Abstract
Background
Cognitive behavioral therapy for adherence and depression (CBT-AD) performed by clinical psychologists is an effective treatment for improving the depression in people living with HIV (PLWH). However, because access to clinical psychologists is limited in most clinics, CBT-AD is rarely performed for PLWH in Korea. This pilot study evaluates whether CBT-AD can be effectively performed by a nurse trained and supervised by a clinical psychologist, with a view to the wider provision of CBT-AD.
Materials and Methods
One clinical psychologist developed manuals, educated and supervised one nurse. PLWH with depression or adherence to self-reported antiretroviral therapy <90% were enrolled, and CBT-AD was conducted once weekly for 12 sessions. PLWH were assessed for adherence by visual analog scale, Beck depression inventory (BDI) for depression, PozQoL for quality of life, and Berger’s 40-item stigma scale for stigma at baseline, after the 6th, 12th session, at 4-, and 8-months after CBT-AD. Acceptability for PLWH and feasibility for providers were evaluated through surveys.
Results
Five male PLWH have completed the study protocols (mean age 29.2 years). All study participants showed improving depression (mean BDI at baseline 33.0 ± 7.0, and after the 12th session 13.4 ± 3.5), and the effect was maintained at the 8-month follow-up (BDI 15.4 ± 6.4). Quality of life showed a tendency to improve (mean PozQoL at baseline 28.0 ± 7.7, after 12th session 36.8 ± 4.4, and at the 8-month follow-up 38.2 ± 7.9), but stigma did not show clear improvement (Berger’s 40-item stigma scale at baseline 121.0 ± 3.9, after 12th session 107.6 ± 8.8. and at the 8-month follow-up 107.6 ± 5.0). All study participants received great help from CBT-AD and expressed their desire to continue. All providers agreed that nurse-delivered CBT-AD could be implemented in routine clinical practice.
Conclusion
Our findings suggest that a nurse-delivered CBT-AD could be feasible and acceptable for PLWH through structured interventions. It has been shown to have the potential to help PLWH, especially for their depression and quality of life.
Trial Registration
ClinicalTrials.gov Identifier: NCT03823261
Keywords: Cognitive behavioral therapy, People living with HIV, Depression, Quality of life, Stigma
Introduction
With the development of antiretroviral therapy (ART) and advances in treatment guidelines, people living with human immunodeficiency virus (HIV) (PLWH) are living longer, and chronic management of their disease, including mental health, has become the main focus of care [1,2]. The prevalence of depression in PLWH is known to be higher than that of non-positive individuals, and a study conducted in Korea reported that the prevalence of anxiety and depressive symptoms of PLWH were 32% and 36%, respectively [3]. Depression of PLWH is a clinically significant problem and is associated with reduced adherence to ART [4]. Additionally, depression is associated with increased odds of dropping out of HIV care, a primary cause for treatment failure, and along with stigma, lowers the self-reported quality of life [5,6]. Also, stigma is a significant hurdle to linkage to care, especially in Korea [7]. In addition, although adherence to ART has improved due to many efforts, such as UNAIDS' '90-90-90' goal and ‘undetectable = untransmittable’ message, some PLWH still report difficulties in taking ART [8,9,10].
Cognitive behavioral therapy (CBT) has been proposed as one of the potential methods for improving mental health and ART adherence of PLWH. CBT is a manualized psycho-social intervention that aims to improve emotional regulation and change unhelpful cognitive distortions [11]. Several studies have investigated whether CBT for adherence and depression (CBT-AD) could be used to improve ART adherence and depression of PLWH and reported that CBT-AD was found to be effective [12,13]. However, most CBT-AD research has been conducted in Western or African countries, and it is not clear whether CBT-AD would be a successful intervention among Asian countries with relatively collectivist cultural backgrounds [14].
Specialists such as a psychiatrist or clinical psychologist would be the best therapist for CBT-AD intervention. However, access to them is limited in many areas, including Korea. Research on nurse-delivered CBT-AD has been conducted in recent years, but there are still relatively few studies given its potential and expected effects [15,16]. Medical personnel within most HIV clinics in Korea include infectious diseases doctors, clinical nurses, and counseling nurses. Hospital-based counseling services with experienced nurses have been provided in many HIV clinics in Korea, and the counseling nurses would be feasible providers for the CBT intervention examined in this study. Therefore, we have evaluated whether CBT-AD can be effectively performed by a nurse trained and supervised by a clinical psychologist, with a view to the wider provision of CBT-AD.
Materials and Methods
1. Study subjects
HIV infected Koreans with depression or ART adherence <90% were enrolled for this study. Eligibility criteria consisted of being an adult (18+ years), being HIV-positive, using ART, being fluent in Korean, having self-reported depression or self-reported ART adherence <90%, and has voluntarily agreed to participate in the research and provided written consent. Participants would be excluded from the study if they are psychotic or have an uncontrolled neurological problem, or expressed suicidal ideation. Additional exclusion criteria included (1) having been initiated on or had their dose of psychotropic medication altered within the past three months, (2) currently receiving psychotherapy for depression, or (3) having previously received CBT.
2. Ethics statement
This study was approved by the Institutional Review Board (IRB) of the Yonsei University Health System Clinical Trial Center (4-2018-0755). Informed consent was obtained from all study participants before enrollment.
3. Intervention
For conducting nurse-delivered CBT-AD, one clinical psychologist developed manuals, and educated and supervised one nurse. The newly developed manuals were based on papers, books, and several existing manuals on CBT-AD for PLWH [13,17]. They were designed for therapists and contained descriptions of effective techniques that might be applied to treatment, and a worksheet for implementing tasks. The manuals also summarized the theoretical concepts of CBT-AD, which were the basis of treatment, and the principles of each technique. The samples of the manual and worksheet in Korean can be found in the supplementary file.
The education process consisted of three sessions of relevant book reading and discussion, six manual education sessions, and 14 supervision sessions conducted by the clinical psychologist to the nurse. Each education session was held for 2 hours. Since the therapist’s attitude is a very important factor in CBT-AD even though it is a structured treatment, we prepared 14 supervision sessions to ensure that the nurse therapist is listening to, supporting, understanding, empathizing, respecting, and accepting clients. After the manual education, an assessment was performed to verify the nurse’s knowledge.
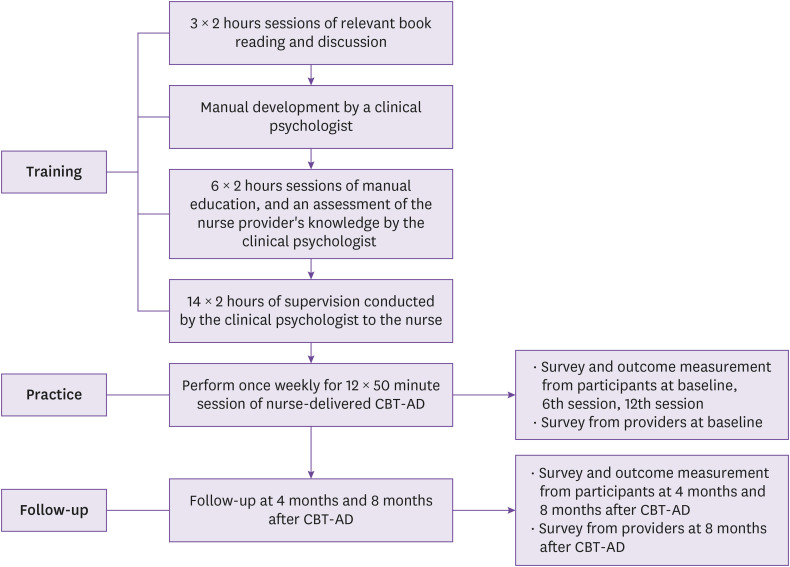
After the education, CBT-AD was conducted by a nurse at the PLWH once weekly for 12 sessions. Each CBT session consisted of 50 minutes. Patients were monitored for their activity, ART adherence, and emotion through a self-written structured worksheet each session. In addition, at the end of each session, the contents and meanings of the session are summarized, and detailed feedback and the therapist's opinions are presented as much as possible. During the study period, two infectious disease doctors and a clinical nurse performed usual medical care to the patients and checked for any side effects. The contents of each session are summarized in Table 1, and the whole process for the implementation of nurse-delivered CBT-AD is shown in Figure 1.
Table 1. The summarized contents in each session of cognitive behavioral therapy for adherence and depression.
| Session order | Summarized contents |
|---|---|
| 1st session | • Introduction of therapist and treatment method |
| • General information collection | |
| • Rapport formation | |
| 2nd session | • Obtain an overview of target symptoms through 12 steps |
| • Focus on training about the importance of medication prescription | |
| • Motivation for treatment through interviews | |
| 3rd session | • Explanation of how cognitive behavioral therapy works |
| • Focus on thinking, emotions, and behaviors: explanation and practice of cognitive errors | |
| 4th session | • Introduction of other cognitive techniques (conversion of perspective, etc.) |
| • Introducing behavior activation techniques | |
| 5th session | • Cognitive technique/behavior activation technique check and correction |
| • Behavior test methods introduction | |
| • Practice of relaxation | |
| 6th session | • Check and readjust cognitive techniques, behavior activation techniques, and behavior experiment techniques |
| 7th session | • Problem solving strategy |
| 8th session | • How to cope with stress |
| 9th session | • Self-assertion training |
| 10th session | • Applying the techniques learned so far on the subject of stigma and self-image |
| 11th session | • Supplemental session: Subjects the patient wants to talk about on a voluntary basis (can cover any session from session 3 to session 10) |
| 12th session | • Summary of sessions, check changes, and setting of future goals |
| • Preventing recurrence and finishing the program |
Figure 1. Study flow of the implementation of nurse-delivered cognitive behavioral therapy for adherence and depression.
CBT-AD, cognitive behavioral therapy for adherence and depression.
4. Outcomes assessment
1) Patient outcomes
To assess the effectiveness of nurse-delivered CBT-AD, we checked whether ART adherence, depression, quality of life, and stigma of PLWH have improved after CBT-AD. For measuring ART adherence, a visual analog scale tool (range 0 - 100%), validated by the World Health Organization, was used [18,19]. Depression was assessed using the Beck depression inventory (BDI, scoring range 0 - 63, higher score means more depressed) [20,21]. Quality of life was evaluated through the PozQoL scale, which is a short, validated and freely available scale assessing the quality of life among PLWH (scoring range 13 - 65, a higher score means a higher quality of life) [22]. Berger’s 40-item the stigma scale was used for assessing stigma of PLWH (scoring range 40 - 160, the higher the score, the greater the stigma) [23]. At last, HIV viral load and CD4 cell count were examined from the participant’s medical records. Patient outcomes were evaluated before the start (baseline), after the 6th session, after the 12th session, 4 months after the CBT-AD, and 8 months after CBT-AD. Since the number of participants was small, the results were presented as mean ± standard deviation or descriptively.
2) Implementation outcomes
The primary outcome of this study is whether nurse-delivered CBT-AD for PLWH is acceptable and feasible for patients and providers in Korea. Acceptability of nurse-delivered CBT-AD to PLWH was evaluated through surveys by PLWH who participated in this study at baseline, after the 6th session, after the 12th session, 4 months after the CBT-AD, and 8 months after CBT-AD. Feasibility was assessed by providers through surveys at baseline and 8 months after CBT-AD. Providers included two infectious diseases doctors, a clinical nurse, and a counseling nurse who participated in this study.
Results
1. Demographics
Five PLWHs met the eligibility criteria and participated in this study. The demographics of the study participants were shown in Table 2. All study participants were men, and the mean age was 29.2 years (range, 26 - 34 years). HIV diagnosis and ART duration were for an average of 5 years (range, 1 - 8 years). At the baseline of the study, the HIV viral load was less than 20 copies/mL in four patients, and the CD4 T-cell count was maintained above 200/mm3 in all participants.
Table 2. Demographics and baseline characteristics of study participants.
| Characteristics | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 |
|---|---|---|---|---|---|
| Age (years) | 29 | 26 | 28 | 29 | 34 |
| Sex | M | M | M | M | M |
| Height (cm) | 182 | 166 | 185 | 183 | 179 |
| Weight (kg) | 76 | 55 | 107 | 91 | 70 |
| Body mass index | 22.9 | 20.0 | 31.3 | 27.2 | 21.8 |
| Transmission mode | MSM | MSM | Hetero | MSM | Bisexual |
| Current smoker | No | Yes | Yes | Yes | No |
| Drinking alcohol | Yes | Yes | Yes | Yes | Yes |
| Educational attainment | University | University | University | University | University |
| Marital status | Single | Single | Single | Single | Single |
| Employment status | Yes | Yes | Yes | Yes | Yes |
| Living situation | Alone | Alone | With mother | With parents | With mother |
| Religion | No | No | Yes | Yes | No |
| Disability | No | No | No | No | No |
| Other diseases | No | No | No | Lymphoma | No |
| Years after HIV diagnosis | 1 year | 2 years | 7 years | 7 years | 8 years |
| Years of taking ART | 1 year | 2 years | 7 years | 7 years | 8 years |
| Initial viral load (copies/mL) | 2.25 × 106 | 1.18 ×106 | >1.0 × 107 | >1.0 × 107 | 6.18 × 104 |
| Initial CD4 T-cell count (/mm3) | 370 | 569 | 129 | 423 | 176 |
| Highest viral load (copies/mL) | 2.25 × 106 | 1.18 × 106 | >1.0 × 107 | >1.0 × 107 | 6.18 × 104 |
| Nadir CD4 T-cell count (/mm3) | 370 | 569 | 129 | 48 | 176 |
| Baseline viral load (copies/mL) | 71.9 | <20 | <20 | <20 | <20 |
| Baseline CD4 T-cell count (/mm3) | 537 | 983 | 1,043 | 264 | 680 |
| ART regimen | 3TC+ABC+DTG | TAF+FTC+DRV/c | TAF+FTC+DRV/c | 3TC+ABC+DTG | 3TC+ABC+EFV |
MSM, men who have sex with men; HIV, human immunodeficiency virus; ART; antiretroviral therapy; 3TC, lamivudine; ABC, abacavir; DTG, dolutegravir; TAF, tenofovir alafenamide; FTC, emtricitabine; DRV/c, cobicistat-boosted darunavir; EFV, efavirenz.
2. Intervention effects upon outcomes
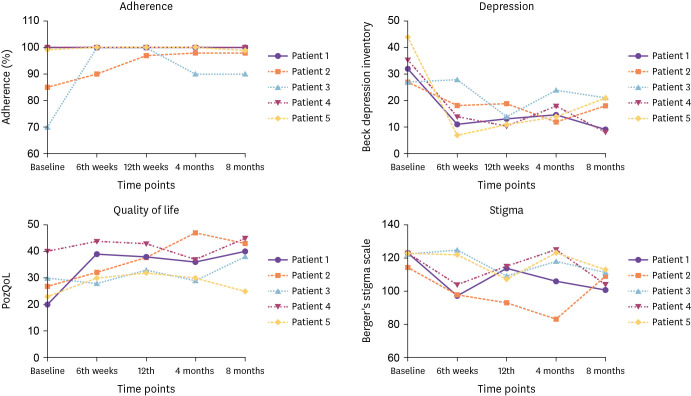
Overall, ART adherence of participants was either achieved or maintained over the study duration (mean adherence at baseline 90.8% ± 13.3%, after 12th session 99.4% ± 1.3%, at the 8-month follow-up 97.4% ± 4.2%), and depression was improved (mean BDI at baseline 33.0 ± 7.0, after 12th session 13.4 ± 3.5, at the 8-month follow-up 15.4 ± 6.4). The quality of life of participants showed some improvement (mean PozQoL at baseline 28.0 ± 7.7, after 12th session 36.8 ± 4.4, and at the 8-month follow-up 38.2 ± 7.9); however, stigma did not show clear improvement effects (Berger’s 40-item stigma scale at baseline 121.0 ± 3.9, after 12th session 107.6 ± 8.8. and at the 8-month follow-up 107.6 ± 5.0). The ART adherence of Patient 1 was maintained at 100% from the baseline until 8 months after CBT-AD. In the case of BDI, the score was improved during CBT-AD and continued to be low afterward. The PozQoL and stigma scale improved with the progress of CBT-AD and was maintained. In Patient 2, ART adherence was improved during CBT-AD, and the BDI and PozQoL scales also improved. The stigma scale was improved until 4 months after CBT-AD; however, after 8 months, it returned to near baseline. The ART adherence of Patient 3 was improved from baseline 70% to 100% during CBT-AD but then decreased again to 90%. Meanwhile, BDI, PozQoL scale, and stigma scale were all improved during the study timeframe. Both Patients 4 and 5 maintained good ART adherence and showed strong improvement in depression, but no significant improvement was observed on the PozQoL or stigma scale. The results are summarized in Figure 2.
Figure 2. Changes of outcome parameters of patients according to cognitive behavioral therapy for adherence and depression implementation.
3. Acceptability
At baseline, participants expressed that their main motivations for participation in CBT-AD were an improvement in quality of life (4 patients) and overcoming depression (3 patients). After the 12th session of CBT-AD, all participants wished to continue CBT-AD, and the main reasons given for continuing were improved quality of life (3 patients), depression (2 patients), and improved ART adherence (1 patient). The participant reported potential improvements in the CBT-AD program, including the desire for continued CBT-AD (3 patients), and that the composition of the program could be improved (2 patients). The questionnaire and results are shown in Table 3.
Table 3. Survey results on the acceptability of the study participants.
| Questions | Time points | |||
|---|---|---|---|---|
| Baseline | 12th session | 8 month | ||
| Q1. Why did you decide to take CBT-AD? (multiple selections possible) | ||||
| A. I want to take the medication better. | 0 | 1 | 1 | |
| B. I want to overcome depression. | 3 | 3 | 4 | |
| C. I want to improve my quality of life. | 4 | 3 | 5 | |
| D. I want to overcome the stigma of myself. | 0 | 0 | 1 | |
| Q2. Are you willing to continue on CBT-AD? | ||||
| A. Absolutely | 3 | 3 | 3 | |
| B. Yes | 2 | 2 | 2 | |
| C. No | 0 | 0 | 0 | |
| D. Not at all | 0 | 0 | 0 | |
| Q3. If you want to continue CBT-AD, why do you want to continue? (multiple selections possible) | ||||
| A. It makes me take medication better. | 0 | 1 | 1 | |
| B. It helps improve depression. | 3 | 2 | 3 | |
| C. It helps improve the quality of life. | 3 | 3 | 4 | |
| D. It helps overcome stigma. | 1 | 0 | 0 | |
| Q4 When receiving CBT-AD, what do you think the program should improve? (multiple selections possible) | ||||
| A. I would like to hear more explanations about the necessity and procedure of CBT-AD. | 1 | 0 | 2 | |
| B. I hope that the program of CBT-AD is better organized. | 3 | 2 | 4 | |
| C. I would like to adjust the time and frequency of receiving CBT-AD. | 0 | 0 | 1 | |
| D. I hope it will continue to be implemented. | 2 | 3 | 2 | |
CBT-AD, cognitive behavioral therapy for adherence and depression.
4. Feasibility
Providers of the study were aware of CBT-AD to some extent at baseline but had not experienced it. After CBT-AD was completed, they all thought that nurse-delivered CBT-AD could be implemented in actual clinical practice. They all thought that ART adherence, depression, and quality of life could be improved through CBT-AD, and half of them agreed on overcoming stigma. To establish CBT-AD in clinical practice, the need for reinforcement of human resources, economic compensation, and institutional support was expressed. Through this study, they thought that nurse-delivered CBT-AD could be applied in routine clinical practice through short-term education and supervision; however, they all agreed that it is difficult to combine it with existing tasks. Table 4 shows the contents of the questionnaire on the feasibility and the results.
Table 4. Survey results on the feasibility of the study providers.
| Questions | Time points | ||
|---|---|---|---|
| Baseline | 8 month | ||
| Q1. How much do you know about CBT-AD? | |||
| A. I have never heard of it. | 0 | 0 | |
| B. I've heard it before, but I don't know the content. | 0 | 0 | |
| C. I am aware of the content to some extent but have not experienced it. | 3 | 0 | |
| D. I have experienced it around me, but I have never actively participated. | 1 | 0 | |
| E. I have actively participated in implementation. | 0 | 4 | |
| Q2. Do you think CBT-AD can be introduced and used in actual clinical practice? | |||
| A. Absolutely | 2 | 4 | |
| B. Yes | 2 | 0 | |
| C. No | 0 | 0 | |
| D. Not at all | 0 | 0 | |
| Q3. If you think CBT-AD has been introduced and can be used, why? (multiple selections possible) | |||
| A. CBT-AD can improve patient compliance. | 3 | 4 | |
| B. Through CBT-AD, the patient's depression can be improved. | 4 | 4 | |
| C. The patient's quality of life can be improved through CBT-AD. | 4 | 4 | |
| D. It helps overcome the patient's stigma through CBT-AD. | 2 | 2 | |
| E. Cost and time consumption are not large compared to the expected effect. | 1 | 0 | |
| Q4. What do you think needs improvement for the settlement of CBT-AD? (multiple selections possible) | |||
| A. I think it is necessary to reinforce human resources as it consumes a lot of time for effective CBT-AD | 4 | 4 | |
| B. I think that economic compensation for the implementation of CBT-AD is necessary for continued promotion. | 4 | 4 | |
| C. I think the program of CBT-AD needs to be better organized. | 1 | 1 | |
| D. I think it is necessary to control the time and frequency of receiving CBT-AD. | 3 | 2 | |
| E. I think there is a need for institutional support for the settlement of CBT-AD. | 2 | 3 | |
| Q5. What do you think about the feasibility of CBT-AD provided by a counseling nurse? (multiple selections possible) | |||
| A. It can be applied in actual clinical practice through the current short-term education period and supervision. | 2 | 2 | |
| B. Since the training period is insufficient, it is difficult to proceed, so extending the training period can be applied well. | 1 | 0 | |
| C. Education is appropriate, but I hope to strengthen supervision and feedback. | 1 | 0 | |
| D. Since the content is professional, it is unreasonable to apply it even if you receive an education. | 0 | 1 | |
| E. CBT-AD can be applied well, but it is difficult to combine it with existing tasks. | 2 | 4 | |
CBT-AD, cognitive behavioral therapy for adherence and depression.
Discussion
In this pilot study, we investigated whether a nurse who received education and supervision from a clinical psychologist could conduct CBT-AD and achieve improvements in patient outcomes ART adherence, depression, stigma, and quality of life of PLWH. This is the first nurse-delivered CBT-AD program for PLWH in Korea, and despite the small number of participants, this study has produced some valuable insights and results.
To enable nurse-delivered CBT-AD, we developed structured manuals, education programs, and supervision sessions. We then applied it to this research and verified whether it is feasible. As a result, as confirmed in questionnaires, all of the providers participating in the study agreed that nurse-delivered CBT-AD could be introduced and used in actual clinical practice and improve the mental health of PLWH. In Korea, a Nationwide Specialized Counseling Program for PLWH has been introduced, and there are nurses in charge of counseling programs [24]. Through this study, it was demonstrated that a nurse could perform CBT-AD if they received suitable education and supervision, which suggests that it may be of great help to PLWH's quality of life and care when linked with Korean counseling programs. On the other hand, as suggested in the survey of providers, some areas need improvement for continuous implementation. The most important issues were those related to human resources and economic compensation. As a considerable amount of time and effort is required to conduct CBT-AD, providers reported it is difficult to perform simultaneously existing work and CBT-AD. This may mean that for the implementation of nurse-delivered CBT-AD, it will be necessary to supplement human and medical resources through government policy support and insurance payments, not just the efforts of some medical staff. Also, as the effectiveness of CBT-AD can be influenced by the competency of a nurse to conduct, it is necessary to verify feasibility in an expanded environment through standardized education and programs such as those developed in this study.
The main motivations of PLWH for participating in this study were improving their depression and quality of life and as reported over multiple time points in this study through questionnaires benefits were observed. In addition, all study participants expressed that nurse-delivered CBT-AD was acceptable and hoped to continue, confirming that nurse-delivered CBT-AD is applicable in actual clinical practice. Meanwhile, the study participants cited improvement in the composition of the CBT-AD program as an item that needed some improvement in addition to wishing to continue receiving CBT-AD after the study period, which warrants the requirement of the program modifications in the future.
In our sample, ART adherence over the 8 months was either achieved or maintained at a very high level although one patient increased adherence to an optimum level during CBT-AD this fell to a reduced level during follow-up at months 4 and 8, albeit still above baseline. In general ART adherence was regarded as well maintained, and viral load and CD4 T cell count remained normal for study participants in continuous tests during the study period.
The most notable effect was observed in the improvement of depression. In all of the study participants, depression was improved during CBT-AD, and the effect was maintained at the 8-month follow-up survey after CBT-AD has stopped. In Patient 5, during the follow-up, the BDI score was increased again, but compared with the initial high BDI score, it could be concluded that the depression improved overall.
The quality of life data was not as pronounced as depression but showed some improvement, however stigma did not show clear improvement effects. This meant that overcoming the stigma is not easily accomplished through CBT-AD. It might have been related to the relatively severe stigma of HIV in Eastern Asian cultures [14,25]. As the stigma of PLWH affects many medical conditions including ART adherence, more efforts to overcome the stigma are required [26,27].
There are several limitations to this study. First, there were only five PLWHs who participated in the study. Although the participants in the study particularly showed improving depression, the statistical analysis regarding the intervention outcomes could not be conducted due to the small number of participants. As this pilot study showed that nurse-delivered CBT-AD could be implemented, statistical validation of intervention effects is needed through sufficient participant enrollment in future studies. Second, CBT-AD was performed by only one nurse in this study. In CBT-AD, the relationship between therapist and participant is an important part of the therapeutic effect. Therefore, although we prepared structured manuals, curricula, examinations, and many supervision sessions, treatment effects may vary depending on the person conducting CBT-AD. This study could not prove whether there were differences in outcomes between nurses due to human resources problems. It should be proved in future large scale studies, and for that, it is necessary to reinforce human and medical resources through government policy support and insurance payments, as in the survey results in this study.
In conclusion, our findings suggest that a nurse-delivered CBT-AD could be feasible and acceptable for PLWH through structured interventions. It has been shown to have the potential to help improve depression and the quality of life in PLWH. The implementation of this nurse-delivered intervention should be studied more widely in clinical practice to promote the mental care of PLWH and its potential contribution to nursing activities.
ACKNOWLEDGEMENT
The authors thank Medical Illustration & Design, part of the Medical Research Support Services of Yonsei University College of Medicine, for the graphic abstract.
Footnotes
Funding: This study was supported by ViiV Healthcare (ViiV Implementation Science Program, eTrack 210029).
Conflict of Interest: No conflict of interest.
- Conceptualization: JYC.
- Data curation: JHK, SN.
- Formal analysis: JHK.
- Funding acquisition: JYC.
- Investigation: JHK, JMK, MY, JIL.
- Methodology: MY, YL.
- Project administration: JYC.
- Resources: JMK, MY, JIL, SN.
- Software: JHK, SN.
- Supervision: MY, YL, JYC.
- Validation: JHK, DS, JYC.
- Visualization: JHK.
- Writing - original draft: JHK.
- Writing - review & editing: JHK, JMK, MY, JIL, SN, YL, DS, JYC.
References
- 1.Korean Society for AIDS. Summary of 2021 clinical guidelines for the diagnosis and treatment of HIV/AIDS in HIV-infected Koreans. Infect Chemother. 2021;53:592–616. doi: 10.3947/ic.2021.0305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wandeler G, Johnson LF, Egger M. Trends in life expectancy of HIV-positive adults on antiretroviral therapy across the globe: comparisons with general population. Curr Opin HIV AIDS. 2016;11:492–500. doi: 10.1097/COH.0000000000000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kee MK, Lee SY, Kim NY, Lee JS, Kim JM, Choi JY, Ku NS, Kang MW, Kim MJ, Woo JH, Kim SW, Song JY, Baek JH, Choi BY, Kim SS. Anxiety and depressive symptoms among patients infected with human immunodeficiency virus in South Korea. AIDS Care. 2015;27:1174–1182. doi: 10.1080/09540121.2015.1035861. [DOI] [PubMed] [Google Scholar]
- 4.Uthman OA, Magidson JF, Safren SA, Nachega JB. Depression and adherence to antiretroviral therapy in low-, middle- and high-income countries: a systematic review and meta-analysis. Curr HIV/AIDS Rep. 2014;11:291–307. doi: 10.1007/s11904-014-0220-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rooks-Peck CR, Adegbite AH, Wichser ME, Ramshaw R, Mullins MM, Higa D, Sipe TA Prevention Research Synthesis Project. Mental health and retention in HIV care: A systematic review and meta-analysis. Health Psychol. 2018;37:574–585. doi: 10.1037/hea0000606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turan B, Budhwani H, Fazeli PL, Browning WR, Raper JL, Mugavero MJ, Turan JM. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav. 2017;21:283–291. doi: 10.1007/s10461-016-1451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi JP, Seo BK. HIV-related stigma reduction in the era of undetectable equals untransmittable: The South Korean perspective. Infect Chemother. 2021;53:661–675. doi: 10.3947/ic.2021.0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cho YM, Chin B. Assessment of human immunodeficiency virus care continuum in Korea using the national health insurance system data. Infect Chemother. 2021;53:477–488. doi: 10.3947/ic.2021.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lazarus JV, Safreed-Harmon K, Barton SE, Costagliola D, Dedes N, Del Amo Valero J, Gatell JM, Baptista-Leite R, Mendão L, Porter K, Vella S, Rockstroh JK. Beyond viral suppression of HIV - the new quality of life frontier. BMC Med. 2016;14:94. doi: 10.1186/s12916-016-0640-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Croome N, Ahluwalia M, Hughes LD, Abas M. Patient-reported barriers and facilitators to antiretroviral adherence in sub-Saharan Africa. AIDS. 2017;31:995–1007. doi: 10.1097/QAD.0000000000001416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brewin CR. Theoretical foundations of cognitive-behavior therapy for anxiety and depression. Annu Rev Psychol. 1996;47:33–57. doi: 10.1146/annurev.psych.47.1.33. [DOI] [PubMed] [Google Scholar]
- 12.Safren SA, O’Cleirigh CM, Bullis JR, Otto MW, Stein MD, Pollack MH. Cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected injection drug users: a randomized controlled trial. J Consult Clin Psychol. 2012;80:404–415. doi: 10.1037/a0028208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Safren SA, Bedoya CA, O’Cleirigh C, Biello KB, Pinkston MM, Stein MD, Traeger L, Kojic E, Robbins GK, Lerner JA, Herman DS, Mimiaga MJ, Mayer KH. Cognitive behavioural therapy for adherence and depression in patients with HIV: a three-arm randomised controlled trial. Lancet HIV. 2016;3:e529–e538. doi: 10.1016/S2352-3018(16)30053-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zang C, Guida J, Sun Y, Liu H. Collectivism culture, HIV stigma and social network support in Anhui, China: a path analytic model. AIDS Patient Care STDS. 2014;28:452–458. doi: 10.1089/apc.2014.0015. [DOI] [PubMed] [Google Scholar]
- 15.Andersen LS, Magidson JF, O’Cleirigh C, Remmert JE, Kagee A, Leaver M, Stein DJ, Safren SA, Joska J. A pilot study of a nurse-delivered cognitive behavioral therapy intervention (Ziphamandla) for adherence and depression in HIV in South Africa. J Health Psychol. 2018;23:776–787. doi: 10.1177/1359105316643375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han S, Hu Y, Relf MV, Mulawa MI, Lu H, Zhang L, Zhu Z, Luo J, Pei Y, Wu B. Effects of nurse-delivered cognitive behavioral intervention on depression and anxiety for persons living with HIV in China: A clinical controlled trial. J Assoc Nurses AIDS Care. 2021;32:79–93. doi: 10.1097/JNC.0000000000000213. [DOI] [PubMed] [Google Scholar]
- 17.Newcomb ME, Bedoya CA, Blashill AJ, Lerner JA, O’Cleirigh C, Pinkston MM, Safren SA. Description and demonstration of cognitive behavioral therapy to enhance antiretroviral therapy adherence and treat depression in HIV-infected adults. Cognit Behav Pract. 2015;22:430–438. doi: 10.1016/j.cbpra.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Giordano TP, Guzman D, Clark R, Charlebois ED, Bangsberg DR. Measuring adherence to antiretroviral therapy in a diverse population using a visual analogue scale. HIV Clin Trials. 2004;5:74–79. doi: 10.1310/JFXH-G3X2-EYM6-D6UG. [DOI] [PubMed] [Google Scholar]
- 19.Finitsis DJ, Pellowski JA, Huedo-Medina TB, Fox MC, Kalichman SC. Visual analogue scale (VAS) measurement of antiretroviral adherence in people living with HIV (PLWH): a meta-analysis. J Behav Med. 2016;39:1043–1055. doi: 10.1007/s10865-016-9770-6. [DOI] [PubMed] [Google Scholar]
- 20.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 21.Saal W, Kagee A, Bantjes J. Utility of the Beck Depression Inventory in measuring major depression among individuals seeking HIV testing in the Western Cape, South Africa. AIDS Care. 2018;30(Suppl 1):29–36. doi: 10.1080/09540121.2018.1499856. [DOI] [PubMed] [Google Scholar]
- 22.Brown G, Mikołajczak G, Lyons A, Power J, Drummond F, Cogle A, Allan B, Cooper C, O’Connor S. Development and validation of PozQoL: a scale to assess quality of life of PLHIV. BMC Public Health. 2018;18:527. doi: 10.1186/s12889-018-5433-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24:518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 24.Kim JM, Kim NJ, Choi JY, Chin BS. History of acquired immune deficiency syndrome in Korea. Infect Chemother. 2020;52:234–244. doi: 10.3947/ic.2020.52.2.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xie T, Yang JP, Simoni JM, Shiu CS, Chen WT, Zhao H, Lu H. Unable to be a human being in front of other people: A qualitative study of self-isolation among people living with HIV/AIDS in China. J Clin Psychol Med Settings. 2017;24:211–222. doi: 10.1007/s10880-017-9513-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, Tsai AC. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(Suppl 2):18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rueda S, Mitra S, Chen S, Gogolishvili D, Globerman J, Chambers L, Wilson M, Logie CH, Shi Q, Morassaei S, Rourke SB. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open. 2016;6:e011453. doi: 10.1136/bmjopen-2016-011453. [DOI] [PMC free article] [PubMed] [Google Scholar]