Abstract
Background:
The current literature lacks an updated review examining return to play (RTP) and return to prior performance (RTPP) after shoulder surgery in professional baseball players.
Purpose:
To summarize the RTP rate, RTPP rate, and baseball-specific performance metrics among professional baseball players who underwent shoulder surgery.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A literature search was performed utilizing the PubMed, MEDLINE, and CINAHL databases and according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Inclusion criteria were English-language studies reporting on postoperative RTP and/or RTPP in professional baseball players who underwent shoulder surgery between 1976 and 2016. RTP rates, RTPP rates, and baseball-specific performance metrics were extracted from qualifying studies. A total of 2034 articles were identified after the initial search. Meta-analysis was performed where applicable, yielding weighted averages of RTP and RTPP rates and comparisons between pitchers and nonpitchers for each type of surgery. Baseball-specific performance metrics were reported as a narrative summary.
Results:
Overall, 26 studies featuring 1228 professional baseball players were included. Patient-level outcome data were available for 529 players. Surgical interventions included rotator cuff debridement (n = 197), rotator cuff repair (RCR; n = 43), superior labrum from anterior to posterior repair (n = 124), labral repair (n = 103), latissimus dorsi/teres major (LD/TM) repair (n = 21), biceps tenodesis (n = 17), coracoclavicular ligament reconstruction (n = 15), anterior capsular repair (n = 5), and scapulothoracic bursectomy (n = 4). Rotator cuff debridement was the most common surgical procedure, while scapulothoracic bursectomy was the least common (37.2% and 0.8% of interventions, respectively). Meta-analysis revealed that the RTP rate was highest for LD/TM repair (84.5%) and lowest for RCR (53.5%), while the RTPP rate was highest for LD/TM repair (100.0%) and lowest for RCR (27.9%). RTP and RTPP rates were generally higher for position players than for pitchers. Nonvolume performance metrics were unaffected by shoulder surgery, while volume statistics decreased or remained similar.
Conclusion:
RTP and RTPP rates among professional baseball players were modest after most types of shoulder surgery. Among surgical procedures commonly performed on professional baseball players, RTP and RTPP rates were highest for LD/TM repair and lowest for RCR.
Keywords: shoulder, baseball, return to play, professional
Professional baseball is one of the most watched sports in the United States, with the Major League Baseball (MLB) World Series averaging more than 17 million viewers annually since 2000. 46 Throwing is integral to the sport, with the ball velocity of professional pitchers often exceeding 90 mph (145 kph). 3,23 Producing such velocity while maintaining control requires intricate functional adjustments at each component of the kinetic chain throughout the throwing motion, most prominently at the shoulder to optimally balance mobility with dynamic stability. 10,30 While acute traumatic injuries of the shoulder are uncommon in baseball, repetitive microtrauma sustained over the course of a career can lead to osseous and soft tissue changes, predisposing players to a variety of injuries such as superior labrum from anterior to posterior (SLAP) tears, rotator cuff tendinitis and tears, impingement, and labral tears and instability. 2,13,22,28,31,47,48,50
Despite increasing implementation of injury prevention measures in professional baseball, epidemiological reports indicate that injury rates have risen in recent years. 4,8,11,12,40 The shoulder is the most commonly affected joint, accounting for 17% of recorded MLB injuries. 20 While nonoperative management is generally the preferred initial mode of treatment for shoulder injuries in elite athletes, athletes who fail to respond to nonoperative measures often require a surgical intervention. 10 While returning to preinjury levels of performance is the goal, outcomes can vary, as anatomic manipulation and scarring associated with surgery have the potential to alter throwing biomechanics and affect velocity and accuracy. 33,41 Moreover, postoperative functional outcomes and rates of return to play (RTP) vary extensively according to the nature of the injury and type of shoulder surgery. 1,9,17,25,36
The aim of this systematic review and meta-analysis was to summarize the rates of RTP and return to prior performance (RTPP; defined as RTP at or above the preinjury level) among professional baseball players (minor leagues [A, AA, AAA] and Major League Baseball) who underwent shoulder surgery. We hypothesized that shoulder surgery would be associated with modest rates of RTP and inferior rates of RTPP, although outcomes would vary according to the injury and procedure type. The study also aimed to summarize the effect of shoulder surgery on baseball-specific performance metrics.
Methods
Using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 34 guidelines, a systematic review of the literature and a meta-analysis of the data were performed. The review was registered in PROSPERO under study identification number CRD42021261339 before initiation.
Search Strategy
An electronic literature search was performed in the PubMed database on July 7, 2021, and in the MEDLINE and CINAHL databases on July 10, 2021, using the search algorithm reported in the Appendix. An additional manual literature search was performed by utilizing the references of articles that were identified via the search of the databases. There were 2 reviewers (C.C.G.-C., E.A.O.) who formulated the search criteria and performed the literature search independently.
Selection Criteria
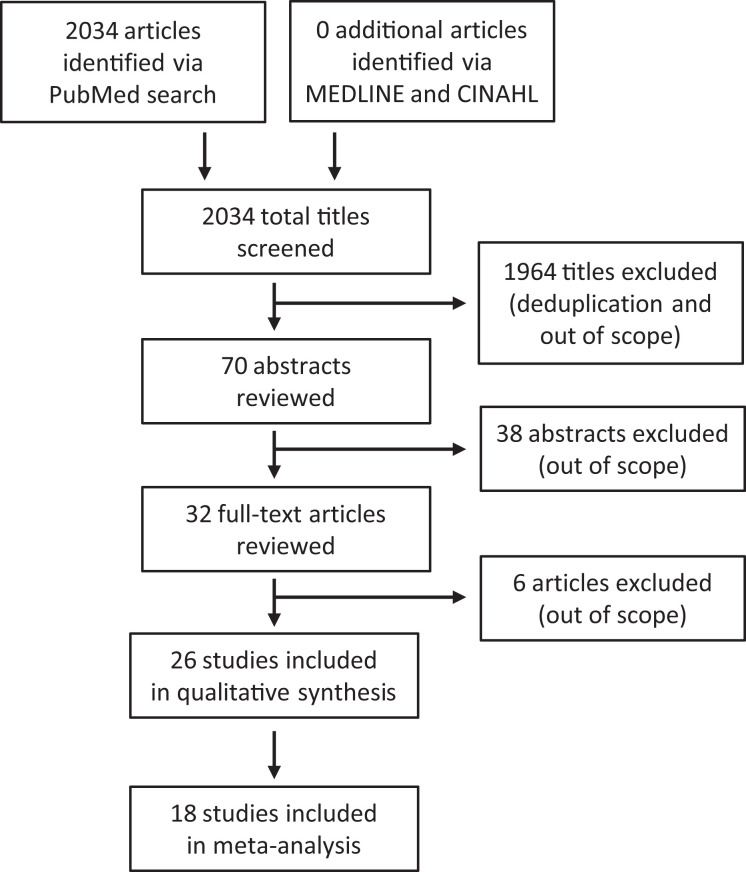
The inclusion criteria were English-language studies reporting postoperative RTP and/or RTPP data in professional baseball players who underwent shoulder surgery with documented abnormalities. Exclusion criteria were review articles or the inclusion of both professional and nonprofessional (high school, college, recreational) baseball players without stratified data by level of play. The initial title search yielded 2034 results. There were 2 independent reviewers (B.L.S., R.E.C.) who analyzed each title for inclusion or exclusion based on the criteria above, yielding 70 studies for an abstract review. The same 2 independent reviewers analyzed the 70 abstracts for inclusion or exclusion based on the above criteria, yielding 32 studies for a final full-text review, which was performed by 4 independent reviewers (C.C.G.-C., B.L.S., R.E.C., E.M.F.). Ultimately, 26 articles were selected for inclusion in the study. Any discrepancies in the title, abstract, and full-text selection process were resolved by the senior author (E.A.O.). Figure 1 illustrates the study-selection process.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) study-selection process.
Extraction of Data
Data extraction was performed according to a standardized protocol that was predefined according to the study aims. Data collected included title, authors, year of publication, journal, level of evidence, study design, quality of the study as defined by the methodological index for non-randomized studies (MINORS) criteria, 44 diagnosis, surgical procedure, dates of procedures, level of play, rate of RTP (defined as RTP at any level), rate of RTPP (defined as RTP at or above the player’s preoperative professional level [ie, A, AA, AAA, MLB]), rehabilitation protocol, baseball-specific performance metrics, patient-reported outcome measures (PROMs), and length of follow-up. If studies included nonprofessional or nonbaseball players, only the stratified data for professional baseball players were extracted.
Data Analysis
Basic data for each included study were aggregated, as were RTP and RTPP data. For shoulder surgical procedures that were featured in ≥2 studies, meta-analysis was performed using Excel (Microsoft) to calculate weighted averages and standard deviations for RTP and RTPP. The weighted averages and standard deviations for RTP and RTPP for each surgical intervention were plotted in forest plot diagrams. A total of 18 studies were included in the meta-analysis (16 for RTP and 17 for RTPP). For surgical procedures that were not featured in ≥2 studies and therefore could not be included in the meta-analysis, RTP and RTPP data were reported individually in a narrative format. For studies that stratified RTP and RTPP data by player position, chi-square tests were performed using Excel to compare RTP and RTPP between pitchers and nonpitchers. Aggregate chi-square tests were also performed for shoulder surgical procedures with RTP and RTPP data stratified by position in >1 study. Data regarding rehabilitation protocols, baseball-specific performance metrics, and PROMs were also recorded and reported as a narrative summary.
Results
Studies and Demographics
Overall, 26 studies ** featuring a total of 1228 professional baseball players who underwent shoulder surgery met the inclusion criteria and were included in the review. Patient-level outcome data were available for 529 players. The level of evidence, MINORS score, diagnosis, surgical intervention, dates of interventions, level of play, number of professional baseball players, and length of follow-up for each study are reported in Table 1. Surgical interventions included rotator cuff debridement (RCD; n = 197), SLAP repair (n = 124), labral repair (n = 103), rotator cuff repair (RCR; n = 43), latissimus dorsi/teres major (LD/TM) repair (n = 21), biceps tenodesis (n = 17), coracoclavicular ligament reconstruction (n = 15), anterior capsular repair (n = 5), and scapulothoracic bursectomy (n = 4). Of note, among reported labral repair procedures, 10 procedures in 2 studies 29,49 were reported as posterior labral repair, while the other 2 studies 5,42 did not specify the location of the remaining 93 labral repair procedures. RCD was the most commonly performed shoulder surgery, accounting for 37.2% of interventions, while scapulothoracic bursectomy was the least common, accounting for 0.8%. The largest study featured 542 professional baseball players, while the smallest featured 1 professional baseball player. The average reported length of follow-up ranged from 12 to 109.2 months. Dates of surgical interventions ranged from 1976 to 2016, with the majority occurring after 2000.
Table 1.
Characteristics of Included Studies a
| Lead Author (Year) | LOE | MINORS Score | Diagnosis | Surgical Intervention | Date of Intervention | Level of Play | No. of Professional Baseball Players | Follow-up, mo |
|---|---|---|---|---|---|---|---|---|
| Higgins 27 (2021) | 3 | 12 | Labral tear, RC tear | Shoulder arthroscopic surgery | 1998-2016 | MLB | 116 | 12 and 24 |
| Erickson 18 (2019) | 4 | 13 | RC tear | RCD or RCR | 2010-2016 | MLB | 151 | 12 |
| Erickson 17 (2019) | 3 | 14 | LD tear, TM tear | Primary repair of LD or TM | 2011-2016 | Professional | 13 | 12 |
| Kercher 29 (2019) | 4 | 6 | Posterior-superior/posterior-inferior/ posterior labral tear | Arthroscopic posterior labral repair | 2009-2015 | Recreational, HS, college, professional | 6 | 41.58 (range, 24-92) |
| Chalmers 6 (2019) | 4 | 6 | Labral, capsular, AC, chondral, subacromial, RC, or biceps abnormality | Labral repair, labral debridement, capsular repair, capsular release, RCR, RCD | 2012-2016 | Professional | 542 | 24 |
| Douglas 15 (2019) | 4 | 9 | SLAP tear | Arthroscopic SLAP repair | 2004-2014 | HS, college, professional | 10 | 109.2 (range, 97.4-120.4) |
| Liu 32 (2018) | 5 | 3 | Grade 3 AC separation | Coracoclavicular ligament reconstruction + distal clavicle excision | NR | MLB | 15 | NR |
| Gilliam 24 (2018) | 4 | 10 | SLAP tear | SLAP repair | 2004-2014 | HS, college, professional | 18 | 78 (range, 27-146) |
| Erickson 19 (2017) | 4 | 11 | LD tear, TM tear | LD or TM repair | 2010-2016 | Recreational, college, professional | 7 | 12 |
| Chalmers 7 (2018) | 4 | 12 | SLAP tear or other indication for biceps tenodesis | Biceps tenodesis | 2010-2013 | Professional | 17 | 24 |
| Smith 45 (2016) | 4 | 12 | SLAP tear | SLAP repair | 2003-2010 | MLB | 24 | NR |
| Dines 14 (2016) | 4 | 10 | FT RC tear | Arthroscopic RCR | NR | MLB | 6 | 66.7 (range, 23.2-94.6) |
| Fedoriw 21 (2014) | 4 | 10 | SLAP tear | SLAP repair/debridement | NR | Professional | 40 | NR |
| Gulotta 25 (2014) | 4 | 7 | Isolated midsubstance anterior capsular tear | Open or arthroscopic anterior capsular repair | 1995-2012 | MLB | 5 | 45.2 (minimum 12) |
| Park 38 (2013) | 4 | 11 | SLAP tear | Arthroscopic SLAP repair | 2006-2010 | College, national team, professional | 8 | 45.8 (range, 24-68) |
| Ellman 16 (2013) | 6 | 8 | Acute LD avulsion | Primary repair of LD avulsion | 2010 | MLB | 1 | 24 |
| Wanich 49 (2012) | 4 | 10 | Batter’s shoulder (posterior labral tear of lead shoulder) | Arthroscopic posterior labral repair | 2006-2009 | HS, college, professional | 4 | 33.6 (range, 18-64) |
| Cohen 10 (2011) | 4 | 10 | Labral tear (n = 23), RC tear (1 FT, 1 PT), capsular contracture (n = 1), outlet impingement (n = 1) | SLAP repair (n = 22), labral debridement (n = 1), RCR (n = 1), RCD (n = 1), acromioplasty (n = 1), capsular release (n = 1) | 2003-2006 | Professional | 27 | 24 |
| Park 39 (2011) | 4 | 10 | Type 2 SLAP tear | Revision arthroscopic type 2 SLAP repair | 2003-2009 | Recreational, college, professional | 2 | 50.5 (range, 8-81) |
| Namdari 35 (2011) | 3 | 10 | RC tear | RC surgery | 1976-2003 | MLB | 33 | 3 seasons |
| Neuman 37 (2011) | 4 | 7 | Type 2 SLAP tear | Type 2 SLAP repair | 2002-2007 | Recreational, college, Olympic, professional | 3 | 42 |
| Ricchetti 42 (2010) | 3 | 12 | Glenoid labral injury | Labral repair | 1995-2004 | MLB | 51 | 49.2 (minimum 3 seasons) |
| Reynolds 41 (2008) | 4 | 6 | RC tear | Arthroscopic RCD | 2002-2005 | Professional | 67 | 38 (range, 18-59) |
| Cerynik 5 (2008) | 4 | 10 | Isolated glenoid labral injury | Labral repair | 1998-2003 | MLB | 42 | Minimum 3 seasons |
| Mazoue 33 (2006) | 4 | 10 | FT RC tear | RCR | 1995-2003 | Professional | 16 | 67 (range, 33-93) |
| Sisto 43 (1986) | 4 | 8 | Scapulothoracic bursitis | Surgical excision of bursa | 1979-1982 | Professional | 4 | 49 (range, 36-60) |
a AC, acromioclavicular; FT, full-thickness; HS, high school; LD, latissimus dorsi; LOE, level of evidence; MINORS, methodological index for non-randomized studies; MLB, Major League Baseball; NR, not reported; PT, partial-thickness; RC, rotator cuff; RCD, rotator cuff debridement; RCR, rotator cuff repair; SLAP, superior labrum from anterior to posterior; TM, teres major.
RTP and RTPP
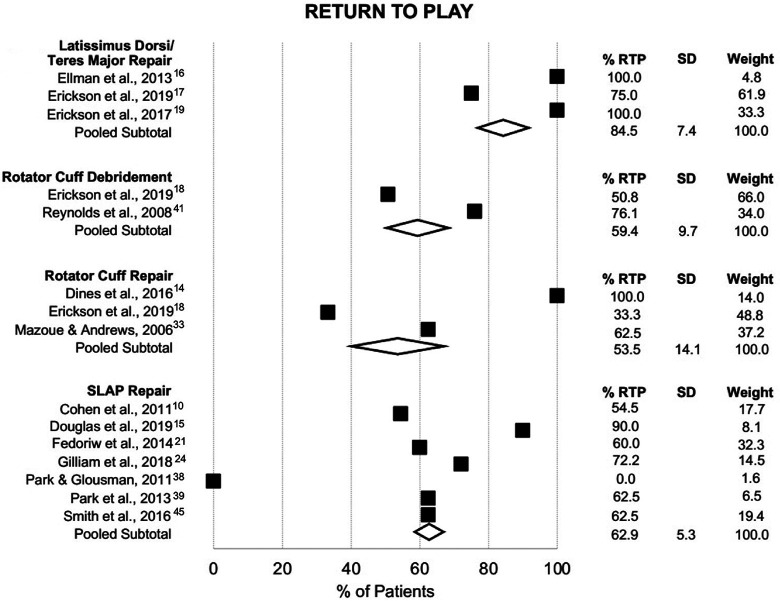
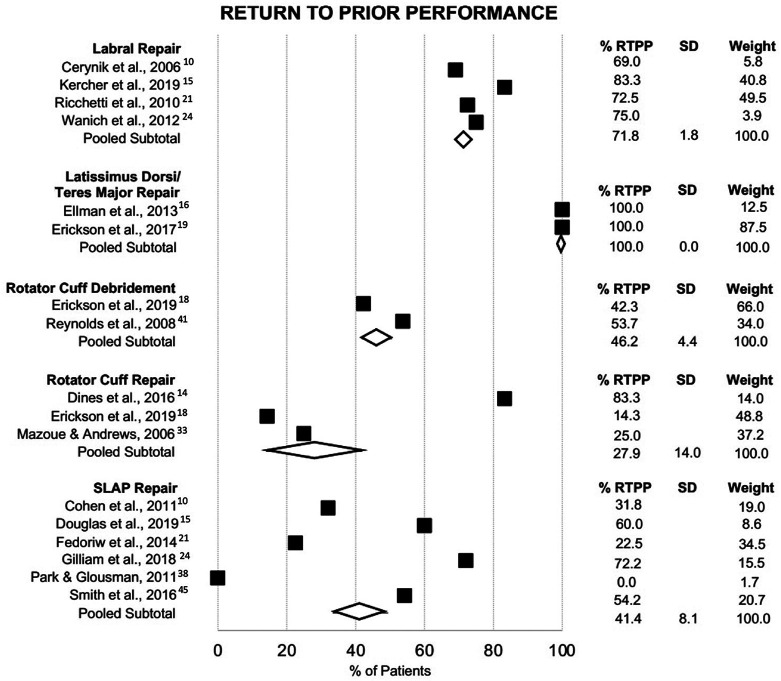
For 5 types of surgery (labral repair, LD/TM repair, RCD, RCR, and SLAP repair), RTP and/or RTPP data were reported in ≥2 studies; meta-analysis to determine weighted averages of RTP and RTPP rates was performed for these 5 types. Table 2 demonstrates the results of RTP and RTPP meta-analysis for each procedure type as well as individual RTP and RTPP data for the surgical procedures that did not qualify for meta-analysis. Notably, RTPP rates for posterior labral repair and non-SLAP labral repair of an unspecified location were similar, so these procedures were considered to be statistically analogous and meta-analyzed together. Meta-analysis revealed the highest RTP rate for LD/TM repair (84.5%), followed by SLAP repair (62.9%) (Figure 2). Of note, Neuman et al 37 did not report objective RTPP data but did report that professional baseball players who underwent SLAP repair subjectively reported an average RTPP rate of 84.1%. The lowest RTP rate was for RCR (53.5%). The RTPP rate was also highest for LD/TM repair (100.0%), followed by labral repair (71.8%) and RCD (46.2%) (Figure 3). The RTPP rate was also lowest for RCR (27.9%). Among surgical procedures that did not qualify for meta-analysis, biceps tenodesis resulted in the lowest RTP and RTPP rates, at 35.3% and 35.3%, respectively, whereas scapulothoracic bursectomy yielded the highest RTP and RTPP rates of 100.0% each.
Table 2.
RTP and RTPP Rates After Shoulder Surgery a
| RTP | RTPP | ||||
|---|---|---|---|---|---|
| Lead Author (Year) | No. of Players | By Study, % | Study Weight, % | By Study, % | Study Weight, % |
| Labral repair | 103 | 75.0 | 100.0 | 71.8 | 100.0 |
| Cerynik 5 (2008) | 42 | NR | — | 69.0 | 40.8 |
| Kercher 29 (2019) | 6 | NR | — | 83.3 | 5.8 |
| Ricchetti 42 (2010) | 51 | NR | — | 72.5 | 49.5 |
| Wanich 49 (2012) | 4 | 75.0 | 100.0 | 75.0 | 3.9 |
| LD/TM repair | 21 | 84.5 | 100.0 | 100.0 | 100.0 |
| Ellman 16 (2013) | 1 | 100.0 | 4.8 | 100.0 | 12.5 |
| Erickson 19 (2017) | 7 | 100.0 | 33.3 | 100.0 | 87.5 |
| Erickson 17 (2019) | 13 | 75.0 | 61.9 | NR | — |
| RCD | 197 | 59.4 | 100.0 | 46.2 | 100.0 |
| Erickson 18 (2019) | 130 | 50.8 | 66.0 | 42.3 | 66.0 |
| Reynolds 41 (2008) | 67 | 76.1 | 34.0 | 53.7 | 34.0 |
| RCR | 43 | 53.5 | 100.0 | 27.9 | 100.0 |
| Dines 14 (2016) | 6 | 100.0 | 14.0 | 83.3 | 14.0 |
| Erickson 18 (2019) | 21 | 33.3 | 48.8 | 14.3 | 48.8 |
| Mazoue 33 (2006) | 16 | 62.5 | 37.2 | 25.0 | 37.2 |
| SLAP repair | 124 | 62.9 | 100.0 | 41.4 | 100.0 |
| Cohen 10 (2011) | 22 | 54.5 | 17.7 | 31.8 | 19.0 |
| Douglas 15 (2019) | 10 | 90.0 | 8.1 | 60.0 | 8.6 |
| Fedoriw 21 (2014) | 40 | 60.0 | 32.3 | 22.5 | 34.5 |
| Gilliam 24 (2018) | 18 | 72.2 | 14.5 | 72.2 | 15.5 |
| Neuman 37 (2011) | 3 | NR | — | NR (84.1 subjectively) | — |
| Park 38 (2013) | 8 | 62.5 | 6.5 | NR | — |
| Park 39 (2011) | 2 | 0.0 | 1.6 | 0.0 | 1.7 |
| Smith 45 (2016) | 24 | 62.5 | 19.4 | 54.2 | 20.7 |
| Other interventions | |||||
| Chalmers 7 (2018) | 17 | 35.3 | 100.0 | 35.3 | 100.0 |
| Chalmers 6 (2019) | 542 | 63.0 | — | 54.2 | — |
| Gulotta 25 (2014) | 5 | 80.0 | 100.0 | 80.0 | 100.0 |
| Higgins 27 (2021) | 116 | NR | — | NR | — |
| Liu 32 (2018) | 15 | 93.3 | 100.0 | 93.3 | 100.0 |
| Sisto 43 (1986) | 4 | 100.0 | 100.0 | 100.0 | 100.0 |
a Dashes indicate not applicable. LD/TM, latissimus dorsi/teres major; NR, not reported; RCD, rotator cuff debridement; RCR, rotator cuff repair; RTP, return to play; RTPP, return to prior performance; SLAP, superior labrum from anterior to posterior.
Figure 2.
Forest plot illustrating the results of return-to-play (RTP) meta-analysis according to the type of surgery. Shown are the pooled subtotal/weighted average (white diamonds) and data for individual studies (black squares).
Figure 3.
Forest plot illustrating the results of return-to–prior performance (RTPP) meta-analysis according to the type of surgery. Shown are the pooled subtotal/weighted average (white diamonds) and data for individual studies (black squares).
Notably, Chalmers et al 6 reported on RTP and RTPP for 542 professional baseball players who underwent shoulder surgery (including labral repair, labral debridement, capsular repair, capsular release, RCR, and RCD) but did not stratify data based on specific surgical procedures. The aggregate RTP rate was 63.0%, and the aggregate RTPP rate was 54.2%.
RTP and RTPP by Player Position
In total, 15 studies stratified RTP data by player position (pitchers vs nonpitchers) (Table 3). Overall, 3 studies 16,17,19 reported stratified RTP data after LD/TM repair; all participants were pitchers, rendering a comparison to nonpitchers impossible. Further, 2 studies 14,33 stratified RTP data after RCR, and no statistically significant difference in RTP based on player position was found. RTP data after SLAP repair were stratified by player position in 3 studies, 21,39,45 and while Fedoriw et al 21 found a significantly higher RTP rate in nonpitchers than in pitchers (P = .03), the statistical significance did not persist when data from all 3 studies were aggregated (P = .09). Among surgical procedures in which stratified data were available from only one study, the RTP rate was significantly higher for nonpitchers than pitchers after biceps tenodesis (P = .01). 7 In the study by Chalmers et al 6 of 542 professional baseball players who underwent a variety of shoulder surgical procedures, the RTP rate was significantly higher for nonpitchers as well (P < .0001).
Table 3.
RTP Rates by Player Position a
| Pitchers | Nonpitchers | ||||
|---|---|---|---|---|---|
| Lead Author (Year) | n | RTP, n (%) | n | RTP, n (%) | P Value |
| LD/TM repair | 21 | 18 (85.7) | 0 | — | — |
| Ellman 16 (2013) | 1 | 1 (100.0) | 0 | — | — |
| Erickson 19 (2017) | 7 | 7 (100.0) | 0 | — | — |
| Erickson 17 (2019) | 13 | 10 (76.9) | 0 | — | — |
| RCR | 18 | 13 (72.2) | 4 | 3 (75.0) | .91 |
| Dines 14 (2016) | 6 | 6 (100.0) | 0 | — | — |
| Mazoue 33 (2006) | 12 | 7 (58.3) | 4 | 3 (75.0) | .55 |
| SLAP repair | 52 | 28 (53.8) | 14 | 11 (78.6) | .09 |
| Fedoriw 21 (2014) | 27 | 13 (48.1) | 13 | 11 (84.6) | .03 |
| Park 39 (2011) | 1 | 0 (0.0) | 1 | 0 (0.0) | >.999 |
| Smith 45 (2016) | 24 | 15 (62.5) | 0 | — | — |
| Other interventions | |||||
| Chalmers 7 (2018) | 12 | 2 (16.7) | 5 | 4 (80.0) | .01 |
| Chalmers 6 (2019) | 325 | 179 (55.1) | 217 | 167 (77.0) | <.0001 |
| Gulotta 25 (2014) | 4 | 3 (75.0) | 1 | 1 (100.0) | .54 |
| Liu 32 (2018) | 15 | 14 (93.3) | 0 | — | — |
| Reynolds 41 (2008) | 67 | 51 (76.1) | 0 | — | — |
| Sisto 43 (1986) | 4 | 4 (100.0) | 0 | — | — |
| Wanich 49 (2012) | 0 | — | 4 | 3 (75.0) | — |
a Dashes indicate not applicable. Boldface P values indicate a statistically significant difference between pitchers and nonpitchers (P < .05; chi-square test). LD/TM, latissimus dorsi/teres major; RCR, rotator cuff repair; RTP, return to play; SLAP, superior labrum from anterior to posterior.
There were 16 studies that stratified RTPP data by player position (Table 4). A total of 3 studies 5,29,42 reported stratified RTPP data after labral repair, with no significant difference between pitchers and nonpitchers. Moreover, 2 studies 16,19 reported position-stratified data after LD/TM repair; again, all participants were pitchers, so no comparison with position players was possible. Additionally, 2 studies 14,33 reported stratified data after RCR, with data reported by Mazoue and Andrews 33 demonstrating a significantly higher RTPP rate in nonpitchers (P = .008), but no statistically significant difference was evident when these data were pooled with those of Dines et al 14 (P = .19). Fedoriw et al 21 demonstrated a significantly higher RTPP rate after SLAP repair in nonpitchers than in pitchers (P = .001), but similarly, no significant difference was found when data were aggregated from all 3 studies reporting stratified data after SLAP repair. 21,39,45 As with RTP, the RTPP rate after biceps tenodesis was also significantly higher in nonpitchers than in pitchers (P = .01). 7
Table 4.
RTPP Rates by Player Position a
| Pitchers | Nonpitchers | ||||
|---|---|---|---|---|---|
| Lead Author (Year) | n | RTPP, n (%) | n | RTPP, n (%) | P Value |
| Labral repair | 93 | 66 (71.0) | 4 | 3 (75.0) | .86 |
| Cerynik 5 (2008) | 42 | 29 (69.0) | 0 | — | — |
| Kercher 29 (2019) | 6 | 37 (72.5) | 0 | — | — |
| Ricchetti 42 (2010) | 51 | — | 4 | 3 (75.0) | — |
| LD/TM repair | 8 | 8 (100.0) | 0 | — | — |
| Ellman 16 (2013) | 1 | 1 (100.0) | 0 | — | — |
| Erickson 19 (2017) | 7 | 7 (100.0) | 0 | — | — |
| RCR | 18 | 7 (38.9) | 4 | 3 (75.0) | .19 |
| Dines 14 (2016) | 6 | 6 (100.0) | 0 | — | — |
| Mazoue 33 (2006) | 12 | 1 (8.3) | 4 | 3 (75.0) | .008 |
| SLAP repair | 52 | 15 (28.8) | 14 | 7 (50.0) | .14 |
| Fedoriw 21 (2014) | 27 | 2 (7.4) | 13 | 7 (53.8) | .001 |
| Park 39 (2011) | 1 | 0 (0.0) | 1 | 0 (0.0) | >.999 |
| Smith 45 (2016) | 24 | 13 (54.2) | 0 | — | — |
| Other interventions | |||||
| Chalmers 7 (2018) | 12 | 2 (16.7) | 5 | 4 (80.0) | .01 |
| Chalmers 6 (2019) | 325 | 146 (44.9) | 217 | 82 (37.8) | .10 |
| Gulotta 25 (2014) | 4 | 3 (75.0) | 1 | 1 (100.0) | .54 |
| Liu 32 (2018) | 15 | 14 (93.3) | 0 | — | — |
| Reynolds 41 (2008) | 67 | 36 (53.7) | 0 | — | — |
| Sisto 43 (1986) | 4 | 4 (100.0) | 0 | — | — |
a Dashes indicate not applicable. Boldface P values indicate a statistically significant difference between pitchers and nonpitchers (P < .05; chi-square test). LD/TM, latissimus dorsi/teres major; RTPP, return to prior performance; RCR, rotator cuff repair; SLAP, superior labrum from anterior to posterior.
Of note, in studies that reported player position, most studies stratified players dichotomously into pitcher and nonpitcher groups. Only 2 of 17 studies (11.8%) reported granular details of the specific field position of nonpitchers. 25,33
Baseball-Specific Performance Metrics
A total of 10 studies utilized baseball-specific performance metrics to assess differences in performance preoperatively and postoperatively. 5,7,14,16 –19,27,42,45 The most commonly reported performance statistics were earned run average (ERA), walks plus hits per inning pitched (WHIP), innings pitched (IP), and other annual volume statistics such as games played per year, runs allowed per year, hits allowed per year, home runs per year, and so on. Postoperative changes in these baseball-specific performance metrics are summarized in Table 5. Additional baseball-specific performance metric data are summarized in a narrative format below. Unless specifically noted, comparisons are between preoperative career averages and postoperative career averages.
Table 5.
Postoperative Changes in Baseball-Specific Performance Metrics a
| Lead Author (Year) | Surgical Intervention | ERA | WHIP | IP | Other Volume Statistics |
|---|---|---|---|---|---|
| Cerynik 5 (2008) | Labral repair | = | = | ↓ | NR |
| Ricchetti 42 (2010) | Labral repair | = | = | = | NR |
| Erickson 19 (2017) | LD/TM repair | = | = | = | = |
| Erickson 17 (2019) | LD/TM repair | NR | = | = | = |
| Ellman 16 (2013) | LD repair | = | NR | NR | NR |
| Erickson 18 (2019) | RCD | = | NR | ↑ | ↑ |
| Dines 14 (2016) | RCR | ↑ (slight increase) | NR | ↓ | NR |
| Erickson 18 (2019) | RCR | = | = | = | = |
| Chalmers 7 (2018) | Biceps tenodesis | = | = | NR | = |
| Higgins 27 (2021) | Shoulder arthroscopic surgery | NR | = | NR | NR |
| Smith 45 (2016) | SLAP repair | = | = | ↓ | NR |
a =, equivalent postoperatively; ↑, increased postoperatively; ↓, decreased postoperatively; ERA, earned run average; IP, innings pitched; LD/TM, latissimus dorsi/teres major; NR, not reported; RCD, rotator cuff debridement; RCR, rotator cuff repair; SLAP, superior labrum from anterior to posterior; WHIP, walks plus hits per inning pitched.
Erickson et al 18 reported extensively on changes in baseball-specific performance metrics after RCD. Notably, pitchers experienced statistically significant increases in volume statistics including wins, losses, games started, complete games, shutouts, IP, hits allowed, runs allowed, earned runs allowed, walks allowed, hit batters, wild pitches, and batters faced per year as well as a significant increase in 0.732 wins above replacement and a significant decrease in fielding independent pitching. Batters also demonstrated an increase in postoperative volume statistics including games, plate appearances, at bats, runs, hits, triples, home runs, runs batted in, stolen bases, times caught stealing, walks, strikeouts, total bases, times hit by a pitch, sacrifice hits, and intentional walks per year. Additionally, batters saw a significant increase in on-base plus slugging after RCD, although no significant increase in wins above replacement was found.
Erickson et al 18 also reported baseball-specific performance metrics for pitchers after RCR; no statistically significant changes in ERA, WHIP, win-loss percentage, average runs allowed, hits per 9 innings, home runs per 9 innings, walks allowed per 9 innings, strikeouts per 9 innings, strikeouts per walk, wins, losses, games, games started, games finished, complete games, shutouts, saves, IP, hits allowed, runs allowed, earned runs allowed, home runs allowed, walks allowed, intentional walks, hit batters, balks, or wild pitches per year were found. In contrast, Dines et al 14 noted a significant decrease in IP after RCR compared with the preoperative career IP, and 3 of 5 pitchers who returned to MLB-level play after RCR demonstrated a “slight” worsening of ERA.
Erickson et al 17 reported on baseball-specific performance metrics after LD/TM repair. In pitchers, there were no statistically significant changes in postoperative career baseball-specific performance metrics (including WHIP, IP, or other volume statistics) compared with preoperative career values. However, pitchers who underwent LD/TM repair did have significantly lower postoperative volume statistics, including games, innings, hits, strikeouts, hit batters, and batters faced per year, compared with a control group. Another study, by Erickson et al, 19 corroborated these findings, with no significant change in baseball-specific performance metrics (including ERA, WHIP, IP, and other volume statistics) after LD/TM repair. Ellman et al 16 examined performance statistics for one MLB pitcher after LD repair; in his second postoperative season, his ERA was comparable to his career average, and he was selected to the All-Star Team.
Cerynik et al 5 reported baseball-specific performance metrics for pitchers after labral repair. Compared with their most recent 3 preoperative seasons, a statistically significant decrease in IP by starting pitchers in their first postoperative MLB season was observed, whereas after 3 postoperative seasons, a statistically significant decrease in IP was observed among relievers; there was no change in postoperative ERA or WHIP. Ricchetti et al 42 also examined pitching performance metrics after labral repair and found no statistically significant change in IP, ERA, or WHIP compared to preoperative career averages.
Smith et al 45 investigated performance metrics in pitchers after SLAP repair and found a statistically significant decrease in IP but no significant change in ERA or WHIP. Higgins et al 27 found no significant change in WHIP for pitchers or on-base plus slugging for nonpitchers between the most recent preinjury season and the first and second postoperative seasons after shoulder arthroscopic surgery. Chalmers et al 7 reported baseball-specific performance metrics for pitchers after biceps tenodesis and found no statistically significant change in ERA, WHIP, IP, games played, games started, losses, wins, shutouts, strikeouts, saves, walks allowed, hits allowed, or home runs allowed when comparing data from up to 144 months preoperatively with data from up to 36 months postoperatively.
PROM Scores
Analysis of PROM scores is presented in the Appendix.
Postoperative Rehabilitation Protocols
Analysis of postoperative rehabilitation protocols is presented in the Appendix.
Discussion
This systematic review and meta-analysis of 26 studies featuring a total of 1228 participants examined RTP, RTPP, and baseball-specific performance metrics after shoulder surgery in professional baseball players. RTP and RTPP rates were found to vary by surgical intervention within the shoulder, with the highest RTP and RTPP rates for LD/TM repair (84.5% and 100.0%, respectively) and the lowest RTP and RTPP rates for RCR (53.5% and 27.9%, respectively). In general, the RTP rate was substantially higher than the RTPP rate. Additionally, RTP and RTPP rates tended to be higher for position players than pitchers. Finally, for players who achieved RTPP after shoulder surgery, nonvolume performance metrics were preserved, but volume-based metrics decreased.
Postoperative athletic performance is of great concern to professional baseball players considering a surgical intervention for shoulder injuries. While numerous studies have examined rates of RTP and RTPP, as well as baseball-specific performance metrics, after specific shoulder surgical procedures, the current literature is lacking an up-to-date systematic review synthesizing the findings of these studies. In 2013, Harris et al 26 published a systematic review examining rates of return to sport in elite pitchers after shoulder surgery; 6 studies qualified for inclusion in that review, and the aggregate rate of return to sport among participants was found to be 68%. Since that time, an abundance of new RTP and RTPP data for professional baseball players undergoing shoulder surgery has become available, and a new systematic review and meta-analysis is required to better define current expectations of performance after shoulder surgery in professional baseball players.
Rates of RTP vary widely depending on the specific shoulder surgery performed. Encouraging rates of RTP were found for scapulothoracic bursectomy (100.0%), coracoclavicular ligament reconstruction and distal clavicle excision (93.3%), LD/TM repair (84.5%), and anterior capsular repair (80.0%), suggesting that professional baseball players who undergo these procedures have a reasonable chance of continuing to play baseball postoperatively. However, RTP rates declined substantially for procedures involving the labrum (75.0% for labral repair; 62.9% for SLAP repair) and fell even further for procedures involving the rotator cuff (59.4% for RCD, 53.5% for RCR). Therefore, it is important for providers and players to recognize preoperatively that RTP after labral and rotator cuff procedures is certainly not guaranteed.
For professional athletes, returning specifically to their prior level of play (represented by RTPP) is also of crucial importance. In general, the RTPP rate was found to be equivalent to or lower than the RTP rate. The one exception was for LD/TM repair, with an RTP rate of 84.5% and an RTPP rate of 100.0%. This paradoxical finding is attributable to a substantially lower number of participants with RTPP data and may be related to the fragility of a small cohort. RCD, RCR, and SLAP repair all demonstrated markedly lower rates of RTPP than RTP, with a difference of 13.2% for RCD, 25.6% for RCR, and 21.5% for SLAP repair, thus highlighting the importance of this distinction between RTP and RTPP. The RTPP rate for RCR was particularly discouraging at 27.9%, suggesting that a professional baseball player who requires surgical repair of the rotator cuff is statistically unlikely to return to his prior level of play.
While preserving shoulder function is certainly of great importance for all professional baseball players, pitchers arguably rely more heavily on elite shoulder function than position players. This distinction is evident in the RTP data; across all interventions, the RTP rate was lower for pitchers than for position players, and while these differences were not all statistically significant, this lack of significance is likely attributable to inadequate sample sizes. Similarly, the RTPP rate was found to be substantially lower in pitchers than in position players for most shoulder surgical procedures, although again, the statistical significance of these conclusions was limited by the sample size. Interestingly, while the Chalmers et al 6 study of 325 pitchers and 217 position players who underwent various shoulder surgical procedures demonstrated a significantly higher RTP rate in position players (55.1% vs 77.0%, respectively; P < .0001), the RTPP rate was actually higher in pitchers (44.9% vs 37.8%, respectively; P = .10), suggesting that pitchers were less likely to return to play at all but that those pitchers who did successfully return were more likely to return to their prior high level of play than their position player counterparts. Studies did not consistently report the specific positions of nonpitchers, although it is reasonable to posit that throwing-heavy positions such as a shortstop or catcher may be more significantly affected by shoulder surgery than less throwing-heavy positions such as a first baseman. It is important for providers and players considering shoulder surgery to understand that pitchers will generally experience inferior outcomes with regard to RTP and RTPP than position players and to factor this distinction into their decision-making process and setting of postoperative expectations.
While RTPP is useful for predicting a player’s successful RTP (or lack thereof) at his prior level, baseball-specific performance metrics arguably provide a more accurate and nuanced representation of a player’s postoperative performance. Overall, few differences were found between preoperative and postoperative baseball-specific performance metrics among professional baseball players who underwent shoulder surgery. There were no statistically significant changes reported for nonvolume pitching statistics, such as ERA and WHIP, suggesting that pitchers who returned after labral repair, LD/TM repair, RCD, RCR, SLAP repair, biceps tenodesis, and shoulder arthroscopic surgery performed at a level comparable with their preoperative capabilities. One study 14 did report a “slight” worsening of ERA in 3 of 5 pitchers who underwent RCR, but the statistical significance or lack thereof was not reported. Several studies did report a decrease in IP after surgery, although other studies reported no change in IP or other volume statistics after similar surgical procedures. Encouragingly, increases in IP and other volume statistics were reported after RCD by Erickson et al, 18 suggesting that RCD led to improved stamina and increased workloads for these players. Overall, the data suggest that players who return to play after shoulder surgery may expect to perform at a level that is reasonably comparable with their preoperative performance, although shoulder surgery may lead to a subsequent decrease in IP and a decrease in the amount of workload the player is able to tolerate. It is important to note that such optimistic expectations are applicable only to players who successfully return to play and that, as discussed extensively above, a significant portion of players who undergo shoulder surgery will fail to return to play, either at their prior level of play or at any level. It is equally important to consider that volume-based metrics are inherently biased postoperatively, as players are often placed on pitch limit/workload management when first returning from surgery, and that it is difficult to determine without a control group if any changes in performance postoperatively are a direct consequence of the surgical procedure itself or merely a result of not playing for the duration of the rehabilitation period.
This systematic review and meta-analysis has numerous strengths. First, the literature search and selection process were conducted rigorously, with multiple reviewers at each step. A total of 26 articles ultimately qualified for inclusion, a substantial improvement over Harris et al’s 26 most recent systematic review of elite baseball players after shoulder surgery, for which only 6 studies qualified. Over 1000 professional baseball players who underwent shoulder surgery were included in the 26 articles, and enough studies reported RTP and RTPP data after labral repair, LD/TM repair, RCD, RCR, and SLAP repair to enable a meta-analysis for these procedures. The comparison of RTP and RTPP between pitchers and position players is another strength of this study, as it is important to recognize that demands on the shoulders of pitchers and position players differ substantially. Overall, the conclusions drawn by this study are directly applicable to professional baseball players and their health care providers with regard to establishing reasonable expectations for outcomes after shoulder surgery.
Limitations
This study is not without weaknesses. There is a scarcity of data available on this topic, and while 26 studies were included in the review, many of these studies are hampered by small sample sizes, which limited the statistical significance of meta-analysis; this problem is difficult to combat in a cohort of professional baseball players that is inherently limited in size. Additionally, several procedures (biceps tenodesis, anterior capsular repair, coracoclavicular ligament reconstruction, distal clavicle excision, and scapulothoracic bursectomy) were featured in only 1 article, and meta-analysis was therefore unable to be performed for these poorly captured procedures. Interestingly, studies reporting on labral repair only intermittently specified the anatomic location of the repair site, and no studies specifically reported on anterior labral repair. As such, anterior shoulder procedures were poorly captured overall, and no significant conclusions can be drawn for these procedures that likely have a substantial impact on throwing performance. Furthermore, numerous studies were excluded from the review because they included both professional and nonprofessional baseball players but did not stratify their data by level of play. It is also important to note that the surgical interventions included in this study occurred over a wide range of dates, from 1976 to 2016. While the majority of surgical procedures were performed more recently (2000 or later), it is imperative to acknowledge that surgical techniques, indications, rehabilitation strategies, and athletic demands of sports change over time and that outcome data from prior decades may not be generalizable to athletes today. Overall, it is clear that to better understand performance outcomes after shoulder surgery in contemporary professional baseball players, additional studies are required with larger sample sizes and more consistent stratification of data by level of play. Finally, while outside the scope of this article, future studies should also aim to compare performance outcomes after the surgical versus nonsurgical management of shoulder injuries in professional baseball players, as studies that qualified for this review did not consistently address this issue.
Conclusion
RTP and RTPP rates among professional baseball players were modest after most types of shoulder surgery. Among surgical procedures commonly performed in professional baseball players, RTP and RTPP rates were highest for LD/TM repair and lowest for RCR. These data enable providers caring for professional baseball players to establish realistic evidence-based expectations for RTP and RTPP after shoulder surgery in this patient population.
APPENDIX
Search Algorithm
((shoulder[Title/Abstract]) OR (rotator cuff[Title/Abstract]) OR (labral[Title/Abstract]) OR (labrum[Title/Abstract]) OR (biceps[Title/Abstract]) OR (biceps tenodesis[Title/Abstract]) OR (latissimus dorsi[Title/Abstract]) OR (teres major[Title/Abstract]) OR (SLAP [Title/Abstract]) OR (instability[Title/Abstract]) OR (repair[Title/Abstract])) AND
((outcomes[Title/Abstract]) OR (return to play[Title/Abstract]) OR (return to sport[Title/Abstract]) OR (competitive play[Title/Abstract])) AND ((baseball[Title/Abstract]) OR (pitcher[Title/Abstract]) OR (catcher[Title/Abstract]) OR (field player[Title/Abstract]) OR (MLB[Title/Abstract]) OR (Major League[Title/Abstract]) OR (Major League Baseball(Title/Abstract])) AND (english[Language])
Analysis of PROM Scores
In total, 7 studies 15,19,24,29,33,38,41 reported PROM scores with respect to professional baseball players undergoing shoulder surgery. PROMs featured in these studies included the American Shoulder and Elbow Surgeons (ASES) score, Western Ontario Shoulder Instability Index (WOSI), Veterans RAND 12-Item Health Survey (VR-12), visual analog scale (VAS) for pain, Kerlan-Jobe Orthopaedic Clinic (KJOC) score, and Athletic Shoulder Outcome Rating Scale (ASORS).
Douglas et al 15 investigated WOSI scores among players who underwent SLAP repair and found that those players with successful RTPP had significantly higher WOSI scores as well as significantly lower individual physical, sports, lifestyle, and emotion domain scores than those who did not achieve RTPP. These authors also demonstrated that pitchers reported significantly lower VR-12 physical scores postoperatively than nonpitchers. Gilliam et al 24 also examined PROM scores after SLAP repair and reported a statistically significant increase in WOSI scores and VR-12 physical scores in players with successful RTP compared with those who did not achieve RTP, although neither difference reached clinical significance. Park et al 38 reported a significant improvement in both VAS pain scores and ASES scores after SLAP repair.
Kercher et al 29 reported a statistically significant improvement in ASES scores from 65.4 points preoperatively to 96.3 points after labral repair. Erickson et al 19 reported excellent ASES, VAS pain, and KJOC scores after LD/TM repair; all 7 participants reported a VAS pain score of 0.0 and an ASES score of 100, and the average KJOC score was 89. Reynolds et al 41 reported ASORS scores after RCD and found that 52.9% of participants had excellent outcomes, 23.5% had good outcomes, 11.7% had fair outcomes, and 11.7% had poor outcomes. Mazoue and Andrews 33 examined ASORS scores after RCR, finding that those players with successful RTPP had scores in the “excellent” range, whereas those with failed RTPP scored in the “poor” range.
Analysis of Postoperative Rehabilitation Protocols
A total of 12 studies †† commented on postoperative rehabilitation protocols. Overall, 5 studies reported rehabilitation protocols for SLAP repair. Douglas et al 15 described a 6- to 9-month protocol featuring progressive glenohumeral joint range of motion via discrete phases of incrementally decreasing protection. Patients in the Park et al 38 study were immobilized in abduction for 6 weeks, followed by 3 weeks of gentle passive range of motion and a subsequent 3 weeks of active-assisted range of motion; participants were allowed to throw beginning at 6 months postoperatively and allowed to return to play at 9 months postoperatively. In contrast, Park and Glousman 39 reported sling immobilization for 7 to 10 days, formal physical therapy for passive range of motion and isometric strengthening at 2 weeks, and full range of motion by 6 to 8 weeks, followed by progressive strengthening through 12 to 16 weeks. Neuman et al 37 required sling immobilization for 3 weeks postoperatively and allowed active range of motion after 1 month, throwing after 4 months, and throwing from a mound after 6 months. Cohen et al 10 reported only that rehabilitation was performed under the guidance of the major league team’s medical staff.
There were 2 studies that reported rehabilitation protocols for labral repair. Kercher et al 29 reported sling immobilization with an allowance for light activities of daily living for 3 weeks after posterior labral repair, with range of motion exercises starting at 3 weeks, resistive exercises starting at 6 weeks, batting off a tee and throwing at 4 months, and unrestricted activities at 6 months. In contrast, Wanich et al 49 utilized sling immobilization for 2 weeks after posterior labral repair and allowed passive range of motion from 2 to 6 weeks, active range of motion at 6 weeks, active strengthening at 12 weeks, and batting against live pitching at 6 months.
There were 2 studies that reported rehabilitation protocols for LD/TM repair. Patients in the Erickson et al 17 study were immobilized in an abduction sling for 6 weeks postoperatively, although gentle pendulum exercises and passive range of motion exercises were allowed beginning at 2 weeks, active range of motion was initiated at 6 weeks, throwing was initiated between 12 and 16 weeks, and RTP was allowed no earlier than 6 months. Ellman et al 16 described a similar rehabilitation program, with abduction sling immobilization for 6 weeks, passive range of motion exercises from 2 to 6 weeks, the addition of active range of motion at 6 weeks, light throwing between 12 and 16 weeks, and full return to pitching between 20 and 30 weeks.
Additionally, 2 studies reported rehabilitation protocols for RCR. Dines et al 14 reported sling immobilization for 4 weeks, passive shoulder range of motion in the scapular plane at 4 weeks, active-assisted shoulder exercises at 6 weeks, isometric strengthening at 8 weeks, eccentric strengthening and weight training at 3 months, and the initiation of a throwing program at 24 weeks. Mazoue and Andrews 33 also reported immobilization for 4 to 6 weeks, followed by adherence to “standard rehabilitation protocols for surgical treatment of full-thickness rotator cuff tears” and subsequent progression to a supervised throwing program with an initial phase of flat-ground throwing before throwing off a mound.
Gulotta et al 25 reported a rehabilitation protocol after anterior capsular repair featuring shoulder immobilization for 3 weeks with an allowance of passive elevation in the scapular plane, active-assisted shoulder range of motion from 4 to 8 weeks, aggressive strengthening from 8 to 16 weeks, and an interval throwing program at 16 weeks.
Footnotes
Final revision submitted September 13, 2022; accepted September 16, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: E.M.F. has received education payments from Kairos Surgical. P.D.A. has received education payments from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Brockmeier SF, Voos JE, Williams RJ, 3rd, et al. Outcomes after arthroscopic repair of type-II SLAP lesions. J Bone Joint Surg Am. 2009;91(7):1595–1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404–420. [DOI] [PubMed] [Google Scholar]
- 3. Bushnell BD, Anz AW, Noonan TJ, Torry MR, Hawkins RJ. Association of maximum pitch velocity and elbow injury in professional baseball pitchers. Am J Sports Med. 2010;38(4):728–732. [DOI] [PubMed] [Google Scholar]
- 4. Camp CL, Dines JS, van der List JP, et al. Summative report on time out of play for Major and Minor League Baseball: an analysis of 49,955 injuries from 2011 through 2016. Am J Sports Med. 2018;46(7):1727–1732. [DOI] [PubMed] [Google Scholar]
- 5. Cerynik DL, Ewald TJ, Sastry A, Amin NH, Liao JG, Tom JA. Outcomes of isolated glenoid labral injuries in professional baseball pitchers. Clin J Sport Med. 2008;18(3):255–258. [DOI] [PubMed] [Google Scholar]
- 6. Chalmers PN, Erickson BJ, D’Angelo J, Ma K, Romeo AA. Epidemiology of shoulder surgery among professional baseball players. Am J Sports Med. 2019;47(5):1068–1073. [DOI] [PubMed] [Google Scholar]
- 7. Chalmers PN, Erickson BJ, Verma NN, D’Angelo J, Romeo AA. Incidence and return to play after biceps tenodesis in professional baseball players. Arthroscopy. 2018;34(3):747–751. [DOI] [PubMed] [Google Scholar]
- 8. Chambless KM, Knudtson J, Eck JC, Covington LA. Rate of injury in Minor League Baseball by level of play. Am J Orthop (Belle Mead NJ). 2000;29(11):869–872. [PubMed] [Google Scholar]
- 9. Cohen DB, Coleman S, Drakos MC, et al. Outcomes of isolated type II SLAP lesions treated with arthroscopic fixation using a bioabsorbable tack. Arthroscopy. 2006;22(2):136–142. [DOI] [PubMed] [Google Scholar]
- 10. Cohen SB, Sheridan S, Ciccotti MG. Return to sports for professional baseball players after surgery of the shoulder or elbow. Sports Health. 2011;3(1):105–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Conte S, Camp CL, Dines JS. Injury trends in Major League Baseball over 18 seasons: 1998-2015. Am J Orthop (Belle Mead NJ). 2016;45(3):116–123. [PubMed] [Google Scholar]
- 12. Conte S, Requa RK, Garrick JG. Disability days in Major League Baseball. Am J Sports Med. 2001;29(4):431–436. [DOI] [PubMed] [Google Scholar]
- 13. Crockett HC, Gross LB, Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30(1):20–26. [DOI] [PubMed] [Google Scholar]
- 14. Dines JS, Jones K, Maher P, Altchek D. Arthroscopic management of full-thickness rotator cuff tears in Major League Baseball pitchers: the lateralized footprint repair technique. Am J Orthop (Belle Mead NJ). 2016;45(3):128–133. [PubMed] [Google Scholar]
- 15. Douglas L, Whitaker J, Nyland J, et al. Return to play and performance perceptions of baseball players after isolated SLAP tear repair. Orthop J Sports Med. 2019;7(3):2325967119829486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ellman MB, Yanke A, Juhan T, et al. Open repair of an acute latissimus tendon avulsion in a Major League Baseball pitcher. J Shoulder Elbow Surg. 2013;22(7):e19–e23. [DOI] [PubMed] [Google Scholar]
- 17. Erickson BJ, Chalmers PN, D’Angelo J, Ma K, Romeo AA. Performance and return to sport after latissimus dorsi and teres major tears among professional baseball pitchers. Am J Sports Med. 2019;47(5):1090–1095. [DOI] [PubMed] [Google Scholar]
- 18. Erickson BJ, Chalmers PN, D’Angelo J, Ma K, Romeo AA. Performance and return to sport following rotator cuff surgery in professional baseball players. J Shoulder Elbow Surg. 2019;28(12):2326–2333. [DOI] [PubMed] [Google Scholar]
- 19. Erickson BJ, Chalmers PN, Waterman BR, Griffin JW, Romeo AA. Performance and return to sport in elite baseball players and recreational athletes following repair of the latissimus dorsi and teres major. J Shoulder Elbow Surg. 2017;26(11):1948–1954. [DOI] [PubMed] [Google Scholar]
- 20. Fares MY, Fares J, Baydoun H, Fares Y. Prevalence and patterns of shoulder injuries in Major League Baseball. Phys Sportsmed. 2020;48(1):63–67. [DOI] [PubMed] [Google Scholar]
- 21. Fedoriw WW, Ramkumar P, McCulloch PC, Lintner DM. Return to play after treatment of superior labral tears in professional baseball players. Am J Sports Med. 2014;42(5):1155–1160. [DOI] [PubMed] [Google Scholar]
- 22. Ferrari JD, Ferrari DA, Coumas J, Pappas AM. Posterior ossification of the shoulder: the Bennett lesion: etiology, diagnosis, and treatment. Am J Sports Med. 1994;22(2):171–175, discussion 175-176. [DOI] [PubMed] [Google Scholar]
- 23. Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23(2):233–239. [DOI] [PubMed] [Google Scholar]
- 24. Gilliam BD, Douglas L, Fleisig GS, et al. Return to play and outcomes in baseball players after superior labral anterior-posterior repairs. Am J Sports Med. 2018;46(1):109–115. [DOI] [PubMed] [Google Scholar]
- 25. Gulotta LV, Lobatto D, Delos D, Coleman SH, Altchek DW. Anterior shoulder capsular tears in professional baseball players. J Shoulder Elbow Surg. 2014;23(8):e173–e178. [DOI] [PubMed] [Google Scholar]
- 26. Harris JD, Frank JM, Jordan MA, et al. Return to sport following shoulder surgery in the elite pitcher: a systematic review. Sports Health. 2013;5(4):367–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Higgins MJ, DeFroda S, Yang DS, Brown SM, Mulcahey MK. Professional athlete return to play and performance after shoulder arthroscopy varies by sport. Arthrosc Sports Med Rehabil. 2021;3(2):e391–e397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jobe CM. Superior glenoid impingement: current concepts. Clin Orthop Relat Res. 1996;330:98–107. [PubMed] [Google Scholar]
- 29. Kercher JS, Runner RP, McCarthy TP, Duralde XA. Posterior labral repairs of the shoulder among baseball players: results and outcomes with minimum 2-year follow-up. Am J Sports Med. 2019;47(7):1687–1693. [DOI] [PubMed] [Google Scholar]
- 30. Kirchhoff C, Imhoff AB. Posterosuperior and anterosuperior impingement of the shoulder in overhead athletes: evolving concepts. Int Orthop. 2010;34(7):1049–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Laudner K, Meister K, Noel B, Deter T. Anterior glenohumeral laxity is associated with posterior shoulder tightness among professional baseball pitchers. Am J Sports Med. 2012;40(5):1133–1137. [DOI] [PubMed] [Google Scholar]
- 32. Liu JN, Garcia GH, Weeks KD, et al. Treatment of grade III acromioclavicular separations in professional baseball pitchers: a survey of Major League Baseball team physicians. Am J Orthop (Belle Mead NJ). 2018;47(7). doi: 10.12788/ajo.2018.0051 [DOI] [PubMed] [Google Scholar]
- 33. Mazoue CG, Andrews JR. Repair of full-thickness rotator cuff tears in professional baseball players. Am J Sports Med. 2006;34(2):182–189. [DOI] [PubMed] [Google Scholar]
- 34. Moher D, Liberati A, Tetzlaff J, Altman DG; the PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6(6):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Namdari S, Baldwin K, Ahn A, Huffman GR, Sennett BJ. Performance after rotator cuff tear and operative treatment: a case-control study of Major League Baseball pitchers. J Athl Train. 2011;46(3):296–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Neri BR, ElAttrache NS, Owsley KC, Mohr K, Yocum LA. Outcome of type II superior labral anterior posterior repairs in elite overhead athletes: effect of concomitant partial-thickness rotator cuff tears. Am J Sports Med. 2011;39(1):114–120. [DOI] [PubMed] [Google Scholar]
- 37. Neuman BJ, Boisvert CB, Reiter B, Lawson K, Ciccotti MG, Cohen SB. Results of arthroscopic repair of type II superior labral anterior posterior lesions in overhead athletes: assessment of return to preinjury playing level and satisfaction. Am J Sports Med. 2011;39(9):1883–1888. [DOI] [PubMed] [Google Scholar]
- 38. Park JY, Chung SW, Jeon SH, Lee JG, Oh KS. Clinical and radiological outcomes of type 2 superior labral anterior posterior repairs in elite overhead athletes. Am J Sports Med. 2013;41(6):1372–1379. [DOI] [PubMed] [Google Scholar]
- 39. Park S, Glousman RE. Outcomes of revision arthroscopic type II superior labral anterior posterior repairs. Am J Sports Med. 2011;39(6):1290–1294. [DOI] [PubMed] [Google Scholar]
- 40. Posner M, Cameron KL, Wolf JM, Belmont PJ, Jr, Owens BD. Epidemiology of Major League Baseball injuries. Am J Sports Med. 2011;39(8):1676–1680. [DOI] [PubMed] [Google Scholar]
- 41. Reynolds SB, Dugas JR, Cain EL, McMichael CS, Andrews JR. Debridement of small partial-thickness rotator cuff tears in elite overhead throwers. Clin Orthop Relat Res. 2008;466(3):614–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ricchetti ET, Weidner Z, Lawrence JT, Sennett BJ, Huffman GR. Glenoid labral repair in Major League Baseball pitchers. Int J Sports Med. 2010;31(4):265–270. [DOI] [PubMed] [Google Scholar]
- 43. Sisto DJ, Jobe FW. The operative treatment of scapulothoracic bursitis in professional pitchers. Am J Sports Med. 1986;14(3):192–194. [DOI] [PubMed] [Google Scholar]
- 44. Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J. Surg. 2003;73:712–716. [DOI] [PubMed] [Google Scholar]
- 45. Smith R, Lombardo DJ, Petersen-Fitts GR, et al. Return to play and prior performance in Major League Baseball pitchers after repair of superior labral anterior-posterior tears. Orthop J Sports Med. 2016;4(12):2325967116675822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Statista. Average TV viewership of Major League Baseball World Series Games in the United States from 2000 to 2020. Accessed October 2, 2021. https://www.statista.com/statistics/235678/world-series-tv-viewership-in-the-united-states/
- 47. Tehranzadeh AD, Fronek J, Resnick D. Posterior capsular fibrosis in professional baseball pitchers: case series of MR arthrographic findings in six patients with glenohumeral internal rotational deficit. Clin Imaging. 2007;31(5):343–348. [DOI] [PubMed] [Google Scholar]
- 48. Walch G, Liotard JP, Boileau P, Noel E. Postero-superior glenoid impingement: another impingement of the shoulder. J Radiol. 1993;74(1):47–50. [PubMed] [Google Scholar]
- 49. Wanich T, Dines J, Dines D, Gambardella RA, Yocum LA. “Batter’s shoulder”: can athletes return to play at the same level after operative treatment? Clin Orthop Relat Res. 2012;470(6):1565–1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wyland DJ, Pill SG, Shanley E, et al. Bony adaptation of the proximal humerus and glenoid correlate within the throwing shoulder of professional baseball pitchers. Am J Sports Med. 2012;40(8):1858–1862. [DOI] [PubMed] [Google Scholar]