Abstract
Fragility fractures of the pelvis are a frequently encountered injury in orthopedic practice. These injuries occur in patients with diminished bone density secondary to low energy mechanisms. This injury is associated with increased mortality and decreased quality of life. These fractures have been treated conservatively and with open or percutaneous surgical fixation. This case report illustrates the use of the Curvafix, a novel intramedullary implant used to treat a patient with a pelvic fragility fracture.
Keywords: Fragility fractures, Pelvic insufficiency fractures, Curvafix, Intramedullary fixation
Introduction
Fragility fractures of the pelvis (FFP) are an increasingly common encounter in today's healthcare system. These injuries are fractures that occur in fragile bone secondary to low energy, or even physiologic forces [5]. Fragile bone is conceptualized as significantly diminished bone density as compared to that of a young adult, due to a variety of causes including osteoporosis, radiation, vitamin D deficiency, chronic steroid use, etc. [3], [5]. In this setting, the bone is weaker than surrounding ligaments and is thus susceptible to fracture with low energy mechanisms, most commonly being ground level falls. The incidence is 90/100,000 and is increasing with the increased median age of the population [1], [5]. Fragility fractures may occur in the vertebrae, distal radius, proximal humerus, proximal femur, pubic rami, and pelvic ring.
While all fragility fractures carry associated complications, FFP carry a significant one year mortality risk of 16.7–19 % from different sources, rising to 22 %–27 % with increasing age or residence in a nursing home [6]. Reduction in mortality rate is centralized upon early mobilization, decreasing the multifold complications associated with prolonged bed rest in the elderly population [4]. Many of these pelvic fractures are treated conservatively with nonoperative management, pain control, and weight bearing as tolerated. Other treatment options include open or percutaneous operative fixation. Studies have demonstrated that operative management results in longer initial hospital stays, yet improved one year mortality rates of 6.7 %, in contrast to 13.5 % with conservative treatment [4]. Additionally, outcomes of operative fixation have shown improved autonomy, functional ambulation, and ability to reside independently [1], [4]. However, operative fixation does come with risk of longer hospital stays with associated urinary tract infections and pneumonia. Open techniques have increased complication rates compared to percutaneous procedures [2].
Overall, the goals of treatment for fragility fractures of the pelvis include early mobilization with an emphasis on less invasive procedures [2]. Curvafix is a novel intramedullary device that can be redirected along the irregular bony curvature of the pelvis. This percutaneous device allows for timely, minimally invasive surgical stabilization of pelvic fractures, allowing for immediate weight bearing and decreased pain in elderly patients. Curvafix may be integral to the future treatment of FFP. The following case is an example of the utility and benefit of this in practice.
Patient
The patient is a 72 year old female who sustained a ground level fall. She was seen at an outlying hospital and had lumbar spine radiographs which were read as negative. Of note, her baseline level of function was independent with all activities of daily living without the use of walking aids, residing at home alone. The patient continued to have significant pain and was unable to ambulate or get out of bed. She presented to the hospital 6 days following her initial fall and was found to have a sacral insufficiency fracture as shown in Fig. 1. A CT scan was also obtained with images shown in Fig. 2. These demonstrate a zone 1 sacral fracture on the right, a zone 2 sacral fracture on the left and a nondisplaced fracture near the left pubic symphysis. This falls into the classification by Rommens as an FFP4c [3] with bilateral posterior instabilities with anterior disruption. This patient was unable to ambulate in the emergency department with the help of a physical therapist and had failed a period of 6 days of nonoperative treatment. I then had a discussion with the patient regarding surgical fixation using the Curvafix implant. After discussing the risks, benefits and early clinical results using this device, the patient agreed to proceed with the surgical plan.
Fig. 1.

AP pelvis at time of injury demonstrating bilateral sacral fractures and nondisplaced left parasymphyseal ramus fractures.
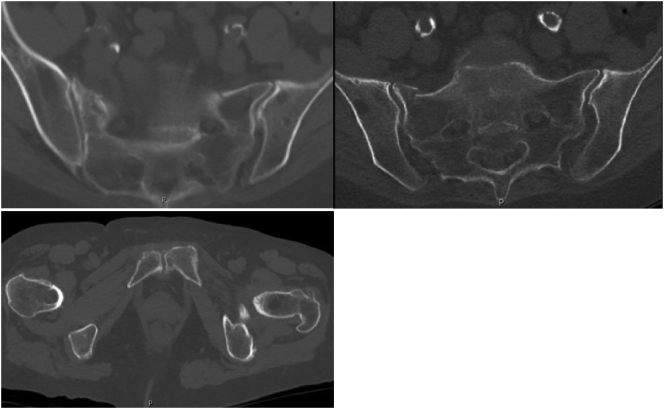
Fig. 2.
Computed tomography at time of injury demonstrating left anterior ring parasymphyseal pubic ramus fracture and bilateral sacral insufficiency fractures. Right zone 1 sacral fracture, left zone 2 sacral fractures.
The patient received her surgical fixation on post injury day 8. The treatment was placement of an S1 trans sacral, trans iliac Curvafix intramedullary device, as shown by intraoperative fluoroscopic images (Fig. 3). The procedure was uneventful. Postoperative CT scan images are shown (Fig. 4). The patient was able to ambulate with a walker on postoperative day 1. The remainder of her hospital stay was uneventful and she was discharged on postoperative day 7. She required discharge to an extended care facility (ECF), where she spent 1 week recuperating. She was able to ambulate with a walker for the duration of her stay in the ECF.
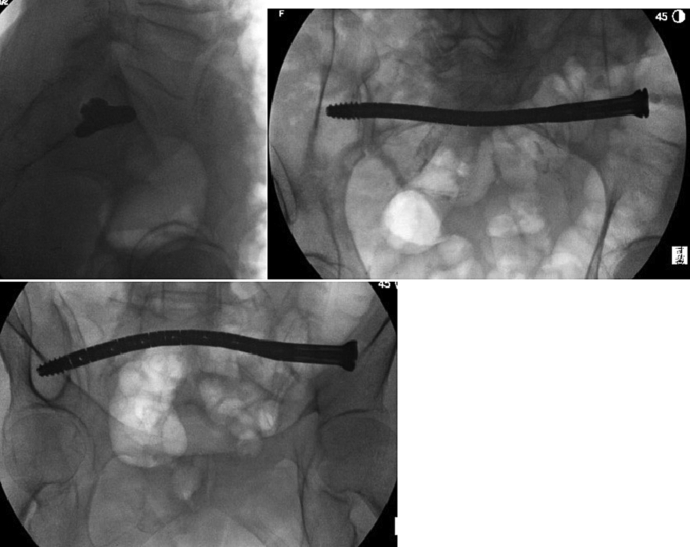
Fig. 3.
Intraoperative fluoroscopic images depicting S1 transiliac, transsacral Curvafix intramedullary device.
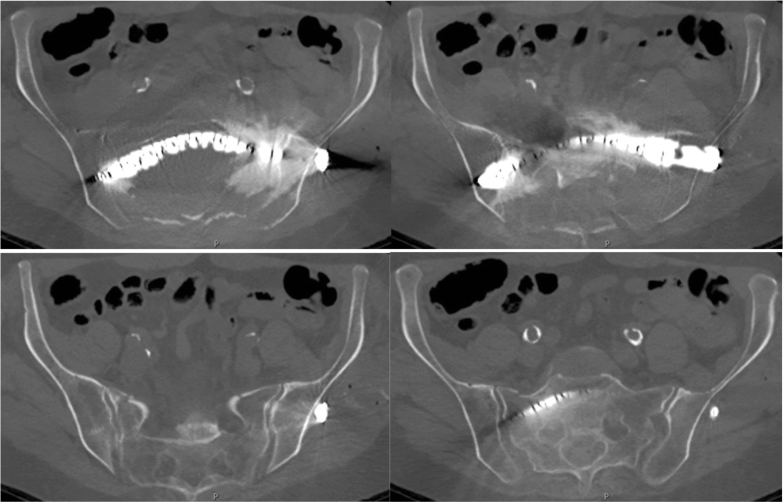
Fig. 4.
Postoperative computed tomography imaging demonstrating intramedullary S1 Curvafix crossing the sacrum and bilateral sacroiliac joints.
The first postoperative visit was at 2 weeks. The patient rated her pain a 3 on a scale of 0–10 and localized it to the surgical site. She was able to walk without an assistive device, but felt unsteady and chose to use a walker for ambulation. Upon return home from ECF at 3 weeks postoperatively, she was told by physical therapy that she no longer required the use of a walker. The patient was able to ambulate without walking aids from that time on. Her next visit was at postoperative week 6, at which she reported a small amount of pain at the surgical site. She was walking without any assistive devices. She was seen at 3 months postoperatively and feels like she is back to her normal life. At 6 months postoperatively, the patient was ambulating well with occasional surgical site discomfort. She felt that she was at 98 % of her baseline function. Post operative films from week 2, week 6, 3 months, and 6 months showed no change in the position of the implant (Fig. 5).
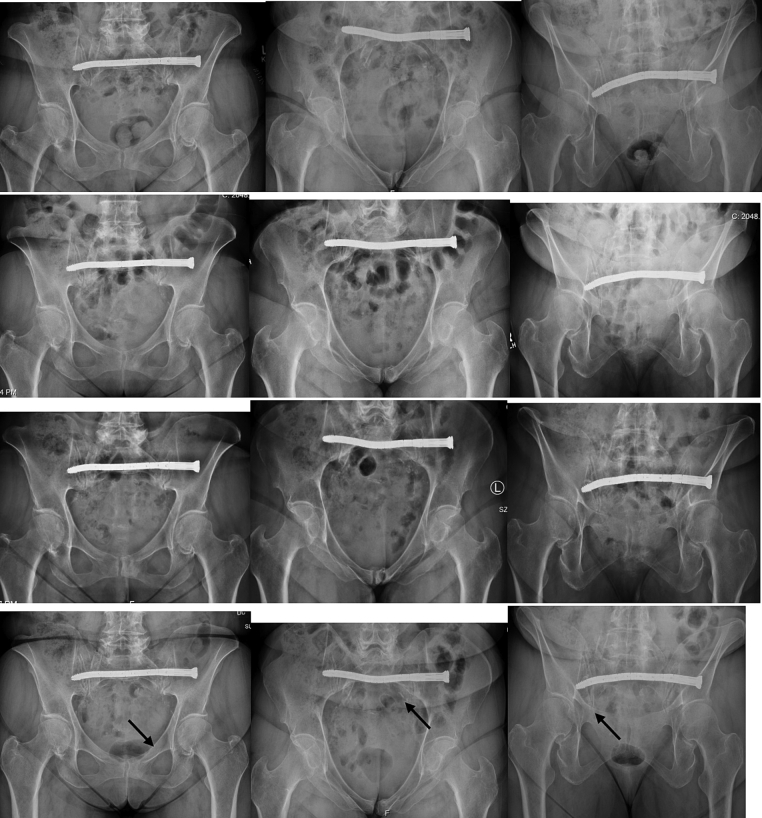
Fig. 5.
Postoperative radiographs at postoperative week 2 (first row), postoperative week 6 (second row), postoperative month 3 (third row), and postoperative month 6 (fourth row). Arrows in fourth row demonstrating interval fracture healing with stable implant positioning.
The surgical options for this patient were traditional straight screws or the Curvafix intramedullary implant. The Curvafix implant was chosen in this situation. It is advantageous because it is easier to implant in certain situations, including anterior ring corridors, dysmorphic S1 corridors, as well as the presence of other hardware obstructing the trajectory of a straight screw. The pelvis is made up of several curved bones and the posterior bony architecture at times makes placement of traditional implants difficult and occasionally impossible. This device can fill the intramedullary canal and conform to the natural curves of the bone. The method of implantation allows the user to maneuver the guide pin around neural foramen and create a safe path, ensuring stability of the implant in the microarchitecture of the bone. Once the implant has a curved path and is locked, it is nearly impossible to back out. The nonlinear structure also prevents rotation around the device, which traditional straight screws are unable to accomplish without multiple screws. More independent biomechanical studies need to be done to further characterize the stability provided by one device and to show what multiplanar curves with multiple devices does to pelvic stability.
The intramedullary corridors for traditional implants have been established [7] and these are important for the Curvafix intramedullary device. This implant is ideal for the curved portions of the bone and adds to the current corridors that we currently use. This device potentially allows us to connect these corridors, allowing longer implants and increased stability. The ability to cross multiple columns of bone with a nonlinear locked implant may allow us the ability to mobilize these patients earlier.
In conclusion, the Curvafix implant is a device that allows fixation and early mobilization of pelvic fragility fracture patients. More experience is needed to learn what corridors are available for this device and to further define its limitations.
References
- 1.Jäckle K., Meier M., Seitz M., Höller S., Spering C., Acharya M., Lehmann W. A retrospective study about functional outcome and quality of life after surgical fixation of insufficiency pelvic ring injuries. BMC Musculoskelet. Disord. 2021;22(1) doi: 10.1186/s12891-021-04925-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rommens P., Hofmann A., Kraemer S., Kisilak M., Boudissa M., Wagner D. Operative treatment of fragility fractures of the pelvis: a critical analysis of 140 patients. Eur. J. Trauma Emerg. Surg. 2021;48(4):2881–2896. doi: 10.1007/s00068-021-01799-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rommens P., Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury. 2013;44(12):1733–1744. doi: 10.1016/j.injury.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 4.Rommens P., Hopf J., Arand C., Handrich K., Boudissa M., Wagner D. Prospective assessment of key factors influencing treatment strategy and outcome of fragility fractures of the pelvis (FFP) Eur. J. Trauma Emerg. Surg. 2022;48(4):3243–3256. doi: 10.1007/s00068-022-01887-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soles G., Ferguson T. Fragility fractures of the pelvis. Curr. Rev. Musculoskelet. Med. 2012;5(3):222–228. doi: 10.1007/s12178-012-9128-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eckardt H., Egger A., Hasler R., Zech C., Vach W., Suhm N., Morgenstern M., Saxer F. Good functional outcome in patients suffering fragility fractures of the pelvis treated with percutaneous screw stabilisation: assessment of complications and factors influencing failure. Injury. 2017;48(12):2717–2723. doi: 10.1016/j.injury.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Bishop J.A., Routt M.L., Jr. Osseous fixation pathways in pelvic and acetabular fracture surgery: osteology, radiology, and clinical applications. J. Trauma Acute Care Surg. 2012 Jun;72(6):1502–1509. doi: 10.1097/TA.0b013e318246efe5. PMID: 22695413. [DOI] [PubMed] [Google Scholar]