Abstract
Objective:
Personality is associated with weight change and the development of obesity across adulthood. The present study examines whether significant weight change, including weight loss and weight gain, is related to personality change in a large longitudinal sample of middle-aged and older adults.
Design:
Participants were adults aged 50 to 92 years (N> 5,000; 59% women, Mean age= 65.51, SD= 8.20) drawn from the Health and Retirement Study (HRS). Personality, demographic, health, and staff assessed weight and height were obtained at baseline and eight years later.
Main Outcome Measures:
Personality traits.
Results:
Both weight loss and weight gain greater than 10% of baseline weight were related to a steeper decline in extraversion, openness and conscientiousness. Weight loss was further associated with the maintenance of neuroticism and to a steeper decline in agreeableness. This overall pattern of personality change was also associated with both unhealthy and healthy weight change. The associations were not moderated by BMI and generally remained significant after accounting for disease burden.
Conclusion:
The present study provides new evidence that both weight loss and weight gain are related to change in personality.
Keywords: Personality, weight, longitudinal, health
Personality traits, as defined by the Five Factor Model (McCrae & John, 1992), are implicated in a range of health-related outcomes across adulthood. In particular, there is robust evidence for the relationship between personality and weight (Jokela et al., 2013; Sutin & Terracciano, 2016a, 2016b; Vainik et al., 2019). Cross-sectional and longitudinal studies found consistently that conscientiousness (the tendency to be organized and self-disciplined) is related to lower adiposity and to lower risk of obesity both concurrently and over time (Chapman, Fiscella, Duberstein, Kawachi, & Coletta, 2009; Jokela et al., 2013; Mõttus, McNeill, Jia, Craig, Starr, & Deary,2013; Sutin, Ferrucci, Zonderman, & Terracciano, 2011; Sutin & Terracciano, 2016a, 2016b; Vainik et al., 2019). Neuroticism (the tendency to experience negative emotions and distress) is associated with higher body mass index (BMI) and higher risk of obesity, but not in all studies (Armon, Melamed, Shirom, Shapira, & Berliner, 2013; Magee & Heaven, 2011; Sutin & Terracciano, 2016a; Vainik et al., 2019). Less consistent evidence exists for the relation between extraversion (the propensity to experience positive emotions and to be sociable), openness (the tendency to be creative and curious) and agreeableness (the tendency to be cooperative and empathetic) and body weight (see Jokela et al., 2013). Most research has focused on personality as a predictor of weight and weight change; comparatively less is known about the extent to which personality change trajectories differ across individuals who do or do not experience substantial weight change over time.
Personality development tends to follow a normative pattern characterized by declines in neuroticism, extraversion, and openness, and increases in conscientiousness and agreeableness during most of adulthood, but not necessarily among older individuals (Lucas & Donnellan, 2011; McCrae et al., 2005; Terracciano, McCrae, & Costa, 2006). Furthermore, there are individual deviations from these trajectories that deserve attention. For example, changes in personality traits such as a steeper decrease in conscientiousness or increase in neuroticism over time may be maladaptive because they are related to higher risk of substance use, lower self-rated health and well-being and higher risk of depression (Choi & Roberts, 2014; Human et al., 2013; Turiano, Whiteman, Hampson, Roberts, & Mroczek, 2012). Therefore, the test of the link between weight change and personality change could contribute to a better understanding of the factors related to maladaptive trait change.
The associations between personality and health are likely to be bidirectional. Indeed, change in health may also be associated with personality change, as in the case of biological dysfunction (Stephan, Sutin, Luchetti, & Terracciano, 2016), onset and development of disease (Jokela, Hakulinen, Singh-Manoux, & Kivimäki, 2014), sensory impairment (e.g., hearing loss) (Stephan, Sutin, Bosselut, & Terracciano, 2017), major depression (Costa, Bagby, Herbst, & McCrae, 2005), or Alzheimer’s disease (Islam et al., 2019). These studies suggest that poor health is related to decreases in emotional stability, extraversion, openness, agreeableness, and conscientiousness (e.g., Jokela et al., 2014; Stephan et al., 2017). This pattern may extend to changes in body weight, and some studies do suggest that weight change is associated with personality. Lathi et al. (2013), for example, found that weight change in childhood and adulthood is associated with personality in late life. Specifically, more weight gain between early adolescence and late adulthood is related to higher extraversion in old age, whereas less weight gain was associated with higher conscientiousness. In addition, less weight gain from early adolescence to adulthood was associated with higher agreeableness in old age. However, this study only focused on weight change and personality in adulthood; it did not address changes in personality across this time. In a pooled analysis of six samples of middle aged and older adults, Jokela et al. (2013) found no overall association between obesity status (e.g. obese vs. not obese) and change in conscientiousness. This study, however, only addressed the relation with change in conscientiousness, not all five traits and not changes in weight. Finally, Sutin et al. (2013) found support for an association between weight change and personality change in two samples. Over a 10-year period, middle aged adults who gained at least 10% in body weight by follow-up were more impulsive (a component of neuroticism) and more deliberative (a component of conscientiousness). At the domain level, weight gain was also associated with small increases in conscientiousness over time, but this association did not replicate across both samples. There was little evidence for an association between weight loss and personality change.
It is likely that weight loss may be associated with changes in personality. Indeed, weight loss is associated with a range of health-related, functional, and cognitive factors that contribute to personality change across adulthood. For example, weight loss is an indicator of frailty (Fried et al., 2001), which has been related to detrimental personality changes, characterized by increased neuroticism and decreased extraversion, openness, agreeableness and conscientiousness over time (Stephan, Sutin, Canada, & Terracciano, 2017). In addition, weight loss may be accompanied by loss of muscle mass and reduced strength which has been found to manifest into higher neuroticism, lower extraversion, agreeableness and conscientiousness (Mueller et al., 2016; Mueller, Wagner, Smith, Voelkle, & Gerstorf 2018). Furthermore, weight loss from midlife to late life is related to cognitive impairment (Alhurani et al., 2016) and is predictive of increased depressive symptoms (Jackson, Steptoe, Beeken, Kivimaki, & Wardle, 2014). In turn, both impaired cognition and depressive symptoms are predictive of an increase in neuroticism, and decrease in extraversion, openness, agreeableness and conscientiousness (Caselli et al., 2018; Donati et al., 2013; Hakulinen et al., 2015).
Based upon a large longitudinal sample of older adults, the present study examined the association between weight change and personality change. In line with Sutin et al. (2013), significant weight loss or gain were defined as a 10% loss or gain from baseline weight. Consistent with existing evidence on the health and cognitive implications of significant weight loss in old age (Alhurani et al., 2016; Fried et al., 2001), it was hypothesized that it would be related to increased neuroticism, and decreased extraversion, openness, agreeableness and conscientiousness. We further tested whether baseline BMI moderated the association between weight change and personality change.
Method
Participants
Participants were drawn from the Health and Retirement Study (HRS), a nationally representative longitudinal study of adults aged 50 years and older conducted by the University of Michigan and funded by the National Institute on Aging (NIAU01AG009740). Starting in 2006, the HRS implemented an enhanced face to face interview including a personality questionnaire and physical measures among a random half of the participants; the other half was assessed in 2008. The two waves were combined as the baseline measure, resulting in a sample of 10,621 participants with complete personality, weight, and demographic data. Follow-up personality and weight data were obtained from the 2014 (for the 2006 sample) and the 2016 (for the 2008 sample) waves. The final sample was composed of 5,053 individuals aged from 50 to 92 years (59% women, Mean age= 65.51, SD= 8.20) who had both personality and staff-assessed weight at baseline and follow-up. Attrition analysis revealed that participants with complete follow-up data were younger (d= .62), more educated (d= .34), more likely to be women and white than those without complete data. In addition, they weighted more (d= .13), and were more extraverted (d= .09), more agreeable (d= .04), more open (d= .16), more conscientious (d= .24), and had lower neuroticism (d= .08).
Measures
Personality.
Personality traits were assessed using the Midlife Development Inventory (MIDI; Zimprich, Allemand, & Lachman, 2012). Participants were asked to indicate how well 26 adjectives assessing neuroticism (4 adjectives, e.g. worrying), extraversion (5 adjectives, e.g. active), openness (7 adjectives, e.g. curious), agreeableness (5 adjectives, e.g. friendly), and conscientiousness (5 adjectives, e.g. hardworking) described themselves on a scale ranging from 1 (not at all) to 4 (a lot). The mean was computed across items for each trait (Cronbach α= .66 to .80).
Weight change.
Respondents were asked to remove their shoes, any bulky clothing and heavy objects from their pockets, and to step on a scale to measure their weight. Weight was recorded to the nearest half pound. Weight loss and weight gain were defined respectively as a 10% decrease and a 10% increase in weight between baseline and follow-up. Relatively stable weight was defined as weight loss and gain lower than 10% between baseline and follow-up.
Covariates.
Demographic covariates were age (in years), sex (coded as 1 for men and 0 for women), education (in years), and race (coded as 1 for white and 0 for other). BMI and disease burden were controlled for in an additional analysis. BMI was computed as kg/m2 from objective measurement of weight and height. Disease burden was the sum of seven diagnosed disease and conditions: high blood pressure, diabetes, cancer, lung disease, heart condition, stroke, and arthritis.
Data analysis
Regression analyses were conducted to test for the association between weight change and personality changes. Two dummy variables were created: the first contrasted weight loss ≥ 10% (coded as 1) to both relatively stable weight (<10% weight loss and < 10% weight gain) and weight gain ≥ 10% (coded as 0), and the second contrasted weight gain ≥ 10% (coded as 1) to relatively stable weight and weight loss ≥ 10% (coded as 0). Each personality trait at follow-up was predicted from the two dummy variables. The covariates age, sex, education, race and baseline personality were all included simultaneously in the analysis with the two dummy variables. BMI and disease burden were further included as additional covariates. Additional analysis tested whether BMI or age moderates the link between weight change and personality change. Both BMI and age were mean-centered before computing the interaction term with the two dummy variables. Supplemental regression analysis also tested whether personality at baseline and personality change were associated with significant weight loss and/or weight gain compared to relatively stable weight over time, controlling for demographic factors.
Additional analysis were conducted using an alternative classification of weight change. Specifically, individuals with follow-up BMI equal or superior to 25, who presented a 10% weight gain, and individuals with BMI lower than 25 who experienced a 10% weight loss were categorized as unhealthy weight change. Individuals with follow-up BMI equal or superior to 25 who experienced a 10% weight loss, and individuals with BMI lower than 25 who experienced a 10% weight gain were categorized as healthy weight change. Two dummy variables were created: unhealthy weight change vs other (stable and healthy weight change) and healthy vs. other (stable and unhealthy). Regression analysis were conducted to test for these associations. Follow-up personality traits were predicted by the two dummy variables, controlling for demographic factors and baseline personality.
Results
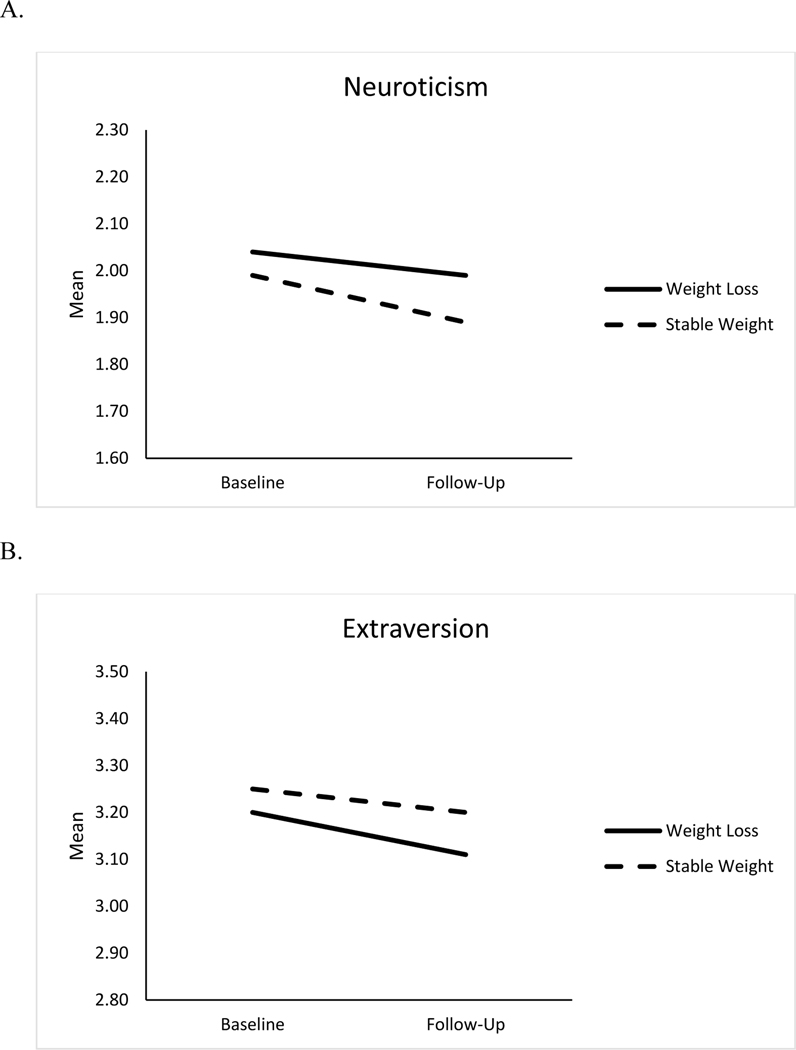
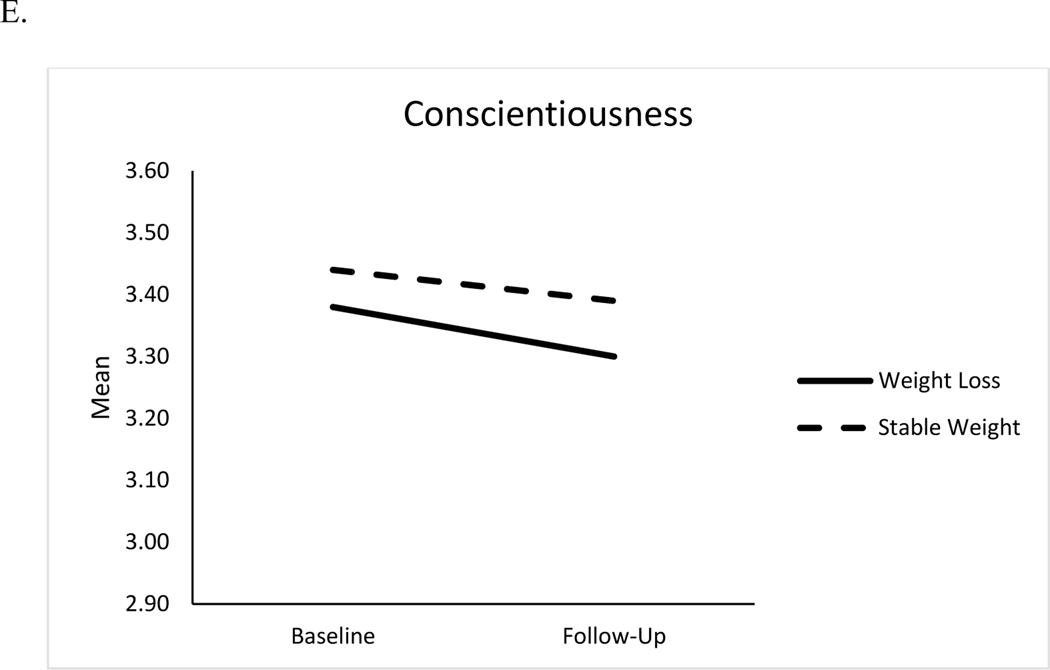
Weight loss ≥10% was related to significant changes in neuroticism, extraversion, openness, agreeableness and conscientiousness, controlling for demographic factors (Table 2). Given that all five traits decline over time in the present study, the pattern of relationship observed suggests that weight loss is related to the relative maintenance of neuroticism, and a steeper decline in extraversion, openness, agreeableness and conscientiousness. Figure 1 presents the difference in personality change between individuals with significant weight loss and those with relatively stable weight. The difference in personality change between individuals with at least 10% weight loss and those with relatively stable weight was d= .10 for neuroticism, d= .11 for extraversion, d= .07 for openness, d= .07 for agreeableness and d= .07 for conscientiousness. These associations remained significant when baseline BMI and disease burden were included in the model, except for openness (Table 2). There was no evidence that BMI or age moderated the relation between weight loss and personality change.
Table 2.
Summary of Analysis on the Association between Weight Change and Personality Change
| Neuroticism | Extraversion | Openness | Agreeableness | Conscientiousness | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 a | Model 1 | Model 2 a | Model 1 | Model 2 a | Model 1 | Model 2 a | Model 1 | Model 2 a | |
|
| ||||||||||
| Sex | −.01 (−.034;.010) | −.01 (−.034;.010) | −.04*** (−.060;−.021) | −.04*** (−.060;−.021) | −.03** (−.052;−.013) | −.03** (−.051;−.012) | −.09*** (−.112;−.068) | −.09*** (−.110;−.066) | −.06*** (−.082;−.040) | −.06*** (−.082;−.040) |
| Age | .01 (−.008;.038) | −.005 (−.029;.019) | − .07*** (−.095;−.054) | − .07*** (−.089;−.045) | − .07*** (−.089;−.049) | − .07*** (−.088;−.045) | − .06*** (−.077;−.033) | − .05*** (−.075;−.029) | −.10*** (−.120;−.076) | −.09*** (−.111;−.065) |
| Education | −.03* (−.051;−.007) | −.03* (−.050;−.005) | .04*** (.023; .063) | .04*** (.019; .059) | .10*** (.077; .118) | .09*** (.074; .114) | .07*** (.045; .087) | .06*** (.043; .086) | .10*** (.084;.126) | .10*** (.078;.121) |
| Race | .05*** (.030; .074) | .05*** (.030; .074) | −.00 (−.025; .015) | −.00 (−.027; .012) | −.01 (−.034; .005) | −.02 (−.036; .003) | .00 (−.016; .027) | .00 (−.018; .024) | .01 (−.007; .035) | .01 (−.012; .030) |
| Baseline Personality | .61*** (.589;.633) | .61*** (.584;.629) | .69*** (.671;.711) | .69*** (.669;.709) | .67*** (.654;.694) | .67*** (.655;.695) | .62*** (.595;.638) | .62*** (.595;.638) | .61*** (.590;.632) | .61*** (.584;.626) |
| Weight lossb | .05*** (.024;.068) | .05*** (.024;.069) | −.04*** (−.057;−.016) | −.03** (−.051;−.010) | −.02* (−.042;−.003) | −.02 (−.040;.001) | −.03** (−.054;−.011) | −.03** (−.052;−.009) | −.03** (−.055;−.012) | −.03* (−.049;−.005) |
| Weight Gainc | .01 (−.012;.031) | .005 (−.017;.027) | −.04*** (−.060;−.020) | −.04*** (−.058;−.018) | −.03** (−.048;−.009) | −.03** (−.047;−.008) | −.01 (−.030;.013) | −.00 (−.027;.016) | −.03** (−.051;−.008) | −.03* (−.048;−.005) |
| BMI | −.04*** (−.062; −.016) | −.00 (−.028; .013) | −.00 (−.025;.016) | −.00 (−.025;.020) | −.02 (−.037;.007) | |||||
| Disease burden | .05*** (.026;.073) | −.03** (−.052;−.009) | −.01 (−.033;.010) | −.01 (−.036;.010) | −.05*** (−.070;−.024) | |||||
| Adjusted R2 | .38 | .39 | .49 | .49 | .51 | .51 | .42 | .42 | .43 | .43 |
| F | 450.90*** | 352.78*** | 704.72*** | 546.02*** | 760.25*** | 588.37*** | 535.46*** | 412.41*** | 550.84*** | 429.26*** |
Note: N= 5,053 ; Coefficients are standardized regression coefficients ; 95% confidence intervals are under parentheses.
p < .05
p < .01
p <.001
N= 5,024
= coded as 1 for weight loss ≥ 10% and 0 for other
= coded as 1 for weight gain ≥ 10% and 0 for other
Figure 1.
Changes in Neuroticism (Panel A), Extraversion (Panel B), Openness to Experience (Panel C), Agreeableness (Panel D), and Conscientiousness (Panel E) for Weight Loss and Stable Weight Groups
Note. Means are adjusted for age, sex, education and race.
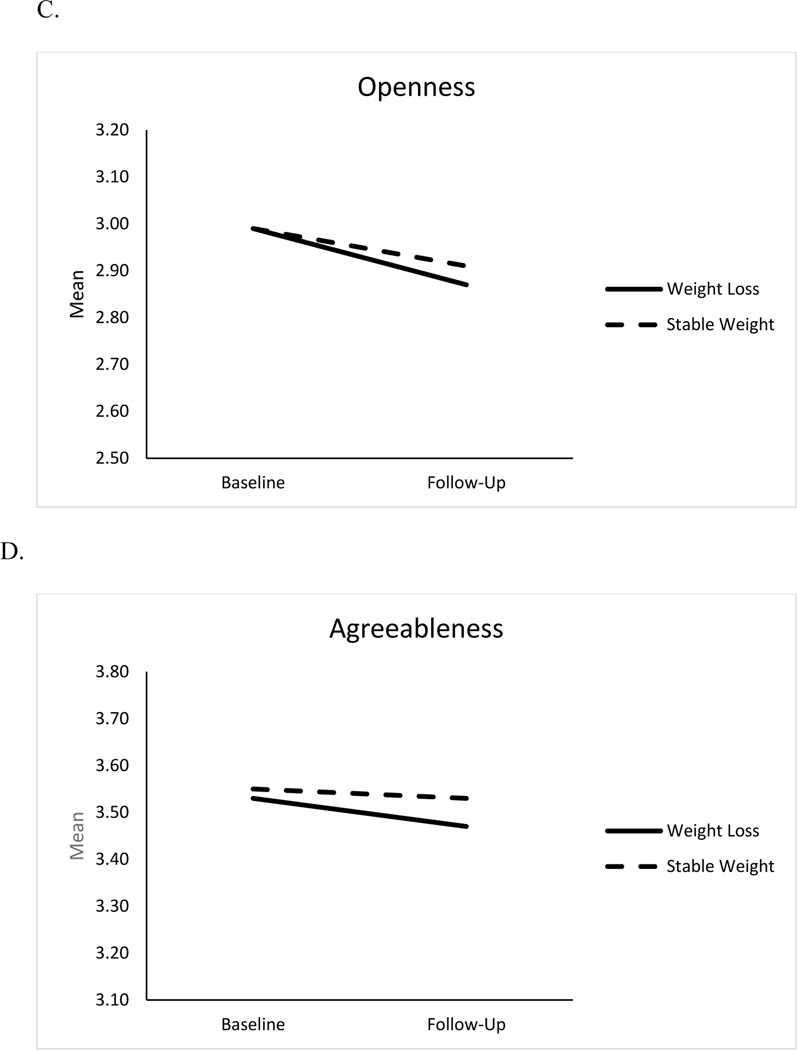
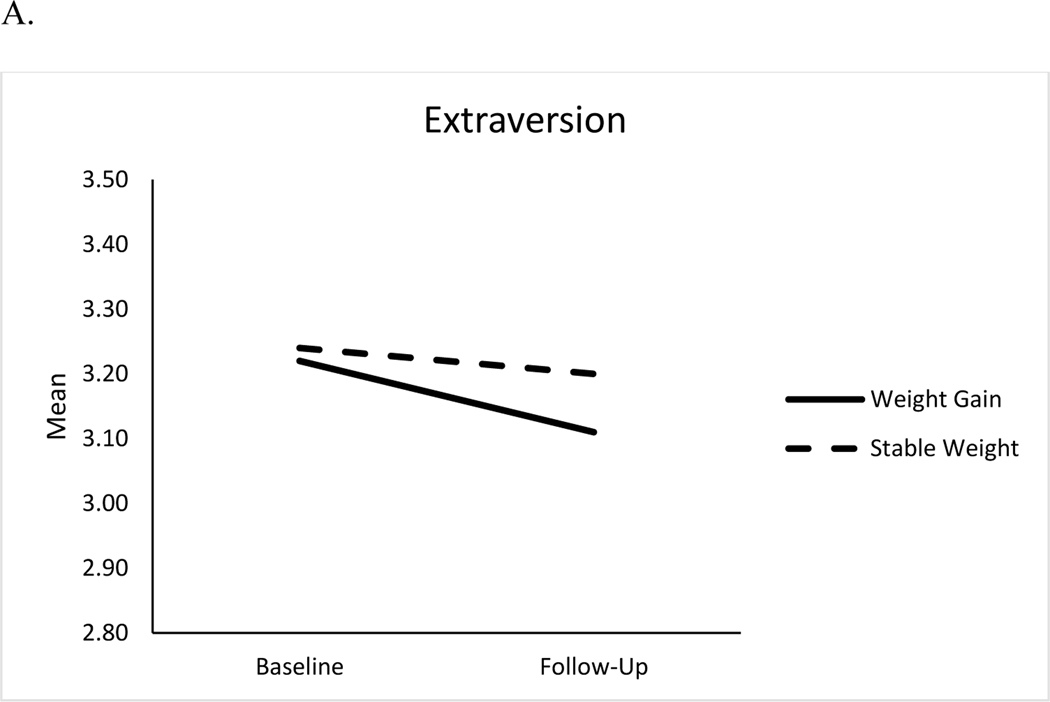
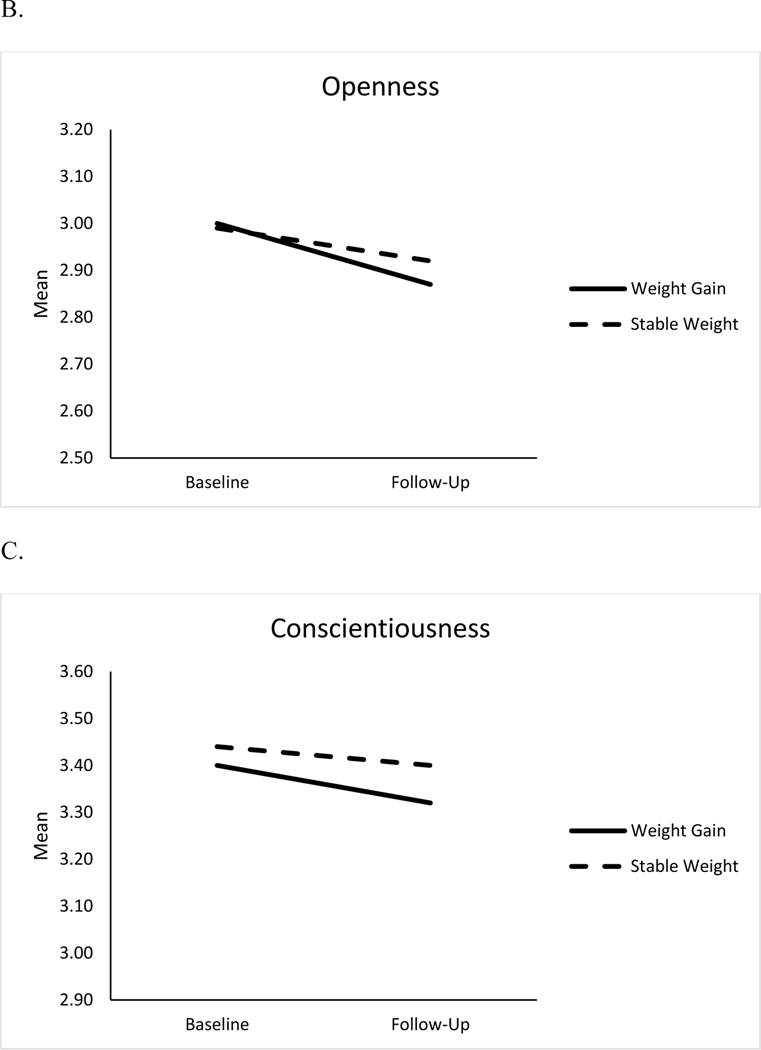
Weight gain ≥10% was related to a greater decline in extraversion, openness and conscientiousness but was unrelated to change in agreeableness and neuroticism (Table 2). Figure 2 presents personality change among individuals with weight gain and those with relatively stable weight. The difference between personality change of individuals who gained weight and those with stable weight was d= .16 for extraversion, d= .15 for openness, and d= .10 for conscientiousness. These associations remained unchanged when BMI and disease burden were included as additional covariates (see Table 2). BMI and age did not moderate the association between weight gain and personality change.
Figure 2.
Changes in Extraversion (Panel A), Openness to Experience (Panel B), and Conscientiousness (Panel C) for Weight Gain and Stable Weight Groups
Note. Means are adjusted for age, sex, education, and race
Supplementary analysis addressed whether personality was related to the likelihood of experiencing significant weight loss and weight gain compared to keeping a relatively stable weight. Baseline higher extraversion and conscientiousness were related to a lower probability of weight loss, whereas higher neuroticism was associated with a higher probability of experiencing both significant weight loss and weight gain (see supplementary material). Personality change was also associated with weight change: An increase in neuroticism over time was related to a higher likelihood of weight loss and an increase in extraversion, openness, agreeableness and conscientiousness was associated with a reduced probability of losing weight over time. An increase in extraversion, openness and conscientiousness were also related to lower risk of weight gain (see supplementary material).
Finally, both unhealthy and healthy weight change were related to increased neuroticism (βunhealthy= .03, p<.01 and βhealthy= .02, p<.05) and to decrease in extraversion (βunhealthy= −.05, p<.001 and βhealthy= −.02, p<.05) and conscientiousness (βunhealthy= −.03, p<.01 and βhealthy= −.03, p<.01). Unhealthy (β= −.03, p<.01), but not healthy (β= −.01, p= .18), weight change was associated with lower openness and healthy (β= −.02, p<.05), but not unhealthy (β= −.02, p=.05), weight change was related to lower agreeableness.
Discussion
The present study examined whether weight change is related to personality change over eight years among middle-aged and older adults. Consistent with the hypothesis, significant weight loss, defined as at least 10% of baseline weight, was related to maintaining neuroticism and to steeper decline for extraversion, openness, agreeableness and conscientiousness. In addition, significant weight gain was associated with decreases in conscientiousness, extraversion, and openness. These associations were independent of individuals’ baseline BMI. Taken as a whole, the present study provides evidence for an association between weight change and personality change across middle and older age.
Individuals who experience significant weight change over time may experience biological, health-related, and cognitive alterations (Alrhumani et al., 2016; Fried et al., 2001; Jackson et al., 2014) that may manifest into lower energy and positive emotions, lower novelty seeking, reduced involvement in social interactions, lower self-discipline and maintained propensity to experience distress (Caselli et al., 2018; Hakulinen et al., 2015; Mueller et al., 2018). In particular, weight loss in old age has a range of health, functional and cognitive implications that may lead to personality change. For example, weight loss is a component of frailty (Fried et al., 2001), which has been related to detrimental personality change (Stephan et al., 2017). In addition, weight loss is associated with functional limitations (Ritchie et al., 2008), depressed mood (Jackson et al., 2014), and cognitive impairment (Alrhumani et al., 2016). In turn, higher limitations in activities of daily living, depressive symptoms, and impaired cognition have been associated with the maintenance of neuroticism and decline in extraversion, openness, agreeableness and conscientiousness over time (Caselli et al., 2018; Donati et al., 2013; Hakulinen et al., 2015; Mueller et al., 2016, 2018). It is also likely that weight loss may reflect disease-related physiological processes that may lead to personality changes. In the same vein, weight gain in adulthood is a risk factor for poor outcomes, including biological dysregulation (Alley et al., 2010), chronic disease (Zheng et al., 2017), and depressive symptoms (Konttinen et al., 2014), resulting in impairment of resources needed to remain enthusiastic and energetic (e.g. extraverted), exploratory and curious (e.g. open to experiences), and self-disciplined and organized (e.g. conscientious) (Hakulinen et al., 2015; Jokela et al., 2014; Stephan et al., 2016). Individuals who gain weight may be more likely to feel stigmatized (Tomiyama et al., 2018) that may reduce social interactions, isolation, and in less novelty seeking behaviors, reflected in lower extraversion and openness. Finally, individuals with significant weight gain or loss may be less likely to be physically active, which is associated with a reduced propensity to experience positive emotions, to be open to new experiences, to be prosocial, and to be self-disciplined (Stephan, Sutin, & Terracciano, 2014).
The present study contributes to existing knowledge in several ways. First, this study adds to knowledge on the factors related to personality change across adulthood. Indeed, a growing body of research has identified a range of behavioral, health-related, cognitive, and physical factors associated with changes in personality traits (Jokela et al., 2014; Stephan, Sutin, Luchetti, Bosselut, & Terracciano, 2018; Stephan et al., 2014; Mueller et al., 2016; 2018; Terracciano, Stephan, Luchetti, Albanese, & Sutin, 2017) and this study is the first to report a significant link with weight loss.
In addition, the present study contributes to knowledge on the implications of weight change in middle and older age by adding personality change to the correlates of weight loss and gain. Of note, weight change was related to personality change independent of the direction of the change, and independent of the extent to which these changes were healthy (i.e., into the range of normal BMI) or unhealthy (i.e., out of the range of normal BMI). Indeed, both loss and gain are both indicators of poor health, with similar deleterious outcomes, that may manifest into similar personality change. Moreover, personality change may explain in part the association between weight change and a range of health and cognitive outcomes. For example, both weight loss and weight gain are predictive of mortality (Park et al., 2018), and higher neuroticism and lower conscientiousness, extraversion, openness, and agreeableness are related to higher mortality risk (Graham et al., 2017). Therefore, it is likely that individuals who experience significant weight changes may be exposed to higher mortality risk in part because they decrease in conscientiousness, extraversion, openness, agreeableness, and emotional stability over time. It is also likely that the association between weight change and mortality risk could be explained by behavioral factors associated with personality traits, such as eating behavior, exercise, and risky behaviors such as smoking or alcohol use. In addition, weight loss is predictive of higher risk of dementia (Singh-Manoux et al., 2018), and higher neuroticism and lower conscientiousness are consistently related to the risk of Alzheimer disease and dementia (Terracciano et al., 2014, 2017). Therefore, weight loss may be related to higher dementia in part through its relationships with the maintenance of neuroticism and decline in conscientiousness. Overall, weight change in older adults has a different pattern of health correlates as compared to younger adults (Murphy et al., 2014; Newman et al., 2001) and such differential patterns may occur for personality traits. As such, weight changes may be associated with different patterns of personality development in younger adulthood. This explanation could account for the difference between our findings and those of Sutin et al. (2013) on the association between weight loss and personality change. The sample of the present study is older (and larger) than the samples in Sutin et al. (2013). Therefore, weight loss may be more salient for personality change in older groups as compared to midlife. Whether such weight and personality change associations are moderated by age should be addressed in future longitudinal studies with a broader age range. The difference in personality measures across the present study and Sutin et al. study may also account for some of the discrepant findings.
The present study has several strengths including the large longitudinal sample of older adults and the use of objective measures of weight. There are also several limitations. The generalizability of the findings is limited by the positive selection of the sample. Specifically, participants in the longitudinal sample had healthier personality profiles and were healthier, younger, and better educated, which could bias the findings and raises the issue of replicability in other samples. The size of the associations, however, may be underestimated by this selection effect, given that individuals who drop out were less healthy and thus may have experienced steeper weight change. In addition, causal relations cannot be determined with an observational design. Although weight change was considered as a predictor of personality change, reciprocal relationships may exist. Indeed, supplementary analysis suggest that personality level and change may predict weight loss or gain over time. More research is needed to further explore these reciprocal relationships. In line with Sutin et al. (2013), future research may use detailed measure of personality to examine whether weight change is related to changes in specific facets. Finally, the present study did not include information about the reasons for weight change, such as whether the weight change was intentional and deliberate or the result of health issues. It is likely that the reasons that underlie weight change may be related to the direction of personality change. Future research should include an assessment of the causes of weight gain or loss to provide a more complete understanding of the associations between weight gain or loss and personality changes.
In sum, the present study provides evidence for an association between weight change and personality change in old age. Both weight loss and weight gain are related to detrimental personality changes. This study thus contributes to a better understanding of factors related to personality change in old age.
Supplementary Material
Table 1.
Characteristics of the Sample
| Total Sample | Weight Lossa | Stable Weightb | Weight Gainc | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Variables | M/% | SD | M/% | SD | M/% | SD | M/% | SD |
|
| ||||||||
| Age (Years) at baseline | 65.51 | 8.20 | 68.71 | 8.38 | 65.21 | 8.01 | 61.64 | 7.21 |
| Sex (% women) | 59% | - | 68% | - | 57% | - | 66% | - |
| Race (% White) | 88% | - | 88% | - | 88% | - | 88% | - |
| Education | 13.39 | 2.67 | 13.05 | 2.71 | 13.46 | 2.69 | 13.42 | 2.41 |
| Body Mass Indexd | 29.36 | 5.58 | 31.08 | 6.18 | 29.09 | 5.38 | 28.20 | 5.33 |
| Disease Burden | 1.69 | 1.20 | 2.06 | 1.22 | 1.61 | 1.17 | 1.62 | 1.21 |
| Baseline Neuroticism | 2.01 | 0.58 | 2.02 | 0.59 | 1.99 | 0.58 | 2.14 | 0.61 |
| Baseline Extraversion | 3.23 | 0.54 | 3.21 | 0.55 | 3.24 | 0.54 | 3.21 | 0.52 |
| Baseline Openness | 2.99 | 0.53 | 2.97 | 0.53 | 2.99 | 0.54 | 3.01 | 0.54 |
| Baseline Agreeableness | 3.55 | 0.46 | 3.56 | 0.46 | 3.55 | 0.45 | 3.55 | 0.46 |
| Baseline Conscientiousness | 3.43 | 0.44 | 3.38 | 0.47 | 3.44 | 0.43 | 3.41 | 0.44 |
| Follow-up Neuroticism | 1.92 | 0.58 | 1.99 | 0.60 | 1.89 | 0.58 | 2.00 | 0.57 |
| Follow-up Extraversion | 3.18 | 0.57 | 3.11 | 0.59 | 3.20 | 0.56 | 3.12 | 0.59 |
| Follow-up Openness | 2.90 | 0.57 | 2.84 | 0.55 | 2.92 | 0.57 | 2.89 | 0.57 |
| Follow-up Agreeableness | 3.52 | 0.49 | 3.48 | 0.52 | 3.52 | 0.48 | 3.53 | 0.48 |
| Follow-up Conscientiousness | 3.37 | 0.48 | 3.29 | 0.52 | 3.39 | 0.47 | 3.35 | 0.48 |
Note. Total Sample= 5,053
Weight loss ≥ 10%, N= 876;
Stable weight (< 10% weight loss and < 10% weight gain), N= 3,747
Weight gain ≥ 10%, N= 430
= Due to missing data, N= 5,024 for the total sample, N= 871 for the weight loss group, N= 3,725 for the stable weight group, and N= 428 for the weight gain group
Acknowledgment:
The present study is based upon the analysis of data collected in the Health and Retirement Study (HRS) is a nationally representative longitudinal study of Americans aged 50 years and older (Grant No. NIA U01AG009740) conducted by the University of Michigan. HRS Data are available at: http://hrsonline.isr.umich.edu/index.php
Funding :
No specific grant from any funding agency, commercial or not-for-profit sectors was received for the present research
Footnotes
Conflicts of Interest: None.
References
- Alhurani RE, Vassilaki M, Aakre JA, Mielke MM, Kremers WK, Machulda MM, … & Roberts RO (2016). Decline in weight and incident mild cognitive impairment: Mayo Clinic Study of Aging. JAMA Neurology, 73(4), 439–446. doi: 10.1001/jamaneurol.2015.4756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alley DE, Metter EJ, Griswold ME, Harris TB, Simonsick EM, Longo DL, & Ferrucci L. (2010). Changes in weight at the end of life: Characterizing weight loss by time to death in a cohort study of older men. American Journal of Epidemiology, 172(5), 558–565. doi: 10.1093/aje/kwq168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armon G, Melamed S, Shirom A, Shapira I, & Berliner S. (2013). Personality traits and body weight measures: Concurrent and across-time associations. European Journal of Personality, 27(4), 398–408. doi : 10.1002/per.1902 [DOI] [Google Scholar]
- Caselli RJ, Langlais BT, Dueck AC, Henslin BR, Johnson TA, Woodruff BK, … & Locke DE (2018). Personality changes during the transition from cognitive health to mild cognitive impairment. Journal of the American Geriatrics Society, 66(4), 671–678. doi: 10.1111/jgs.15182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman BP, Fiscella K, Duberstein P, Kawachi I, & Coletta M. (2009). Can the influence of childhood socioeconomic status on men’s and women’s adult body mass be explained by adult socioeconomic status or personality? Findings from a national sample. Health Psychology, 28(4), 419–427. doi: 10.1037/a0015212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow PI, & Roberts BW (2014). Examining the relationship between changes in personality and changes in depression. Journal of Research in Personality, 51, 38–46. doi : 10.1016/j.jrp.2014.04.007 [DOI] [Google Scholar]
- Costa PT Jr, Bagby RM, Herbst JH, & McCrae RR (2005). Personality self-reports are concurrently reliable and valid during acute depressive episodes. Journal of Affective Disorders, 89, 45–55. doi : 10.1016/j.jad.2005.06.010 [DOI] [PubMed] [Google Scholar]
- Donati A, Studer J, Petrillo S, Pocnet C, Popp J, Rossier J, & Von Gunten A. (2013). The evolution of personality in patients with mild cognitive impairment. Dementia and Geriatric Cognitive Disorders, 36(5–6), 329–339. doi: 10.1159/000353895. [DOI] [PubMed] [Google Scholar]
- Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, … & McBurnie MA (2001). Frailty in older adults: Evidence for a phenotype. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 56(3), M146–M157. [DOI] [PubMed] [Google Scholar]
- Graham EK, Rutsohn JP, Turiano NA, Bendayan R, Batterham PJ, Gerstorf D, … & Mroczek DK (2017). Personality predicts mortality risk: An integrative data analysis of 15 international longitudinal studies. Journal of Research in Personality, 70, 174–186. doi: 10.1016/j.jrp.2017.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakulinen C, Elovainio M, Pulkki-Råback L, Virtanen M, Kivimäki M, & Jokela M. (2015). Personality and depressive symptoms: Individual participant meta-analysis of 10 cohort studies. Depression and Anxiety, 32(7), 461–470. doi: 10.1002/da.22376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Human LJ, Biesanz JC, Miller GE, Chen E, Lachman ME, & Seeman TE (2013). Is change bad? Personality change is associated with poorer psychological health and greater metabolic syndrome in midlife. Journal of Personality, 81, 249–260. doi: 10.1111/jopy.12002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam M, Mazumder M, Schwabe-Warf D, Stephan Y, Sutin AR, & Terracciano A. (2019). Personality changes with dementia from the informant perspective: New data and meta-analysis. Journal of the American Medical Directors Association, 20, 131–137. doi: 10.1016/j.jamda.2018.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson SE, Steptoe A, Beeken RJ, Kivimaki M, & Wardle J. (2014). Psychological changes following weight loss in overweight and obese adults: A prospective cohort study. PloS One, 9(8), e104552. doi : 10.1371/journal.pone.0104552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jokela M, Hakulinen C, Singh-Manoux A, & Kivimäki M. (2014). Personality change associated with chronic diseases: Pooled analysis of four prospective cohort studies. Psychological Medicine, 44(12), 2629–2640. doi: 10.1017/S0033291714000257. [DOI] [PubMed] [Google Scholar]
- Jokela M, Hintsanen M, Hakulinen C, Batty GD, Nabi H, Singh-Manoux A, & Kivimäki M. (2013). Association of personality with the development and persistence of obesity: A meta-analysis based on individual–participant data. Obesity Reviews, 14, 315–323. doi : 10.1111/obr.12007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konttinen H, Kiviruusu O, Huurre T, Haukkala A, Aro H, & Marttunen M. (2014). Longitudinal associations between depressive symptoms and body mass index in a 20-year follow-up. International Journal of Obesity, 38(5), 668–674. doi: 10.1038/ijo.2013.151. [DOI] [PubMed] [Google Scholar]
- Lahti M, Räikkönen K, Lemola S, Lahti J, Heinonen K, Kajantie E, …& Eriksson JG (2013). Trajectories of physical growth and personality dimensions of the Five-Factor Model. Journal of Personality and Social Psychology, 105(1), 154–169.doi: 10.1037/a0032300 [DOI] [PubMed] [Google Scholar]
- Lucas RE & Donnellan MB (2011). Personality development across the life span: Longitudinal analyses with a national sample from Germany. Journal of Personality and Social Psychology, 101, 847–861. doi: 10.1037/a0024298 [DOI] [PubMed] [Google Scholar]
- Magee CA, & Heaven PC (2011). Big-Five personality factors, obesity and 2-year weight gain in Australian adults. Journal of Research in Personality, 45(3), 332–335. doi : 10.1016/j.jrp.2011.02.009 [DOI] [Google Scholar]
- McCrae RR, & John OP (1992). An introduction to the five-factor model and its applications. Journal of Personality, 60(2), 175–215. doi : 10.1111/j.1467-6494.1992.tb00970.x [DOI] [PubMed] [Google Scholar]
- McCrae RR, Terracciano A, & Members of the Personality Profiles of Cultures Project. (2005). Universal features of personality traits from the observer’s perspective: Data from 50 cultures. Journal of Personality and Social Psychology, 88, 547–561. doi: 10.1037/0022-3514.88.3.547 [DOI] [PubMed] [Google Scholar]
- Mõttus R, McNeill G, Jia X, Craig LCA, Starr JM, & Deary IJ (2013). The associations between personality, diet and body mass index in older people. Health Psychology, 32(4), 353–360. doi: 10.1037/a0025537 [DOI] [PubMed] [Google Scholar]
- Mroczek DK, & Spiro A III (2007). Personality change influences mortality in older men. Psychological Science, 18, 371–376. doi: 10.1111/j.1467-9280.2007.01907.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller S, Wagner J, Drewelies J, Duezel S, Eibich P, Specht J, … & Gerstorf D. (2016). Personality development in old age relates to physical health and cognitive performance: Evidence from the Berlin Aging Study II. Journal of Research in Personality, 65, 94–108. doi : 10.1016/j.jrp.2016.08.007 [DOI] [Google Scholar]
- Mueller S, Wagner J, Smith J, Voelkle MC, & Gerstorf D. (2018). The interplay of personality and functional health in old and very old age: Dynamic within-person interrelations across up to 13 years. Journal of Personality and Social Psychology, 115(6), 1127–1147. doi: 10.1037/pspp0000173 [DOI] [PubMed] [Google Scholar]
- Murphy RA, Patel KV, Kritchevsky SB, Houston DK, Newman AB, Koster A, … & Harris TB (2014). Weight change, body composition, and risk of mobility disability and mortality in older adults: a population-based cohort study. Journal of the American Geriatrics Society, 62(8), 1476–1483. doi: 10.1111/jgs.12954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman AB, Yanez D, Harris T, Duxbury A, Enright PL, Fried LP, & Cardiovascular Study Research Group. (2001). Weight change in old age and its association with mortality. Journal of the American Geriatrics Society, 49(10), 1309–1318. doi : 10.1046/j.1532-5415.2001.49258.x [DOI] [PubMed] [Google Scholar]
- Park SY, Wilkens LR, Maskarinec G, Haiman CA, Kolonel LN, & Marchand LL (2018). Weight change in older adults and mortality: the Multiethnic Cohort Study. International Journal of Obesity, 42(2), 205–212. doi: 10.1038/ijo.2017.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie CS, Locher JL, Roth DL, McVie T, Sawyer P, & Allman R. (2008). Unintentional weight loss predicts decline in activities of daily living function and life-space mobility over 4 years among community-dwelling older adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 63(1), 67–75. doi : 10.1093/gerona/63.1.67 [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Dugravot A, Shipley M, Brunner EJ, Elbaz A, Sabia S, & Kivimaki M. (2018). Obesity trajectories and risk of dementia: 28 years of follow-up in the Whitehall II Study. Alzheimer’s & Dementia, 14(2), 178–186. doi: 10.1016/j.jalz.2017.06.2637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephan Y, Sutin AR, Bosselut G, & Terracciano A. (2017). Sensory functioning and personality development among older adults. Psychology and Aging, 32, 139–147. doi: 10.1037/pag0000159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephan Y, Sutin AR, Canada B, & Terracciano A. (2017). Personality and frailty: Evidence from four samples. Journal of Research in Personality, 66, 46–53. doi: 10.1016/j.jrp.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephan Y, Sutin AR, Luchetti M, Bosselut G, & Terracciano A. (2018). Physical activity and personality development over twenty years: Evidence from three longitudinal samples. Journal of Research in Personality, 73, 173–179. doi : 10.1016/j.jrp.2018.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephan Y, Sutin AR, Luchetti M, & Terracciano A. (2016). Allostatic load and personality: A 4-year longitudinal study. Psychosomatic Medicine, 78(3), 302–310. doi: 10.1097/PSY.0000000000000281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephan Y, Sutin AR, & Terracciano A. (2014). Physical activity and personality development across adulthood and old age: Evidence from two longitudinal studies. Journal of Research in Personality, 49, 1–7. doi: 10.1016/j.jrp.2013.12.003 [DOI] [Google Scholar]
- Sutin AR, Costa PT Jr, Chan W, Milaneschi Y, Eaton WW, Zonderman AB, … & Terracciano A. (2013). I know not to, but I can’t help it: Weight gain and changes in impulsivity-related personality traits. Psychological Science, 24(7), 1323–1328. doi: 10.1177/0956797612469212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, Ferrucci L, Zonderman AB, & Terracciano A. (2011). Personality and obesity across the adult life span. Journal of Personality and Social Psychology, 101(3), 579–592. doi: 10.1037/a0024286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, & Terracciano A. (2016a). Personality traits and body mass index: Modifiers and mechanisms. Psychology & Health, 31(3), 259–275. doi: 10.1080/08870446.2015.1082561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, & Terracciano A. (2016b). Five-factor model personality traits and the objective and subjective experience of body weight. Journal of Personality, 84(1), 102–112. doi: 10.1111/jopy.12143. [DOI] [PubMed] [Google Scholar]
- Terracciano A, McCrae RR, & Costa PT Jr. (2006). Longitudinal trajectories in Guilford-Zimmerman Temperament Survey data: Results from the Baltimore Longitudinal Study of Aging. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 61, 108–116. doi: 10.1093/geronb/61.2.P108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Stephan Y, Luchetti M, Albanese E, & Sutin AR (2017). Personality traits and risk of cognitive impairment and dementia. Journal of Psychiatric Research, 89, 22–27. doi: 10.1016/j.jpsychires.2017.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Sutin AR, An Y, O’Brien RJ, Ferrucci L, Zonderman AB, & Resnick SM (2014). Personality and risk of Alzheimer’s disease: New data and meta-analysis. Alzheimer’s & Dementia, 10(2), 179–186. doi: 10.1016/j.jalz.2013.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turiano NA, Whiteman SD, Hampson SE, Roberts BW, & Mroczek DK (2012). Personality and substance use in midlife: Conscientiousness as a moderator and the effects of trait change. Journal of Research in Personality, 46, 295–305. doi: 10.1016/j.jrp.2012.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y, Manson JE, Yuan C, Liang MH, Grodstein F, Stampfer MJ, … Hu FB (2017). Associations of weight gain from early to middle adulthood with major health outcomes later in life. JAMA, 318(3), 255–269. doi: 10.1001/jama.2017.7092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimprich D, Allemand M, & Lachman ME (2012). Factorial structure and age-related psychometrics of the MIDUS personality adjective items across the lifespan. Psychological Assessment, 24, 173–186. doi : 10.1037/a0025265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vainik U, Dagher A, Realo A, Colodro-Conde L, Mortensen EL, Jang K, … & Mõttus R. (2019). Personality-obesity associations are driven by narrow traits: A meta-analysis. Obesity Reviews, 20, 1121–1131. doi: 10.1111/obr.12856. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.