, do not differentiate more effective from less effective therapists 54 . The strongest predictor of effectiveness is a set of interpersonal skills of the therapists displayed in interpersonally challenging situations57, 58.
In Anderson et al's study 57 , the facilitative interpersonal skills of the therapist were the only factor accounting for variability of therapy outcomes. These skills included verbal fluency; therapist communication of hope and positive expectations; persuasiveness; emotional expression; warmth, acceptance and understanding; empathy; alliance bond capacity; and alliance rupture‐repair responsiveness. Anderson et al59, 60 as well as others 58 assessed the interpersonal skills of psychotherapy trainees and were able to use these skills to predict therapy outcomes two to five years in the future.
Does the alliance differ among various forms of psychotherapy?
According to Bordin 1 , the alliance is important for all healing practices involving a person seeking help and a clinician offering help, although he recognized that the nature of the alliance might be different among the various therapies. Plumbing the depths of the psyche in psychoanalysis might well require a different type of alliance than exposure for a socially anxious patient in cognitive‐behavior therapy (CBT), although both tasks can be extremely demanding emotionally.
The most basic question is whether the alliance predicts outcomes across various types of therapy. In their meta‐analysis, Flückiger et al 35 examined the size of the correlation for different treatments, including CBT, counseling, psychodynamic therapy, humanistic therapy, interpersonal therapy, and unspecified and eclectic therapies. They found no statistically significant differences in the size of the correlation among the various treatments, which indicates that the magnitude of the impact of alliance is high for all psychotherapies. This result is in line with Bordin's suggestion that alliance is vital for change in all psychotherapies, and indeed in all healing practices. However, it is important to examine Bordin's conjecture that the nature of the alliance may be different among various treatments.
There are several investigations that shed light on the nature of the alliance in different treatments. Webb et al 61 examined data from two randomized trials of cognitive therapy (CT) for depression, with WAI measured early and later in therapy. Early in therapy, only the agreement on tasks and goals of therapy predicted depression symptom change, whereas the bond factor did not. Later in therapy, the bond factor, as well as the agreement on goals and tasks, predicted symptom change. These results suggest that in CBT the goals and tasks dimensions of the alliance are more important than the bond dimension in the critical early phase of therapy.
Hagen et al 62 disaggregated the therapist and patient contributions to the alliance in exposure and response prevention treatment for obsessive‐compulsive disorder. They found that the therapist contribution to the goals and tasks dimensions predicted outcomes, but the therapist contribution to the bond dimension did not. This result suggests again that the bond dimension is not as important in CBT, but it also corroborates the notion that the therapist contribution to the alliance (here only to the goals and tasks aspects) is what is important to the outcomes of the treatment.
The impact of the bond dimension on the outcome of psychodynamic psychotherapy and of CT for patients with Cluster C personality disorders was investigated by Ulvenes et al 63 . They found that, in psychodynamic psychotherapy, therapist's avoidance of affect negatively influenced symptom reduction and suppressed the relation of bond to that reduction. In contrast, in CT, therapist's avoidance of affect was positively related to both the formation of the bond and to symptom reduction. Thus, the impact of the bond dimension is different in the various forms of psychotherapy, and this dimension interacts with therapeutic actions.
Clearly, the alliance is important across therapies, but exactly how it works in various treatments is complex and needs further investigation.
How are characteristics of the patients related to the alliance‐outcome correlation?
Are there patient variables that affect the size of the alliance‐outcome correlation? There is reason to expect that the patient's diagnosis might be relevant in this regard. For example, the alliance, which depends on agreement on the goals and tasks of therapy, may not be strong for a patient who is ambivalent about change 64 , such as in substance use disorders and eating disorders65, 66. Furthermore, a patient with attachment difficulties may have problems to form an alliance; therefore, treatment may not progress adequately, unless the relationship with an empathic therapist provides an attachment corrective experience 52 resulting in therapeutic benefits.
Flückiger et al 35 examined the size of the alliance‐outcome correlation across various diagnoses and reported several informative findings. For eating disorders, the alliance‐outcome correlation was smaller than it was generally (r=.15 vs. r=.28 in general). Some experts in the field have gone so far as to affirm that the alliance is relatively unimportant in the treatment of patients with eating disorders 67 . However, a meta‐analysis 68 suggested that the alliance has a stronger relationship to outcomes in younger (vs. older) patients, over and above the variance shared with early symptom improvement, and that early alliance shows a greater association with outcomes in non‐behavioral therapies than in those with a strong behavioral component. Clearly, the role of the alliance in the treatment of eating disorders is complex and not well understood.
A second diagnosis where the alliance‐outcome is attenuated relative to other diagnoses is substance use disorders (r=.14). Similar to those with eating disorders, patients with substance use disorders may have difficulties to agree on the goals and tasks of therapy. However, there is evidence that adding motivational interviewing to CBT in the presence of ambivalence and resistance to treatment69, 70 can improve the alliance and the outcomes in these patients 71 .
Many of the outcome‐alliance correlation studies of substance use disorders have been conducted in the US, and the samples contained a high proportion of patients from racial/ethnic minority groups, particularly African Americans. There is evidence that cultural micro‐aggressions perceived by the patient during therapy are negatively associated with psychological well‐being, and that the alliance mediates this relationship 72 . Here, the alliance may well be the consequence of a therapy process (e.g., perceived cultural micro‐aggressions), which leads to a further discussion of the mechanisms involved in the alliance as well as of the therapist actions that may lead to stronger alliances.
A third diagnosis that is theoretically and clinically interesting is personality disorder. In Flückiger et al's meta‐analysis 35 , the alliance‐outcome correlation for borderline personality disorder (r=.32) and other personality disorders (r=.32) was larger than the average correlation across various diagnoses (r=.28), but the differences were not statistically significant. A large variability was observed: the alliance‐outcome correlation for borderline personality disorder in the nine relevant studies ranged from r=.00 to r=.78. This variability suggests that the alliance in personality disorder is particularly complex.
It would be informative to examine other characteristics of patients that moderate aspects of the alliance‐outcome association. As an example, Zimmermann et al 73 found that the bond feature of the alliance was not predictive of outcomes among patients with sufficient social support, whereas it was a strong predictor in patients with little social support. Further research is clearly warranted in this area.
Are there methodological aspects that affect the size of the alliance‐outcome correlation?
There are a number of methodological threats to the validity of the alliance‐outcome association. It may well be that the rater of the alliance makes a difference in the size of the correlation. Typically, in the alliance‐outcome studies, the outcome measures are rated by the patient, so it might be that, if the patient also rates the alliance, the correlation might be larger because of method variance. However, Flückiger et al's meta‐analysis 35 did not find significant differences based on who made the rating, although there was a trend, when observers rated the alliance, for the correlation to be slightly lower. Similarly, there were no differences in the alliance‐outcome correlation due to who rated the outcomes. So, it seems that method variance is not a major threat to the validity of the association between the alliance and outcomes.
We have reported that the alliance measured early in treatment predicts outcomes, which is the typical study method. However, there are studies that measure the alliance mid‐treatment or near the end of treatment (e.g., the last three sessions). The correlations for early, mid and late assessment were r=.22, .21 and .30, respectively. It is not surprising that the alliance measured late in therapy is a stronger predictor of outcomes, as variables measured proximally tend to have a larger effect than variables measured distally, regardless of what psychological variables are being assessed. What is important to reiterate here is that the alliance measured early in treatment is predictive of outcomes.
Previously we discussed several alliance measures. Although all of them have demonstrated adequate reliability and validity, it is informative to determine whether the various measures produce different magnitudes of alliance‐outcome correlation. Flückiger et al's meta‐analysis 35 found no differences in the alliance‐outcome correlation among the various alliance assessment instruments. In terms of outcomes, there was a slightly larger alliance‐outcome correlation for broader outcome measures, such as quality of life, than for disorder‐specific symptom measures. Furthermore, there was no difference in the size of the alliance‐outcome correlation depending on whether the data were derived from randomized trials or from naturalistic settings.
It appears that the alliance is a robust predictor of treatment outcomes, regardless of many factors that might have mitigated the size of the correlation. The alliance is associated with outcomes controlling for early symptom change; the level of the alliance at each session predicts subsequent level of symptoms in longitudinal analyses; and the therapist contribution to the alliance predicts outcomes. On the basis of this evidence, it can be argued that the alliance is clearly an important therapeutic factor. Nevertheless, there is a perspicuous limitation to the evidence cited: this evidence heretofore is correlational. It is true that major threats to the causal validity of the alliance have been addressed and adequately ruled out, yet experimental evidence would be needed to bolster a causal relationship between the alliance and outcomes. In psychotherapy, it is unethical to randomly assign patients to levels of the alliance as well as pragmatically difficult to design therapies with different levels of the alliance. However, in medicine and particularly in placebo studies, experimental designs have been used to examine various aspects of the relationship between the clinician and the patient. That evidence will now be reviewed.
ALLIANCE IN MEDICINE AND PLACEBO STUDIES
Up to now our focus has been on the alliance in psychotherapy, but, as Bordin 1 discussed, the alliance is germane to all healing practices that involve a clinician and a patient. The nature of the alliance depends on the particular healing practice. Moreover, various healing practices use the term alliance without much thought about the classical definition of the concept.
Our review of research in medicine and placebo studies will demonstrate the importance of the alliance and its generalizability to practices other than psychotherapy. We begin with a general discussion of healing, as this discussion will clarify the role of the alliance in non‐psychotherapy contexts.
Natural, specific and contextual effects
When exposed to disease or trauma, human healing is composed of three effects: natural, specific and contextual 74, 75.
Biological mechanisms have evolved to protect humans from disease and enable the organism to heal (e.g., blood coagulation, immune functions, barriers such as the skin). Healing that occurs as a result of these defenses is called natural healing 75 . Natural effects refer to the change in the patient's status due to the natural course of disease as impacted by these defenses.
Specific effects are those due to the particular treatment administered to a patient with a given diagnosis. The medicine or procedure addresses a particular biological deficit or process, resulting in patient cure or improvement. A patient with a gastric ulcer will respond to a course of antibiotics and proton pump inhibitors. Cataract surgery will restore vision, which would have progressively failed without intervention (i.e., natural healing is insufficient in this case). Specific effects compose what is generally referred to as modern or Western medicine.
The final component of healing involves contextual effects. These effects are due to a number of psychosocial factors, including patient expectations, symbolic meaning of a healing setting (e.g., a physician's white coat, syringes, diplomas on the wall), the relationship between the healer and the patient, and conditioned responses to various medications or procedures74, 76, 77. These psychosocial factors are closely related to the factors that have been identified as generating the placebo response75, 78, 79, 80. However, contextual effects in medicine are not placebo effects, because no placebo has been administered. They have been called placebo‐like effects 81 .
There are two critical points to make here. First, the contextual effects are, to varying degrees, present in all healing practices, including medicine, psychiatry and psychotherapy, contributing to healing experienced by the patient. Second, the alliance is the backbone of the contextual factors – the various contextual factors are, in one way or another, wired to the alliance as conceptualized by Bordin 1 .
We now review the literature in medicine that establishes the importance of the relationship for healing. The term alliance is rarely used in this literature and, when it is, it is often misused. Nevertheless, this literature confirms experimentally the importance of the alliance and adds to our understanding of it. We will use the generic term relationship and make reference to the alliance for particular studies.
Alliance in somatic medicine
There is a limited number of experimental studies in medicine that have examined variables related to the relationship. This is due to two factors: first, there is little interest in medicine in establishing the importance of the relationship for producing health outcomes; second, it is difficult to manipulate relationship in medical settings.
In the studies that do examine the relationship in medical settings, this is often discussed as consisting of two components: an emotional and a cognitive one76, 82. The emotional component corresponds to the “real relationship” conceptualization of the bond, comprising warmth, empathy and genuineness. The cognitive component is usually described as “information gathering, sharing medical information, patient education, and expectation management” 82, p.1 , and is conceptualized as effective communication about the disorder and the treatment.
There is an unstated assumption that an effective communication will lead to belief in the treatment and to belief that the clinician has the technical expertise to produce positive outcomes, which are similar to aspects of the alliance, particularly the emphasis on agreement on goals and on the component of bond oriented toward the competence of the clinician.
Di Blasi et al 76 found 25 randomized controlled trials (RCTs) exploring the effects of contextual factors, although most of them examined the extent to which the clinicians provided information about the treatment. Clinicians who attempted to influence patient's beliefs about the treatment achieved better outcomes. No studies examined the effects of emotional care only, but four trials evaluated the combination of providing information and emotional care. The results of these studies suggested that providing information in a warm and accepting way produced better health outcomes than a neutral situation. The authors concluded: “Practitioners who attempted to form a warm and friendly relationship with their patients, and reassured them that they would soon be better, were found to be more effective than practitioners who kept their consultations impersonal, formal, or uncertain” 76, p.760 .
Kelley et al 82 meta‐analyzed medical studies that manipulated the clinician‐patient relationship and used validated or objective health outcomes. The results indicated that better relationship conditions produced better health outcomes than poorer relationship, although the effect was small (SMD=0.11). The authors concluded: “This systematic review and meta‐analysis of RCTs suggests that the patient‐clinician relationship has a small, but statistically significant effect on healthcare outcomes…. relatively few RCTs met our eligibility criteria, and… the majority of these trials were not specifically designed to test the effect of the patient‐clinician relationship on healthcare outcomes” 82, p.1 .
Thus, the experimental evidence for a relationship effect in medicine is sparse and the quality of evidence available is relatively poor. On the other hand, there are several well‐conducted and informative experimental studies of relationship variables using placebos.
Placebos
Placebos are substances or procedures without ingredients that should, from a biological perspective, affect the health status of an individual 83 . They are designed to resemble the verum (i.e., the treatment under investigation) in every way except the presence of the therapeutic ingredients. They may consist of sham pills, inoculations, creams or surgery.
Placebos have demonstrated effects on subjective outcomes (e.g., pain ratings) as well as creating physiological changes for a variety of conditions, including pain (acute, chronic as well as experimentally induced), Parkinson's disease, menopausal symptoms, irritable bowel syndrome, headaches, osteoarthritis, respiratory illnesses, and mental disorders (primarily anxiety and depression)78, 79, 80.
The effects of placebos “depend on a person's psychological and brain responses to the treatment context, which influence appraisals of future well‐being”78, p.73 (emphasis added). The treatment context includes the relationship between the patient and the clinician, the information about the intervention that is communicated to the patient, the physical healing space, the healing rituals, and cultural beliefs about healing and healers. These psychosocial factors create in the patient the experience of being cared for and understood by the clinician, and the expectation that the treatment delivered by that particular clinician will be effective. Placebo effects can be induced without a face‐to‐face interaction, say by written materials, or by prior conditioning77, 84, 85, 86, 87. The placebo studies we will review first are those in which aspects of the relationship were experimentally manipulated.
Kaptchuk et al 88 explored if augmenting the therapeutic relationship would increase the placebo response for the treatment of irritable bowel syndrome. The placebo was sham acupuncture (the needles did not pierce the skin although they provided the sensation of doing so). The first arm was usual treatment by the physician, but no sham acupuncture. In the second arm, the patient received sham acupuncture twice a week for three weeks, with the acupuncturist who explained the acupuncture procedure but did not exhibit warmth or caring (called a limited interaction). In the third condition, called the augmented interaction, the same procedure was implemented, but with a 45 min interaction prior to the first sham acupuncture session, including questions about the patient's symptoms, curiosity about the effects of irritable bowel syndrome on functioning, and inquiries about how the patient understood the cause and meaning of the syndrome. In this condition, the acupuncturist did not provide any advice, treatment or coping strategies.
The results of the study showed that the limited interaction procedure was superior to treatment‐as‐usual with regard to reduction of symptom severity, relief from distress, global improvement, and quality of life, but the augmented interaction provided additional benefit on all outcomes. According to the authors, “the magnitude of non‐specific effects in the augmented arm is not only statistically significant but also clearly clinically significant in the management of irritable bowel syndrome” 88, p.6 , supporting the notion that the relationship effect on healing is clinically important. In this study, the actions in the augmented interaction condition resemble those associated with the bond, although there were some actions that might be associated with agreement on goals (e.g., talking about the symptoms that were distressing).
Notably, a follow‐up analysis 89 showed that there were differences between acupuncturists in patient improvements. Indeed, after controlling for treatment condition (augmented vs. limited) and patient characteristics, acupuncturists accounted for an additional 6.9% of the variance in outcomes. In contrast, after controlling for acupuncturist and patient characteristics, treatment condition accounted for 3.0% of outcome variance. So, the effect attributable to different acupuncturists was more than twice as large as the effect attributable to treatment condition (augmented vs. limited), supporting the psychotherapy evidence about the role of the interpersonal skills of the therapist in shaping the alliance‐outcome correlation.
In a study of pain intensity and pain sensitivity of patients with chronic back pain, Fuentes et al 90 explored how the “alliance” augmented the effect of both placebo and verum. Patients received either active interferential current therapy (IFC, the verum) or sham IFC in conjunction with either a limited relationship or an enhanced relationship, which the authors labelled as “alliance”. In the limited relationship condition, the practitioners introduced themselves and explained the purpose of the treatment, whereas in the other condition “the therapeutic interaction was enhanced through verbal behaviors, including active listening (i.e., repeating the patient's words, asking for clarifications), tone of voice, nonverbal behaviors (i.e., eye contact, physical touch), and empathy” 90, p.480 . Again, the clinician actions were oriented toward the “real relationship” conceptualization of the bond. The clinicians left the room during the procedure in the limited relationship condition, but they remained in the enhanced condition. For both the verum and the placebo, the augmented relationship condition produced superior outcomes relative to the limited relationship condition. The authors concluded: “The context in which physical therapy interventions are offered has the potential to dramatically improve therapeutic effects” 90, p.477 .
As mentioned previously, there is a conjecture that the therapeutic relationship in medicine is composed of two components, emotional and cognitive76, 82, 91. Howe et al 92 examined physician warmth and perceived competence, two characteristics that map onto the emotional and cognitive components of the relationship. In their study, the participants were given a physical examination, which was explained to the participants as a screen for a subsequent purported medical study. The examination included measurement of vital signs, respiration, as well as a skin prick “allergy test”. In actuality, the skin was pricked with histamine, which caused a reaction in all participants. The participants were informed that this outcome disqualified them from the subsequent study, and they were administered a cream, which they were told would attenuate the skin irritation. The cream was a placebo (i.e., contained no antihistamine). These procedures were executed in four conditions: warmth (high vs. low) crossed with competence (high vs. low). High warmth involved an inviting office furnishing (e.g., posters with calming images) and physician use of the participant's name and warm nonverbal behavior (eye contact, proximal seating, and smiling facial features), whereas the low warmth condition did not include these features. In the high competence condition, the physician was verbally fluent (e.g., gave a confident and cogent explanation of various procedures), the tests were administered efficiently without mistakes, and the examination room was well organized, whereas the low competence lacked these features. The diameter of the wheal (circle of irritated tissues) on the skin and the rate of change in diameter were the outcome measures. The wheal diameter decreased most rapidly and the final wheal diameter was smallest in the high warmth/high competence condition, whereas the wheal diameter decreased most slowly and the final wheal diameter was largest in the low warmth/low competence condition. The results of the mismatched conditions (low competence/high warmth and high competence/low warmth) were intermediate between the low/low and high/high conditions, indicating that warmth and competence both contributed to the response to placebo. In this study, the warmth and perceived competence of the clinician affected the physiological response to the administered histamine, experimentally establishing relationship effects.
Czerniak et al 93 manipulated the relationship between healer and recipient in relation to pain tolerance. An actor portraying a physician administered placebo cream to healthy volunteers who participated in a cold‐pressor test. In one condition, the “physician” portrayed a traditional doctor‐patient relationship and in the other the “physician” role emphasized “attentiveness and strong suggestion, elements… present in ritual healing” 93, p.1 . Pain tolerance was assessed before and after placebo administration. In the enhanced relationship condition, participants showed greater change in pain tolerance after administration. The authors concluded that a “structured manipulation of physician's verbal and non‐verbal performance, designed to build rapport and increase faith in treatment, is feasible and may have a significant beneficial effect on the size of the response to placebo analgesia” 93, p.2 .
Implications of medical and placebo research for understanding the alliance
The design of the above experimental studies establishes the importance of the relationship in healing. Whereas the previously reviewed alliance‐outcome studies were correlational, the placebo studies (and some medical studies) have experimentally manipulated the relationship. Furthermore, placebos are inert and therefore an interaction of the relationship with specific effects is ruled out. Moreover, some of these studies establish that the relationship between healer and patient does not simply have an effect on the patient's subjective experience, as an effect on physiology was also demonstrated (e.g., the size of the wheal created by histamine).
A second consideration is how the relationship in these studies maps onto the alliance. As mentioned, in the medical context, two aspects of the relationship have been emphasized: a) warmth, caring, trust and understanding (emotional component), and b) competence and conveyance of information (cognitive component). These two dimensions need further clarification. Clearly, the first aspect maps well onto the “real relationship”, which to many is the essence of the bond feature of the alliance. This aspect has obviously an emotional dimension. The second aspect is not simply conveying information in a clear and cogent manner. The relationship enhances the persuasive salience of the information, thereby influencing the patient to believe that the treatment will effectively remediate distress and restore health94, 95, 96. In this way, the patient comes to believe that goals can be accomplished through adherence to the recommended actions. Thus, this second aspect of the medical interaction maps onto agreement on goals as well as assignment of tasks of treatment.
Howe et al 91 authored an article on the above two dimensions of the relationship with the memorable title When Your Doctor “Gets it” and “Gets You”: The Critical Role of Competence and Warmth in the Patient‐Provider Interaction. Actually, the two factors converge with various theoretical and empirical claims, starting from J. Frank's classic discussion of psychotherapy as an example of the universe of healing practices10, 97, 98, 99. The belief in the healing myth and ritual, central to Frank's exposition, is essentially the belief that the clinician understands the nature of the problem, will administer a treatment that will be remedial to the problem, and has the competence to administer the treatment. On the other hand, Frank also discussed the importance of the patient's belief that the clinician understands, cares for, and will make extraordinary efforts to assist him/her (i.e., the bond that is created).
Over the years, there have been many relationship concepts discussed in the literature. Recently, Norcross and Lambert 100 published an anthology of meta‐analyses on relationship factors in psychotherapy, including the alliance itself (as measured by the instruments discussed earlier), collaboration, goal consensus, empathy, positive regard and affirmation, congruence/genuineness, cultivating positive expectations, real relationship, and treatment credibility, all of which were associated with better outcomes. Clearly, these constructs are not independent, which raises the question about what latent factors underlie the various relationship constructs.
Finsrud et al 101 conducted a study to identify the latent factors of various relationship constructs. In this study, a large sample (N=332) of patients undergoing intensive psychotherapy for a variety of disorders completed at each session a compressive measure of the relationship, with items assessing agreement on goals, agreement on tasks, expectations, treatment credibility, therapist empathy, and perceptions of therapist expertise. The results yielded two factors, which were invariant over the course of treatment and were validated across subsamples. These two factors were described as “confidence in the therapist” and “confidence in the treatment”, which mirror the two factors discussed by Howe et al 91 and are consistent with the theoretical positions of Bordin 1 , Frank10, 97, 98, 99, Horvath and Luborsky 14 , and Wampold44, 102.
It appears that the alliance is not distinct from other relationship concepts that have been discussed and investigated. As well, the various relationship constructs, including the alliance, might best be considered as being composed of two factors: being cared for and understood by the clinicians (corresponding to Bordin's bond), and belief in the competence of the therapist to select and administer an effective treatment (corresponding to Bordin's agreement on goals and therapist's assignment of tasks).
We have previously reported the evidence suggesting that in psychotherapy the benefits of the alliance are mostly due to the therapist contribution, in particular the facilitative interpersonal skills of the therapist 57 . This has been confirmed in healing contexts other than psychotherapy. In the context of a double‐blind RCT103, 104, psychiatrists administered either an antidepressant or placebo “plus minimal supportive therapy”, which involved a warm, empathic and caring atmosphere, but no advice or coping strategies. The antidepressant was found to be superior to placebo, accounting for about 3% of the variability in outcomes 104 . However, differences in outcomes due to psychiatrists themselves accounted for about 9% of that variability 105 . The more effective psychiatrists delivering placebo had better outcomes than the less effective psychiatrists delivering antidepressant medication. Because this was a double‐blind RCT, the difference among the psychiatrists was likely due to what took place in the clinical management, supporting the role of clinicians' interpersonal skills.
Alliance in other contexts and beyond the therapist‐patient dyad
There is evidence to support the idea that face‐to‐face interaction is not needed to develop a collaborative relationship. For example, various Internet‐based therapies have been developed, most of which are variations of CBT (IBCT) 106 . These therapies involve the following components. First, the patient is screened to ensure that his/her problem is consistent with the goals and tasks of the treatment. Second, the therapist, through asynchronous text messages, orients the patient to the program, describing the sequence of modules to be completed. The modules mirror the components of the CBT for the particular disorder. Third, after each module is completed, the patient answers an essay question, and the therapist provides a brief personalized comment on patient progress (although there are efforts to use artificial intelligence to provide this feedback). Meta‐analytic evidence indicates that IBCT is as effective as face‐to‐face CBT for various psychiatric and somatic conditions 106 .
In these Internet‐based therapies, the assessed alliance between the patient and the clinician/program, despite the distal and short interaction, is reported to be correlated with outcomes. For example, Zalaznik et al 107 , examining the alliance with the program and with the therapist in ICBT for panic disorder, found that patient‐rated alliance with the program predicted treatment outcomes, whereas alliance with the therapist predicted adherence to treatment. There have been two meta‐analyses of the association of the alliance and outcomes in electronically mediated treatments, and both detected an effect comparable to face‐to‐face psychotherapy35, 108.
The findings with Internet‐based therapies suggest that the concept of alliance extends beyond the individual clinician and applies to a program or treatment and the context in which it is implemented. A patient's belief that the treatment will be effective for the disease or distress he/she is experiencing (agreement about goals and tasks of treatment) seems to be forged by multiple factors other than the clinician.
This system perspective is supported by other mental health care findings. Wampold and Brown 109 studied the variability of outcomes due to psychotherapists in a naturalistic study in managed care. Consistent with the previously reported therapist effects studies, about 5% of the variability in the outcomes was due to the therapists: some of them consistently achieved better outcomes than others. Of these therapists, fifteen had 586 patients who began pharmacotherapy with a psychiatrist. A remarkable finding was that the patients of the most effective psychotherapists had the largest medication effects, even though the psychotherapists had no or little contact with the psychiatrist. Thus, the relationship between the patient and the psychotherapist, and the expectations for medication that were created therein, affected the outcomes of care from a different mental health professional.
Further evidence for system effects comes from a meta‐analysis by Falkenström et al 110 , based on 19 studies that examined the variability in the outcomes of mental health treatments due to organizational differences. They found that “all studies showed some evidence for organization effects, and there was some evidence for organizational climate and culture explaining differences in outcome” 110, p.76 (emphasis added).
The alliance, and in particular its component related to confidence in the treatment, is influenced by many contextual variables. The relationship between the clinician and the patient is the most proximal place for the alliance to be formed. This level of understanding has attracted the greatest attention, theoretically, clinically and empirically. However, the context where the treatment takes place also contributes to the alliance.
It has been speculated that a high prestige clinic will increase belief in the efficacy of a treatment 86 . There is also evidence that the climate and culture of the clinic matter, most likely at least in part by creating an organization where therapists can thrive 111 . Furthermore, it is a mistake to assume that the treating clinician is the only influencer in such organizations. Patients interact on the phone, through email, and in person with non‐clinician staff. Do these interactions communicate warmth, caring, respect as well as competence? As well, how a patient perceives a clinician and the treatment being offered may well depend on the patient's interaction with other clinicians.
It is important to consider the context in which a treatment is delivered, with attention to the alliance of the patient with other clinicians and the clinic staff, as well as to aspects of the physical space and clinic reputation. Mental health services are increasingly being delivered electronically, and patients use various Internet‐based mediated services not involving a face‐to‐face interaction with a clinician; nevertheless, as the research suggests, the alliance with the program and a presumed clinician is critical to the optimal effectiveness of such programs. Clearly, more research into how consideration of the alliance in such programs can improve outcomes is needed.
MECHANISMS OF THE ALLIANCE AND CLINICAL ACTIONS
We will discuss now how the alliance might be healing and what might promote clinically a strong alliance. We describe three pathways to healing, each involving the alliance, which are shown in Figure 1.
Figure 1.
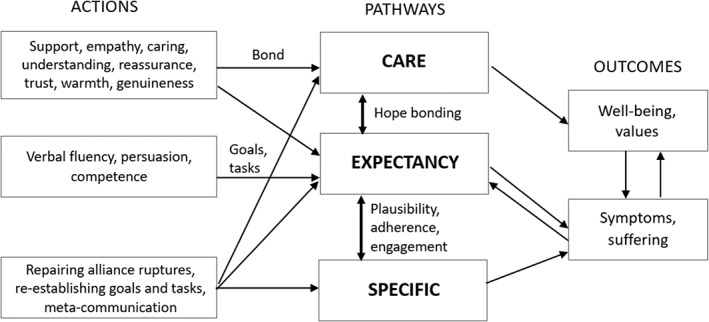
Three pathways to healing involving the alliance
The caring, attentive, real and empathic (CARE) pathway
The CARE pathway has been described in several ways. In Bordin's 1 conceptualization of the alliance, this pathway is described as the bond. In the medical literature, it is often called the emotional component of the relationship76, 83. In placebo studies, the terms warmth 90 and interpersonal healing 75 have been used. The therapist actions associated with this pathway have been labeled as support, empathy, reassurance, warmth, caring, and non‐transference‐based real relationship, among others. The question is: what about these therapist actions leads to healing? Here we tentatively suggest a few mechanisms that underlie this pathway to healing.
When patients present to a clinician for treatment, they often experience emotional distress that originates from the disorder, disease or injury. A pain in the gut may create fear of cancer; a diagnosis of Parkinson's disease may lead to depression due to an understanding of the progressive nature of the illness. The clinician, through his/her empathic and reassuring behavior, reduces the patient's emotional distress.
Humans are a social species, and rely on the assistance of others for survival18, 94, 112, 113. Individuals without adequate social support and connection will not flourish, particularly when under threat. Lack of exercise, smoking, obesity, excessive drinking, and environmental pollution increase the risk of morbidity and mortality; interestingly, loneliness is a greater risk for mortality than any of these factors114, 115. A warm and understanding clinician may well provide emotional support to patients who lack social connection, perceive themselves as lonely, or who feel that those close to them do not understand their problems. In mental health care, the clinician – with some exceptions – is available, in an understanding way, at each and every session, regardless of what the patient discloses and however shameful, fearful or difficult the material may be. With increased pressure to expand services, the time spent with each patient is becoming shorter, which increases the need to focus on the relationship.
Patients' emotional dysregulation negatively affects mental and physical health, and consequently several mental health treatments are focused on reducing this dysregulation. In these interventions, the locus is typically the patient. For example, meditation is predicated on assisting the patient regulate his/her emotions. However, there is evidence that emotion regulation is an unconscious dyadic process, in that the presence of an intimate other can attenuate arousal and distress through a process that is referred to as co‐regulation, social regulation, or interpersonal emotion regulation116, 117, 118. Dyadic emotion regulation “refers to the process by which relationship partners form a dyadic emotional system involving an oscillating pattern of affective arousal and dampening that dynamically maintains an optimal emotional state” 116, p.202 .
Co‐regulation between intimates has been investigated experimentally. In a study of maritally satisfied women, it was found that holding the hand of their husbands reduced arousal in a stressful situation in comparison to holding the hand of a stranger or not holding anyone's hand; furthermore, the more maritally satisfied the women were, the greater the effect 119 . In psychotherapy, interpersonal co‐regulation has been detected in moment‐to‐moment emotional states of the patient and therapist120, 121. Indeed, the beneficial effects of empathy in medicine have been attributed to co‐regulation74, 91, 122.
The CARE pathway is not focused on particular patient problems and should have its effect primarily on the general well‐being of the patient. This was evident in the study on irritable bowel syndrome we discussed earlier, as the largest effect of the enhanced therapeutic relationship was on the quality of life outcome 88 .
The EXPECTANCY pathway
Expectations have a strong influence on our experience of the world, particularly our expectations of our internal sensations, both physical and mental78, 79, 123. For example, taste aversions, which have evolved to protect organisms from ingesting harmful substances and which are easily conditioned, can be influenced in humans by expectations124, 125.
The influence of expectations on well‐being is established most persuasively in the placebo literature, where placebo administration influences health outcomes. Placebos “depend on a person's psychological and brain responses to the treatment context, which influence appraisals of future well‐being” 78, p.73 (emphasis added). The effects of placebos on mental disorders are well documented 126 . The EXPECTANCY pathway will affect primarily symptoms (or, more accurately, it will affect the purported outcomes of the treatment on which the clinician and patient agree).
There are many ways to acquire expectations. As discussed earlier, placebo effects can be generated without face‐to‐face interactions84, 85, 86. However, an effective and efficient way to create expectations is through verbal persuasion 95 . The verbal transmission of information about healthy behaviors is important in everyday life, as well as in health settings. Wampold 74 describes how the expectation that inserting a metal object into an electrical socket will create a painful shock is unlikely to have been acquired through classical conditioning or vicarious learning. Most people have learned not to insert metal objects into electrical sockets by being told by someone they trust, most likely a parent, that this was a dangerous practice.
Indeed, as Lieberman 94 pointed out, “our brains are designed to be influenced by others”. That is, patients are wired to believe in the explanations provided by a clinician, particularly if the clinician is perceived to be competent and expert and the patient trusts that the therapist is acting in his/her best interest. As shown in Figure 1, expectations are created by both the “warmth” and the “competence” dimensions of Howe et al's conceptualization 91 . Attention to how the clinician informs the patient about the disorder and the persuasiveness of the explanation of the treatment to be delivered are critical aspects of mental health care.
The SPECIFIC pathway
To varying degrees, the specific ingredients of mental health and in general medical treatments have an effect on the disorders. For both psychotropic medications and psychotherapies, there is a debate about the size of this effect44, 127, 128. This debate is orthogonal to the discussion of the alliance, as the alliance is necessary in most cases for the specific effects to occur. Without an agreement about the goals and tasks of therapy as well as a trusting relationship, the patient is unlikely, or at least less likely, to be engaged in and adhere to the treatment.
In medicine, there is evidence that physician's communication is associated with patient's adherence129, 130. In the schema of Figure 1, it is conjectured that expectations partially mediate the relationship between clinician's actions and the specific effects. Agreement about the tasks of therapy implies that the patient believes that the treatment will be effective, which is essentially expectations.
There is one complication of the distinction between specific effects and the alliance, not emphasized heretofore. To this point the alliance has been treated as a static entity – measurement of the alliance at a particular point in time is associated with symptoms, say at another time. However, the alliance is not stationary, but rather oscillates over the course of a session, between sessions, and over the course of therapy. Relational psychodynamic approaches to psychotherapy consider the alliance a specific effect, in that the development of the alliance over the course of therapy is therapeutic in and of itself52, 131, 132, 133. The primary mechanism is that disordered relationships underlie mental disorders and that the creation of a strong relationship with the therapist is reparative. Moreover, according to this school, there will be inevitable relationship disruptions in therapy, often called “ruptures”, due to the difficult work, and addressing these issues is therapeutic, as it models how strong interpersonal bonds are negotiated.
Whether one agrees with this approach or not, it is clear that addressing ruptures in the alliance is critical, as unaddressed problems will lead to decrements in the bond and in agreement about the goals and tasks of therapy. There is relatively strong meta‐analytic evidence that “repairing ruptures” in psychotherapy is associated with better outcomes 131 . Such repairs can be addressed by renegotiating the goals and tasks of therapy or by meta‐communication about the patient‐clinician relationship131, 133.
Interdependence of pathways
In the previous discussions of the alliance and how it relates to outcomes, it is clear that there are reciprocal and interdependent effects. For example, over time alliance predicts subsequent symptoms, and level of symptoms predicts the alliance 50 . As well, expectations reflected by agreement on goals and tasks predict final outcomes, but alliance mediates the effects of outcome expectations at the beginning of therapy and final outcomes 48 . Feeling cared for and understood by a trustworthy clinician will increase expectations. In Figure 1, we have shown various recursive effects. The pathways to healing are presented as a means to understand the complexity of how the alliance can be therapeutic.
CONCLUSIONS
The alliance, a concept that originated with Bordin's 1 discussion in 1979, has been generally accepted and empirically established in psychotherapy, and, as Bordin predicted, is now acknowledged as a therapeutic factor in any healing setting. A patient who has a warm, understanding, caring and empathic clinician, and who perceives that the treatment offered by the clinician will effectively remediate distress and restore health, will have better treatment outcomes. Understanding how the alliance works and using the interpersonal skills needed to produce a strong alliance will improve outcomes, in psychotherapy, in other mental health care, and most likely in all healing contexts.
Despite the rather extensive research on the alliance, there are a number of areas that need further exploration. There is evidence to suggest that a set of facilitative interpersonal skills demonstrated by the therapist in challenging interpersonal situations creates stronger alliances and better outcomes. However, there is a need for further research on how these skills should be applied in different contexts as well as with different patients. It is important to be cognizant that some patients will respond to the same therapeutic action differently. A patient with attachment difficulties, who has difficulty decoding emotions in interpersonal situations, or who is culturally different from the clinician, may respond in ways different from what the clinician routinely expects.
It was beyond the scope of this paper to discuss whether the interpersonal skills are born or made. There is evidence that the interpersonal skills of psychotherapy trainees at the beginning of training predict outcomes several years later58, 60, suggesting that these skills are formed before an individual receives training for professional practice. However, from studies of expert performance134, 135, there is also evidence that therapists can deliberately practice interpersonal skills and improve performance111, 136, 137, 138.
Research and clinical attention have mostly focused on the alliance between the clinician and the patient in face‐to‐face interactions. However, there is preliminary evidence concerning the alliance of patients with other clinic staff, systems of care, or the program in Internet mediated services. Those involved in the design and delivery of mental health services, whether in person or delivered electronically, should attend to how the alliance can be strengthened in ways that improve the quality of care. Education and training of mental health professionals need to incorporate deliberate efforts to utilize what is known about the alliance, in order to foster the development of the interpersonal skills necessary for these professionals to form strong alliances across a range of patients.
REFERENCES
- 1. Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy 1979;16:252‐60. [Google Scholar]
- 2. Sterba R. The fate of the ego in analytic therapy. Int J Psychoanal 1934;15:117‐26. [Google Scholar]
- 3. Menninger KA. Theory of psychoanalytic technique. New York: Basic Books, 1958. [Google Scholar]
- 4. Greenson RR. The technique and practice of psychoanalysis. New York: International Universities, 1967. [Google Scholar]
- 5. Gelso CJ. The real relationship in a postmodern world: theoretical and empirical explorations. Psychother Res 2009;19:253‐64. [DOI] [PubMed] [Google Scholar]
- 6. Oddli HW, McLeod J, Nissen‐Lie HA et al. Future orientation in successful therapies: expanding the concept of goal in the working alliance. J Clin Psychol 2021;77:1307‐29. [DOI] [PubMed] [Google Scholar]
- 7. Oddli HW, McLeod J, Reichelt S et al. Strategies used by experienced therapists to explore client goals in early sessions of psychotherapy. Eur J Psychother Couns 2014;16:245‐66. [Google Scholar]
- 8. Yulish NE, Goldberg SB, Frost ND et al. The importance of problem‐focused treatments: a meta‐analysis of anxiety treatments. Psychotherapy 2017;54:321‐38. [DOI] [PubMed] [Google Scholar]
- 9. Wampold BE. The great psychotherapy debate: model, methods, and findings. Mahwah: Lawrence Erlbaum, 2001. [Google Scholar]
- 10. Frank JD, Frank JB. Persuasion and healing: a comparative study of psychotherapy, 3rd ed. Baltimore: Johns Hopkins University, 1991. [Google Scholar]
- 11. Constantino MJ, Vîslă A, Coyne AE et al. A meta‐analysis of the association between patients' early treatment outcome expectation and their posttreatment outcomes. Psychotherapy 2018;55:473‐85. [DOI] [PubMed] [Google Scholar]
- 12. Rogers CR. Client‐centered therapy. Boston: Houghton Mifflin, 1951. [Google Scholar]
- 13. Hatcher RL, Barends AW. How a return to theory could help alliance research. Psychotherapy 2006;43:292‐9. [DOI] [PubMed] [Google Scholar]
- 14. Horvath AO, Luborsky L. The role of the therapeutic alliance in psychotherapy. J Consult Clin Psychol 1993;61:561‐73. [DOI] [PubMed] [Google Scholar]
- 15. Luborsky L. Helping alliance in psychotherapy. In: Cleghhorn JL (ed). Successful psychotherapy. New York: Brunner/Mazel, 1976:92‐116. [Google Scholar]
- 16. Horvath AO. Research on the alliance: knowledge in search of a theory. Psychother Res 2017;28:499‐516. [DOI] [PubMed] [Google Scholar]
- 17. Kenny DA. Interpersonal perception: the foundation of social relationships. New York: Guilford, 2020. [Google Scholar]
- 18. Baumeister RF. The cultural animal: human nature, meaning, and social life. New York: Oxford University Press, 2005. [Google Scholar]
- 19. Falconier MK, Jackson JB, Hiplert P et al. Dyadic coping and relationship satisfaction: a meta‐analysis. Clin Psychol Rev 2015;42:28‐46. [DOI] [PubMed] [Google Scholar]
- 20. Malloy TE. Social relations modeling of behavior in dyads and groups. London: Academic Press, 2018. [Google Scholar]
- 21. Kenny DA, Judd CM. Consequences of violating the independence assumption in analysis of variance. Psychol Bull 1986;99:422‐31. [Google Scholar]
- 22. Huppert JD, Kivity Y, Cohen L et al. A pilot randomized clinical trial of cognitive behavioral therapy versus attentional bias modification for social anxiety disorder: an examination of outcomes and theory‐based mechanisms. J Anxiety Disord 2018;59:1‐9. [DOI] [PubMed] [Google Scholar]
- 23. Marmar CR, Horowitz MJ, Marziali E. The development of the therapeutic alliance rating system. In: Greenberg LS, Pinsof WM (eds). Psychotherapeutic process: a research handbook. New York: Guilford, 1986:367‐90. [Google Scholar]
- 24. Alexander LB, Luborsky L. The Penn Helping Alliance Scales. In: Greenberg LS, Pinsof WM (eds). Psychotherapeutic process: a research handbook. New York: Guilford, 1986:325‐56. [Google Scholar]
- 25. Suh CS, Strupp HH, O'Malley SS. The Vanderbilt process measures: the Psychotherapy Process Scale (VPPS) and the Negative Indicators Scale (VNIS), In: Greenberg LS, Pinsof WM (eds). Psychotherapeutic process: a research handbook. New York: Guilford, 1986:285‐323. [Google Scholar]
- 26. Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. J Couns Psychol 1989;36:223‐33. [Google Scholar]
- 27. Flückiger C, Horvath AO, Brandt H. The evolution of patients' concept of the alliance and its relation to outcome: a dynamic latent‐class structural equation modeling approach. J Couns Psychol 2022;69:51‐62. [DOI] [PubMed] [Google Scholar]
- 28. Hoyt WT, Melby JN. Dependability of measurement in counseling psychology: an introduction to generalizability theory. Couns Psychol 1999;27:325‐52. [Google Scholar]
- 29. Hamovitch EK, Choy‐Brown M, Stanhope V. Person‐centered care and the therapeutic alliance. Community Ment Health J 2018;54:951‐8. [DOI] [PubMed] [Google Scholar]
- 30. Horvath AO. An exploratory study of the working alliance: its measurement and relationship to therapy outcome. EdD Thesis, University of British Columbia, Vancouver, 1981. [Google Scholar]
- 31. Horvath AO, Symonds BD. Relation between working alliance and outcome in psychotherapy: a meta‐analysis. J Couns Psychol 1991;38:139‐49. [Google Scholar]
- 32. Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: a meta‐analytic review. J Consult Clin Psychol 2000;68:438‐50. [PubMed] [Google Scholar]
- 33. Horvath AO, Bedi RP. The alliance. In: Norcross JC (ed). Psychotherapy relationships that work: therapist contributions and responsiveness to patients. New York: Oxford University Press, 2002:37‐69. [Google Scholar]
- 34. Horvath AO, Del Re AC, Flückiger C et al. Alliance in individual psychotherapy. Psychotherapy 2011;48:9‐16. [DOI] [PubMed] [Google Scholar]
- 35. Flückiger C, Del Re AC, Horvath AO et al. The alliance in adult psychotherapy: a meta‐analytic synthesis. Psychotherapy 2018;55:316‐40. [DOI] [PubMed] [Google Scholar]
- 36. Karver MS, De Nadai AS, Monahan M et al. Meta‐analysis of the prospective relation between alliance and outcome in child and adolescent psychotherapy. Psychotherapy 2018;55:341‐55. [DOI] [PubMed] [Google Scholar]
- 37. Friedlander ML, Escudero V, Welmers‐van de Poll M et al. Meta‐analysis of the alliance‐outcome relation in couple and family therapy. Psychotherapy 2018;55:356‐71. [DOI] [PubMed] [Google Scholar]
- 38. Alldredge CT, Burlingame GM, Yang C et al. Alliance in group therapy: a meta‐analysis. Group Dyn 2021;25:13‐28. [Google Scholar]
- 39. Owen J, Adelson J, Budge S et al. Trajectories of change in psychotherapy. J Clin Psychol 2015;71:817‐27. [DOI] [PubMed] [Google Scholar]
- 40. Baldwin SA, Berkeljon A, Atkins DC et al. Rates of change in naturalistic psychotherapy: contrasting dose‐effect and good‐enough level models of change. J Consult Clin Psychol 2009;77:203‐11. [DOI] [PubMed] [Google Scholar]
- 41. DeRubeis RJ, Brotman MA, Gibbons JC. A conceptual and methodological analysis of the nonspecifics argument. Clin Psychol 2005;12:174‐83. [Google Scholar]
- 42. Tang TZ, DeRubeis RJ. Reconsidering rapid early response in cognitive behavioral therapy for depression. Clin Psychol 1999;6:283‐8. [DOI] [PubMed] [Google Scholar]
- 43. Ilardi SS, Craighead WE. The role of nonspecific factors in cognitive‐behavior therapy for depression. Clin Psychol 1994;1:138‐56. [Google Scholar]
- 44. Wampold BE, Imel ZE. The great psychotherapy debate: the evidence for what makes psychotherapy work, 2nd ed. New York: Routledge, 2015. [Google Scholar]
- 45. Flückiger C, Del Re AC, Wlodasch D et al. Assessing the alliance‐outcome association adjusted for patient characteristics and treatment processes: a meta‐analytic summary of direct comparisons. J Couns Psychol 2020;67:706‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Beard JIL, Delgadillo J. Early response to psychological therapy as a predictor of depression and anxiety treatment outcomes: a systematic review and meta‐analysis. Depress Anxiety 2019;36:866‐78. [DOI] [PubMed] [Google Scholar]
- 47. Baier AL, Kline AC, Feeny NC. Therapeutic alliance as a mediator of change: a systematic review and evaluation of research. Clin Psychol Rev 2020;82:101921. [DOI] [PubMed] [Google Scholar]
- 48. Constantino MJ, Coyne A. Goodwin BJ et al. Indirect effect of patient outcome expectation on improvement through alliance quality: a meta‐analysis. Psychother Res 2021;31:711‐25. [DOI] [PubMed] [Google Scholar]
- 49. Curran PJ, Bauer DJ. The disaggregation of within‐person and between‐person effects in longitudinal models of change. Annu Rev Psychol 2011;62:583‐619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Flückiger C, Rubel JA, Del Re AC et al. The reciprocal relationship between alliance and early treatment symptoms: a two‐stage individual participant data meta‐analysis. J Consult Clin Psychol 2020;88:829‐43. [DOI] [PubMed] [Google Scholar]
- 51. Baldwin SA, Wampold BE, Imel ZE. Untangling the alliance‐outcome correlation: exploring the relative importance of therapist and patient variability in the alliance. J Consult Clin Psychol 2007;75:842‐52. [DOI] [PubMed] [Google Scholar]
- 52. Zilcha‐Mano S. Is the alliance really therapeutic? Revisiting this question in light of recent methodological advances. Am Psychol 2017;72:311‐25. [DOI] [PubMed] [Google Scholar]
- 53. Baldwin SA, Imel ZE. Therapist effects: finding and methods. In: Lambert MJ (ed). Bergin and Garfield's handbook of psychotherapy and behavior change. New York: Wiley, 2013:258‐97. [Google Scholar]
- 54. Wampold BE, Owen J. Therapist effects: history, methods, magnitude, and characteristics of effective therapists. In: Barkham M, Lutz W, Castonguay LG (eds). Bergin and Garfield's handbook of psychotherapy and behavior change. New York: Wiley, 2021:301‐30. [Google Scholar]
- 55. Del Re AC, Flückiger C, Horvath AO et al. Therapist effects in the therapeutic alliance‐outcome relationship: a restricted‐maximum likelihood meta‐analysis. Clin Psychol Rev 2012;32:642‐9. [DOI] [PubMed] [Google Scholar]
- 56. Del Re AC, Flückiger C, Horvath AO et al. Examining therapist effects in the alliance‐outcome relationship: a multilevel meta‐analysis. J Consult Clin Psychol 2021;89:371‐8. [DOI] [PubMed] [Google Scholar]
- 57. Anderson T, Ogles BM, Patterson CL et al. Therapist effects: facilitative interpersonal skills as a predictor of therapist success. J Clin Psychol 2009;65:755‐68. [DOI] [PubMed] [Google Scholar]
- 58. Schöttke H, Flückiger C, Goldberg SB et al. Predicting psychotherapy outcome based on therapist interpersonal skills: a five‐year longitudinal study of a therapist assessment protocol. Psychother Res 2017;27:642‐52. [DOI] [PubMed] [Google Scholar]
- 59. Anderson T, Crowley MEG, Himawan L et al. Therapist facilitative interpersonal skills and training status: a randomized clinical trial on alliance and outcome. Psychother Res 2016;26:511‐29. [DOI] [PubMed] [Google Scholar]
- 60. Anderson T, McClintock AS, Himawan L et al. A prospective study of therapist facilitative interpersonal skills as a predictor of treatment outcome. J Consult Clin Psychol 2016;84:57‐66. [DOI] [PubMed] [Google Scholar]
- 61. Webb CA, DeRubeis RJ, Amsterdam JA et al. Two aspects of the therapeutic alliance: differential relations with depressive symptom change. J Consult Clin Psychol 2011;79:279‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Hagen K, Solem S, Opstad HB et al. Therapist variability in the task/goal dimension of the early working alliance predicts outcome in exposure and response prevention treatment for obsessive‐compulsive disorder. Clin Neuropsychiatry 2016;13:94‐9. [Google Scholar]
- 63. Ulvenes PG, Berggraf L, Hoffart A et al. Different processes for different therapies: therapist actions, therapeutic bond, and outcome. Psychotherapy 2012;49:291‐302. [DOI] [PubMed] [Google Scholar]
- 64. Krebs P, Norcross JC, Nicholson JM et al. Stages of change and psychotherapy outcomes: a review and meta‐analysis. J Clin Psychol 2018;74:1964‐79. [DOI] [PubMed] [Google Scholar]
- 65. Vrabel KR, Ulvenes PG, Wampold BE. Alliance and symptom improvement in inpatient treatment for eating disorder patients: a study of within‐patient processes. Int J Eat Disord 2015;48:1113‐21. [DOI] [PubMed] [Google Scholar]
- 66. Flückiger C, Del Re AC, Horvath AO et al. Substance use disorders and racial/ethnic minorities matter: a meta‐analytic examination of the relation between alliance and outcome. J Couns Psychol 2013;60:610‐6. [DOI] [PubMed] [Google Scholar]
- 67. Brown A, Mountford VA, Waller G. Is the therapeutic alliance overvalued in the treatment of eating disorders? Int J Eat Disord 2013;46:779‐82. [DOI] [PubMed] [Google Scholar]
- 68. Graves TA, Tabri N, Thompson‐Brenner H et al. A meta‐analysis of the relation between therapeutic alliance and treatment outcome in eating disorders. Int J Eat Disord 2017;50:323‐40. [DOI] [PubMed] [Google Scholar]
- 69. Miller WR. Sacred cows and greener pastures: reflections from 40 years in addiction research. Alcohol Treat Q 2016;34:92‐115. [Google Scholar]
- 70. Moyers TR, Miller WR, Hendrickson SML. How does motivational interviewing work? Therapist interpersonal skill predicts client involvement within motivational interviewing sessions. J Consult Clin Psychol 2005;73:590‐8. [DOI] [PubMed] [Google Scholar]
- 71. Westra HA, Norouzian N. Using motivational interviewing to manage process markers of ambivalence and resistance in cognitive behavioral therapy. Cogn Ther Res 2018;42:193‐203. [Google Scholar]
- 72. Owen J, Imel Z, Tao KW et al. Cultural ruptures in short‐term therapy: working alliance as a mediator between clients' perceptions of microaggressions and therapy outcomes. Couns Psychother Res 2011;11:204‐12. [Google Scholar]
- 73. Zimmermann D, Wampold BE, Rubel JA et al. The influence of extra‐therapeutic social support on the association between therapeutic bond and treatment outcome. Psychother Res 2021;31:726‐36. [DOI] [PubMed] [Google Scholar]
- 74. Wampold BE. Healing in a social context: the importance of clinician and patient relationship. Front Pain Res 2021;2:684768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Miller FG, Colloca L, Kaptchuk TJ. The placebo effect: illness and interpersonal healing. Perspect Biol Med 2009;52:518‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Di Blasi Z, Harkness E, Ernst E et al. Influence of context effects on health outcomes: a systematic review. Lancet 2001;357:757‐62. [DOI] [PubMed] [Google Scholar]
- 77. Moerman DE, Jones WB. Deconstructing the placebo effect and finding the meaning response. Ann Int Med 2002;136:471‐6. [DOI] [PubMed] [Google Scholar]
- 78. Ashar YK, Chang LJ, Wager TD. Brain mechanisms of the placebo effect: an affective appraisal account. Annu Rev Clin Psychol 2017;13:73‐98. [DOI] [PubMed] [Google Scholar]
- 79. Benedetti F. Placebo effects: understanding the other side of medical care, 3rd ed. Oxford: Oxford University Press, 2021. [Google Scholar]
- 80. Price DP, Finniss DG, Benedetti F. A comprehensive review of the placebo effect: recent advances and current thought. Annu Rev Psychol 2008;59:565‐90. [DOI] [PubMed] [Google Scholar]
- 81. Benedetti F. Mechanisms of placebo and placebo‐related effects across diseases and treatments. Annu Rev Pharmacol Toxicol 2008;48:33‐60. [DOI] [PubMed] [Google Scholar]
- 82. Kelley JM, Kraf‐Todd G, Schapira L et al. The influence of the patient‐clinician relationship on healthcare outcomes: a systematic review and meta‐analysis of randomized controlled trials. PLoS One 2014;9:e94207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Grünbaum A. The placebo concept. Behav Res Ther 1981;19:157‐67. [DOI] [PubMed] [Google Scholar]
- 84. Kam‐Hansen S, Jakubowski N, Kelly JM et al. Altered placebo and drug labeling changes the outcome of episodic migraine attacks. Sci Transl Med 2014;6:218ra5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Gaab J, Kossowski J, Ehlert U et al. Effects and components of placebos with a psychological treatment rationale – three randomized‐controlled studies. Sci Rep 2019;9:1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Liberman BL. The role of mastery in psychotherapy: maintenance of improvement and prescriptive change. In: Frank JD, Hohen‐Saric R, Imber SD et al (eds). Effective ingredients of successful psychotherapy. Baltimore: Johns Hopkins University, 1978:35‐72. [Google Scholar]
- 87. Colloca L, Miller FG. How placebo responses are formed: a learning perspective. Philos Trans R Soc Lond B Biol Sci 2011;366:1859‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Kaptchuk TJ, Kelly JM, Conboy LA et al. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ 2008;336:999‐1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Kelley JM, Lembo AJ, Ablon JS et al. Patient and practitioner influences on the placebo effect in irritable bowel syndrome. Psychosom Med 2009;71:789‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Fuentes J, Armijo‐Olivo S, Funabashi M et al. Enhanced therapeutic alliance modulates pain intensity and muscle pain sensitivity in patients with chronic low back pain: an experimental controlled study. Phys Ther 2014;94:477‐89. [DOI] [PubMed] [Google Scholar]
- 91. Howe LC, Leibowitz KA, Crum AJ. When your doctor “gets it” and “gets you”: the critical role of competence and warmth in the patient‐provider interaction. Front Psychiatry 2019;10:475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Howe LC, Goyer JP, Crum AJ. Harnessing the placebo effect: exploring the influence of physician characteristics on placebo response. Health Psychol 2017;36:1074‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Czerniak E, Biegon A, Ziv A et al. Manipulating the placebo response in experimental pain by altering doctor's performance style. Front Psychol 2016;7:874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Lieberman MD. Social: why our brains are wired to connect. New York: Crown Publishing Group, 2013. [Google Scholar]
- 95. Geers AL, Briñol P, Vogel A et al. The application of persuasion theory to placebo effects. Int Rev Neurobiol 2018;138:113‐36. [DOI] [PubMed] [Google Scholar]
- 96. Petty RE, Briñol P. The elaboration likelihood and metacognitive models of attitudes. Implications for prejudice, the self, and beyond. In: Sherman JW, Gawronski B, Trope Y (eds). Dual‐process theories of the social mind. New York: Guilford, 2013:172‐87. [Google Scholar]
- 97. Frank JB, Wampold BE. Persuasion and healing, 4th ed. Baltimore: Johns Hopkins University; (in press). [Google Scholar]
- 98. Frank JD. Persuasion and healing: a comparative study of psychotherapy, 2th ed. Baltimore: Johns Hopkins University, 1973. [Google Scholar]
- 99. Frank JD. Persuasion and healing: a comparative study of psychotherapy. Baltimore: Johns Hopkins University, 1961. [Google Scholar]
- 100. Norcross JC, Lambert MJ (eds). Psychotherapy relationships that work, Vol. 1: Evidence‐based therapist contributions, 3rd ed. New York: Oxford University Press, 2019. [Google Scholar]
- 101. Finsrud I, Nissen‐Lie, HA , Vrabel K et al. It's the therapist and the treatment: the structure of common therapeutic relationship factors. Psychother Res 2022;32:139‐50. [DOI] [PubMed] [Google Scholar]
- 102. Wampold BE. How important are the common factors in psychotherapy? An update. World Psychiatry 2015;14:270‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Elkin I, Parloff MB, Hadley et al. NIMH Treatment of Depression Collaborative Research Program: background and research plan. Arch Gen Psychiatry 1985;42:305‐16. [DOI] [PubMed] [Google Scholar]
- 104. Elkin I, Shea MT, Watkins JT et al. National Institute of Mental Health Treatment of Depression Collaborative Research Program. General effectiveness of treatments. Arch Gen Psychiatry 1989;46:971‐82. [DOI] [PubMed] [Google Scholar]
- 105. McKay KM, Imel ZE, Wampold BE. Psychiatrist effects in the psychopharmacological treatment of depression. J Affect Disord 2006;16:236‐42. [DOI] [PubMed] [Google Scholar]
- 106. Carlbring P, Andersson G, Cuijpers P et al. Internet‐based vs. face‐to‐face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta‐analysis. Cogn Behav Ther 2018;47:1‐18. [DOI] [PubMed] [Google Scholar]
- 107. Zalaznik D, Strauss AY, Halaj A et al. Patient alliance with the program predicts treatment outcomes whereas alliance with the therapist predicts adherence in internet‐based therapy for panic disorder. Psychother Res 2021;31:1022‐35. [DOI] [PubMed] [Google Scholar]
- 108. Kaiser J, Hanschmidt F, Kersting A. The association between therapeutic alliance and outcome in internet‐based psychological interventions: a meta‐analysis. Comp Hum Behav 2021;114:106512. [Google Scholar]
- 109. Wampold BE, Brown GS. Estimating therapist variability: a naturalistic study of outcomes in managed care. J Consult Clin Psychol 2005;73:914‐23. [DOI] [PubMed] [Google Scholar]
- 110. Falkenström F, Grant J, Holmqvist R. Review of organizational effects on the outcome of mental health treatments. Psychother Res 2018;28:76‐90. [DOI] [PubMed] [Google Scholar]
- 111. Goldberg SB, Babins‐Wagner R, Rousmaniere T et al. Creating a climate for therapist improvement: a case study of an agency focused on outcomes and deliberate practice. Psychotherapy 2016;53:367‐75. [DOI] [PubMed] [Google Scholar]
- 112. Wilson EO. On human nature. Cambridge: Harvard University Press, 1978. [Google Scholar]
- 113. Wilson EO. The social conquest of earth. New York: Liveright, 2012. [Google Scholar]
- 114. Cacioppo S, Cacioppo JT. Decoding the invisible forces of social connections. Front Integr Neurosci 2012;6:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Holt‐Lunstad J, Robles TF, Sbarra DA. Advancing social connection as a public health priority in the United States. Am Psychol 2017;72:517‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Butler EA, Randall AK. Emotional coregulation in close relationships. Emot Rev 2013;5:202‐10. [Google Scholar]
- 117. Reeck C, Ames DR, Ochsner KN. The social regulation of emotion: an integrative, cross‐disciplinary model. Trends Cogn Sci 2016;20:47‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Williams WC, Morelli SA, Ong DC et al. Interpersonal emotion regulation: implications for affiliation, perceived support, relationships, and well‐being. J Pers Soc Psychol 2018;115:224‐54. [DOI] [PubMed] [Google Scholar]
- 119. Coan JA, Schaefer HS, Davidson RJ. Lending a hand: social regulation of the neural response to threat. Psychol Sci 2006;17:1032‐9. [DOI] [PubMed] [Google Scholar]
- 120. Soma CS, Baucom BRW, Xiao B et al. Coregulation of therapist and client emotion during psychotherapy. Psychother Res 2020;30:591‐603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Wieder G, Wiltshire TJ. Investigating coregulation of emotional arousal during exposure‐based CBT using vocal encoding and actor‐partner interdependence models. J Consult Clin Psychol 2020;67:337‐48. [DOI] [PubMed] [Google Scholar]
- 122. Decety J, Fotopoulou A. Why empathy has a beneficial impact on others in medicine: unifying theories. Front Behav Neurosci 2015;8:457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Kirsch I. How expectancies shape experience. Washington: American Psychological Association, 1999. [Google Scholar]
- 124. Nitschke JB, Dixon GE, Sarinopoulos I et al. Altering expectancy dampens neural response to aversive taste in primary taste cortex. Nat Neurosci 2006;9:435‐42. [DOI] [PubMed] [Google Scholar]
- 125. Sarinopoulos I, Dixon GE, Short SJ et al. Brain mechanisms of expectation associated with insula and amygdala response to aversive taste: implications for placebo. Brain Behav Immun 2006;20:120‐32. [DOI] [PubMed] [Google Scholar]
- 126. Kirsch I. Placebo effect in the treatment of depression and anxiety. Front Psychiatry 2019;10:407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Kirsch I, Deacon BJ, Huedo‐Medina TB et al. Initial severity and antidepressant benefits: a meta‐analysis of data submitted to the Food and Drug Administration. PLoS Med 2008;5:e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Kirsch I, Moore TJ, Scoboria A et al. The emperor's new drugs: an analysis of antidepressant medication data submitted to the U.S. Food and Drug Administration. Prev Treat 2002;5:23. [Google Scholar]
- 129. Stavropoulou C. Non‐adherence to medication and doctor‐patient relationship: evidence from a European survey. Patient Educ Couns 2011;83:7‐13. [DOI] [PubMed] [Google Scholar]
- 130. Zolnierek KBT, DiMatteo MR. Physician communication and patient adherence to treatment: a meta‐analysis. Med Care 2009;47:826‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Eubanks CF, Muran JC, Safran JD. Alliance rupture repair: a meta‐analysis. Psychotherapy 2018;55:508‐19. [DOI] [PubMed] [Google Scholar]
- 132. Zilcha‐Mano S, Muran JC, Eubanks CF et al. Not just a non‐specific factor: moderators of the effect of within‐ and between‐clients alliance on outcome in CBT. Cogn Ther Res 2018;42:146‐58. [Google Scholar]
- 133. Safran JD, Muran JC. Negotiating the therapeutic alliance. New York: Guilford, 2000. [Google Scholar]
- 134. Ericsson KA, Krampe RT, Tesch‐Römer C. The role of deliberate practice in the acquisition of expert performance. Psychol Rev 1993;100:363‐406. [Google Scholar]
- 135. Ericsson KA, Lehmann AC. Expert and exceptional performance: evidence of maximal adaptation to task constraints. Annu Rev Psychol 1996;47:273‐305. [DOI] [PubMed] [Google Scholar]
- 136. Rousmaniere T. Deliberate practice for psychoherapists: a guide to improving clinical effectiveness. New York: Routledge, 2016. [Google Scholar]
- 137. Rousmaniere T, Goodyear R, Miller SD et al (eds). The cycle of excellence: using deliberate practice to improve supervision and training. Hoboken: Wiley, 2017. [Google Scholar]
- 138. Chow DL, Miller SD, Seidel JA et al. The role of deliberate practice in the development of highly effective psychotherapists. Psychotherapy 2015;52:337‐45. [DOI] [PubMed] [Google Scholar]


