Abstract
Introduction
Obesity prevalence has almost tripled in Europe since 1980, and the obesogenic (food) environment is hypothesised to be one of the main drivers. Still, empirical evidence is rare for Europe.
Objective
This ecological study explores spatial patterns of obesity prevalence of adults (aged 19+) in the Netherlands in 2016. It studies, in particular, its global associations with (un)healthy food store accessibility while assessing local differences and evaluating the importance of the immediate versus the wider food surroundings.
Methods
In our ecological study, we used small-area estimated obesity prevalence (adults, aged 19+) from 2836 neighbourhoods (six-digit postal codes, wijken) and combined this with measures from Statistics Netherlands on accessibility to (unhealthy) fast food and (healthy) fresh food. Spatial lag of X (SLX) models were estimated for the entire Netherlands to explore global associations. Separate models for urban, suburban, and rural neighbourhoods and a geographically weighted regression (GWR) were estimated to explore and visualise local variations in the associations. Total associations from the SLX models were then decomposed to yield contributions of the immediate and wider food surroundings.
Results
Regional clusters of high obesity were observed in selected areas in the north-east, the south-west, and south-east. Limited accessibility to unhealthy food was globally associated with lower obesity prevalence, whereas better accessibility to fresh food stores and supermarkets was not. The association regarding worse accessibility to unhealthy food was strongest for urban neighbourhoods, especially for the Randstad region. In urban settings, also better accessibility to fresh food stores proved relevant. The wider food surrounding proved more important than the immediate food surrounding, throughout.
Discussion
Public policies addressing obesity might be more effective when reducing the presence of unhealthy food rather than expanding healthy food supply. Moreover, they should focus on urban regions and high obesity clusters, thereby considering wider food surroundings.
Keywords: Local food environment, Obesity, Spatial analysis, Spatial lag of X model, Geographically weighted regression
Highlights
-
•
Evidence on the spatial association of food supply with obesity is rare for Europe.
-
•
Unhealthy & healthy food accessibility are globally related to obesity prevalence.
-
•
There are local differences in the associations between regional subtypes.
-
•
Unhealthy food accessibility proved most important for obesity in urban regions.
-
•
The wider food surrounding is more important than the immediate food surrounding.
1. Introduction
Obesity prevalence globally has more than doubled since 1980 (NCD Risk Factor Collaboration, 2019) and is a growing public health concern. Within Europe, obesity prevalence has almost tripled since 1980 (WHO World Health Organization, 2022). The emergence of obesogenic (food) environments is thought to be one of the main drivers of the rapid increase in obesity prevalence, as postulated by the obesogenic environment theory (Egger & Swinburn, 1997, WHO World Health Organization, 2022). The World Health Organisation therefore recommends creating a health-promoting environment (WHO World Health Organization, 2022). However, empirical evidence on the association between unhealthy and healthy food accessibility and obesity is rare for Europe, and previous research, primarily conducted for the US, has revealed mixed results (Brown et al., 2019, Morales & Berkowitz, 2016). Knowing about the importance of food accessibility for obesity is essential for developing policy interventions to fight against obesity and its burden.
It is assumed that the obesogenic food environment can affect obesity in two ways, either at the macro level through the food laws and food technology in the country, or at the micro level through the physical presence of or access to food that can influence people's diets (Egger & Swinburn, 1997). The micro-level food environment in particular is seen as one of the most important risk factors for obesity (Giskes et al., 2011; Lim et al., 2020). That is, easy access to unhealthy food combined with limited access to healthy food may lead to supernutrition, e.g. intake of food with a high proportion of fat and a high energy-density (Swinburn et al., 1999; Swinburn et al., 2011).
Previous studies on the association between food environments and obesity — either using individual-level or spatial-level data — have focused on the USA and reveal inconsistent results (see Cobb et al., 2015 for a systematic literature reviews). One cross-sectional study from the US using census tracts data on local food stores and individual-level data on obesity found that the presence of healthy food stores (supermarkets) is related to lower obesity prevalence, and the presence of convenience stores to higher obesity prevalence (Morland et al., 2006). Another cross-sectional study from the US using individual-level data on BMI and GIS-derived data on food proximity found that proximity of fast food and non-fast food restaurants to home or work were not associated with BMI (Jeffery et al., 2006).
However, the previous studies in the US that found these associations did not show that healthy or unhealthy food environments are globally associated with lower or higher obesity/being overweight (Michimi & Wimberly, 2010, Morland et al., 2006, see Cobb et al., 2015 for a review). In fact, important differences were observed between regional subtypes (see Lam et al., 2021 for a systematic literature review). A spatial analysis based on county-level data for the US found a positive association between access to supermarkets and obesity in metropolitan districts and a negative association in non-metropolitan districts (Michimi & Wimberly, 2010). People living in disadvantaged neighbourhoods, so called “healthy food deserts”, are forced to travel longer distances to reach food environments that offer healthy and fresh foods, compared to people in wealthier neighbourhoods, where grocery stores are easier to reach (Larson et al., 2009). These differences in outcomes by regional subtype could, in fact, also be (part of) the reason why previous studies have revealed mixed results. Most of these studies have focused on global associations in the entire study region instead of (additionally) differing between regional subtypes.
Very little research for European countries has been conducted (Fraser et al., 2012; Mackenbach et al., 2019; Walker et al., 2020); there are hardly any spatial analyses on the relationship between food accessibility and obesity. This is unfortunate, as such analyses may help to support (regional) decision makers in addressing public health concerns and indicating where interventions are most needed. Furthermore, it is not possible to translate the findings for the US directly to the European context due to the significant differences in their spatial structures and population composition (Burleyson, 2020; Eurostat, 2021) as well as in food laws and regulations. For instance, EU regulations regarding additives in food products are stricter than in the US (Lehto et al., 2017).
This ecological study explores spatial patterns of obesity prevalence of adults (aged 19+) in the Netherlands in 2016, focusing on global associations with (un)healthy food store accessibility while assessing local differences and evaluating the importance of the immediate versus the wider food surroundings.
We formulated three research questions.
-
1)
How is unhealthy and healthy food accessibility associated with obesity prevalence in the Netherlands?
-
2)
How does the association between food accessibility and obesity prevalence vary locally in the Netherlands?
-
3)
How relevant for predicting obesity prevalence is unhealthy and healthy food supply in either the immediate or the wider surrounding of people?
The first two research questions build on the existing research, thereby extending it to a European setting. The third research question represents an additional step compared to most of the previous studies concerning local differences in the association between food accessibility and obesity. This is likely to provide additional evidence on where to focus public policies.
Based on the discussed theoretical and empirical background we formulated these three hypotheses;
Our first hypothesis is that better accessibility to unhealthy food is globally associated with higher obesity prevalence and better accessibility to healthy food with lower obesity prevalence, in line with the obesogenic environment theory.
Our second hypothesis is that food accessibility is more relevant for obesity prevalence in regions characterised by higher degrees of urbanisation in line with the previous studies from the US.
Our third hypothesis is that the direct food surrounding is more important than the wider food surrounding, due to the proximity to people's homes.
2. Material and methods
2.1. Setting
Our ecological study was based on all adults aged 19 or older living in private households in 2016 in the Netherlands. The spatial units of interest are neighbourhoods (according to a six-digit postal code, wijken) which are coherent regions of neighbourhoods without a formal status that are based on characteristics such as age structure, geographical barriers (e.g. busy roads), having similar urban and/or architectural features, or having similar functional, social, or political characteristics (Statistics Netherlands, 2017).
All spatial units with valid data on the variables used were included in our analysis. Of the initial 2960 neighbourhoods, 77 neighbourhoods – most of them small - could not be included in this study due either to missing information in obesity prevalence (n = 30) or to a missing value in any other variable of interest (n = 47). The final study sample covered 2836 neighbourhoods in total.
We explored spatial patterns for the entire Netherlands and also differentiated between regional subtypes: urban (≥1500 addresses per km2), suburban (500 ≤ 1500 addresses per km2), and rural neighbourhoods (<500 addresses per km2) in line with the definition of Statistics Netherlands (Statistics Netherlands, 2022a). This resulted in 785 neighbourhoods defined as urban, 756 as suburban, and 1295 as rural neighbourhoods. Urban neighbourhoods were more predominant in the west (see Supplementary Fig. S1 for the spatial distribution across the Netherlands).
In a sensitivity analysis, we used a different definition of urban and suburban subtypes developed by the OECD (OECD, 2019) which were based on functional urban areas (FUA), thereby differing between urban cores (n = 1007) and commuting zones (n = 1032).
2.2. Outcome: obesity data
The adult obesity prevalence data by neighbourhood in 2016 were obtained from the National Institute of Public Health and the Environment (RIVM) website (RIVM National Institute of Public Health and the Environment (2022a), ). The data represent estimated small-area proportions of obese (BMI ≥30) people and were available every four years. We decided to use the 2016 data instead of the most recent 2020 data because the 2020 data were affected by the COVID-19 pandemic. RIVM calculated small-area estimators for different health and lifestyle determinants across neighbourhoods in the Netherlands in 2016, using individual-level data from the Dutch Health Monitor 2016 collecting data from about 3.5% of the whole Dutch population (n = 457,153, age 19+, RIVM National Institute of Public Health and the Environment, 2022b). This monitor (“De Gezondheidsmonitor”) is a national survey database conducted every four years to observe the public health and lifestyle characteristics of Dutch individuals. Small-area estimations are necessary because the number of cases gathered in the Dutch Health Monitor are generally not sufficient to deliver per se valid measures for small-area characteristics. To yield small-area estimations, the RIVM uses generalized structured additive regression (STAR) modelling to carry out parameters via restrictive maximum likelihood (REML). 12 indicators at individual (age, sex, ethnicity, marital status), household (household type, size, capital, yearly income, income source, and home ownership) and neighbourhood (urbanisation, neighbourhood code) level were used to predict the small area obesity, smoking, and alcohol intake prevalence data for 2016. For further information on the methodology used, see van de Kassteele et al., 2017.
2.3. Exposure: food environment data
We studied unhealthy and healthy food supply in people's surroundings simultaneously by focusing on accessibility to three different food environment domains, namely 1) fast food stores (including grill/lunch rooms), which were defined as unhealthy food supply, 2) fresh food stores (e.g. vegetable shops, bakeries, health food shops), which were defined as healthy food supply, and 3) supermarkets, which were defined as healthy food supply in accordance with previous studies (Helbich et al., 2017; Michimi & Wimberly, 2010). For more detailed definitions of these three food environment domains, see Supplementary Table S1 showing English translations of the Dutch definitions, or see the original source (Statistics Netherlands, 2017). Accessibility is defined here as access to food store locations operationalised by their proximity in a person's surroundings (Downs et al., 2020). Proximity was measured by the average Euclidean distance to the next food facilities in 2016 and reflects the average distance between a resident's address and the nearest food store locations in a neighbourhood.
2.4. Confounding variables: sociodemographic, SES, and lifestyle data
We combined the obesity and food environment data at neighbourhood level additionally with socioeconomic and lifestyle data. As socioeconomic determinants, obtained from Statistics Netherlands (Statistics Netherlands, 2022b), we included sex (male inhabitants as a percentage), age (people aged 19 to 44 as a percentage, people aged 45 to 64 as a percentage, people aged 65 or older as a percentage), population density (number of people per km2), migration status (non-western immigrants as a percentage), unemployment (social welfare recipients as a percentage), and income (yearly income per inhabitant * 1000 Euros).
Lifestyle factors covered low alcohol consumption (percentage of those drinking not more than one glass of alcohol per day) and smoking (percentage of current smokers). Like the obesity prevalence data, these lifestyle data stem from the small-area estimations from the National Institute of Public Health and the Environment (RIVM National Institute of Public Health and the Environment, 2022c; van de Kassteele et al., 2017).
2.5. Methods
We linked the neighbourhood-level data obtained from the different sources by their unique six-digit postal codes.
As an explorative pre-analysis, univariate Global Moran's I was calculated for each of the variables used to test for spatial dependency. The spatial weights matrix used assumed a queen contiguity pattern, that is neighbourhoods share a common edge or a common vertex .
Subsequently, this weighting matrix was used to calculate Global Moran's I ranging from −1 (perfect dispersion) to 1 (perfect clustering):
| (i) |
where and index the neighborhoods, is the mean value of the variable of interest, and is the weight matrix.
We then mapped the spatial distribution of obesity prevalence across Dutch neighbourhoods in 2016 and visualised regional clusters of high obesity prevalence based on a local indicator of spatial association (LISA), which was done using local Moran's I:
| (ii) |
with .
In regard to our first research question on the global associations between (un)healthy food accessibility and obesity prevalence, we estimated multivariable (linear) Spatial Lag of X models (SLX) controlling for sociodemographic, SES, and lifestyle confounders:
| (iii) |
where represents an vector consisting of one observation on the dependent variable for every unit in the sample (), denotes an matrix of explanatory variables associated with the parameter vector , and is a vector of independently and identically distributed disturbance terms with zero mean and variance . The matrix of exogenous spatial lags is a vector. Consequently, the vector of response parameters θ is just like of order . We checked whether the residuals of obesity, the outcome of interest, was distributed normally among the neighbourhoods studied (Supplementary Fig. S2).
Robust Lagrange Multiplier diagnostics for spatial dependence in linear models showed coherently that spatial econometric models outperform OLS regressions (error dependence p < 0.001, spatially lagged dependent variable p < 0.001). We further decided that SLX outperformed SEM because spatial Hausman tests (p < 0.001) revealed that SEM would deliver biased estimators. We controlled all models for age, e.g. the proportions of people in the age of 45–64 and in the age of 65 or older, but not additionally for the proportion of people in the age of 19–44 due to multicollinearity and a VIF >10 when including this variable. Multicollinearity diagnostics revealed then acceptable correlations between the exogenous variables (VIF <2 for the entire Netherlands, VIF <5 for urban neighbourhoods, VIF <3 for suburban neighbourhoods, VIF <2 for rural neighbourhoods).
In regard to our second research question on the local variations in the associations between food accessibility and obesity, we first estimated an interaction model by regional subtype and food accessibility and for the entire Netherlands, and then stratified for regional subtypes (i.e. urban, suburban, and rural settings). Second, we estimated a geographically weighted regression (GWR). The GWR approach opens up the possibility of showing specific regional effect variations in the entire study region that do not necessarily relate only to global urban-rural differences.
A GWR estimates local parameters values. is the value if the outcome variable (here obesity prevalence) at each location with the coordinates (). represents the local estimated intercept and is the local estimated effect parameter of a variable .
| (iv) |
The estimations of the parameters were realised by using a kernel density estimation, which is a non-parametric way of estimating probability density functions (Brunsdon et al., 1996). For that purpose, the optimal kernel function and the bandwidth to be used have to be chosen. The bandwidth was then used as a smoothing parameter for the shape of the kernel function. The optimisation of the bandwidth was evaluated based on both Akaike's Information Criterion (AIC) and Cross Validation (CV). We decided to use the GWR model showing the best fit to the data based on highest R2 and lowest AIC. This was true for an adaptive kernel with a bisquare kernel function, which showed the best model fit when the AIC method was used. To find out exactly where in the Netherlands a reduction of unhealthy food accessibility would be beneficial to fight obesity, we performed the GWR for unhealthy fast food accessibility solely (but still controlled for all confounding variables). This was necessary because we found a (partially) high local correlation between unhealthy and healthy food accessibility which would bias the GWR estimations.
In regard to our third research question, we further decomposed each of the total effects yielded (TE, contribution of both the immediate and wider food surrounding) from the SLX approach into a direct effect (DE) and an indirect effect (IE). The direct effect shows the contribution of the local food environment on the local obesity prevalence, the indirect effect shows the contribution of the food environment in bordering locations (i.e. neighbourhood) on the local obesity prevalence. This indirect effect is also called spatial spillover effect. The indirect effects in the SLX models (equation iii) are reflected by the parameter estimates of the variables, and the direct effects by the parameter estimates of the variables.
All calculations were conducted on R 4.1.1 (R Core Team, 2021) using packages sp, spdep, spatialreg, spgwr.
3. Results
3.1. Descriptive results and mapping: the explorative pre-analyses
The average prevalence of obesity was 14.26% in the entire Netherlands in 2016. Obesity prevalence was slightly higher in urban neighbourhoods (14.61%) compared to suburban (14.19%) and rural (14.09%) settings (Table 1).
Table 1.
Descriptive statistics and spatial correlations of the variables used for the neighbourhoods: study participants ages 19 and older in the Netherlands in 2016.
| Variable |
Descriptive statistics |
Univariate Moran's I |
||||||
|---|---|---|---|---|---|---|---|---|
| Regional (sub-) type |
Netherlands |
Urban |
Suburban |
Rural |
Netherlands |
Urban |
Suburban |
Rural |
| Number of neighbourhoods | n = 2836 | n = 785 | n = 756 | n = 1295 | n = 2836 | n = 785 | n = 756 | n = 1295 |
| Outcome | ||||||||
| Obesity prevalence, % (sd) | 14.26 | 14.61 | 14.19 | 14.09 | 0.60** | 0.67** | 0.51** | 0.68** |
| (2.71) | (3.23) | (2.47) | (2.48) | |||||
| Food environment | ||||||||
| Average distance to next fast food store [km], % (sd) | 1.39 | 0.50 | 0.84 | 2.24 | 0.35** | 0.30** | 0.12** | 0.25** |
| (1.37) | (0.26) | (0.38) | (1.61) | |||||
| Average distance to next fresh food store [km], % (sd) | 1.29 | 0.51 | 0.87 | 2.00 | 0.27** | 0.32** | 0.08* | 0.18** |
| (1.24) | (0.27) | (0.39) | (1.50) | |||||
| Average distance to next supermarket [km], % (sd) | 1.52 | 0.63 | 0.97 | 2.38 | 0.27** | 0.31** | 0.07* | 0.15** |
| (1.36) | (0.26) | (0.41) | (1.59) | |||||
| Confounders | ||||||||
| Males, % (sd) | 50.27 | 49.22 | 49.80 | 51.17 | 0.17** | 0.16** | 0.06 | 0.09** |
| (2.10) | (2.26) | (1.82) | (1.74) | |||||
| People ages 19 to 44, % (sd) | 28.49 | 33.50 | 27.93 | 25.79 | 0.51** | 0.49** | 0.14** | 0.26** |
| (6.31) | (7.99) | (4.91) | (3.44) | |||||
| People ages 45 to 64, % (sd) | 30.29 | 26.76 | 29.96 | 32.62 | 0.34** | 0.35** | 0.11** | 0.24** |
| (4.81) | (4.40) | (4.18) | (3.97) | |||||
| People ages 65 and older, % (sd) | 19.09 | 18.23 | 19.60 | 19.31 | 0.27** | 0.28** | 0.20** | 0.30** |
| (5.97) | (7.50) | (6.30) | (4.52) | |||||
| Population density, no. of inhabitants/km2 (sd) | 2082.53 | 5749.22 | 1492.02 | 204.60 | 0.68** | 0.55** | 0.26** | <0.01 |
| (3388.40) | (4371.99) | (1635.99) | (349.85) | |||||
| Non-western immigrants, % (sd) | 7.14 | 16.67 | 6.13 | 1.95 | 0.61** | 0.53** | 0.16** | 0.10** |
| (9.65) | (12.69) | (5.57) | (2.38) | |||||
| Social welfare recipients, % (sd) | 3.33 | 3.50 | 3.39 | 3.19 | 0.21** | 0.43** | 0.23** | 0.24** |
| (1.30) | (0.84) | (1.15) | (1.57) | |||||
| Yearly net income [*1000 Euros], % (sd) | 25.04 | 25.31 | 25.64 | 24.52 | 0.47** | 0.51** | 0.40** | 0.48** |
| (4.80) | (6.28) | (4.28) | (3.90) | |||||
| Low alcohol consumption, % (sd) | 39.36 | 42.40 | 39.52 | 37.41 | 0.62** | 0.62** | 0.54** | 0.76** |
| (6.43) | (7.83) | (5.26) | (5.28) | |||||
| Smokers, % (sd) | 20.17 | 23.81 | 19.17 | 18.55 | 0.58** | 0.54** | 0.29** | 0.62** |
| (4.15) | (4.64) | (3.05) | (2.83) | |||||
Abbreviations: No, number; sd, standard deviation; km, kilometre(s).
Footnote: Significant results are denoted with *p < 0.05, **p < 0.01.
The average distance to the nearest fresh food store was 1.29 km, which was slightly lower compared to a fast-food store (average 1.39 km) or a supermarket (average 1.52 km). In rural settings, the same pattern was visible (fresh food: 2.0 km, fast food: 2.24 km, supermarket: 2.38 km). In urban and suburban settings, however, the next fast food store was more proximate (urban: 0.50 km, suburban: 0.84 km) than the next fresh food store (urban: 0.51 km, suburban: 0.87 km) or supermarket (urban: 0.63, suburban: 0.97 km).
All variables used were significantly spatially correlated (Moran's I with p < 0.001) showing that proximal neighbourhoods were more similar in the characteristics observed than more distal neighbourhoods. This was true for the entire Netherlands, but also when we stratified into urban, suburban, and rural regional subtypes (Table 1).
Higher obesity was observed in the north-east, south-west, and south-east of the country (Fig. 1, A), which were shown to be statistically significant clusters of high obesity (evaluated by local Moran's I/LISA map) (Fig. 1, B).
Fig. 1.
The spatial distribution of obesity prevalence and significant obesity clusters in the Netherlands in 2016
Abbreviations: No, number; km, kilometre(s); %, percentage. Footnote: Obesity prevalence in the Netherlands in 2016 (A), significant LISA clusters of obesity (B). Neighbourhoods that are not part of the analysis sample are coloured white.
Accessibility to both unhealthy and healthy food was generally better in the south of the Netherlands than in the north (Fig. 2A and B, C).
Fig. 2.
The spatial distribution of unhealthy and healthy food accessibility in the Netherlands in 2016
Abbreviations: No, number; km, kilometre(s); %, percentage. Footnote: Accessibility to fast food stores defined as unhealthy food (A); accessibility to fresh food stores defined as healthy food (B); accessibility to supermarkets defined as healthy food (C). Neighbourhoods that are not part of the analysis sample are coloured white.
3.2. The global associations between unhealthy and healthy food accessibility and obesity prevalence in the Netherlands in 2016
In regard to our first research question, our Spatial lag of X model for the entire Netherlands showed that worse fast food accessibility (i.e. increase in the average distance to the next fast food store) was associated with lower obesity prevalence (TE: −0.15, p = 0.02) (Table 1, model Netherlands). For the average distance to the next fresh food store and supermarkets we found no significant global associations for the entire Netherlands. We further found in the multivariate model that obesity prevalence was higher in suburban (TE: +1.03, p < 0.01), but not in rural neighbourhoods, compared to urban neighbourhoods.
3.3. Regional variations in the association between food accessibility and obesity: regional subtype analyses
In regard to our second research question focusing on differences in the association between food accessibility and obesity between regional subtypes, we first introduced interaction terms among all of the three food accessibility variables (fast food, fresh food, supermarkets) and the regional subtype variable in the model for the entire Netherlands (we will only refer to the total effects (TE)). This interaction model revealed significant interactions for fast food accessibility and rural neighbourhoods (TE: +2.73, p < 0.01, ref. urban), and fresh food accessibility and suburban (TE: −4.65, p < 0.01, ref. urban) as well as rural neighbourhoods (−5.03, p < 0.01, ref. urban) (Supplementary Table S2).
We then estimated Spatial Lag of X models stratified by the regional subtype, meaning separately for urban, suburban, and rural neighbourhoods. The stratified models showed that worse accessibility to fast food (i.e. an increase in the average distance to the next fast food store) was related to lower obesity prevalence in urban (TE: −2.94, p < 0.01), suburban (TE: −0.65, p = 0.03), and rural neighbourhoods (TE: −0.12, p = 0.04) with the highest effect size for urban settings (Table 2, models urban & suburban & rural).
Table 2.
The associations between unhealthy and healthy food accessibility and obesity prevalence at the ecological level among study participants ages 19 and older in the Netherlands in 2016: results from Spatial Lag of X models.
| Variable | Netherlands |
Urban |
Suburban |
Rural |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DEb | IEc | TEd | DEb | IEc | TEd | DEb | IEc | TEd | DEb | IEc | TEd | |
| Food environment | ||||||||||||
| Average distance to next fast food store, km | −0.02 | −0.13* | −0.15* | −0.98** | −1.94** | −2.94** | −0.09 | −0.56* | −0.65* | −0.04 | −0.08 | −0.12* |
| Average distance to next fresh food store, km | −0.07 | 0.10 | 0.03 | 1.17** | 2.54** | 3.71** | −0.36 | 0.23 | −0.13 | −0.08 | 0.07 | −0.01 |
| Average distance to next supermarket, km |
−0.02 |
0.13 |
0.11 |
−0.21 |
0.17 |
−0.05 |
−0.27 |
0.36 |
0.09 |
0.02 |
0.03 |
0.04 |
| Confounders | ||||||||||||
| Males, % |
−0.10** |
−0.04 |
−0.14** |
−0.08** |
<0.01 |
−0.08* |
−0.05 |
−0.04 |
−0.09* |
−0.03 |
−0.08** |
−0.12** |
| People ages 19 to 44, % (ref.) | – | – | – | – | – | – | – | – | – | – | – | – |
| People ages 45 to 64, % | 0.12** | 0.14** | 0.26** | 0.15** | 0.07** | 0.22** | 0.12** | 0.05* | 0.16** | 0.07** | 0.13** | 0.21** |
| People ages 65 and older, % | 0.06** | 0.02 | 0.07** | 0.05** | 0.04* | 0.09** | 0.03** | 0.01 | 0.04** | 0.08** | 0.01 | 0.09** |
| Population densitya, no. of inhabitants/km2 | – | – | – | −1.14 | −4.82 | −5.97** | 4.04 | −1.08 | 2.97 | 43.81** | −27.65 | 16.17 |
| Non-western immigrants, % | <0.01 | −0.03* | −0.03** | −0.02 | 0.02 | <0.01 | 0.01 | −0.03 | −0.02 | −0.04 | −0.09 | −0.12** |
| Social welfare recipients, % | 0.22** | 0.10* | 0.32** | 0.43** | 0.30** | 0.73** | 0.24** | −0.08 | 0.17* | 0.14** | 0.13* | 0.26** |
| Yearly net income [*1000 Euros] | −0.10** | −0.11** | −0.21** | −0.10** | −0.05** | −0.15** | −0.19** | −0.06** | −0.25** | −0.09** | −0.06* | −0.15** |
| Low alcohol consumption, % | 0.18** | 0.02 | 0.20** | 0.24** | −0.05** | 0.19** | 0.14** | 0.02 | 0.16** | 0.12** | 0.06** | 0.18** |
| Smokers, % | 0.28** | −0.02 | 0.26** | 0.20** | −0.02 | 0.18** | 0.22** | 0.09** | 0.31** | 0.45** | −0.06 | 0.39** |
| Regional subtype, ref. Urban | ||||||||||||
| Suburban | 0.26* | 0.77** | 1.03** | |||||||||
| Rural |
0.36* |
−0.10 |
0.25 |
|||||||||
| R2 | 0.6796 | 0.8182 | 0.6964 | 0.5983 | ||||||||
Abbreviations: No, number; sd, standard deviation; km, kilometre(s).
Footnote: Significant results are denoted with *p < 0.05, **p < 0.01. The models were controlled for sex, age, population density or regional subtype, migration status, unemployment, income, alcohol consumption, and smoking.
Point estimators × 10–5.
DE = direct effect, which is the contribution of the local food environment on the local obesity prevalence (immediate food surrounding).
IE = indirect effect, which is the contribution of the food environment in bordering locations on the local obesity prevalence (wider food surrounding).
TE = total effect, which is the sum of the direct and indirect effect and the total contribution of the food environment.
For fresh food accessibility, we found statistically significant associations only for urban neighbourhoods. That is to say, worse accessibility to the next fresh food store (i.e. increase in the average distance to the store) was associated with higher obesity prevalence (TE: +3.71, p < 0.01).
For supermarket accessibility, no statistically significant associations were observed in the SLX models.
We estimated a sensitivity analysis using a different definition of urban and suburban subtypes developed by the OECD (OECD, 2019), which were based on functional urban areas (FUA). This model confirmed the results from our main models (Supplementary Table S3), but showed worse model performances (R2 FUA urban cores = 0.7803 < R2 Main urban = 0.8182; R2 FUA commuting zone = 0.6351 < R2 Main suburban = 0.6964).
3.4. Visualisation of local differences in the association between unhealthy food accessibility and obesity prevalence across the Netherlands in 2016
In regard to our second research question and our interest in visualising local differences in food accessibility-obesity associations, we also performed a geographically weighted regression revealing local variations across the entire Netherlands. The GWR was performed for fast food accessibility and not for the other food accessibility variables due to the importance of fast food accessibility found in the global associations (Spatial Lag of X models).
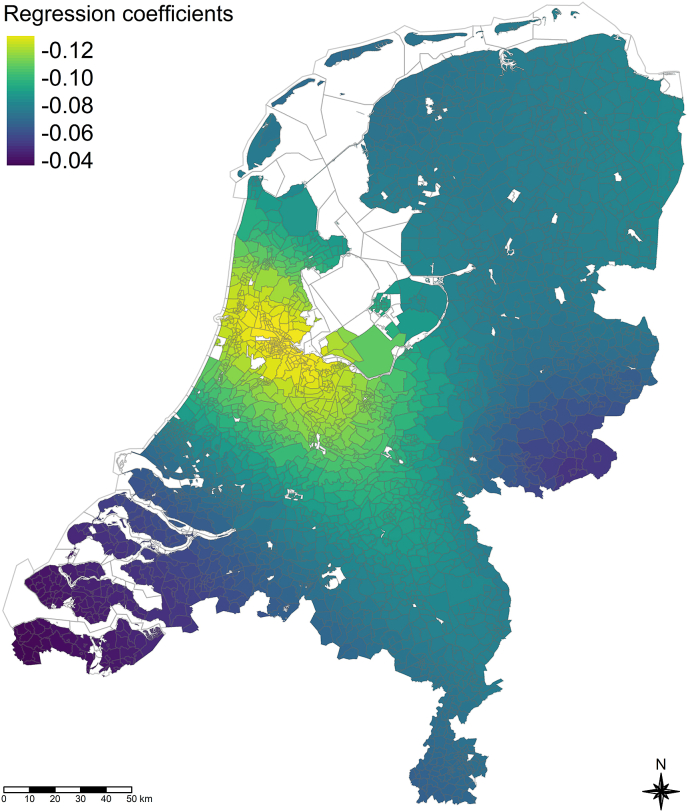
Also, our GWR analysis did indeed show important local effect variations of unhealthy food accessibility on obesity prevalence in 2016 (Fig. 3). That is, stronger relationships (coloured yellow and bright green, β: −0.12 to −0.10) were observed in the Randstad — a conurbation in the central-western Netherlands consisting mainly of the four largest Dutch cities (Amsterdam, Rotterdam, The Hague, and Utrecht) and one of the largest metropolitan regions in Europe. The strongest relationships were seen around the metropolitan region of Amsterdam (yellow). The weakest relationships were observed for the south-west around the region of Zeeland (β: −0.06 to −0.04), that is mainly characterized by rural neighbourhoods. Model performance was good (Global R2 = 0.6760), but slightly worse than the Spatial Lag of X model for the entire Netherlands and unhealthy food (R2 = 0.6817, Supplementary Table S4, Netherlands).
Fig. 3.
The spatial variations in the associations between fast food accessibility and obesity prevalence in the Netherlands in 2016 (geographically weighted regression). Footnote: The map shows the regression coefficients for fast food accessibility (measured in average distance to the next fast food store) on obesity prevalence (in %) across the Netherlands. Coefficients were estimated by a geographically weighted regression (GWR) model using a bisquare weighting function and an adaptive bandwidth evaluated by using Akaike's Information Criterion (AIC). Neighbourhoods that are not part of the analysis sample are coloured white. The model was controlled for sex, age, regional subtype, migration status, unemployment, income, alcohol consumption, and smoking.
3.5. The decomposition of global and local associations between food accessibility and obesity
In regard to our third research question and our interest in the contributions of the immediate versus the wider food environment in the food accessibility-obesity associations, we decomposed each of the total associations into a direct effect (DE, immediate food surrounding) and an indirect effect (IE, wider food surrounding).
The decomposition showed that for the entire Netherlands and unhealthy fast food, the contribution of the wider food surrounding was more important (IE: −0.13, p < 0.01, 87% of the TE) than the contribution of the non-significant immediate food surrounding (−0.02, p = 0.671, 13% of the TE) (Table 2, Netherlands).
For the regional subtypes, we found that the wider food surrounding was more important than the immediate food surrounding throughout. Significant contributions were found for fast food accessibility in urban (IE: 1.94, p < 0.01, 66% of the TE) and suburban (IE: 0.59, p = 0.032, 83% of the TE) but not in rural settings. For fresh food accessibility, we found a significant contribution of the wider food surrounding in urban settings only (IE: +2.54, p < 0.01, 69% of the TE) (Table 2, urban & suburban).
4. Discussion
4.1. Key findings
Regarding the geographic distribution of obesity prevalence in the Netherlands in 2016, our results show that obesity prevalence was slightly higher in urban neighbourhoods (14.61%) compared to suburban (14.19%) and rural (14.09%) settings. In the univariate analysis, regional clusters of high obesity were observed in selected areas in the north-east, south-west, and south-east of the country, which are characterised by lower population density and mainly suburban and rural neighbourhoods. When we controlled for food accessibility, socio-demographic and socio-economic determinants, obesity prevalence proved significantly higher in suburban than in urban or rural neighbourhoods. This illustrates that the clusters of obesity prevalence we observed are also the regions that perform less regarding socio-economic development, and exhibit a higher extent of ageing.
Regarding the nationwide association of obesity prevalence with (un)healthy food store accessibility, we observed that worse accessibility to unhealthy food was globally associated with lower obesity prevalence in the entire Netherlands, but there were no associations for healthy food and supermarket accessibility.
Regarding the local differences in the food accessibility-obesity associations, we found that worse accessibility to unhealthy food was associated with lower obesity prevalence in urban, suburban, and rural neighbourhoods taken separately, but this seems to be more important for urban and suburban than for rural neighbourhoods. Better accessibility to fresh food stores was only relevant for obesity in urban settings. Again, no associations were found for supermarket accessibility. Interesting variations across the entire Netherlands were visualised, and the associations were strongest in the Randstad, one of the largest metropolitan regions in Europe.
Regarding the contribution of the immediate versus wider food surrounding, we found for the entire Netherlands and the regional subtypes that the contributions of the wider food surrounding (= food environment in bordering neighbourhoods) on obesity were more important than the contributions of the immediate food surrounding (= food environment in the same neighbourhood).
In line with previous research, this study found for the confounding variables that higher prevalence of obesity is associated with a higher share of males, middle age, unemployment, lower income, higher alcohol consumption, and smoking.
4.2. Discussion of our findings
Our finding that food accessibility is relevant for obesity (research question 1) has already been shown in previous studies conducted for the US, which used either BMI (Chen et al., 2019) or obesity (Huang, 2021, Mazidi et al. 2017; Michimi & Wimberly) as outcomes. Our results indicate that this association – and the underlying theory of an obesogenic environment - might be important for European countries as well, as illustrated by the case of the Netherlands.
In line with the obesogenic environment theory, we found that unhealthy fast food was more relevant than healthy fresh food. One explanation for this finding could be that if people have to decide to buy convenience food, they use the option with the lowest (relative) time costs (Probst et al., 2006; Pucher & Renne, 2005). Unhealthy fast food is often ready-to-eat so that the effort required to prepare meals is eliminated. If (convenient) healthy fresh food is not easy to reach, people could switch to other, potentially unhealthier food sources in the closer surroundings. This explanation is supported by our finding that better accessibility to unhealthy food was associated with higher obesity (but not better healthy food accessibility to lower obesity prevalence) also in rural neighbourhoods, although healthy fresh food is, on average, more proximate there.
Another interesting finding of our study was that accessibility to supermarkets, which were defined as locations offering healthy food in accordance with previous research (Michimi & Wimberly, Helbich et al., 2010), was not spatially related to obesity prevalence. This could be explained by the fact that supermarkets do not offer a clear assortment of unhealthy or healthy foods, but rather a mixture of both. For the Netherlands, however, a previous study on the proportion of healthy and unhealthy foods promoted in the country came to the result that the majority, about 70%, of promotions were categorised as unhealthy food in Dutch supermarkets (Ravensbergen et al., 2015). On the other hand, the intention to go to a supermarket is likely to be more deliberate with a view for healthy food consumption, compared to fast food restaurants. Second, we know for fast food restaurants that the main motivation to go there is to have a quick, spontaneous meal nearby (Rydell et al., 2008). Because we did not measure which products people really bought and eat, but only measured their accessibility, we were not able to disentangle the factual mechanisms explaining this finding. More research is needed here to explore and combine shopping motivations and the real nutrition behaviours of people shopping in supermarkets.
Our finding that unhealthy fast food accessibility and healthy fresh food accessibility play a more important role in regions with a higher degree of urbanity (research question 2) — which was also found for the USA (Michimi & Wimberly, 2010) — might be explained by the existence of a certain threshold distance, beyond which the distance to healthy food locations no longer impacts obesity, as postulated by Michimi & Wimberly, 2010. Rural residents have to travel longer distances when they do their daily activities (Probst et al., 2006; Pucher & Renne, 2005), which means that their relative (time) costs weigh less heavy when they want to reach an appropriate and healthier food location, especially when cars have to be used for transportation (Zijlstra et al., 2022). Our findings are in line with previous results for the US which — by using census data from 2006 at the county level — found relationships between healthy food accessibility and adult obesity prevalence for metropolitan (urban) regions, but not for non-metropolitan (rural) regions (Michimi & Wimberly, 2010). Compared to the previous research for the US, our study yielded further evidence of the importance of a distinction between regional subtypes when studying the associations between food accessibility and obesity. This was underlined by both approaches used in this paper, namely the multivariate global regression approach (Spatial Lag of X model) and by the local regression approach (geographically weighted regression). Taking the findings from both approaches together, we can conclude that for the Netherlands especially the risk of obesity for inhabitants living in the Randstad could be most affected by easy access to unhealthy food. There is an expected increase in the next decades in urban population in Europe (Pineda et al., 2018) and the Netherlands (Statistics Netherlands, 2019), which calls for special attention to food environment risks in such high-urbanicity regions.
Another interesting finding of our study was that the indirect effects (i.e. wider food environment) contributed more to the total effects compared to the direct effects (i.e. immediate food environment), and this was true for the healthy as well as the unhealthy food environments and independent of the regional subtype (research question 3). The food environment (both healthy and unhealthy) in bordering neighbourhoods may therefore be more important for developing obesity than the food environment in people's direct, immediate surroundings. This is in line with a study for the US, which showed that the average distance between the food establishments and homes was 2.6 miles and only 34% of the food establishments people went to were in participants neighbourhood census tract (Liu et al., 2015). One pathway explaining this finding could be that residential areas are normally further away from commercial areas, where food locations are more present. This would indicate that people usually travel across administrative borders to buy most of their daily food. Furthermore, most people do not work in the same neighbourhood in which they live in. More than 20% of Europeans commute at least 90 min daily (SD Worx, 2018). The Netherlands Environmental Assessment Agency found that Dutch commute on average 19 km per day (Netherlands Environmental Assessment Agency, 2020). This would explain why people have to necessarily travel between neighbourhoods in their daily lives, and may then purchase food on their way home.
Another explanation for the relevance of the indirect effects could lie in the existence and usage of delivery services and outlets in the wider surroundings of people, so people could buy food easily from a larger radius. A previous Dutch study found that between 2004 and 2018 a remarkable increase in delivery outlets was observed (Pinho et al., 2020). Of note, delivered (fast) food is primarily classified as unhealthy food (Partridge et al., 2020).
Finally, a possible explanation for the importance of the wider food surrounding could simply lie in the small area units we used (neighbourhood level).
In sum, we argue that our findings based on data for 2016 are suitable to derive appropriate policy implications for the post-Covid era in the Netherlands. General patterns and differences in the food landscapes between urban, suburban, and rural settings were already existent in the Netherlands in 2016 (Pinho et al., 2020) and additional descriptive results showed that, from 2016 to 2019, there were just slight changes in the accessibility to the different food locations for the entire Netherlands, but also for urban, suburban, and rural settings (results not shown). Pinho et al. (2020) observed for example a small increase in the availability of fast food restaurants from 2004 to 2018. If this trend has continued until today, the associations between unhealthy food and obesity observed in our study could be even stronger, which is why our results are still of public and policy relevance.
4.3. Evaluation of data and methods
The added value of our study lies in the following three aspects:
First, we have distinguished different regional subtypes in order to consider structural urban-suburban-rural differences contributing to varying associations between food accessibility and obesity (see Lam et al., 2021).
Second, we have used spatial econometric modelling, which was possible due to the ecological design of our study. This has rarely been used in previous research (see the studies using non-spatial econometric regression models: de Vogli et al., 2011; Mazidi & Speakman, 2017), so that it has been difficult to derive policy interventions where they are most needed.
Third, our study integrates both unhealthy and healthy food accessibility, considering that different kinds of food locations may stand in a competitive relationship when people buy food (Mason, Pearce, & Cummins, 2018; Walker et al., 2020).
However, our study is not without limitations.
First, obesity and the lifestyle confounders used all stem from small-area estimations conducted by the RIVM (RIVM National Institute of Public Health and the Environment (2022a), ; van de Kassteele et al., 2017). This was done because the small sample size of the health survey requires the use of small-area estimations in order to reach a valid outcome. Even when the data are based on estimations, they come from an extensive individual-level data source covering 457,153 Dutch adults. Validity analyses showed good model performance for the small-area estimation models (van de Kassteele et al., 2017).
Second, we used obesity prevalence as an outcome instead of a more continuous measure such as (metric) body weight or BMI. Exploring the effects of food environment on body weight or BMI may draw a more differentiated picture of both the regional differences in excessive weight and the dose-response-relationship. However, at small area levels, these data are generally not available, and would result in additional difficulties in obtaining robust values at the small area level.
Third, we decided to take the definitions for unhealthy and healthy food from Statistics Netherlands because no other data were available to measure food environments more adequately. Although this makes the definitions specific for the Dutch context, it is difficult to compare the results to other countries, which may use different definitions of unhealthy fast food and healthy fresh food.
Fourth, our study used the average distance to nearest food locations as an indicator to measure the extent to which people have access to unhealthy or healthy food. This, however, does not imply that people indeed purchase (and eat) food from these food locations. Additionally, we do not know how long people are exposed to the food environmental characteristics measured in 2016 due to the cross-sectional design and missing information on the duration of residence. A previous longitudinal study in the Netherlands found that, over 18 months, an increase of the number of grocery stores was associated with a decrease in BMI, while an increase in the number of fast-food restaurants was associated with an increase in BMI (Acciai et al., 2022). This suggests that already shorter exposure durations can change the factual nutrition behaviour and subsequently people's BMI or risk of obesity. We tried to integrate this by introducing a time lag between the independent variables (most from 2015) and the dependent variable (from 2016). This lagged model confirmed our main results (Supplementary Table S5).
Future studies could try to regard the exposure time, differ between accessibility and actual access, exploring whether better accessibility to unhealthy food does indeed lead to an increase in unhealthy food consumption. Currently such data, when available, tend to be used purely for individual-level studies. We recommend using these data for ecological studies as well, because they can answer different questions. Individual-level studies could investigate the lagged association between food environmental characteristics and obesity by using longitudinal data to gain insights into how long it takes until (changes) in the food environment lead to changes in BMI and the risk of obesity.
5. Conclusion
The findings of our ecological study for the Netherlands suggest that Dutch public health policies and urban planners should focus more on reducing unhealthy food supply than on expanding healthy food supply when they aim to reduce obesity prevalence.
Attention is especially demanded in urban areas of the Netherlands and specifically in the Randstad region, which have the strongest associations between unhealthy fast food accessibility and obesity prevalence, but also in the suburban and rural areas in the northeast, southwest, and southeast that showed high obesity clusters, which are linked to their socio-demographic and socio-economic situation.
The larger importance of the wider food surroundings compared to the immediate food surroundings thus calls for a superordinate policy strategy across municipal administrative borders in fighting obesogenic food environments.
Ethical statement
This research was conducted in accordance with the principles embodied in the Declaration of Helsinki and in accordance with local statutory requirements (Netherlands Code of Conduct for Research Integrity). The study is approved by the Research Ethics Committee of the Faculty of Spatial Sciences (FSS) of the University of Groningen, the Netherlands. Because the used data were aggregated at the neighbourhood level, disclosure and tracing of individuals was not possible.
Author statement
Benjamin Aretz: Conceptualization, Methodology, Software, Formal analysis, Investigation, Data curation, Writing - original draft, Writing – review & editing, Visualization. Rafael Costa: Conceptualization, Methodology, Formal analysis, Investigation, Writing - original draft, Writing – review & editing. Gabriele Doblhammer: Conceptualization, Writing - original draft, Writing – review & editing, Supervision. Fanny Janssen: Conceptualization, Investigation, Visualization, Writing - original draft, Writing - original draft, Project administration, Supervision.
Declaration of competing interest
The authors declare they have no current or potential competing (financial) interests.
Acknowledgements
We thank Statistics Netherlands for providing the data, the GIS centre in Groningen for the support in processing the geodata, and Renée Lüskow for language editing. Special thanks go to Anna-Victoria Holtz, who contributed to the literature review. No conflict of interest to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2022.101332.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
Data availability
Data will be made available on request.
References
- Acciai F., DeWeese R.S., Yedidia M.J., Lloyd K., Tulloch D., DeLia D., Ohri-Vachaspati, Punam Differential associations between changes in food environment and changes in body mass index among adults living in urban, low-income communities. Journal of Nutrition. 2022 doi: 10.1093/jn/nxac186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown A.G.M., Esposito L.E., Fisher R.A., Nicastro H.L., Tabor D.C., Walker J.R. Food insecurity and obesity: Research gaps, opportunities, and challenges. Translational behavioral medicine. 2019;9(5):980–987. doi: 10.1093/tbm/ibz117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunsdon C., Fotheringham A.S., Charlton M.E. Geographically weighted regression: A method for exploring spatial nonstationarity. Geographical Analysis. 1996;28(4):281–298. doi: 10.1111/j.1538-4632.1996.tb00936.x. [DOI] [Google Scholar]
- Burleyson C. 2020. U.S. Census state and county population estimates 2000-2019. [Google Scholar]
- Chen M., Creger T., Howard V., Judd S.E., Harrington K.F., Fontaine K.R. Association of community food environment and obesity among US adults: A geographical information system analysis. Journal of Epidemiology & Community Health. 2019;73(2):148–155. doi: 10.1136/jech-2018-210838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb L.K., Appel L.J., Franco M., Jones-Smith, Jessica C., Nur A., Anderson C.A.M. The relationship of the local food environment with obesity: A systematic review of methods, study quality, and results. Obesity. 2015;23(7):1331–1344. doi: 10.1002/oby.21118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downs S.M., Ahmed S., Fanzo J., Herforth A. Food environment typology: Advancing an expanded definition, framework, and methodological approach for improved characterization of wild, cultivated, and built food environments toward sustainable diets. Foods. 2020;9(4) doi: 10.3390/foods9040532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger G., Swinburn B. An "ecological" approach to the obesity pandemic. BMJ. 1997;315(7106):477–480. doi: 10.1136/bmj.315.7106.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eurostat Eurostat regional yearbook. 2021. https://ec.europa.eu/eurostat/documents/3217494/13389103/KS-HA-21-001-EN-N.pdf/1358b0d3-a9fe-2869-53a0-37b59b413ddd?t=1631630029904 Online available under.
- Fraser L.K., Clarke G.P., Cade J.E., Edwards K.L. Fast food and obesity: A spatial analysis in a large United Kingdom population of children aged 13-15. American Journal of Preventive Medicine. 2012;42(5):e77–e85. doi: 10.1016/j.amepre.2012.02.007. [DOI] [PubMed] [Google Scholar]
- Giskes K., van Lenthe F., Avendano-Pabon M., Brug J. A systematic review of environmental factors and obesogenic dietary intakes among adults: Are we getting closer to understanding obesogenic environments? Obesity Reviews: An Official Journal of the International Association for the Study of Obesity. 2011;12(5):e95–e106. doi: 10.1111/j.1467-789X.2010.00769.x. [DOI] [PubMed] [Google Scholar]
- Helbich M., Schadenberg B., Hagenauer J., Poelman M. Food deserts? Healthy food access in Amsterdam. Applied Geography. 2017;83:1–12. doi: 10.1016/j.apgeog.2017.02.015. [DOI] [Google Scholar]
- Huang H. A spatial analysis of obesity: Interaction of urban food environments and racial segregation in chicago. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2021;98(5):676–686. doi: 10.1007/s11524-021-00553-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery R.W., Baxter J., McGuire M., Linde J. The international journal of behavioral nutrition and physical activity 3. 2006. Are fast food restaurants an environmental risk factor for obesity? 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Kassteele J., Zwakhals L., Breugelmans O., Ameling C., van den Brink, Carolien Estimating the prevalence of 26 health-related indicators at neighbourhood level in The Netherlands using structured additive regression. International Journal of Health Geographics. 2017;16(1):23. doi: 10.1186/s12942-017-0097-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam T.M., Vaartjes I., Grobbee D.E., Karssenberg D., Lakerveld J. Associations between the built environment and obesity: An umbrella review. International Journal of Health Geographics. 2021;20(1):7. doi: 10.1186/s12942-021-00260-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson N.I., Story M.T., Nelson M.C. Neighborhood environments: Disparities in access to healthy foods in the U.S. American Journal of Preventive Medicine. 2009;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- Lehto S., Buchweitz M., Klimm A., Straßburger R., Bechtold C., Ulberth F. Comparison of food colour regulations in the EU and the US: A review of current provisions. Food Additives & Contaminants: Part A. 2017;34(3):335–355. doi: 10.1080/19440049.2016.1274431. [DOI] [PubMed] [Google Scholar]
- Lim H.J., Xue H., Wang Y. In: Handbook of eating and drinking. Interdisciplinary perspectives. Herbert H., Meiselman L., editors. Springer; Cham: 2020. Global trends in obesity; pp. 1217–1235. [Google Scholar]
- Liu J.L., Han B., Cohen D.A. Beyond neighborhood food environments: Distance traveled to food establishments in 5 US cities, 2009-2011. Preventing Chronic Disease. 2015;12:E126. doi: 10.5888/pcd12.150065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenbach J.D., Charreire H., Glonti K., Bárdos H., Rutter H., Compernolle S., et al. Exploring the relation of spatial access to fast food outlets with body weight: A mediation analysis. Environment and Behavior. 2019;51(4):401–430. doi: 10.1177/0013916517749876. [DOI] [Google Scholar]
- Mason K.E., Pearce N., Cummins S. Associations between fast food and physical activity environments and adiposity in mid-life: Cross-sectional, observational evidence from UK biobank. The Lancet Public Health. 2018;3(1):e24–e33. doi: 10.1016/S2468-2667(17)30212-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazidi M., Speakman J.R. Higher densities of fast-food and full-service restaurants are not associated with obesity prevalence. American Journal of Clinical Nutrition. 2017;106(2):603–613. doi: 10.3945/ajcn.116.151407. [DOI] [PubMed] [Google Scholar]
- Michimi A., Wimberly M.C. Associations of supermarket accessibility with obesity and fruit and vegetable consumption in the conterminous United States. International Journal of Health Geographics. 2010;9:49. doi: 10.1186/1476-072X-9-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales M.E., Berkowitz S.A. The relationship between food insecurity, dietary patterns, and obesity. Current nutrition reports. 2016;5(1):54–60. doi: 10.1007/s13668-016-0153-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland K., Roux D., Ana V., Wing S. Supermarkets, other food stores, and obesity: The atherosclerosis risk in communities study. American Journal of Preventive Medicine. 2006;30(4):333–339. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- NCD Risk Factor Collaboration Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature. 2019;569(7755):260–264. doi: 10.1038/s41586-019-1171-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netherlands Environmental Assessment Agency Afstanden woon-werkverkeer nemen toe; hoogopgeleide fulltime werkende man reist het verst. 2020. https://www.pbl.nl/nieuws/2020/afstanden-woon-werkverkeer-nemen-toe-hoogopgeleide-fulltime-werkende-man-reist-het-verst Online available under.
- OECD Functional urban areas. 2019. https://www.oecd.org/cfe/regionaldevelopment/Netherlands.pdf Online available under.
- Partridge S.R., Gibson A.A., Roy R., Malloy J.A., Raeside R., Jia S.S., et al. Junk food on demand: A cross-sectional analysis of the nutritional quality of popular online food delivery outlets in Australia and New Zealand. Nutrients. 2020;12(10) doi: 10.3390/nu12103107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pineda E., Sanchez-Romero, Maria L., Brown M., Jaccard A., Jewell J., Galea G., et al. Forecasting future trends in obesity across Europe: The value of improving surveillance. Obesity facts. 2018;11(5):360–371. doi: 10.1159/000492115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinho M.G.M., Mackenbach J.D., Braver N.R. den, Beulens J.J.W., Brug J., Lakerveld J. Recent changes in the Dutch foodscape: Socioeconomic and urban-rural differences. International Journal of Behavioral Nutrition and Physical Activity. 2020;17(1):43. doi: 10.1186/s12966-020-00944-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Probst J.C., Laditka S.B., Moore C.G., Harun N., Powell M.P., Baxley E.G. Rural-urban differences in depression prevalence: Implications for family medicine. Family Medicine. 2006;38(9):653–660. [PubMed] [Google Scholar]
- Pucher J., Renne J.L. Rural mobility and mode choice: Evidence from the 2001 national household travel survey. Transportation. 2005;32(2):165–186. doi: 10.1007/s11116-004-5508-3. [DOI] [Google Scholar]
- R Core Team . 2021. R: A language and environment for statistical computing.https://www.R-project.org/ Vienna, Austria. Online available under. [Google Scholar]
- Ravensbergen E.A.H., Waterlander W.E., Kroeze W., Steenhuis I.H.M. Healthy or unhealthy on sale? A cross-sectional study on the proportion of healthy and unhealthy foods promoted through flyer advertising by supermarkets in The Netherlands. BMC Public Health. 2015;15:470. doi: 10.1186/s12889-015-1748-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RIVM National Institute of Public Health and the Environment (2022a): Obesity data at neighbourhood level ("wijken"). Online available under https://www.vzinfo.nl/overgewicht/regionaal/obesitas, zuletzt geprüft am 05.05.2022.
- RIVM National Institute of Public Health and the Environment . 2022. De Gezondheidsmonitors. Online available under monitorgezondheid.nl. [Google Scholar]
- RIVM National Institute of Public Health and the Environment Gezondheidsmonitor Volwassenen en Ouderen. 2022. https://www.monitorgezondheid.nl/gezondheidsmonitor-volwassenen-en-ouderen Online available under.
- Rydell S.A., Harnack L.J., Oakes J.M., Story M., Jeffery R.W., French S.A. Why eat at fast-food restaurants: Reported reasons among frequent consumers. Journal of the American Dietetic Association. 2008;108(12):2066–2070. doi: 10.1016/j.jada.2008.09.008. [DOI] [PubMed] [Google Scholar]
- Statistics Netherlands . 2017. Toelichting Wijk- en Buurtkaart 2015, 2016 en 2017.https://www.cbs.nl/-/media/_pdf/2017/36/2017ep37-toelichting-wijk-en-buurtkaart-2017.pdf Online available under. [Google Scholar]
- Statistics Netherlands PBL/CBS Regionale bevolkings- en huishoudensprognose 2019–2050. 2019. https://www.cbs.nl/nl-nl/achtergrond/2019/41/pbl-cbs-regionale-bevolkings-en-huishoudensprognose-2019-2050 Online available under.
- Statistics Netherlands Degree of urbanisation. 2022. https://www.cbs.nl/en-gb/news/2007/07/young-people-live-in-cities-children-in-rural-areas/degree-of-urbanisation Online available under.
- Statistics Netherlands . 2022. Kerncijfers wijken en buurten 2004-2021.https://www.cbs.nl/nl-nl/reeksen/kerncijfers-wijken-en-buurten Online available under. [Google Scholar]
- Swinburn B., Egger G., Raza F. Dissecting obesogenic environments: The development and application of a framework for identifying and prioritizing environmental interventions for obesity. Preventive Medicine. 1999;29(6):563–570. doi: 10.1006/pmed.1999.0585. [DOI] [PubMed] [Google Scholar]
- Swinburn B.A., Sacks G., Hall K.D., McPherson K., Finegood D.T., Moodie M.L., Gortmaker S.L. The global obesity pandemic: Shaped by global drivers and local environments. The Lancet. 2011;378(9793):804–814. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- de Vogli R., Kouvonen A., Gimeno D. ‘Globesization’: Ecological evidence on the relationship between fast food outlets and obesity among 26 advanced economies. Critical Public Health. 2011;21(4):395–402. doi: 10.1080/09581596.2011.619964. [DOI] [Google Scholar]
- Walker B.B., Shashank A., Gasevic D., Schuurman N., Poirier P., Teo K., et al. The local food environment and obesity: Evidence from three cities. Obesity. 2020;28(1):40–45. doi: 10.1002/oby.22614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO World Health Organization European regional obesity report 2022. 2022. https://apps.who.int/iris/bitstream/handle/10665/353747/9789289057738-eng.pdf Online available under.
- Worx S.D. More than 20% of Europeans commute at least 90 minutes daily. 2018. https://www.sdworx.com/about-sd-worx/press/2018-09-20-more-20-europeans-commute-least-90-minutes-daily Online available under.
- Zijlstra T., Bakker S., Wite J.-J. The widespread car ownership in The Netherlands. 2022. https://english.kimnet.nl/publications/publications/2022/02/22/the-widespread-car-ownership-in-the-netherlands Online available under.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.