Abstract
Objective:
Examine the factors that influence a patient’s likelihood of participating in clinical pharmacy services so that pharmacists can use this knowledge to effectively expand clinical services.
Methods:
An online survey was distributed to U.S. citizens 55 years of age or older through a market research company. The survey assessed pharmacy and medication use, general health, interest in clinical pharmacy services, and general demographics. The specific clinical services examined included medication therapy management (MTM) and a collaborative practice agreement (CPA). Logistic regression and best-worst scaling were used to predict the likelihood of participating and determine the motivating factors to participate in clinical pharmacy services, respectively.
Results:
Two hundred eight (58.45%) respondents reported being likely to participate in MTM services, and 108 (50.6%) reported being likely to participate in the services offered by a pharmacist with a CPA, if offered. The motivations to participate in MTM were driven by pharmacist management of medication interactions and adverse effects (best-worst scores 0.62 and 0.51, respectively). The primary motivator to participate in a CPA was improved physician-pharmacist coordination (best-worst score 0.80). Those with a personal pharmacist were more likely to participate in MTM (odds ratio [OR] 2.43 [95% CI 1.41–4.22], P = 0.002) and a pharmacist CPA (2.08 [1.26–3.44], P = 0.004). Previous experience with MTM increased the likelihood of participating again in MTM (5.98 [95% CI 2.50–14.35], P < 0.001). Patient satisfaction with the pharmacy increased the likelihood of participating in a pharmacist CPA (1.47 [95% CI 1.01–2.13], P = 0.04).
Conclusion:
Patients are interested in clinical pharmacy services for the purposes of medication interaction management, adverse effect management, and improved physician-pharmacist coordination. The factors that influenced the likelihood of participating included having a personal pharmacist, previous experience with MTM, and pharmacy satisfaction. These results suggest a potential impact of the patient-pharmacist relationship on patient participation in clinical services.
Background
The Medicare Prescription Drug, Improvement, and Modernization Act mandated that Medicare Part D plan sponsors design medication therapy management (MTM) programs for their beneficiaries. MTM programs aim to optimize therapeutic outcomes and reduce adverse events for eligible beneficiaries.1,2 The eligibility criteria for MTM services are set annually by the Centers for Medicare & Medicaid Services (CMS) and include a minimum number of multiple chronic diseases, number of medications, and annual drug-cost threshold.3 Since 2006, MTM services have grown and transformed under the guidance of CMS. The minimum level of MTM services provided by Part D plan sponsors for MTM enrollees includes an annual comprehensive medication review (CMR), quarterly targeted medication reviews, and interventions for both beneficiaries and prescribers.3
An annual CMR, usually provided by a pharmacist, includes an assessment of a patient’s medications to identify medication-related problems; development of a plan to resolve the problems with the patient, caregiver, and prescriber; and provision of medication-related education to improve patient disease self-management.3 Previous research has demonstrated economic advantages and improved clinical outcomes when MTM services were provided. Favorable outcomes have been observed among a variety of disease states, including hypertension, dyslipidemia, diabetes, and asthma.4–9 The provision of additional clinical services may also be provided in the setting of a pharmacist collaborative practice agreement (CPA). A CPA is a formal agreement and protocol between a pharmacist and a licensed provider. Generally, in a CPA the provider diagnoses and supervises patient care, and refers the patient to a pharmacist for specified patient care activities.10 Several successful pharmacist-based services provided through a CPA have been reported on, and include management of group A streptococcus, influenza, and hepatitis C infections.11–13 In addition, a pharmacist-led antimicrobial stewardship program has been shown to improve guideline-based antimicrobial prescribing in an urgent care setting.14
As pharmacy continues its transition to provision of direct patient-centered care and clinical services, patients’ perception of pharmacists is evolving. One pilot study conducted in Louisiana indicated that most of the participants surveyed perceived their pharmacists to be health care providers, and this had an impact on their willingness to participate in pharmacist-provided services.15 However, there is limited information on the perception of patients regarding clinical services performed by pharmacists in a nationally representative sample. Most of the information currently available focuses on Medicare beneficiaries, and generally indicates unfamiliarity with these services. Historically, patient surveys indicated unfamiliarity with MTM, and the perception of the pharmacist’s role for many revolved around the dispensing function.16,17 However, the patient’s perception of the pharmacist role often changes once patients participate in MTM. Surveys of Medicare beneficiaries indicate that participants find the service beneficial, value information on how to use their medication, and that MTM improves their medication use.18,19
Despite the growing awareness of clinical pharmacy services and demonstrated benefit of these services, patient participation remains a challenge for service implementation.20–22 Since 2016, CMR completion rates for Medicare plans have been reported as a Medicare Star Rating. Medicare Star Ratings provide a score on a 5-point scale that indicates the quality of a plan and also determines a plan’s qualification for bonus federal payments. CMR completion rates remain lower than desired: in 2017, the average CMR completion rate was 71% for Medicare Advantage prescription drug plans (PDPs), and 38% for Medicare Part D PDPs.23 Previous studies have examined the reasons for declining MTM services. The common barriers include time required to participate, potential cost, concern that pharmacists’ recommendations would conflict with physicians’ plans, or patients’ belief that they did not need the service.15–17,21,24
Given these challenges, there is a current interest in elucidating the factors that influence patient interest in clinical pharmacy services. Previous studies have shown associations between an interest in MTM services and a variety of factors, including number of medications, medication-related problem, presence of chronic disease states, and poor health.16,22,25–29 The purpose of this study was to gain additional insight into patient perceptions of clinical pharmacy services provided in the pharmacy setting through a nationwide, Internet-based survey. Previous studies have focused on Medicare Part D members who have already participated in MTM services, or specific populations defined by place of employment or geographic location. Limited information exists regarding other patient populations, acceptance of clinical services provided by pharmacists beyond MTM alone, and the impact of the patient-pharmacist relationship on acceptance of clinical services.
Objectives
The primary objective of this study was to determine and prioritize patients’ specific motivations for seeking 2 clinical pharmacy services: MTM and expanded pharmacist care under a CPA. The secondary objectives were to determine the impact of patients’ geographic and demographic characteristics on acceptance of pharmacist services, and assess if pharmacy type or a patient-pharmacist relationship influences acceptance of pharmacist services.
Methods
An Internet-based survey (Appendix 1) was created by 2 investigators (L.S. and M.D.) and distributed to the survey participants through the market research company Survey Sampling International (SSI). The study participants were drawn from a panel of Internet users administered by SSI who voluntarily agreed to receive invitations to fill out the questionnaires. The SSI subject pool approximates the U.S. Census on education level, race, and income. Participants 55 years of age or older were eligible to receive a questionnaire invitation. An age of 55 years or older was selected to represent a large U.S. sample while maintaining the likelihood that the participants were on chronic pharmacologic therapy and had previous experience interacting with a pharmacist. The only exclusion criterion was not completing the entire survey. All participants who completed the survey received a small monetary reimbursement. The surveys were completed between August 15, 2017, and August 21, 2017, to reach a pre-specified 356 responses owing to financial constraints. This study was granted exempt status by the University of Michigan Institutional Review Board.
Survey components
The survey contained 28 items assessing medication and pharmacy use, general health, likelihood of participating in clinical pharmacy services, and motivations to seek such services, as well as general demographics. The survey was derived from relevant questions originating from published literature and questions of interest from the research team. The survey was piloted with a small sample of older adults and reviewed for feedback. The specific clinical pharmacy services assessed included MTM and expanded pharmacist roles under a CPA. MTM was described as a telephonic or in-person appointment where a pharmacist completes a medication review, addresses medication-related concerns, and works with the patient and physician to improve medication therapy outcomes. Pharmacist participation in a CPA was described as extended pharmacist roles, including ordering laboratory tests; refilling medications; and initiating, modifying, or discontinuing treatment when appropriate, per protocol, in collaboration with a physician. Details of the potential cost of the services, including insurance reimbursement, were not described to the survey participants for consideration.
Data analysis
Best-worst scaling (BWS) was used to determine the participants’ motivations to seek these clinical services.30–32 BWS is thought to overcome challenges related to ranking or rating scales. Ranking is limited to understanding extremes and the order of importance, not necessarily the strength (i.e., quantitative measure of how much 1 option is preferred over another). The results achieved with rating may not be effectively discriminating, and they also lack strength. By using BWS, the results can be analyzed in terms of the order and strength to better understand patient preference.30–33 The participants were asked to select the 1 most appealing and the 1 least appealing reason for participation in 1 of these services. All participants received the same BWS profile and the same set of attributes. See Appendix 2 for an example of BWS, and for the formula used to calculate the best-worst score. The number of times an item is chosen as the “worst” or least appealing is subtracted from the number of times an item is chosen as the “best” or most appealing across all patients. This value is then divided by the total number of times the item is voted on as “best” or “worst.” The final value for each item ranges from −1 to +1. The more positive the number, the more appealing the reason for participating in the service. The more negative the number, the less appealing the reason for participating in the service. The participants were shown the following options for MTM: free health service, chronic disease management, more information about a medication, adverse effect check and management, medication interaction check and management, creation of a medication schedule, potential cost savings, and doctor recommendation. The options for pharmacist services under a CPA were as follows: standard office co-pay for primary care visit with a pharmacist, chronic disease management, improved coordination between physicians and pharmacist, easier access to health care provider, more interactions with a pharmacist, and doctor recommendation. The participants could only choose 1 option as the “best” and 1 option as the “worst” in each question.
Data analysis was conducted using SAS version 9.4 (SAS Institute Inc). Chi-square analysis and Fisher exact test were used for categorical data where appropriate. Continuous data were analyzed with t test for normally distributed data and Wilcoxon rank-sum test for non-normal data. BWS data were prepared through aggregate statistics on Microsoft Excel (Microsoft Corporation) for MTM and CPA separately.15 A bivariate analysis was used initially to identify the factors associated with the likelihood of participating in clinical pharmacy services. Only variables in the bivariate analysis with a P-value < 0.1 were included in the final multivariable model using logistic regression. For the logistic models, the likelihood of participating in clinical services were dichotomized. Thus, the dependent variable in the logistic model for MTM was those likely to participate in MTM (i.e., very likely and somewhat likely) compared with those not likely (i.e., indifferent, somewhat unlikely, or very unlikely). Similarly, the logistic model for CPA was those likely to participate in CPA (i.e., very likely and somewhat likely) compared with those not likely (i.e., indifferent, somewhat unlikely, or very unlikely). The questions addressing previous experience with MTM or CMR were also dichotomized to those with previous experience compared with those without previous experience or not sure.
Results
Among the 356 responders to the questionnaire, 51.1% of the participants were women, 76.6% were Caucasian, and the average age was 63.8 ± 7.4 years. A total of 309 (86.8%) participants reported using a prescription medication within the past year, averaging 4.0 ± 3.1 prescriptions per month. Of those participants, 35.6% primarily used a large chain pharmacy, 14.3% used a pharmacy within a grocery store, 12.7% used a pharmacy within a department store, and 8.9% used an independent pharmacy. The respondents reported using their primary pharmacy for an average of 9.2 ± 9.1 years, and 65.4% indicated being extremely satisfied with their pharmacy. A total of 115 respondents (37.2%) indicated that they had at least 1 person that they considered their personal pharmacist (Table 1). See Appendix 3 for a figure that displays the location of survey respondents on the basis of coordinate data.
Table 1.
Participant demographic data
| Respondent characteristics | N = 356a |
|---|---|
| Female | 182 (51.1) |
| Average age, y | 63.8 ± 7.4 |
| Household income | |
| < $50,000 | 151 (42.4) |
| $50,000–$100,000 | 132 (37.1) |
| > $100,000 | 73 (20.5) |
| Employment status | |
| Employed | 155 (43.5) |
| Retired | 145 (40.7) |
| Unemployed | 56 (15.7) |
| Spanish, Hispanic, or Latino | 48 (13.5) |
| Race | |
| Caucasian | 265 (74.4) |
| Black | 46 (12.9) |
| Other | 35 (9.8) |
| Did not answer | 10 (2.8) |
| Education level | |
| ≤ GRE | 69 (19.4) |
| Some college, no degree | 96 (26.9) |
| College degree | 191 (53.6) |
| U.S. region | |
| Northeast | 68 (19.1) |
| Midwest | 77 (21.6) |
| South | 131 (36.8) |
| West | 80 (22.5) |
| Urban-rural region | |
| Urban | 323 (90.7) |
| Rural | 33 (9.3) |
| Health status | |
| Excellent | 42 (11.8) |
| Good | 176 (49.4) |
| Fair | 94 (26.4) |
| Poor | 44 (12.4) |
| Poor health affecting usual activities within the past month, Yes | 119 (33.4) |
| Days affected by poor health within the past month (n = 119) | 4.0 [2, 10] |
| Have used prescription medication within past year | 309 (86.8) |
| No. medications used in the past month (n = 309) | 3 [2, 5] |
| Type of pharmacy used (n = 309) | |
| Chain | 108 (35) |
| Grocery store | 44 (14.2) |
| Department store | 40 (12.9) |
| Independent pharmacy | 28 (9.1) |
| Other (e.g., VA, Internet, mail order) | 89 (28.8) |
| Total no. pharmacies used (n = 309) | 1.3 ± 1.0 |
| Years with primary pharmacy (n = 309) | 9.2 ± 9.1 |
| Satisfaction with primary pharmacy (n = 309) | |
| Extremely satisfied | 202 (65.4) |
| Somewhat satisfied | 90 (29.1) |
| Neither satisfied or dissatisfied | 9 (2.9) |
| Somewhat dissatisfied | 7 (2.3) |
| Extremely dissatisfied | 1 (0.3) |
| Have at least 1 person you consider your personal pharmacist (n = 309) | 115 (37.2) |
| Comfort level speaking with your pharmacist (n = 115) | |
| Extremely comfortable | 72 (62.6) |
| Somewhat comfortable | 38 (33.0) |
| Neither comfortable or uncomfortable | 5 (4.4) |
| Somewhat or extremely uncomfortable | 0 (0) |
| Previous MTM experience | 59 (16.6) |
| Previous pharmacist CPA experience | 33 (9.3) |
Abbreviations used: CPA, collaborative practice agreement; GRE, Graduate Record Examinations; VA, Veterans’ Administration pharmacy; MTM, medication medication therapy management.
Note: Continuous data reported as mean ± SD and median [Q1, Q3], categorical data reported as n (%).
Unless otherwise noted, reduced sample on questions is due to branching logic in the survey.
MTM
Two hundred eight (58.4%) respondents reported being likely to participate in MTM services, if offered. Figure 1 presents the results from the corresponding BWS analysis. The motivations to participate in MTM were driven by an interest in drug interaction management and adverse effect management (best-worst scores 0.62 and 0.51, respectively). The respondents were least likely to select chronic disease management and medication schedule assistance as motivating factors to participate in MTM services (best-worst scores −0.44 and −0.72, respectively).
Figure 1.
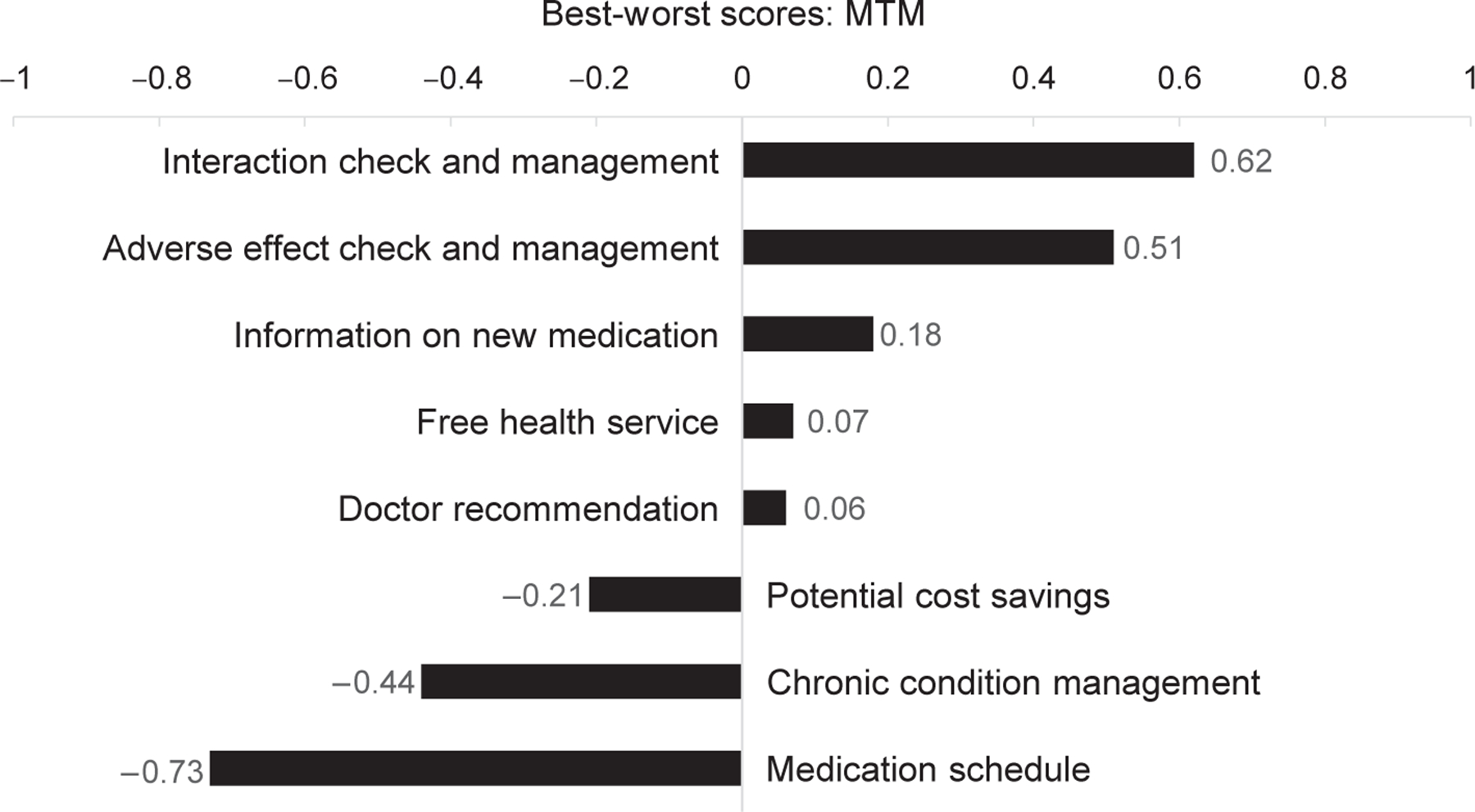
Best-worst scaling analysis for motivations to participate in medication therapy management. Positive values closer to 1 indicate factor more likely to be chosen as the most motivating. Negative values closer to −1 indicate factor more likely to be chosen as the least motivating. Abbreviation used: MTM, medication therapy management.
Table 2 presents the bivariate analysis of the factors associated with the likelihood of participating in MTM services. The respondents who stated that they have at least 1 person that they consider their personal pharmacist were significantly more likely to be interested in MTM services (likely 47.8% vs. indifferent or unlikely 22.5%, P < 0.001). Previous experience with MTM was also associated with a significant interest in participation (likely 25% vs. indifferent or unlikely 4.7%, P < 0.001). Education level, poor health affecting usual activities within the past month, number of prescriptions used in the past month, total number of pharmacies used, and satisfaction with their primary pharmacy were all significant on bivariate analysis. On multivariable analysis, some college education compared with having a college degree (odds ratio [OR] 2.04 [95% CI 1.08–3.84]), presence of a personal pharmacist (2.43 [95% CI 1.41–4.22]), and previous MTM experience (5.98 [95% CI 2.50–14.35]) remained statistically significant. See Figure 2 for a forest plot for the multivariable model.
Table 2.
Factors that influence the likelihood of participating in medication therapy management
| Variable | Likelya n (%) | Indifferent or unlikelyb n (%) | P-value (bivariate) |
|---|---|---|---|
| Female | 111 (53.4) | 71 (48.0) | 0.316 |
| Age | 62.3 ± 7.9 | 63.0 ± 7.3 | 0.364 |
| Race | |||
| Caucasian | 150 (73.9) | 115 (80.4) | 0.254 |
| Black | 32 (15.8) | 14 (9.8) | |
| Other | 21 (10.3) | 14 (9.8) | |
| Spanish, Hispanic, or Latino | 27 (13.0) | 21 (14.2) | 0.742 |
| Employment status | |||
| Employed | 113 (45.2) | 61 (41.2) | 0.303 |
| Retired | 78 (37.5) | 67 (45.3) | |
| Unemployed | 36 (17.3) | 20 (13.5) | |
| Education level | |||
| ≤ GRE | 41 (19.7) | 28 (18.9) | 0.036 |
| Some college, no degree | 66 (31.7) | 30 (20.3) | |
| College degree | 101 (48.6) | 90 (60.8) | |
| Household income | |||
| < $50,000 | 93 (44.7) | 58 (39.2) | 0.294 |
| $50,000–$100,000 | 78 (37.5) | 54 (36.5) | |
| > $100,000 | 37 (17.8) | 36 (24.3) | |
| U.S. region | |||
| Northeast | 42 (20.2) | 26 (17.6) | 0.853 |
| Midwest | 45 (21.6) | 32 (21.6) | |
| South | 73 (35.1) | 58 (39.2) | |
| West | 48 (23.1) | 32 (21.6) | |
| Urban-rural region | |||
| Urban | 188 (90.4) | 135 (91.2) | 0.790 |
| Rural | 20 (9.6) | 13 (8.8) | |
| Health status | |||
| Excellent | 23 (11.1) | 19 (12.8) | 0.166 |
| Good | 98 (47.1) | 78 (52.7) | |
| Fair | 64 (30.8) | 30 (20.3) | |
| Poor | 23 (11.1) | 21 (14.2) | |
| Poor health affecting usual activities within the past month, Yes | 79 (38.0) | 40 (27.0) | 0.031 |
| Days affected by poor health | 5 [2, 10] | 4 [3, 12] | 0.979 |
| No. prescriptions used in the past month | 3 [2, 5] | 2 [1, 5] | 0.004 |
| Primary pharmacy type | |||
| Chain | 60 (33.3) | 48 (37.2) | 0.727 |
| Grocery store | 24 (13.3) | 20 (15.5) | |
| Department store | 27 (15.0) | 13 (10.1) | |
| Independent pharmacy | 17 (9.4) | 11 (8.5) | |
| Other (e.g., VA, mail order) | 52 (28.9) | 37 (28.7) | |
| No. years using primary pharmacy | 7 [3, 15] | 5 [2, 10] | 0.137 |
| Total no. pharmacies used | 1 [1, 2] | 1 [1, 1] | 0.007 |
| Satisfaction with primary pharmacy | 4.7 ± 0.6 | 4.4 ± 0.8 | 0.006 |
| Presence of a personal pharmacist | 86 (47.8) | 29 (22.5) | < 0.001 |
| Previous MTM experience | 52 (25.0) | 7 (4.7) | < 0.001 |
Abbreviations used: MTM, medication therapy management; GRE, Graduate Record Examinations; VA, Veterans’ Administration pharmacy. Note: Continuous data reported as mean ± SD and median [Q1, Q3], categorical data reported as n (%).
Likely to participate included those who responded “very likely” and “somewhat likely.”
Indifferent/unlikely to participate included those who responded “indifferent,” “somewhat unlikely,” or “very unlikely.”
Figure 2.
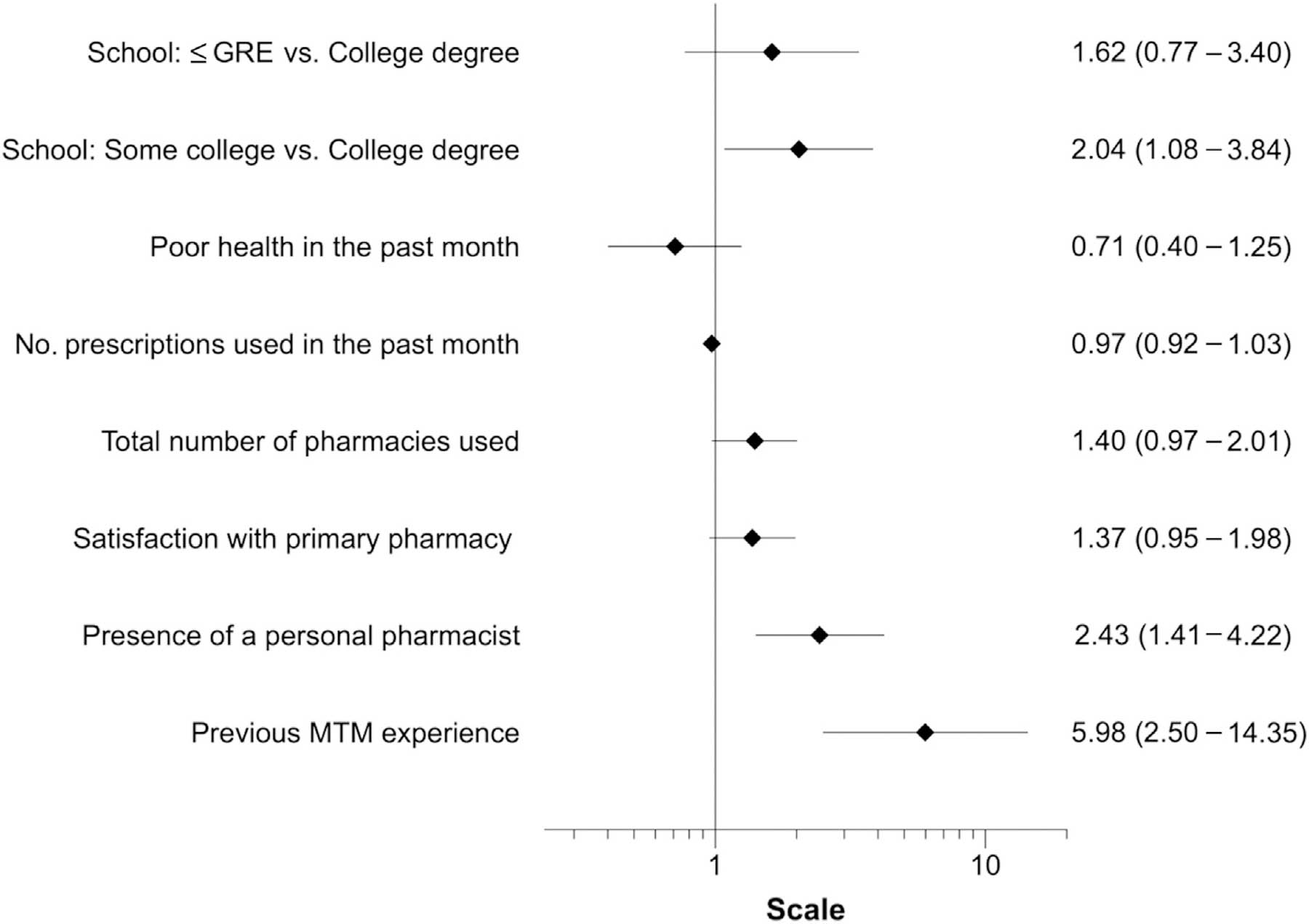
Multivariable analysis of the factors that influence the likelihood of participating in MTM. The dependent variable was participant likelihood of participating in the service; responses dichotomized to those likely to participate (i.e., very likely and somewhat likely) compared with those not likely (i.e., indifferent, somewhat unlikely, or very unlikely). Statistics are reported as odds ratio (95% CI). Scale is logarithmic. Variables included are those with P < 0.1 on bivariate analysis. Multivariable model P < 0.001. Abbreviation used: GRE, Graduate Record Examinations; MTM, medication therapy management.
Pharmacist CPA
One hundred eighty (50.6%) respondents reported being likely to participate in services offered by a pharmacist practicing under a CPA. Figure 3 presents the results from the corresponding BWS analysis. Improved physician-pharmacist coordination (best-worst score 0.80), doctor recommendation (0.37), and easier health care provider access (0.24) were the primary motivators for participation in a CPA. The least selected factors included increased pharmacist interactions and a primary care visit with standard co-pay (−0.65 and −0.68, respectively).
Figure 3.
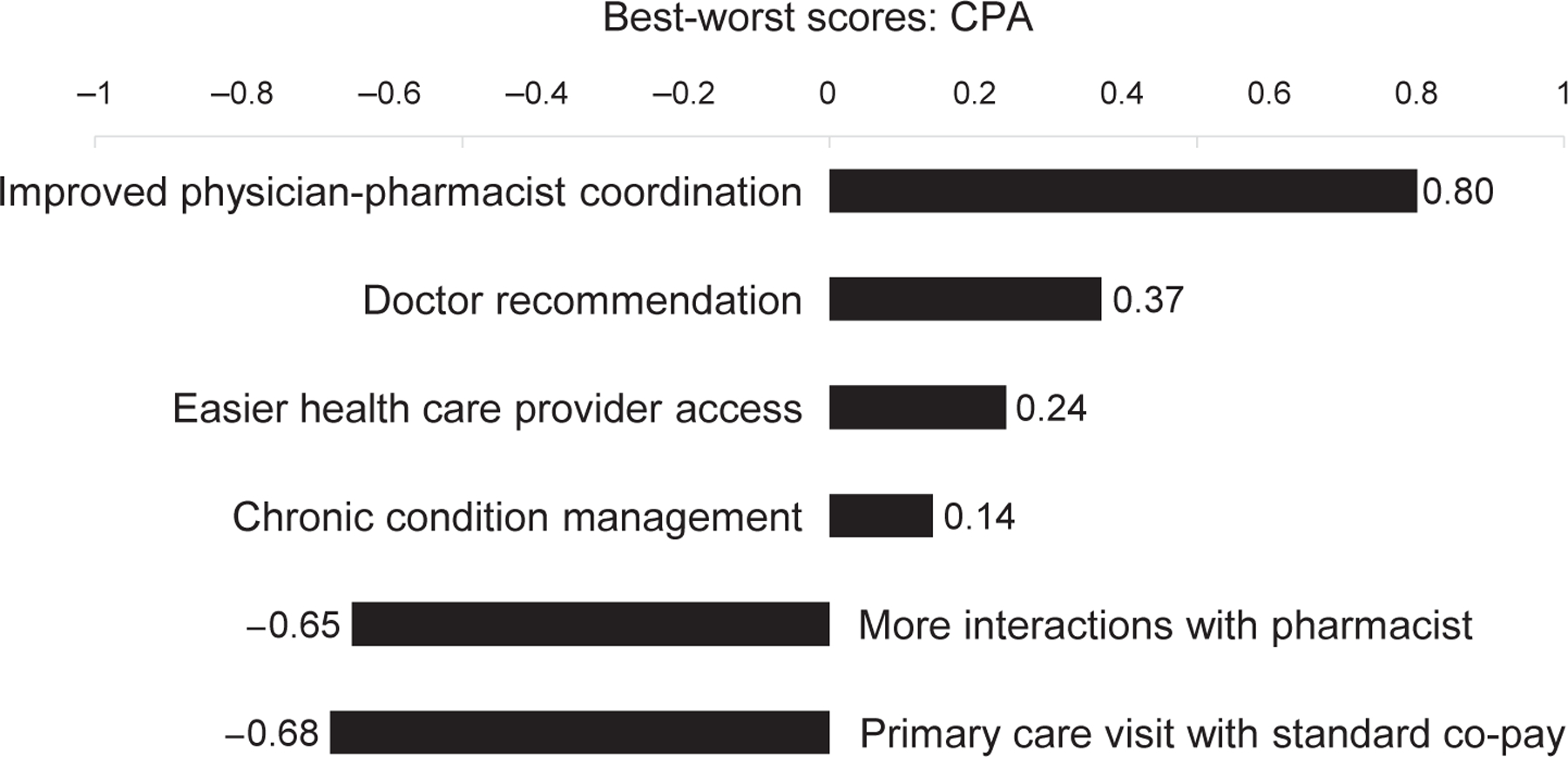
Best-worst scaling analysis for motivations to participate in clinical services provided by a pharmacist with a collaborative practice agreement. Positive values closer to 1 indicate factor more likely to be chosen as the most motivating. Negative values closer to −1 indicate factor more likely to be chosen as the least motivating. Abbreviation used: CPA, collaborative practice agreement.
Table 3 presents the bivariate analysis of the factors associated with the likelihood of participating in clinical services provided by a pharmacist under a CPA. The respondents who stated that they have at least 1 person that they consider their personal pharmacist were significantly more likely to be interested in pharmacist services (likely 47.4% vs. indifferent or unlikely 26.8%, P < 0.001). Previous experience with a CPA (likely 17.8% vs. indifferent or unlikely 0.6%, P < 0.001) and satisfaction with their primary pharmacy (likely 4.7 ± 0.7 vs. indifferent or unlikely 4.5 ± 0.7, P = 0.013) were also associated with a significant higher likelihood of participating in a CPA. On multivariable analysis, satisfaction with their primary pharmacy (1.47 [95% CI 1.01–2.13]) and the presence of a personal pharmacist (2.08 [95% CI 1.26–3.44]) remained associated with a higher likelihood of participating in a CPA. See Figure 4 for a forest plot for the multivariable model.
Table 3.
Factors that influence the likelihood of participating in services offered by a pharmacist practicing under a collaborative practice agreement
| Variable | Likelya n (%) | Indifferent or unlikelyb n (%) | P-value (bivariate) |
|---|---|---|---|
| Female | 89 (49.4) | 93 (52.8) | 0.522 |
| Age | 61.1 ± 7.8 | 63.0 ± 7.5 | 0.253 |
| Race | |||
| Caucasian | 125 (71.4) | 140 (81.9) | 0.056 |
| Black | 30 (17.1) | 16 (9.4) | |
| Other | 20 (11.4) | 15 (8.8) | |
| Spanish, Hispanic, or Latino | 21 (11.7) | 27 (15.3) | 0.310 |
| Employment status | |||
| Employed | 82 (45.6) | 73 (41.5) | 0.680 |
| Retired | 72 (40) | 73 (41.5) | |
| Unemployed | 26 (14.4) | 30 (17.1) | |
| Education level | |||
| ≤ GRE | 35 (19.4) | 34 (19.3) | 0.059 |
| Some college, no degree | 58 (32.2) | 38 (21.6) | |
| College degree | 87 (48.3) | 104 (59.1) | |
| Household income | |||
| < $50,000 | 73 (40.6) | 78 (44.3) | 0.541 |
| $50,000–$100,000 | 66 (36.7) | 66 (37.5) | |
| > $100,000 | 41 (20.8) | 32 (18.2) | |
| U.S. region | |||
| Northeast | 37 (20.6) | 31 (17.6) | 0.536 |
| Midwest | 43 (23.9) | 34 (19.3) | |
| South | 63 (35.0) | 68 (38.6) | |
| West | 37 (20.6) | 43 (24.4) | |
| Urban-rural region | |||
| Urban | 167 (92.8) | 156 (88.6) | 0.178 |
| Rural | 13 (7.2) | 20 (11.4) | |
| Health status | |||
| Excellent | 25 (13.9) | 17 (9.7) | 0.364 |
| Good | 85 (47.2) | 91 (51.7) | |
| Fair | 51 (28.3) | 43 (24.4) | |
| Poor | 19 (10.6) | 25 (14.2) | |
| Poor health affecting usual activities within the past month, Yes | 66 (36.7) | 53 (30.1) | 0.190 |
| Days affected by poor health | 4 [2, 7] | 5 [3, 15] | 0.126 |
| No. prescriptions used in the past month | 3 [2, 5] | 3 [1, 5] | 0.611 |
| Primary pharmacy type | |||
| Chain | 51 (32.7) | 57 (37.3) | 0.263 |
| Grocery store | 25 (16.0) | 19 (12.4) | |
| Department store | 20 (12.8) | 20 (13.1) | |
| Independent pharmacy | 19 (12.2) | 9 (5.9) | |
| Other (e.g., VA, mail order) | 41 (26.3) | 48 (31.4) | |
| No. years using primary pharmacy | 7 [2.5, 15] | 5 [3, 10] | 0.228 |
| Total no. pharmacies used | 1 [1, 2] | 1 [1, 1] | 0.109 |
| Satisfaction with primary pharmacy | 4.7 ± 0.7 | 4.5 ± 0.7 | 0.013 |
| Presence of a personal pharmacist | 74 (47.4) | 41 (26.8) | < 0.001 |
| Previous CPA experience | 32 (17.8) | 1 (0.6) | < 0.001 |
Abbreviations used: CPA, collaborative practice agreement; GRE, Graduate Record Examinations; VA, Veterans’ Administration pharmacy. Note: Continuous data reported as mean ± SD and median [Q1, Q3], categorical data reported as n (%).
Likely to participate included those who responded “very likely” and “somewhat likely.”
Indifferent/unlikely to participate included those who responded “indifferent,” “somewhat unlikely,” or “very unlikely.”
Figure 4.
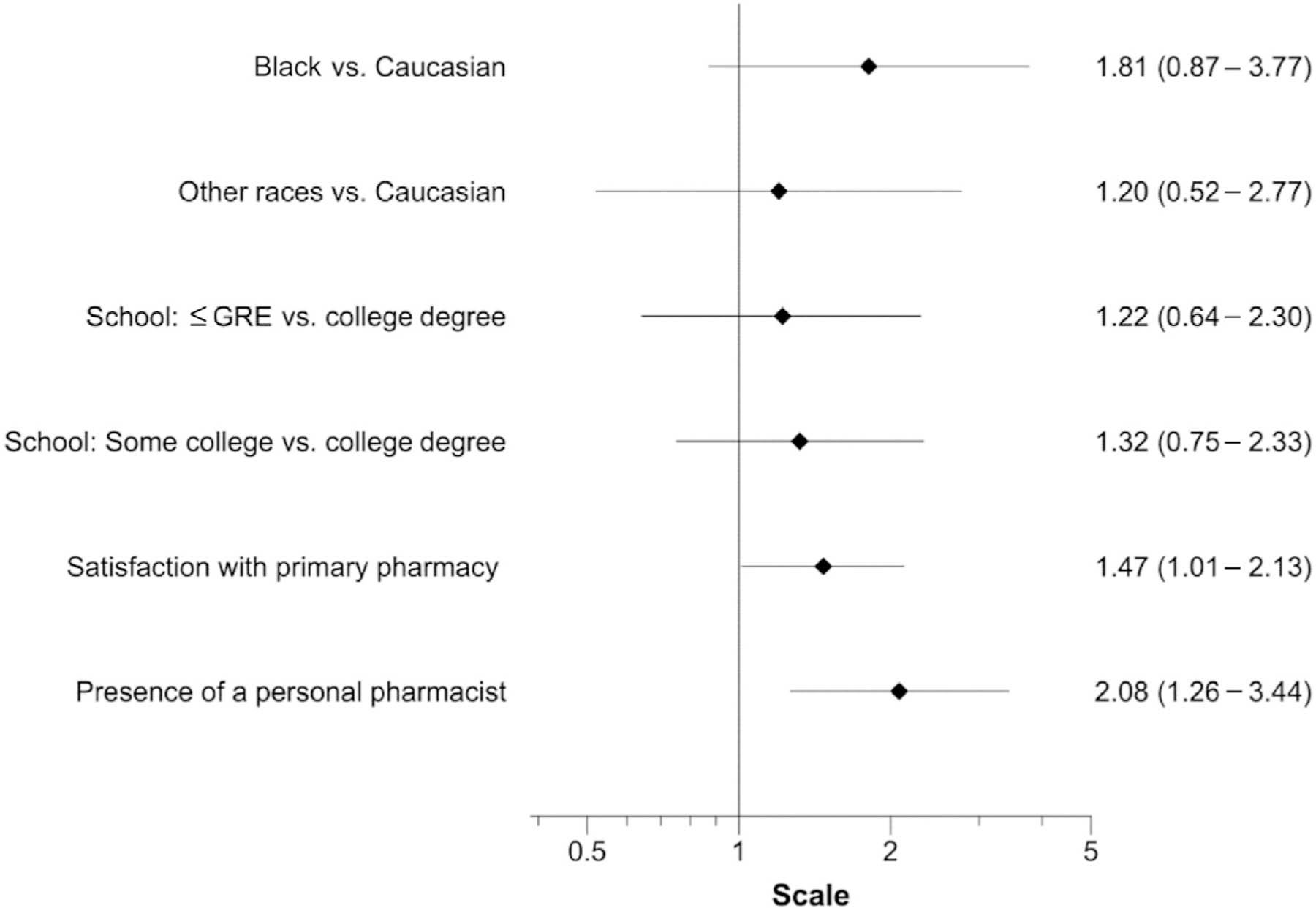
Multivariable analysis of the factors that influence the likelihood of participating in services offered by a pharmacist practicing under a collaborative practice agreement. The dependent variable was participant likelihood of participating in the service; responses dichotomized to those likely to participate (i.e., very likely and somewhat likely) compared with those not likely (i.e., indifferent, somewhat unlikely, or very unlikely). Statistics are reported as odds ratio (95% CI). Scale is logarithmic. Variables included are those with P < 0.1 on bivariate analysis. Multivariable model P = 0.002. Abbreviation used: GRE, Graduate Record Examinations.
Discussion
On the basis of the survey results, the participants were collectively interested in MTM and pharmacist services under a CPA for the purposes of review and management of medication interactions, adverse effect management, and improved physician-pharmacist coordination. These findings indicate that the medication safety aspect of these services may be more valuable to patients than other aspects, including chronic disease management, cost savings, and developing a medication schedule. A similar study involving only Medicare beneficiaries determined the primary motivators for participation in MTM to include better understanding of medication therapy, review of medication efficacy, potential cost savings, and pharmacist’s expertise.21 A large Internet survey of adults on 3 or more medications identified specific MTM services of the greatest interest to be potential cost savings and advice on taking medications as prescribed.27 The variation in findings highlights the need to discern the motivations for patients among different populations to participate in clinical services provided by pharmacists. However, improved communication among health care providers has been a common motivator noted in other studies across populations.24,34
Slightly more than half of the patients surveyed expressed an interest in clinical pharmacy services. This figure is similar to a previous study in which 50.5% of the respondents indicated a willingness to accept MTM services.27 The factors associated with an increased likelihood of participating in clinical services were similar between both services investigated with this survey. The significant factors that applied to both services included previous experience and participants who identified at least 1 person as their personal pharmacist. Exposure to advanced pharmacy services has been previously associated with favorable views of clinical pharmacy services. A survey of Medicare beneficiaries identified favorable attitudes toward pharmacist-provided counseling and MTM activities among patrons of clinic pharmacies.12 Similarly, a recent study associated the likelihood of accepting an offer for a CMR with previous participation in the MTM program.28 The impact of the patient-pharmacist relationship on the acceptance of clinical services has not been previously described to our knowledge. Interestingly, our multivariable model did not find an association between other previous influencers (i.e., number of medications, medication-related problem, presence of chronic disease states, and poor health) and the likelihood of participating in clinical services.17,22,25–29
Given the demonstrated benefit of MTM, CMS is continuing to expand services.35 Similar to other studies in which 8%-16% of the participants had been exposed to clinical services, only a fraction of our participants had previously experienced 1 of these services (16.6% MTM and 9.3% CPA).15,16,28 CMS aims to increase beneficiary awareness and increase the services provided through an enhanced MTM pilot program developed by the CMS Innovation Center. The pilot program will provide medical data to PDPs that often do not have access to medical data and incentives to align with the services provided.35 This is an important step to help overcome the common barriers that pharmacists face, including compensation and documentation.35 In the future, it may be of benefit to take into consideration the findings of this study and of additional studies to understand what will motivate patients to take advantage of these services. The patient-pharmacist relationship seems to be a strong motivator, and can possibly be used positively to increase participation because it is already known that patients prefer services such as CMR at their own pharmacy.34
Limitations
There are several limitations to take into account when reviewing the results of this study. This is the first time that the survey has been used. Future work should validate the survey content using quantifiable measures of validity. Specifically, the construct validity of the questions designed by the researchers (e.g., “Do you have one person you think of as your personal pharmacist?”) and the predictive validity of this survey have not been evaluated. This survey did not evaluate the reasons for unwillingness to participate in clinical services, nor how the potential cost of the service may affect patient participation.
The survey sampled a small fraction of the population of patients who take prescription medications or could benefit from clinical pharmacy services, and excluded patients younger than 55 years of age. In addition, only Internet users were surveyed, and the findings may under-represent those with limited Internet access. Finally, previous experience with MTM or CPA may have occurred with any pharmacist, not necessarily the participant’s personal pharmacist. This may have implications with regard to the influence of the patient-pharmacist relationship and the ability to influence overall participation in clinical pharmacy services.
Limitations related to BWS to determine the motivations to seek clinical pharmacy services could be present. BWS can use multiple scaling tasks to measure the strength of participant preference. In this survey, all participants were presented with a single, identical scaling task for each service, and therefore the best-worst scores cannot be interpreted as the true strength of preferences. In addition, the BWS choices presented to the patients were not all-inclusive, but rather selected from an informed literature search. It is possible that we did not capture other significant motivators owing to the approach we used.
A strength of this study was the use of a marketing company that used a sample population that was representative of the current U.S. Census. The survey results should be generalizable to our targeted population because the eligible participants were limited to those 55 years of age or older to increase the likelihood that the participants used prescription medications and had previous experiences with clinical pharmacy services.
Conclusion
The study participants were interested in seeking clinical pharmacy services for the purposes of review and management of medication interactions, adverse effect management, and improved physician-pharmacist coordination. Several factors seemed to predict willingness for these services, most notably the patient-pharmacist relationship. As clinical pharmacy services continue to grow, and patients are encouraged to use these services to improve health care outcomes, pharmacists should be cognizant of the factors that patients value and the influence of the pharmacist-patient relationship on the successful implementation and uptake of clinical pharmacy services.
Key Points.
Background:
Surveys of Medicare beneficiaries who participated in medication therapy management showed that they generally found value in the service, and primarily appreciated the potential cost savings, medication efficacy review, and medication therapy education.
The barriers to patient acceptance of clinical pharmacy services include time required to participate, potential cost, concern that pharmacists’ recommendations would conflict with physicians’ plans, or patients’ belief that they did not need the service.
Potential factors that may influence patient interest in clinical services include number of medications, medication-related problems, presence of chronic disease states, and poor health.
Findings:
The motivations to participate in clinical pharmacy services seem to be related to previous clinical pharmacy experiences and the patient-pharmacist relationship.
The participants were most interested in clinical services for the purpose of adverse effect management, medication interaction management, and increased collaboration with their physician.
Funding:
Antoinette B. Coe is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (award number KL2TR002241). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix 1. Survey
You are invited to be a part of a study to help researchers understand how a pharmacist can help manage medications and medical conditions.
The purpose of this research is to determine factors that influence a patient’s acceptance of pharmacist services and motivations to seek pharmacist services. We expect the survey to take no longer than 10 minutes.
The University of Michigan Institutional Review Board for the Medical School has determined that this study is exempt from IRB oversight.
Please click continue to proceed with the survey
Continue
No thank you (Leave survey)
-
Have you used prescription medications in the past year?
Yes
No (skip → 10)
-
In a typical month, how many different pharmacies do you get prescription medications from (including mail order)?
________ # of pharmacies
- Select your primary pharmacy (the pharmacy you use to get most of your prescription drugs from) from the following:
- Big drugstore chain pharmacy such as Walgreens or CVS
- Pharmacy inside a grocery store or supermarket
- Pharmacy inside a chain department store such as Wal-Mart or Kmart
- Independent pharmacy (pharmacy that is locally owned)
- Veterans’ Administration pharmacy
- Pharmacy inside a medical clinic or hospital
- By mail order
- Over the internet
- Free samples from physician
- Other (Please specify: ________)
- I do not have a primary pharmacy (Skip → 6)
-
Please rate your satisfaction with your primary pharmacy: (1 to 5 scale)
5 (Completely satisfied)
4
3
2
1 (Not satisfied at all)
-
How many years have you been using your primary pharmacy?
Less than one year
1–3 years
3–5 years
More than 5 years
-
How many different prescription medications did you use in the last month?
_______ # of prescription drugs
-
How many non-prescription medications did you use in the last month? This includes over-the counter vitamins, supplements and herbals.
________ # of over-the-counter medications
-
Do you have one person you think of as your personal pharmacist?
Yes, only one
More than one
No
-
How comfortable do you feel speaking to your pharmacist about health-related topics?
5 (Very comfortable)
4
3
2
1 (Completely uncomfortable)
-
Would you say that in general your health is –?
Excellent
Very good
Good
Fair
Poor
-
During the past 30 days, for about how many days did poor physical or mental health keep you from doing your usual activities, such as self-care, work, or recreation?
_______ Number of days
None
Not sure
Researchers are interested in how you would use a pharmacist to help you manage your medications and medical conditions.
Pharmacists are trained to provide services to help you get the best results from your medications. They are able to review your medications and work closely with you and your doctors to solve any problems related to your medicines. Sometimes the pharmacy can get busy and hectic so the following questions are about a specific service some pharmacists provide to focus on the patient.
Medication therapy management (MTM) is an example of this type of service. It involves a meeting with a pharmacist, who will review your medications, address any concerns you have with your medications, including cost issues and drug reactions, discuss how best to take your medications and answer any questions you have about your medications and health conditions. This review is done in person or over the phone and typically lasts 30–45 minutes. After the medication review is complete, the pharmacist reviews your therapy goals, look at your medication regimen and reach out to you and your physician(s) to make recommendations to improve your medication therapy outcomes.
-
Have you had an interaction like this with a pharmacist?
Yes
No
Not sure
-
How likely would you be to participate in this type of service, if offered?
5 (Very likely)
4
3
2
1 (Not at all likely)
-
Which of the following would MOST likely make you want to participate in a service like this?
Free health service
Started a new prescription or more information about medication
Pharmacist checks the safety of your medication and the best way to manage side effects
Pharmacist helps manage health conditions, such as diabetes, high blood pressure, asthma, etc.
Pharmacist checks for interactions between medications and can help manage interactions
Help understand and create best medication schedule, including how many times a day a medication is taken and what time of day
Potential medication cost savings by reducing number of medications taken or switching to cheaper medication
Doctor recommendation
-
Which of the following would LEAST likely make you want to participate in a service like this?
Free health service
Started a new prescription or more information about medication
Pharmacist checks the safety of your medication and the best way to manage side effects
Pharmacist checks for interactions between medications and can help manage interactions
Pharmacist helps manage health conditions, such as diabetes, high blood pressure, asthma, etc.
Help understand and create best medication schedule, including how many times a day a medication is taken and what time of day
Potential medication cost savings by reducing number of medications taken or switching to cheaper medication
Doctor recommendation
Now, imagine if your physician had an agreement with a pharmacist to allow for assistance with some of the physician duties. Qualified pharmacists, following a protocol, and working in collaboration with a physician, would be allowed to order labs, refill medications, and initiate, modify, or discontinue treatment when appropriate. Currently, 48 states plus the District of Columbia allow for some degree of practice agreements between pharmacists and other health care providers.
-
Have you had an interaction like this with a pharmacist?
Yes
No
Not sure
-
How likely would you be to participate in this type of service, if offered?
5 (Very likely)
4
3
2
1 (Not at all likely)
-
Which of the following would MOST likely make you want to participate in a service like this?
Standard office visit copay for primary care visit with pharmacist
Pharmacist helps you manage chronic health conditions, such as diabetes, high blood pressure, asthma, etc.
Improved coordination between your physicians and pharmacist
Easier access to a health care provider when you need it
More interactions with a pharmacist
Doctor recommendation
-
Which of the following would LEAST likely make you want to participate in a service like this?
Standard office visit copay for primary care visit with pharmacist
Pharmacist helps you manage chronic health conditions, such as diabetes, high blood pressure, asthma, etc.
Improved coordination between your physicians and pharmacist
Easier to meet with a healthcare provider when you need it
More interactions with a pharmacist
Doctor recommendation
In what state do you currently reside? (drop down menu)
What is your Zip Code? _____
-
What is your sex?
Male
Female
What is your year of birth? _____
-
Are you Spanish, Hispanic, or Latino or none of these?
Yes
None of these
- Choose one or more races that you consider yourself to be:
- White
- Black or African American
- American Indian or Alaska Native
- Asian
- Native Hawaiian or Pacific Islander
- Other: ______
- Age
-
What is the highest level of school you have completed or the highest degree you have received?
Less than high school degree
High school graduate (high school diploma or equivalent including GED)
Some college but no degree
Associate degree in college (2-year)
Bachelor’s degree in college (4-year)
Master’s degree
Doctoral degree
Professional degree (JD, MD)
-
Which statement best describes your current employment status?
Working (paid employee)
Working (self-employed)
Not working (temporary layoff from a job)
Not working (looking for work)
Not working (retired)
Not working (disabled)
Not working (other)
Prefer not to answer
-
Information about income is very important to understand. Would you please give your best guess? Please indicate the answer that includes your entire household income in (previous year) before taxes.
Less than $20,000
$20,000 to $34,999
$35,000 to $49,999
$50,000 to $74,999
$75,000 to $99,999
$100,000 to $149,999
$150,000 or more
Appendix 2. Best-worst scaling example
Which of the following would most/least likely make you want to participate in a service like this?
| Most likely (“Best”) | Variable | Least likely (“Worst”) |
|---|---|---|
| X | Standard office visit co-pay for primary care visit with pharmacist | |
| Pharmacist helps you manage chronic health conditions, such as diabetes, high blood pressure, asthma, etc. | ||
| Improved coordination between your physicians and pharmacist | ||
| Easier access to a health care provider when you need it | X | |
| More interactions with a pharmacist | ||
| Doctor recommendation |
Note: Owing to the survey structure, the best-worst score was represented by 2 separate questions within the questionnaire. See questions 3 and 4 within MTM and CPA sections of survey above.
Appendix 3. Survey respondent location
Factors that influence patient acceptance of clinical pharmacy services: A nationwide survey. Each dot represents survey participant location.
Footnotes
Disclosure: The authors declare no relevant conflicts of interest or financial relationships.
Previous presentation: The results of this study have been reported at a poster presentation at the American Society of Health-System Pharmacists Midyear Clinical Meeting in Orlando, December 4, 2017.
Institutional Review Board exemption: The University of Michigan Institutional Review Board for the Medical School has determined that this study is exempt from institutional review board oversight (HUM00119964).
Contributor Information
Lauren Schumacher, University of Michigan College of Pharmacy, Ann Arbor, MI.
Antoinette B. Coe, University of Michigan College of Pharmacy, Ann Arbor, MI.
Corey A. Lester, University of Michigan College of Pharmacy, Ann Arbor, MI.
Mary Rothermal, Care Management at Blue Cross Blue Shield of Michigan, MI.
Michael P. Dorsch, University of Michigan College of Pharmacy, Ann Arbor, MI.
References
- 1.Touchette DR, Burns AL, Bough MA, Blackburn JC. Survey of medication therapy management programs under medicare part D. J Am Pharm Assoc (2003) 2006;46(6):683–691. [DOI] [PubMed] [Google Scholar]
- 2.American Pharmacists Association; National Association of Chain Drug Stores Foundation. Medication therapy management in pharmacy practice: core elements of an MTM service model (version 2.0). J Am Pharm Assoc (2003) 2008;48(3):573–579. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Medicare and Medicaid Services. 2018 medicare part D medication therapy management (MTM) programs:fact sheet summary of 2018 MTM programs Available at: https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/CY2018-MTM-Fact-Sheet.pdf. Accessed March 4, 2019.
- 4.Brummel A, Carlson AM. Comprehensive medication management and medication adherence for chronic conditions. J Manag Care Spec Pharm 2016;22(1):56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bunting BA, Smith BH, Sutherland SE. The Asheville project: clinical and economic outcomes of a community-based long-term medication therapy management program for hypertension and dyslipidemia. J Am Pharm Assoc (2003) 2008;48(1):23–31. [DOI] [PubMed] [Google Scholar]
- 6.Bunting BA, Cranor CW. The Asheville project: long-term clinical, humanistic, and economic outcomes of a community-based medication therapy management program for asthma. J Am Pharm Assoc (2003) 2006;46(2):133–147. [DOI] [PubMed] [Google Scholar]
- 7.Cranor CW, Bunting BA, Christensen DB. The Asheville project: long-term clinical and economic outcomes of a community pharmacy diabetes care program. J Am Pharm Assoc (Wash) 2003;43(2):173–184. [DOI] [PubMed] [Google Scholar]
- 8.Ramalho de Oliveira D, Brummel AR, Miller DB. Medication therapy management: 10 years of experience in a large integrated health care system. J Manag Care Pharm 2010;16(3):185–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jokanovic N, Tan EC, Sudhakaran S, et al. Pharmacist-led medication review in community settings: an overview of systematic reviews. Res Social Adm Pharm 2017;13(4):661–685. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Collaborative practice agreements and pharmacists’patient care services: a resource for pharmacists. Atlanta, GA: Centers for Disease Control and Prevention; 2013. https://www.cdc.gov/dhdsp/pubs/docs/Translational_Tools_Pharmacists.pdf. Accessed March 4, 2019. [Google Scholar]
- 11.Klepser DG, Klepser ME, Dering-Anderson AM, Morse JA, Smith JK, Klepser SA. Community pharmacist-physician collaborative streptococcal pharyngitis management program. J Am Pharm Assoc (2003) 2016;56(3): 323–329.e1. [DOI] [PubMed] [Google Scholar]
- 12.Klepser ME, Klepser DG, Dering-Anderson AM, Morse JA, Smith JK, Klepser SA. Effectiveness of a pharmacist-physician collaborative program to manage influenza-like illness. J Am Pharm Assoc (2003) 2016;56(1):14–21. [DOI] [PubMed] [Google Scholar]
- 13.Mikolas LA, Jacques K, Huq M, Krasner C, Mambourg SE. Utilizing clinical pharmacist specialist to manage Hepatitis C virus patients on direct-acting antiviral therapy. J Pharm Pract 2019;32(6):655–663. [DOI] [PubMed] [Google Scholar]
- 14.Fay LN, Wolf LM, Brandt KL, et al. Pharmacist-led antimicrobial stewardship program in an urgent care setting. Am J Health Syst Pharm 2019;76(3):175–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ekenga V, Bailey-Wheeler J, Hart T, Sarpong D, Earls M. Patients’ perception of community pharmacists as healthcare providers and willingness to participate in pharmacist services: a pilot study. J Pharm Health Serv Res 2018;9(4):297–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Truong HA, Layson-Wolf C, de Bittner MR, Owen JA, Haupt S. Perceptions of patients on Medicare Part D medication therapy management services. J Am Pharm Assoc (2003) 2009;49(3):392–398. [DOI] [PubMed] [Google Scholar]
- 17.Law AV, Okamoto MP, Brock K. Perceptions of Medicare Part D enrollees about pharmacists and their role as providers of medication therapy management. J Am Pharm Assoc (2003) 2008;48(5):648–653. [DOI] [PubMed] [Google Scholar]
- 18.Doucette WR, Witry MJ, Alkhateeb F, Farris KB, Urmie JM. Attitudes of Medicare beneficiaries toward pharmacist-provided medication therapy management activities as part of the Medicare Part D benefit. J Am Pharm Assoc (2003) 2007;47(6):758–762. [DOI] [PubMed] [Google Scholar]
- 19.Moczygemba LR, Barner JC, Brown CM, et al. Patient satisfaction with a pharmacist-provided telephone medication therapy management program. Res Social Adm Pharm 2010;6(2):143–154. [DOI] [PubMed] [Google Scholar]
- 20.Doucette WR, Pendergast JF, Zhang Y, et al. Stimulating comprehensive medication reviews among Medicare Part D beneficiaries. Am J Manag Care 2015;21(6):e372–e378. [PubMed] [Google Scholar]
- 21.Huet AL, Frail CK, Lake LM, Snyder ME. Impact of passive and active promotional strategies on patient acceptance of medication therapy management services. J Am Pharm Assoc (2003) 2015;55(2):178–181. [DOI] [PubMed] [Google Scholar]
- 22.Friedrich M, Zgarrick D, Masood A, Montuoro J. Patients’ needs and interests in a self-pay medication therapy management service. J Am Pharm Assoc (2003) 2010;50(1):72–77. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Medicare and Medicid Services. Medicare; 2019 Part C, Star D. Ratings technical notes Available at: https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovGenIn/Downloads/2019-Part-C-and-D-Medicare-Star-Ratings-Data-v04-12-2019.zip. Accessed July 18, 2019.
- 24.Garcia GM, Snyder ME, McGrath SH, Smith RB, McGivney MS. Generating demand for pharmacist-provided medication therapy management: identifying patient-preferred marketing strategies. J Am Pharm Assoc (2003) 2009;49(5):611–616. [DOI] [PubMed] [Google Scholar]
- 25.Schultz H, Westberg SM, Ramalho de Oliveira D, Brummel A. Patient-perceived value of medication therapy management (MTM) services: a series of focus groups. Innov Pharm 2012;3(4). Article 96. https://pubs.lib.umn.edu/index.php/innovations/article/view/278. Accessed July 9, 2019 [Google Scholar]
- 26.Shimp LA, Kucukarslan SN, Elder J, et al. Employer-based patient-centered medication therapy management program: evidence and recommendations for future programs. J Am Pharm Assoc (2003) 2012;52(6):768–776. [DOI] [PubMed] [Google Scholar]
- 27.Brown LM, Rashrash ME, Schommer JC. The certainty in consumers’ willingness to accept pharmacist-provided medication therapy management services. J Am Pharm Assoc (2003) 2017;57(2):211–216. [DOI] [PubMed] [Google Scholar]
- 28.Miguel A, Hall A, Liu W, et al. Improving comprehensive medication review acceptance by using a standardized recruitment script: a randomized control trial. J Manag Care Spec Pharm 2017;23(1):13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Farris KB, Salgado TM, Aneese N, et al. Effect of clinical and attitudinal characteristics on obtaining comprehensive medication reviews. J Manag Care Spec Pharm 2016;22(4):388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cheung KL, Wijnen BF, Hollin IL, et al. Using best-worst scaling to investigate preferences in health care. Pharmacoeconomics 2016;34(12):1195–1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flynn TN. Valuing citizen and patient preferences in health: recent developments in three types of best-worst scaling. Expert Rev Pharmacoecon Outcomes Res 2010;10(3):259–267. [DOI] [PubMed] [Google Scholar]
- 32.Flynn TN, Louviere JJ, Peters TJ, Coast J. Best–worst scaling: what it can do for health care research and how to do it. J Health Econ 2007;26(1): 171–189. [DOI] [PubMed] [Google Scholar]
- 33.UNIVERSITY of Technology Sydney. Centre for the Study of Choice. Best-worst scaling (MaxDiff) Available at: https://www.uts.edu.au/sites/default/files/CenSoC_BestWorstScaling_Overview.pdf. Accessed July 16, 2017.
- 34.Doucette WR, Zhang Y, Chrischilles EA, et al. Factors affecting Medicare Part D beneciaries’ decision to receive comprehensive medication reviews. J Am Pharm Assoc (2003) 2013;53(5):482–487. [DOI] [PubMed] [Google Scholar]
- 35.Brandt NJ, Cooke CE. Centers for Medicare and Medicaid Services support for medication therapy management (enhanced medication therapy management): testing strategies for improving medication use among beneficiaries enrolled in Medicare Part D. Clin Geriatr Med 2017;33(2): 153–164. [DOI] [PubMed] [Google Scholar]


