Abstract
Aims
The protracted COVID-19 pandemic has overwhelmed health systems globally, including many aspects of cancer control. This has underscored the multidimensional nature of cancer control, which requires a more comprehensive approach involving taking a wider perspective of health systems. Here, we investigated aspects of health system resilience in maintaining cancer services globally during the COVID-19 pandemic. This will allow for health systems to be resilient to different types of system stressors/shocks in the future, to allow cancer care to be maintained optimally.
Materials and methods
Using the World Health Organization health system framework (capturing aspects of service delivery, health workforce, information, medical products, vaccines and technologies, financing and governance and leadership), we carried out a comparative analysis of the impact of COVID-19 and the synthesis of the findings in responses in cancer care in 10 countries/jurisdictions across four continents comprising a wide diversity of health systems, geographical regions and socioeconomic status (China, Colombia, Egypt, Hong Kong SAR, Indonesia, India, Singapore, Sri Lanka, UK and Zambia). A combination of literature and document reviews and interviews with experts was used.
Results
Our study revealed that: (i) underlying weaknesses of health systems before the pandemic were exacerbated by the pandemic (e.g. economic issues in low- and middle-income countries led to greater shortage of medication and resource constraints compounded by inadequacies of public financing and issues of engagement with stakeholders and leadership/governance); (ii) no universal adaptive strategies were applicable to all the systems, highlighting the need for health systems to design emergency plans based on local context; (iii) despite the many differences between health systems, common issues were identified, such as the lack of contingency plan for pandemics, inadequate financial policies for cancer patients and lack of evidence-based approaches for competing priorities of cancer care/pandemic control.
Conclusion
We identified four key points/recommendations to enhance the resilient capacity of cancer care during the COVID-19 pandemic and other system stressors: (i) effective pandemic control approaches in general are essential to maintain the continuity of cancer care during the emergency health crises; (ii) strong health systems (with sufficient cancer care resources, e.g. health workforce, and universal health coverage) are fundamental to maintain quality care; (iii) the ability to develop response strategies and adapt to evolving evidence/circumstances is critical for health system resilience (including introducing systematic, consistent and evidence-based changes, national support and guidance in policy development and implementation); (iv) preparedness and contingency plans for future public health emergencies, engaging the whole of society, to achieve health system resilience for future crises and to transform healthcare delivery beyond the pandemic.
Key words: Cancer, COVID-19, health policy, health systems, resilience
Introduction
The protracted COVID-19 pandemic has overwhelmed different health systems for over 2 years and continues to cause significant disruption globally. Public health measures to prevent the transmission of the novel coronavirus SARS-CoV-2 to allow the continuation of essential healthcare services, including services for cancer care, have proved to be a great challenge. Many aspects of cancer control have been affected globally by the pandemic. There have been delays and a reduction in cancer services [1,2] with a decline in new cancer diagnoses due to the disruption of screening [3] and referrals [4]. The delivery of treatment has also been adversely affected, including chemotherapy, radiotherapy [[5], [6], [7]] and surgery [8], as well as hospital and outpatient visits and palliative care [[9], [10], [11]]. A study modelled that a 3-month/6-month delay in surgery for operable cancers led to a 19%/43% change in life-years, highlighting the impact of survival due to delay [12]. In addition to clinical services, several aspects of cancer research and related activities were also adversely affected [[13], [14], [15]]. These diverse aspects of cancer services being affected have underscored that cancer control requires a multidimensional approach, as recommended by the World Health Organization (WHO) cancer control frameworks [16]. A comprehensive approach taking into account the wider perspective of health systems to maintain cancer control is therefore important.
Strategies and changes related to cancer care services during the pandemic have been reported in different countries throughout the pandemic; most studies being institutional-based and focused primarily on healthcare delivery. For example, frameworks have been developed for cancer treatment prioritisation during the pandemic [17,18]. Telemedicine strategies, like virtual tumour board, virtual outpatient counselling and medication management, have also been implemented following social distancing measures [19]. Some institutions learnt to improve practices around infection control and to transit continued care delivery to outpatient settings [20]. There was also a coming together of cancer specialists in solidarity to maintain cancer care, with adaptive treatment approaches such as the rapid implementation of the hypofractionation schedule for breast radiotherapy [21]. The effect of all these adaptive strategies to maintain cancer care is ultimately influenced by how different health systems are organised, governed and financed.
In view of the above, we have applied the concept of health system resilience to cancer care, which focuses on the need to improve the functioning of health systems not only to meet emerging health needs caused by unforeseen shocks, but also to provide effective care for routine health needs [22,23]. Resilience is defined as the ability to absorb, adapt and transform from shocks [24]. Several factors are important for countries to build up resilience; improving the organisation of health systems and pandemic preparedness, prioritising and ensuring equity in access to essential health services, building trust in governance and leadership through community engagement and identifying health system gaps for preparedness, readiness and responses to public health management [25].
The COVID-19 pandemic has therefore acted as a call to evaluate and enhance the resilience of health systems [26]. Taking this perspective [22], we investigated aspects of health system resilience in maintaining cancer services globally during the COVID-19 pandemic. Multiple jurisdictions with diverse systems and geographical regions were selected and responses and adaptations were identified.
Materials and Methods
This was a comparative analysis of the impact of COVID-19 and the synthesis of the findings in responses in cancer care in 10 countries/jurisdictions, through a combination of literature and document review and interviews with experts. Oncologists from 10 countries/jurisdictions across four continents with a wide range of health system organisations were recruited as coinvestigators for the study. The investigators were from China, Colombia, Egypt, Hong Kong SAR, Indonesia, India, Singapore, Sri Lanka, UK and Zambia; they were recruited from the participants of the global health webinars addressing the impact and mitigation strategies of COVID-19 and oncology care in 2020 and 2021. This was expanded to other jurisdictions in a purposeful attempt to cover countries with a wide diversity of health systems, geographical regions and socioeconomic status. The study received ethical approval from an academic institution.
Our conceptual framework was grounded in the WHO health system framework, which consists of six building blocks, namely service delivery, health workforce, information, medical products, vaccines and technologies, financing, and governance and leadership [27]. We developed the data collection instrument based on the WHO health system framework, capturing the health system characteristics, impact on cancer care, adaptations and innovations, and key lessons learnt for health system resilience. Data were collected from the literature, official documents and websites, institutional guidelines and instructions and supplementary data were also collected by investigators from interviews of relevant experts and decision-makers. A series of web-based deliberations were conducted to generate a common understanding and agreement of the study, the data collection instrument and the data to be collected.
The panel was engaged in a collaborative-learning approach to discuss the analysis and synthesis of the codified information, to generate the findings for the study and the implications for health systems resilience in the global context.
Results
As shown in Table 1 , this study included 10 countries, covering four continents, with a wide diversity in terms of demographics, socioeconomics and health system characteristics. Participating jurisdictions consisted of three high-income regions, two upper–middle-income countries and five lower–middle-income countries, assigned accordingly to their gross domestic product (GDP) per capita. The population size of the jurisdictions varied from around 5 million to 1400 million. According to 2019 data, two regions had their average life expectancy at birth lower than 70 years, five regions had it between 70 and 80 years and three regions were reported to have it higher than 80 years. The jurisdictions shared a mixture of different health financing systems. Three jurisdictions had higher than 6% of GDP as health expenditure in 2019, whereas six had 3–6% and one had lower than 3%.
Table 1.
Economic, demographic and health system characteristics of 10 jurisdictions
| Jurisdiction | Income category | GDP per capita (USD constant 2005) | Population size (1000) | Infant mortality rate (deaths/1000 live births) | Life expectancy at births (years) | Health spending (%GDP) | Government health spending (% of total health expenditure) | Out-of-pocket health spending (% of total health expenditure) |
|---|---|---|---|---|---|---|---|---|
| China | Upper middle | 10 170 | 1 433 784 | 9.595 | 76.91 | 5.4 | 56.0 | 35.2 |
| Colombia | Upper middle | 6546 | 50 339 | 12.315 | 77.29 | 7.7 | 71.9 | 14.9 |
| Egypt | Lower middle | 3019 | 100 388 | 15.117 | 71.80 | 4.7 | 27.8 | 62.7 |
| Hong Kong | High | 48 354 | 7507 | 1.292 | 85.08 | 6.5 | 53.5 | 29.6 |
| India | Lower middle | 2101 | 1 366 417 | 30.924 | 69.66 | 3.0 | 32.8 | 54.8 |
| Indonesia | Lower middle | 4196 | 270 626 | 18.311 | 71.72 | 2.9 | 48.9 | 34.8 |
| Singapore | High | 65 641 | 5804 | 1.584 | 83.50 | 4.1 | 51.7 | 30.2 |
| Sri Lanka | Lower middle | 3852 | 21 800 | 7.347 | 76.89 | 3.9 | 47.2 | 45.4 |
| UK | High | 42 417 | 67 530 | 3.678 | 81.20 | 10.2 | 79.5 | 17.1 |
| Zambia | Lower middle | 1272 | 17 861 | 44.358 | 63.89 | 5.3 | 40.1 | 10.2 |
GDP, gross domestic product.
Data sources: GDP per capita, population size, life expectancy at birth: the World Bank (https://www.worldbank.org/en/home).
infant mortality rate: UN Inter-agency Group for Child Mortality Estimation (https://childmortality.org/), health spending (https://apps.who.int/nha/database/Home/Index/en), Hong Kong (https://www.healthbureau.gov.hk/statistics/download/dha/en/dha_summary_report_1920.pdf).
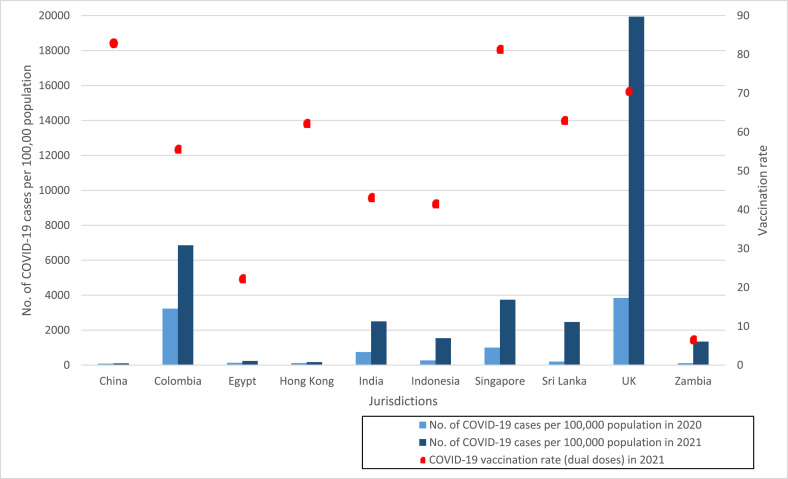
In terms of COVID-19, as shown in Figure 1 , participating jurisdictions generally had an increased number of cases in 2021 compared with 2020. COVID-19 vaccination rates in the jurisdictions were also diverse. Up to 2021, there were two jurisdictions with a higher than 75% vaccination rate of dual doses, four with 50–75%, two with 25–50% and two with a lower than 25% vaccination rate. We organised our results into six domains using the WHO health system framework. The adaptive strategies implemented in each domain to reduce the disruption of cancer care during the pandemic are summarised in Table 2 . Summaries of collected data can be found in the Supplementary Material.
Fig 1.
COVID-19 cases and vaccination rates in 2020 and 2021 in the health systems included.
Table 2.
Adaptive strategies targeting cancer care implemented in 2020 and 2021
| Adaptive policies | 2020 | 2021 |
|---|---|---|
| Healthcare delivery – any adaptive strategies implemented to reduce the exposure to COVID-19 and maintain the capacity/services for cancer patients with limited resource constraint | ||
| 1. Telemedicine |
|
|
| 2. Restructure the cancer care provider system |
|
|
| 3. Reduction of supportive treatments |
|
|
| 4. Adaptation of treatment |
|
|
| 5. Prioritisation and triage |
|
|
| 6. Reduction of palliative care |
|
|
| 7. Reduction of patient involvement in clinical trials and research |
|
|
| Healthcare workforce – any adaptive strategies implemented to maintain training of oncology professionals | ||
| 1. Online seminars/classes |
|
|
| 2. Restructure training and teaching into smaller groups |
|
|
| 3. Restructure the training syllabus |
|
|
| Healthcare workforce – any adaptive strategies implemented to maintain the cancer service workforce | ||
| 1. Rapid COVID-19 testing |
|
|
| 2. Relocation of healthcare workforce to one or selected institutions |
|
|
| 3. Work-from-home arrangement for supporting staffs |
|
|
| 4. Psychological support interventions |
|
|
| 5. Sympathetic working scheduling |
|
|
| 6. Outsourcing of treatment services |
|
|
| Information – any adaptive strategies implemented to provide related information about cancer services | ||
| 1. Tailored public health messaging for patients about the risk of COVID-19 |
|
|
| 2. Evidence-based information for healthcare workers to manage cancer patients at risk of COVID-19 |
|
|
| 3. Evidence-based guidance for the healthcare workers to ration healthcare resources |
|
|
| Health financing – any adaptive strategies implemented to enhance financial affordability of cancer patients | ||
| 1. Government cancer funding/financial assistance |
|
|
| 2. NGO-related initiatives and financial assistance |
|
|
NGO, non-government organisation.
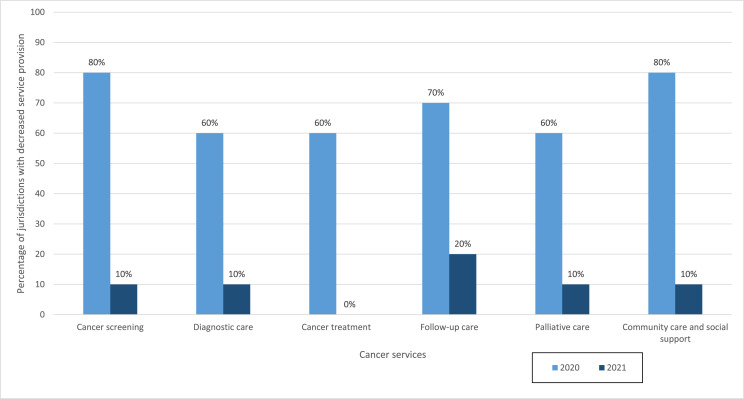
Service Delivery
Figure 2 shows the disruptions of different types of cancer care in 2020 and 2021. In 2020, cancer services, including cancer diagnosis and treatment, were reported to decrease in health systems with a large number of COVID-19 cases, i.e. Colombia, Egypt, India, Indonesia, UK and Zambia, compared with 2019. Except for the UK, the magnitude of the decrease was reported to be moderate or substantial. Only China and Hong Kong reported increases in cancer diagnosis and treatment (Supplementary Table S1). Similar trends were also observed in cancer screening, follow-up and palliative care, and home and social care.
Fig 2.
Decrease in service provision of cancer control continuum reported by the 10 health systems in 2020 and 2021.
The situation of cancer service delivery generally did not worsen in 2021. Fewer countries reported delays in care due to the COVID-19 outbreak, while most countries recorded increased or no change in cancer diagnosis and treatment compared with 2020 (Supplementary Table S1). Some countries that experienced a substantial increase in COVID-19 cases in 2021 recorded worsening cancer service delivery.
Almost all jurisdictions, irrespective of the prevalence of COVID-19 cases, introduced adaptive strategies to maintain cancer services in 2020 (Table 2). At a micro-level, or patient care level, the most commonly reported strategy was the use of telemedicine, followed by an adaptation of treatment (e.g. modification of surgery, an altered fraction of radiotherapy and dose-scheduling of chemotherapy), reduction of supportive treatment (e.g. rehabilitation and allied health services) and a reduction in palliative care. At a meso-level, all the jurisdictions except Hong Kong reported the strategy of prioritisation and triage (e.g. to prioritise critical treatment and postponement of non-emergency treatment) and the restructure of cancer care provider systems (e.g. transfer cancer care to one or selected institutions). Furthermore, most systems reported a reduction in patient involvement in clinical trials and research. Telemedicine, an adaptation of treatment, and service prioritisation and triage were suggested to be the most effective in maintaining the capacity of cancer patients with limited resources during the pandemic, while the effectiveness of other strategies was reported to be minimal.
The magnitude of adaptive strategies generally increased, especially for telemedicine, whereas other strategies experienced a reduction in scale or were cancelled in response to the control of the pandemic; for example, China cancelled the prioritisation of patients when the COVID-19 outbreak was under control in 2021.
Health Workforce
In 2020, cancer care manpower was generally affected in all jurisdictions during the pandemic, except Sri Lanka, and most of the countries with high COVID-19 cases reported moderate and substantial reallocation/loss of manpower and suspension of professional training due to the outbreak (Supplementary Table S2). However, there were still enough personnel to provide uninterrupted cancer treatment and care in most of the jurisdictions, except for some Southeast Asian countries.
Infection rates among cancer healthcare professionals were generally the same in 2021 compared with 2020. There was a loss of manpower in all jurisdictions mainly due to reallocation to COVID-19-related services. Some countries, like India, Indonesia and Egypt, reported minor improvements, whereas some jurisdictions started to experience insufficient labour to provide cancer treatments in 2021 (e.g. Zambia and the UK; see Supplementary Table S2).
Adaptive strategies were implemented in most jurisdictions to maintain the cancer service workforce in 2020 (Table 2). Work-from-home arrangements were most popular to facilitate social distancing in institutions for supporting staff, except in Sri Lanka. Other supportive measures, such as rapid COVID-19 testing, psychological support interventions and sympathetic work scheduling, were also common and were reported to be effective in multiple countries. Some jurisdictions arranged some services to other providers to reduce workloads or the relocation of healthcare workforce to selected institutions. However, the effectiveness of these strategies was reported to be limited. In addition, most countries tried to maintain training through online seminars, which proved to be successful, whereas others tried to restructure the teaching syllabus and reduce class group sizes.
In 2021, in response to the situation, adaptive strategies, like rapid COVID-19 testing, were enhanced in order to contain the outbreak within hospitals and to free more personnel. In particular, Egypt started to implement multiple manpower-related adaptive strategies in 2021. In terms of professional training, further increases in online classes and restructuring into smaller teaching groups were carried out to reduce physical contact.
Information
As shown in Table 2, most of the countries provided COVID-19-related information to patients and healthcare professionals in 2020, including tailored messages to patients about the risks of COVID-19 and the risks of cancelling and delaying cancer services. Guidance and information for healthcare workers to balance the risks of COVID-19 and the benefits of cancer procedures and ration healthcare resources were also provided in different countries. Most countries increased the intensity of providing relevant information to both patients and healthcare workers, especially the evidence-based information for healthcare workers to manage the patients at risk of COVID-19, in 2019. In general, countries with substantial coverage of the intended audience reported that the information was effective.
Medical Products, Vaccines and Technologies
Access to cancer-related resources was affected during 2020 (Supplementary Table S3). Medications and radiotherapy services were mainly affected in low- and middle-income countries (LMICs). The supply of personal protective equipment (PPE) was mainly adequate for professionals, but there was insufficient supply for caregivers and patients in some LMICs. COVID-19 testing was mandatory for patients in most countries, while fewer countries required testing for caregivers and professionals. Most countries had sufficient COVID-19 testing for all stakeholders.
In 2021, the supply of cancer medications and access to radiotherapy services were slightly improved in general, whereas some LMICs, such as Indonesia and Zambia, were still experiencing reductions (Supplementary Table S3). In terms of COVID-19-related resources, PPE supply had become sufficient in most countries. Most of the countries also had adequate COVID-19 testing supplies. New policies in the requirements of viral testing were further implemented in a few countries as the pandemic evolved through 2021; for example, viral testing was required before cancer treatment in Indonesia. COVID-19 vaccines, introduced in 2021, were also reported to be generally sufficient and evenly distributed in each country. Policies related to vaccination were initiated when different jurisdictions started public vaccination, for example, Hong Kong required frequent testing for individuals who were not vaccinated, Sri Lanka carried out patient education, whereas some countries, such as China, implemented compulsory vaccination. Involvement of the media in promoting vaccine uptake was also seen in some countries, such as Colombia. At the same time, countries with high vaccination rates, like the UK, did not implement strategies to incentivise vaccination uptake.
Financing
As presented in Supplementary Table S4, in 2020, most of the LMICs not achieving universal health coverage reported increased numbers of patients facing difficulties in paying for treatment due to the adverse economic impact of the pandemic, necessitating the need to delay or cancel treatments. However, most of the countries did not provide any adaptive strategies to assist cancer patients financially at the beginning of the pandemic, except for Sri Lanka, which reported financial assistance from non-government organisations (NGOs). The economic status of patients in LMICs did not improve in 2021 as the pandemic continued, while the situation of some countries worsened. Only Sri Lanka had adaptive strategies, like engaging NGO assistance; Indonesia introduced minor government and NGO financial assistance for cancer patients, while other jurisdictions did not implement relevant strategies.
Governance and Leadership
In 2020, civil society, including NGOs and volunteers, were more involved in the emergency responses of cancer services in some LMICs (Supplementary Table S5). The private sector in most countries was also involved in emergency responses to COVID-19 to maintain cancer care, except in Hong Kong and the UK. Most countries did not develop a contingency framework for patient and treatment prioritisation until the time of the pandemic and the entity responsible for prioritisation was generally at the hospital level. Most of the countries had communication channels and crisis response teams in response to the pandemic.
In 2021, most governments maintained current frameworks, communication channels and crisis response teams. China removed prioritisation and provided the full scope of state-of-the-art services due to rapid responses to COVID-19 risk strategies and a low number of cases that did not affect cancer services. Hong Kong still did not establish prioritisation frameworks and communication channels as their cancer services were also not affected during this period.
Discussion
This cross-country comparative study examined health system resilience in maintaining cancer care during the global pandemic. Using the WHO health system framework, we examined the impact of COVID-19 on cancer care in 2020 and 2021. We identified various health systems' responses to maintain cancer care and the functioning of health systems over the 2 years. Although there were no universal strategies applicable to all health systems, common issues were identified, such as the lack of preparedness and contingency plans for public health emergencies, the lack of financial support for patients during the pandemic and the lack of special arrangements to protect cancer patients and their carers from COVID-19 health risks in almost all systems. These were more pronounced in health systems with underlying weaknesses.
Health system resilience is about enhancing the capacity to proactively and positively manage unforeseen shocks by absorbing, adapting and transforming. With this perspective, we categorised the lessons learnt from the pandemic into four aspects to enhance cancer service resilience and capacity: (i) effective management control of the COVID-19 outbreak in general serves as the foundation to reduce disruption during the pandemic; (ii) Health system functions should be improved beyond the pandemic as underlying weaknesses can be exacerbated during shocks and stressors; (iii) introducing adaptive strategies during the pandemic is critical to maintain health system functions and reduce the consequences of unpreparedness. This can be facilitated by national support and guidance during implementation, which may lead to transformative changes upon institutionalisation; (iv) governments should develop preparedness and contingency plans for future public health emergencies to enable a systematic and effective response to maintain essential services, like cancer care. The above can enhance adaptive capacity and allow for transformative changes that will yield benefits beyond the pandemic.
Management of the COVID-19 Outbreak
Health systems that effectively contained the spread of COVID-19 reported the least disruption of cancer care. With the evolving epidemiological situation and the emerging new evidence, health systems in our study also adapted their strategies over time, such as introducing rapid antigen tests and promoting universal vaccination to patients and healthcare workers, in order to contain the spread of COVID-19 and to reduce infection-related mortality.
Even though cancer patients are a vulnerable population with a high risk of infection and mortality from COVID-19 [5], we found the protection of cancer patients from the health risks of COVID-19 to be inadequate. PPE supply for cancer patients and their carers in 2020 was reported to be insufficient in some LMICs, and the vaccination of cancer patients was reported to be suboptimal, partly due to public ambivalence and reluctance to vaccinate in multiple health systems. National support is needed for special arrangements for cancer patients when allocating resources to protect them from the health risks of COVID-19 or future public health emergencies.
Improving the Functioning of Health Systems
Our research found that the weakness of health systems before the pandemic was exacerbated by the pandemic; such as in some LMICs with inadequate resources [28]. During the pandemic, limited cancer care resources, such as a professional workforce, medication, chemotherapy and brachytherapy sources, were a major challenge in LMICs. The slowing of economic growth exacerbated the problem further. Recent WHO data showed that Southeast Asia and Africa contributed only 1–2% of global spending on health in 2020 [29].
The lack of universal healthcare coverage is another significant weakness in LMICs. The impact of the pandemic has been most severe in countries that rely on out-of-pocket payments or lack public financing. For example, in India, over 50% of healthcare expenditure is from out-of-pocket payments. Hence, all health system functions were vulnerable during the pandemic, and the increasing financial burden led to disrupted cancer care. Proper provision of publicly funded health care is critical to mitigate the disruption due to future pandemics.
Although systems provided good essential care before the pandemic in, for example, Hong Kong, Singapore and the UK, a shortage of healthcare workers has long been an issue in these health systems due to the rapid growth of an aging population and chronic diseases. The pandemic further highlighted inadequacies in the healthcare workforce at all levels from doctors to carers, which has been reported to be the most vulnerable part of these health systems. Long-term strategies are needed to mitigate this, with buffers to allow the operation of cancer services efficiently and to prevent these services from being overwhelmed by future shocks.
Adaptive Strategies to Reduce the Consequences of Unpreparedness
We found that all the systems introduced adaptive strategies to maintain cancer care in 2020 and made further adaption in 2021 in response to the evolving epidemiological situation. As an example, in the aspect of care delivery, all systems except Hong Kong adapted their cancer treatment care to mitigate the disruption of the COVID-19 pandemic, with all countries doing so in 2020 and Singapore in 2021; these measures were generally reported to be effective. Other effective strategies reported included introducing telemedicine to minimise virus transmission while maintaining care, providing rapid COVID-19 tests, psychological support, sympathetic work scheduling to maintain the workforce, providing tailored information to patients for them to balance the risk of infection and the benefits of receiving treatment and providing guidance and communication channels by governments to hospitals. Comparing 2021 with 2020, although most jurisdictions experienced an increase in the number of COVID-19 cases, the situation of cancer services was not reported to be worse in 2021 in the health systems studied. These measures may have played an important role in strengthening health system resilience to maintain care during the pandemic.
There were also some measures reported to have limited effectiveness. According to expert opinion, the adaptive strategies not effective in maintaining healthcare services and workforce include reorganising the cancer care provider system, reducing supportive treatments and palliative care, reducing patient involvement in clinical trials, relocating the healthcare workforce to one or selected institutions and arranging for support staff to work from home. These measures were intuitively designed to protect healthcare resources, but the implementation could be inhibited by some factors. For example, ‘work-from-home arrangements’ were designed to minimise the risks of COVID-19 transmission, but could be challenging in some LMICs due to limited resources, in particular human resources and access to electronic devices. Even though some adaptive strategies were not applicable in all countries, other strategies, such as psychological support and sympathetic work scheduling, with low cost and relative ease of implementation, are worthy of attention in all countries, especially LMICs. Further research is needed to examine the effectiveness of these measures and to identify different facilitators and inhibitors of implementation in different health systems.
Although we did not find adaptation strategies that were universally applicable to all systems, some common issues merit attention, such as the lack of financial policies to address the economic problems facing cancer patients during pandemics and the inadequate communication with patients to calm the anxiety of infection. More importantly, we identified an imperative need for better communications of the strategies between governments and healthcare providers when responding to fast-changing epidemiological situations and evolving scientific evidence [30].
Preparedness Plan for Future System Shocks, Including Pandemics
Almost all of the health systems in our study did not have preparedness and contingency plans for adaption and prioritisation of services until the pandemic, even in countries previously scoring well in traditional health security and universal health coverage. Because of the lack of preparedness of many health systems during the COVID-19 pandemic, many adaptations were implemented expeditiously, encountering challenges in implementation and resulting in limited effectiveness. This is consistent with the fact that the current global health security systems mainly focus on pandemic prevention and detection with less emphasis on managing the response [31]. Governments should have emergency health crisis protocols prepared ahead of time that can be implemented immediately at the time of crisis so that the departments and institutions can work together with healthcare staff to deliver strategies systematically and effectively. Furthermore, the preparedness plan can guide the engagement of civil society and private (both for-profit and not-for-profit) sectors, which requires mutual trust and communication channels to be built up beforehand.
Adaptive strategies that were found to be effective during the COVID-19 pandemic can be further integrated into preparedness plans for future shocks. Furthermore, the transformation of health systems could be required as part of preparedness planning. For example, implementing telemedicine requires prior preparation of relevant resources, such as electronic devices, for integration into routine practice. Preceding readiness could tackle weaknesses and barriers during implementation.
Conclusion
Using the health system framework, our research identified four key points to enhance the resilient capacity of cancer care during the COVID-19 pandemic and beyond. First, effective management and control of COVID-19 are critical to maintaining cancer care. Second, a strong health system with sufficient cancer care resources, for example, a healthcare workforce, and universal health coverage play a fundamental role to maintain quality care. Continuous efforts to address fundamental gaps in health systems and cancer control plans are therefore needed, not only to achieve population health, but also to prepare for future shocks or stressors to health systems, including emergency health crises. Third, the ability to develop response strategies and related measures on time and adapt the strategies to evolving evidence and changing circumstances is critical [32,33]. Specifically, to introduce systematic, consistent and evidence-based changes, national support and guidance are important in the development and implementation of policy. Last, but not least, preparedness and contingency plans for future public health emergencies to enable systematic and effective response will be needed, which will also facilitate the preparedness of engaging the whole society and transform healthcare delivery beyond the pandemic.
Ethics approval
The study received ethical approval from the Survey and Behavioral Research Ethics Committee of the Chinese University of Hong Kong (reference no. SBRE-21-0675).
Author contributions
KY is the guarantor of integrity of the entire study. KY, YW and EKY were responsible for study concepts and design. KY, YW and HMS carried out the literature research.
KY, YW, SC, GE, SG, NJ, AWML, HHL, SCM-C, AVO, BFT, TR, HMS and EKY were responsible for experimental studies/data analysis. KY, YW and HMS carried out the statistical analysis. KY, YW, SC, GE, SG, NJ, AWML, HHL, SCM-C, AVO, BFT, TR, HMS and EKY prepared and edited the manuscript.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgement
The authors acknowledge the Royal College of Radiologists, London, UK for hosting and co-ordinating the RCR Learning Series on the Global Impact of COVID-19 on Cancer and Natalie McGregor for her help in the coordination and organisation of the RCR Learning series and in this study. The Centre for Health Systems and Policy Research, Chinese University of Hong Kong, funded by The Tung Foundation, is acknowledged for their support throughout the conduct of this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.clon.2023.01.004.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Multimedia component 1
References
- 1.Greenwood E., Swanton C. Consequences of COVID-19 for cancer care – a CRUK perspective. Nat Rev Clin Oncol. 2021;18:3–4. doi: 10.1038/s41571-020-00446-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . World Health Organization; Geneva: 2022. Third round of the global pulse survey on continuity of essential health services during the COVID-19 pandemic: November–December 2021: interim report, 7 February 2022. [Google Scholar]
- 3.Patt D., Gordan L., Diaz M., Okon T., Grady L., Harmison M., et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform. 2020;4:1059–1071. doi: 10.1200/CCI.20.00134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morris E.J.A., Goldacre R., Spata E., Mafham M., Finan P.J., Shelton J., et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol. 2021;6:199–208. doi: 10.1016/S2468-1253(21)00005-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuderer N.M., Choueiri T.K., Shah D.P., Shyr Y., Rubinstein S.M., Rivera D.R., et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395:1907–1918. doi: 10.1016/S0140-6736(20)31187-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lai A.G., Pasea L., Banerjee A., Hall G., Denaxas S., Chang W.H., et al. Estimated impact of the COVID-19 pandemic on cancer services and excess 1-year mortality in people with cancer and multimorbidity: near real-time data on cancer care, cancer deaths and a population-based cohort study. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-043828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spencer K., Jones C.M., Girdler R., Roe C., Sharpe M., Lawton S., et al. The impact of the COVID-19 pandemic on radiotherapy services in England, UK: a population-based study. Lancet Oncol. 2021;22:309–320. doi: 10.1016/S1470-2045(20)30743-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.COVIDSurg Collaborative Effect of COVID-19 pandemic lockdowns on planned cancer surgery for 15 tumour types in 61 countries: an international, prospective, cohort study. Lancet Oncol. 2021;22:1507–1517. doi: 10.1016/S1470-2045(21)00493-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmidt A.L., Bakouny Z., Bhalla S., Steinharter J.A., Tremblay D.A., Awad M.M., et al. Cancer care disparities during the COVID-19 pandemic: COVID-19 and cancer outcomes study. Cancer Cell. 2020;38:769–770. doi: 10.1016/j.ccell.2020.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guven D.C., Aktas B.Y., Aksun M.S., Ucgul E., Sahin T.K., Yildirim H.C., et al. COVID-19 pandemic: changes in cancer admissions. BMJ Support Palliat Care. 2020 doi: 10.1136/bmjspcare-2020-002468. [DOI] [PubMed] [Google Scholar]
- 11.Amador M., Matias-Guiu X., Sancho-Pardo G., Contreras Martinez J., de la Torre-Montero J.C., Penuelas Saiz A., et al. Impact of the COVID-19 pandemic on the care of cancer patients in Spain. ESMO Open. 2021;6 doi: 10.1016/j.esmoop.2021.100157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sud A., Jones M.E., Broggio J., Loveday C., Torr B., Garrett A., et al. Collateral damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann Oncol. 2020;31:1065–1074. doi: 10.1016/j.annonc.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zon L., Gomes A.P., Cance W.G., Ribas A., Tuveson D., Postel-Vinay S., et al. Impact of COVID-19 pandemic on cancer research. Cancer Cell. 2020;38:591–593. doi: 10.1016/j.ccell.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boughey J.C., Snyder R.A., Kantor O., Zheng L., Chawla A., Nguyen T.T., et al. Impact of the COVID-19 pandemic on cancer clinical trials. Ann Surg Oncol. 2021;28:7311–7316. doi: 10.1245/s10434-021-10406-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewis P.J., Morris E.J.A., Chan C.S.K., Darley K., Sebag-Montefiore D., Evans M. COVID RT – assessing the impact of COVID-19 on radiotherapy in the UK. A National Cancer Research Institute Clinical and Translational Radiotherapy Research Working Group Initiative in Partnership with the Royal College of Radiologists, the Society of Radiographers and the Institute of Physics and Engineering in Medicine. Clin Oncol. 2021;33:e69–e72. doi: 10.1016/j.clon.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization . 1995. National cancer control programmes: policies and managerial guidelines. [Google Scholar]
- 17.Hanna T.P., Evans G.A., Booth C.M. Cancer, COVID-19 and the precautionary principle: prioritizing treatment during a global pandemic. Nat Rev Clin Oncol. 2020;17:268–270. doi: 10.1038/s41571-020-0362-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schrag D., Hershman D.L., Basch E. Oncology practice during the COVID-19 pandemic. JAMA. 2020;323:2005–2006. doi: 10.1001/jama.2020.6236. [DOI] [PubMed] [Google Scholar]
- 19.Jazieh A.R., Akbulut H., Curigliano G., Rogado A., Alsharm A.A., Razis E.D., et al. Impact of the COVID-19 pandemic on cancer care: a global collaborative study. JCO Glob Oncol. 2020;6:1428–1438. doi: 10.1200/GO.20.00351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Graetz D., Agulnik A., Ranadive R., Vedaraju Y., Chen Y., Chantada G., et al. Global effect of the COVID-19 pandemic on paediatric cancer care: a cross-sectional study. Lancet Child Adolesc Health. 2021;5:332–340. doi: 10.1016/S2352-4642(21)00031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brunt A.M., Haviland J.S., Kirby A.M., Somaiah N., Wheatley D.A., Bliss J.M., et al. Five-fraction radiotherapy for breast cancer: FAST-Forward to implementation. Clin Oncol. 2021;33:430–439. doi: 10.1016/j.clon.2021.04.016. [DOI] [PubMed] [Google Scholar]
- 22.Haldane V., Ong S.E., Chuah F.L., Legido-Quigley H. Health systems resilience: meaningful construct or catchphrase? Lancet. 2017;389:1513. doi: 10.1016/S0140-6736(17)30946-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nuzzo J.B., Meyer D., Snyder M., Ravi S.J., Lapascu A., Souleles J., et al. What makes health systems resilient against infectious disease outbreaks and natural hazards? Results from a scoping review. BMC Public Health. 2019;19:1310. doi: 10.1186/s12889-019-7707-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thomas S., Sagan A., Larkin J., Cylus J., Figueras J., Karanikolos M. European Observatory on Health Systems and Policies; Copenhagen: 2020. (Strengthening health systems resilience: key concepts and strategies). PMID: 32716618. [PubMed] [Google Scholar]
- 25.World Health Organization . World Health Organization; Geneva: 2021. Building health systems resilience for universal health coverage and health security during the COVID-19 pandemic and beyond: WHO position paper. [Google Scholar]
- 26.Haldane V., De Foo C., Abdalla S.M., Jung A.S., Tan M., Wu S., et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27:964–980. doi: 10.1038/s41591-021-01381-y. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization . World Health Organization; Geneva: 2010. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. [Google Scholar]
- 28.Horton S., Gauvreau C.L. In: Cancer: disease control priorities. 3rd edition (Volume 3). Washington: Gelband H., Jha P., Sankaranarayanan R., Horton S., editors. The International Bank for Reconstruction and Development / The World Bank; 2015. Cancer in low- and middle-income countries: an economic overview. [PubMed] [Google Scholar]
- 29.World Health Organization . World Health Organization; Geneva: 2020. Global spending on health 2020: weathering the storm. [Google Scholar]
- 30.Al Saidi A.M.O., Nur F.A., Al-Mandhari A.S., El Rabbat M., Hafeez A., Abubakar A. Decisive leadership is a necessity in the COVID-19 response. Lancet. 2020;396:295–298. doi: 10.1016/S0140-6736(20)31493-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wenham C. What went wrong in the global governance of covid-19? BMJ. 2021;372:n303. doi: 10.1136/bmj.n303. [DOI] [PubMed] [Google Scholar]
- 32.Wang Z., Duan Y., Jin Y., Zheng Z.J. Coronavirus disease 2019 (COVID-19) pandemic: how countries should build more resilient health systems for preparedness and response. Glob Health J. 2020;4:139–145. doi: 10.1016/j.glohj.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Graetz D.E., Sniderman E., Villegas C.A., Kaye E.C., Ragab I., Laptsevich A., et al. Resilient health care in global pediatric oncology during the COVID-19 pandemic. Cancer. 2022;128:797–807. doi: 10.1002/cncr.34007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1