With the challenges in medical education created by the COVID-19 pandemic and the increasing competitiveness of surgical specialties, early exposure is critical for engaging medical students and providing them with the resources to pursue these fields.1 , 2 While clerkship rotations provide an immersive experience for medical students, they can only experience a limited number of specialties. Virtual medical education, which has become achievable due to technological advances prompted by the pandemic, can address these unmet needs. The COVID-19 pandemic has propelled many institutions to offer virtual electives; these experiences have largely focused on visiting medical students3 , 4 and those already in their clinical years.5 , 6
We present a novel and interactive way to engage preclinical (first- and second-year) medical students in virtual surgical education. A series of livestream surgeries was developed to provide students with early exposure to various surgical specialties in order to: (1) inform their decision-making about which clerkship rotations to choose; (2) assess level of interest in surgical specialties; and (3) facilitate mentorship.
All first- and second-year medical students (n = 212) at a single institution (Yale School of Medicine) were sent a survey link via the university email list server to indicate their interest in the livestream series by providing their email address and to indicate their level of interest in a surgical specialty. 77 of 212 (36.3%) students responded positively, while none responded negatively. The remaining 135 (63.7%) did not respond to the invitation. Prior to each livestream session, all 77 students who indicated interest were emailed details about the procedure and operating surgeon and a Zoom link. There were no requirements for student attendance, and students were free to choose which sessions to attend based on their own interests and/or availability. Five livestream sessions (each lasting 2–3 hours) were coordinated across 6 surgical specialties: Surgical Oncology, Cardiac Surgery, Urology, Plastic Surgery, Otolaryngology, and Neurosurgery. Procedures included cranioplasty, robotic prostatectomy, sinus surgery, breast reduction with lumpectomy, and aortic root replacement with coronary bypass surgery. These surgical specialties and selected cases were determined by availability of operating surgeons and their case schedules. Patient consent to livestream was obtained preoperatively.
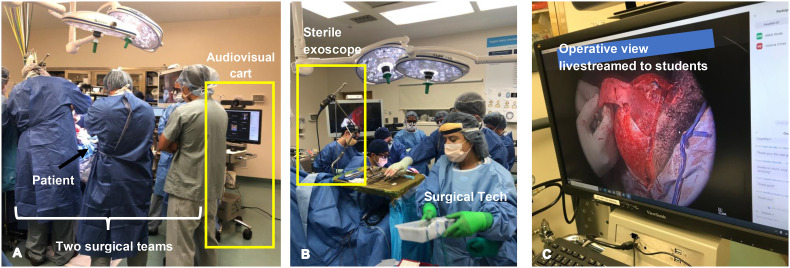
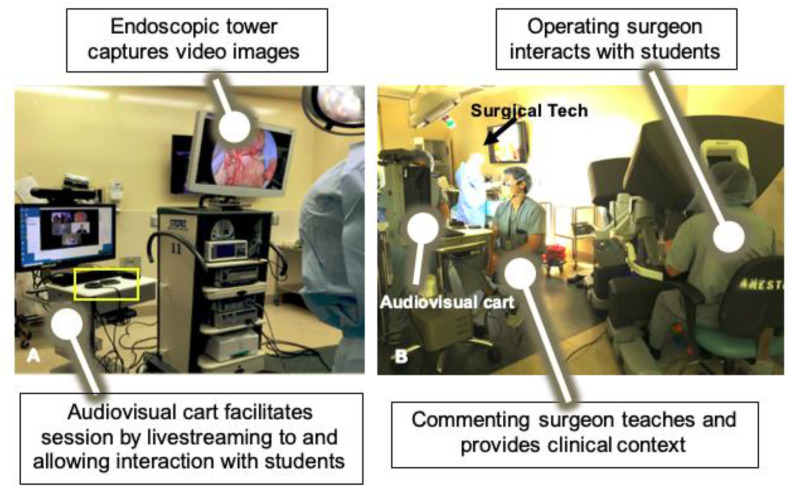
A mobile audiovisual cart (Fig. 1 ; Fig. 2 ), comprising a computer mounted with webcam and microphone/speaker, was utilized to live-stream via Zoom from 5 possible sources: exoscope,7 microscope, endoscope, robot, and operating room overhead light camera. The audiovisual cart and exoscope for this project was previously purchased by the hospital for clinical use and were temporarily repurposed for this project, thus no new funding or equipment purchases were necessary. Existing audiovisual personnel from the hospital IT department assisted with the initial set up for the first session (which took 1 h), after which members of the project team (H.P.S. and Y.H.L.) were able to set up and manage the equipment self-sufficiently in subsequent sessions. A commenting faculty member, fellow, or resident (“commenting or facilitating surgeon”), who was not the operating surgeon, was present to answer questions and facilitate student understanding of the procedure by reviewing anatomy, surgical instruments, patients’ clinical presentation and imaging, etc. (Fig. 2). While the commenting surgeons were the ones to primarily interact with the students, the operating surgeons also provided comments and teaching intermittently. To facilitate communication between the students, the operating surgeon, and the commenting surgeon, the microphone was moved around the operating room by the project team (H.P.S. and Y.H.L.). Commenting surgeon and project team members worked to adjust images and image sources based on clinical experience and real-time student feedback to ensure that students had an optimal view of the operative field.
Fig. 1.
Audiovisual cart (outlined by yellow rectangle in image A) consists of a computer and microphone/speaker that enables livestreaming and interaction with students via Zoom. The audiovisual cart takes up minimal space in a busy operating room with two teams (neurosurgery and plastic surgery) comprising the following gowned individuals: 2 operating surgeons, 4 residents, 1 surgical technologist. Sterile exoscope (yellow rectangle in image B), placed on operating room table, is used to livestream images to the audiovisual cart. Image C shows the audiovisual cart monitor displaying an example of a high-definition zoomed image seen from the exoscope, in this case, for a craniosynostosis repair.
Fig. 2.
A) Audiovisual cart (movable microphone outlined in yellow box) that enables livestreaming from multiple sources (endoscopic tower, robot) and B) interactions with the operating and commenting surgeons.
All operating surgeons were faculty within our institution who were recruited via email by the corresponding author. Recruitment was prioritized towards surgeons who had previously expressed interest in medical student education, such as residency and fellowship program directors and medical student clerkship directors. These operating surgeons were asked to recruit a resident or fellow within their surgical specialty to act as a commenting surgeon during the case, typically a resident working on the operating surgeon's service. Three cases each had one operating surgeon and one commenting surgeon, while two cases each had 2 operating surgeons each and one commenting surgeon; each commenting surgeon facilitated one case. Operating surgeons and commenting surgeons were able to participate in the livestream sessions without any prior training. Participation of all faculty, facilitators, project team members, and students was voluntary; there were no incentives or reimbursements offered or given for participation.
Following each livestream session, students were sent an anonymous survey via Qualtrics (Provo, UT) to gather feedback about the experience and its impact on their consideration of pursuing a surgical career. Descriptive analyses for each question were performed and figures were created using GraphPad Prism version 8 (San Diego, CA). A paired t-test was performed to compare students’ experiences with the operating surgeon versus the facilitating surgeon. The surveys were deemed exempt by the Institutional Review Board of Yale University.
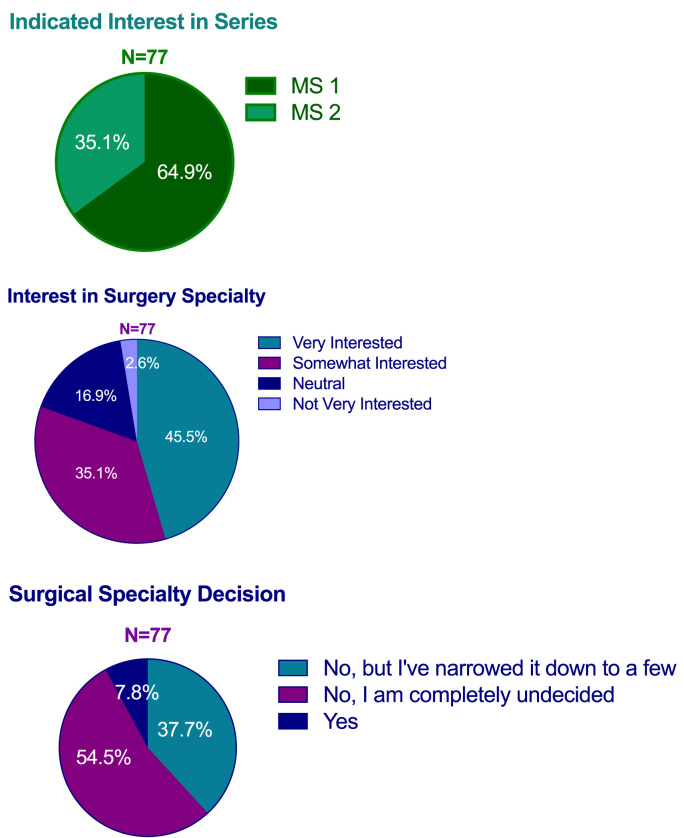
In the pre-session survey, 77 medical students indicated interest in the livestream surgery series: 50 (64.9%) were in their first year and 27 (35.1%) in their second year. Before participating in the livestream series, students had mixed levels of interest in a surgical field with 45.5% ‘Very interested’ in surgery, 35.1% ‘Somewhat interested’, 16.9% ‘Neutral’, and 2.6% ‘Not very interested’ in surgery (Fig. 3 ). Nearly half (54.5%) indicated that they were undecided about which surgical specialty to pursue. While we could not assess the total number of unique students that participated in one or more of the livestream sessions, given the voluntary and flexible design of the series, the number of students that joined each session ranged between 5 and 20.
Fig. 3.
Pre-session student interest in livestream surgery series and surgical fields.
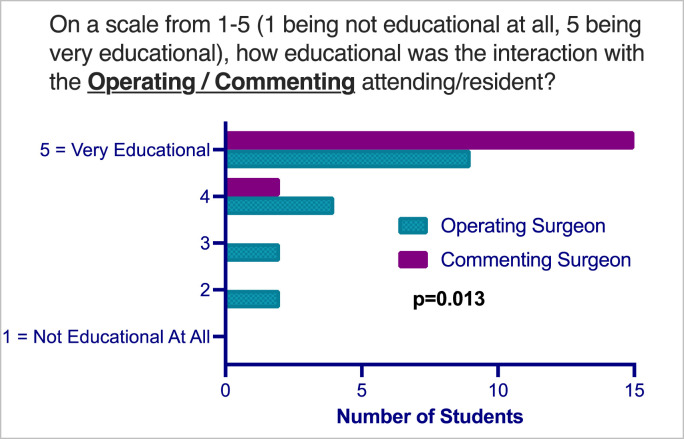
Seventeen students completed the anonymous post-session survey: 70.6% were in their first year and 29.4% in their second. In terms of the technology used, 100% of students reported that they had technical difficulties less than 20% of the time. All respondents said the quality of the audio and video were ‘Good’ or ‘Very Good’. On a 5-point scale, with 1 indicating ‘Not Educational at All’ and 5 indicating ‘Very Educational’, average rating of interactions with the facilitating surgeon was significantly higher than with the operating surgeon (4.9 ± 0.3 vs. 4.2 ± 1.1, respectively, p = 0.013) (Fig. 4 ). All respondents (100%) said having a dedicated commenting surgeon improved the educational experience. In the post-session survey, a large majority of participants (94%) indicated that the livestream series increased their interest in surgery; 6% said ‘no change’ after participating in the series. Most (88.2%) students would recommend this series to colleagues.
Fig. 4.
Assessment of interaction with operating and facilitating surgeons.
Innovations in virtual surgical education can widen the breadth of exposure, provide mentorship and research opportunities, and support informed decision-making about specialty choice. Virtual electives and virtual reality technologies8 have the capacity to enhance and transform medical education. While virtual viewing of surgeries cannot fully replace in-person operating room experiences, our livestream surgery series can guide students’ decision-making about which surgical specialties to dedicate time to experiencing in-person.
The decision to pursue surgery is multifactorial and driven by experience and mentorship. In their systematic review, Schmidt et al. found that mentorship, experience in surgery, and timing of exposure were among the top 5 factors that influence medical students decision to pursue surgery.9 This livestream surgery series enabled preclinical medical students to experience various types of surgeries (e.g. endoscopic, robotic, open procedures) and across multiple surgical specialties. Furthermore, the livestream sessions appealed to students with varying levels of interest in surgery, suggesting the utility of such educational innovations in guiding specialty decision-making. The presence of a dedicated commenting surgeon to teach during each session enhanced students’ learning experience and also provided access to additional potential mentors. Students interacted with both operating and commenting surgeons, many of whom provided their contact information to students and encouraged them to reach out for mentorship.
Often times in-person operating room experiences can be limiting for medical students when surgical teams consist of numerous individuals (Fig. 1) and the operative field is narrow. The livestreaming technology7 we employed provided high-resolution, zoomed-in aerial views of open procedures, enabling students to see more of the operative field and the surgical techniques. The audiovisual cart and movable microphone mitigated the onus of wearing additional equipment, such as a head-mounted camera, headphones, or microphones, which can be cumbersome for operating surgeons. The presence of project team member(s) to manage the equipment also enabled the operating and commenting surgeons to focus on their respective roles. In addition to optimized views, the design of this virtual surgery series allowed students flexibility: students could join the sessions for the full livestream length (2–3 hours) or for a portion of time suitable for their schedules.
The majority of students surveyed would recommend the livestream series to colleagues. In their free text responses, students independently indicated a desire for livestream sessions throughout the summer and in the future. Medical students who have participated in other virtual rotations have also agreed that virtual rotations should be continued in the future.10 Thus, virtual electives are a promising avenue for future medical education.
Virtual surgical education is not a true replacement for in-person operating room experience. Limitations include inability to acquire and demonstrate procedural skills and inability to learn how to be helpful in the operating room as a trainee. Future directions include periodically asking participants about the impact of the livestream series on their specialty decision-making and access to research and career mentorship. Additionally, because attendance was not mandated or recorded, we were unable to assess the total number of unique students who joined the series overall. Furthermore, the design of this livestream series and study may be impacted and limited by the Hawthorne Effect,11 which refers to changes in behavior resulting from subjects' awareness of being observed and to an unspecified number of unspecified effects on results due to participation in a study; future work may help address this effect. Limitations in our methods include lack of follow up on participating students. In future livestreaming series, we intend to include anonymous identifiers for students so that we can longitudinally assess the impact of this series on students’ decision to pursue surgical careers.
We present a novel interactive way to engage preclinical medical students in surgical education and provide exposure to a breadth of surgery types and specialties. Students reported that this livestream surgery series increased their interest in surgical fields. This livestream series may further enhance teaching efficiency by introducing a large number of students to surgery through virtual platforms that are not limited by the size of an operating room. Future efforts will expand the series to showcase other surgical specialties and at other hospitals and aim to periodically ask about research and career mentorship.
Financial disclosure
None.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
We have no known conflicts of interest to disclose.
References
- 1.Jarvis T., Aime V., Smith A. The impact of early exposure to plastic surgery on medical student specialty choice. Plast Reconstr Surg-Global Open. 2021;9(2S):13. doi: 10.1097/01.Gox.0000734996.96025.02. 23. [DOI] [Google Scholar]
- 2.Hicks K.E., Doubova M., Winter R.M., Seabrook C., Brandys T. Surgical exploration and discovery program: early exposure to surgical subspecialties and its influence on student perceptions of a surgical career. J Surg Educ. Sep-Oct 2019;76(5):1248–1257. doi: 10.1016/j.jsurg.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 3.Khoei A.A., Stocks B.T., Zhuo J., et al. Design and evaluation of a virtual Urology sub-internship during the COVID-19 pandemic. Curriculum, instruction, and pedagogy. Frontiers in Urology. 2022-June-03 2022 doi: 10.3389/fruro.2022.904484. 2doi. [DOI] [Google Scholar]
- 4.Patel S., Chawla A., Unruh M., et al. A proposed model for a comprehensive virtual subinternship in vascular surgery. J Vasc Surg. Dec 2021;74(6):2064–2071. doi: 10.1016/j.jvs.2021.05.045. e5. [DOI] [PubMed] [Google Scholar]
- 5.Chao T.N., Frost A.S., Brody R.M., et al. Creation of an interactive virtual surgical rotation for undergraduate medical education during the COVID-19 pandemic. J Surg Educ. Jan-Feb 2021;78(1):346–350. doi: 10.1016/j.jsurg.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Satnarine T., Lee Kin C.M. A review of virtual medical student rotations during the COVID-19 pandemic: their role, advantages, disadvantages, and future prospects. Cureus. 2022;14(4) doi: 10.7759/cureus.24280. e24280-e24280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shah H.P., Narwani V., Lee Y.H. Live-streaming otolaryngology surgical procedures for virtual medical student rotations. J Laryngol Otol. Mar 2022;136(3):261–264. doi: 10.1017/s0022215121004680. [DOI] [PubMed] [Google Scholar]
- 8.Pottle J. Virtual reality and the transformation of medical education. Future Healthc J. Oct 2019;6(3):181–185. doi: 10.7861/fhj.2019-0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmidt L.E., Cooper C.A., Guo W.A. Factors influencing US medical students' decision to pursue surgery. J Surg Res. Jun 1 2016;203(1):64–74. doi: 10.1016/j.jss.2016.03.054. [DOI] [PubMed] [Google Scholar]
- 10.Mason M.W., Aruma J.C. An orthopaedic virtual clinical clerkship for visiting medical students: early successes and future implications. J Surg Educ. Mar-Apr 2022;79(2):535–542. doi: 10.1016/j.jsurg.2021.09.019. [DOI] [PubMed] [Google Scholar]
- 11.McCambridge J., Witton J., Elbourne D.R. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. Mar 2014;67(3):267–277. doi: 10.1016/j.jclinepi.2013.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]