Abstract
Background
To evaluate the long-term outcome after re-attempt CTO-PCI.
Methods
This is a retrospective cohort study that included 113 re-attempt CTO-PCI patients who were consecutively registered from January 2019 to December 2020 at Beijing Anzhen Hospital's Center of Coronary Artery Disease. All patients were divided into two groups based on procedural success or failure. The primary endpoint was major adverse cardiac events (MACE), a composite of all-cause mortality, myocardial infarction and target vessel revascularization (TVR). The secondary endpoint was angina after PCI.
Results
Overall, the successful re-attempt CTO-PCI was archived in 77 patients, the failed CTO-PCI was performed in 36 patients. After a median follow-up of 21.7 months (interquartile range: 10.9–26.0), the incidence of the primary outcome was significantly lower in the success group [14.2% vs. 38.9%, adjusted hazard ratio (HR) 0.351, 95% CI 0.134–0.917, P = 0.033], mainly driven by the reduction of TVR (9.1% vs. 30.6%, adjusted HR 0.238, 95% CI: 0.078–0.72, P = 0.011). Furthermore, patients who had successful re-attempt CTO-PCI had a lower risk of angina after PCI (27.3% vs.61.1%, adjusted HR 0.357, 95% CI 0.167–0.76, P = 0.008). The risk factors of TVR in the patients with successful re-attempt CTO-PCI were stent length > 100 mm (adjusted HR 21.805, 95% CI 1.765–269.368, P = 0.016) and J-CTO score > 3(adjusted HR: 9.733, 95% CI:1.533–61.797, P = 0.016).
Conclusions
For the patients with previous CTO-PCI failure, a successful re-attempt CTO-PCI was associated with significantly lower MACE, which was primarily driven by a lower TVR rate. More complex CTO lesions and longer stents were the independent predictors of TVR after successful CTO-PCI.
Keywords: Chronic total occlusion, Percutaneous coronary intervention, Long-term outcomes, TVR, MACE
Background
With the introduction of novel devices and techniques, the success rate of chronic total occlusion (CTO)-percutaneous coronary intervention (PCI) has increased considerably [1]. Interventional revascularization was frequently considered for patients with CTO lesions. However, approximately 21% of patients did not have their arteries reopened, and this group should not be neglected. Furthermore, the prognosis for these patients was previously considered poor, and it is unknown whether re-attempting CTO-PCI can enhance the clinical outcome [2, 3]. Thus, we conducted this study to determine the long-term prognosis for the patients who had re-attempt CTO-PCI.
Methods
Patient population
The patients who received re-attempt CTO-PCI at Center of Coronary Artery Disease, Capital medical university, Beijing Anzhen Hospital, Beijing, China, between January 2019 and December 2020 were enrolled in this retrospective cohort study. Inclusion criteria were age > 18 years old, at least one native coronary artery occlusion, anginal symptoms and myocardial viability or ischemia in the territory of the occluded artery. Exclusion criteria were the estimated duration of a total occlusion less than three months, acute myocardial infarction (MI), venous grafts as target occluded vessels, side branch occlusion (i.g. diagonal or marginal branches), and life expectancy < 1 year. The optimal medical therapy was provided to all patients. All CTO-PCI procedures were performed by high-volume operators with significant experience in CTO-PCI. The study protocol fulfilled the ethical guidelines of the 1975 Declaration of Helsinki. This study was approved by the institutional ethics committee of Beijing Anzhen Hospital.
Patients were categorized into two groups according to procedural results: (1) success group, (2) failure group. The clinical data were gathered retrospectively through a review of hospital records by physicians. J-CTO (Multicenter CTO Registry in Japan) score and procedural data were retrospectively evaluated by experienced physicians. Clinical follow-up after discharge was frequently performed by telephone interviews or outpatient visits. Follow-up visits were set up every three months for the first year following discharge. Follow-up visits were arranged every 6 months for more than a year following discharge. During the follow-up visit, data on angina, mortality and MI, as well as target vessel revascularization (TVR) were obtained.
Definitions and endpoints
A CTO was defined as a total obstruction of a native coronary artery with thrombolysis in myocardial infarction (TIMI) flow vessel grade 0 for a duration greater than 3 months. Calcification and bending was defined according to the definition in J-CTO score sheet [4]. Procedural success was defined as technical success without any in hospital adverse events. In hospital adverse events included all-cause death, Q-wave MI, stroke, recurrent angina requiring TVR with PCI, or coronary artery bypass grafting (CABG). Angina was defined as typical symptoms with a corresponding change in electrocardiogram or stress test. Angina after PCI was defined as ischemia induced chest discomfort, including recurrent angina, residual angina and CTO target vessel related angina. MI was defined according to the fourth universal definition of myocardial infarction [5]. Multi-vessel disease (MVD) was defined as a stenosis > 70% of the coronary lumen diameter in ≥ 2 of major epicardial arteries in vessels ≥ 2.5 mm or a left main stenosis > 50%. Complete revascularization was defined as treating all lesions with ≥ 50% stenosis in major epicardial coronary vessels at the index hospitalization. TVR was defined as any repeat recanalization (PCI or CABG) of any segment of the target treated CTO vessel. The primary endpoint was the major adverse cardiac events (MACE) and it was defined as a composite of all-cause mortality, MI and TVR. The secondary endpoint was angina after PCI.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation or median (inter quartile range, IQR) and compared using the student’s t-test or Mann–Whitney U test. Categorical variables were presented as numbers and percentages (%) and compared using Chi-square test or Fisher’s exact test. To determine event-free survival, the Cox proportional hazards model was utilized. Age, hypertension, ejection fraction less than 50%, calcification, MVD, J-CTO > 3, reference vessel diameter, retrograde approach were all taken into account when calculating adjusted hazard ratios(HR) and 95 percent confidence intervals(CI).Cox regression analysis was utilized to select covariates that were linked with an increased incidence of TVR following successful recanalization.The variables with P value < 0.10 on univariate analysis or clinical significance were included in the multivariate regression. A two-sided P value < 0.05 was considered statistically significant. SPSS 25.0 (IBM, USA) was applied for all statistical analyses.
Results
Baseline characteristic
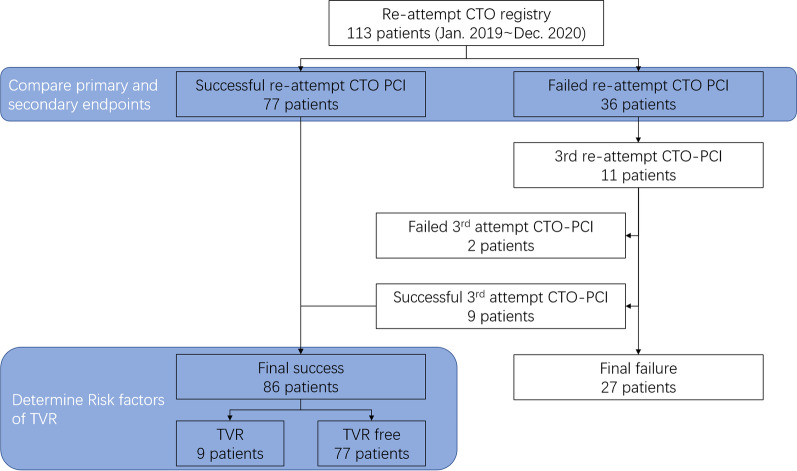
Baseline characteristics of the study participants were reported in Table 1. Among 113 consecutive patients who underwent re-attempt CTO-PCI in our center, procedural success was obtained in 77 patients whereas the procedure failed in 36 patients (Fig. 1). Patients with successful procedure had less frequent hypertension, while no difference in age, sex, body mass index, history of diabetes, lipid disorder, chronic kidney disease, previous MI, previous CABG and smoking.
Table 1.
Baseline and procedural characteristics
| Success (n = 77) | Failure (n = 36) | P value | |
|---|---|---|---|
| Age | 57.86 ± 10.30 | 59.44 ± 10.38 | 0.448 |
| Male | 64 (83.1%) | 33 (91.7%) | 0.225 |
| BMI | 26.78 ± 5.65 | 26.65 ± 3.91 | 0.898 |
| Hypertension | 51 (66.2%) | 32 (88.9%) | 0.011 |
| Diabetes | 30 (39.0%) | 11 (30.6%) | 0.387 |
| Lipid disorder | 61 (79.2%) | 30 (83.3%) | 0.607 |
| CKD | 6 (7.8) | 4 (11.1%) | 0.723 |
| Previous MI | 21 (27.2%) | 13 (36.1%) | 0.340 |
| Previous CABG | 2 (2.6%) | 2 (5.6%) | 0.591 |
| Smoking | 38 (49.4%) | 17 (47.2%) | 0.833 |
| CTO target vessel | 0.225 | ||
| LAD | 30 (39.0%) | 15 (41.7%) | |
| LCX | 4 (5.2%) | 5 (13.9%) | |
| RCA | 43 (55.8%) | 16 (44.4%) | |
| MVD | 50 (64.9%) | 24 (66.7%) | 0.927 |
| Retrograde approach | 35 (45.5%) | 14 (38.9%) | 0.512 |
| EF ≤ 50% | 10 (13.0%) | 3 (8.3%) | 0.546 |
| Duration since last attempt ≥ 3 months | 36 (46.8%) | 21 (58.3%) | 0.251 |
| CTO segment length ≥ 20 mm | 30 (39.0%) | 21 (58.3%) | 0.054 |
| Calcification | 29 (37.7%) | 24 (66.7%) | 0.004 |
| Bending | 20 (26.0%) | 8 (22.2%) | 0.667 |
| Tapered proximal cap | 34 (44.2%) | 11 (30.6%) | 0.169 |
| J-CTO score > 3 | 16 (20.8%) | 16 (44.4%) | 0.009 |
| Reference vessel diameter | 2.71 ± 0.41 | 2.42 ± 0.55 | 0.002 |
| Bifurcation | 51 (66.2%) | 29 (80.6%) | 0.119 |
| ISR | 4 (5.2%) | 3 (8.3%) | 0.519 |
| Stent implantation | 76 (98.7%) | – | |
| Stent length > 100 mm | 10 (13.0%) | – | |
| Re-attempt failure reason | |||
| GW failure | 31 (86.1%) | ||
| Device failure | 2 (5.6%) | ||
| Complication | 3 (8.3%) | ||
Values are mean ± standard deviation, or n(%). BMI body mass index; CKD chronic kidney disease; MI myocardial infarction; CABG coronary artery bypass graft; CTO chronic total occlusion; LAD left anterior descending; LCX left circumflex; RCA right coronary artery; MVD multi-vessel disease; EF ejection franction; ISR in-stent restenosis
Fig. 1.
Study flowchart. CTO: chronic total occlusion; PCI: percutaneous coronary intervention; TVR: target vessel revascularization
Angiographic characteristics were presented in Table 1. Presence of calcification and J-CTO score > 3 was more frequent in failure group (66.7% vs. 37.7%, P = 0.004, 44.4% vs. 20.8%, P = 0.009, respectively). Larger reference vessel diameter was observed in failure group (2.71 ± 0.41 mm vs. 2.42 ± 0.55 mm, P = 0.002). 55 out of 77 patients (71.4%) received complete revascularization in the success group.
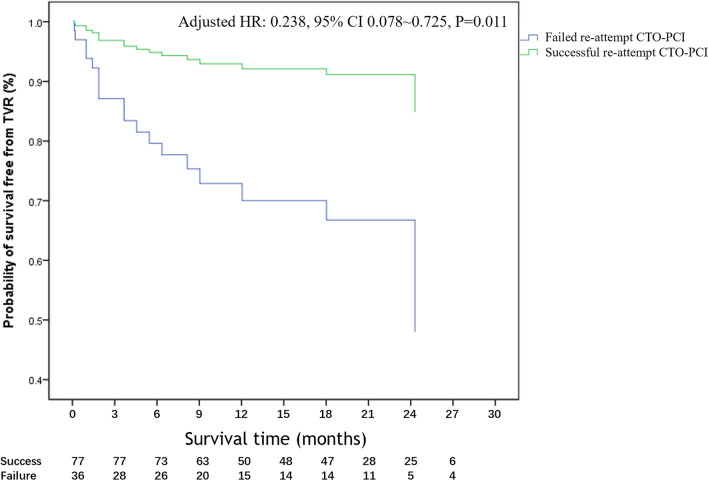
Clinical outcomes and follow-up
Table 2 shows occurrence rates for the success and failure groups using Cox proportional hazards regression. All of the patients in this research were followed up in person or by phone. With in one year of discharge, 47.8% of patients had attended the hospital for their follow-up, and after one year, most patient had telephone follow-up. Because of the outbreak of COVID-19, other patients who did not dwell in Beijing were contacted by phone. The median follow-up time was 21.7 months (IQR 10.9–26.0). 25 patients were adjudicated to have all-cause mortality, MI or TVR. MACE were significantly lower in the success group than in the failure group (14.2% vs. 38.9%, adjusted hazard ratio (HR): 0.351, 95% CI 0.134–0.917. P = 0.033). The significant reduction of MACE in the success group was mainly driven by the improved outcome of TVR (9.1% vs. 30.6%, adjusted HR: 0.238, 95% CI 0.078–0.724, P = 0.011, Fig. 2). Subsequent PCI was underwent to achieved TVR. There was no statistically significant difference in all-cause mortality and MI in our analysis. During the follow-up period, patients who had a successful re-attempt CTO-PCI had fewer angina after PCI than those who had a failed operation (27.3% vs.61.1%, adjusted HR 0.357, 95% CI 0.167–0.762, P = 0.011).
Table 2.
Cumulative event rates between patients with different results
| Success (n = 77) | Failure (n = 36) | Adjusted HR (95% CI) | P value | |
|---|---|---|---|---|
| MACE | 11 (14.2%) | 14 (38.9%) | 0.351 (0.134–0.917) | 0.033 |
| All-cause mortality | 3 (3.9%) | 5 (13.9%) | 0.782 (0.113–5.400) | 0.803 |
| MI | 5 (6.5%) | 2 (5.6%) | 5.609 (0.478–65.881) | 0.170 |
| TVR | 7 (9.1%) | 11 (30.6%) | 0.238 (0.078–0.724) | 0.011 |
| Angina after PCI | 21 (27.3%) | 22 (61.1%) | 0.357 (0.167–0.762) | 0.008 |
Adjusted covariates: age, hypertension, EF ≤ 50%, MVD, calcification, J-CTO score > 3, retrograde approach and reference vessel diameter. MACE major adverse cardiac event; MI myocardial infarction; TVR target vessel revascularization
Fig. 2.
Kaplan–Meier event-free survival curve of TVR. CI: confidence intervals; CTO: chronic total occlusion; HR: hazard ratio; PCI: percutaneous coronary intervention; TVR: target vessel revascularization
Risk factor of TVR after success CTO recanalization
Eleven patients in the failure group had a third CTO-PCI attempt due to their prolonged anginal symptoms after PCI, and in some cases, patients requested (Fig. 2). Because of successful recanalization, 9 of them were reclassified to the success group. Overall, 76.1 percent of the procedures were successful. Of the 86 patients who ultimately had a successful re-attempt CTO-PCI, 9 (10.5%) had a TVR, 7 of 77 had successful recanalization on the second attempt, and 2 of 9 had successful recanalization on the third attempt. A COX regression analysis was used to determine the independent predictor of TVR after successful CTO recanalization. After adjusted covariates, the independent risk factors included J-CTO score > 3 and stent length > 100 mm were significant (Table 3; p < 0.05).
Table 3.
Multivariate Cox regression analyses assess the risk factors of TVR in 86 cases with successful percutaneous revascularization
| Adjusted HR (95% CI) | P value | |
|---|---|---|
| Age | 0.924 (0.829–1.029) | 0.151 |
| Hypertension | 1.713 (0.189–15.523) | 0.632 |
| J-CTO > 3 | 9.733 (1.533–61.797) | 0.016 |
| MVD | 3.557 (0.388–32.592) | 0.261 |
| Retrograde approach | 3.180 (0.319–31.655) | 0.324 |
| EF ≤ 50% | 2.464 (0.165–36.792) | 0.513 |
| Stent length > 100 mm | 21.805 (1.765–269.368) | 0.016 |
| Vessel reference diameter | 0.750 (0.061–9.232) | 0.822 |
MVD multi vessel disease. EF ejection fraction
Discussion
The success rate of CTO-PCI and prognosis are currently unsatisfactory, particularly for re-attempt procedures. This retrospective observational study evaluated the outcomes and MACE rate after successful or failed re-attempt CTO-PCI. The main finding of this study was that successful re-attempt recanalization dramatically reduced MACE and alleviated symptoms of angina. We also demonstrated that the stent length > 100 mm and J-CTO score > 3 were risk factors for TVR following a successful re-attempt CTO-PCI.
Angina after PCI The symptom of angina and quality of life (QoL) can be improved by CTO-PCI [6]. The presence of angina was also an indication of percutaneous recanalization [7]. A meta-analysis encompassed 7288 patients and observed an average of 6 years of follow-up time conducted [8]. The prognosis following successful vs. failed CTO-PCI was examined in this study. Successful recanalization was associated with a significant reduction in residual/recurrent angina (OR = 0.45, 95% CI 0.30–0.67) and subsequent CABG surgery (OR = 0.22, 95% CI 0.17–0.27). Moreover, compared to non-successful PCI, a recent meta-analysis showed a significant improvement in Seattle Angina Questionnaire(SAQ)- QoL post successful PCI [9]. Borgia et al. [10] observed 302 patients with CTO-PCI, 78% of patients had a successful procedure. This trial revealed that after a median follow-up of 4 years the CTO recanalization significantly improved the angina-related QoL than before (82 vs. 53, P < 0.05). In the success group of our study, the ischemia was mitigated and the symptoms of angina were alleviated immediately after recanalization. After nearly three years of follow-up, the incidence of angina after PCI in the success group was remained statistically lower than in the failure group. We also discovered that angina after PCI was the most common reason for patients receiving the third attempt. In our study, 11 patients in the failure group underwent a third attempt. Nine of them were successfully reopened the CTO target vessel. Therefore, we argued that re-attempt CTO-PCI should still be recommended for patients who had a prior failed CTO and have clear evidence of ischemia. In patients who have had a successful re-attempt CTO-PCI, the emergence of angina pectoris is linked to incomplete revascularization, but it may also be linked to the incidence of target vessel failure.
MACE and TVR Failed CTO recanalization not only affected the patients’ QoL, but it also increased the risk of MACE. The long-term effects of successful CTO recanalization were the subject of debate. In most observational studies, successful CTO-PCI has been shown to improve patients' long-term MACE. A meta-analysis of 25 observational studies compared the long-term outcomes of successful versus failed CTO-PCI, and the findings revealed that successful CTO-PCI was associated with lower mortality [6]. Regardless of the quality of the collateral circulation, Jang et al. [11] observed a lower incidence of MACE after aggressive revascularization as compared with optimal medical therapy (OMT) alone. In contrast, the DECISION-CTO trial, which involved over 800 patients with CTO and was the first randomised controlled trial, came up with a negative outcome [1]. In this trial, the primary endpoint was the three-year rate of MACE (all-cause death, MI, stroke and revascularization). The incidence of MACE in PCI + OMT group was 20.6%, while OMT group was 19.6% (P = 0.008 for non-inferiority). There was also no difference in the evaluation of QoL. These results and conclusions were challenged due to delayed and incomplete patient recruitment, revascularization of other non-occlusive lesions in addition to CTO-PCI after randomization and baseline health status assessment, a high crossover rate to the PCI group (15–20%), and the inclusion of periprocedural MI in the primary outcome. Our research supports the hypothesis that CTO recanalization can improve MACE. The current study found that after a mean follow-up of 21.7 months, the incidence of MACE were significantly lower in the success group than in the failure group. MACE were reduced predominantly as a result of decreased TVR, whereas death and MI rates were comparable across the two groups.
Risk factors of TVR This study demonstrated that J-CTO score > 3 and stent length > 100 mm as the risk factor of TVR after successful re-attempt CTO recanalization. J-CTO score which as the earliest scoring system was frequently utilized in daily clinical practice [4], J-CTO score > 3 was considered as a very difficult lesion. Abe et al. argued that J-CTO score can predict the prognosis of patients with CTO [12]. In a five years follow-up study involving over 2000 patients, J-CTO score and residual SYNTAX score were independently associated to TVR (HR, 1.31; 95% CI: 1.11–1.54; P < 0.01) [13]. However, a small observational study enrolled only 93 patients identified that reduced TIMI flow of target vessel (OR: 11.0, 95% CI: 2.7–45.5, P = 0.001) as well as female (OR: 11.0, 95% CI: 2.1–58.5, p = 0.005) were the predictors of adverse events, indicating the predictive value of target vessel failure [14]. Surprisingly, the pre-procedural J-CTO score in our cohort did not predict the occurrence of TVR, possibly due to the small sample size. Our study found that J-CTO score > 3 was one of the risk factors for TVR. Lesions with J-CTO score of 3 or higher were complex and difficult to treat, advanced and aggressive techniques that could result in long severe dissection and intimal damage, eventually leading to TVR.
Excessive long stents related TVR may be caused in part by the negative vessel remodeling beyond the occlusion. As we know, distal vessels shrink due to insufficient perfusion pressure, and it is all too easy for the operator to misinterpret normal vessels as stenosis and select an unnecessary long stent to cover the shrunk segment [15]. Studies have shown that the perfusion pressure was restored after CTO recanalization, and the shrunk lumen was significantly increased by 15.9% from baseline to follow-up (2.06 ± 0.62 mm vs. 2.30 ± 0.55 mm, p < 0.001) [16]. Stent malposition and TVR could occur in a positive remodeling vascular bed. On the other hand, the long stent may be related to extensive dissection and hematoma which is caused by guidewire manipulation into false lumen during the intervention. The subintimal tracking and reentry (STAR) technique also require stenting of a longer coronary segment, which may lead to in-stent restenosis [17]. Deferred stenting may be a solution for reducing TVR [18, 19].
Our study had several limitations. First, selection bias is an inherent limitation in retrospective studies. Second, the sample size was not large due to the high success rate of the first CTO-PCI today and the impact of the COVID-19 pandemic on patient enrolment. Our findings should be confirmed in the future by a larger multi-center clinical trial.
Conclusions
The group of patients who successfully re-attempt CTO recanalization had a 65% lower risk of MACE during long-term follow-up than the group of patients who failed re-attempt CTO recanalization. This association was primarily owing to a lower rate of TVR. Longer stents and more difficult CTO lesions were independent predictors of TVR after successful recanalization.
Acknowledgements
The authors would like to thank all the reviewers who participated in the review and MJEditor (www.mjeditor.com) for its linguistic assistance during the preparation of this manuscript.
Abbreviations
- CTO
Chronic total occlusion
- PCI
Percutaneous coronary intervention
- MACE
Major adverse cardiac events
- TVR
Target vessel revascularization
- HR
Hazard ratio
- CI
Confidence intervals
- TIMI
Thrombolysis In Myocardial Infarction
- CABG
Coronary artery bypass grafting
- MI
Myocardial infarction
- MVD
Multi-vessel disease
- QoL
Quality of life
Author contributions
WZL made contribution to the conception and design. JHL made contribution to the administrative support. ZW, TL, XFW were responsible for provision of study materials or patients. Collection and assembly of data: TL collected and assembled data. Data analysis and interpretation: TL analysed and interpreted the research data. All authors wrote and finally approved the manuscript.
Funding
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Beijing Anzhen Hospital's Research Committee authorized all of the study's protocols, which followed the 1964 Declaration of Helsinki (2021115X). Because this was an observational retrospective study, patient consent was not required, all data were gathered from medical records.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lee S-GS-WWSG, Lee PH, Ahn J-MM, Park D-WW, Yun S-CC, Han S, et al. Randomized trial evaluating percutaneous coronary intervention for the treatment of chronic total occlusion: the DECISION-CTO trial. Circulation. 2019;139:1674–1683. doi: 10.1161/CIRCULATIONAHA.118.031313. [DOI] [PubMed] [Google Scholar]
- 2.Guan C, Yang W, Song L, Chen J, Qian J, Wu F, et al. Association of acute procedural results with long-term outcomes after CTO PCI. JACC Cardiovasc Interv. 2021;14:278–288. doi: 10.1016/j.jcin.2020.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Wilson WM, Walsh SJ, Yan AT, Hanratty CG, Bagnall AJ, Egred M, et al. Hybrid approach improves success of chronic total occlusion angioplasty. Heart. 2016;102:1486–1493. doi: 10.1136/heartjnl-2015-308891. [DOI] [PubMed] [Google Scholar]
- 4.Morino Y, Abe M, Morimoto T, Kimura T, Hayashi Y, Muramatsu T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes. JACC Cardiovasc Interv. 2011;4:213–221. doi: 10.1016/j.jcin.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 5.Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018) J Am Coll Cardiol. 2018 doi: 10.1016/j.jacc.2018.08.1038. [DOI] [PubMed] [Google Scholar]
- 6.Christakopoulos GE, Christopoulos G, Carlino M, Jeroudi OM, Roesle M, Rangan BV, et al. Meta-analysis of clinical outcomes of patients who underwent percutaneous coronary interventions for chronic total occlusions. Am J Cardiol. 2015;115:1367–1375. doi: 10.1016/j.amjcard.2015.02.038. [DOI] [PubMed] [Google Scholar]
- 7.Brilakis ES, Mashayekhi K, Tsuchikane E, Abi Rafeh N, Alaswad K, Araya M, et al. Guiding principles for chronic total occlusion percutaneous coronary intervention: a global expert consensus document. Circulation. 2019;140:420–433. doi: 10.1161/CIRCULATIONAHA.119.039797. [DOI] [PubMed] [Google Scholar]
- 8.Joyal D, Afilalo J, Rinfret S. Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am Heart J. 2010;160:179–187. doi: 10.1016/j.ahj.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 9.Abuzeid W, Zivkovic N, Elbaz-Greener G, Yaranton B, Patel V, Strauss B, et al. Association between revascularization and quality of life in patients with coronary chronic total occlusions: a systematic review. Cardiovasc Revasc Med. 2021;25:47–54. doi: 10.1016/j.carrev.2020.10.006. [DOI] [PubMed] [Google Scholar]
- 10.Borgia F, Viceconte N, Ali O, Stuart-Buttle C, Saraswathyamma A, Parisi R, et al. Improved cardiac survival, freedom from mace and angina-related quality of life after successful percutaneous recanalization of coronary artery chronic total occlusions. Int J Cardiol. 2012;161:31–38. doi: 10.1016/j.ijcard.2011.04.023. [DOI] [PubMed] [Google Scholar]
- 11.Jang WJ, Yang JH, Choi SH, Bin SY, Hahn JY, Choi JH, et al. Long-term survival benefit of revascularization compared with medical therapy in patients with coronary chronic total occlusion and well-developed collateral circulation. JACC Cardiovasc Interv. 2015;8:271–279. doi: 10.1016/j.jcin.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Abe M, Morimoto T, Morino Y, Tanaka H, Akao M, Hayashi Y, et al. Association between J-CTO score and long-term target lesion revascularization rate after successful chronic total coronary occlusion angioplasty (from the J-CTO registry) Catheter Cardiovasc Interv. 2019;93:1025–1032. doi: 10.1002/ccd.28104. [DOI] [PubMed] [Google Scholar]
- 13.Tian T, Guan C, Gao L, Yuan J, Cui J, Hu F, et al. Predictors for adverse outcomes of patients with recanalized chronic total occlusion lesion. Eur J Clin Invest. 2021 doi: 10.1111/eci.13368. [DOI] [PubMed] [Google Scholar]
- 14.Geyer M, Wild J, Hirschmann M, Dimitriadis Z, Münzel T, Gori T, et al. Predictors for target vessel failure after recanalization of chronic total occlusions in patients undergoing surveillance coronary angiography. J Clin Med. 2020;9:178. doi: 10.3390/jcm9010178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gomez-Lara J, Teruel L, Homs S, Ferreiro JL, Romaguera R, Roura G, et al. Lumen enlargement of the coronary segments located distal to chronic total occlusions successfully treated with drug-eluting stents at follow-up. EuroIntervention. 2014;9:1181–1188. doi: 10.4244/EIJV9I10A199. [DOI] [PubMed] [Google Scholar]
- 16.Okuya Y, Saito Y, Takahashi T, Kishi K, Hiasa Y. Novel predictors of late lumen enlargement in distal reference segments after successful recanalization of coronary chronic total occlusion. Catheter Cardiovasc Interv. 2019;94:546–552. doi: 10.1002/ccd.28143. [DOI] [PubMed] [Google Scholar]
- 17.Galassi AR, Boukhris M, Tomasello SD, Marzà F, Azzarelli S, Giubilato S, et al. Long-term clinical and angiographic outcomes of the mini-STAR technique as a bailout strategy for percutaneous coronary intervention of chronic total occlusion. Can J Cardiol. 2014;30:1400–1406. doi: 10.1016/j.cjca.2014.07.016. [DOI] [PubMed] [Google Scholar]
- 18.Goleski PJ, Nakamura K, Liebeskind E, Salisbury AC, Grantham JA, McCabe JM, et al. Revascularization of coronary chronic total occlusions with subintimal tracking and reentry followed by deferred stenting: experience from a high-volume referral center. Catheter Cardiovasc Interv. 2019;93:191–198. doi: 10.1002/ccd.27783. [DOI] [PubMed] [Google Scholar]
- 19.Visconti G, Focaccio A, Donahue M, Briguori C. Elective versus deferred stenting following subintimal recanalization of coronary chronic total occlusions. Catheter Cardiovasc Interv. 2015;85:382–390. doi: 10.1002/ccd.25509. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.