Abstract
Studies of mouse models of Alzheimer's disease (AD) have demonstrated that nitric oxide synthase 2 (NOS2) is involved in AD pathology. However, the effects of NOS2 on the pathology of Parkinson’s disease (PD) are not well studied. To address this gap, we examined the impact of NOS2 on disease-associated phenotypes in a mouse model of PD. Transgenic mice carrying the A53T mutation of α-synuclein (SynA53T) and newly generated double transgenic mice with deletion of NOS2 (SynA53T/NOS2−/−) were used. Compared with SynA53T mice, the loss of nos2 decreased α-synuclein phosphorylation at serine 129 and reduced α-synuclein-induced microglial and astrocyte activation in SynA53T/NOS−/− mice. Additionally, neuroinflammation-related gene clusters in the deep mesencephalic nucleus (DpMe) were altered in SynA53T/NOS−/− mice compared with SynA53T mice. Taken together, our results suggest that deletion of nos2 alleviates α-synuclein pathology and α-synuclein-associated neuroinflammatory responses in the brain.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13041-023-00996-1.
Keywords: α-Synuclein, nos2, Neuroinflammation, Parkinson’s disease
Main text
Nitric oxide (NO) is a bioactive free radical that is involved in various physiological and pathological processes in several organ systems and the central nervous system (CNS) [1]. In the brain, nitric oxide synthase 2 (NOS2) plays an important role in neurotransmission, neural development, and the immune defense response [2]. Interestingly, several recent studies have reported that NOS2 differentially regulates Alzheimer’s disease (AD) pathology. For instance, deletion of nos2 in mice results in the expression of mutant amyloid precursor protein (APP) and hyperphosphorylation of tau in the brain [3]. Compared with APPSwDI mice, APPSwDI/NOS2−/− mice exhibit spatial memory impairment and tau pathology [4]. However, the effects of NOS2 on α-synuclein-induced Parkinson’s disease (PD) pathology remain unclear.
To address this gap, we generated SynA53T/NOS2−/− mice by hybridizing human SynA53T-expressing transgenic mice and nos2 knockout (NOS2−/−) mice. Generation of the SynA53T/NOS2−/− mice was confirmed by RT–PCR, which failed to detect nos2 mRNA (Additional file 1: Fig. S1).
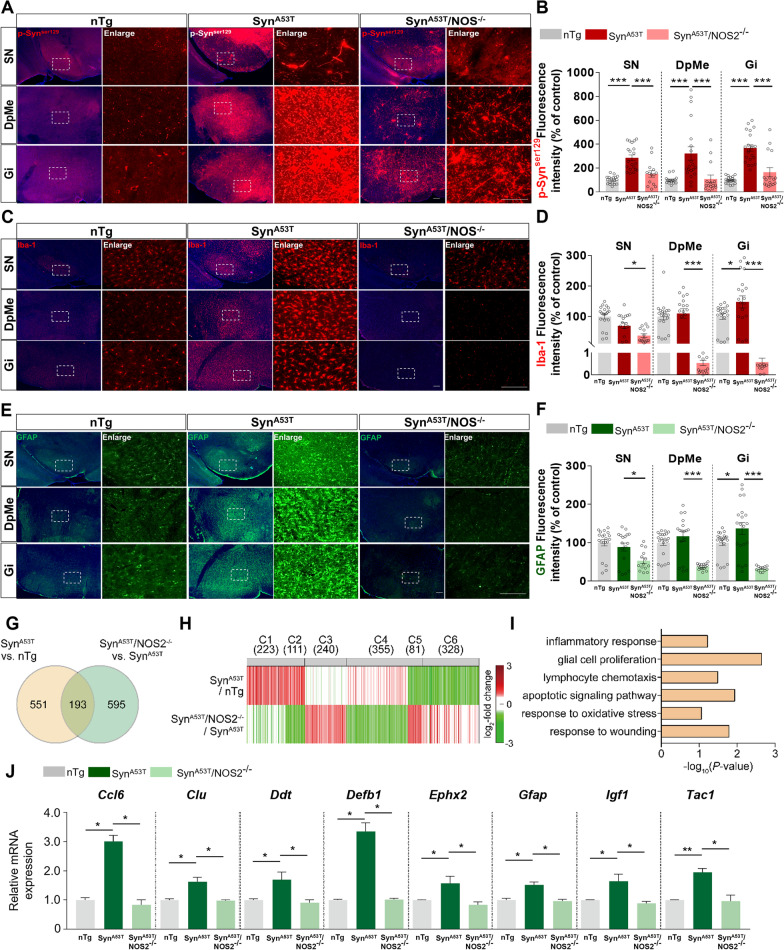
We then examined whether genetic deletion of nos2 affects α-synuclein-induced PD pathology. The brains of 10- to 11-month-old non-transgenic (nTg), SynA53T, and SynA53T/NOS2−/− mice were subjected to immunofluorescence staining with an anti-p-Synser129 antibody. Compared with nTg mice, p-Synser129 levels in the substantia nigra (SN), deep mesencephalic reticular nucleus (DpMe), and granular insular cortex (Gi) were significantly higher in SynA53T mice (Fig. 1A, B). Importantly, p-Synser129 levels in the SN, DpMe, and Gi were significantly lower in SynA53T/NOS2−/− mice than in SynA53T mice (Fig. 1A, B). Moreover, p-Synser129 levels in the cortex, caudate and putamen (CPu) and hippocampus (Hippo) were significantly reduced in SynA53T/NOS2−/− mice compared with SynA53T mice (Additional file 1: Fig. S2A, B). These data suggest that genetic deletion of nos2 alleviates synucleinopathy in the brain.
Fig. 1.
Deletion of nos2 alleviates synuclein pathology and neuroinflammatory responses in SynA53T/NOS2−/− mice. A Immunofluorescence staining of the substantia nigra (SN), deep mesencephalic nucleus (DpMe), and granular insular cortex (Gi) of 10- to 11-month-old nTg, SynA53T, and SynA53T/NOS2−/− mice with an anti-p-Synser129 antibody. B Quantification of the data in A (SN, DpMe, Gi region; nTg: n = 17–20 brain slices/5 mice; SynA53T: n = 20–22 brain slices/5 mice; SynA53T/NOS2−/−: n = 14–16 brain slices/4 mice). C Immunofluorescence staining of the SN, DpMe, and Gi of 10- to 11-month-old nTg, SynA53T, and SynA53T/NOS2−/− mice with an anti-Iba-1 antibody. D Quantification of the data in C (SN, DpMe, Gi region; nTg: n = 20 brain slices/5 mice; SynA53T: n = 17–20 brain slices/5 mice; SynA53T/NOS2−/−: n = 11–15 brain slices/4 mice). E Immunofluorescence staining of the SN, DpMe, and Gi of 10- to 11-month-old nTg, SynA53T, and SynA53T/NOS2−/− mice with an anti-GFAP antibody. F Quantification of the data in E (SN, DpMe, Gi region; nTg: n = 20 brain slices/5 mice; SynA53T: n = 17–20 brain slices/5 mice; SynA53T/NOS2−/−: n = 12–16 brain slices/4 mice). G Differentially expressed genes (DEGs) were identified by comparing SynA53T/NOS2−/− mice with SynA53T mice and SynA53T mice with nTg mice. The numbers of DEGs in each comparison and the number of overlapping DEGs are indicated. H Six clusters (C1–6) of DEGs were identified from the two comparisons. The color bar represents the gradient of log2 fold changes. The number of DEGs in each cluster is denoted in parentheses. I Cellular processes represented by the DEGs in C2. The x-axis is the −log10(P), where P is the enrichment P value from ConsensusPathDB software. J DEGs involved in the inflammatory response (n = 3 mice/group). *p < 0.05, **p < 0.01, ***p < 0.001, scale bar = 100 μm
Since genetic deletion of nos2 diminished α-synuclein aggregation in the brain, we further investigated the impact of nos2 deletion on α-synuclein-induced glial activation. The brains of 10- to 11-month-old nTg, SynA53T, and SynA53T/NOS2−/− mice were subjected to immunofluorescence staining with anti-Iba-1 and anti-GFAP antibodies. Compared with nTg mice, microglial/astrocyte fluorescence intensity, the number of Iba-1-positive cells, and the Iba-1/GFAP % area were increased in the DpMe and Gi but not in the SN in SynA53T mice (Fig. 1C, D and Additional file 1: Fig. S3). Importantly, Iba-1 fluorescence intensity, the number of Iba-1-positive cells, and the Iba-1-positive % area in the SN, DpMe, and Gi were significantly lower in SynA53T/NOS2−/− mice than in SynA53T mice (Fig. 1C, D and Additional file 1: Fig. S3). Moreover, GFAP fluorescence intensity in the SN, DpMe, and Gi was significantly reduced in SynA53T/NOS2−/− mice compared with SynA53T mice (Fig. 1E, F). The α-synuclein-induced number of GFAP-positive cells and GFAP-positive % area in the DpMe and Gi were significantly diminished in SynA53T/NOS2−/− mice compared with SynA53T mice (Additional file 1: Fig. S3). In addition, Iba-1/GFAP fluorescence intensity, the number of Iba-1/GFAP-positive cells and the Iba-1/GFAP % area in the cortex, CPu, and hippocampus were significantly reduced in SynA53T/NOS2−/− mice compared with nTg and SynA53T mice (Figs. S4-S5). Taken together, these data suggest that deletion of nos2 diminishes α-synuclein-stimulated microglial and astrocyte activation and that NOS2 is required for α-synuclein-mediated neuroinflammation in the brain.
To investigate the effects of nos2 deletion on gene expression in the mouse model of PD, we isolated the DpMe region (which exhibited the greatest regulatory effects of nos2) from 10- to 11-month-old nTg, SynA53T, and SynA53T/NOS2−/− mice and conducted RNA sequencing. A total of 1,339 differentially expressed genes (DEGs) were identified in SynA53T versus nTg mice and SynA53T/NOS2−/− versus SynA53T mice (744 and 788 DEGs, respectively) (Fig. 1G and Additional file 2: Table S1). Among the 1339 DEGs, 193 overlapped between the two comparisons (Fig. 1G). These results indicate that nos2 deletion significantly alters gene expression in this mouse model of PD (Additional file 3).
To systematically investigate the cellular processes affected by nos2 deletion, we classified the 1,339 DEGs into 6 clusters (C1-6) based on their differential expression in the two comparisons (Fig. 1H). C2 was upregulated in SynA53T mice compared with nTg mice but downregulated in SynA53T/NOS2−/− mice compared with SynA53T mice. Thus, we focused on this cluster because it likely includes genes associated with the effects of NOS2 on PD pathology. The cellular processes represented by the DEGs in C2 were identified by gene set enrichment analysis using Consensus Path DB [5]. Interestingly, the DEGs in C2 were mainly involved in neuroinflammatory responses, glial cell proliferation, oxidative stress, and apoptosis (Fig. 1I). Notably, genes involved in neuroinflammatory response-related processes were strongly downregulated in SynA53T/NOS2−/− mice compared with SynA53T mice (Fig. 1J).
In summary, α-synuclein phosphorylation, α-synuclein-induced neuroinflammation, and the expression of related genes were significantly suppressed in the brains of SynA53T/NOS2−/− mice. Overall, our results suggest that NOS2 is a crucial regulator of the synucleinopathy and neuroinflammatory response associated with PD pathology.
A recent study demonstrated that NOS2 overexpression induces NO production and α-synuclein aggregation in PC12 neurons [6]. In SH-SY5Y cells, NOS2 expression induces the formation of cytotoxic nitrated α-synuclein [7]. However, the effects of nos2 deletion on α-synuclein pathology have not been investigated. The significant reduction in p-Synser129 levels in SynA53T/NOS2−/− mice compared with SynA53T mice suggests that decreasing NOS2 expression may help alleviate α-synucleinopathy in the brain.
Interestingly, several recent studies have shown that NOS2 regulates neuroinflammatory responses in the brain. For instance, the lipopolysaccharide (LPS)-induced increase in TNF-α levels is significantly reduced in nos2 knockout mice [8], and deletion of nos2 decreases the number of Iba-1/GFAP-positive cells in the brain compared with wild-type mice [9]. In addition, GFAP expression is diminished by one-third in NOS2−/− mice compared with nTG mice [10]. In the present study, microglial and astrocyte activation in the brain, which are associated with severe synuclein pathology, were dramatically reduced in SynA53T/NOS2−/− mice compared with SynA53T mice. It is possible that brain region-specific synuclein aggregation and pathology contribute to Iba-1/GFAP expression when nos2 is knocked out. Another possibility is that unknown synuclein pathology/NOS2-associated molecular targets contribute to glial hypoactivity/degradation when nos2 is deleted in vivo. Future studies will focus on identifying the molecules that contribute to glial inactivation and the amelioration of synuclein pathology when nos2 is deleted. Overall, the available data suggest that NOS2 has critical functions in the modulation of glial homeostasis in this mouse model of PD.
In conclusion, we generated SynA53T/NOS2−/− mice for the first time by crossing human α-synuclein A53T mutant mice and nos2 knockout mice and found that α-synuclein pathology, neuroinflammatory responses, and neuroinflammation-associated gene expression were reduced in the double transgenic mice compared with SynA53T mice. Our data indicate that NOS2 may be a therapeutic target for modulating PD pathology in the brain.
Supplementary Information
Additional file 1: Figure S1. The nos2 mRNA expression was not detected in SynA53T/NOS2−/− mice. Figure S2. The p-SynSer129 levels in the cortex, caudate and putamen, and hippocampus were significantly diminished in SynA53T/NOS2−/− mice compared with SynA53T mice. Figure S3. The number of Iba-1/GFAP-positive cells and % area fractions in the substantia nigra, deep mesencephalic nucleus, and granular insular cortex were significantly reduced in SynA53T/NOS2−/− mice compared with SynA53T mice. Figure S4. The Iba-1-fluorescence intensity, number of Iba-1-positive cells, and % area fractions in the cortex, caudate and putamen, and hippocampus were significantly suppressed in SynA53T/NOS2−/− mice compared with SynA53T mice. Figure S5. The GFAP-fluorescence intensity, number of GFAP-positive cells, and % area fractions in the cortex, caudate and putamen, and hippocampus were significantly downregulated in SynA53T/NOS2−/− mice compared with SynA53T mice. Materials and methods.
Additional file 2: Table S1. The lists of the 1,339 DEGs included in the individual clusters.
Additional file 3: Table S2. One-way ANOVA (Tukey’s test) and significance of the results of the in vivo experiments in this study.
Acknowledgements
Confocal microscopy (Nikon, Nikon A1Rsi) and slide scanner (3DHistech, panoramic scan) data were acquired at the Brain Research Core Facilities of the Korea Brain Research Institute. We thank previous and current members of the neurodegenerative diseases lab for conducting double blind-analysis, editing and valuable comments on our manuscript and for technical assistance with in vivo studies.
Abbreviations
- AD
Alzheimer’s disease
- CPu
Caudate and putamen
- DEGs
Differentially expressed genes
- DpMe
Deep mesencephalic reticular nucleus
- Gi
Granular insular cortex
- Hippo
Hippocampus
- LPS
Lipopolysaccharide
- NOS2
Nitric oxide synthase 2
- PD
Parkinson’s disease
- SN
Substantia nigra
Author contributions
SC, YPC, KK, and HSH designed the experiments. JK, SC, and HSH wrote the original and revised manuscript. JK, JYH, YL, and SC performed the experiments. JK and SC analyzed the data and generated the figures. All authors read and approved the final manuscript.
Funding
This work was supported by the KBRI basic research program through KBRI funded by the Ministry of Science, ICT & Future Planning (Grant Numbers 22-BR-02–12 and 22-BR-02–03, H.S.H.; 19-BR-03–03, Y.P.C.; 22-BR-01–02, S.C.; and 22-BR-05–02, K.K, H.S.H).
Availability of data and materials
All data generated and/or analyzed during this study are included in this published article and its supplementary information. The materials and methods are presented in Additional file 1.
Declarations
Ethics approval and consent to participate
All animal experiments were approved by the Institutional Animal Care and Use Committee of the Korea Brain Research Institute (KBRI) (Approval Nos. IACUC-18-0007 and IACUC-19-0010).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jieun Kim and Jung-Youn Han contributed equally to this work
Contributor Information
Young Pyo Choi, Email: cyp0201@kbri.re.kr.
Sehyun Chae, Email: shchae@kbri.re.kr.
Hyang-Sook Hoe, Email: sookhoe72@kbri.re.kr.
References
- 1.Saha RN, Pahan K. Regulation of inducible nitric oxide synthase gene in glial cells. Antioxid Redox Signal. 2006;8(5–6):929–947. doi: 10.1089/ars.2006.8.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tuteja N, Chandra M, Tuteja R, Misra MK. Nitric oxide as a unique bioactive signaling messenger in physiology and pathophysiology. J Biomed Biotechnol. 2004;2004(4):227–237. doi: 10.1155/S1110724304402034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Colton CA, Vitek MP, Wink DA, Xu Q, Cantillana V, Previti ML, et al. NO synthase 2 (NOS2) deletion promotes multiple pathologies in a mouse model of Alzheimer's disease. Proc Natl Acad Sci U S A. 2006;103(34):12867–12872. doi: 10.1073/pnas.0601075103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilcock DM, Lewis MR, Van Nostrand WE, Davis J, Previti ML, Gharkholonarehe N, et al. Progression of amyloid pathology to Alzheimer's disease pathology in an amyloid precursor protein transgenic mouse model by removal of nitric oxide synthase 2. J Neurosci. 2008;28(7):1537–1545. doi: 10.1523/JNEUROSCI.5066-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kamburov A, Wierling C, Lehrach H, Herwig R. ConsensusPathDB–a database for integrating human functional interaction networks. Nucleic Acids Res. 2009;37:D623–D628. doi: 10.1093/nar/gkn698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stone DK, Kiyota T, Mosley RL, Gendelman HE. A model of nitric oxide induced alpha-synuclein misfolding in Parkinson's disease. Neurosci Lett. 2012;523(2):167–173. doi: 10.1016/j.neulet.2012.06.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu Y, Qiang M, Wei Y, He R. A novel molecular mechanism for nitrated {alpha}-synuclein-induced cell death. J Mol Cell Biol. 2011;3(4):239–249. doi: 10.1093/jmcb/mjr011. [DOI] [PubMed] [Google Scholar]
- 8.Okamoto T, Gohil K, Finkelstein EI, Bove P, Akaike T, van der Vliet A. Multiple contributing roles for NOS2 in LPS-induced acute airway inflammation in mice. Am J Physiol Lung Cell Mol Physiol. 2004;286(1):L198–209. doi: 10.1152/ajplung.00136.2003. [DOI] [PubMed] [Google Scholar]
- 9.Issy AC, Nascimento GC, Abreu GHD, Tristao FS, Del-Bel E, Duarte T, et al. Differential behavioral and glial responses induced by dopaminergic mechanisms in the iNOS knockout mice. Behav Brain Res. 2018;350:44–53. doi: 10.1016/j.bbr.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 10.Raposo C, Luna RL, Nunes AK, Thome R, Peixoto CA. Role of iNOS-NO-cGMP signaling in modulation of inflammatory and myelination processes. Brain Res Bull. 2014;104:60–73. doi: 10.1016/j.brainresbull.2014.04.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1. The nos2 mRNA expression was not detected in SynA53T/NOS2−/− mice. Figure S2. The p-SynSer129 levels in the cortex, caudate and putamen, and hippocampus were significantly diminished in SynA53T/NOS2−/− mice compared with SynA53T mice. Figure S3. The number of Iba-1/GFAP-positive cells and % area fractions in the substantia nigra, deep mesencephalic nucleus, and granular insular cortex were significantly reduced in SynA53T/NOS2−/− mice compared with SynA53T mice. Figure S4. The Iba-1-fluorescence intensity, number of Iba-1-positive cells, and % area fractions in the cortex, caudate and putamen, and hippocampus were significantly suppressed in SynA53T/NOS2−/− mice compared with SynA53T mice. Figure S5. The GFAP-fluorescence intensity, number of GFAP-positive cells, and % area fractions in the cortex, caudate and putamen, and hippocampus were significantly downregulated in SynA53T/NOS2−/− mice compared with SynA53T mice. Materials and methods.
Additional file 2: Table S1. The lists of the 1,339 DEGs included in the individual clusters.
Additional file 3: Table S2. One-way ANOVA (Tukey’s test) and significance of the results of the in vivo experiments in this study.
Data Availability Statement
All data generated and/or analyzed during this study are included in this published article and its supplementary information. The materials and methods are presented in Additional file 1.