Abstract
Objective
To examine by age, the veterans' report on whether components of age‐friendly health systems were discussed during primary care visits.
Data Sources and Study Setting
Veterans Affairs (VA) Survey of Healthcare Experience of Patients from October 2015 to September 2019.
Study Design
Cross‐sectional survey of VA users by age group (18–44 years, 45–64 years, 65+ years; N = 1,042,318). We used weighted logistic regression models to evaluate disparities in whether veterans discussed with anyone in their provider's office: health goals, depression symptoms, stress, personal problems, and medications. Models were adjusted for socio‐demographic characteristics (sex, socioeconomic status, education, rurality) and comorbidity.
Data Collection/Extraction Method
Surveys were administered by mail and online. Additional veteran characteristics were extracted from VA administrative data.
Principal Findings
In unadjusted analyses, VA users age 18–44 had a higher (−8.2%; CI: −9.0, −7.3) and users aged 45 to 64 had lower (4.0%; CI: 3.7, 4.3) predicted, probably discussing health goals compared to age 65+. Fewer VA users age 65+ reported discussing depression symptoms, personal problems, and stress than other age groups, whereas more VA users age 65+ discussed medications. Results were unchanged after adjusting for socio‐demographics and comorbidity.
Conclusions
Delivery of goal‐concordant care relies on understanding the needs of individual patients. Lower rates of discussing what matters and mood represent potential missed opportunities to deliver age‐friendly care for older veterans.
Keywords: geriatrics, goal concordance, health services for older adults, health care, patient experience, psychosocial functioning, veterans
What is known about this topic
Prior research has shown that patient‐reported experiences are less favorable for individuals of younger age, female sex, lower education, lower socioeconomic status, and poorer self‐rated health.
There is no consensus in the literature about why patient experiences differ by age.
Limited information exists regarding patient experiences of being asked about health goals, psychosocial concerns, and medications, and how these responses differ by age.
What this study adds
Veterans ages 45–64 had a predicted probability of 71% for being asked about health goals, compared to 67% for Veterans age 65+ and 59% for age 18–44.
Veterans ages 65+ had a predicted probability of 45% for being asked about personal problems, compared to 57% of Veterans ages 45–64 and 59% 18–44.
Age disparities in discussing health goals and psychosocial needs during medical visits persisted after adjusting models for other characteristics known to be associated with disparities in patient experience, including sex, education, socioeconomic status, and health status.
1. INTRODUCTION
The U.S. veteran population is aging and will increasingly require age‐appropriate care planning and delivery. Approximately 50% of veterans nationally and 47.1% of Veterans Health Administration (VA) users are 65 years of age or older, compared to about 21% of the general adult population. 1 , 2 Care of older adults is of primary concern at the VA, especially considering the disproportionately adverse health outcomes experienced by older veterans. 2 , 3 , 4 To this end, the VA has adopted the Age‐Friendly Health Systems initiative, which aims to align care delivery with the specific health goals of older adults. 5 The age‐friendly initiative focuses on addressing the “4Ms” when caring for older adults: what matters, mental health, mobility, and medication. Such a framework can guide clinicians in having and recording conversations with veteran patients about health goals, personal problems and stressors, and medications. 6
The delivery and measurement of appropriate, goal‐concordant care relies on providers recognizing the individual needs of their patients. The VA uses a Patient‐Centered Medical Home (PCMH) approach to manage primary care. 7 This model is intended to improve access and care management by tailoring team‐based care to individual veterans. As the largest integrated health care system in the U.S., VA users have fewer disparities in accessing care than non‐veterans. 4
Nonetheless, existing literature documents health disparities in care by age, sex, race, and other characteristics that persist across different health and payment systems. For example, outside of the VA, Medicare beneficiaries with depressive symptoms have reported worse experiences with care in both fee‐for‐service and managed care compared to beneficiaries without depression. 8 Management of chronic illness among older adults, women, socioeconomically disadvantaged people, those with less than a high school education, and racial/ethnic minoritized people reveals persistent inequalities in access to care, preventive services, and disease treatment. 9 , 10 , 11 , 12 , 13 Older adults are more likely than those under age 65 to report that their health care provider listens to them 14 ; however, few studies have evaluated whether patient‐reported experiences related to the elements of age‐friendly health systems vary by age.
In addition to these documented inequities in disease prevention, management, and access, poor health goal communication has been reported among young adults and racial/ethnic minoritized individuals in and out of VA. 9 , 15 , 16 Conceptually, a health disparity in goal‐concordant care is a difference in patient‐provider communication in which disadvantaged social groups systematically experience worse communication quality and greater health risk than social groups with relatively more advantage. 17 While multiple studies examine advance care planning at the end of life, 18 the literature provides scant insight into the provision of goal‐concordant care among community‐dwelling older adults, especially older veterans.
The purpose of this study is to examine differences by age in VA users' self‐reports of whether health goals and psychosocial needs were discussed with their providers or PCMH teams. Given the cumulative inequality of health and social arrangements across the life course, this study examines a diverse population of veterans of all ages. 19 , 20 , 21
2. METHODS
This study builds from the National Veteran Health Equity Report 2021 (NVHER). 22 We compared VA user age groups (18–44 years, 45–64 years, 65+ years) on patient experience measures.
2.1. Participants and design
Data were obtained from the VA Survey of Healthcare Experience of Patients (SHEP)‐PCMH national survey responses from October 2015 to September 2019. SHEP‐PCMH is based on the Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys and evaluates patient experiences of care from the previous 6 months. 23 The SHEP‐PCMH is administered annually to a national stratified random sample of veterans who have visited the VA in the previous month. 24 , 25 Sample stratification is by VA site.
2.2. Data collection
Surveys were conducted by mail and online with an average response rate of 35%. 24 Additional demographic data were extracted from the VA Corporate Data Warehouse (CDW) and merged with the SHEP‐PCMH data.
2.3. Outcome measures
Key outcomes included whether the veteran reported that anyone in the provider's office discussed the following with them during a primary care visit: health goals, depression, stress, personal problems, and medications. We used items from the SHEP‐PCMH as proxies for three of the 4Ms. The following are the questions as they appear in SHEP‐PCMH:
Health goals: In the last 6 months, did anyone in this provider's office talk with you about specific goals for your health? (what Matters)
Depression symptoms: In the last 6 months, did anyone in this provider's office ask you if there was a period of time when you felt sad, empty, or depressed? (Mentation)
Stress: In the last 6 months, did you and anyone in this provider's office talk about things in your life that worry you or cause you stress? (what Matters)
Personal problems: In the last 6 months, did you or anyone in this provider's office talk about a personal problem, family problem, alcohol use, drug use, or a mental or emotional illness? (what Matters)
Medications: In the last 6 months, how often did you and someone from this provider's office talk about all the prescription medicines you were taking? (Medications)
The first four items have dichotomous yes/no response options. Responses to the medication question use a 4‐point Likert‐type scale with response options of “always,” “usually,” “sometimes,” or “never.” The medication item was dichotomized as “always” versus all other categories.
2.4. Independent variables
We included three age categories (18–44, 45–64, and 65+). We selected these cut points to facilitate comparison with prior reports on veteran health disparities. 4 , 22 , 26 , 27 The cut point between younger and middle‐aged adults is frequently used to distinguish between military service eras and reproductive health differences. 27 Age 65 is used as the cut point for older adults to reflect policy standards, including Medicare eligibility. Socio‐demographic characteristics associated with disparities in patient experience may vary by patient age and therefore were assessed. 17 Education level and self‐rated physical and mental health were obtained from SHEP‐PCMH responses. Age, sex, race, ethnicity, and rurality were obtained from the VA CDW administrative data. Socioeconomic status (SES) was derived from income information from the VA enrollment priority group using previously established methods 28 and included three categories: high, low, and indeterminate. The Gagne comorbidity index (GCI) score was also calculated using data from the VA CDW. 29 The GCI was designed to predict short‐ and long‐term mortality by combining elements of two other comorbidity indices (Charlson and Elixhauser). Race and ethnicity were combined to create race/ethnicity categories in which veterans who self‐identified as Hispanic were categorized as such. All other groups were categorized by race.
2.5. Data analysis
We tested weighted unadjusted logistic regression models on each outcome of interest with age category as the independent variable. We then tested three weighted adjusted models, each of which added successively more covariates, including sex, SES, education, rurality, self‐rated mental and physical health, and GCI. We selected these variables as they have been shown to contribute to differences in patient experience on CAHPS. 10 , 30 , 31 , 32 After fitting unadjusted logistic regression models for age differences on each outcome (model 1), models were adjusted by adding covariates successively, including sex (model 2), SES, education, and rurality (model 3), and self‐rated physical and mental health and GCI (model 4). In all models, we expressed the effects of age as differences in the experience of outcome probabilities between the age 65+ group and each of the younger age groups. We also conducted sensitivity analyses, adding race/ethnicity to evaluate whether doing so changed the relationship between the age category and each outcome. All model estimates incorporated sampling design characteristics, including stratification by site. Analyses were conducted using Stata version 17. This project was evaluated by the Institutional Review Board of VA Greater Los Angeles and received a determination of non‐research because the primary purpose was to inform VA operations and program improvement and the design was limited to analysis of deidentified data that are collected as part of normal business operations.
3. RESULTS
3.1. Participants
Descriptive data about the sample are summarized in Table 1 (N = 1,042,318). We report weighted percentages for all characteristics; raw sample sizes are reported in Table S1. The weighted sample distribution by age group is 16.4% aged 18–44, 32.5% aged 45–64, and 51.0% aged 65+. Compared to those aged 65+, the younger cohorts had larger proportions of female and racial/ethnic minoritized veterans. The 65+ age group had the largest proportion of rural‐residing veterans (36.8%).
TABLE 1.
Sample characteristics (weighted percentage)
| Variable | Age 18–44 n = 39,033 | Age 45–64 n = 238,322 | Age 65+ n = 764,962 |
|---|---|---|---|
| Male | 74.3% | 86.2% | 97.8% |
| Race/ethnicity a | |||
| AI/AN | 0.7% | 0.7% | 0.5% |
| Asian | 3.5% | 1.4% | 0.7% |
| Black | 17.7% | 26.1% | 10.8% |
| Hispanic/Latino | 14.1% | 7.7% | 5.1% |
| Multi‐race | 1.6% | 0.8% | 0.6% |
| NH/OPI | 1.1% | 0.9% | 0.6% |
| Unknown | 3.4% | 3.8% | 5.1% |
| White | 57.9% | 58.6% | 76.7% |
| Rural | 24.3% | 29.7% | 35.8% |
| Socio‐economic status | |||
| High | 5.9% | 12.8% | 21.1% |
| Low | 8.6% | 22.2% | 20.2% |
| Indeterminate | 85.5% | 65.0% | 58.8% |
| Education (greater than high school) | 87.9% | 71.7% | 58.5% |
| Self‐reported physical health | |||
| 1 – Excellent | 7.8% | 6.0% | 6.3% |
| 2 – Very Good | 23.2% | 20.4% | 22.4% |
| 3 – Good | 37.4% | 37.7% | 37.9% |
| 4 – Fair | 25.1% | 28.1% | 26.7% |
| 5 – Poor | 6.6% | 7.9% | 6.8% |
| Self‐reported mental health | |||
| 1 – Excellent | 13.3% | 17.3% | 21.9% |
| 2 – Very Good | 18.7% | 23.1% | 28.2% |
| 3 – Good | 27.4% | 27.5% | 28.5% |
| 4 – Fair | 28.3% | 23.8% | 17.4% |
| 5 – Poor | 12.4% | 8.4% | 4.0% |
| Gagne Comorbidity Index, b weighted mean (SE) | 0.22 (0.07) | 0.39 (0.004) | 0.84 (0.003) |
AI/AN denotes American Indian/Alaska Native. NH/OPI denotes Native Hawaiian or Other Pacific Islander. Race/Ethnicity includes mutually exclusive categories of Hispanic/Latino and non‐Hispanic race groups.
Gagne Comorbidity Index represents the increase in odds of dying in the next year due to 37 comorbid conditions, based on age and sex. Thus, 0.22 represents a comorbidity burden that increases the risk of death by 22%.
3.2. Outcomes
Results of weighted logistic regression models are shown in Table 2, and model fit statistics are reported in Table S2. In model 1 (unadjusted), the largest age‐group differences were in discussing personal problems; VA users age 65+ had a lower predicted probability of discussing personal problems (45.0%) than VA users aged 18–44 (58.9%) or 45–64 (57.4%). The addition of sequential adjustments in models 2–4 did not alter the finding of lower patient experience ratings for those age 65+. We observed similar patterns for the outcomes of discussing depression symptoms and stress (Figure 1). The 65+ group had a higher predicted probability than the 18–44 group but a lower predicted probability than the 45–64 group for reporting and discussing health goals. VA users age 65+ had the highest predicted probability of discussing medications.
TABLE 2.
Results of tests of unadjusted and adjusted differences between older‐age and younger‐age Veterans in proportions of respondents who reported discussions on selected topics
| Model 1 (unadjusted) | Model 2 | Model 3 | Model 4 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Discussion outcome | Age category | % | Difference (95% CI) | % | Difference (95% CI) | % | Difference (95% CI) | % | Difference (95% CI) |
| Health goals | 18–44 | 58.9 | −8.2 (−9.0,‐7.3) | 59.6 | −7.1 (−7.9,‐6.2) | 59.5 | −7.3 (−8.1,‐6.4) | 60.3 | −6.0 (−6.9,‐5.1) |
| 45–64 | 71.0 | 4.0 (3.7, 4.3) | 71.2 | 4.5 (4.2, 4.9) | 71.1 | 4.3 (4.0, 4.7) | 71.5 | 5.2 (4.8, 5.5) | |
| 65+ (ref) | 67.0 | 66.7 | 66.8 | 66.3 | |||||
| Depression | 18–44 | 82.3 | 8.6 (8.0, 9.3) | 82.2 | 8.4 (7.7, 9.0) | 81.3 | 7.0 (6.3, 7.7) | 81.5 | 7.5 (6.9, 8.2) |
| 45–64 | 79.2 | 5.5 (5.2, 5.8) | 79.1 | 5.3 (5.0, 5.6) | 79.2 | 4.9 (4.6, 5.2) | 79.3 | 5.3 (5.0, 5.6) | |
| 65+ (ref) | 73.7 | 73.8 | 74.3 | 74.0 | |||||
| Stress | 18–44 | 64.1 | 9.1 (8.3, 9.9) | 63.9 | 8.8 (8.0, 9.7) | 62.5 | 6.8 (5.9, 7.6) | 62.4 | 6.7 (5.8, 7.6) |
| 45–64 | 63.0 | 8.0 (7.7, 8.4) | 63.0 | 7.9 (7.5, 8.3) | 62.9 | 7.2 (6.8, 7.6) | 63.1 | 7.4 (7.0, 7.7) | |
| 65+ (ref) | 55.0 | 55.1 | 55.7 | 55.7 | |||||
| Personal problems | 18–44 | 58.9 | 13.9 (13.0,14.7) | 59.4 | 14.6 (13.7,15.5) | 58.4 | 13.1 (12.2,14.0) | 57.6 | 12.0 (11.1,12.9) |
| 45–64 | 57.4 | 12.4 (12.0,12.8) | 57.6 | 12.8 (12.4,13.1) | 57.4 | 12.1 (11.7,12.5) | 57.3 | 11.7 (11.3,12.1) | |
| 65+ (ref) | 45.0 | 44.8 | 45.3 | 45.6 | |||||
| Medications | 18–44 | 43.2 | −8.7 (−9.6,‐7.8) | 43.1 | −8.9 (−9.9,‐8.0) | 43.0 | −9.1 (−10.0,‐8.1) | 44.2 | −7.2 (−8.1,‐6.2) |
| 45–64 | 50.9 | −1.0 (−1.4,‐0.7) | 50.8 | −1.1 (−1.5,‐0.8) | 51.1 | −1.0 (−1.4,‐0.6) | 51.6 | 0.2 (−0.2, 0.6) | |
| 65+ (ref) | 51.9 | 52.0 | 52.0 | 51.4 | |||||
Note: Model 1: unadjusted. Model 2: adjusted for sex. Model 3: adjusted for sex, socioeconomic status (SES), education and urbanicity/rurality. Model 4: adjusted for sex, SES, education, urbanicity/rurality, self‐rated health, self‐rated mental health and Gagne comorbidity index. Differences with positive values indicate worse outcomes for the 65+ age group. Differences with negative values indicate better outcomes for the 65+ age group.
FIGURE 1.
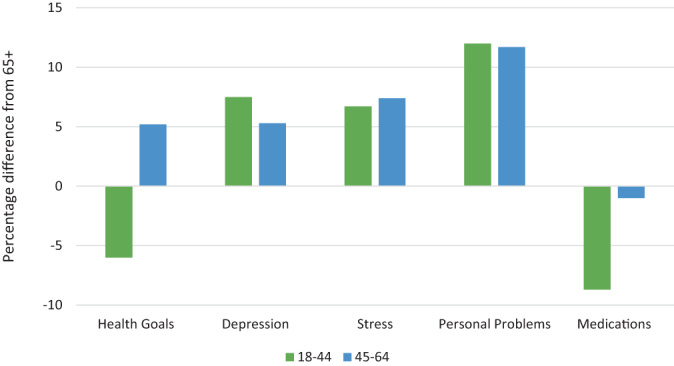
Unadjusted differences in discussion of outcomes compared to the 65+ age group. Positive values indicate that an age group had a higher predicted probability of achieving the outcome compared to the 65+ group. Negative values indicate that an age group had a lower predicted probability of achieving the outcome compared to the 65+ group. [Color figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
In a national sample of veterans, we found evidence of moderate age disparities in predicted probabilities of discussing depression, stress, and personal problems between the oldest‐age and younger‐age groups. Evidence of a smaller disparity was found between the older‐age and middle‐age groups on discussion of health goals. Discussion of medications was greatest in the older‐age group. Overall, the presence and magnitudes of age disparities were comparable in the unadjusted, partially adjusted, and fully adjusted models of all outcomes. Lower reported probabilities of discussing psychosocial issues and health goals represent potential missed opportunities to deliver person‐centered, age‐friendly care aimed at addressing pertinent problems with older veterans.
Like the SHEP‐PCMH, CAHPS surveys patients' experiences with health care providers and staff in primary care and specialty care settings. 33 Though CAHPS is widely used, there is a dearth of literature on the influence of personal problems, health goals, stress, and medications on patient experience as well as age differences within these categories. These areas warrant further investigation across health systems. In addition, given the performance gaps highlighted in these analyses, changes in patient experience after the introduction of the Age‐Friendly Health Systems approach should be evaluated.
Although there was a lower predicted probability of discussing depression among VA users aged 65+ compared to the younger cohorts, overall reported screening rates were high, which is consistent with prior research. 12 Providers should be encouraged to specifically discuss health goals, personal problems, alcohol and drug use, and mental or emotional health during routine visits for VA users aged 65+. Longitudinal continuity of care is associated with higher quality patient‐provider communication 34 ; thus, future research should consider continuity of primary care in the context of these specific items being addressed.
Although age differences favored those aged 65+, the low rate of medications being discussed presents an opportunity to engage interprofessional team members in closing care gaps. For instance, medications may influence mentation and interact with alcohol or other substances, resulting in negative impacts on health. In particular, prior research has demonstrated that more than half of Medicare‐eligible veterans who use both VA and non‐VA health services do not regularly discuss outside prescription medications with their VA physician. 35 In this context, it is important to understand health goals and patient priorities to monitor such risks.
4.1. Limitations
As this study represents a secondary data analysis, we were limited to existing variables and were not able to evaluate all factors that may contribute to disparities in patient experience. It is possible that younger veterans are asked about depression, stress, and personal problems more often because a larger proportion of them have a mental health‐related service‐connected disability. Prior research on CAHPS in non‐VA settings has shown that people with depressive symptoms reported worse experiences in all aspects of care 36 ; we were not able to control for the presence of depressive symptoms specifically. Although the VA SHEP‐PCMH asks about discussion of mood and stress, which are elements of mentation, it does not ask about discussion of cognition.
We selected age categories to facilitate comparisons with prior publications; however, we acknowledge that there could be variation within each age category. We also do not have an item specifically about mobility, therefore not all of the 4Ms were represented. Prior research has shown that users of both VA and non‐VA care report more health care hassles than VA‐only users 37 ; although questions were framed around VA experiences, it is possible that respondents could have attributed experiences from non‐VA sites. This issue is relevant because, compared to younger cohorts, veterans age 65+ may use more non‐VA care because they have access to Medicare.
A strength of this study is the use of data from the largest integrated health care system in the US and a national probability sample of users of this system. The VA's PCMH model is a prominent example of a team‐based approach to patient‐centered care.
5. CONCLUSIONS
We examined by age the veterans' report on whether health goals and psychosocial needs were discussed during primary care visits. Older VA users (65+) had lower probabilities of discussing personal problems, depression, and stress with their health care team compared to younger veterans. Not discussing psychosocial and quality of life issues among those 65+ represent potential missed opportunities to deliver person‐centered, age‐friendly care for older veterans.
Supporting information
Table S1. Sample characteristics (unweighted n sizes).
Table S2. Model fit statistics.
ACKNOWLEDGMENTS
This work was conducted through the Department of Veterans Affairs (VA) Health Equity (OHE)–Quality Enhancement Research Initiative (QUERI) National Partnered Evaluation Center, funded by the VA OHE and QUERI (grant #PEC‐15‐239). This work utilized code derived from VA Health Services Research and Development grant #IIR‐17‐289. SHEP‐PCMH data were obtained through a data use agreement with the VHA Office of Quality and Patient Safety– Analytics and Performance Integration (QPS‐API) (10A8). Kimberly A. Lynch, MD, MS, was supported by the VA Office of Academic Affiliations through the National Clinician Scholars Program. Stephen Frochen, PhD, was supported by the VA Office of Academic Affiliations Health Services Research and Development Fellowship. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or of the U.S. government.
Cogan AM, Saliba D, Steers WN, et al. Provider discussion of health goals and psychosocial needs: Comparing older to younger veteran experience. Health Serv Res. 2023;58(Suppl. 1):9‐15. doi: 10.1111/1475-6773.14054
Funding information Department of Veterans Affairs (VA) Office of Health Equity (OHE)‐Quality Enhancement Research Initiative (QUERI) National Partnered Evaluation Initiative, Grant/Award Number: PEC‐15‐239; VA Office of Academic Affiliations Health Services Research and Development Fellowship, Grant/Award Number: IIR‐17‐289; VA Office of Academic Affiliations through the National Clinician Scholars Program; Health Services Research and Development
REFERENCES
- 1. U.S. Census Bureau . Sex by age by Veteran status for the Civilian population 18 years and over. 2022. Accessed March 9, 2022. https://data.census.gov/cedsci/table?q=veteran%20age&tid=ACSDT1Y2019.B21001
- 2. U.S. Department of Veterans Affairs . Department of Veterans Affairs FY 2018–2024 strategic plan. U.S. Department of Veterans Affairs. 2019. https://www.va.gov/oei/docs/va2018-2024strategicplan.pdf
- 3. Popham L, Tavares J, Cohen M. A Profile of Older U.S. Veterans. National Council on Aging. 2019. Accessed February 18, 2022. https://www.ncoa.org/article/a-profile-of-older-us-veterans
- 4. Agency for, Healthcare Research and Quality. National Healthcare Quality and Disparities Report Chartbook on Healthcare for Veterans. 2020. https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/chartbooks/veterans/2020qdr-chartbook-veterans.pdf [PubMed]
- 5. Fulmer T. Discovering the 4Ms: A framework for creating age‐friendly health systems. The John a Hartford Foundation Published August 7, 2018. Accessed March 8, 2022. https://www.johnahartford.org/blog/view/discovering‐the‐4ms‐a‐framework‐for‐creating‐age‐friendly‐health‐systems/
- 6. U.S. Department of Veterans Affairs . VA Age‐Friendly Health Systems Initiative. Published September 10, 2021. Accessed March 9, 2022. https://www.va.gov/geriatrics/pages/VA_Age_Friendly_Health_Systems_Initiative.asp
- 7. Rosland AM, Nelson K, Sun H, et al. The patient‐centered medical home in the veterans health administration. Am J Manag Care. 2013;19(7):e263‐e272. [PubMed] [Google Scholar]
- 8. Martino SC, Elliott MN, Haviland AM, Saliba D, Burkhart Q, Kanouse DE. Comparing the health care experiences of Medicare beneficiaries with and without depressive symptoms in Medicare managed care versus fee‐for‐service. Health Serv Res. 2016;51(3):1002‐1020. doi: 10.1111/1475-6773.12359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Saha S, Freeman M, Toure J, Tippens KM, Weeks C, Ibrahim S. Racial and ethnic disparities in the VA health care system: a systematic review. J Gen Intern Med. 2008;23(5):654‐671. doi: 10.1007/s11606-008-0521-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. MacCarthy S, Burkhart Q, Haviland AM, et al. Exploring disparities in influenza immunization for older women. J Am Geriatr Soc. 2019;67(6):1268‐1272. doi: 10.1111/jgs.15887 [DOI] [PubMed] [Google Scholar]
- 11. May FP, Yano EM, Provenzale D, Steers WN, Washington DL. Race, poverty, and mental health drive colorectal cancer screening disparities in the veterans health administration. Med Care. 2019;57(10):773‐780. doi: 10.1097/MLR.0000000000001186 [DOI] [PubMed] [Google Scholar]
- 12. Leung LB, Chu K, Rose D, et al. Electronic population‐based depression detection and management through universal screening in the veterans health administration. JAMA Netw Open. 2022;5(3):e221875. doi: 10.1001/jamanetworkopen.2022.1875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Washington DL, Steers WN, Huynh AK, et al. Racial and ethnic disparities persist at veterans health administration patient‐centered medical homes. Health Aff Proj Hope. 2017;36(6):1086‐1094. doi: 10.1377/hlthaff.2017.0029 [DOI] [PubMed] [Google Scholar]
- 14. DeVoe JE, Wallace LS, Fryer GEJ. Patient age influences perceptions about health care communication. Fam Med. 2009;41(2):126‐133. [PMC free article] [PubMed] [Google Scholar]
- 15. Shen MJ, Peterson EB, Costas‐Muñiz R, et al. The effects of race and racial concordance on patient‐physician communication: a systematic review of the literature. J Racial Ethn Health Disparities. 2018;5(1):117‐140. doi: 10.1007/s40615-017-0350-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chen Y, Lee YT, Pethtel OL, Gutowitz MS, Kirk RM. Age differences in coal concordance, time use, and well‐being. Educ Gerontol. 2012;38(11):742‐752. doi: 10.1080/03601277.2011.645424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167‐194. doi: 10.1146/annurev.publhealth.27.021405.102103 [DOI] [PubMed] [Google Scholar]
- 18. Morrison RS, Meier DE, Arnold RM. What's wrong with advance care planning? JAMA. 2021;326(16):1575‐1576. doi: 10.1001/jama.2021.16430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ferraro KF, Shippee TP. Aging and cumulative inequality: how does inequality get under the skin? Gerontologist. 2009;49(3):333‐343. doi: 10.1093/geront/gnp034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mehta NK, Zheng H, Myrskylä M. How do age and major risk factors for mortality interact over the life‐course? Implications for health disparities research and public health policy. SSM ‐ Popul Health. 2019;8:100438. doi: 10.1016/j.ssmph.2019.100438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Maclean A. The things they carry: combat, disability and unemployment among US men. Am Sociol Rev. 2010;75(4):563‐585. doi: 10.1177/0003122410374085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Washington D. Selected findings: National Veteran Health Equity Report 2021. Presented at: focus on health equity and action cyberseminar series, Veterans Health Administration; May 12, 2021. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=3985
- 23. Hays RD, Shaul JA, Williams VS, et al. Psychometric properties of the CAHPS 1.0 survey measures. Consumer assessment of health plans study. Med Care. 1999;37(3Suppl):MS22‐MS31. doi: 10.1097/00005650-199903001-00003 [DOI] [PubMed] [Google Scholar]
- 24. Stratford D. VA's survey of healthcare experience of patients. 2021. Accessed March 9, 2022. https://blogs.va.gov/VAntage/83755/vas-survey-healthcare-experience-patients/
- 25. Budzi D, Lurie S, Singh KP, Hooker RS. Veterans' perceptions of care by nurse practitioners, physician assistants, and physicians: a comparison from satisfaction surveys. J Am Acad Nurse Pract. 2010;22(6):330. doi: 10.1111/j.1745-7599.2010.00516.x [DOI] [PubMed] [Google Scholar]
- 26. VA Office of Health Equity . National Veteran Health Equity Report‐‐FY2013. US Department of Veterans Affairs. 2016. http://www.va.gov/healthequity/nvher.asp
- 27. Washington DL, Farmer MM, Mor SS, Canning M, Yano EM. Assessment of the healthcare needs and barriers to VA use experienced by women veterans: findings from the national survey of women veterans. Med Care. 2015;53(4 Suppl 1):S23‐S31. doi: 10.1097/MLR.0000000000000312 [DOI] [PubMed] [Google Scholar]
- 28. Upchurch DM, Wong MS, Yuan AH, et al. COVID‐19 infection in the veterans health administration: gender‐specific racial and ethnic differences. Womens Health Issues. 2022;32(1):41‐50. doi: 10.1016/j.whi.2021.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol. 2011;64(7):749‐759. doi: 10.1016/j.jclinepi.2010.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Meyers DJ, Rahman M, Mor V, Wilson IB, Trivedi AN. Association of Medicare Advantage star ratings with racial, ethnic, and socioeconomic disparities in quality of care. JAMA Health Forum. 2021;2(6):e210793. doi: 10.1001/jamahealthforum.2021.0793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Weech‐Maldonado R, Elliott MN, Adams JL, et al. Do racial/ethnic disparities in quality and patient experience within Medicare plans generalize across measures and racial/ethnic groups? Health Serv Res. 2015;50(6):1829‐1849. doi: 10.1111/1475-6773.12297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rodriguez HP, Crane PK. Examining multiple sources of differential item functioning on the clinician & group CAHPS® survey. Health Serv Res. 2011;46(6pt1):1778‐1802. doi: 10.1111/j.1475-6773.2011.01299.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Solomon LS, Hays RD, Zaslavsky AM, Ding L, Cleary PD. Psychometric properties of a group‐level consumer assessment of health plans study (CAHPS) instrument. Med Care. 2005;43(1):53‐60. [PubMed] [Google Scholar]
- 34. Katz DA, McCoy K, Sarrazin MV. Does improved continuity of primary care affect clinician‐patient communication in VA? J Gen Intern Med. 2014;29(Suppl 2):S682‐S688. doi: 10.1007/s11606-013-2633-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Stroupe KT, Smith BM, Hogan TP, et al. Medication acquisition across systems of care and patient‐provider communication among older veterans. Am J Health Syst Pharm. 2013;70(9):804‐813. doi: 10.2146/ajhp120222 [DOI] [PubMed] [Google Scholar]
- 36. Martino SC, Elliott MN, Kanouse DE, Farley DO, Burkhart Q, Hays RD. Depression and the health care experiences of Medicare beneficiaries. Health Serv Res. 2011;46(6pt1):1883‐1904. doi: 10.1111/j.1475-6773.2011.01293.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Noël PH, Barnard JM, Barry FM, et al. Patient experience of health care system hassles: dual‐system vs single‐system users. Health Serv Res. 2020;55(4):548‐555. doi: 10.1111/1475-6773.13291 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Sample characteristics (unweighted n sizes).
Table S2. Model fit statistics.


