Abstract
Lemmel's syndrome is a rare cause of obstructive jaundice caused by a periampullary duodenal diverticulum compressing the intrapancreatic common bile duct with resultant bile duct dilatation, patients with Lemmel's syndrome usually present with abdominal pain or jaundice. Cross-sectional imaging is beneficial in making the diagnosis noninvasively, thus eliminating other pathologies of the peri-ampullary region. Although rare, we recognize the importance of considering this syndrome to be able to make a diagnosis and offer timely treatment. We present 2 cases of Lemmel's syndrome whose diagnosis is retained based on a CT scan and magnetic resonance cholangiopancreatography.
Keywords: Lemmel syndrome, Periampullary duodenal diverticulum, Bile duct obstruction, Imaging
Introduction
Lemmel's syndrome is a rare cause of obstructive jaundice caused by a periampullary duodenal diverticulum compressing the intrapancreatic common bile duct with resultant bile duct dilatation. Duodenal diverticulum occurs in 5 to 10% of the general population; its incidence increases with age [1], and it is generally discovered at the age of 80 years [1]. The duodenal diverticulum often arises out of the second or third part of the duodenum [2]. Juxta-ampullary diverticulum represents 75% of the duodenal diverticula [2], and its wall is located within 2 or 3 cm of the ampulla of Vater [3]. The duodenal diverticulum is mainly asymptomatic and was discovered incidentally [2]; only 1–5% were reported with complications [3]. Lemmel syndrome was first described in 1934 by Lemmel is an infrequent cause of biliary tract obstruction [3]. Its physiopathology isn't specific, but reported mechanisms include three leading causes: chronic fibrosis of the papilla might occur secondary to periampullary diverticulitis and chronic inflammation of the ampulla. Additionally, the location of the duodenal diverticulum may cause the sphincter of Oddi to malfunction, leading to a functional obstruction. Alternatively, obstructive jaundice can result from external compression of the common bile duct or the ampulla of Vater [3]. Imaging plays an essential role in the noninvasive diagnosis of this condition. We report the cases of 2 patients with Lemmel syndrome diagnoses that were retained.
Case reports
Case 1
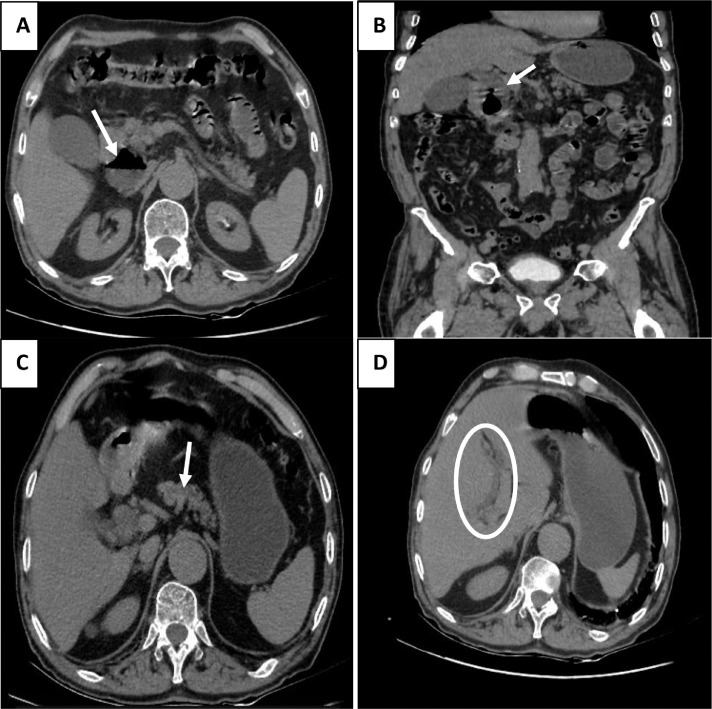
An 80-year-old man without previous pathologic antecedents was admitted to the emergency department for acute abdominal pain. Ultrasound of the abdomen revealed a thin-walled gallbladder with vesicular lithiasis associated with dilatation of the common bile duct measured at 12 mm. A complimentary abdominal CT scan performed showed a periampullary diverticulum containing fluid and air (Fig. 1A), exerting a mass effect on the distal portion of the bile duct (Fig. 1B), causing a dilatation of the common bile duct (12 mm), the Wirsung's duct (6.5 mm) (Fig. 1C), and the proximal intrahepatic bile ducts (Fig. 1D).This diverticulum measures about 54 × 40 × 38 mm (CC × T × AP).
Fig. 1.
1: An 80 years man was admitted for acute abdominal pain. An abdominal CT scan demonstrated a duodenal diverticulum with air-fluid level (A) exerts pressure on the distal end of the common bile duct with resultant upstream dilatation of the common bile duct (B), The Wirsung duct (C), and the proximal intrahepatic bile ducts (D)Hysterosalpingogram image showing beaded appearance of both fallopian tubes with multiple outpouchings (arrows). Contrast from left fallopian tube is seen entering the bowel lumen (arrowhead). No free intraperitoneal spillage of contrast is seen on either side.
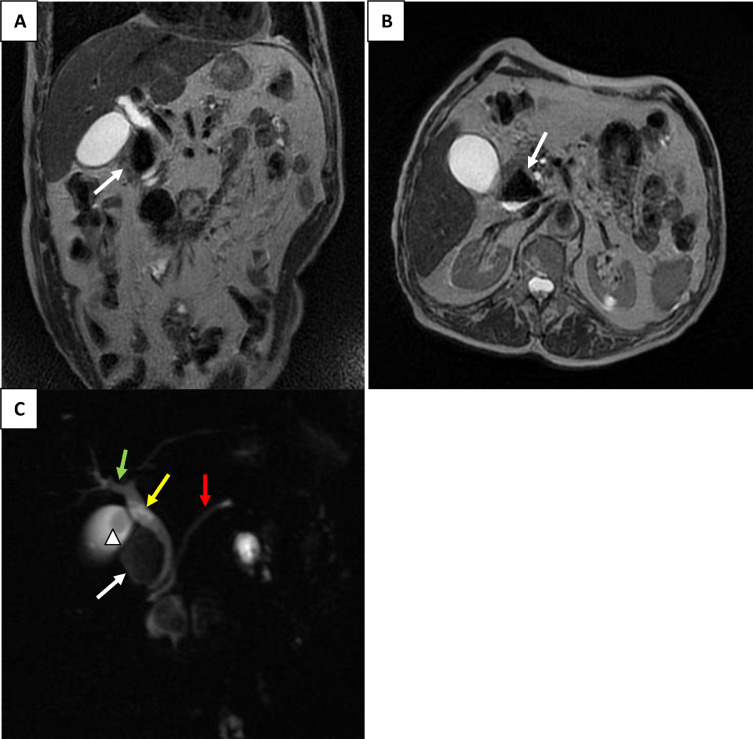
Magnetic resonance cholangiopancreatography also revealed a juxta-ampullary diverticulum (Figs. 2A and B); the diverticulum appeared to cause common bile duct compression with resultant upstream dilatation of the extra and intrahepatic bile ducts (Fig. 2C).
Fig. 2.
Magnetic resonance cholangiopancreatography: axial and coronal T2 sections showed a periampullary duodenal diverticulum (A, B). Biliary sequence (C) shows a periampullary duodenal diverticulum (white arrow) causes a dilatation of the common bile duct (yellow arrow), the Wirsung (red arrow), and the proximal part of intrahepatic bile duct dilatation (green arrow). Note a gallbladder stone (arrowhead).
Case 2
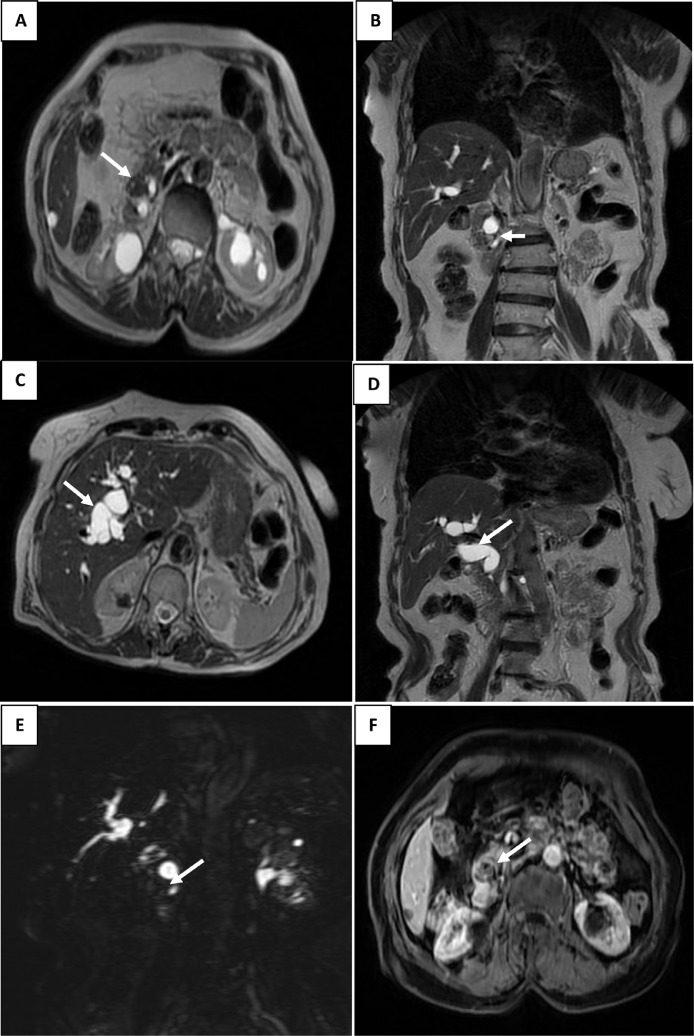
An 85-year-old woman was admitted to the emergency department for acute abdominal pain. On physical examination, she was icteric. An abdominal ultrasound showed dilatation of the intrahepatic and common bile ducts. A Magnetic resonance cholangiopancreatography revealed a periampullary diverticulum (Figs. 3A, B, E). This diverticulum contains fluid and air, nonenhanced after gadolinium injection (Fig. 3F), measuring 15 × 16 × 16 mm (AP × T × CC). It's Compressing the intrapancreatic part of the common bile duct with dilatation upstream of the common bile duct (16 mm) (Fig. 3D), the Wirsung duct (6. 4mm), and the intrahepatic bile ducts (Fig. 3C).
Fig. 3.
Magnetic resonance cholangiopancreatography in axial T2 weighted images (A, C), coronal T2 weighted images (B, D), 3D bili sequence (E), and axial T1 after injection of Gadolinium (F): showing a peri-ampullary diverticulum (A, B, E) with dilatation upstream of the common biliary tract (D) and intrahepatic biliary tracts (C) not enhanced after Gadolinium injection (F).
Discussion
Duodenal diverticula are mucosal pouches without muscular [2]; 75% of these diverticula are located in the second portion of the duodenum adjacent to the ampulla of Vater [2,4]. They are mainly solitary diverticula [2]. There are 2 types of duodenal diverticula, extramural and intramural diverticula [2]. Extramural diverticula are the most frequent; they are acquired from a defect in the duodenal wall secondary to a transparietal vessel trajectory [2]. The second type, intramural diverticula, is sporadic, congenital, and secondary to an incomplete canalization of the duodenal lumen [2].
Most duodenal diverticula (95%) are asymptomatic [5]. They are discovered incidentally in 22% of cases [1,6]. Around 1%-5% of patients may be complicated by pancreaticobiliary and non-pancreaticobiliary complications [6]. Non-pancreaticobiliary complications are rare and may present as diverticulitis, hemorrhage, perforation, or fistula formation [3]. Pancreaticobiliary complications can include recurrent gallbladder or bile duct stones, cholangitis, acute pancreatitis, or obstructive jaundice causing Lemmel syndrome [3].
Lemmel's syndrome is defined by extrinsic compression of the distal common bile duct by a periampullary diverticulum in the absence of choledocholithiasis or pancreaticobiliary tumor [5]. There are few case reports on this condition, first named in 1934 by Dr. Gerhard Lemmel [5]. Lemmel's syndrome's clinical symptoms are nonspecific, mainly manifested by right hypochondrial pain, recurrent attacks of acute abdominal pain, and jaundice [1,7].
Imaging plays an essential role in diagnosing Lemmel syndrome [4]. Ultrasound may be helpful in the evaluation of upstream bile duct dilatation [1]. Barium examination may show contrast-filled pockets in the descending duodenum's medial wall [4,8].
Cross-sectional imaging is the gold standard imaging modality for characterizing periampullary duodenal diverticula, which appear as thin-walled cavitating lesions that sit at the level of the 2nd portion of the duodenum, compressing the intrapancreatic part of the common bile duct [3,8].
CT scan is the reference imaging modality for a rapid, noninvasive, and specific evaluation of the periampullary diverticulum associated with Lemmel syndrome [1,9]; Concomitant oral contrast could help confirm size-related symptoms. It can also reveal underlying extrinsic compression on the common bile duct [1]; injected CT is of interest, especially for differential diagnosis [1]; diverticulum walls demonstrate weak homogeneous enhancement, greatest in the venous phase [1].
Magnetic resonance cholangiopancreatography may be necessary to confirm the diagnosis or to exclude other causes of acute abdominal pain and obstructive jaundice [9].
It has a diagnostic and therapeutic interest by allowing a sphincterotomy with the placement of a biliary stent, especially in high-risk patients [10].
The differential diagnosis of Lemmel's syndrome is mainly in front of the following pathologies:
-
•
Todani type 2 choledochal cyst may mimic Lemmel syndrome [11]. In our 2 cases, the magnetic resonance cholangiopancreatography was consistent with a periampullary duodenal diverticulum.
-
•
Pancreatic pseudocyst and infected necrotic collection related to pancreatitis [11] were unlikely in this case, as the absence of pancreatic abnormality and history of pancreatitis. In addition, serum pancreatic enzyme level was not elevated.
-
•
Pancreaticobiliary tumors [11] were thought to be unlikely, as the presenting symptoms were acute compared with a neoplastic cause.
-
•
Metastatic lymph node [11]: In our cases, the absence of neoplastic history made this an unlikely diagnosis.
Para duodenal pancreatitis, also known as groove pancreatitis, is a type of chronic pancreatitis occurring in a particular anatomical area between the duodenum, the head of the pancreas, and the common bile duct. It is characterized by cystic thickening of the duodenal wall and fibrous pancreatic duodenal furrow in the form of a curvilinear crescent [11,12].
The therapeutic management of patients with Lemmel syndrome varies according to symptomatology and pathophysiological mechanism [7].
In asymptomatic patients, conservative treatment with endoscopic retrograde cholangiography with sphincterotomy and stent placement is recommended [2,7].
If Lemmel's syndrome is due to chronic papillary fibrosis or sphincter of Oddi dysfunction can be successfully treated by endoscopic sphincterotomy to release biliary obstruction [11].
In patients with symptoms consistent with biliary obstruction or cholangitis, endoscopic extraction, extracorporeal shock wave lithotripsy, or surgical intervention such as diverticulectomy may be indicated [7]. Surgical treatment may also be indicated in case of complication, recurrence, or failure of conservative measures [9].
Conclusion
Lemmel's syndrome is an unrecognized cause of biliary tract obstruction. Due to the nonspecificity of clinical symptoms, careful analysis of cross-sectional imaging data is essential to diagnose this pathology; CT scan is the crucial modality for a rapid, noninvasive, and specific diagnosis of Lemmel's syndrome. Magnetic resonance cholangiopancreatography may be necessary to confirm the diagnosis and eliminate differential diagnoses.
Patient consent
Informed consent was obtained for publication.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Frauenfelder G, Maraziti A, Ciccone V, Maraziti G, Caleo O, Giurazza F, Zobel BB, Carbone M. Computed tomography imaging in lemmel syndrome: a report of two cases. J Clin Imaging Sci. 2019;9:23. doi: 10.25259/JCIS-17-2019. PMID: 31448174; PMCID: PMC6702893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khan BA, Khan SH, Sharma A. Lemmel's Syndrome: a rare cause of obstructive jaundice secondary to periampullary diverticulum. Eur J Case Rep Intern Med. 2017;4(6) doi: 10.12890/2017_000632. PMID: 30755952; PMCID: PMC6346791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Desai K, Wermers JD, Beteselassie N. Lemmel syndrome secondary to duodenal diverticulitis: a case report. Cureus. 2017;9(3):e1066. doi: 10.7759/cureus.1066. PMID: 28409067; PMCID: PMC5376190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yanagaki M, Shiba H, Hagiwara S, Hoshino M, Sakuda H, Furukawa Y, Yanaga K. A successfully treated case of Lemmel syndrome with pancreaticobiliary maljunction: a case report. Int J Surg Case Rep. 2020;72:560–563. doi: 10.1016/j.ijscr.2020.06.080. Epub 2020 Jun 24. PMID: 32698288; PMCID: PMC7327874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gao AR, Matta A, Seth R, Bande D. Lemmel's syndrome secondary to common bile duct compression by an inflamed duodenal diverticulum. Cureus. 2021;13(8):e16959. doi: 10.7759/cureus.16959. PMID: 34527452; PMCID: PMC8418959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Díaz Alcázar MDM, Martín-Lagos Maldonado A, García Robles A. Lemmel syndrome: an uncommon complication of periampular duodenal diverticulum. Rev Esp Enferm Dig. 2021;113(6):477–478. doi: 10.17235/reed.2020.7537/2020. PMID: 33267603. [DOI] [PubMed] [Google Scholar]
- 7.Bernshteyn M, Rao S, Sharma A, Masood U, Manocha D. Lemmel's syndrome: usual presentation of an unusual diagnosis. Cureus. 2020;12(4):e7698. doi: 10.7759/cureus.7698. PMID: 32431977; PMCID: PMC7233497. [DOI] [PMC free article] [PubMed]
- 8.Tobin R, Barry N, Foley NM, Cooke F. A giant duodenal diverticulum causing Lemmel syndrome. J Surg Case Rep. 2018;2018(10):rjy263. doi: 10.1093/jscr/rjy263. PMID: 30349662; PMCID: PMC6189375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azzam AZ, Alsinan TA, Alrebeh GA, Alhaider T, Alnaqaeb LJ, Amin TM. Lemmel syndrome as a rare cause of prolonged right hypochondrial pain: a case report. Cureus. 2021;13(12):e20093. doi: 10.7759/cureus.20093. PMID: 35003949; PMCID: PMC8723720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goroztieta-Rosales LM, Gómez-Farías J, López-García KD, Davila-Rodriguez DO. Lemmel syndrome: an extraordinary cause of obstructive jaundice-a case report. J Surg Case Rep. 2022;2022(1):rjab593. doi: 10.1093/jscr/rjab593. PMID: 35047177; PMCID: PMC8763606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Venkatanarasimha N, Yong YR, Gogna A, Tan BS. Case 265: Lemmel syndrome or biliary obstruction due to a periampullary duodenal diverticulum. Radiology. May 2019;291(2):542–545. doi: 10.1148/radiol.2019162375. PMID: 30998446. [DOI] [PubMed] [Google Scholar]
- 12.Wang YL, Tong CH, Yu JH, Chen ZL, Fu H, Yang JH, Zhu X, Lu BC. Complete duodenal obstruction induced by groove pancreatitis: a case report. World J Clin Cases. 2019;7(23):4106–4110. doi: 10.12998/wjcc.v7.i23.4106. PMID: 31832415; PMCID: PMC6906566. [DOI] [PMC free article] [PubMed] [Google Scholar]