Abstract
Objectives:
Risky sexual behavior among sexual minorities (lesbian, gay and bisexual individuals) are partly attributed to mental health and other social disparities; but this may be confounded by correlated genetic and environmental influences. As pre-registered, the present study investigated indirect associations between sexual minority status and increased lifetime sexual partners through increased psychosocial adversity (depressive and anxiety symptoms, intimate partner violence and early-life adversities) and substance use (alcohol, cannabis and other illicit drugs), confounding by correlated genetic and environmental influences, and sex differences in these relationships.
Method:
The sample comprised sexual minority and heterosexual twins who participated in the first and second phases of the latest wave of data collection in the UK population-based Twins Early Development Study cohort (June 2017 through February 2019, n=9697 and 8718 respectively, mean age: 22.3±0.92 years). Structural equation modelling was used to specify psychosocial adversity and substance use as mediators while genetic and environmental confounding was further determined by biometrical genetic analyses in which similarities in identical and non-identical twins were compared.
Results:
Increased psychosocial adversity and substance use fully mediated increased lifetime sexual partners in sexual minority women while this effect was partial (31.1%) in men. The best-fitting genetic models indicated that these relationships were not confounded by correlated genetic and environmental influences.
Conclusions:
The relationships between sexual minority status, psychosocial adversity, substance use and sexual health disparities appeared independent of genetic and environmental influences. Individual and systemic interventions to reduce psychosocial disadvantage and substance use can also decrease sexual health disparities among sexual minorities.
Keywords: Mental health, psychosocial adversity, substance use, sexual minority, risky sexual behavior, behavior genetics
Introduction
Compared to heterosexual individuals, sexual minorities (those who identify as lesbian, gay and bisexual or who report same-sex sexual attraction) report poorer sexual health outcomes such as higher rates of sexually transmitted infections including HIV (Bränström & Pachankis, 2018; Charlton et al., 2011). This is partly attributed to consequences of minority stress (i.e. negative social and psychological experiences due to membership of a sexual minority group, Meyer, 2013; Xu et al., 2017). Minority stress is also associated with higher rates of substance use problems and psychosocial adversities such as depressive and anxiety disorders, early-life adversities and intimate partner violence which are more prevalent among sexual minorities (King et al., 2008; Meyer, 2013; Roberts et al., 2012; Rollè et al., 2018). Evidence of syndemic associations between psychosocial adversities, substance use problems and risky sexual behavior including multiple sexual partners, inconsistent condom use, commercial sex and sex under the influence of psychoactive substances (Cabecinha et al., 2017) among sexual minority individuals (Stall et al., 2003) suggests the possibility that psychosocial disparities and substance use may mediate the relationship between sexual minority status and increased risky sexual behavior indexed by higher lifetime sexual partners.
In addition to the direct consequences of minority stress on depressive and anxiety symptoms among sexual minority individuals (Hatzenbuehler, 2009), minority stress may increase the likelihood of these mental health difficulties through increased social adversities. For example, minority stress may manifest earlier in life as childhood maltreatment which may in turn increase the likelihood of later mental health difficulties (Roberts et al., 2012). Similarly, minority stress may also partly explain the higher rates of intimate partner violence among sexual minority individuals (Rollè et al., 2018), thus resulting in higher rates of these mental health difficulties among them. These psychosocial factors (depressive and anxiety symptoms, early-life adversities and intimate partner violence) have in turn been shown to be associated with increased HIV risk behaviors including multiple sexual partners in the general population and among sexual minorities both directly (Tsai & Burns, 2015) and through increased substance use (Turner et al., 2018). However, many studies investigating these relationships have focused on bivariate relationships between these factors rather than possible mediation relationships.
To our knowledge, only one population-based study has investigated this possibility. Using a twin sample, mental health disparities were shown to mediate ten percent of the higher risky sexual behavior among sexual minorities (Oginni et al., 2020). By incorporating the genetic information from the sample (i.e., comparing similarities in identical and non-identical twins), it was further shown that in contrast to previous findings indicating genetic correlations between sexual orientation, psychosocial factors and risky sexual behavior including higher lifetime sexual partners (Ganna et al., 2019; Zietsch et al., 2010; Zietsch et al., 2012); this mediation relationship was not confounded by correlated (or overlapping) etiological genetic and individual-specific environmental influences. An extreme interpretation of such genetic correlations is that they reflect pleiotropic genetic influences on sexual orientation, psychosocial adversity and risky sexual behavior (i.e., common genetic loci simultaneously influencing all three outcomes). Similarly, individual-specific environmental correlations may be interpreted as reflecting simultaneous effects of nonfamilial factors on sexual orientation and adverse health outcomes. However, Oginni et al. (2020) demonstrated that these etiological (genetic and environmental) correlations are best understood as being transmitted through the mediation paths rather than reflecting true pleiotropy. This finding indicates the potential that the observed mediation relationships can be elaborated, targeted for further intervention and psychosocial disparities completely eliminated.
However, despite recognized associations between psychosocial adversities and risky sexual behavior (Stall et al., 2003; Tsai & Burns, 2015), Oginni et al. (2020) did not include social adversity variables were included in their analytic model. Furthermore, they did not investigate the possibility that substance use represents a distinct factor as suggested by previous research (Halkitis et al., 2013). This latter possibility is further supported by prospective evidence that higher alcohol use problems among sexual minority compared to heterosexual young adults was partly mediated by higher depressive symptoms during adolescence (Pesola et al., 2014). Thus, in addition to psychosocial adversities and substance use problems jointly mediating the association between sexual minority status and risky sexual behavior, substance use may further mediate the association between psychosocial adversity and risky sexual behavior.
Because these complex patterns may also be confounded by unmeasured genetic and environmental influences, it is important to investigate these associations using a genetically-informed design such as the classical twin design which allows the estimation of etiological genetic and environmental influences on individual differences by comparing the correlations in monozygotic (identical) and dizygotic (non-identical) twins. To account for these gaps in existing research, we test a model consisting of three mediation pathways to explain increased risky sexual behavior among sexual minority individuals: a single course mediation via psychosocial adversity, another via substance use, and a two-course mediation via both factors. Furthermore, considering the novel nature of the earlier finding by Oginni et al. (2020); replication using a different twin cohort will provide further validation.
Our objectives, therefore, were to test whether increased psychosocial adversity and substance use, on their own and jointly, mediated increased risky sexual behavior indexed by number of lifetime sexual partners among sexual minority individuals; and whether this mediation was confounded by genetic and environmental influences. Considering that these relationships are understudied among sexual minority women, we also investigated sex differences in the tested models.
Methods
The sample comprised participants in the two phases of the latest wave of data collection (June 2017 to February 2019) from the UK Twins Early Development Study (TEDS) cohort (mean age: 22.3 ±0.92 years). Of the 16810 families in the original TEDS sample, email and paper invitations were sent to 10571 in the first phase (2180, 2270 and 1780 had withdrawn, were inactive or uncontactable respectively). In the second phase, 8611 twin pairs were similarly invited (about 1640 twin pairs had not participated in the first phase or could not be contacted). Questionnaires were administered via mailed paper booklets, a mobile phone application, and a web-based platform. In total, 9697 and 8718 twin individuals participated in the first and second phases of data collection respectively. Further details of the recruitment and are available at the TEDS website (https://www.teds.ac.uk/datadictionary/studies/21yr.htm) and previous descriptions (e.g., Rimfeld et al., 2019). Ethical approval was granted by King’s College London’s ethics committee for the Institute of Psychiatry, Psychology and Neuroscience.
Only participants with at least 75% completed responses to items per variable were included in analyses and 416 participants were further excluded for medical reasons (Supplementary Tables S1 and S2). Imputation was not required as missingness for the predictor and mediator variables was less than 5% (Kline, 2016). Zygosity (whether twins were monozygotic or dizygotic) was assessed during childhood using a parent-reported questionnaire which had an accuracy of 95% when compared to DNA testing (Price et al., 2000). Informed consent was obtained from all participants via web-based and online consent forms.
Measures
Predictor
Sexual orientation was assessed using a single question assessing sexual attraction with responses recoded as “Always opposite sex” scored 1, “Mostly opposite sex but sometimes same sex” (2), “Equally same and opposite sexes” (3), “Mostly same sex but sometimes opposite sex” (4) and “Always same sex” (5) corresponding to “Exclusively Heterosexual”, “Mostly Heterosexual”, ‘Bisexual”, “Mostly Gay/Lesbian” and “Exclusively Gay/Lesbian” respectively. Participants who responded, “Little or no sexual attraction” and “Unsure or do not know” were excluded from the analyses (n = 216) as we did not have any a priori hypotheses about them. Sexual orientation was included in analyses as a liability threshold variable with its five ordered categories assumed to reflect an underlying liability which is normally distributed (Rijsdijk & Sham, 2002). Scores of 1 thus indicate heterosexuality while scores greater than 1 indicate increasing non-heterosexuality or sexual minority status respectively.
Mediators
Psychosocial adversities.
(1) Depressive symptoms, assessed using the Brief 8-item Mood and Feelings Questionnaire (MFQ), a shorter version of the short MFQ which rates the presence and severity of depressive symptoms such as sad mood, low energy and low self-worth over the past two weeks (Angold et al., 1995). A sample item was: “In the past two weeks, I cried a lot”. Each item was rated on a 3-point Likert scale ranging from 0 (Not at all) to 2 (True). (2) Generalized anxiety symptoms, assessed using the 10-item Severity Measure for Generalized Anxiety Disorder – Adult (Craske et al., 2013) which rates the frequency of each symptom over the past week. Symptoms included feeling worried and tense, having palpitations and difficulty making decisions and a sample item was: “During the past seven days, I have felt anxious, worried or nervous” and each item was rated on a 5-point Likert scale ranging from 0 (Never) to 4 (All of the time). (3) Early-life adverse experiences including physical and psychological abuse, assessed using eight questions derived from items in the Avon Longitudinal Study of Parents and Children (https://www.teds.ac.uk/datadictionary/studies/measures/21yr_measures.htm). Items such as “When you were a child, how often did an adult in your family shout at you?” were each scored on a 5-point Likert scale ranging from 0 (Never) to 4 (Very often). (4) Intimate partner violence, assessed via 6 questions adapted from the questions designed by the Centers for Disease Control and Prevention (Basile et al., 2007) to elicit physical and emotional abuse victimization by a partner in past or current intimate relationships. Items such as “Your partner (current or past) pushed, hit, kicked, or otherwise physically hurt you” were each rated on a 5-point Likert scale ranging from 1 (Strongly disagree) to 5 (Strongly agree). Total scores for each scale were derived by summing item responses and used in analyses with higher scores indicating more adversities. Cronbach’s alphas in this study were 0.87, 0.91, 0.86 and 0.91 respectively.
Substance use problems.
These were assessed for: (1) Alcohol, using the Alcohol Use Disorder Identification Test (AUDIT; Babor et al., 2001) which comprises ten questions rating the level of alcohol use and frequency of alcohol-related problems such as “During the past year, how often have you had six or more units of alcohol on one occasion?”. Each item is rated on a 5-point response scale ranging from 0 (No/Never) to 4 (Yes/Daily or almost daily). (2) Cannabis, using the 6-item Cannabis Abuse Screening Test (CAST; Legleye et al., 2007) which elicits the frequency of cannabis-related problems over the past year. Items such as “During the past 12 months, how often have you tried to reduce or stop your cannabis use without succeeding?” were rated on a 5-point Likert scale ranging from 0 (Never/almost never) to 4 (Often). (3) Other illicit drug use, using supplementary questions about the frequency of use of cocaine, crack, amphetamine-type stimulants, inhalants, hallucinogens and sedatives and opioids without prescription such as “Have you ever taken cocaine (charlie, ‘c’, coke, etc.)?”. Individuals who had never used the substances assessed by each scale were scored 0. Total scores for each measure were derived by summing responses to individual items and used in analyses with higher scores indicating more problematic substance use. Cronbach’s alpha for the AUDIT, CAST and the illicit drug use measure were 0.80, 0.84 and 0.74 respectively.
Outcome
Number of lifetime sexual partners was used as a proxy for risky sexual behavior based on common practice in HIV risk research (Slaymaker, 2004) and its association with other sexual risk behaviors (Cabecinha et al., 2017). It was assessed using a single question “How many people have you had sexual intercourse with?” and responses were categorized to limit the effects of extreme scores on the distribution as follows as is often done (e.g., Penke & Asendorpf, 2008): No partners or never had sex (scored 0), 1 partner (1), 2–3 partners (scored 2), 4–7 partners (scored 3), 8–14 partners (scored 4) and 15 or more partners (scored 5).
Covariates
Participants’ age and birth sex were ascertained using single questions asked during earlier waves of data collection and included as covariates as is typically done in twin studies (McGue & Bouchard, 1984). Confounding by other unmeasured variables is captured by genetic models.
Latent factors
Sexual orientation (SO), Psycho-Social Adversity (PSA), Substance Use (SU) and Lifetime Sexual Partners (LSP) were specified as latent factors indicated by their respective variable sum scores to facilitate genetic analyses. We specified Psycho-Social Adversity and Substance Use as separate factors based on smaller cross-factor variables correlations (r = .05 to .13) compared to larger within-factor correlations for the PSA and SU factors (r = .21 to.53 and .19 to .45 respectively) and consistent with previous research among gay and bisexual men (Halkitis et al., 2013). Factors were scaled by fixing one factor loading per factor to 1 (Kline, 2016).
Statistical Analysis
Data cleaning, preliminary summary statistics and investigation of sex differences were carried out using SPSS version 26 and STATA version SE 14.2. Structural Equation Model fitting was carried out using OpenMx (Neale et al., 2016). Mean effects of covariates were regressed out from the study variables before transformation to normality (Kline, 2016).
Phenotypic and Genetic Correlations
Maximum likelihood phenotypic correlations were estimated using a model in which within-person correlations were constrained to be equal across birth order and zygosity and cross-trait cross-twin correlations were constrained to be symmetrical. Phenotypic correlations indicate observed correlations which are not further parsed into genetic and environmental components. These contrast with biometric genetic analyses which resolve variances and correlations/covariances into genetic and environmental components.
Biometric genetic1 analyses involved the comparison of similarities between monozygotic and dizygotic twin pairs to estimate genetic and environmental influences. A genetic multivariate model was specified to resolve variable and factor variances and covariances into latent genetic (A), and shared (C) and individual-specific (E) environmental components (Rijsdijk & Sham, 2002). A influences represent the sum of effects at each allele on a trait across the whole genome, C influences incorporate aspects of the environment that make family members similar to each other such as parenting styles and socio-economic status, whereas E influences include factors that make family members different from such as differential parental treatment or differential prenatal exposures and accidents, but also measurement error. This method assumes that monozygotic and dizygotic twin pairs raised together are 100% and 50% genetically similar respectively, are influenced by their shared environment to the same degrees but do not share any E influences.
Phenotypic and Genetic Mediation models
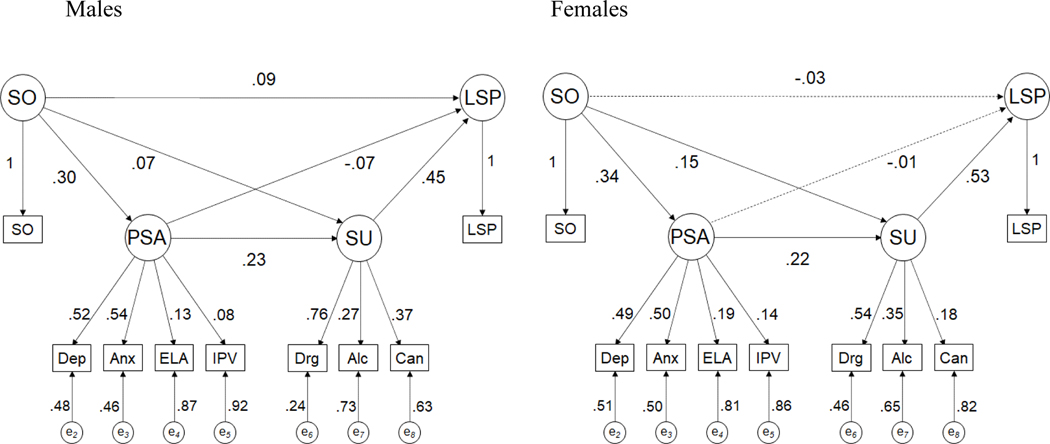
A phenotypic mediation model was specified for the latent factors (Figure 1) and the direct effect indicated by the standardized coefficient of the SO-LSP path, while indirect effects included: i. the product of the standardized coefficients of the SO-PSA and PSA-LSP paths, ii. the product of the SO-SU and SU-LSP paths and iii. the product of the SO-PSA, PSA-SU and SU-LSP paths. The overall indirect effect was derived as the sum of these indirect effects and the proportion mediated derived as a ratio of the indirect effect to the total effect (the sum of the direct and indirect effects).
Figure 1. Phenotypic factor mediation model in males and females.
Note. Path diagram depicting mediation relationships between Sexual Orientation (SO), Psychosocial Adversity (PSA), SU (Substance Use) and Lifetime Sexual Partners (LSP) latent factors with standardized path coefficients. Factors were scaled by fixing one loading per factor to 1. SO = Sexual orientation, Dep = Depressive symptoms, Anx = Generalized anxiety symptoms, Alc = Alcohol Use, Can = Cannabis use, Drg = Other illicit drug use, ELA = Early-life adversity, IPV = Intimate partner violence. e1 – e7 = residual variances for corresponding indicator variables. Solid lines indicate significant paths while dotted lines indicate nonsignificant paths.
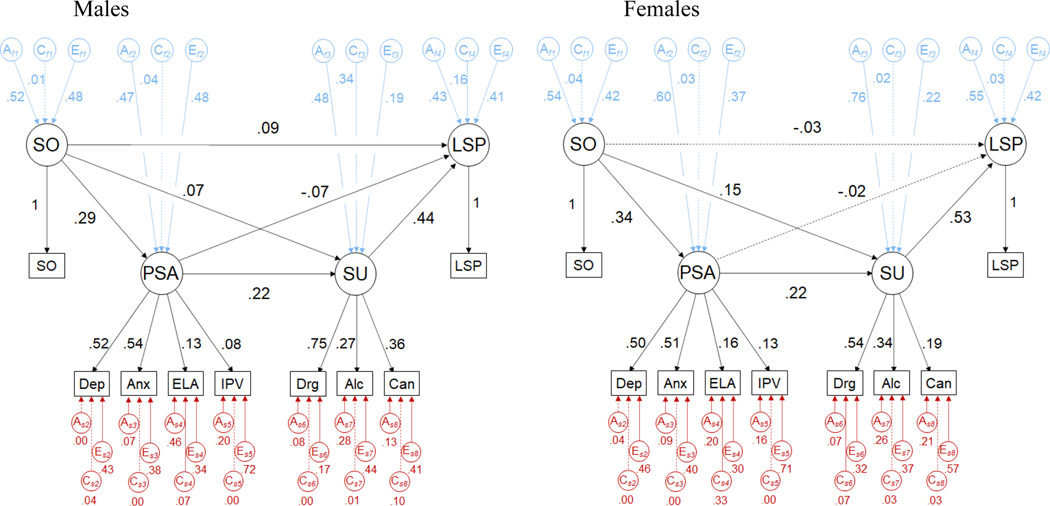
Three genetic factor models were specified and compared to determine the best explanation for the genetic and environmental influences on the relationships between the latent factors. A Cholesky decomposition (Genetic Model 1; Supplementary Figure S2b) tested whether the mediation relationships could be explained completely in terms of covariances between the ACE influences without mediation paths. The second model, the common-factor independent pathway model (CFIP, Genetic Model 2; Supplementary Figure S2b) tested whether the factor relationships were completely due to pleiotropic genetic and environmental effects without mediation paths. In the third model, the biometric mediation model (Genetic Model 3, Figure 2), ACE components and mediation paths were specified; allowing comparison with other genetic models to test for confounding of the mediation paths by ACE influences (Rosenström et al., 2019). Model selection for best fit for nested models was based on likelihood ratio testing using chi squared values and degrees of freedom while AIC and BIC were used for non-nested models (Kline, 2016).
Figure 2. Biometric mediation model in males and females.
Note. Path diagrams depicting mediation relationships between Sexual Orientation (SO), Psychosocial adversity (PSA), Substance use (SU) and Lifetime Sexual Partners (LSP) latent factors, standardized variance component influences on latent factors and standardized path coefficients. Factors were scaled by fixing one loading per factor to 1. SO = Sexual orientation, Dep = Depressive symptoms, Anx = Generalized anxiety symptoms, ELA = Early-life adversity, IPV = Intimate partner violence, Drg = Other illicit drug use, Alc = Alcohol Use, Can = Cannabis use. Af1-Af4, Cf1-Cf4 and Ef1-Ef4 = Factor-specific additive genetic and shared and individual-specific environmental influences respectively (in blue). As2-As8, Cs2-Cs8 and Es2-Es8 = Variable-specific additive genetic, shared and individual-specific environmental influences respectively (in red). Solid lines indicate significant paths while dotted lines indicate nonsignificant paths.
Sex differences and secondary analyses
Sex differences were investigated by comparing change in model fit when the parameters were freed to differ by sex and then constrained to be equal across sex. To ensure that similar constructs were being investigated in males and females, configural, metric, scalar and residual measurement invariance were investigated in the phenotypic mediation model with at least partial metric invariance required for valid group comparisons (Vandenberg & Lance, 2000). To replicate findings from the previous study (Oginni et al., 2020), secondary analyses were carried out using a reduced factor structure in which we modelled a single mediator factor indicated by depressive and anxiety symptoms, and alcohol and tobacco use problems.
The present study was pre-registered (https://osf.io/24bc6/) and we departed from the proposed analyses by excluding tobacco smoking because its correlations with the other variables was close to zero, and by specifying two mediator factors rather than one. However, all other analyses, including tests for sex differences, were as stated in the pre-registered analyses.
Results
Descriptive statistics, and phenotypic and genetic correlations
The majority (80.9%) of the sample identified as heterosexual with female participants being significantly more likely to identify as non-heterosexual (i.e. mostly heterosexual through exclusively gay/lesbian, Table 1), have higher median depressive and generalized anxiety symptom scores; while male participants had higher median alcohol use problem and intimate partner violence scores.
Table 1.
Descriptive statistics of observed variables and sex comparisons
| Variable | Total | Male | Female | Coef (95% CI)/ Statistic |
|||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Sexual orientation [n (%)] | |||||||
| Exclusively Heterosexual | 7306 | (80.9) | 2888 | (84.7) | 4418 | (78.6) | −0.34 (−0.45, −0.22)‡ |
| Mostly Heterosexual | 1040 | (11.5) | 213 | (6.3) | 827 | (14.7) | |
| Bisexual | 182 | (2.0) | 34 | (1.0) | 148 | (2.6) | |
| Mostly Gay/Lesbian | 175 | (1.9) | 62 | (1.8) | 113 | (2.0) | |
| Exclusively Gay/Lesbian | 327 | (3.6) | 211 | (6.2) | 116 | (2.1) | |
| Depressive symptoms [Median (Range)] |
3 | (0–16) | 3 | (0–16) | 4 | (0–16) | 12.20†*** |
| Generalized anxiety symptoms [Median (Range)] |
5 | (0–40) | 4 | (0–40) | 6 | (0–40) | 16.24†*** |
| Early-life adversities [Median (Range)] |
4 | (0–32) | 4 | (0–32) | 4 | (0–32) | −2.77†* |
| Intimate partner violence [Median (Range)] |
8 | (6–30) | 9 | (6–30) | 8 | (6–30) | −3.57†*** |
| Other illicit drug use [Median (Range)] |
0 | (0–28) | 0 | (0–28) | 0 | (0–24) | −9.24†*** |
| Alcohol use problems [Median (Range)] |
6 | (0–36) | 7 | (0–36) | 5 | (0–36) | −10.86†*** |
| Cannabis use [Median (Range)] |
0 | (0–21) | 0 | (0–21) | 0 | (0–21) | −10.57†*** |
| Lifetime sexual partners [n (%)] | |||||||
| 0 | 1338 | (15.4) | 550 | (16.7) | 788 | (14.6) | −0.01 (−0.07, 0.06)‡‡ |
| 1 | 1617 | (18.6) | 574 | (17.5) | 1043 | (19.3) | |
| 2–3 | 2037 | (23.4) | 799 | (24.3) | 1238 | (22.9) | |
| 4–7 | 1845 | (21.2) | 628 | (19.1) | 1217 | (22.5) | |
| 8–14 | 1157 | (13.3) | 420 | (12.8) | 737 | (13.6) | |
| >14 | 704 | (8.1) | 319 | (9.7) | 385 | (7.1) | |
Coef – Regression coefficient, 95% CI – 95% confidence intervals,
Unstandardized ordinal logistic regression coefficient and 95% CIs,
Wilcoxon Signed rank test (Mann-Whitney U),
Unstandardized linear regression coefficient with 95% CIs.
p<0.001,
p<0.05
The within-person correlations among the observed variables and the latent factors were positive (Supplementary Tables S3 and S4). Specifically, non-heterosexuality was associated with increased psychosocial adversity (r = 0.33, 95% CI: 0.29–0.36), substance use (r = 0.17, 95% CI: 0.14–0.21) and lifetime sexual partners (r = 0.11, 95% CI: 0.08–0.14) while psychosocial adversity and substance use were significantly associated with greater lifetime sexual partners (r = 0.10, 95% CI: 0.08–0.13 and r = 0.46, 95% CI: 0.44–0.49 respectively). Sex differences in the factor correlations were significant (χ2[36] = 90.2, p<0.001) and driven by higher correlations of substance use with sexual orientation and lifetime sexual partners in females and a higher correlation between sexual orientation and lifetime sexual partners in males compared to females (Table 2).
Table 2.
Factor correlations and standardized variance component influences on latent factors (first genetic model - Cholesky decomposition) in male and female twins and 95% confidence intervals
| Males | Females | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 1. | 2. | 3. | 4. | 1. | 2. | 3. | 4. | |
| Factor correlation |
||||||||
| 1. Sexual orientation | 1.00 | 1.00 | ||||||
| 2. Psychosocial adversity | .30 (.23, .35) | 1.00 | .35 (.31, .40) | 1.00 | ||||
| 3. Substance use | .13 (.07, .19) | .26 (.21, .31) | 1.00 | .24 (.19, .28) | .28 (.24, .32) | 1.00 | ||
| 4. Lifetime sexual partners | .13 (.08, .18) | .07 (.03, .11) | .43 (.39, .47) | 1.00 | .09 (.05, .12) | .12 (.09, .16) | .54 (.51, .57) | 1.00 |
|
| ||||||||
| Standardized variance component influences on factors | ||||||||
| h2 | .39 (.02, .61) | .39 (.16, .59) | .48 (.29, .70) | .45 (.27, .61) | .53 (.31, .63) | .62 (.37, .71) | .60 (.41, .74) | .47 (.35, .60) |
| c2 | .13 (.00, .45) | .09 (.00, .28) | .33 (.13, .50) | .15 (.01, .30) | .02 (.00, .21) | .03 (.00, .24) | .15 (.04, .31) | .11 (.00, .22) |
| e2 | .48 (.36, .63) | .52 (.40, .63) | .19 (.14, .25) | .40 (.35, .46) | .45 (.37, .53) | .35 (.29, .42) | .25 (.19, .32) | .42 (.38, .46) |
|
| ||||||||
| Variables | Standardized factor loadings |
As | Cs | Es | Standardized factor loadings |
As | Cs | Es |
|
| ||||||||
| Sexual orientation | 1.00 | 1.00 | ||||||
| Depressive symptoms | .52 (.47, .58) | .00 (.00, .10) | .05 (.00, .10) | .43 (.37, .49) | .50 (.47, .54) | .03 (.03, .08) | .00 (.00, .06) | .46 (.42, .51) |
| Anxiety symptoms | .54 (.49, .60) | .08 (.00, .14) | .00 (.00, .07) | .38 (.32, .44) | .51 (.48, .55) | .09 (.02, .13) | .00 (.00, .05) | .40 (.35, .44) |
| ELA | .13 (.11, .16) | .46 (.10, .54) | .06 (.02, .39) | .34 (.29, .40) | .16 (.14, .19) | .20 (.09, .31) | .33 (.23, .42) | .30 (.27, .34) |
| IPV | .08 (.06, .10) | .20 (.06, .28) | .00 (.00, .11) | .72 (.65, .79) | .14 (.11, .16) | .16 (.06, .21) | .00 (.00, .08) | .71 (.66, .76) |
| Other illicit drug use | .76 (.71, .82) | .09 (.02, .16) | .01 (.01, .05) | .14 (.10, .19) | .52 (.48, .57) | .07 (.00, .18) | .08 (.00, .17) | .32 (.27, .36) |
| Alcohol use | .27 (.24, .31) | .28 (.13, .34) | .01 (.00, .14) | .44 (.38, .50) | .34 (.31, .38) | .27 (.15, .34) | .02 (.00, .13) | .36 (.32, .40) |
| Cannabis use | .37 (.33, .40) | .13 (.00, .25) | .10 (.02, .21) | .41 (.34, .48) | .19 (.17, .22) | .20 (.10, .28) | .03 (.00, .11) | .57 (.52, .63) |
| Lifetime sexual partners | 1.00 | 1.00 | ||||||
Note. ELA = Early-Life Adversity, IPV = Intimate Partner Violence.
h2, c2, e2 = Standardized proportions contributed by additive genetic, shared and unique environmental factors, respectively to the variable variances (diagonals) and their covariances (off-diagonals).
As, Cs and Es = Standardized variable-specific additive genetic, shared and individual-specific influences.
Additive genetic and individual-specific environmental influences were significant for all the latent factors with the additive genetic influences ranging between 39% and 62% (95% CIs: 0.02–0.61 and 0.37–0.71; for sexual orientation in males and substance use in females respectively, Table 2), while individual-specific environmental influences ranged between 19% and 45% (95% CIs: 0.14–0.25 and 0.37–0.53; for substance use in males and sexual orientation in females respectively). Sex differences in the etiological influences on the latent factors were significant (χ2[30] = 350.62; p<0.001): additive genetic influences were larger in females while the shared environmental influences on sexual orientation and substance use were larger in males (Table 2).
Phenotypic and biometric mediation models
In the sample as a whole, the association between sexual orientation and lifetime sexual partners was partly mediated by two paths: (1) a single mediation path whereby non-heterosexuality was associated with increased substance use (standardized coefficient: 0.11, 95% CI: 0.07–0.12) which was in turn associated with more lifetime sexual partners (standardized coefficient: 0.45, 95% CI: 0.42–0.45), and (2) a two-course mediation path whereby non-heterosexuality was associated with increased psychosocial adversity (standardized coefficient: 0.32, 95% CI: 0.29–0.33) which was in turn associated with increased substance use (standardized coefficient: 0.17, 95% CI: 0.17–0.18) which was then associated with increased lifetime sexual partners (Supplementary Table S6, Figure S1). Both paths jointly explained 67.3% (95% CI: 0.49–0.95) of the association between sexual orientation of lifetime sexual partners.
Sex differences were significant (χ2[6] = 151.2, p<0.001) whereby these two mediation paths completely mediated the association between sexual orientation and lifetime sexual partners in females while in males, an additional path through psychosocial adversity was significant with the proportion mediated being smaller (31.1%, Figure 1, Supplementary Table S7). The factor constructs were comparable in male and female participants based on full configural invariance, partial metric invariance (χ2[2] = 1.34, p = 0.51), partial scalar invariance (χ2[2] = 3.23, p = 0.20) and partial residual invariance (χ2[1] = 0.82, p = 0.37, Supplementary Table S5; Vandenberg & Lance, 2000).
Of the three fitted genetic factor models, the biometric mediation model had the lowest AIC and BIC (86401.55 and −427381 respectively) compared to those for the Cholesky (86412.43 and −427290 respectively) and the common factor-independent pathway models (86436.70 and −427306 respectively, Supplementary Table S8). This indicates that the genetic and environmental influences on the relationships between the latent factors may be best explained as being transmitted through the mediation paths i.e., the mediation paths between sexual orientation, psychosocial adversity, substance use and lifetime sexual partners are not confounded by shared genetic and environmental influences. Model selection was also consistent with that from the secondary analyses using the simplified measurement model (Supplementary Table S8).
The mediation path coefficients in the biometric mediation model remained consistent with those in the phenotypic mediation model (Figures S1 and S3) and the latent factors were predominantly influenced by additive genetic and individual-specific environmental influences. Sex differences were significant (χ2[18] = 312.62, p < 0.001) such that in addition to the differences in the mediation paths previously described, shared environmental influences on substance use and lifetime sexual partners were larger in males (0.34, 95% CI: 0.31–0.51, and 0.16, 95% CI: 0.16–0.30, respectively) compared to females (0.02 and 0.03, 95% CIs: 0.00–0.03 and 0.00–0.12 respectively) while additive genetic influences on psychosocial adversity, substance use and lifetime sexual partners were larger in females (0.60, 0.76 and 0.55, 95% CIs: 0.41–0.68, 0.76–0.81 and 0.45–0.60 respectively) compared to males (0.47, 0.48 and 0.43, 95% CIs: 0.18–0.60, 0.28–0.47 and 0.26–0.55 respectively; Figure 2, Supplementary Table S12).
Discussion
Consistent with previous literature, non-heterosexuality was associated with increased risky sexual behavior indicated by lifetime sexual partners in the present study (Bränström & Pachankis, 2018; Charlton et al., 2011), psychosocial adversity (depressive and anxiety symptoms, early-life adversities and intimate partner violence) and substance use (King et al., 2008; Roberts et al., 2012; Rollè et al., 2018). Using a reduced factor structure, we replicated the finding from a previous study (Oginni et al., 2020) whereby mental health indicators partly mediated increased risky sexual behavior among sexual minority men and women. Our findings demonstrated that two mediation paths, through a separate substance use factor and in combination with increased psychosocial adversity, explained a larger proportion of the higher lifetime sexual partners among sexual minorities, especially women. Possible explanations for these indirect effects include higher substance use by sexual minority individuals as a direct consequence of minority stress (Hatzenbuehler, 2009) or to manage increased distress from minority-related psychosocial adversity (Turner et al, 2018); with substance use in turn increasing sexual risk-taking by impairing judgement or lowering inhibitions (McKirnan et al., 1996). After accounting for substance use among men, psychosocial adversity was associated with lower lifetime sexual partners and may be explained by the lower sexual interest associated with anxiety and depressive disorders (Laurent & Simons, 2009). Furthermore, the proportion of the association between sexual minority status and lifetime sexual partners mediated by substance use and psychosocial adversity was smaller in males compared to females. This highlights the need to further investigate additional biopsychosocial mechanisms for increased risky sexual behavior among sexual minority men.
Further genetic analyses showed that although sexual minority status, psychosocial adversity, substance use and lifetime sexual partners, and their associations with each other appeared to be influenced by latent genetic and environmental factors (Ganna et al., 2019; Zietsch et al., 2010; Zietsch et al., 2012); as previously demonstrated (Oginni et al., 2020), the mediation paths were not confounded by overlapping effects of these factors. These genetic and environmental influences are thus better understood as being transmitted through the mediation paths rather than as pleiotropic (i.e., direct independent) genetic and/or environmental effects.
We further found that the genetic influences on psychosocial adversity, substance use and lifetime sexual partners were larger in females compared to males while the shared environmental influences on substance use and lifetime sexual partners were larger in males. Sex differences in etiological influences on lifetime sexual partners were consistent with those in our previous study (Oginni et al., 2020), and raise the possibility that men and women differ in the extents to which the environment may shape their social (including sexual) behavior. Specifically, the larger shared environmental influences on lifetime sexual partners and substance use among male compared to female participants suggest that the impact of the home environment on these behaviors is larger in men compared to women.
Implications
Interventions to improve sexual health among sexual minorities should target eliminating psychosocial disadvantage and substance use disparities among sexual minorities, since the present study suggests these disparities are not genetic in nature. However, based on the independent negative association between psychosocial adversity and lifetime sexual partners in sexual minority men, these interventions need to specifically target sexual health in men to prevent a paradoxical increase in risky sexual behavior as psychosocial adversity reduces. As psychosocial and substance use disparities have been shown to reflect consequences of minority stress (Hatzenbuehler, 2009; Meyer, 2013), ongoing structural and societal-level efforts to discrimination based on sexual orientation should be reinforced. These efforts include decriminalization and depathologization same-sex attraction including banning sexual orientation change efforts, enacting anti-discrimination laws and policies, legalizing same-sex marriage, increased representation in media and politics, and increased access to affirming support in health and educational institutions (Russell & Fish, 2016). Our finding that these indirect pathways are independent of shared genetic and/or environmental influences further underline the utility of targeting these pathways for preventive interventions and extending these strategies to less tolerant environments. Considering that the psychosocial adversities in the present study include those occurring in early-life, these interventions should be begun as early as possible.
Strengths and limitations
The strengths of the present study include the use of recent data from a large population-based twin cohort and the comparison of monozygotic and dizygotic twins to exclude confounding by unmeasured genetic and environmental influences. Our findings also replicate and extend those from our earlier work (Oginni et al., 2020), indicating the validity of findings from both studies; however, the following limitations should be considered. The cross-sectional nature of the data precludes causal inference; however, our model specification was consistent with theory (Hatzenbuehler, 2009; Meyer, 2013; Stall et al., 2003) and prospective findings (Oginni et al., 2019; Pesola et al., 2014). Although the TEDS cohort is representative of the British population (Rimfeld et al., 2019), the underrepresentation of ethnic minorities may limit the generalizability of our findings. Relatedly, the genetic and environmental variance component influences as estimated by the classical twin design are time- and population-specific; thus, replications among non-Caucasian twin samples will provide further external validation. Furthermore, as gender identity was not assessed in the study sample; the mediation relationships could not be investigated among trans- and/or non-binary individuals. Finally, higher lifetime sexual partners alone may not necessarily indicate sexual risk as safe sex practices can be carried out with multiple partners. However, our use is consistent with evidence that multiple sexual partners, a recommended indicator of HIV-risk behavior among young people (Slaymaker, 2004), is significantly associated with other sexual risk behaviors (Cabecinha et al., 2017).
Supplementary Material
Acknowledgments
The Twins Early Development Study (TEDS) is supported by a program grant to Professor Robert Plomin from the UK Medical Research Council (MR/M021475/1 and previously G0901245), with additional support from the US National Institutes of Health (AG046938). We gratefully acknowledge the ongoing contribution of the participants in the TEDS and their families. OAO is supported by the Commonwealth Scholarship, a global scholarship programme funded by the Foreign and Commonwealth Office, United Kingdom. PJ is funded by grants no. 274521, 284385 and 319403 from the Academy of Finland.
Footnotes
We have no conflicts of interest to disclose.
“Biometric” indicates that the genetic and environmental influences are determined statistically based on similarities between monozygotic and dizygotic twins. This contrasts with genomic methods in which DNA samples are processed and specific genetic variants identified.
References
- Angold A, Costello EJ, Messer SC, Pickles A, Winder F, & Silver D. (1995). Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research 5, 237–249. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, & Monteiro MG. (2001). AUDIT. The alcohol use disorders identification test: Guidelines for use in primary health care. Geneva: World Health Organization. [Google Scholar]
- Basile KC, Hertz MF, & Back SE. (2007). Intimate partner violence and sexual violence victimization assessment instruments for use in healthcare settings: Version 1. Atlanta: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. 10.1037/e410572008-001 [DOI] [Google Scholar]
- Bränström R, & Pachankis JE. (2018). Validating the syndemic threat surrounding sexual minority men’s health in a population-based study with national registry linkage and a heterosexual comparison. Journal of Acquired Immune Deficiency Syndromes 78, 376–382. 10.1097/QAI.0000000000001697 [DOI] [PubMed] [Google Scholar]
- Cabecinha M, Mercer CH, Gravningen K, Aicken C, Jones KG, Tanton C, Wellings K, Sonnenberg P, & Field N. (2017). Finding sexual partners online: prevalence and associations with sexual behaviour, STI diagnoses and other sexual health outcomes in the British population. Sexually Transmitted Infections 93, 572–582. 10.1136/sextrans-2016-052994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlton BM, Corliss HL, Missmer SA, Frazier AL, Rosario M, Kahn JA, & Austin SB. (2011). Reproductive health screening disparities and sexual orientation in a cohort study of US adolescent and young adult females. Journal of Adolescent Health 49, 505–510. 10.1016/j.jadohealth.2011.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske M, Wittchen U, Bogels S, Stein M, Andrews G, & Lebeu R. (2013). Severity measure for Generalized Anxiety Disorder-adult. Educational resources: Online assessment measures. Retrieved from https://www.psychiatry.org/psychiatrists/practice/dsm/educational-resources/assessmentmeasures [Google Scholar]
- Ganna A, Verweij KJ, Nivard MG, Maier R, Wedow R, Busch AS, Abdellaoui A, Guo S, Sathirapongsasuti JF, 23andMe Research Team, Lichtenstein P, Lundström S, Långström N, Auton A, Harris KM, Beecham GW, Martin ER, Sanders AR, Perry JRB, . . . Zietsch BP. (2019). Large-scale GWAS reveals insights into the genetic architecture of same-sex sexual behavior. Science 365, eaat7693. 10.1126/science.aat7693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Moeller RW, Siconolfi DE, Storholm ED, Solomon TM, & Bub KL. (2013). Measurement model exploring a syndemic in emerging adult gay and bisexual men. AIDS and Behavior 17, 662–673. 10.1007/s10461-012-0273-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML. (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin 135, 707–730. 10.1037/a0016441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, & Nazareth I. (2008). A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry 8, 70. 10.1186/1471-244X-8-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. (2016). Principles and practice of structural equation modeling, 4th Edn. New York: The Guilford Press. [Google Scholar]
- Laurent SM & Simons AD. (2009). Sexual dysfunction in depression and anxiety: conceptualizing sexual dysfunction as part of an internalizing dimension. Clinical Psychology Review 29, 573–585. 10.1016/j.cpr.2009.06.007 [DOI] [PubMed] [Google Scholar]
- Legleye S, Karila L, Beck F, & Reynaud M. (2007). Validation of the CAST, a general population Cannabis Abuse Screening Test. Journal of Substance Use 12, 233–242. 10.1080/14659890701476532 [DOI] [Google Scholar]
- McGue M, & Bouchard TJ. (1984). Adjustment of twin data for the effects of age and sex. Behavior Genetics, 14, 325–343. 10.1007/BF01080045 [DOI] [PubMed] [Google Scholar]
- McKirnan DJ, Ostrow DG, & Hope B. (1996). Sex, drugs and escape: A psychological model of HIV-risk sexual behaviours. AIDS Care 8, 655–670. 10.1080/09540129650125371 [DOI] [PubMed] [Google Scholar]
- Meyer IH. (2013). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychology of Sexual Orientation and Gender Diversity 1, 3–26. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neale MC, Hunter MD, Pritikin JN, Zahery M, Brick TR, Kirkpatrick RM, Estabrool R, Bates TC, Maes HH, & Boker SM. (2016). OpenMx 2.0: Extended structural equation and statistical modeling. Psychometrika 81, 535–549. 10.1007/s11336-014-9435-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oginni O, Robinson E, Jones A, Rahman Q, & Rimes K. (2019). Mediators of increased self-harm and suicidal ideation in sexual minority youth: a longitudinal study. Psychological Medicine 49, 2524–2532. 10.1017/S003329171800346X [DOI] [PubMed] [Google Scholar]
- Oginni OA, Jern P, & Rijsdijk FV. (2020). Mental Health Disparities Mediating Increased Risky Sexual Behavior in Sexual Minorities: A Twin Approach. Archives of Sexual Behavior 49, 2497–2510. 10.1007/s10508-020-01696-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penke L, & Asendorpf JB. (2008). Beyond global sociosexual orientations: a more differentiated look at sociosexuality and its effects on courtship and romantic relationships. Journal of Personality and Social Psychology 95, 1113–1135. 10.1037/0022-3514.95.5.1113 [DOI] [PubMed] [Google Scholar]
- Pesola F, Shelton KH, & van den Bree MB. (2014). Sexual orientation and alcohol problem use among UK adolescents: an indirect link through depressed mood. Addiction 109, 1072–1080. 10.1111/add.12528 [DOI] [PubMed] [Google Scholar]
- Price TS, Freeman B, Craig I, Petrill SA, Ebersole L, & Plomin R. (2000). Infant zygosity can be assigned by parental report questionnaire data. Twin Research and Human Genetics 3, 129–133. 10.1375/136905200320565391 [DOI] [PubMed] [Google Scholar]
- Rijsdijk FV, & Sham PC. (2002). Analytic approaches to twin data using structural equation models. Briefings in Bioinformatics 3, 119–133. 10.1093/bib/3.2.119 [DOI] [PubMed] [Google Scholar]
- Rimfeld K, Malanchini M, Spargo T, Spickernell G, Selzam S, McMillan A, Dale PS, Eley TC, & Plomin R. (2019). Twins early development study: A genetically sensitive investigation into behavioral and cognitive development from infancy to emerging adulthood. Twin Research and Human Genetics, 22, 508–513. 10.1017/thg.2019.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AL, Rosario M, Corliss HL, Koenen KC, & Austin SB. (2012). Elevated risk of posttraumatic stress in sexual minority youths: Mediation by childhood abuse and gender nonconformity. American Journal of Public Health 102, 1587–1593. 10.2105/AJPH.2011.300530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollè L, Giardina G, Caldarera AM, Gerino E, & Brustia P. (2018). When intimate partner violence meets same sex couples: A review of same sex intimate partner violence. Frontiers in Psychology 9, 1506. 10.3389/fpsyg.2018.01506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenström T, Czajkowski NO, Ystrom E, Krueger RF, Aggen SH, Gillespie NA, Eilertsen E, Reichborn-Kjennerud T, & Torvik FA. (2019). Genetically informative mediation modeling applied to stressors and personality-disorder traits in etiology of alcohol use disorder. Behavior Genetics 49, 11–23. 10.1007/s10519-018-9941-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell ST, & Fish JN. (2016). Mental health in lesbian, gay, bisexual, and transgender (LGBT) youth. Annual Review of Clinical Psychology, 12, 465–487. 10.1146/annurev-clinpsy-021815-093153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slaymaker E. (2004). A critique of international indicators of sexual risk behaviour. Sexually Transmitted Infections 80, ii13–ii21. 10.1136/sti.2004.011635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, Pollack L, Binson D, Osmond D, & Catania JA. (2003). Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health 93, 939–942. 10.2105/ajph.93.6.939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, & Burns BF. (2015). Syndemics of psychosocial problems and HIV risk: A systematic review of empirical tests of the disease interaction concept. Social Science and Medicine 139, 26–35. 10.1016/j.socscimed.2015.06.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner S, Mota N, Bolton J, & Sareen J. (2018). Self-medication with alcohol or drugs for mood and anxiety disorders: A narrative review of the epidemiological literature. Depression and Anxiety 35, 851–860. 10.1002/da.22771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenberg RJ, & Lance CE. (2000). A review and synthesis of the measurement invariance literature: Suggestions, practices, and recommendations for organizational research. Organizational Research Methods 3, 4–70. 10.1177/109442810031002 [DOI] [Google Scholar]
- Xu W, Zheng L, Xu Y, & Zheng Y. (2017). Internalized homophobia, mental health, sexual behaviors, and outness of gay/bisexual men from Southwest China. International Journal for Equity in Health 16, 36. 10.1177/109442810031002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zietsch B, Verweij K, Bailey J, Wright M, & Martin N. (2010). Genetic and environmental influences on risky sexual behaviour and its relationship with personality. Behavior Genetics 40, 12–21. 10.1007/s10519-009-9300-1 [DOI] [PubMed] [Google Scholar]
- Zietsch BP, Verweij KJ, Heath AC, Madden PA, Martin NG, Nelson EC, & Lynskey MT. (2012). Do shared etiological factors contribute to the relationship between sexual orientation and depression? Psychological Medicine, 42, 521–532. 10.1017/S0033291711001577 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.