Abstract
Background:
Referral for kidney transplantation is influenced by patient education; digital technologies can enhance broad information accessibility. This single-group study tested the feasibility and acceptability of patient-centered self-directed educational animated videos to improve mediators of kidney transplant referral.
Methods.
Community-based adults with chronic kidney disease stage ≥4 invited from a clinical registry viewed 8 sequential videos (19:36 minutes total duration) remotely on their own device. Change in kidney transplant knowledge, concerns, and confidence talking about kidney transplantation to doctors was assessed with self-report surveys before and immediately after viewing. Program feedback was assessed by survey and self-selected exit interview.
Results.
Viewers of the video set (n=50) demonstrated increases in mean kidney transplantation knowledge by +22%, confidence discussing with their doctor by +6%, and reductions in concerns by −2%. Knowledge results were consistent across age, race, and literacy level. Over 90% indicated positive ratings on understanding, engaging, and helpfulness. In post-study interviews viewers indicated the videos promoted confidence in obtaining a kidney transplant and none reported that the 19-minute duration of the home education was too long.
Conclusion.
The animated video education is promising to improve diverse individuals’ knowledge, concerns, and communication confidence about kidney transplantation and is highly acceptable.
Keywords: kidney transplant, Kidney transplant access, community-based participatory research, digital media, health education, animation
INTRODUCTION
Over a half million Americans are dialysis-dependent or nearing dialysis; yet, only 20% are waitlisted for a kidney transplant,1,2 the best treatment for a better, longer life.3,4 The first step to waitlist placement is referral to a transplant center. In one study of 690 southeastern dialysis facilities, only one-third of kidney failure patients were referred for transplant within one year of dialysis.5 Low referral is generated, in part, by patient knowledge gaps and fears of transplant, and poor patient-provider communication.6,7 Transplant education influences receptivity of kidney failure patients to transplant and referral for transplantation,8–10 yet adequate education may not be provided,11 perhaps because the available educational resources are time intensive for providers to deliver and not appealing or accessible to patients.12
Animated video is a powerful medium to deliver information and can be deployed as standalone education.13–17 Animated video can bring education to people and is easy for anyone to deliver, including administrative staff and lay intermediaries; it can also greatly improve the quality of information while addressing many of the root causes for poor information access, such as language and literacy barriers. Preliminary studies of standalone animated video on various kidney transplant access topics indicate positive impacts on individuals’ knowledge,13–17 concerns,14,17 and decisional and communication self-efficacy16,17 as well as learning satisfaction.13–17 Few standalone videos have been designed to empower patients’ transplant referral or pursuit in the early phases of the path to transplant.16,18
Since 2018, we have been developing an animated-video curriculum (called KidneyTIME) to increase kidney transplant access with an emphasis on living kidney donor transplantation.17 Participant feedback during video formative and development work indicated the need to add content to empower patients to be referred to a transplant center, and resulted in 8 new videos being produced and added to the intervention curriculum. Our intervention development is guided by an agile scientific framework for producing a product and testing hypotheses,19 which includes a series of feasibility and usability studies testing each intervention component that is the smallest meaningful and self-containing entity and making improvements iteratively. Each video in the curriculum is therefore preliminarily tested, as a single video or set of videos, to obtain preliminary effect data and pilot measurement tools and to inform full intervention use wherein researchers may select specific videos tailored to users’ informational needs.
This report describes how a set of 8 videos was used in an online pilot study with a one-group pretest-posttest design followed by individual interviews to: (1) assess the feasibility of the 8-video set to improve participants’ kidney transplant knowledge (primary outcome), concerns, and comfort communicating about kidney transplantation with their doctors (communication self-efficacy); (2) examine program acceptability; and (3) understand the patient’s perspective about the video set content, delivery, sharing utility, and ability to promote confidence in navigating the transplant process to guide the next stage in intervention implementation.
METHODS
To assess the 8-video set feasibility, acceptability, content, delivery, sharing utility, and ability to promote confidence navigating transplant access, we conducted an online pre-post study followed by participant interviews. The Institutional Review Board of the University at Buffalo, State University of New York approved this study.
Video Set
A team of academic researchers and community members previously collaborated—using a community-based participatory research process—to develop the 8-video set to meet the information needs of people in the earliest stages of the kidney transplant path and to be culturally grounded to the majority of the members in our community.20 The 8-video set describes in 19:36 minutes the kidney transplant access process (from the starting point of primary care), benefits, risks, and expected outcomes.20 The video production process incorporated the theoretical underpinnings of Elaboration Theory, communication and multimedia learning best practices, and a self-efficacy framework, which we have used to design prior educational videos and are fully described elsewhere.17,20
Measures development
Survey measures were developed with input from transplant experts and our community advisory board comprised of 9 local community members with a relationship to kidney disease who are predominantly of minoritized race or ethnicity. The academic surgeon developed questions aligned with educational content to assess kidney transplant knowledge and concerns and also presented a question related to communication self-efficacy21 used in previous transplant studies. The questions were reviewed and revised by the community member lead, followed by experts in community-based research, communication, anthropology, transplant nephrology, and then the full community advisory board to ensure item clarity and relevance. Their responses were used to modify the questions and ensured that the items were worded in a culturally appropriate way. The final instruments consisted of 1 communication self-efficacy, 7 concerns, and 8 knowledge questions (Table 1).
Table 1.
Pre-post Surveys for Kidney Transplant Knowledge, Concerns, and Communication Self-efficacy.
| Question | Pre Video | Post Video |
|---|---|---|
| Knowledge (% correct) | ||
| You can get a kidney transplant before you need dialysis. | 50% | 92% |
| Transplant centers have financial specialists that will help you keep your out of pocket costs to a minimum | 78% | 96% |
| If you get a kidney transplant, you’ll probably live longer than if you had just stayed on dialysis | 84% | 88% |
| If you are 70 years of age or older you cannot get a kidney transplant. | 84% | 82% |
| The kidney transplant surgery takes about 12 hours. | 44% | 86% |
| After your transplant surgery, you’ll have to stay in bed for 2 weeks to recover. | 62% | 70% |
| After your kidney transplant, you’ll have to take some medications for the life of the kidney | 92% | 98% |
| After you get a kidney transplant you should drink as little as possible to keep the kidney healthy. | 76% | 84% |
| Concerns (mean and standard deviation) 1 | ||
| I’m worried that I’m not healthy enough to get a kidney transplant. | 2.12 ± 0.82 | 2.02 ± 0.80 |
| My life will be just as good on dialysis as it would be with a kidney transplant. | 1.32 ± 0.82 | 1.82 ± 0.80 |
| I’m worried that kidney transplant surgery is a dangerous procedure. | 2.28 ± 0.83 | 2.32 ± 0.82 |
| I’m worried about the recovery time after kidney transplantation. | 2.14 ± 0.81 | 2.02 ± 0.80 |
| I’m worried that I won’t be able to afford the transplant medications. | 2.24 ± 0.85 | 1.96 ± 0.78 |
| I’m worried that the transplanted kidney won’t work. | 2.36 ± 0.80 | 2.16 ± 0.79 |
| I’m worried the transplant medications will make me feel sick. | 2.36 ± 0.69 | 2.28 ± 0.73 |
| Communication Self-efficacy (% agree and strongly agree) | ||
| I feel comfortable discussing kidney transplantation with my doctor. | 70% | 80% |
Likert scale responses were scored as follows: strongly disagree=1, disagree=2, agree=3, and strongly agree=4.
Recruitment
Between October 2021 and March 2022, we recruited community-based adults with stage 4 or 5 chronic kidney disease that were not currently being evaluated at our transplant center. Additional inclusion criteria were at least 18 years of age, English speaking, and email or SMS access. Potential participants responded to flyers posted in the dialysis center and nephrology office of the transplant hospital. Potential participants were also identified through a University at Buffalo clinical registry. Registry members were mailed invitations to participate. Those who did not opt out were called up to 3 times.
Participation
All participants received an email or SMS invitation containing a link to the study. They opened the link on the device of their choice, which delivered the study on the Alchemer platform (Alchemer, Boulder, CO). Following electronic consent, participants completed 18 questions about their sociodemographic characteristics (sex, age, race, employment status, education level, marital status, total annual household income), dialysis vintage, health literacy, technology access, and measures of kidney transplant knowledge (8-item true/false), concerns (7-item, 4-point Likert scale), and communication self-efficacy (1-item, 4 response options).
After survey completion, the participants were taken to the video set, which they started by pushing the play button and watched sequentially. The videos could be watched, paused, or restarted by participants until the “next” button was pushed, leading to a question about the device used to view the videos, followed immediately by identical post-survey questions with the sociodemographic questions replaced with program acceptability questions (7-items, 4-point Likert scale) developed by the researchers (α=0.92) and adapted by the team. All survey questions were posed sequentially without the option of going backward. At least 7 electronic reminders or phone call attempts were made during the day and evening to reach participants who did not complete the online survey.
At study completion, all participants were invited to telephone interviews. To initiate the interview, pre-scripted open-ended questions were used to explore participants’ perceptions of their kidney disease and kidney transplantation, followed by questions about their experience and likes/dislikes of the videos, and how they could be improved. We then asked if the videos changed their perception of kidney transplantation, what content was particularly helpful, if there were recommended changes, what the preferred viewing format was, and whether, given the opportunity, they would share the videos with others. These sessions were conducted by research coordinators trained to conduct qualitative interviews. Interviews were conducted and audio-recorded via Zoom and transcribed using Temi, a speech transcription service available online. Participants were mailed a US $25 gift card at completion of post-baseline surveys and the exit interview to compensate for their time (maximum total $50).
Analysis
We attempted to recruit a minimum of 40 participants to have an 80% power to detect a 30% difference in knowledge scores, assuming a coefficient of variation-0.5 for a 2-tailed paired test Type 1 error rate of 0.05.
Statistical analyses were conducted using SPSS Version 24 (IBM Corp, Armonk, NY). Frequencies were computed for all categorical variables and summarized numeric variables using simple descriptive statistics. Categorical data were compared using McNemar’s test. Continuous data of knowledge (percent correct), concerns, and self-efficacy scores were not normally distributed. The standardized effect size of the change between same day pre-intervention and post-intervention exposure was calculated as the test statistic (z score) divided by the square root of the total observations for the whole cohort and subgroups (Effect size, (r) = Z/√N) with 0.1, 0.24, and 0.37 representing small, medium, and large effects.22 Knowledge scores were calculated by summing the number of correct answers. All Likert scales were anchored by strongly agree and strongly disagree. Higher scores reflect greater knowledge, concerns, and self-efficacy, respectively. We provided categorical level data attributing to participants’ animation acceptability data using a bar graph. Statistical significance was established at a 2-tailed alpha of 0.05.
Content analysis was used to thematically analyze the interview data. Two of the authors (L.K. and J.S.) independently read the transcripts and identified multiple codes based on remarks raised from interview questions and thereafter checked for comprehension with the co-authors. These codes were compared, revised, and clustered into categories by conceptual similarity, and larger meaningful themes were extracted from these categories to identify feedback from the transcripts to describe how the videos can improve patient transplant access, identify potential improvements in video content, and plan future online delivery conditions necessary to promote effectiveness.
RESULTS
Participant characteristics
We invited 175 adults with chronic kidney disease stage 4 and 5 who were English-speaking and had not been evaluated at the local transplant center. The first 54 that opted in participated in the online study. Four were removed because their survey answers were incomplete. Of 50 participants within the final analytic sample, 56% did not require chronic dialysis treatment and 60% had not been referred for a kidney transplantation. The majority was non-Hispanic White, older than age 60, had less than a college education, and were not employed (Table 2). Almost half (48%) had an annual household income <$30,000, and 40% classified themselves as being Black or African American race. Most had watched videos online (80%) prior to the study, and 58% used the internet at least once weekly.
Table 2.
Participant Sociodemographic Characteristics
| Characteristic % or median (range or numerator/denominator) | Pilot Study Participants N=50 | Interview Participants N=29 |
|---|---|---|
|
| ||
| Age < 50 years | 14% (7/50) | 10% (3/29) |
| Age 50–60 years | 26% (13/50) | 35% (10/29) |
| Age > 60 years | 60% (30/50) | 55% (16/29) |
|
| ||
| Sex, Male | 40% (20/50) | 45% (13/29) |
|
| ||
| Race, Black or African American | 40% (20/50) | 31% (9/29) |
|
| ||
| Dialysis duration | ||
| Not on dialysis | 56% (28/50) | 41% (12/29) |
| < 1 year | 16% (8/50) | 24% (7/29) |
| 1–3 years | 12% (6/50) | 14% (4/29) |
| >3 years | 16% (8/50) | 21% (6/29) |
|
| ||
| Prior Kidney transplant | 4% (2/50) | 7% (2/29) |
|
| ||
| Not referred for a kidney transplant | 60% (30/50) | 48% (14/29) |
|
| ||
| Education, no college degree | 58% (29/50) | 55% (16/29) |
|
| ||
| Full- or part-time employment | 16% (8/50) | 10% (3/29) |
|
| ||
| Total household yearly income | ||
| ≤US$ 30,000 | 48% (24/50) | 59% (17/29) |
| US$ 30,000–75,000 | 22% (11/50) | 14% (4/29) |
| >US$ 75,000 | 12% (6/50) | 10% (3/29) |
| No response | 18% (9/50) | 17% (5/29) |
|
| ||
| Watches videos online | 80% (40/50) | 76% (22/29) |
| Internet and Social Media use at least once weekly | 58% (29/50) | 55% (16/29) |
| Uses social media at least once a week | 22% (11/50) | 17% (5/29) |
| Has active Facebook account | 72% (36/50) | 76% (22/29) |
|
| ||
| Access to Technologya | ||
| Participant has a working internet capable cellular phone | 90% (45/50) | 90% (26/29) |
| Participant has a working computer | 70% (35/50) | 76% (22/29) |
| Participant sends or receives text messages | 92% (46/50) | 90% (26/29) |
| Participant sends or receives email | 86% (43/50) | 79% (23/29) |
|
| ||
| Frequency that someone helps you read hospital materialsb | ||
| Never | 62% (31/50) | 59% (17/29) |
| Sometimes | 28% (14/50) | 35% (10/29) |
| Often | 4% (2/50) | 3% (1/29) |
| Always | 6% (3/50) | 3% (1/29) |
|
| ||
| Confident filling out forms alone b | ||
| Not at all confident | 2% (1/50) | 0% (0/29) |
| Somewhat confident | 22% (11/50) | 14% (4/29) |
| Quite confident | 36% (18/50) | 41% (12/29) |
| Extremely confident | 40% (20/50) | 45% (13/29) |
|
| ||
| Device used to watch the videos | ||
| Computer/Laptop | 26% (13/50) | 28% (8/29) |
| Phone | 64% (32/50) | 62% (18/29) |
| iPad/Tablet | 10% (5/50) | 10% (3/29) |
|
| ||
| Watched the videos with someone else | 18% (9/50) | 10% (3/29) |
Technology access was measured using 4 questions adapted from an 11-item yes/no format questionnaire previously used in several studies that evaluated a prototype mobile health system for enhancing adherence to medical regimens.35,36
Health literacy was measured with a 2-item survey37 with two items scored on Likert-type scales: “How often do you have someone help you read hospital materials?” and “How confident are you filling out forms by yourself?”
During the study, 64% watched the study videos on a cell phone, and 88% without pause. Only 18% watched the videos with someone else during the single time-frame that video viewing was available to them.
Knowledge, concerns, and communication self-efficacy outcomes
Compared with pre-exposure, the mean total knowledge score increased post-exposure by +22% (mean 5.70 to 6.96, r=0.67), communication self-efficacy by +6% (3.07 to 3.24; r=0.24) and concerns reduced by −2% (mean 2.12 to 2.08, r=0.07) (Tables 3 and 4). Large effect sizes for knowledge score (pre- vs. immediate post-exposure) were seen by subgroups in the context of Black race (r=0.64), age >60 years (r=0.62), low health literacy (r=0.75), <college educational attainment (r=0.70), dialysis requirement (r=0.74), non-referred for kidney transplantation (r=0.71), and low technology access (r=0.71) (Table 3).
Table 3.
Main and Subgroup Participant Knowledge Scores Before and After Video Set Viewing
| Knowledge (range 0–8) Mean ± Standard Deviation | T0 | T1 | T0–T1 % change | Z | T0–T1 Effect size (r) 1 | P-value |
|---|---|---|---|---|---|---|
| Total Cohort (n= 50) | 5.70 ± 1.51 | 6.96 ± 1.09 | 22% | 4.73 | 0.67 | <0.01 |
| Referred to transplant (n=20) 2 | 6.30 ± 1.13 | 7.15 ± 1.00 | 13% | 2.72 | 0.61 | <0.01 |
| Not referred to transplant (n=30) 2 | 5.30 ± 1.62 | 6.83 ± 1.15 | 29% | 3.91 | 0.71 | <0.01 |
| Black race (n=20) 2 | 5.55 ± 1.32 | 6.80 ± 1.15 | 23% | 2.84 | 0.64 | <0.01 |
| Non-Black race (n=30) 2 | 5.80 ± 1.65 | 7.07 ± 1.05 | 22% | 3.87 | 0.71 | <0.01 |
| Education, less than college (n=29) 2 | 5.24 ± 1.48 | 6.76 ± 1.21 | 29% | 3.79 | 0.70 | <0.01 |
| Education, college level (n=21) 2 | 6.33 ± 1.34 | 7.24 ± 0.83 | 14% | 2.98 | 0.65 | <0.01 |
| 25th percentile literacy (n=18) 2 | 5.00 ± 1.81 | 6.72 ± 1.27 | 34% | 3.18 | 0.75 | <0.01 |
| 26th–100th percentile literacy (n=32) 2 | 6.09 ± 1.17 | 7.09 ± 0.96 | 16% | 3.58 | 0.63 | <0.01 |
| Age >60 years (n=30) 2 | 6.17 ± 1.21 | 7.23 ± 1.00 | 17% | 3.38 | 0.62 | <0.01 |
| Age ≤ 60 years (n=20) 2 | 5.00 ± 1.69 | 6.55 ± 1.10 | 31% | 3.33 | 0.74 | <0.01 |
| Dialysis – none (n=28) 2 | 5.75 ± 1.71 | 6.89 ± 1.17 | 20% | 3.26 | 0.62 | <0.01 |
| Dialysis > none (n=22) 2 | 5.63 ± 1.26 | 7.05 ± 1.00 | 25% | 3.46 | 0.74 | <0.01 |
| 25th percentile technology access (n=22) 2 | 5.09 ± 1.60 | 6.64 ± 1.29 | 30% | 3.35 | 0.71 | <0.01 |
| 26th-100th technology access (n=28) 2 | 6.18 ± 1.28 | 7.21 ± 0.83 | 17% | 3.38 | 0.64 | <0.01 |
SD, standard deviation; T0, pre-exposure; T1, immediately post-exposure
Effect size, r; Interpretation: 0.1=small effect, 0.24= medium effect, 0.37=large effect
Corrected for multiple comparisons using Bonferroni
Table 4.
Kidney Transplant Concerns and Communication Self-efficacy Scores Before and After Video Set Viewing
| Outcome Mean ± Standard Deviation | T0 | T1 | T0-T1 % change | Z | T0-T1 Effect size (r) 1 | P-value |
|---|---|---|---|---|---|---|
| Transplant concerns (range 1–4) 1 | 2.12 ± 0.44 | 2.08 ± 0.54 | 2% | 0.51 | 0.07 | 0.61 |
| Communication self-efficacy (range 1–4) 1 | 3.07 ± 1.00 | 3.24 ± 0.90 | 6% | 1.17 | 0.17 | 0.24 |
T0, pre-exposure; T1, immediately post-exposure;
r: Effect size, r; Interpretation: 0.1=small effect, 0.24= medium effect, 0.37=large effect
Likert scale responses were scored as follows: strongly disagree=1, disagree=2, agree=3, and strongly agree=4.
Video Acceptability and Feedback
Of the 50 participants included in baseline analysis, all completed the video acceptability questionnaire. Over 90% of participants agreed or strongly agreed that the videos were interesting and engaging, credible, and helpful, and that they would use videos like these in the future (Figure 1).
Figure 1.
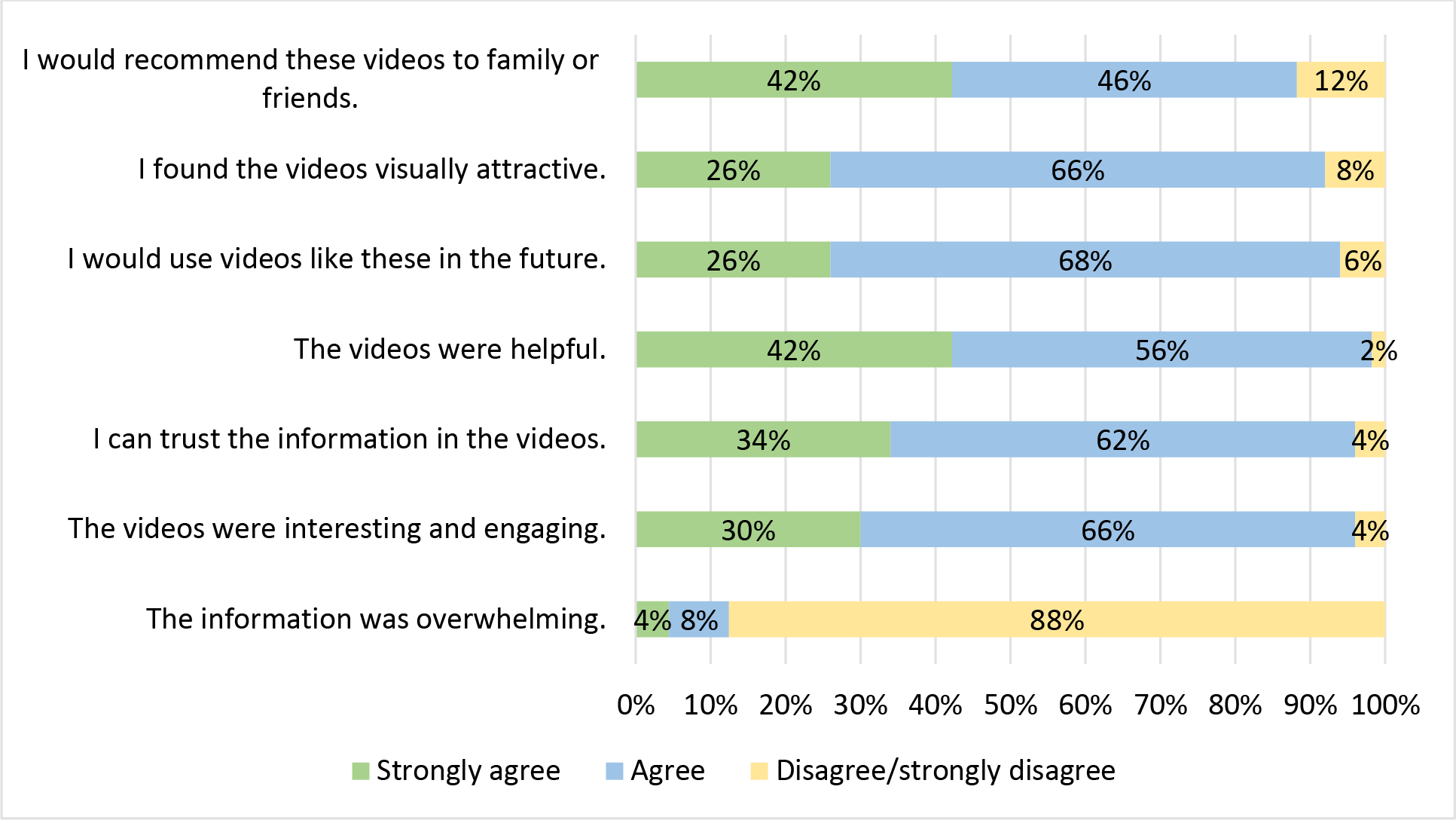
Animation Acceptability Survey Responses Immediately Post-Exposure
Within 3 weeks after study completion, interview feedback was obtained from 29 participants. Most were >60 years of age and 55% were women. Nearly half had not been referred for a kidney transplant. Interviews lasted between 10 and 43 minutes. The categories and subcategories are depicted in Table 5, and representative quotes are provided in Table 6. We reached saturation on the main themes, meaning that participants repeated similar ideas related to previous interviews.
Table 5.
Themes, Categories and Subcategories of Interviews with Participants
| Theme | Main Category | Subcategory |
|---|---|---|
| Content | Learning ease | Engaging |
| Gentle | ||
| Easy-to-understand | ||
| Comprehensive without overwhelm | Covers the basics | |
| Manageable | ||
| Missing features and content | Absence of closed captions | |
| Recommended topics | ||
| Confidence | Motivation for transplant | Support from transplant providers |
| Hopeful about transplant | ||
| Positive emotions about transplant | ||
| Self-confidence to get a transplant | ||
| Online video delivery preferences | Deliver prescribed videos as a whole within <30 minutes duration, including option of re-watching | Deliver all pertinent videos as a whole |
| Keep content under 30 minutes duration | ||
| Ability to re-watch | ||
| Anticipated sharing of the videos | Most would share the videos to inform support persons, close family, and peers. | Share to inform support persons |
| Share to help family understand transplant | ||
| Share to educate peers in same circumstance | ||
| Share at dialysis center | ||
| Decline sharing to avoid burdening family |
Table 6.
Representative Quotes by Subcategory from Participants
| Subcategory | Representative Quotes |
|---|---|
| Engaging | “They kept my attention, so I don’t know what they did, if it’s the way they talked or if it was the drawings or I don’t know. It kept me glued.” “It all kinda spoke to me. I guess that I could kind of relate.” “It was actually a little better with cartoon figures than real people. Cuz then you could focus a little bit more on what they were saying.” |
| Gentle | “It was a very cute way of promoting and explaining, you know, in a gentle way.” |
| Easy-to-understand | “They was plain and clear. That’s what I like about the videos. They was on a level that everybody can understand.” “Pretty simple. And I understand it. It was sort of like in layman’s terms.” “I just feel like I got a lot more information that I needed to know… because I’m a visual person. So that helped me a lot.” |
| Covers the basics | “It covers the basics, you know costs, recovery time, uh um, surgery time, you know, your support system in a nutshell. Covers everything.” “The videos were very short and precise, and they showed you every facet.” |
| Manageable | “I thought it was comprehensive, but not overdone.” “I think it was perfect. Just enough. Put everything, summed it all up in a little video.” “I just think it just had enough to kind of put me at ease. I don’t think it was too much. I don’t think it was too little. I think it was just enough. I didn’t feel overwhelmed.” |
| Lack of captions | “If there’s captioning for like the hearing impaired?” |
| Missing content | “I want information to motivate me [to find a donor], to get out there and start asking.” “It didn’t speak about, uh, failures.” “I had questions on possibly getting my children tested.” “I want more explained about diet. I wanted to make sure that I’m not eating stuff that I’m not supposed to…that’s going to speed up the deterioration.” |
| Hopeful about transplantation |
“My doctor said there ain’t no way. They not going to give it [a kidney] to you. Now it’s [videos] just flipped the script…I was like, it’s a chance you know. It gave me hope where I had lost it.” “I thought because of my age, you know, I’m 63…I just feel like now I might have a chance. I really thought at first that I probably wouldn’t be a good candidate for a transplant because of my age. And I’m not really well. I’m not gonna say my hope is bad, but I do have other problems. So, but now I feel like I do have a chance.” |
| Self-confidence to get a transplant | “There was something that caught me there, and make me feel as though that I was like, ‘I can do this.’” “See. I was scared at first, but now I’m not scared. I’m determined.” |
| Feeling support from transplant providers | “I think they’re supportive, they’re [transplant team] much more caring and compassionate, and they’re there for you, um, you know, they want a good outcome as well as I do.” “I do think it’s pretty cool that, you know, even after a transplant, that they got the pharmacist that links up and helps you, like understand the medications, and then they give you the medicine box and they set everything up. That gives the personal relief, like, you know, okay, this is what I gotta deal with.” |
| Positive emotions about transplant | “So, I said yesterday [after watching the videos], maybe I will talk to my kidney doctors about the transplant. It was great because where I was thinking negative of transplant, and now I’m thinking positive of it.” “It was more enlightening. Transplant is not as gloomy though.” |
| Deliver all pertinent videos as a whole | “You don’t ever give a person that’s seeking anything a chance to choose anything because he/she may choose something and then miss something on the other. You give them all the videos. Ask them to look at all the videos. And look at them very closely.” “The way I watched them, it seemed like they were placed in the way I needed to receive them.” “One piece. I didn’t wanna lose the train of thought, but I see where I could have gotten up and done something else. There was a little commercial in between.” |
| Keep content under 30 minutes duration | “I wouldn’t go more than half an hour though. You go too long, I have to be honest, I get annoyed. You know, keep just concise and move it along.” “It was good to have it all in one block as long as I knew the overall time you would watch it.” “I feel like I got all the information I need right now, and I can become easily overwhelmed.” |
| Provide option to re-watch | “You think you pick up most things that aren’t familiar, but when you go back over something, something else might come, so it’s good to reiterate things, you know, especially with me being mildly dyslexic.” |
| Share to inform support persons | “I think all my supports would be interested to see what it’s about and see if they can get anything more about it.” |
| Share to help family understand | “If my family wants to know some information, I would tell them to watch.” “My family, to give them more of an idea of what a transplant entailed.” “I think it might help my sisters to see it, you know, ‘cause they could probably get a better understanding, you know, what’s really going on.” |
| Share to potential donors | “I would probably share them with my children [potential donors] so they can understand it more.” |
| Share to educate peers | “To keep them informed as much as they can inform them about their disease and, uh, give them positive outlook on it.” |
| Share with provider | “Actually, I wanted to, uh, see if I could get a copy of it because, uh, as I went back to dialysis and was doing some talking to the dietician, I couldn’t explain some of the things I saw in the video.” |
| Declined sharing | “I don’t want my family to worry about me.” |
The video content was reported to be easy to learn, comprehensive without being overwhelming, and motivational about kidney transplantation. One reported displeasure with cartoon characters but said they were preferable over real video to optimize learning focus. The videos promoted patient confidence in obtaining a kidney transplant, primarily by giving hope about eligibility, promoting positive emotions about transplantation, and highlighting medical provider support. Recommended features were closed captions and additional topics about transplant complications, dialysis, and outreach to potential living kidney donors. When asked if the videos should be delivered in a prescribed order or self-directed, all participants preferred prescribed delivery to ensure that they received all the information deemed important by the provider. Some specified that the education should last no longer than 30 minutes and recommended the opportunity to re-watch later. When asked if they would share the videos with others, most indicated an interest in sharing the videos with caregivers, family members, potential donors, and other kidney failure patients. One wanted to share with their dialysis provider for further discussion. One declined sharing, explaining that they did not want to burden others.
DISCUSSION
This paper describes a web-based pre-post study with immediate follow-up, by which the feasibility and acceptability of a set of educational animated videos designed to influence kidney transplant referral were evaluated in a population of patients with chronic kidney disease stage 4 and 5 who were not within our transplant center’s pre-transplant system. We found that the intervention was acceptable and increased kidney transplant knowledge with a large effect size. There were also improvements in known mediators of kidney transplant participation, including addressing transplant concerns and communication self-efficacy. As a result of the qualitative feedback from the feasibility study, we identified several changes to be made to the intervention to maximize value at the time of implementation.
The online educational content was provided using animated video. The improvements in kidney transplant knowledge that we found may be attributed to learning through reinforcing audio and visual elements, which reduces cognitive load and enhances information processing, as suggested by Mayer’s cognitive theory of multimedia learning.23 Other studies have also reported significant knowledge increases using standalone animation13 or blended animation and live action24 in transplantation and other health contexts.25 Our report’s 21% knowledge gain with a r=0.54 effect size is considered large and promising and is similar to a meta-analysis of standalone animated video education in different healthcare contexts that found a small to medium effect size (Cohen’s d =0.38) across 20 studies.26
Our study tested 8 videos sequentially for a total duration of 19:36 minutes. This learning time would be considered long compared to prior studies of standalone animation wherein video exposure spanned 2 minutes to 16 minutes according to a recent review.26 Longer video duration may have diminishing returns with respect to patient learning.26 Therefore, we had segmented the information into individual videos to allow participants to take breaks and come back to the information; however, in viewing the metadata, we noted that participants tended to watch all the videos back-to-back in one sitting. This finding was confirmed in our qualitative interviews. None of the participants found the delivery of the education to be overwhelming, and one commented that up to 30 minutes duration would be acceptable for home viewing. Further research is needed to determine the optimal suggested length of prescribed content delivered online.
Knowledge improvements in our study were also seen among a diverse sample, with similar effect sizes attained between older and younger groups, Black and non-Black, low- and moderate/high literacy. These findings may be due to development of the videos based on our formative research and input from learners and experts that guided changes to the animations to optimize learning based on viewers’ capabilities, such as reduction of extraneous information, clarifying content, and reducing speed.20 The need for interventions that enhance patient learning is crucial given that limited health literacy affects more than a quarter of individuals with chronic kidney disease and is associated with poorer health outcomes.27–31
We also found small to medium improvements in self-reported transplant concerns and comfort talking with a doctor pre-post exposure. These outcomes are typically thought to be mediated by increased knowledge and may also derive from decreased learner anxiety and improved attitudes towards health behaviors, as suggested by our recent scoping review of educational animations.25 Learner anxiety might arise when the content is complex and in relation to the procedure itself. Ease of learning with animation32 may help to resolve anxiety of learning. Anxiety reduction may also be due to the fact that the animations, especially cartoons, may be appealing or amusing to viewers33 and may focus on positive framing of information, resulting in enjoyment of learning and less fear of the procedure. Anecdotal reports from our interview findings suggest the videos promoted positive emotions about transplantation. For example, one participant reported, “Where I was thinking negative of transplant and now I’m thinking positive of it.” Other participants said they felt encouraged (“It gave me hope where I had lost it.”), less fear (“I was scared at first, but now I’m not scared.”), and confidence pursuing a transplant (“Made me feel as though that I was like ‘I can do this.’”).
Although our findings of gains in several transplant-pursuit indicators are promising, they require validation compared to a control group. In a recent randomized controlled trial conducted at 3 Canadian sites, animation mixed with live action yielded significant knowledge increases, but did not impact self-efficacy, quality of life, or medication beliefs relative to usual care among transplant candidates.24 The authors attributed this to a “one-size fits all” video delivery strategy and suggested tailoring and a multicomponent intervention approach to improve these outcomes. Feedback from the participants in our study suggest that optimal video delivery strategy may involve completion of core content in a specific order to ensure that users access relevant topics. Relevant video content is more feasible to deliver with education chunked into short video segments.
Feedback from participants viewing the videos suggested high acceptability and ease of learning, including 64% who accessed the videos with a cellular phone. Research on the use of animations in advertising34 suggests that ratings of favorability and level of attention beget learning gains when viewing animated videos versus static text information. Appealing content that can be learned without supervision has great potential to be used in busy clinical sites and to reach a broad spectrum of viewers seeking to learn independently.12
Limitations
The study has several limitations. Generalizability is compromised, mainly due to the small sample size and a predominance of a Black and White race population drawn from a single geographic location. There was a selection bias of patients that have internet access. Requiring internet access excludes patients who do not have internet or do not know how or have means to use the internet. This could exclude older patients. Nevertheless, the age of the participants was similar to those found in the dialysis population. We used a pre-post design; thus, we were not able to draw causal inferences. There may be test-retest bias since all the questions were repeated immediately after delivery of the education. It was not possible to verify whether the participants answered the surveys themselves as the study was online. Qualitative data was collected from participants to identify future revisions to the interventional education and structure. However, some of the qualitative data is not reported in the present manuscript. Although our study’s findings are promising, it is unclear if the videos will improve outcomes (transplant referrals) compared to usual care. Many questions remain about how best to deliver the information. Choosing the right sources, channels, and messages that will motivate different populations to pay attention and to use health information are among the greatest health communication challenges. Additionally, interventions are needed to overcome well-known structural and organizational barriers that patients face to obtaining transplant referral.
In conclusion, this single-center prospective pre-post study found that our 8 educational video set was a feasible and acceptable method for increasing kidney transplant knowledge in both low- and adequate-health literacy individuals, increasing confidence to communicate about kidney transplantation with their doctor, and reducing concerns about kidney transplantation, among kidney failure patients not previously exposed to transplant center education. Educational videos that improve knowledge and attitudes and that empower patient-driven conversations about kidney transplantation may hold one of the keys to advancing transplant access and to reducing known disparities in transplant participation and outcomes.
We are currently evaluating the full video intervention in a randomized controlled trial of patients referred for transplant evaluation to a single transplant program in New York State to determine whether exposure to the full intervention condition will positively influence patient access to waitlist placement and living-donor kidney transplantation. The addition of the videos analyzed in this study will enable our future aim of implementing the intervention earlier in the transplant continuum--at nephrology offices and dialysis centers--to additionally activate timely transplant referral.
Acknowledgements
We thank Dr. Beth Dolph of University at Buffalo for proofreading the manuscript. Special thanks to the Kidney Health Together community advisory board for their help crafting study measurement questions. We would like to acknowledge the assistance of the following persons during data collection: Sydney Pelino and Suneet Singh.
Funding Acknowledgements
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH) under award number UL1TR001412 to the University at Buffalo. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
We acknowledge participation in the Transplant Peer Review Network and complied with the journal’s author guidelines and policies.
Footnotes
Disclosures: The authors declare no conflicts of interest.
Data statement:
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon request.
REFERENCES
- 1.Organ Procurement and Transplantation Network. https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/#. Accessed 5/9/20.
- 2.United States Renal Data System. https://usrds.org/. Accessed May 27, 2020.
- 3.Rana A, Gruessner A, Agopian VG, et al. Survival benefit of solid-organ transplant in the United States. JAMA Surg. 2015;150(3):252–259. [DOI] [PubMed] [Google Scholar]
- 4.USRDS 2015 Annual Report. https://www.usrds.org/2015/download/vol2_USRDS_ESRD_15.pdf.
- 5.Patzer RE, McPherson L, Wang Z, et al. Dialysis facility referral and start of evaluation for kidney transplantation among patients treated with dialysis in the Southeastern United States. Am J Transplant. 2020;20(8):2113–2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gillespie A, Hammer H, Lee J, et al. Lack of listing status awareness: results of a single-center survey of hemodialysis patients. Am J Transplant. 2011;11(7):1522–1526. [DOI] [PubMed] [Google Scholar]
- 7.Harding JL, Perez A, Patzer RE. Nonmedical barriers to early steps in kidney transplantation among underrepresented groups in the United States. Curr Opin Organ Transplant. 2021;26(5):501–507. [DOI] [PubMed] [Google Scholar]
- 8.Browne T, Amamoo A, Patzer RE, et al. Everybody needs a cheerleader to get a kidney transplant: a qualitative study of the patient barriers and facilitators to kidney transplantation in the Southeastern United States. BMC Nephrol. 2016;17(1):108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Waterman AD, Peipert JD, Hyland SS, et al. Modifiable patient characteristics and racial disparities in evaluation completion and living donor transplant. Clin J Am Soc Nephrol. 2013;8(6):995–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Waterman AD, Peipert JD, Xiao H, et al. Education Strategies in Dialysis Centers Associated With Increased Transplant Wait-listing Rates. Transplantation. 2020;104(2):335–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Waterman AD, Peipert JD, Goalby CJ, et al. Assessing Transplant Education Practices in Dialysis Centers: Comparing Educator Reported and Medicare Data. Clin J Am Soc Nephrol. 2015;10(9):1617–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kayler LK, Ranahan M, Keller M, et al. Using Focus Groups to Understand Dialysis Staff Perspectives on Delivering Transplant Education. Prog Transplant. 2022;32(1):12–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Axelrod DA, Kynard-Amerson CS, Wojciechowski D, et al. Cultural competency of a mobile, customized patient education tool for improving potential kidney transplant recipients’ knowledge and decision-making. Clin Transplant. 2017;31(5). [DOI] [PubMed] [Google Scholar]
- 14.Kayler LK, Dolph B, Ranahan M, et al. Kidney Transplant Evaluation and Listing: Development and Preliminary Evaluation of Multimedia Education for Patients. Ann Transplant. 2021;26:e929839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kayler L, Dolph B, Cleveland C, et al. Educational Animations to Inform Transplant Candidates About Deceased Donor Kidney Options: An Efficacy Randomized Trial. Transplantation Direct. 2020;6(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kayler LK, Keller MM, Crenesse-Cozien N, et al. Development and preliminary evaluation of ilearnKAS: An animated video about kidney allocation to support transplant decision-making. Clin Transplant. 2019;33(8):e13638. [DOI] [PubMed] [Google Scholar]
- 17.Kayler LK, Seibert RE, Dolph BA, et al. Video education to facilitate patient outreach about living kidney donation: A proof of concept. Clin Transplant. 2021:e14477. [DOI] [PubMed] [Google Scholar]
- 18.Morinelli TA, Taber DJ, Su Z, et al. A Dialysis Center Educational Video Intervention Increases Patient Self-Efficacy and Kidney Transplant Evaluations. Prog Transplant. 2022;32(1):27–34. [DOI] [PubMed] [Google Scholar]
- 19.Hekler EB, Klasnja P, Riley WT, et al. Agile science: creating useful products for behavior change in the real world. Transl Behav Med. 2016;6(2):317–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kayler L, Breckenridge B, Sierra E, et al. An academic-community partnership to close the race and ethnicity gap in access to kidney transplantation. 2021 Clinical and Translational Research Virtual Colloquium; 10/15/21, 2021; Buffalo, NY. [Google Scholar]
- 21.Delair S, Feeley TH, Kim H, et al. A peer-based intervention to educate liver transplant candidates about living donor liver transplantation. Liver Transpl. 2010;16(1):42–48. [DOI] [PubMed] [Google Scholar]
- 22.Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141(1):2–18. [DOI] [PubMed] [Google Scholar]
- 23.Mayer RE. Multimedia learning. Cambridge; New York: Cambridge University Press; 2001. [Google Scholar]
- 24.Mansell H, Rosaasen N, Wichart J, et al. A Randomized Controlled Trial of a Pretransplant Educational Intervention in Kidney Patients. Transplant Direct. 2021;7(10):e753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.MM K, T L, M Z, et al. A Scoping Review of Animated Video’s Effect on Individual Health Knowledge. Austin Med Sci. 2021;6(1). [Google Scholar]
- 26.Feeley TH, Keller M, Kayler L. Using Animated Videos to Increase Patient Knowledge: A Meta-Analytic Review. Health Education & Behavior.0(0):10901981221116791. [DOI] [PubMed] [Google Scholar]
- 27.Taylor DM, Fraser SDS, Bradley JA, et al. A Systematic Review of the Prevalence and Associations of Limited Health Literacy in CKD. Clin J Am Soc Nephrol. 2017;12(7):1070–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taylor DM, Fraser S, Dudley C, et al. Health literacy and patient outcomes in chronic kidney disease: a systematic review. Nephrol Dial Transplant. 2018;33(9):1545–1558. [DOI] [PubMed] [Google Scholar]
- 29.Devraj R, Gordon EJ. Health literacy and kidney disease: toward a new line of research. Am J Kidney Dis. 2009;53(5):884–889. [DOI] [PubMed] [Google Scholar]
- 30.Ricardo AC, Yang W, Lora CM, et al. Limited health literacy is associated with low glomerular filtration in the Chronic Renal Insufficiency Cohort (CRIC) study. Clin Nephrol. 2014;81(1):30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cavanaugh KL, Wingard RL, Hakim RM, et al. Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol. 2010;21(11):1979–1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Doak LG, Doak CC, Meade CD. Strategies to improve cancer education materials. Oncol Nurs Forum. 1996;23(8):1305–1312. [PubMed] [Google Scholar]
- 33.Leiner M, Handal G, Williams D. Patient communication: a multidisciplinary approach using animated cartoons. Health Educ Res. 2004;19(5):591–595. [DOI] [PubMed] [Google Scholar]
- 34.Alan JBaLGG. The communication effects of animation. Journal of Applied Communication Research.14(1):59–65, year = 1986. [Google Scholar]
- 35.Price M, Williamson D, McCandless R, et al. Hispanic migrant farm workers’ attitudes toward mobile phone-based telehealth for management of chronic health conditions. J Med Internet Res. 2013;15(4):e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McGillicuddy JW, Weiland AK, Frenzel RM, et al. Patient attitudes toward mobile phone-based health monitoring: questionnaire study among kidney transplant recipients. J Med Internet Res. 2013;15(1):e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23(5):561–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon request.


