Abstract
Objective
To describe a feasibility pilot study for older adults that addresses the digital divide, unmet health care needs, and the 4Ms of Age‐Friendly Health Systems via the emergency department (ED) follow‐up home visits supported by telehealth.
Data Sources and Study Setting
Data sources were a pre‐implementation site survey and pilot phase individual‐level patient data from six US Department of Veterans Affairs (VA) EDs.
Study Design
A pre‐implementation survey assessed existing geriatric ED processes. In the pilot called SCOUTS (Supporting Community Outpatient, Urgent care & Telehealth Services), sites identified high‐risk patients during an ED visit. After ED discharge, Intermediate Care Technicians (ICTs, former military medics), performed follow‐up telephone, or home visits. During the follow‐up visit, ICTs identified “what matters,” performed geriatric screens aligned with Age‐Friendly Health Systems, observed home safety risks, assisted with video telehealth check‐ins with ED providers, and provided care coordination. SCOUTS visit data were recorded in the patient's electronic medical record using a standardized template.
Data Collection/Extraction Methods
Sites were surveyed via electronic form. Administrative pilot data extracted from VA Corporate Data Warehouse, May–October 2021.
Principle Findings
Site surveys showed none of the EDs had a formalized way of identifying the 4 M “what matters.” During the pilot, ICT performed 56 telephone and 247 home visits. All home visits included a telehealth visit with an ED provider (n = 244) or geriatrician (n = 3). ICTs identified 44 modifiable home fall risks and 99 unmet care needs, recommended 80 pieces of medical equipment, placed 36 specialty care consults, and connected 180 patients to a Patient Aligned Care Team member for follow‐up.
Conclusions
A post‐ED follow‐up program in which former military medics perform geriatric screens and care coordination is feasible. Combining telehealth and home visits allows providers to address what matters and unmet care needs.
Keywords: caregivers, emergency medicine, geriatrics, house calls, military personnel, telemedicine, veterans
What is known on this topic
Integrating the 4Ms (what Matters, Mentation, Medication, Mobility) of Age‐Friendly Health Systems into emergency medicine is challenging due to staff and patient factors
Geriatric Emergency Departments provide a pathway for identifying high‐risk older adults who would benefit from comprehensive screening
Intermediate Care Technicians (former military Navy Corpsman, Air Force and Coast Guard Medical Technicians, or Army Combat Medics) can perform Geriatric Emergency Department Screens
What this study adds
A Veterans Affairs (VA) Emergency Department follow‐up program promoting 4Ms of Age‐Friendly Health Systems through assisted telehealth is feasible
Combining telehealth and home visits allow VA Emergency Medicine Physicians to address what matters and identify unmet care needs
Intermediate Care Technicians can perform geriatric and home safety screens in Veteran's homes with the support of VA Emergency Medicine Physicians
1. INTRODUCTION
More than 1 million Veterans aged 65 years and older visit the US Department of Veterans Affairs (VA) Emergency Departments (ED) each year. 1 Within VA EDs, adults 65 years and older account for 45% of all ED visits, compared to 18% in community hospitals. 1 , 2 In general, compared to younger patients, older adults experience longer ED visits, higher admission rates, and more frequent ED revisits. 3 , 4 , 5 , 6 Older adult ED visits are often driven by unmet needs or unrecognized geriatric syndromes. Identifying and addressing those needs and syndromes leads to decreased hospital admissions and health care costs. 7 , 8 In 2014, Geriatric ED Guidelines were published by a collaboration of emergency and geriatric organizations to provide a framework for addressing these health care disparities and opportunities to improve care. 9 Based on the guidelines, the American College of Emergency Physicians developed a three leveled Geriatric ED Accreditation standardized system to promote these best practices and allow facilities to receive recognition for providing a specific level of focused geriatric Emergency Medicine care. 9 , 10
VA is an ideal place to implement geriatric ED programming and promote accreditation given the high proportion of older Veterans within the system, the broad range of patient‐centered resources available, and the integration of health care across the enterprise. In addition to the geriatric ED principles promoted by accreditation, the VA is also an ideal place for large‐scale implementation of the 4 M model of Age‐Friendly Health Systems. 11 , 12 The 4 M Model (what Matters, Mobility, Mentation, and Medication) was developed by a partnership with the John A Hartford Foundation and the Institute for Healthcare Improvement to address the interrelated health care needs of older adults. 11 In addition to the 4 M model, the Institute for Healthcare Improvement has structured frameworks for implementing the 4Ms in inpatient and outpatient office settings. 11 While the VA is an ideal system for adopting these frameworks, implementing either in the ED can be challenging for the following reasons: (1) the current clinical condition of the patient; (2) time constraints of ED staff; (3) lack of a previous relationship with the patient; and (4) the nuances of the available frameworks, which do not lend themselves to an ED setting. 13 , 14 Success of geriatric ED programs using a screening model in which they identify high risk older adults, then provide additional screening and care coordination by geriatric emergency medicine trained champions provides an innovative framework for integrating the 4Ms into ED care that does not rely on either the inpatient or outpatient Institute for Healthcare Improvement framework. 7 , 8 , 15
In 2020, the VA Offices of Emergency Medicine and Geriatrics & Extended Care launched 20 VA facilities toward a goal of geriatric ED accreditation as phase one of a three‐phase initiative to promote geriatric emergency medicine across the VA enterprise. 16 This phased approach allowed the VA to identify implementation barriers and allow for collaboration across VA service lines. VAs sought innovative responses to address: (1) emergency department 4 M delivery, (2) transitions of care, and (3) social determinants of health, including the digital divide experienced by older adults. This approach resulted in the VA launching a feasibility pilot program, SCOUTS (Supporting Community, Outpatient, Urgent Care & Telehealth Services), at six of the 20 VA geriatric EDs. 17 , 18 Additional motivations for addressing the digital divide were the VA goals of increasing access to care through telehealth and decreasing the number of patients requiring health care facility visits during the COVID pandemic. 19 , 20 SCOUTS is a post‐ED follow‐up program where Intermediate Care Technicians (ICTs) perform in‐home screenings based on the 4Ms of age‐friendly health systems, screen for unmet care needs, provide care coordination, and make telehealth connections to VA ED providers or acute care geriatricians. ICTs are former military Navy Corpsmen, Air Force and Coast Guard Medical Technicians, or Army Combat Medics integrated into interdisciplinary care teams within VA to provide high‐level clinical support.
We describe the implementation of a clinical pilot program to identify unmet needs for older Veterans by integrating the 4 M model into geriatric ED processes using dedicated staff and by promoting a follow‐up program to complete screening and care coordination and provide a second touch.
2. METHODS
2.1. SCOUTS workforce
The SCOUTS program includes ICTs and emergency medicine physicians. In the military, medics, and corpsmen receive extensive standardized medical training to provide support to military operations. 21 VA started a pilot in 2012 to employ former corpsmen and medics as ICTs in VA EDs. 21 , 22 ICTs are unlicensed personnel who work under the direction and clinical oversight of a physician or licensed independent provider. ICTs require VA‐specific training and competencies to perform tasks such as geriatric screens, splint placement, or wound care. 21 Being Veterans themselves, ICTs are in a unique position to connect with Veteran patients and assist with VA health and benefit navigation. 21 , 22 Each SCOUTS site has an emergency medicine physician serving as a local champion to oversee training compliance, competency completion, local workflow, documentation, and quality improvement. Finally, a core team from the VA Office of Primary Care is responsible for the overall program coordination, development, training plan, data collection, and analysis.
2.2. SCOUTS program support
The SCOUTS program is under the VA Office of Primary Care which oversees the ICT Program but was developed as a collaboration between Offices of Primary Care, Geriatrics & Extended Care, Home Based Primary Care, and Emergency Medicine with additional input from VA telehealth.
SCOUTS content was based on the Louis Stokes Cleveland VA Medical Center geriatric ED model. The Cleveland program, developed in 2016, uses ICTs to perform geriatric screens and care coordination in the ED and was the first VA Geriatric ED accredited at the highest level by the American College of Emergency Physicians. 1 , 8 , 16 The VA expanded geriatric ED programming into an additional 20 VA EDs in 2019–2020.
2.3. Site selection
From the first 20 VA EDs, six sites were identified to participate in the SCOUTS pilot program in 2021. These sites were chosen by the Office of Primary Care pilot core team due to their successful onboarding of geriatric ED programming and existing ICTs programs. These sites were also chosen to represent various ED sizes based on the annual patient census and those serving predominately urban or rural dwelling populations.
2.4. Description of sites
The six sites represent EDs ranging from 5 beds‐40 beds. Total ED visits/year (2019–2021) ranged from 7500 to 39,000, with an average of 45% of the ED visits by patients 65 years and older per internal VA ED management. The percent of Veterans living in a rural area served by the six pilot sites in 2021 ranged from 4% to 55% per internal VA rural health data. Each site had an existing geriatric ED process in which they identified and performed screens and care coordination on high‐risk older adults. Descriptions of each site's ED programs were collected in a pre‐implementation survey. Sites were asked to develop an additional process to identify patients who would be offered a SCOUTS post‐ED follow‐up visit.
2.5. Site onboarding
SCOUTS sites received support through three phases of guided implementation from the core team. Phase one included site application approval by the SCOUTS core team, followed by a memorandum of understanding outlining requirements for participation. Phase two included the identification of participating employee personnel, a pre‐implementation of site‐specific geriatric ED practices, training, and competency of all SCOUTS ICTs, and development of the local workflow. Phase three was the “green light” from the core team to start SCOUTS home visits. As SCOUTS ICTs continue to provide ED follow‐up care in the home, phase three includes data collection and sharing, continuous program improvement, and quality evaluation.
2.6. The SCOUTS visit
Older Veterans are eligible for a 48–72 h follow‐up SCOUTS visit if they are (1) identified as high risk through ED screening, (2) not currently living in a skilled nursing facility, and (3) discharged home from the ED. Each site developed its own protocol to identify high‐risk patients as part of their local geriatric ED workflow, with the Identification of Seniors at Risk (ISAR) screen 23 being a common initial identifier. Patients identified as eligible are offered a follow‐up home visit during their ED visit or via a follow‐up phone call. Visits may be scheduled at the time of the ED visit or after discharge. Prior to the home visit, the ICT performs a chart review for existing and previous VA services, behavior flags, connection to the primary care team, presence of advanced directives or goals of care notes, and previous orders for durable medical equipment. Telephone visits are offered if a home visit is declined.
During the home visit, the ICTs perform vital signs and record the patient's goals for the visit. ICTs can also perform screens for delirium (Delirium Triage Screen plus Brief Confusion Assessment Method), cognitive impairment (Abbreviated Mental Test‐4 and Mini‐Cog), caregiver burden (Zarit 4), function (Katz Activities of Daily Living), fall risk (STopping Elderly Accidents, Deaths, & Injuries [STEADI]), and elder mistreatment (EM‐SART [Elder Mistreatment Screening AND Response Tool] modified to questions and observations only). 24 , 25 , 26 , 27 , 28 , 29 , 30 ICTs also inquire about food insecurity, instrumental activities of daily living, medication risk/polypharmacy, home accessibility (entrance, stairs, and bathroom), transportation, home environment (fall risks, cleanliness, working utilities), and social support. 31 Veterans are asked to identify a caregiver, for permission to interview that caregiver, and to include the caregiver in the plan (either in person at the time of the visit or via phone). Caregivers are asked about activities of daily living and instrumental activities of daily living assistance, the amount of time spent weekly as a caregiver, and if they have any help (either paid or unpaid) to assist them with supporting the Veteran. The caregiver's questions can be provided verbally, or the caregiver can fill out a paper form. If any of the screens were performed in the ED as part of the site's regular geriatric ED practice, they were not repeated in the home, with the exception of the Abbreviated Mental Test‐4.
2.7. 4 M integration
During the home visit, the ICTs garner trust and learn “what matters most” through an unstructured interview with the patient. Caregivers are asked specifically “Is there anything else you would like us to know about the Veteran?” so that the health care team has an alternate way to understand “what matters.” Medication is addressed using the polypharmacy screen and the ICT's ability to view the medication organization. Mobility is addressed via the STEADI screen, 29 a mobility trial or functional screen, and observation of fall risks in the home. Mentation is addressed via delirium and cognitive impairment screening. ICTs introduce VA services to the patient based on positive screens and patient/caregiver inquiries. SCOUTS summary notes are sent to Veterans' primary care providers and care coordination can occur both during and after the home visit. While in the home, the ICTs facilitate video telehealth visits with VA emergency medicine physicians (five sites) or acute care geriatricians (one site). This telehealth visit serves as an opportunity for post‐ED follow up including assessment of acute conditions and reinforcement of ED discharge instructions. Additionally, the ICT works with the physician to develop an action plan to address positive screens, unmet care needs, and home safety risks. ICTs bridge Veterans back to their primary care team and specialty providers by assisting with health care system navigation and providing warm handoffs. Eligible patients can also receive a VA‐issued tablet for future telehealth appointments similar to the device used for the telehealth visit (Table S1). The VA provides devices that include cellular service; therefore, home Internet availability is not a requirement.
2.8. Data collection and analysis
A pre‐implementation survey was sent to each of the pilot sites via Microsoft Forms in March 2021. The survey was completed by the SCOUTS physician or nurse champion. Sites were asked about existing geriatric ED resources such as social work and pharmacy. Surveys requested information on the current ICT program at each site including ED procedures performed, geriatric screens performed including those that align with Age‐Friendly Health System 4Ms, and elements of care coordination completed by ICTs. Sites were asked about the current geriatric ED accreditation level and the plan to increase their level of accreditation.
Data from the pilot was collected during the SCOUTS patient encounter using the standardized electronic health record template, located in the VA electronic medical record that was provided to the sites.
Data for the SCOUTS pilot program evaluation was extracted from the electronic medical record through the VA Corporate Data Warehouse. Data points extracted were screens and observations from the SCOUTS patient encounters recorded in the electronic health record template, consult and referral orders, telehealth documentation, and Patient Alignment Care Team visits. VA Patient Alignment Care Teams include an assigned primary care provider, social worker, pharmacist, dietician, and nurse case manager. 32 Descriptive statistics are presented for the 6‐month pilot feasibility evaluation from May–October 2021.
The SCOUTS pilot program and evaluation plan were submitted to the Office of VA Research and Development and deemed exempt from Institutional Review Board review.
3. RESULTS
3.1. Pre‐implementation site survey
All 6 six sites (100%) completed the pre‐implementation survey. ICTs performed multiple ED procedures such as wound closure and extremity splinting (Appendix A; Figures A1, A2). ED social work was available at 67% (4/6) sites for at least part of the week, and 83% (5/6) had ED pharmacist support. Of the six sites, one site is applying for Level 1 geriatric ED accreditation, one is currently a Level 2 accredited geriatric ED, and four are currently Level 3 accredited geriatric EDs. All current levels 2 and 3 s are applying to increase to the next highest level in 2022.
ICTs performed a variety of different geriatric screens in the ED depending on existing ICT programs and ED processes. The Mini‐Cog was the most common screen (4/6) followed by bCAM, delirium triage screen, ambulation observation, Katz activities of daily living, and Zarit‐4 Caregiver screen (all 3/6) (Figure 1). ICTs continued to perform these high‐risk screens in the ED throughout the SCOUTS pilot. Per the pre‐implementation survey, ICTs also performed a variety of care coordination roles in 3/6 sites; coordination with ED social work and physical therapy being the most common (3/6) (Appendix A; Figures A1, A2). None of the sites regularly counseled patients on telehealth technology or had a standardized way to obtain or document what matters.
FIGURE 1.
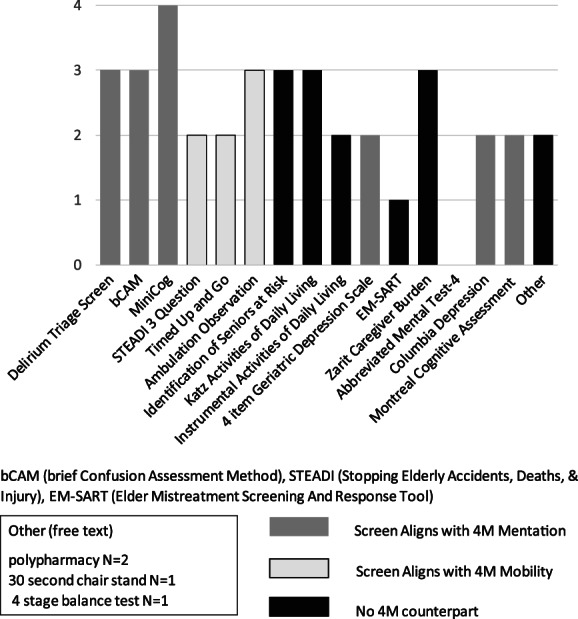
Pre‐Pilot geriatric screens performed by ICTs n = 6 sites. bCAM (brief confusion assessment method), STEADI (stopping elderly accidents, deaths, and injury), EM‐SART (elder mistreatment screening and response tool). Other (free text). Polypharmacy N = 2. 30‐s chair stand N = 1. 4‐stage balance test N = 1.
3.2. Pilot
ICTs performed 303 visits, 247 of which were home visits. The remainders were telephone visits. All home visits included a telehealth visit with an ED provider (n = 244) or acute care geriatrician (n = 3). Additional telehealth visits were made with social work (n = 1) and pharmacy (n = 1).
ICTs performed geriatric screens on 208 Veterans in the home (Figure 2). Unmet home needs and social determinants of health, such as lack of social support, inadequate bathroom access, food insecurity, and sanitation/housekeeping problems, were identified 99 times. ICTs identified 44 modifiable home fall risks, 45 activities of daily living needs, and 142 instrumental activities of daily living needs not previously identified in the ED and ordered 80 pieces of durable medical equipment from VA stock (Figure 3). ICTs identified immediate concerns requiring intervention by the ED physician or acute care geriatrician on 31 occasions.
FIGURE 2.
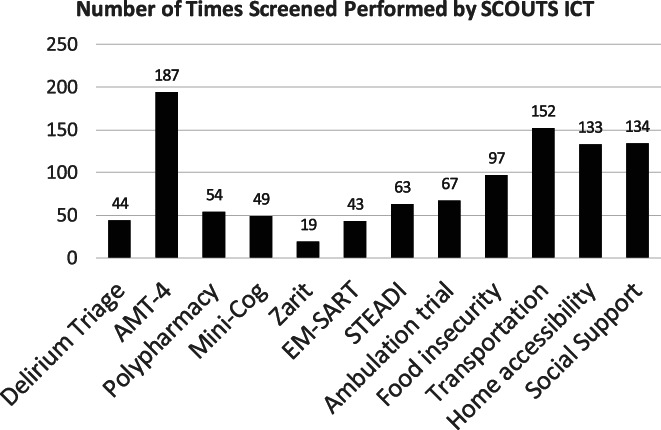
SCOUTS geriatric screens performed May–Oct 2021, n = 208 patients
FIGURE 3.
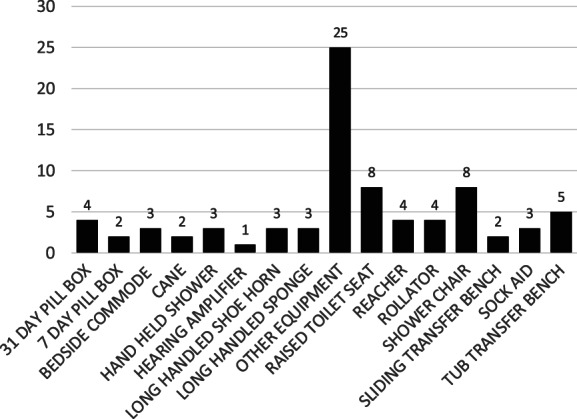
Durable medical equipment ordered May–October 2021, n = 208 SCOUTS patients
Thirty‐six consults were placed for specific services and 180 (73%) patients were connected back to at least one member of their Patient Aligned Care Team for follow‐up services. Thirteen patients were ordered tablets for future home visits and six patients received specific education on their own devices.
Patients identified 126 individuals who provided them with social support. Nineteen caregivers were interviewed about their role in helping the Veterans and screened for caregiver burden (Figure 3). The most common tasks they assisted with were shopping (14/19), assisting Veterans to receive medical care (12/19), transportation (12/19), laundry (13/19), and housekeeping (12/19).
4. DISCUSSION
The SCOUTS pilot program is innovative in that it not only assists with ED to home transitions of care but also identifies unmet needs and increases access to health care services using telehealth technologies, based on the 4Ms framework. We found that VA ICTs trained on geriatric‐specific syndromes can successfully identify health care needs and assist with transitions of care in a home‐based environment. The SCOUTS program suggests that home‐based interventions focusing on the 4Ms framework for older adults are feasible and can identify needs beyond those in a traditional office or ED‐based setting. Sites previously not performing all 4Ms in the ED were able to complete mobility, mentation, and medication screens in the home. ICTs were able to identify what mattered to the patient and his/her caregiver in the patient's own environment.
The ICT SCOUTS program provides multiple opportunities to intervene both during and after the ED visit. Acute ambulatory care conditions can be seen as a multi‐visit evaluation and treatment opportunity within the VA that includes a home visit rather than through hospital admission. Adults aged 65 years and older represent the fastest‐growing population in the US. 2 Older adults requiring admission are at risk for “hazards of hospitalization,” which include cognitive impairment, a decline in functional status, and discharge to skilled nursing facilities. 33 , 34 In response to the unique challenges of older adult care in the ED, emergency medicine and geriatric organizations have evidence‐based strategies for redesigning the clinical structure of geriatric emergency medicine and promoting a comprehensive geriatric ED evaluation. 9 , 35 This evaluation is done by staff with specific geriatric ED education and time to perform care coordination. 9 , 35 Furthermore, studies have demonstrated improved outcomes with multi‐strategy and multi‐touch interventions to prevent functional decline and hospital admission. 36 , 37
Strategies to address the 4Ms must take into account the practice setting and fair distribution of services. 12 Patients who are unstable or are suffering with pain or discomfort may not be able to participate in screening. Likewise, patients who have minor acute issues may not be in the ED long enough to participate in extensive screening. Extending the ED length of stay may not be feasible given the ED volume and fair distribution of ED space amongst all of the patients seeking care. Additionally, caregivers are not always available in the ED secondary to COVID‐19 or other infectious disease protocols or timing of the visit. 38 This feasibility pilot demonstrates that patients identified as high risk can have care plans initiated in the ED completed in the home, including screening for unmet care needs and geriatric syndromes. Sites that do not have a process to address all 4Ms in the ED for these older adults can accomplish this through a SCOUTS visit. This study also supports a targeted approach to 4 M screening in the ED rather than a blanket approach. 12
Each of the 4Ms was addressed via the geriatric ED process or SCOUTS process. What matters was ascertained using an unstructured interview, chart review for the presence of advanced directives, and discussions with the caregiver to provide additional information. In this way, “what matters” could be obtained even if the patient was unable to participate in the conversation. The ICT documented these findings and then shared them with the Veterans Primary Care team in addition to the telehealth ED provider. Additional social determinants of health that are not directly related to what matters traditionally, but significantly impact quality of life and overall well‐being, such as food insecurity, access to transportation, ability to perform instrumental activities of daily living, access to heat, water, electricity; and clean living environment were also addressed. ICTs were empowered to recommend interventions based on positive 4 M screens and provide patient and caregiver education, via their training, competency, and telehealth connection to emergency physicians.
This intervention also addressed the digital divide that older adults with chronic illnesses may experience. 39 , 40 Older adults are often willing to try tablet technology but may need assistance with navigation and ongoing support. 40 In this program, Veterans were able to experience a video visit from their home in addition to receiving instructions on how to use a personal or VA‐issued device for future telehealth appointments. The digital device program within the VA includes cellular service (5G) and ongoing technologic support. Additional training is also available through this program and assists patients remotely with the use of their VA tablet.
SCOUTS addresses care transition gaps within the VA that affect health outcomes. 17 ED providers can send patients home knowing that there will be an additional opportunity to “get eyes” on the patient, reinforce discharge instructions, and the ability to participate in the home safety check via video. Access to rapid follow‐up to recheck acute ambulatory conditions are a component of emergency physician admission decision making process. 41 This program allows the ED providers to own the acute care condition evaluation regardless of the day of the week and in situations where direct primary care visit scheduling is not feasible or accessible. Additionally, care transitions that are typically limited by cognitive impairment, social isolation, or economic disadvantages within the VA can be ameliorated with a SCOUTS home visit and introduction of telehealth to patients and their caregivers. 17 , 42
This pilot has several strengths. First, we conducted this pilot in the VA, the largest integrated health care system with many resources available for older Veterans. For this reason, we were able to not only screen for a variety of unmet needs but also connect these Veterans to existing services to meet these needs. We utilize ICTs, unique to the VA, for this program. ICTs have an inimitable skillset allowing for (1) Veteran to Veteran connection, (2) ability to perform screening tools, and (3) medical interventions such as wound care. 21 , 22 This constellation of skills make them an ideal provider for home‐based interventions for older adults. Additionally, given nurse and homecare staffing shortages nationwide, ICTs were able to perform home safety evaluations and identify unmet needs that otherwise may not have been addressed for months.
There are several limitations in this program evaluation. Screens that were done in the ED were not repeated in the home and consults placed or equipment ordered during the ED visit were not counted in this program review, thus our data may not fully describe the care needs of the patients served. Given the variation between site processes for offering home visits to patients, a comparison to care‐eligible patients is not possible, nor was a calculation of the percentage of eligible patients who received a home visit. Additionally, there are likely high‐risk patients who may have benefited but did not receive a home visit.
This study was conducted in the VA and may not be generalizable to non‐VA settings, but integrated health care systems may be able to implement similar programs. ICTs are a unique position within the United States Department of VA allowing former military medics without civilian certification to practice as unlicensed personnel. Currently, only the state of Virginia has passed legislation establishing the Military Medics and Corpsman Program which allows transitioning Veterans to use their skills in a civilian setting, but within one year they must be enrolled in a state‐approved education program working toward a licensed/credentialed profession. 43 In non‐VA settings nurses, social workers, or paramedics may perform geriatric screens in the ED or in the home and future studies could evaluate if the addition of telehealth with an acute care provider could promote patient‐centered outcomes or improve accountable care organization metrics.
While this study focused on a pilot implementation program, future data analysis will include the number of patients who go on to engage in telehealth and specific screen outcomes. Additional site participation and modifications in the pilot scope allowing post‐ED follow‐up for Veterans seen at community hospitals and Veterans served by VA urgent care telehealth platforms will be explored. Return on investment calculations will consider both short‐term outcomes such as ED revisit rates and long‐term outcomes such as extended care facility admissions or hospital bed occupation days.
5. CONCLUSION
SCOUTS, a post‐ED follow‐up program in which former military medics perform geriatric screens and care coordination, is feasible. Using a home visit by an ICT to connect the patient via telehealth to a licensed provider, allows for the identification and management of unmet care needs and optimizes care using the 4Ms of Age‐Friendly Health Systems‐mobility, mentation, medication, and what matters.
FUNDING INFORMATION
The VA Geriatric ED Accreditation described within the background and method sections is supported through a National VA partnership with the John A Hartford Foundation (JAHF) and the Gary and Mary West Health Institute (WHI). Geriatric ED Accreditation was a criterion for pilot site selection and all 10 pilot sites' accreditation processes occurred prior to SCOUTS and were part of the VA/JAHF/WHI partnership. The partnership supported accreditation fee waivers, provided education for the accreditation through the Geriatric Emergency Department Collaborative, and supported in part, a VA National Geriatric ED Core Team program lead, a VA program manager, and a VA analyst.
The SCOUTS pilot program received support in part from Veterans Health Administration (VHA) finance through Congressional COVID/Care Act Relief funding. VHA finance supports the ICT SCOUTS pilot implementation, program analysts' time, field coordinators' time, the pilot medical director, and medical direction at 10 participating VA Medical Centers. ICT SCOUTS program is a VA collaborative pilot through the Office of Primary Care, Office of Emergency Medicine and Office of Geriatrics and Extended Care. We report no conflicts of interest with any of the authors and none are supported by JAHF or WHI.
Supporting information
Table S1. VA Eligibility criteria: VA issued tablet for home telehealtha.
ACKNOWLEDGMENTS
We would like to thank our Veterans Affairs colleagues Dr. Sunah Song and Ms. Tongyezhi Sheng for their assistance with data collection and Dr. Thomas Edes, Dr. Thomas Matras, Ms. Dayna Cooper, and Ms. Darlene Davis for their mentorship and advocacy in the pilot development and sustainment.
APPENDIX A.
FIGURE A1.
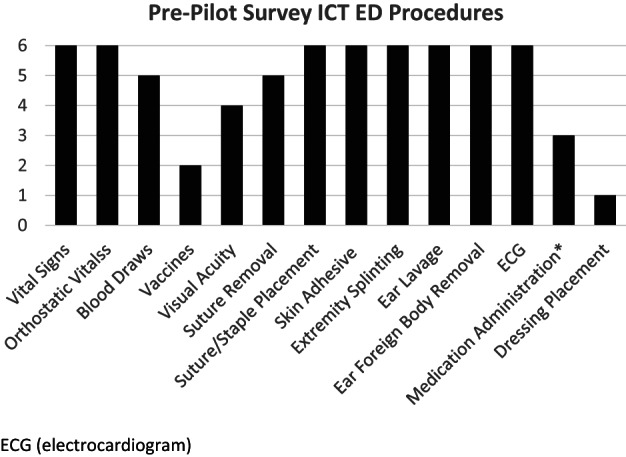
ICT emergency department procedures performed during pre‐pilot period. N = 6 sites. ECG, electrocardiogram.
FIGURE A2.
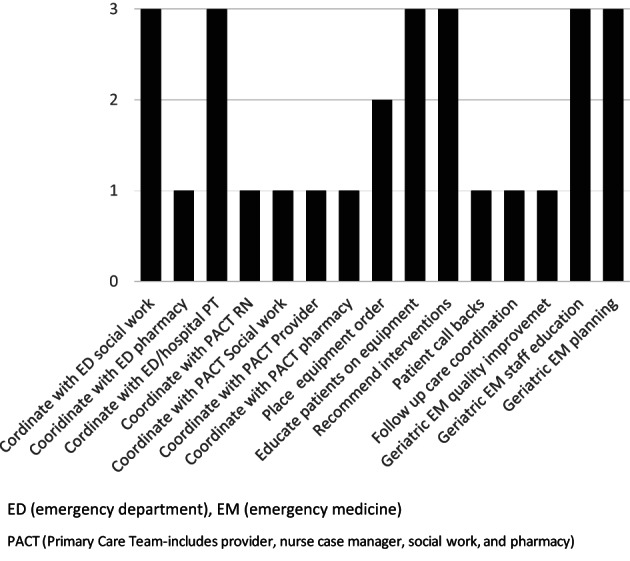
Pre implementation survey: Additional ICT geriatric emergency department tasks n = 6 sites. ED, emergency department; EM, emergency medicine.
McQuown CM, Snell KT, Abbate LM, Jetter EM, Blatnik JK, Ragsdale LC. Telehealth for geriatric post‐emergency department visits to promote age‐friendly care. Health Serv Res. 2023;58(Suppl. 1):16‐25. doi: 10.1111/1475-6773.14058
Funding information Gary and Mary West Health Institute; John A. Hartford Foundation
REFERENCES
- 1. Huded JM, Lee A, McQuown CM, et al. Implementation of a geriatric emergency department program using a novel workforce. Am J Emerg Med. 2021;46:703‐707. [DOI] [PubMed] [Google Scholar]
- 2. Center for Disease Control and Prevention . National Hospital Ambulatory Medical Care Survey: 2018 Emergency Department Summary Tables. Accessed January 7, 2022. https://www.cdc.gov/nchs/data/nhamcs/web_tables/2018-ed-web-tables-508.pdf
- 3. Hastings SN, Barrett A, Weinberger M, et al. Older patients' understanding of emergency department discharge information and its relationship with adverse outcomes. J Patient Saf. 2011;7(1):19‐25. [DOI] [PubMed] [Google Scholar]
- 4. Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39(3):238‐247. [DOI] [PubMed] [Google Scholar]
- 5. Lowenstein SR, Crescenzi CA, Kern DC, Steel K. Care of the elderly in the emergency department. Ann Emerg Med. 1986;15(5):528‐535. [DOI] [PubMed] [Google Scholar]
- 6. Schnitker L, Martin‐Khan M, Beattie E, Gray L. Negative health outcomes and adverse events in older people attending emergency departments: a systematic review. Australas Emerg Nurs J. 2011;14(3):141‐162. [Google Scholar]
- 7. Hwang U, Dresden SM, Vargas‐Torres C, et al. Association of a geriatric emergency department innovation program with cost outcomes among medicare beneficiaries. JAMA Netw Open. 2021;4(3):e2037334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Huded JM, Lee A, Song S, et al. Association of a geriatric emergency department program with healthcare outcomes among veterans. J Am Geriatr Soc. 2022;70(2):601‐608. [DOI] [PubMed] [Google Scholar]
- 9. Carpenter CR, Bromley M, Caterino JM, et al. Optimal older adult emergency care: introducing multidisciplinary geriatric emergency department guidelines from the American College of Emergency Physicians, American Geriatrics Society, emergency nurses association, and Society for Academic Emergency Medicine. J Am Geriatr Soc. 2014;62(7):1360‐1363. [DOI] [PubMed] [Google Scholar]
- 10. Kennedy M, Lesser A, Israni J, et al. Reach and adoption of a geriatric emergency department accreditation program in the United States. Ann Emerg Med. 2021;S0196‐0644(21):513‐518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fulmer T, Mate KS, Berman A. The age‐friendly health system imperative. J Am Geriatr Soc. 2018;66(1):22‐24. [DOI] [PubMed] [Google Scholar]
- 12. Burke RE, Brown RT, Kinosian B. Selecting implementation strategies to drive age‐friendly health system adoption. J Am Geriatr Soc. 2022;70(1):313‐318. [DOI] [PubMed] [Google Scholar]
- 13. Bambach K, Southerland LT. Applying geriatric principles to transitions of care in the emergency department. Emerg Med Clin North Am. 2021;39(2):429‐442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Megalla M, Avula R, Manners C, Chinnery P, Perrella L, Finefrock D. Using the 4M model to screen geriatric patients in the emergency department. J Geriatr Emerg Med. 2021;2(9):1‐6. [Google Scholar]
- 15. Wallis M, Marsden E, Taylor A, et al. The geriatric emergency department intervention model of care: a pragmatic trial. BMC Geriatr. 2018;18(1):297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. VA launches program to improve emergency care for nation's older veterans. John a. Hartford Foundation. Published September 9, 2021. Accessed February 08, 2022. https://www.johnahartford.org/newsroom/view/va-launches-program-to-improve-emergency-care-for-nations-older-veterans
- 17. Gettel CJ, Voils CI, Bristol AA, et al. Care transitions and social needs: a geriatric emergency care applied research (GEAR) network scoping review and consensus statement. Acad Emerg Med. 2021;28(12):1430‐1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Adams SV, Mader MJ, Bollinger MJ, Wong ES, Hudson TJ, Littman AJ. Utilization of interactive clinical video telemedicine by rural and urban veterans in the veterans health administration health care system. J Rural Health. 2019. Jun;35(3):308‐318. [DOI] [PubMed] [Google Scholar]
- 19. Department of Veterans Affairs. FY 2018‐2024 Strategic Plan. Updated May 31, 2019. Accessed March 14, 2022. https://www.ea.oit.va.gov/EAOIT/docs/July2019/VA2018-2024strategicPlan.pdf
- 20. U.S. Government Accountability Office . Veterans Affairs: Use of Additional Funding for COVID‐19 Relief. Published May 05, 2021. Accessed March 14, 2022. https://www.gao.gov/products/gao-21-379
- 21. McQuown CM, Snell KT, Edes T. Intermediate care technicians‐a novel workforce for veterans affairs geriatric emergency departments. J Geriatr Emerg Med. 2021;2(12):S1‐S4. [Google Scholar]
- 22. Watts B, Lawrence RH, Schaub K, et al. Transitioning former military medics to civilian health care jobs: a novel pilot program to integrate medics into ambulatory care teams for high‐risk patients. Mil Med. 2016;181(11):e1464‐e1469. [DOI] [PubMed] [Google Scholar]
- 23. Warburton RN, Parke B, Church W, McCusker J. Identification of seniors at risk: process evaluation of a screening and referral program for patients aged 75 and over in a community hospital emergency department. Int J Health Care Qual Assur. 2004;17(6):339‐348. [DOI] [PubMed] [Google Scholar]
- 24. Han JH, Wilson A, Vasilevskis EE, et al. Diagnosing delirium in older emergency department patients: validity and reliability of the delirium triage screen and the brief confusion assessment method. Ann Emerg Med. 2013;62(5):457‐465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Borson S, Scanlan JM, Chen P, Ganguli M. The mini‐cog as a screen for dementia: validation in a population‐based sample. J Am Geriatr Soc. 2003;51(10):1451‐1454. [DOI] [PubMed] [Google Scholar]
- 26. Carpenter CR, Banerjee J, Keyes D, et al. Accuracy of dementia screening instruments in emergency medicine: a diagnostic meta‐analysis. Acad Emerg Med. 2019;26(2):226‐245. [DOI] [PubMed] [Google Scholar]
- 27. Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, O'Donnell M. The Zarit burden interview: a new short version and screening version. Gerontologist. 2001;41(5):652‐657. [DOI] [PubMed] [Google Scholar]
- 28. Katz S. Assessing self‐maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983;31(12):721‐727. [DOI] [PubMed] [Google Scholar]
- 29. Helsel BC, Kemper KA, Williams JE, Truong K, Van Puymbroeck M. Multidimensional risk score to stratify community‐dwelling older adults by future fall risk using the Stopping elderly accidents, deaths and injuries (STEADI) framework. Inj Prev. 2021;27(5):461‐466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Platts‐Mills TF, Sivers‐Teixeira T, Encarnacion A, Tanksley B, Olsen B. EM‐SART: a scalable elder mistreatment screening and response tool for emergency departments. Generations. 2020;44(1):51‐58. [Google Scholar]
- 31. Cohen AJ, Rudolph JL, Thomas KS, et al. Food insecurity among veterans: resources to screen and intervene. Fed Pract. 2020;37(1):16‐23. [PMC free article] [PubMed] [Google Scholar]
- 32. Sullivan JL, Eisenstein R, Price T, Solimeo S, Shay K. Implementation of the geriatric patient‐aligned care team model in the veterans health administration (VA). J Am Board Fam Med. 2018;31(3):456‐465. doi: 10.3122/jabfm.2018.03.170272 [DOI] [PubMed] [Google Scholar]
- 33. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118(3):219‐223. [DOI] [PubMed] [Google Scholar]
- 34. Lindquist LA, Go L, Fleisher J, Jain N, Baker D. Improvements in cognition following hospital discharge of community dwelling seniors. J Gen Intern Med. 2011;26(7):765‐770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hwang U, Carpenter C. Assessing geriatric vulnerability for post emergency department adverse outcomes: challenges abound while progress is slow. Emerg Med J. 2016;33(1):2‐3. [DOI] [PubMed] [Google Scholar]
- 36. Hughes JM, Freiermuth CE, Shepherd‐Banigan M, et al. Emergency department interventions for older adults: a systematic review. J Am Geriatr Soc. 2019;67(7):1516‐1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Karam G, Radden Z, Berall LE, Cheng C, Gruneir A. Efficacy of emergency department‐based interventions designed to reduce repeat visits and other adverse outcomes for older patients after discharge: a systematic review. Geriatr Gerontol Int. 2015;15(9):1107‐1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Biese K, Lock SL, Agha Z. Caregivers are not visitors. J Am Coll Emerg Phys Open. 2022;3(1):e12659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Frydman JL, Gelfman LP, Goldstein NE, Kelley AS, Ankuda CK. The digital divide: do older adults with serious illness access telemedicine? J Gen Intern Med. 2021;37(4):984‐998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gleason K, Suen JJ. Going beyond affordability for digital equity: closing the "digital divide" through outreach and training programs for older adults. J Am Geriatr Soc. 2022;70(1):75‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Carmel AS, Steel P, Tanouye R, et al. Rapid primary care follow‐up from the ED to reduce avoidable hospital admissions. West J Emerg Med. 2017;18(5):870‐877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gettel CJ, Falvey JR, Gifford A, et al. Emergency department care transitions for patients with cognitive impairment: a scoping review. J Am Med Dir Assoc. 2022;S1525‐8610(22):154‐152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Virginia Department of Veterans Services . Military Medics and Corpsman Program. Accessed June 28th, 2022. https://www.dvs.virginia.gov/education-employment/military-medics-corpsmen-mmac-program
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. VA Eligibility criteria: VA issued tablet for home telehealtha.


