Abstract
Background
The incidence of second anterior cruciate ligament (ACL) injury after ACL reconstruction (ACLR) is high in young, active populations. Failure to successfully meet return-to-sport (RTS) criteria may identify adult athletes at risk of future injury; however, these studies have yet to assess skeletally mature adolescent athletes.
Objective
To determine if failure to meet RTS criteria would identify adolescent and young adult athletes at risk for future ACL injury after ACLR and RTS. The tested hypothesis was that the risk of a second ACL injury after RTS would be lower in participants who met all RTS criteria compared with those who failed to meet all criteria before RTS.
Design
Prospective case-cohort (prognosis) study.
Setting
Laboratory.
Patients or Other Participants
A total of 159 individuals (age = 17.2 ± 2.6 years, males = 47, females = 112).
Main Outcome Measure(s)
Participants completed an RTS assessment (quadriceps strength, functional hop tests) and the International Knee Documentation Committee patient survey (0 to 100 scale) after ACLR and were then tracked for occurrence of a second ACL tear. Athletes were classified into groups that passed all 6 RTS tests at a criterion level of 90% (or 90 of 100) limb symmetry and were compared with those who failed to meet all criteria. Crude odds ratios and 95% CIs were calculated to determine if passing all 6 RTS measures resulted in a reduced risk of second ACL injury in the first 24 months after RTS.
Results
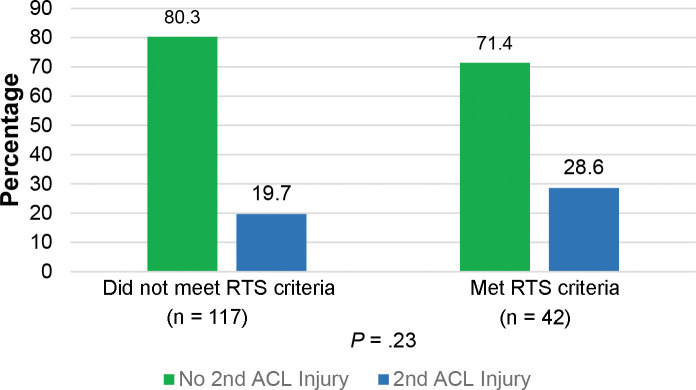
Thirty-five (22%) of the participants sustained a second ACL injury. At the time of RTS, 26% achieved ≥90 on all tests, and the remaining athletes scored less than 90 on at least 1 of the 6 assessments. The second ACL injury incidence did not differ between those who passed all RTS criteria (28.6%) and those who failed at least 1 criterion (19.7%, P = .23). Subgroup analysis by graft type also indicated no differences between groups (P > .05).
Conclusions
Current RTS criteria at a 90% threshold did not identify active skeletally mature adolescent and young adult athletes at high risk for second ACL injury.
Keywords: knee, second injury, functional assessment
Key Points
Rates of second anterior cruciate ligament injuries in skeletally mature adolescent and young adult athletes who undergo reconstruction are high, and many of these athletes fail to return to their preinjury levels of function after rehabilitation.
This study adds to existing knowledge in that the current return-to-sport (RTS) criteria commonly implemented as a decision tool to permit return to sport in skeletally mature adolescent and young adult athletes failed to identify those at risk for a second anterior cruciate ligament injury after RTS. These findings underscore the critical need to identify more appropriate RTS criteria for these athletes and other populations.
Wide variations in outcomes have been observed after anterior cruciate ligament (ACL) reconstruction (ACLR) in young, active patients. The incidence of second ACL injury after ACLR and return to sport (RTS) ranges from 1 in 4 to 1 in 3 among young, active populations, with the greatest risk in the first 12 months after RTS.1,2 The authors3 of a systematic review and meta-analysis reported that the percentage of patients who returned to their preinjury level of activity within the first year after ACLR could be as low as 65%, with only 55% able to return to competitive levels of sports. As a result, consistent successful outcomes have yet to be achieved at a reliable level after ACLR.
One factor that contributed to these variations in outcome was a lack of consensus on appropriate, standardized objective criteria to evaluate an athlete's readiness to safely RTS after ACLR. In 2004, Kvist4 noted the absence of consistent objective measures for determining readiness to RTS after ACLR. Specifically, researchers in as few as 33% of studies recommended isokinetic strength assessment, and fewer than 75% recommended functional hop testing. In a systematic review of more than 264 manuscripts in 2011, Barber-Westin and Noyes5 confirmed that a standard set of discharge criteria had yet to be identified in the literature. More recently, in a 2019 scoping review, Burgi et al6 observed that time was the sole criterion for RTS after ACLR in 42% of the 209 studies examined. Collectively, the existent literature demonstrated that a set of objective measures to identify an athlete's readiness to safely RTS was still needed to improve outcomes after ACLR.
Attempts have been made to assess the risk of future injury in populations of patients after ACLR who have failed to meet the requirements of a discharge algorithm. Grindem et al7 reported that among a population of patients between the ages of 13 and 60 years after ACLR, those who failed to meet the current criteria before RTS had a higher reinjury rate. Specifically, the RTS criteria were >90% on the Limb Symmetry Index (LSI) for isokinetic quadriceps and hamstrings strength and all 4 functional hop tests; reinjury was defined as any type of knee injury to either the involved or contralateral limb rather than a second ACL injury. More specific to ACL reinjury, Kyritsis et al8 identified a 4 times greater risk of ACL graft rupture among a population of professional male soccer players who failed to meet 6 clinical discharge criteria before RTS. Their RTS criteria were isokinetic strength, a running T-test, and 3 single-legged functional hop tests. Collectively, these studies indicated that regular use of the current RTS criteria could be sufficient to help reduce future knee and ACL injury rates. However, these investigators did not evaluate the effectiveness of these RTS criteria in the highest-risk populations, particularly adolescent athletes in pivoting-and-cutting sports.9 Therefore, the ability of current RTS measures to identify outcomes in the athletic adolescent population has yet to be validated.
The purpose of our study was to determine if failure to meet all current standard RTS criteria would identify skeletally mature adolescent and young adult athletes at risk for future ACL injury after primary ACLR and RTS. Our hypothesis was that the likelihood of second ACL injury in the 1-year and 2-year follow-ups after RTS would be higher in patients who failed to meet all RTS criteria before initiation of pivoting-and-cutting activity than in those who met all RTS criteria.
METHODS
Participants
This analysis was a subset of the larger prospective, longitudinal ACL-RELAY study10 that recruited 159 participants (female = 112, male = 47, age = 17.2 ± 2.6 years) from local orthopaedic practices, physical therapy clinics, and the community and were successfully contacted at 24 months post-RTS. The participants (1) were between 13 and 25 years; (2) underwent primary, unilateral ACLR; (3) had pursued rehabilitation and been released to return to pivoting-and-cutting sports by their physician and rehabilitation specialist; and (4) intended to return to a level I or II pivoting-and-cutting sport11 after completing rehabilitation. Rehabilitation and the decision for RTS clearance were not controlled by the study researchers. Participants were enrolled in the prospective, observational cohort study, completed an RTS assessment at a mean of 7.0 ± 2.2 months postsurgery (Table 1), and were then tracked for occurrence of a second ACL injury for 24 months after RTS. Exclusion criteria were a history of low back or lower extremity injury or surgery (beyond ACL injury) that required the care of a physician in the past year, a concomitant ligament injury (beyond grade I medial collateral ligament injury) to the involved limb, or skeletal immaturity as defined by an ACLR procedure that was modified due to open epiphyseal plates in the tibia or femur. All participants, and guardians when required, provided written consent and assent approved by the Institutional Review Board of Cincinnati Children's Hospital Medical Center, which also approved the study.
Table 1.
Characteristics at the RTS Testing Session for the Entire Sample and by Second Injury Sustained in the First 12 and 24 Months After ACLR and RTS
| Characteristic |
Overall Sample (N = 159) |
Second ACL Injury After RTS |
|||||
| First 12 mo |
First 24 mo |
||||||
| Yes (n = 26) |
No (n = 133) |
P Value |
Yes (n = 35) |
No (n = 124) |
P Value |
||
| Sex, No, (%) | |||||||
| Female | 112 (70.4) | 21 (18.8) | 91 (81.3) | .25 | 27 (24.1) | 85 (75.9) | .40 |
| Male | 47 (29.6) | 5 (10.6) | 42 (89.4) | 8 (17.0) | 39 (83.0) | ||
| Age, mean ± SD, y | 17.2 ± 2.6 | 16.2 ± 1.2 | 17.4 ± 2.7 | <.0001 | 16.1 ± 1.3 | 17.6 ± 2.7 | <.0001 |
| Height, mean ± SD, cm | 168.9 ± 9.3 | 167.2 ± 8.3 | 169.2 ± 9.5 | .33 | 167.9 ± 10.6 | 169.1 ± 9.0 | .51 |
| Weight, mean ± SD, kg | 68.9 ± 14.4 | 65.5 ± 14.4 | 69.6 ± 14.4 | .18 | 66.3 ± 14.5 | 69.7 ± 14.4 | .23 |
| Graft type, No. (%) | |||||||
| Hamstrings | 86 (54.1) | 14 (16.3) | 72 (83.7) | .97 | 20 (23.3) | 66 (76.7) | .92 |
| Bone-patellar tendon-bone | 59 (37.1) | 10 (16.9) | 49 (83.1) | 12 (20.3) | 47 (79.7) | ||
| Allograft | 14 (8.8) | 2 (14.3) | 12 (85.7) | 3 (21.4) | 11 (78.6) | ||
| Meniscus injury, No. (%) | |||||||
| No | 84 (52.8) | 15 (17.9) | 69 (82.1) | .37 | 20 (23.8) | 64 (76.2) | .35 |
| Yes | 75 (47.2) | 11 (14.7) | 64 (85.3) | 15 (20.0) | 60 (80.0) | ||
| Time from surgery to RTS test, mean ± SD, mo | 7.0 ± 2.2 | 6.90 ± 1.8 | 7.1 ± 2.3 | .77 | 6.90 ± 2.5 | 7.1 ± 2.2 | .74 |
Abbreviations: ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; RTS, return to sport.
The RTS Testing Session
Each patient participated in an RTS assessment within 4 weeks of medical clearance to RTS. The assessment included standard measures commonly used to assess readiness to RTS by clinicians: patient-reported function, lower extremity strength, and functional hop testing.
Patient-Reported Measure of Function
Each patient completed the subjective portion of the International Knee Documentation Committee (IKDC) patient-reported outcome tool.12 The IKDC was both reliable and valid in participants after ACLR12 and validated in a population of young athletes. Commonly used with patients after ACLR, the IKDC assesses patient perspectives on knee-related symptoms, daily function, and sports activities. On a scale of 0 to 100, 100 represents a high level of knee function13
Strength Assessment
Quadriceps strength was evaluated in each patient using a maximal voluntary isometric contraction (MVIC) on an isokinetic dynamometer (Biodex Medical Systems) and previously described methods.14 Each participant was stabilized using static straps and placed in a seated position with 90° of hip flexion, 60° of knee flexion, and the knee joint center aligned with the dynamometer axis of rotation. After a practice trial, the patient executed 3 maximal-effort knee-extension kicks for 5 seconds with a 15-second rest between trials. Peak torque of the 3 trials was recorded, and the average was used to calculate the LSI (involved-limb peak torque/uninvolved-limb peak torque × 100%). A score of <100% indicated weakness in the involved limb.
Functional Hop Testing
Each participant completed 4 single-legged hop tests15 for evaluation of physical performance in a closed kinetic chain. These hop tests have been used most often clinically as an RTS measure after ACLR,4 in part due to their ease of administration and few resources needed, which allows them to be conducted in diverse clinic and athletic settings. The hop tests were administered sequentially, beginning with the single-legged hop for distance, followed by the triple-hop test for distance, the triple-crossover–hop test for distance, and then the 6-m single-legged timed-hop test. Each participant completed 1 practice trial using each limb and then performed 2 randomly selected trials using each limb. The average of the 2 trials was used for data analysis. In addition, the LSI was calculated as described earlier. As the single-limb timed-hop test was the only test in which a lower score represented better performance, we determined the LSI by dividing the uninvolved by the involved limb and multiplying by 100%. Collectively, a score of <100% indicated worse performance with the involved limb.
Injury Tracking
Each patient was tracked for 24 months after RTS testing to determine the incidence of a second ACL injury to either the ipsilateral or contralateral limb. Tracking was conducted during regularly attended longitudinal follow-up assessments. As part of the parent study, patients agreed to longitudinal data-collection sessions for ≥24 months after RTS. Second-injury data were obtained at this time. Each patient who failed to participate in the longitudinal data collections was contacted by telephone to confirm his or her second-injury status. If a second ACL injury occurred, this was confirmed by either magnetic resonance imaging or arthroscopy report in the case of a second surgery. During the 24-month observation period after RTS, 35 patients sustained a second ACL injury, 26 of which occurred in the first 12 months post-RTS.
Statistical Analysis
We computed means, SDs, and frequencies to describe the study sample characteristics, graft type, history of meniscal injury, and time from surgery to RTS. Chi-square test analyses were used to compare the percentage differences for each RTS measure between those who experienced a second ACL injury in the first 12 and first 24 months after RTS and those who did not. To test our primary hypothesis, we defined passing each RTS measure a priori as 90% LSI on strength and functional performance test assessments and 90/100 on the IKDC instrument. Participants were then classified as meeting all 6 RTS tests or failing to meet all RTS tests if he or she scored <90 on any RTS test. A cutoff value of 90 was selected as evidence7,8,16 indicated that values of ≥90% on the LSI and 90/100 on the IKDC tool were recommended for RTS. Adjusted odds ratios (AORs) and 95% CIs were calculated using multiple variable logistic regression, adjusting for sex and time to test, to determine if passing all 6 RTS measures at ≥90 resulted in a reduced risk of second ACL injury in the 24 months after RTS.
RESULTS
At the time of RTS testing, the average age of the 159 participants was 17.2 ± 2.6 years (range = 13–25 years). In the 24 months after RTS, 35 patients (22%) sustained a second ACL injury, 16 (10%) sustained an ipsilateral graft rupture, and 19 (12%) sustained a contralateral ACL injury. Of those who experienced a second ACL injury, 26 (74%) incurred their second ACL injury within 12 months after RTS. No differences in height, weight, time from surgery to RTS, distribution of sex or graft type, or presence of meniscal injury between those who sustained a second ACL injury and those who did not were present (Table 1). Participants who sustained a second ACL injury during the 2-year observation period were younger (age = 16.1 ± 1.3 years) than those who did not (age = 17.6 ± 2.7 years; P < .0001).
At the time of RTS testing, the average IKDC score of the entire cohort was 89.4 ± 10.1, average quadriceps strength LSI was 91.5% ± 17.4%, and average single-legged–hop test limb symmetry ranged from 95.5% ± 6.6% to 97.3% ± 7.3% (Table 2). When differences in each of these RTS measures were compared between those who sustained a second ACL injury 0 to 12 months after RTS and those who did not, no differences were seen (P values > .05). Similarly, when differences between each of these RTS measures were compared between those who sustained a second ACL injury 0 to 24 months after RTS and those who did not, no differences were found in any measures except the IKDC score (P = .05). Those athletes who experienced a second ACL injury within 24 months of RTS reported higher IKDC scores at the time of RTS (91.7 ± 6.6) than those who did not (88.8 ± 10.9; P = .05). However, the magnitude of this difference did not achieve the clinically significant difference of 11.5 points.17
Table 2.
Variables of Interest at the RTS Testing Session for the Entire Sample and by Second Injury Sustained in the First 12 and 24 Months After ACLR and RTSa
| Variable |
Overall Sample (N = 159) |
Second ACL Injury After RTS |
|||||
| First 12 mo |
First 24 mo |
||||||
| Yes (n = 26) |
No (n = 133) |
P Value |
Yes (n = 35) |
No (n = 124) |
P Value |
||
| International Knee Documentation Committee Subjective Knee Form score (range = 0–100, 100 = perfect) | 89.4 ± 10.1 | 90.8 ± 7.0 | 89.1 ± 10.7 | .44 | 91.7 ± 6.6 | 88.8 ± 10.9 | .05 |
| Quadriceps Limb Symmetry Index (100 = no strength deficit), distance, % | 91.5 ± 17.4 | 93.7 ± 13.3 | 91.1 ± 18.0 | .48 | 94.2 ± 12.9 | 90.8 ± 18.4 | .30 |
| Single-legged hop for distance, % | 95.5 ± 6.6 | 96.5 ± 6.5 | 95.3 ± 6.7 | .39 | 95.9 ± 6.1 | 95.4 ± 5.4 | .72 |
| Triple hop for distance, % | 96.0 ± 6.7 | 95.3 ± 6.1 | 96.1 ± 6.8 | .55 | 95.3 ± 5.4 | 96.2 ± 7.0 | .49 |
| Crossover hop for distance, % | 95.9 ± 8.4 | 95.4 ± 5.2 | 96.0 ± 8.8 | .76 | 96.2 ± 5.7 | 95.8 ± 8.9 | .82 |
| 6-m Timed hop, % | 97.3 ± 7.3 | 98.7 ± 7.2 | 97.1 ± 7.3 | .31 | 98.5 ± 7.4 | 97.0 ± 7.2 | .26 |
Abbreviations: ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; RTS, return to sport.
Data are mean ± SD unless otherwise indicated.
Regarding the ability to obtain a score of ≥90 on all RTS testing measures, only 42 patients (26%) achieved these metrics and were subsequently classified as passing all RTS measures. The remaining 117 patients (74%) scored <90 on at least 1 of the 6 assessments (Table 3) and were classified as failing to meet all RTS criteria. At this criterion level, after adjusting for sex and the time to RTS testing, the incidence of second ACL injury incidence in the 24 months after RTS was not significantly associated with passing all RTS criteria (12/42, 28.6%) or failing ≥1 criterion (23/117, 19.7%; P = .24; Figure). Similarly, when the initial 12 months after ACLR and RTS were evaluated and we adjusted for sex and the time to RTS testing, no significant association was demonstrated between those who passed all 6 test criteria and those who did not (P = .30).
Table 3.
Crude Odds Ratiosa for Associations Between Functional Tests and Second ACL Injury at 12 or 24 Months After RTS
| Test Variables |
Total (Second Injury in First 12 Mo After RTS) |
Total (Second Injury in First 24 Mo After RTS) |
||||||||
| No. at Risk |
No. Injured (%) |
AOR |
95% CI |
P Value |
No. at Risk |
No. Injured (%) |
AOR |
95% CI |
P Value |
|
| International Knee Documentation Committee Subjective Knee Form score | ||||||||||
| ≥90 (Passed) | 89 | 15 (16.9) | 1.00 | Reference | 89 | 22 (24.7) | 1.00 | Reference | ||
| ≤89 (Failed) | 70 | 11 (15.7) | 0.94 | 0.4, 2.2 | .88 | 70 | 13 (18.6) | 0.71 | 0.3, 1.5 | .39 |
| Quadriceps Limb Symmetry Index | ||||||||||
| ≥90 (Passed) | 86 | 15 (17.4) | 1.00 | Reference | 86 | 20 (23.3) | 1.00 | Reference | ||
| ≤89 (Failed) | 72 | 10 (13.9) | 0.71 | 0.3, 1.7 | .45 | 72 | 14 (19.4) | 0.77 | 0.4, 1.7 | .52 |
| Single-legged hop for distance | ||||||||||
| ≥90 (Passed) | 120 | 21 (17.5) | 1.00 | Reference | 120 | 28 (23.3) | 1.00 | Reference | ||
| ≤89 (Failed) | 33 | 4 (12.1) | 0.56 | 0.2, 1.8 | .34 | 33 | 6 (18.2) | 0.72 | 0.3, 2.0 | .52 |
| Triple hop for distance | ||||||||||
| ≥90 (Passed) | 123 | 20 (16.3) | 1.00 | Reference | 123 | 29 (23.6) | 1.00 | Reference | ||
| ≤89 (Failed) | 28 | 5 (17.9) | 1.11 | 0.4, 3.4 | .82 | 28 | 5 (17.9) | 0.73 | 0.3, 2.1 | .56 |
| Crossover hop for distance | ||||||||||
| ≥90 (Passed) | 115 | 20 (17.4) | 1.00 | Reference | 115 | 20 (24.3) | 1.00 | Reference | ||
| ≤89 (Failed) | 32 | 3 (9.4) | 0.48 | 0.1, 1.8 | .27 | 32 | 4 (12.5) | 0.45 | 0.2, 1.4 | .17 |
| 6-m Timed hop | ||||||||||
| ≥90 (Passed) | 125 | 22 (17.6) | 1.00 | Reference | 125 | 30 (24.0) | 1.00 | Reference | ||
| ≤89 (Failed) | 24 | 2 (8.3) | 0.40 | 0.1, 1.9 | .24 | 24 | 3 (12.5) | 0.45 | 0.1, 1.6 | .22 |
| Met criteria for all 6 tests | ||||||||||
| ≥90 (Passed) | 42 | 9 (21.4) | 1.00 | Reference | 42 | 12 (28.6) | 1.00 | Reference | ||
| ≤89 (Failed) | 117 | 17 (14.5) | 0.62 | 0.3, 1.5 | .30 | 117 | 23 (19.7) | 0.61 | 0.3, 1.4 | .24 |
Abbreviations: ACL, anterior cruciate ligament; AOR, adjusted odds ratio; RTS, return to sport.
Adjusted for sex and time (in mo) to test.
Figure.
Incidence of second anterior cruciate ligament (ACL) injury after ACL reconstruction and return to sport (RTS) by ability to meet RTS criteria at ≥90 criteria.
Subgroup analysis by graft type showed no significant associations in second-injury risk at 24 and 12 months in the group of patients who had ACLR with a hamstrings (HS) graft or those with a patellar bone-tendon-bone (BTB) graft with an RTS criteria of 90 on all tests (Tables 4 and 5). Specifically, 45% (39/86) of patients with HS grafts passed all RTS criteria of 90, while the remaining 55% failed to meet at least 1 of the 6 RTS criteria. After adjusting for sex and time to RTS testing, we observed no difference in second ACL injury incidence between the patients with HS grafts who passed all RTS criteria (10/39, 25.6%) and those who failed at least 1 criterion (10/47, 21.3%; P = .62). Among the patients who received ACLR with a BTB graft, only 5% (3/59) passed all RTS criteria at 90, while the remaining 95% failed to meet at least 1 of the 6 criteria. After adjusting for sex and time to RTS testing, we identified no difference in the second ACL injury incidence between patients with BTB grafts who passed all RTS criteria (2/3, 66.7%) and those who failed at least 1 criterion (10/56, 17.9%; P = .07). Similarly, after adjusting for sex and time to RTS testing, no differences were seen in the incidence of second ACL injury at 12 months post-RTS for patients with HS grafts (P = .71) or BTB grafts (P = .06).
Table 4.
Crude Odds Ratiosa for Associations Between Functional Tests and Second ACL Injury at 12 Months After RTS by Graft Type
| Test Variables |
Hamstrings |
Bone-Patellar Tendon-Bone |
||||||||
| No. at Risk |
No. Injured (%) |
AOR |
95% CI |
P Value |
No. at Risk |
No. Injured (%) |
AOR |
95% CI |
P Value |
|
| International Knee Documentation Committee Subjective Knee Form score | ||||||||||
| ≥90 (Passed) | 62 | 10 (16.1) | 1.00 | Reference | 24 | 4 (16.7) | 1.00 | Reference | ||
| ≤89 (Failed) | 24 | 4 (16.7) | 1.08 | 0.3, 3.9 | .90 | 35 | 6 (17.1) | 1.19 | 0.3, 5.0 | .81 |
| Quadriceps Limb Symmetry Index | ||||||||||
| ≥90 (Passed) | 65 | 11 (16.9) | 1.00 | Reference | 16 | 20 (18.8) | 1.00 | Reference | ||
| ≤89 (Failed) | 20 | 2 (10.0) | 0.48 | 0.1, 2.4 | .38 | 43 | 14 (16.3) | 0.83 | 0.2, 3.8 | .81 |
| Single-legged hop for distance | ||||||||||
| ≥90 (Passed) | 74 | 11 (14.9) | 1.00 | Reference | 37 | 8 (22.6) | 1.00 | Reference | ||
| ≤89 (Failed) | 10 | 2 (20.0) | 1.18 | 0.2, 6.9 | .85 | 18 | 2 (11.1) | 0.48 | 0.1, 2.8 | .41 |
| Triple hop for distance | ||||||||||
| ≥90 (Passed) | 75 | 10 (13.3) | 1.00 | Reference | 36 | 8 (22.2) | 1.00 | Reference | ||
| ≤89 (Failed) | 9 | 3 (33.3) | 3.22 | 0.7, 15.3 | .14 | 17 | 2 (11.8) | 0.50 | 0.1, 2.8 | .43 |
| Crossover hop for distance | ||||||||||
| ≥90 (Passed) | 69 | 10 (14.5) | 1.00 | Reference | 37 | 8 (21.6) | 1.00 | Reference | ||
| ≤89 (Failed) | 14 | 2 (14.3) | 0.97 | 0.2, 5.1 | .98 | 14 | 1 (7.1) | 0.30 | 0.1, 2.8 | .30 |
| 6-m Timed hop | ||||||||||
| ≥90 (Passed) | 71 | 11 (15.5) | 1.00 | Reference | 43 | 9 (20.9) | 1.00 | Reference | ||
| ≤89 (Failed) | 12 | 1 (8.3) | 0.49 | 0.1, 4.2 | .51 | 10 | 1 (10.0) | 0.40 | 0.1, 3.6 | .41 |
| Met criteria for all tests | ||||||||||
| ≥90 (Passed) | 39 | 7 (17.9) | 1.00 | Reference | 3 | 2 (66.7) | 1.00 | Reference | ||
| ≤89 (Failed) | 47 | 7 (14.9) | 0.80 | 0.3, 2.5 | .71 | 56 | 8 (14.3) | 0.08 | 0.1, 1.1 | .06 |
Abbreviations: ACL, anterior cruciate ligament; AOR, adjusted odds ratio; RTS, return to sport.
Adjusted for sex and time (in mo) to test.
Table 5.
Crude Odds Ratiosa for Associations Between Functional Tests and Second ACL Injury at 24 Months After RTS by Graft Type
| Test Variables |
Hamstrings |
Bone-Patellar Tendon-Bone |
||||||||
| No. at Risk |
No. Injured (%) |
AOR |
95% CI |
P Value |
No. at Risk |
No. Injured (%) |
AOR |
95% CI |
P Value |
|
| International Knee Documentation Committee Subjective Knee Form score | ||||||||||
| ≥90 (Passed) | 62 | 16 (25.8) | 1.00 | Reference | 24 | 4 (16.7) | 1.00 | Reference | ||
| ≤89 (Failed) | 24 | 4 (16.7) | 0.60 | 0.2, 2.0 | .41 | 35 | 8 (22.9) | 1.76 | 0.4, 7.0 | .42 |
| Quadriceps Limb Symmetry Index | ||||||||||
| ≥90 (Passed) | 65 | 15 (23.1) | 1.00 | Reference | 16 | 4 (25.0) | 1.00 | Reference | ||
| ≤89 (Failed) | 20 | 4 (20.0) | 0.77 | 0.2, 2.7 | .68 | 43 | 8 (18.6) | 0.61 | 0.2, 2.7 | .72 |
| Single-legged hop for distance | ||||||||||
| ≥90 (Passed) | 74 | 16 (21.6) | 1.00 | Reference | 37 | 9 (24.3) | 1.00 | Reference | ||
| ≤89 (Failed) | 10 | 3 (30.0) | 1.44 | 0.3, 6.7 | .64 | 18 | 3 (16.7) | 0.64 | 0.1, 3.0 | .57 |
| Triple hop for distance | ||||||||||
| ≥90 (Passed) | 75 | 16 (21.3) | 1.00 | Reference | 36 | 10 (27.8) | 1.00 | Reference | ||
| ≤89 (Failed) | 9 | 3 (33.3) | 1.77 | 0.4, 7.9 | .46 | 17 | 2 (11.8) | 0.37 | 0.1, 2.0 | .25 |
| Crossover hop for distance | ||||||||||
| ≥90 (Passed) | 69 | 16 (23.2) | 1.00 | Reference | 37 | 9 (24.3) | 1.00 | Reference | ||
| ≤89 (Failed) | 14 | 2 (14.3) | 0.54 | 0.1, 2.7 | .45 | 14 | 2 (14.3) | 0.53 | 0.1, 3.0 | .47 |
| 6-m Timed hop | ||||||||||
| ≥90 (Passed) | 71 | 17 (23.9) | 1.00 | Reference | 43 | 10 (23.3) | 1.00 | Reference | ||
| ≤89 (Failed) | 12 | 1 (8.3) | 0.28 | 0.1, 2.4 | .25 | 10 | 2 (20.0) | 0.75 | 0.1, 4.2 | .74 |
| Met criteria for all tests | ||||||||||
| ≥90 (Passed) | 39 | 10 (25.6) | 1.00 | Reference | 3 | 2 (66.7) | 1.00 | Reference | ||
| ≤89 (Failed) | 47 | 10 (21.3) | 0.77 | 0.3, 2.1 | .62 | 56 | 10 (17.9) | 0.09 | 0.1, 1.3 | .07 |
Abbreviations: ACL, anterior cruciate ligament; AOR, adjusted odds ratio; RTS, return to sport.
Adjusted for sex and time (in mo) to test.
DISCUSSION
The purpose of our study was to determine if failing to achieve RTS criteria (patient-reported outcomes, physical performance testing, and muscle strength) would be associated with an increased likelihood of future ACL injury in the 24 months after RTS in skeletally mature adolescent and young adult athletes. These data failed to support the hypothesis that athletes who met the current RTS criteria would incur fewer second ACL injuries when compared with those who failed to meet all RTS criteria, as no difference was present in the relative proportions of second ACL injuries between groups during the 24 months after RTS. These findings were consistent when using passing criteria scores of ≥90.
With respect to second-injury rates in a young, athletic population and the athletes' ability to achieve standard RTS criteria, these data were consistent with the current literature. Although the second-injury rate was reported to be as low as 6% in heterogeneous populations,18 more recent evidence19 indicated a much higher second-injury rate in particular high-risk populations. Specifically, rates of second ACL injuries were as high as 35% in adolescent athletes returning to pivoting-and-cutting sports after ACLR. At 24 months after ACLR and RTS, Paterno et al2 identified the second-injury rate to either the ipsilateral or contralateral limb as 29%. In their systematic review, Wiggins et al20 observed that athletes younger than 25 years who returned to sport had a secondary ACL injury risk of 23%. Therefore, consistent evidence supports that particularly among young, pivoting-and-cutting athletes, a relatively high second-injury rate persists. Importantly, in corroboration of the current findings, 2 recent meta-analyses21,22 showed that passing RTS criteria did not lead to a decreased risk of second ACL injury. Although Webster and Hewett21 reported a 60% decrease in graft ruptures, they also noted a 235% increase in risk for a second contralateral ACL injury among patients who passed all RTS criteria and no difference among all patients combined.
In addition to consistent second-injury rates, these data were consistent with the relatively low percentage of participants who met current RTS criteria when they returned to sport or at a 6-month postoperative evaluation.23,24 Published recommendations and clinical practice guidelines16 advocated for minimum RTS criteria to include patient-reported outcome measures of function, physical performance testing, and objective measures of lower extremity strength. Further, these guidelines advised meeting or exceeding an LSI of 90% on measures versus the contralateral limb and minimum scores of 90/100 on patient-reported measures.16 Wellsandt et al25 suggested that the LSI may have underestimated the return to the preinjury level of function, as the contralateral limb may have weakened during the postoperative period of inactivity, thereby lowering the baseline targets in strength and hop measures. Despite this, several researchers demonstrated that a high percentage of participants failed to achieve these metrics by 6 months after ACLR or before RTS.26 Di Stasi et al27 found that only 48% of their patients met all RTS criteria at the 90% metric at 6 months after ACLR. Welling et al23 added the ACL-Return to Sport after Injury (ACL-RSI) patient-reported outcome and a quality-of-movement assessment to the current RTS criteria and determined that only 3.2% of patients met all criteria at 6 months post-ACLR and only 11.3% met all criteria at 9 months post-ACLR. Similarly, our results supported these findings as only 26% met the RTS criteria at a ≥90 level at 7 months post-ACLR. Collectively, these data supported the work of investigators21 who cited the low rate of patients who achieved the current RTS criteria at 6 months post-ACLR and often at the time of RTS.
Given the low rate of success in patients' ability to meet current RTS criteria after ACLR, these gaps in function and strength may have been related to second ACL injury rates. Preliminary support for this theory has been provided. Grindem et al7 evaluated 2-year outcomes of 106 patients after ACLR. These authors noted that 38.2% of participants who failed RTS criteria (passing defined as ≥90) sustained a second knee injury, though it was not specific to ACL injury. Conversely, only 5.6% of patients who passed the RTS criteria before RTS experienced a second knee injury. No difference was present in second ACL injury rates between groups; however, the authors highlighted a higher second knee injury rate in those who failed RTS testing. More specifically, Kyritsis et al8 assessed the prevalence of ACL graft rupture in groups that successfully met 6 RTS criteria compared with those that failed to meet 6 RTS criteria. In a cohort of 158 professional male soccer players, those who failed to meet standard discharge criteria were 4 times more likely to incur an ACL injury. Collectively, these studies support the theory that failure to pass the RTS criteria, including patient-reported outcomes, lower extremity strength, and functional hop testing, may relate to future injury in some populations, particularly adults.
Conversely, our data demonstrated no difference in the ACL second-injury prevalence based on the ability to meet the current RTS criteria at 90% levels. Notably, no difference occurred in the proportion of participants who passed or failed the RTS criteria and subsequently sustained a second ACL injury. One partial potential explanation for the divergent results may have been the populations tested. Specifically, Grindem et al7 recruited a more heterogeneous sample based on age and activity level and included all subsequent knee injuries, whereas we evaluated only second ACL injuries in young athletes who returned to pivoting-and-cutting sports. Kyritsis et al8 recruited a group of professional soccer players, all men. Neither of these research groups focused their populations on female and male skeletally mature adolescent and young adult athletes who participated in pivoting-and-cutting sports, who historically had the highest injury and second-injury rates, and, consequently, their results may not be generalizable to this high-risk population.1,2,20
The inability of the current RTS criteria (including patient-reported outcomes, objective strength testing, and physical functional testing) to identify young female and male pivoting-and-cutting–sport athletes at risk for future ACL injuries is concerning and results in a significant gap in the literature. Importantly, valid and reliable RTS tools that accurately assess and predict the future injury risk and ability to successfully return to preinjury activity are lacking. Beyond patient-reported outcomes, strength, and physical function assessment, some have suggested more specifically evaluating quality-of-movement and psychological factors. Altered movement patterns have been identified in patients after ACLR. The most frequently observed factors were decreased knee-flexion angles and knee-extensor moments during gait and single-legged–landing tasks.28–30 Unfortunately, none of these variables have been identified as a predictive risk factor for future ACL injury risk. Paterno et al31 characterized movement patterns that were related to future ACL injury risk after ACLR. They studied prospectively identified biomechanical and neuromuscular variables that predicted future ACL injury risk in a population of young female and male athletes after ACLR and return to pivoting-and-cutting sports. Altered hip internal-rotation moment, knee valgus, and asymmetries in sagittal-plane knee moments during the landing phase of the drop-vertical jump, as well as altered postural stability, were predictive variables. Despite producing a very sensitive and specific risk model, the variables used to assess risk were collected using 3-dimensional motion analysis. Therefore, these measures may not be generalizable to all clinical settings. Other clinical movement screening tools have been developed32,33 to assess future risk in populations after ACLR; however, these tools have yet to be identified as predicting future injury.
The participant's psychological readiness to RTS, or more specifically, the fear of future injury, has been evaluated using measures such as the Tampa Scale of Kinesiophobia34,35 or the ACL-RSI Scale36 and was a critical factor to consider in RTS decision making.37 The relationship between self-reported psychological factors and measures of physical function and performance has been explored,34,35 but few associations between these factors and future injury were demonstrated.38 Paterno et al38 identified high self-reported fear on the Tampa Scale of Kinesiophobia as predictive of the future ipsilateral ACL injury risk after ACLR and RTS. Knee-related confidence on the Knee injury and Osteoarthritis Outcome instrument and the ACL-RSI in young, skeletally mature athletes also predicted future injury.10,38,40,41 Future work must better define the relationship of patient-reported psychological factors and future injury to better determine its utility as an RTS measure in this population.
Limitations
The limitations in this study were noteworthy. Our focus was on assessing the ability of the current RTS criteria to categorize patients at risk of a second ACL injury, including both ipsilateral and contralateral injuries. We did not evaluate the ability of the current criteria to independently assess an ipsilateral versus a contralateral injury. Future analyses in larger cohorts are needed to better examine this aspect. In addition, although the participants' characteristics were comparable with those of similar studies,7,8 the sample was relatively small, thus limiting the ability to control for potential confounding variables. The current standard of care suggests criterion values of >90 to pass the RTS criteria.7,8,24 Further, the relatively smaller size of some subgroups (ie, HS graft, patellar tendon graft) in these analyses raises the concern for type II error, considering the inability of these measures to identify the risk of a future outcome. Confirming these findings by replicating this study in a larger sample would be beneficial. A third limitation relates to the use of the IKDC instrument. The Pediatric IKDC (Pedi-IKDC) was developed specifically for patients under the age of 18 after we began collecting data, so we continued to use the IKDC tool. A fourth limitation of the study was the generalizability to a more heterogeneous sample. These participants, by design, represented a very high-risk sample of patients with an increased likelihood of sustaining a second ACL injury, as they were young (13 to 25 years old) and active and intended to return to pivoting-and-cutting sports. Whether these findings also apply to potentially higher-risk subgroups, such as female athletes, and potentially lower-risk subgroups, such as older or less active patients, is unknown. Also, because rehabilitation and RTS decision making were not controlled, the average time to RTS was earlier (7.0 ± 2.2 months) than more recent recommendations of ≥9 months. Future authors must carefully evaluate these metrics in more diverse populations to determine the generalizability of the results. Finally, given that our primary aim was to determine the relationship between the ability to meet RTS criteria and a subsequent outcome, rehabilitation was not controlled in these participants. Research designed to identify optimal interventions for improving outcomes must focus on the effects of unique interventions.
CONCLUSIONS
The current RTS measures, including patient-reported functional outcomes (≥90/100), isokinetic strength tests (≥90% LSI), and functional hop testing (≥90% LSI), did not accurately identify skeletally mature adolescent and young adult athletes at increased risk for ACL injury after ACLR and RTS. Future work in this area should focus on the identification and validation of clinically relevant and feasible measures that can accurately assess the risk of future ACL injury and potentially be implemented in a novel RTS algorithm after ACLR.
REFERENCES
- 1.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med . 2012;22(2):116–121. doi: 10.1097/JSM.0b013e318246ef9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med . 2014;42(7):1567–1573. doi: 10.1177/0363546514530088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med . 2014;48(21):1543–1552. doi: 10.1136/bjsports-2013-093398. [DOI] [PubMed] [Google Scholar]
- 4.Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med . 2004;34(4):269–280. doi: 10.2165/00007256-200434040-00006. [DOI] [PubMed] [Google Scholar]
- 5.Barber-Westin SD, Noyes FR. Objective criteria for return to athletics after anterior cruciate ligament reconstruction and subsequent reinjury rates: a systematic review. Phys Sportsmed . 2011;39(3):100–110. doi: 10.3810/psm.2011.09.1926. [DOI] [PubMed] [Google Scholar]
- 6.Burgi CR, Peters S, Ardern CL, et al. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review. Br J Sports Med . 2019;53(18):1154–1161. doi: 10.1136/bjsports-2018-099982. [DOI] [PubMed] [Google Scholar]
- 7.Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med . 2016;50(13):804–808. doi: 10.1136/bjsports-2016-096031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med . 2016;50(15):946–951. doi: 10.1136/bjsports-2015-095908. [DOI] [PubMed] [Google Scholar]
- 9.Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med . 2014;42(3):641–647. doi: 10.1177/0363546513517540. [DOI] [PubMed] [Google Scholar]
- 10.Paterno MV, Huang B, Thomas S, Hewett TE, Schmitt LC. Clinical factors that predict a second ACL injury after ACL reconstruction and return to sport: preliminary development of a clinical decision algorithm. Orthop J Sports Med . 2017;5(12):2325967117745279. doi: 10.1177/2325967117745279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med . 1994;22(5):632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 12.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med . 2001;29(5):600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 13.Kocher MS, Smith JT, Iversen MD, et al. Reliability, validity, and responsiveness of a modified International Knee Documentation Committee Subjective Knee Form (Pedi-IKDC) in children with knee disorders. Am J Sports Med . 2011;39(5):933–929. doi: 10.1177/0363546510383002. [DOI] [PubMed] [Google Scholar]
- 14.Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc . 2015;47(7):1426–1434. doi: 10.1249/MSS.0000000000000560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med . 1991;19(5):513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 16.Logerstedt DS, Scalzitti D, Risberg MA, et al. Knee stability and movement coordination impairments: knee ligament sprain revision 2017. J Orthop Sports Phys Ther . 2017;47(11):A1–A47. doi: 10.2519/jospt.2017.0303. [DOI] [PubMed] [Google Scholar]
- 17.Irrgang JJ, Anderson AF, Boland AL, et al. International Knee Documentation Committee. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med . 2006;34(10):1567–1573. doi: 10.1177/0363546506288855. [DOI] [PubMed] [Google Scholar]
- 18.Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med . 2007;35(7):1131–1134. doi: 10.1177/0363546507301318. [DOI] [PubMed] [Google Scholar]
- 19.Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med . 2016;44(11):2827–2832. doi: 10.1177/0363546516651845. [DOI] [PubMed] [Google Scholar]
- 20.Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med . 2016;44(7):1861–1876. doi: 10.1177/0363546515621554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Webster KE, Hewett TE. What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Sports Med . 2019;49(6):917–929. doi: 10.1007/s40279-019-01093-x. [DOI] [PubMed] [Google Scholar]
- 22.Losciale JM, Zdeb RM, Ledbetter L, Reiman MP, Sell TC. The association between passing return-to-sport criteria and second anterior cruciate ligament injury risk: a systematic review with meta-analysis. J Orthop Sports Phys Ther . 2019;49(2):43–54. doi: 10.2519/jospt.2019.8190. [DOI] [PubMed] [Google Scholar]
- 23.Welling W, Benjaminse A, Seil R, Lemmink K, Zaffagnini S, Gokeler A. Low rates of patients meeting return to sport criteria 9 months after anterior cruciate ligament reconstruction: a prospective longitudinal study. Knee Surg Sports Traumatol Arthrosc . 2018;26(12):3636–3644. doi: 10.1007/s00167-018-4916-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Toole AR, Ithurburn MP, Rauh MJ, Hewett TE, Paterno MV, Schmitt LC. Young athletes cleared for sports participation after anterior cruciate ligament reconstruction: how many actually meet recommended return-to-sport criterion cutoffs? J Orthop Sports Phys Ther . 2017;47(11):825–833. doi: 10.2519/jospt.2017.7227. [DOI] [PubMed] [Google Scholar]
- 25.Wellsandt E, Failla MJ, Snyder-Mackler L. Limb symmetry indexes can overestimate knee function after anterior cruciate ligament injury. J Orthop Sports Phys Ther . 2017;47(5):334–338. doi: 10.2519/jospt.2017.7285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sousa PL, Krych AJ, Cates RA, Levy BA, Stuart MJ, Dahm DL. Return to sport: does excellent 6-month strength and function following ACL reconstruction predict midterm outcomes? Knee Surg Sports Traumatol Arthrosc . 2017;25(5):1356–1363. doi: 10.1007/s00167-015-3697-2. [DOI] [PubMed] [Google Scholar]
- 27.Di Stasi SL, Logerstedt D, Gardinier ES, Snyder-Mackler L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med . 2013;41(6):1310–1318. doi: 10.1177/0363546513482718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Welling W, Benjaminse A, Seil R, Lemmink K, Gokeler A. Altered movement during single leg hop test after ACL reconstruction: implications to incorporate 2-D video movement analysis for hop tests. Knee Surg Sports Traumatol Arthrosc . 2018;26(10):3012–3019. doi: 10.1007/s00167-018-4893-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young athletes with quadriceps femoris strength asymmetry at return to sport after anterior cruciate ligament reconstruction demonstrate asymmetric single-leg drop-landing mechanics. Am J Sports Med . 2015;43(11):2727–2737. doi: 10.1177/0363546515602016. [DOI] [PubMed] [Google Scholar]
- 30.Slater LV, Hart JM, Kelly AR, Kuenze CM. Progressive changes in walking kinematics and kinetics after anterior cruciate ligament injury and reconstruction: a review and meta-analysis. J Athl Train . 2017;52(9):847–860. doi: 10.4085/1062-6050-52.6.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med . 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc . 2017;25(1):192–199. doi: 10.1007/s00167-016-4246-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chao W-C, Shih J-C, Chen K-C, Wu C-L, Wu N-Y, Lo C-S. The effect of functional movement training after anterior cruciate ligament reconstruction: a randomized controlled trial. J Sport Rehabil . 2018;27(6):541–545. doi: 10.1123/jsr.2017-0022. [DOI] [PubMed] [Google Scholar]
- 34.Chmielewski TL, Jones D, Day T, Tillman SM, Lentz TA, George SZ. The association of pain and fear of movement/reinjury with function during anterior cruciate ligament reconstruction rehabilitation. J Orthop Sports Phys Ther . 2008;38(12):746–753. doi: 10.2519/jospt.2008.2887. [DOI] [PubMed] [Google Scholar]
- 35.Lentz TA, Zeppieri G, Jr, George SZ, et al. Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med . 2015;43(2):345–353. doi: 10.1177/0363546514559707. [DOI] [PubMed] [Google Scholar]
- 36.Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport . 2008;9(1):9–15. doi: 10.1016/j.ptsp.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 37.Lentz TA, Paterno MV, Riboh JC. So you think you can return to sport? Br J Sports Med . 2018;52(23):1482–1483. doi: 10.1136/bjsports-2017-099006. [DOI] [PubMed] [Google Scholar]
- 38.McPherson AL, Feller JA, Hewett TE, Webster KE. Psychological readiness to return to sport is associated with second anterior cruciate ligament injuries. Am J Sports Med . 2019;47(4):857–862. doi: 10.1177/0363546518825258. [DOI] [PubMed] [Google Scholar]
- 39.Paterno MV, Flynn K, Thomas S, Schmitt LC. Self-reported fear predicts functional performance and second ACL injury after ACL reconstruction and return to sport: a pilot study. Sports Health . 2018;10(3):228–233. doi: 10.1177/1941738117745806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McPherson AL, Feller JA, Hewett TE, Webster KE. Smaller change in psychological readiness to return to sport is associated with second anterior cruciate ligament injury among younger patients. Am J Sports Med . 2019;47(5):1209–1215. doi: 10.1177/0363546519825499. [DOI] [PubMed] [Google Scholar]
- 41.Paterno MV, Thomas S, VanEtten KT, Schmitt LC. Confidence, ability to meet return to sport criteria, and second ACL injury risk associations after ACL-reconstruction. J Orthop Res . 2022;40(1):182–190. doi: 10.1002/jor.25071. [DOI] [PubMed] [Google Scholar]