Abstract
To address the Quintuple Aim of health care improvement, the profession of pharmacy is on the verge of a practice transformation that incorporates continuous learning from medication-related data into existing clinical and dispensing roles. The pharmacists’ patient care process (PPCP) enables a learning pharmacy practice through the systematic and standardized collection of real-world medication-related data from pharmacists’ patient care activities. A learning pharmacy practice continually generates data-powered discoveries as a byproduct of PPCP interactions. In turn, these discoveries improve our medication knowledge while upgrading our predictive powers, thus helping all people achieve optimal health outcomes. Establishing a practice management system connected to the PPCP means that data are generated from every PPCP interaction, combined with existing data, and analyzed by teams of pharmacists and data scientists. The resulting new knowledge is then incorporated into all future PPCP interactions in the form of predictions coupled to actionable advice. The primary purpose of a learning pharmacy practice is to combine the power of predictive modeling with evidence-based best practices to achieve and sustain population-level health improvements. This purpose is achieved by systematically optimizing individual medication use in an equitable manner on a global scale.
To achieve the Quintuple Aim of combining improved patient outcomes, patient experience, and pharmacist well-being with lower costs and more equitable care, it is imperative that pharmacists perform their work with the best possible pharmacy knowledge available. Pharmacists’ are poised to meet these aims in more effective ways by continuously learning from the growing amount of real-world medication use data and using the knowledge to inform their daily practice. Continuous learning expands the scope of pharmacists’ work to also include systematically collecting medication use and outcomes data, performing data analyses to generate reliable medication-related knowledge before implementing that knowledge in practice.
The pharmacists’ patient care process (PPCP) enables pharmacists to participate more fully in the work of continuously learning about medication use during patient care. The PPCP provides the necessary structure to formalize pharmacists’ patient care activities and optimize treatment outcomes for individual patients.1 In this article, we place PPCP within the larger context of a learning pharmacy practice (Table 1).
Table 1.
Definition of a learning pharmacy practice
| A learning pharmacy practice is one that continually generates generalizable data-powered discoveries from patient care activities to improve our medication knowledge and help all people to achieve optimal health outcomes. |
Developed by The Joint Commission for Pharmacy Practitioners, the PPCP is a standardized, systematic approach for pharmacists who perform patient-centered care involving patients and their caregivers, providers, family members, and insurers. The PPCP connects 5 patient care steps into a cycle: patient data collection, assessment and analysis, care planning, implementing care plans, and monitoring plans in effect. At the critical care planning step, individualization leads to patient-centered care plans that account for patient characteristics and preferences. Therapeutic goals are also established and clarified in concert with other health care providers. These goals set parameters for future measurement of therapeutic effects and other patient outcomes.
Although PPCP interactions are currently targeted at an individual-level, these patient-pharmacist interactions also offer an opportunity to systematically produce shared knowledge that can be shared as real-time patient care advice. By focusing only on individual patient care, we limit the potential value of the PPCP. Greater value is realized when the PPCP is viewed as a central component of a larger, transformed practice management system. We envision the PPCP situated within a transformed practice management system that encompasses continuous learning across patients and health care organizations. Our view highlights growing opportunities to accelerate learning, improve medication use on a broad scale, and rapidly advance pharmacy practice.
PPCP’s creators note that the process is embedded within the larger pharmaceutical care model from Hepler and Strand.2 Some view PPCP as the second part in a 3-part model of professional practice, which includes (1) a philosophy of practice, (2) a patient care process, such as PPCP, and (3) a practice management system.3,4 We agree that the PPCP must be founded on a philosophy of ethical and appropriate practice. Furthermore, a practice management system comprising accountable organizational structures and technologies that sustain pharmacy practice is needed to support the PPCP.
However, our current practice management system primarily supports the PPCP for individual patient interactions and is not adapting fast enough to rapid changes in biomedical knowledge production and the introduction of data science. The result is that pharmacists do not always have the best possible evidence at their fingertips to support high-performance clinical decision making.5–9 We raise the potential for remaking the pharmacy practice management system into a learning pharmacy practice. A learning pharmacy practice supports continuous learning when diverse data are routinely aggregated from PPCP iterations across most patients, analyzed to produce new medication knowledge in computer-readable forms, and communicated directly back into practice for patients and authorized health care workers to use.
This article describes the concept of a learning pharmacy practice and explains how it facilitates continuous learning. We believe this kind of practice management system is especially important and relevant as pharmacists rethink their care roles, enhance their capabilities and expertise,10 adopt new technologies to support patient care,11,12 and determine how to transform the pharmacy profession to support the practice of the future.13
Vision of a learning pharmacy practice
The learning pharmacy practice concept is an outgrowth of recent work to build Learning Health Systems at various levels of scale.14 The U.S. Institute of Medicine, now the National Academy of Medicine, first advanced the concept of Learning Health Systems in 2007. A Learning Health System is defined as one, “in which evidence is both applied and developed as a natural product of the care process.”15 The following are 5 activities that Learning Health Systems do: (1) aggregate data about the health-related experiences and outcomes of many persons, (2) routinely analyze aggregated data to produce new knowledge of best practices, (3) continuously implement the new best practices learned from data analysis, (4) develop and adopt infrastructure to support the activities of continuous learning, and (5) institute and inculcate pervasive, inclusive cultures of ongoing learning about health.
The PPCP directly supports the first 3 of these learning activities. In contrast, the PPCP can be supported by the other 2 activities. The PPCP enables continuous learning from real-world data because as it unfolds over multiple iterations within and across many patients, it generates outcomes data that are suitable for aggregation and analysis. Predictive models can be developed that lead to safer, more effective medication use practices using these data. The planning step of the PPCP provides a critical entry point to translate knowledge into practice. This happens when individualized models are coupled with current knowledge about best practices, treatment options, and adverse events on behalf of patients. In this way, the value of individual PPCP cycles are appreciably expanded to include continuous learning through data analytics.
The systematic collection of diverse outcomes data and the inflow of reliable predictions, new medication use knowledge, and updated best practices into care planning are supported by embedding the PPCP into a larger practice management system that learns from real-world data continuously. We refer to pharmacy practice functioning in this way as a learning pharmacy practice. The challenge of generating and delivering accurate predictions for individual patients informed by the most complete and up-to-date medication use knowledge possible becomes central to safe, effective care by pharmacists. A learning pharmacy practice cannot exist without consistent care processes and workflows such as the PPCP.
Few outcomes data and evidence exist to date about the impacts of continuous learning in pharmacy. Although clinical pharmacy practice has yet to be transformed by big data analytics, the experiences of other industries suggest this transformation is likely to come.16 The stage is set for a new pharmacy practice paradigm shift focused on the use of high-performance artificial intelligence from comprehensive, validated, and standardized data produced by PPCP interactions.17,18 Spurring the readiness for a learning pharmacy practice are changes in the pharmacy health technology landscape such as widespread electronic health records and electronic prescribing, adoption of digital pharmacy services, and remote monitoring of patient-generated outcomes.13,19,20
In addition, the economics of a learning pharmacy practice needs to be addressed. The opportunity exists to build industry around the identification and use of new medication knowledge in PPCP interactions. A learning pharmacy practice model brings value to stakeholders including patients, pharmacies, and insurers through fewer adverse events and improved quality of care. Perhaps a learning pharmacy practice can be sustained in the way patient safety organizations are funded today.21 Regardless of the funding mechanism, teams of pharmacists, data scientists, biostatisticians, and implementation scientists must be compensated appropriately for performing the activities of establishing generalizable medication use knowledge in these organizations.
Building a learning pharmacy practice
A learning pharmacy practice comes into view when considering the people, processes, and technologies required to expand beyond supporting the PPCP for individual-level patient care to supporting the PPCP also as a critical enabler of ‘learning while doing’ in all patient care settings (Figure 1). It was during our work in Learning Health Systems and Information Science that we noticed the potential for a learning pharmacy practice and further developed the idea within our pharmacy informatics research group at the University of Michigan.
Figure 1.
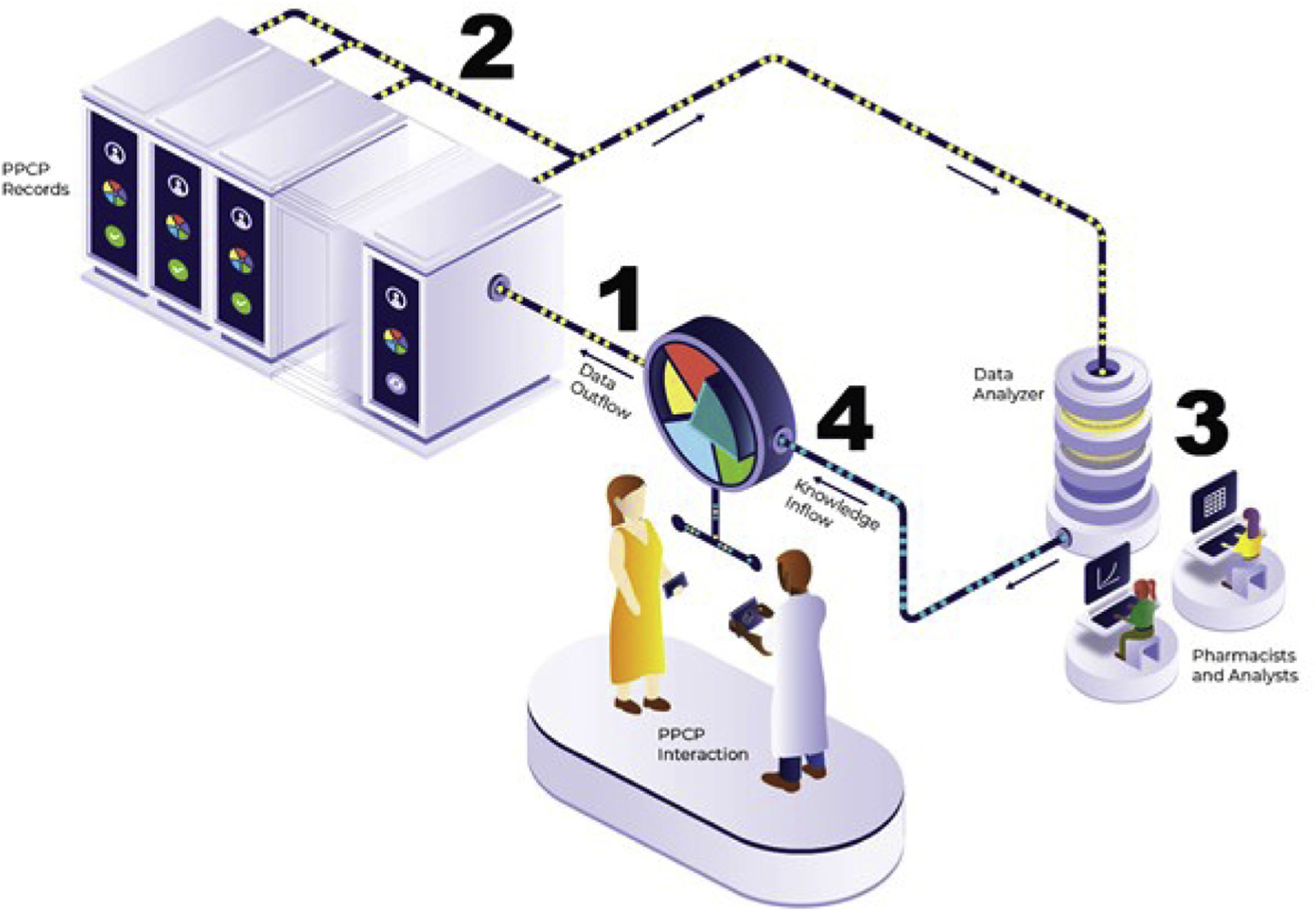
A learning pharmacy practice enabled by PPCP in support of continuous learning. Abbreviation used: PPCP, pharmacists’ patient care process.
Starting at step 1 (Figure 1), a learning pharmacy practice collects many types of real-world data arising from the individually focused PPCP interaction to create population-spanning data sources. At step 2, data obtained from past PPCP interactions are stored as electronic PPCP records (e.g., Pharmacist eCare Plan developed by the National Council for Prescription Drug Programs22). A learning pharmacy practice aggregates these PPCP records at step 2 to provide sufficiently large datasets for analysis. Then, at step 3, pharmacists and data scientists work together to perform data management, build and test predictive models, and continuously review statistics to inform better analyses as more data are collected. When predictive models generate new knowledge that should be implemented to improve pharmacy practice, clinical practice guidelines are updated accordingly. To facilitate this, the guidelines themselves should be in computer-readable forms, allowing for faster, easier, and more reliable integration of predictive models into guideline recommendations.23 Finally, at step 4, these computer models produce useful knowledge to patients and pharmacists that are integrated into all relevant individual PPCP interactions as best practice tools. Communicating useful advice from current best practice knowledge in computer-readable formats to pharmacists ensures patients optimize their medication use.
Imagine this as a 4-step cycle repeating continuously so that patients routinely and consistently benefit from the most up-to-date medication and treatment knowledge available. The medication use knowledge is updated and improved as thousands of new PPCP-based patient interactions occur every hour of every day. A more detailed discussion of the components and process depicted in Figure 1 follows.
Step 1: Collection of diverse real-world data stemming from the PPCP interactions
In Figure 1, the PPCP is ongoing and the co-creation of a care plan occurs among patients, pharmacists, and other health care providers. A patient and a pharmacist discuss past outcomes and make shared plans for future medication use. The depicted instance of the PPCP unfolds as a face-to-face interaction; however, the PPCP may also occur remotely through real-time observation, electronic messaging, or telepharmacy. At step 1, with approval from the patient, the data generated from conducting the PPCP are represented by yellow dots flowing away from the interaction into a PPCP record for the patient. A PPCP record may include images, structured data, free-text, video, voice, or data in other forms that are collected from the PPCP interactions. Examples of the data sources include social media, contact tracing, physical activity tracking, streaming drug concentrations, and patient-provider conversations. In a learning pharmacy practice, patients have control over their personal data, determine which types of data are shared, and how those data can be used by the system. Patients are encouraged to share their data so that continuous learning about medication use and patient outcomes can take place to benefit all.
A learning pharmacy practice applies data standards and security protocols consistent with state and federal laws as these real-world data are collected. Some data standards already exist (e.g., Health Level Seven International, Fast Healthcare Interoperability Resources, and National Council for Prescription Drug Program SCRIPT standards), but the profession of pharmacy will need to advance a host of other data standards as part of the work of establishing a learning pharmacy practice. Data standardization and security measures help ensure that the reliable data and knowledge produced by successive PPCP interactions taking place throughout the learning pharmacy practice are accessible to those who are authorized to use them and not to others.
Step 2: Aggregation and storage of PPCP interaction data
Diverse data about individuals from PPCP interactions are aggregated to form large repositories of current and historical medication use and patient care outcomes data. Data from these sources can be combined at individual, organizational, and societal levels to ensure that consistent, tailored, and equitable care for each patient is based on the best possible predictions and the most up-to-date medication knowledge. As past outcomes data are collected in large quantities, different types of data analyses can reveal detailed patient-level trends and changes in exposure and response to medications over time. In a learning pharmacy practice, enough real-world medication use data can be collected to support investigations of relatively rare phenomena and diseases. These may also be actively combined with other sources of data (e.g., socioeconomic data) to further inform best practice and treatment for individuals. The ability to bring continuous learning at scale to rare problems is 1 of the most important potential benefits of a learning pharmacy practice.
Building data repositories can occur in more than 1 way. Using a large group of federated databases in conjunction with remote queries, real-world data arising from PPCP interactions can be stored locally but still made available for large-scale analyses across many locations. Alternatively, it is also possible that extremely large data lakes filled with diverse and deidentified real-world data could be established to support a learning pharmacy practice in the future. Aggregating real-world data arising from PPCP interactions for use is not as much of a technical challenge as it is a matter of public policy and ethics. It is clear, however, that aggregating data to support continuous learning about medication use raises new ethical issues, including the issue of having everyone in society potentially contribute to the common purpose of improving the quality and value of patient care.24,25
Step 3: Knowledge generation resulting from continuous data analysis
Aggregation, organization, and preparation of the PPCP-derived data for analysis occur at step 2. Then, at step 3, pharmacists, data scientists, and patients study the data collaboratively to produce informative results that are used to guide PPCP interactions for future patient and pharmacist shared decision making. At this step, pharmacists and data scientists work together to clean data and design statistical procedures and tests to generate insights in the form of predictive models, dosing, risk, and other useful mathematical equations and also tables, graphs, and other visuals. When results of these types are generated, more pharmacists and also patients have roles in a learning pharmacy practice that give them the purview to oversee the interpretation of results and to determine whether new results are meaningful and actionable. If so, something new and important has been learned that carries the potential to improve pharmacy practice and drive medication use outcomes.
In a learning pharmacy practice, the analyses focus on 3 core areas: (1) determining what is happening with the patient, (2) predicting what will happen to the patient, and (3) making recommendations to improve care for the patient. Recent health care examples using computer models to identify patients experiencing adverse drug events, predicting future acute kidney injury, and recommending patient-specific treatment options provide insight into the benefits of a learning pharmacy practice.26–28 However, in addition to these potential benefits, the profession must also consider the potential unintended consequences of adopting these kinds of models in practice. Before the results of analyses lead to new knowledge being deployed and implemented into practice, all appropriate policy, trust, bias, equity, and quality considerations must be accounted for to prevent damaging unintended consequences.29
Step 4: Implementing new knowledge into the PPCP interaction
By step 4, we have almost completed the cycle in Figure 1. At this final step, better predictions, new knowledge of best practices, and other outcomes of previous analyses are applied at every step in a patient-pharmacist PPCP interaction. This incoming new knowledge from analytics is depicted by teal dots flowing into the PPCP at its planning step. Examples of new knowledge being implemented as the PPCP unfolds include notifying pharmacists and patients about the likelihood of adverse effects, the effectiveness of treatment alternatives, or the probabilities of specific outcomes. With this capability to deliver accurate, reliable predictions on the basis of the experiences of many patients in conjunction with actionable advice based on best practice knowledge, the pharmacist and the patient engaged in the PPCP interaction within the larger context of a learning pharmacy practice now have the best possible information available to guide their shared decision making.
This last step relies on not just what knowledge is communicated back into the PPCP interaction, but equally important, on how the knowledge is communicated.26 Incorporating predictions, new knowledge, and other outcomes of data analysis requires careful consideration about the interpretation of the results, design of data visualization, the user interface and experience, and the work environment of a learning pharmacy practice. Coupling predictions with related actionable advice in the right form, time, and place ensures that pharmacists and patients use best practice knowledge appropriately and effectively.30 To do this, pharmacists must work directly with systems engineers, information scientists, and implementation scientists to design effective human interactions with data-driven knowledge that support the PPCP and meet the needs of a larger learning pharmacy practice.26,29,31,32
Contrasting current practice with a learning pharmacy practice
Table 2 provides examples in a before-and-after comparison for describing how the PPCP unfolds today for an individual compared with how the PPCP would unfold in a future where a learning pharmacy practice has been established. Although the PPCP shares attributes with current and prospective applications in health care, the implementation of the PPCP in a learning pharmacy practice routinely applies and develops data-driven decision making in real time to help set tailored therapeutic goals, avoid unnecessary exposure to medications, and monitor medication use outcomes. These objectives can only be achieved when a learning pharmacy practice is achieved. Reinforcing this point, prediction is a critical element that threads its way through every PPCP component in a learning pharmacy practice. Although today, most pharmacists on the front lines executing the PPCP do so without the benefit of any data-driven predictions, in a learning pharmacy practice, pharmacists would enjoy data-driven knowledge about critical aspects of the patient’s past, current, and future medication use.
Table 2.
Comparison of the PPCP unfolding for an individual patient before and after the advent of a learning pharmacy practice
| PPCP component | Current pharmacy practice | Learning pharmacy practice |
|---|---|---|
| Collect | Common, descriptive, and periodic measures
|
Adds patient-specific, predictive, and fast-changing measures
|
| Assess | Analyze imprecise patient data
|
Shifts to precise patient assessments
|
| Plan | Ad hoc care plans
|
Shifts to evidence-based care plans that go beyond medication use
|
| Implement | Plans with mostly general and basic instructions
|
Shifts to personalized plans with instructions supported by ongoing tailored messaging
|
| Monitoring/follow-up | In-person and infrequent monitoring inconsistent with care plans
|
Shifts to remote, ongoing monitoring driven by care plans
|
Abbreviations used: Hb, hemoglobin; PHQ, patient health questionnaire; PPCP, pharmacists’ patient care process.
Although each step of the PPCP is necessary to achieve a learning pharmacy practice, the benefits are greatest at the critical planning step. Pharmacists accessing a patient’s comprehensive medical profile have a suite of tools that support the pharmacist evaluating the patient’s medication use and making care decisions with interpretable computer models. Designed by teams of pharmacists and data scientists, these tools provide patient-specific outcome predictions and treatment recommendations to help the pharmacist decide, for example, which medication the patient should take for their worsening disease. Pharmacists can see the predicted improvement in the clinical outcome measures between drugs and treatment options. An index that communicates patient-specific risk of adverse drug reactions they may experience could also be available. Although these examples highlight how a learning pharmacy practice can transform the profession, innovative knowledge tools will be created as pharmacists collaborate with data scientists in the future.
Call to action for a learning pharmacy practice
Pharmacists can embrace this practice transformation and support it through the systematic collection of data produced during PPCP interactions with all their patients. Pharmacy leaders can support this idea by implementing care processes that tend to formalize PPCP interactions and establish data-sharing procedures that allow for the aggregation and analysis of these real-world medication use data. In addition, integration of pharmacy PPCP records with health information exchanges can advance a learning pharmacy practice. Pharmacists and researchers should be focused on generating useful predictive models and other results that will offer needed insights from the data produced by PPCP interactions. It is essential to upgrade our knowledge of medication use through high-performance computer modeling. Pharmacists should have adequate training in the interpretation of novel predictive models and design strategies to facilitate use of that best practice knowledge for individual patients during PPCP interactions.
To have and maintain a learning pharmacy practice, we anticipate that as a core and permanent part of every pharmacist’s professional practice, pharmacists who provide direct patient care and execute the PPCP would be given some protected work-time during each week, each month, or each year, allowing them to participate in crucial activities needed to support continuous learning. These activities focus work on data standards, data use policy and ethics, conducting data science and analytics, communicating user-centered analytical results through graphical display, and implementing continuous practice improvement. For this to happen, professional societies must promulgate corresponding policies, state health codes must be amended to require that pharmacists devote some portion of work-time away from direct patient care to support the process of continuous learning, and federal policies must be aligned accordingly.
Conclusion
A learning pharmacy practice has the potential to revolutionize the profession of pharmacy and pave the way for achieving the Quintuple Aim. The purpose of a learning pharmacy practice is to gain and sustain population health improvements by systematically and precisely optimizing individual medication use in an equitable manner on a global scale. A learning pharmacy practice positions pharmacists as health care providers who conduct the PPCP, as drug experts who guide medication use analytics, and as producers and users of medication use predictions and knowledge. Ultimately, the use of a learning pharmacy practice will be tested on severe, relentless problems of patient safety, quality, and effectiveness. We believe that going for a continuous learning approach for the future of pharmacy practice will result in pharmacists and patients collaboratively demonstrating the value of a learning pharmacy practice in terms of useful predictions, more rapid production of knowledge, better health outcomes, more equitable care, improved patient experience, increased pharmacist well-being, and lower costs.
Key Points.
Background:
Pharmacists have critical new roles to develop and play as practice is transformed by data.
The collection and analysis of big data is bringing useful predictive models into pharmacy practice.
Findings:
A learning pharmacy practice is one that continually generates generalizable data-powered discoveries from patient care activities to improve our medication knowledge and help all people to achieve optimal health outcomes.
Pharmacists must establish a learning pharmacy practice to learn from every patient.
Funding:
Antoinette B. Coe is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number KL2;TR002241. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosure: Allen J. Flynn reports membership on the Autonomous Pharmacy Advisory Board and receives honoraria from the Omnicell corporation. Michael P. Dorsch reports honoraria from Janssen Pharmaceuticals, Inc and Amgen, Inc, outside the submitted work. The authors declare no other relevant conflicts of interest or financial relationships.
Contributor Information
Corey A. Lester, Department of Clinical Pharmacy, College of Pharmacy, University of Michigan, Ann Arbor, MI.
Antoinette B. Coe, Department of Clinical Pharmacy, College of Pharmacy, University of Michigan, Ann Arbor, MI.
Michael P. Dorsch, Department of Clinical Pharmacy, College of Pharmacy, University of Michigan, Ann Arbor, MI.
Karen B. Farris, Department of Clinical Pharmacy, College of Pharmacy, University of Michigan, Ann Arbor, MI.
Allen J. Flynn, Department of Learning Health Sciences, School of Medicine, University of Michigan, Ann Arbor, MI.
References
- 1.Joint Commission of Pharmacy Practitioners. Pharmacists’ patient care process Available at: https://jcpp.net/wp-content/uploads/2016/03/PatientCareProcess-with-supporting-organizations.pdf. Accessed December 2, 2019.
- 2.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm 1990;47(3):533–543. [PubMed] [Google Scholar]
- 3.Cipolle RJ, Strand LM, Morley PC. Pharmaceutical care practice Available at: https://pdfs.semanticscholar.org/d694/76b0563d0c5619c8bf174c2742b77663b055.pdf. Accessed December 5, 2019.
- 4.Kolar C, Hager KD, Losinski V. Beyond the pharmacists’ patient care process: cultivating patient care practitioners by utilizing the pharmaceutical care framework. Innov Pharm 2017;8(3):1–7. [Google Scholar]
- 5.Friedman CP, Rubin JC, Sullivan KJ. Toward an information infrastructure for global health improvement. Yearb Med Inform 2017;26(1):16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carayannis EG, Campbell DFJ. Mode 3 Knowledge Production in Quadruple Helix Innovation Systems New York, NY: Springer-Verlag New York; 2012. [Google Scholar]
- 7.Wuchty S, Jones BF, Uzzi B. The increasing dominance of teams in production of knowledge. Science 2007;316(5827):1036–1039. [DOI] [PubMed] [Google Scholar]
- 8.Balas EA, Boren SA. Managing clinical knowledge for health care improvement. Yearb Med Inform 2000;1(1):65–70. [PubMed] [Google Scholar]
- 9.Behrman RE, Benner JS, Brown JS, McClellan M, Woodcock J, Platt R. Developing the sentinel systemda national resource for evidence development. N Engl J Med 2011;364(6):498–499. [DOI] [PubMed] [Google Scholar]
- 10.Thomas MH, Goode JV. Development and implementation of a pharmacist-delivered Medicare annual wellness visit at a family practice office. J Am Pharm Assoc (2003) 2014;54(4):427–434. [DOI] [PubMed] [Google Scholar]
- 11.Flynn A Using artificial intelligence in health-system pharmacy practice: finding new patterns that matter. Am J Health Syst Pharm 2019;76(9): 622–627. [DOI] [PubMed] [Google Scholar]
- 12.Frey CB, Osborne MA. The future of employment: how susceptible are jobs to computerisation? Technol Forecast Soc Change 2017;114:254–280. [Google Scholar]
- 13.Spiro S Digital transformation of pharmacists’ clinical services. J Am Pharm Assoc (2003) 2019;59(2S):S8–S12. [DOI] [PubMed] [Google Scholar]
- 14.Williams MS, Buchanan AH, Davis FD, et al. Patient-centered precision health in a learning health care system: Geisinger’s genomic medicine experience. Health Aff (Millwood) 2018;37(5):757–764. [DOI] [PubMed] [Google Scholar]
- 15.Institute of Medicine (US). Roundtable on Evidence-Based Medicine. In: Olsen L, Aisner D, McGinnis JM, eds. The Learning Healthcare System: Workshop Summary Washington, DC: National Academy Press; 2007. [PubMed] [Google Scholar]
- 16.Agrawal A, Gans J, Goldfarb A. Prediction Machines: The Simple Economics of Artificial Intelligence Boston, MA: Harvard Business Review Press; 2018. [Google Scholar]
- 17.Rough K, Dai AM, Zhang K, et al. Predicting inpatient medication orders from electronic health record data [e-pub ahead of print]. Clin Pharmacol Ther doi: 10.1002/cpt.1826, accessed February 25, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen JH, Asch SM. Machine learning and prediction in medicine - beyond the peak of inflated expectations. N Engl J Med 2017;376(26): 2507–2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baldoni S, Amenta F, Ricci G. Telepharmacy services: present status and future perspectives: a review. Medicina (Kaunas) 2019;55(7):327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Badowski ME, Michienzi S, Robles M. Examining the implications of analytical and remote monitoring in pharmacy practice. Clin Pharm 2017;9(6):184–192. [Google Scholar]
- 21.Fassett WE. Patient Safety and Quality Improvement Act of 2005. Ann Pharmacother 2006;40(5):917–924. [DOI] [PubMed] [Google Scholar]
- 22.National Council for Prescription Drug Programs. Pharmacist eCare plan. Version 1.0. Guidance on the use of HL7 CDA consolidated templates for clinical notes R2.1 care plan Available at: https://www.ncpdp.org/NCPDP/media/pdf/Pharmacist-eCare-Plan.pdf. Accessed December 5, 2019.
- 23.Peleg M, Tu SW. Design patterns for clinical guidelines. Artif Intell Med 2009;47(1):1–24. [DOI] [PubMed] [Google Scholar]
- 24.Faden RR, Kass NE, Goodman SN, Pronovost P, Tunis S, Beauchamp TL. An ethics framework for a learning health care system: a departure from traditional research ethics and clinical ethics. Hastings Cent Rep 2013. Spec No:6-S27. [DOI] [PubMed] [Google Scholar]
- 25.Vayena E, Blasimme A, Cohen IG. Machine learning in medicine: addressing ethical challenges. PLoS Med 2018;15(11):e1002689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.London AJ. Artificial intelligence and black-box medical decisions: accuracy versus explainability. Hastings Cent Rep 2019;49(1):15–21. [DOI] [PubMed] [Google Scholar]
- 27.Tomašev N, Glorot X, Rae JW, et al. A clinically applicable approach to continuous prediction of future acute kidney injury. Nature 2019;572(7767):116–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Uzuner Ö, Stubbs A, Lenert L. Advancing the state of the art in automatic extraction of adverse drug events from narratives. J Am Med Inform Assoc 2020;27(1):1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matheny M, Israni ST, Ahmed M, et al. Artificial Intelligence in Health Care: The Hope, the Hype, the Promise, the Peril Washington, DC: National Academy of Medicine; 2019. [PubMed] [Google Scholar]
- 30.Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med 2019;25(1):44–56. [DOI] [PubMed] [Google Scholar]
- 31.National Science and Technology Council. Federal health information technology research and development strategic framework Available at: https://www.nitrd.gov/pubs/Federal-Health-IT-Strategic-Framework-2020.pdf. Accessed February 25, 2020.
- 32.Roth MG, Rubin JC, Omollo K, Friedman CP, Seagull FJ. The learning health-system: a new frontier for human factors. Proc Int Symp Hum Factors Ergon Health Care 2016;5(1):141–144. [Google Scholar]


