Abstract
HIV stigma remains a barrier in achieving optimal HIV treatment. We studied the prevalence and predictors of HIV stigma among adolescents and youth with HIV (AYWHIV) ages 15–24 years in Western Kenya. Of 1011 AYWHIV, 69% were female with a median age of 18 years. Most (59%) attended adolescent clinic days, and 40% attended support groups. One-quarter (27%) had experienced physical, 18% emotional, and 7% sexual violence. The majority of AYWHIV (88%) reported disclosure concerns, 48% reported perceived community stigma, 36% experienced, and 24% internalized stigma. Compared to AYWHIV attending adolescent clinics, those in general/adult clinics had higher internalized stigma. Similarly, having dropped out of school was associated with higher internalized stigma. AYWHIV in sexual relationships had higher experienced stigma and disclosure concerns. Lastly, exposure to violence was associated with higher experienced, internalized, perceived community stigma and disclosure concerns. These risk factors can be targeted when developing stigma-prevention interventions.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10461-023-03982-9.
Keywords: HIV stigma, Stigma types, Adolescent, Youth, Violence, Sexual behavior
Introduction
Stigma is a socially damaging phenomenon where people living with HIV (PLHIV) are considered socially undesirable, lose their social standing, lose power when relating with people in their communities, and are denied certain benefits and freedoms enjoyed by other members of their communities [1]. Functioning as a multi-level process consisting of intrapersonal, interpersonal, community, institutional and structural domains [2], stigma is an important driver of the HIV pandemic, and remains a barrier in achieving optimal HIV treatment targets [1, 3, 4]. The experience of stigmatizing attitudes and actions from others (experienced stigma) may result in PLHIV feeling less valued (internalized stigma). How close family and friends, community members and institutions treat PLHIV shapes their perception of the community’s tolerance (perceived community stigma) and influences their expectation of how they may be treated in future (anticipated stigma).
HIV stigma is associated with poor HIV outcomes including antiretroviral therapy (ART) non-adherence, viral non-suppression, and poor mental health [5]. Among adolescents and youth with HIV (AYWHIV), HIV stigma is a particularly challenging experience since they are starting to consciously nurture meaningful relationships. These include peer relationships, which are important sources of social support [6, 7], and often may require or lead to involuntary disclosure of HIV status, presenting a potential risk of rejection, discrimination, and violence including intimate partner violence and emotional harm [8–10]. The lack of self-efficacy to deal with rejection and other negative reactions from others HIV status gets known remains a key challenge that further accentuates poor outcomes for AYWHIV faced with stigma [11]. The experience of HIV stigma is also in the context of significant intersectionality including with other stigmatized identities including minority sexual orientation and gender identity, and in some contexts race and ethnicity [12–15]. Mental illness, which for some diagnoses like depression peaks in adolescence is highly stigmatized in some contexts and is accentuated by HIV stigma [15]. In addition to the non-adherence and viral non-suppression, HIV stigma among AYWHIV has also been associated with lowered quality of life [16], and increased use of alcohol and tobacco [17]. There is therefore merit in intervening against HIV stigma, including at the level of the predictors and the effects of stigma. The four HIV stigma types described in the health stigma and discrimination framework (experienced, internalized, anticipated, and perceived community stigma) [3, 18] are hypothesized to impact specific aspects of physical and mental health, health-seeking behaviors, social self-concept, and interpersonal relationships [3, 4, 19–25].
Interventions to reduce HIV stigma have been developed for diverse contexts. However, in systematic reviews [26–33] most stigma intervention studies were considered to be of low quality, non-specific, and few interventions demonstrated a direct effect on HIV stigma reduction. The complex, multi-layered nature of HIV stigma is likely a key reason for lack of intervention effectiveness. Interventions that focused on more than one stigma type and on multiple levels (individual to structural levels) showed higher effectiveness in reducing stigma [34, 35]. Structural interventions like the scale up of antiretroviral treatment, decriminalizing HIV [36], and poverty reduction have also been shown to significantly reduce stigma among adults living with HIV [28]. Few stigma interventions have been developed specifically for AYWHIV [34, 37], particularly those living in sub-Saharan Africa [34]. Improved understanding of factors that predict or co-occur with HIV stigma could enhance the development of stigma interventions. Previously identified upstream factors that were associated with HIV stigma include self-disclosure of HIV status, healthcare setting and judgement by providers, lower education, violence and poor HIV-related health [38–41]. None of these studies were among AYWHIV, and most did not evaluate specific stigma types [41]. Understanding co-occurrence of different HIV stigma types may also inform intervention development. We determined the prevalence of HIV stigma and HIV stigma types, and identified correlates of HIV stigma and types among AYWHIV.
Methods
Study Design
This was a nested cross-sectional analysis within a prospective cohort study of AYWHIV conducted in nine facilities in Western Kenya between April 2019 and March 2020 [42]. The primary goal of the parent study, Data-Informed Stepped Care (DiSC) to improve Adolescent HIV outcomes, was to conduct formative work towards the development of a data-driven, health systems intervention to improve engagement in care among AYWHIV ages 10–24 years in Kenya. In this analysis, we included participants aged 15–24 years. Western Kenya has a high burden of HIV among adolescents and youth [43]. Before the scale up of HIV testing and ART, many children and adolescents in the area were orphaned, with many either taking up parental responsibilities for their siblings, or having been assimilated by their extended families [44]. Relevant socio-cultural factors in this population include ‘widow-inheritance’ [45], where a close relative of her late husband assumes spousal responsibilities, and not practicing male circumcision [46]. Like other regions in Kenya, AYWHIV in Western Kenya go through the public school system, with a substantial proportion attending high schools with boarding facilities. The boarding schools especially pose a challenge for the learners in terms of storage of medication and keeping to required schedules for taking them medication and clinic attendance [47]. HIV care is largely provided through the donor-funded public health system, which in most places is not integrated with other health services.
Theoretical Model
In this project, we seek to expand the health stigma and discrimination framework, which proposes relationships between HIV stigma types and health/behavioral/interpersonal outcomes [3, 48]. In this paper, we do not assess stigma-outcomes relationships, but focus on the relationships between HIV stigma and factors likely more proximal to HIV stigma. We hypothesize that individual, interpersonal, community, institutional and structural level factors predict the severity of HIV stigma types (Fig. 1). The upstream factors were included based on evidence from previous studies showing relationships between the factor and HIV stigma [38–41]. We propose various mechanisms for the relationships between the factors and HIV stigma. We hypothesized that the structure of HIV clinics where adolescents and adults are seen in the same space and time, and where providers may not be trained to offer adolescent friendly services may increase HIV stigma. Similarly, an unconducive school environment, especially boarding schools where inadvertent disclosure is likely to occur would also expose AYWHIV to stigmatizing situations with fellow students and staff. We hypothesized that for AYWHIV, sexual relationships are potential sources of HIV stigma, again due to the likelihood of inadvertent disclosure and potential for rejection. Other experiences including having experienced violence, whether sexual, physical or emotional while likely being a result of HIV stigma, may also result in lower self-esteem and internalization of stigmatizing attitudes. Physical signs and association with someone suspected or known to be living with HIV may also predispose one to stigmatizing situations. For the factors included in the analysis, we discuss in detail probable mechanisms of their relationships with HIV stigma in the discussion section of this paper. We also discuss possible mechanisms for the influence these factors have on specific stigma types.
Fig. 1.
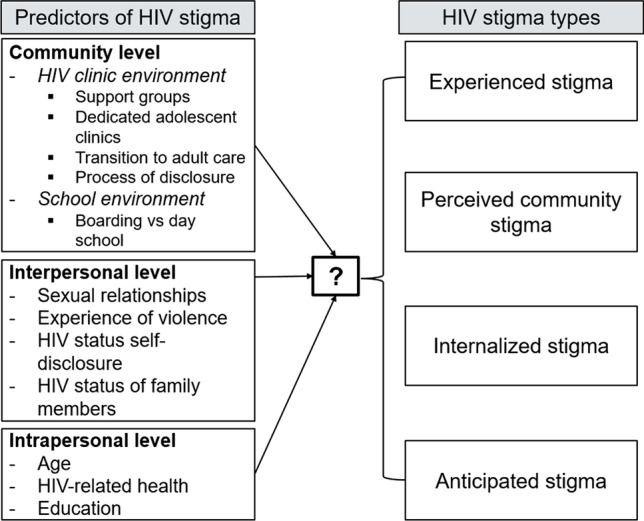
Health stigma and discrimination framework with hypothesized predictors of HIV stigma
Study Procedures
Recruitment and Enrollment
Recruitment was conducted in HIV clinics and maternal and child health (MCH) clinics serving pregnant or parenting AYWHIV commonly referred to prevention of mother to child transmission of HIV (PMTCT) clinics. Those who consented completed an enrollment questionnaire with socio-demographic information including age, sex, education, income, and food security. They provided HIV-related information including age at diagnosis, process of knowing their HIV status, perception of mode of HIV acquisition, participation in peer support groups, clinic type (adolescent, general/adult, PMTCT), self-disclosure of one’s HIV status, and information related to sexual activity.
Measures
HIV stigma was assessed using a 10-item Youth HIV Stigma Scale [49], an abbreviation of the 40-item Berger’s stigma scale [50]. Each question was assessed on a 5-item Likert scale (strongly disagree to strongly agree). The scale assessed four HIV stigma types—experienced/personalized stigma, internalized stigma/negative self-image, perceived community stigma/public attitudes towards people with HIV, and disclosure concerns which has a component clearly indicating anticipated stigma (worrying that those who know their status may disclose to someone), and being careful whom they disclose to—which may indicate anticipated stigma, a need for privacy, or so that others are not worried about them. We assessed the reliability of the scale using the Cronbach’s alpha [51]: overall stigma scale—α = 0.79; experienced stigma (3 questions)—α = 0.70; internalized stigma (3 questions)—α = 0.80; perceived community stigma (2 questions)—α = 0.74; disclosure concerns (2 questions)—α = 0.44. Social support was assessed using the 12-item Multidimensional Scale of Perceived Social Support (MPSS) [52]—α = 0.78, while the 2-item Connor Davidson Resilience Scale was used to assess resilience [53]—α = 0.59. Independence in care was measured using two questions assessing the AYWHIV’s ability to adhere to clinic schedules, and ability to adhere to medication without involvement of a caregiver. Experience of violence (physical, sexual, and emotional) was assessed using three questions derived from the WHO Violence Against Women Instrument [54]. Questions were gender-neutral and asked about ever, and recently (last 6 months) having experienced physical, emotional or sexual violence, with examples provided for each type of violence.
Definition of Key Variables
We dichotomized the HIV stigma and the HIV stigma types variables as follows: overall stigma—answering ‘strongly agree’ or ‘agree’ to any of 10 questions among those who answered all the 10 questions for overall and for the subset of questions for the specific stigma type. The binary variables were utilized to describe the prevalence of HIV stigma and the different stigma types and compare the same with prior studies, while the mean scores represented the severity/level of the experience of stigma. We defined mode of HIV infection as vertical if the ART start date was < 15 years of age, and behavioral if ≥ 15 years. For those with missing ART start date information, we classified those who knew their HIV status before age 15 years in the vertical category and at or after age 15 in the behavioral category [55]. We included those previously married (divorced/widowed) and those currently married or cohabiting or in a relationship in the marriage variable as ‘ever married’. The school enrollment variable was dichotomized into (a) those who were still in school (primary or secondary) or had completed secondary school, and (b) those who had dropped out of primary or secondary school and were currently out of school. The point of care in the facility was either (a) adolescent/pediatric clinic, (b) adult or general clinic, or (c) PMTCT clinic. No independence in care was defined as requiring caregiver support in clinic attendance and medication adherence, full independence was if support was not required for either, while partial independence was if either was required. The three categories for experiencing any violence (physical/sexual/emotional) were no violence, past violence (experienced but not in the last 6 months) and recent violence (experienced in the last 6 months). Sexual relationships were categorized as never, previously, and current.
Ethical Considerations
The DiSC study was approved by the Maseno University Ethics Review Committee (MUERC/00642/18), and the University of Washington Institutional Review Board (#STUDY00005767). Participants ≥ 18 years and emancipated minors (< 18 years) provided informed written consent at the time of recruitment. We received a waiver allowing AYWHIV ages 15–17 attending clinic alone to self-consent. Caregivers for the other minors provided parental consent with the minors providing assent.
Statistical Analysis
We summarized the sociodemographic and HIV-related characteristics, and other measures using counts, proportions, median and interquartile range (IQR) as appropriate, and calculated mean (standard deviation [SD]) overall stigma across the variable categories. We reported the mean (SD) and prevalence of overall HIV stigma and the four stigma types, and described the co-occurrence of different HIV stigma types across individuals.
We estimated the association between overall HIV stigma and sociodemographic, HIV-related characteristics and other measures. Guided by the multilevel stigma model [27], we included modifiable factors at the interpersonal level (example: sexual relationships, experience of violence, self-disclosure and being in a support group) and institutional levels (example: type of clinic, school). Overall stigma (outcome) was included in the generalized linear models (family = ‘gaussian’) as a continuous variable. The continuous variable was preferred over the binary variable to allow interpretation of results as factors being associated with higher or lower levels of stigma, rather than the absolute states of ´having stigma´ or `not having stigma`. We reported mean differences (MD) from bivariate analyses, and adjusted mean differences (aMD) after adjusting for age and gender. Previous literature demonstrated intersectionality between HIV stigma and age, and gender [15]. Similar analyses were conducted to estimate the associations between the four HIV stigma types and the factors in the overall stigma models with a significant association in the bivariate analyses. Lastly, we conducted stratified analyses to determine whether the associations between overall HIV stigma and the selected factors were different across age groups (15–19 years and 20–24 years). The 95% confidence intervals (95% CI) for the mean differences and p values (p) were computed using bootstrapping to account for clustering of participants by facility. Power calculations were done with the assumption of a sample size of ~ 1000 AYWHIV and a standard deviation of 10 for the overall HIV stigma score. We had > 80% power to detect a mean difference in overall stigma levels of 5 (out of a maximum possible score of 40) between groups for factors with a prevalence of 3%, and mean difference of 2 between groups for factors with a prevalence of 50%. All analyses were completed using R studio (R Foundation for Statistical Computing, Vienna, Austria).
Results
Description of the Study Population
Of 1,011 AYWHIV included in this analysis, 701 (69%) were female with a median age of 18 years (interquartile range [IQR]: 16–21). The majority 534 (57%) knew their HIV status before they were 15 years old and 564 (58%) were classified as having acquired HIV vertically. Fifty-nine percent received care at the adolescent/pediatric clinic, 31% at the adult or general HIV clinic, and 10% at the PMTCT clinic. Overall, 405 (40%) were in a support group. The majority (52%) of those in adolescent/pediatric clinics, 28% of those in adult/general clinics and 10% of those in PMTCT clinics were in a support group; 920 (92%) were independent in care. Majority of AYWHIV, 647 (64%) had ever had sex, and 328 (51%) of those with a sexual partner had disclosed their status to their partner. Further, 280 (27%) had experienced physical violence, 178 (18%) emotional violence, and 68 (7%) sexual violence. The median social support score (range 10–60) was 43 (IQR 38–48), while the median resilience score (range 2–10) was 8 (IQR 6–9) (Table 1).
Table 1.
Characteristics of adolescents and youth living with HIV
| Factor | N | Overall n (%) |
Mean (SD) HIV stigma score |
|---|---|---|---|
| Age (years) | 1011 | ||
| 15–19 | 597 (59) | 24 (6.6) | |
| 20–24 | 414 (41) | 27 (7.2) | |
| Gender | 1011 | ||
| Female | 701 (69) | 26 (7.0) | |
| Male | 310 (31) | 24 (6.9) | |
| School enrollment | 1005 | ||
| In school | 607 (60) | 24 (6.5) | |
| Completed secondary | 180 (18) | 26 (6.7) | |
| Dropped out of school | 218 (22) | 28 (7.6) | |
| In boarding school (Those in school) | 603 | ||
| No | 443 (73) | 24 (6.1) | |
| Yes | 160 (27) | 25 (7.4) | |
| Relationship status | 992 | ||
| Never married | 681 (69) | 25 (6.7) | |
| aEver married | 311 (31) | 27 (7.2) | |
| Point of care | 1005 | ||
| Adolescent/pediatric clinic | 595 (59) | 24 (6.5) | |
| General/adult clinic | 311 (31) | 27 (7) | |
| Maternal and Child Health Clinic | 99 (10) | 26 (7.6) | |
| Process of learning HIV status | 989 | ||
| Told by parent/provider/others | 424 (43) | 24 (6.6) | |
| Underwent HIV testing | 565 (57) | 26 (7.1) | |
| Perception of mode of HIV infection | 990 | ||
| Vertical | 441 (44) | 24 (6.9) | |
| Sexual | 217 (22) | 28 (7.3) | |
| Other | 77 (8) | 25 (7.6) | |
| Don’t know | 255 (26) | 25 (6.1) | |
| Age at knowing HIV status (years) | 929 | ||
| < 15 | 534 (57) | 24 (6.8) | |
| ≥ 15 | 395 (43) | 27 (7.0) | |
| Mode of HIV infection | 969 | ||
| Vertical | 564 (58) | 24 (6.9) | |
| Behavioral | 405 (42) | 26 (6.9) | |
| In a peer support group | 1003 | ||
| No | 598 (60) | 26 (6.9) | |
| Yes | 405 (40) | 24 (7.0) | |
| Independent in care | 1002 | ||
| No | 15 (1) | 24 (8.3) | |
| *Partial | 67 (7) | 23 (5.7) | |
| Full | 920 (92) | 25 (7) | |
| Ever experienced physical violence | 1011 | ||
| No | 731 (72) | 25 (6.8) | |
| Yes (but not in last 6 months) | 146 (14) | 27 (7.5) | |
| Yes (including last 6 months) | 134 (13) | 27 (6.6) | |
| Ever experienced emotional violence | 1011 | ||
| No | 833 (82) | 25 (6.6) | |
| Yes (but not in last 6 months) | 83 (8) | 27 (8) | |
| Yes (including last 6 months) | 95 (10) | 29 (7.1) | |
| Ever experienced sexual violence | 1011 | ||
| No | 943 (93) | 25 (6.8) | |
| Yes (but not in last 6 months) | 42 (4) | 27 (8.8) | |
| Yes (including last 6 months) | 26 (3) | 30 (7.1) | |
| Ever had sex | |||
| No | 1011 | 364 (36) | 23 (6.1) |
| Yes | 647 (64) | 26 (7.1) | |
| Self-disclosed to family members | 1005 | ||
| No | 467 (46) | 25 (7.2) | |
| Yes | 538 (54) | 26 (6.7) | |
| Self-disclosed to sexual partner | 646 | ||
| No | 318 (49) | 26 (7.1) | |
| Yes | 328 (51) | 27 (7.0) | |
| Self-disclosed to others | 1005 | ||
| No | 840 (84) | 25 (7.0) | |
| Yes | 165 (16) | 25 (7.0) |
Severity and Prevalence of Overall, Experienced, Internalized, Perceived Community Stigma and Disclosure Concerns
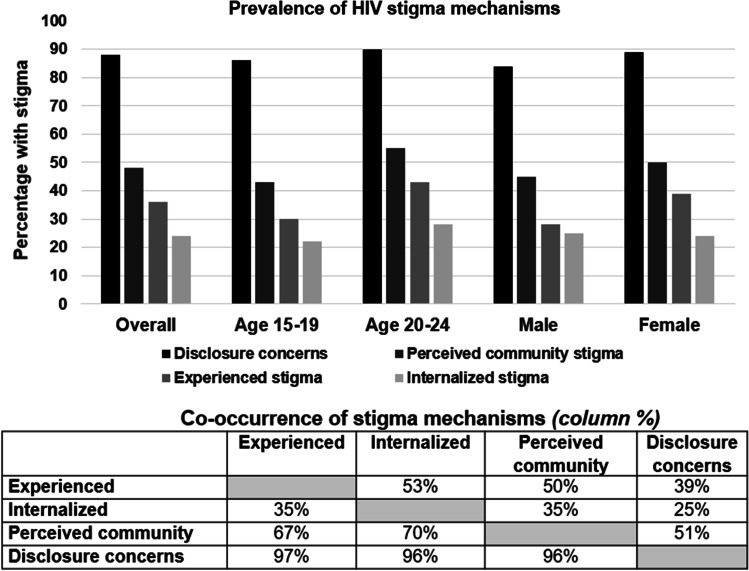
The overall stigma score was normally distributed with a median of 25 (IQR 21–29) and mean 25 (SD: 7), range 10–50. The mean scores for the stigma types were: experienced stigma 7 (SD: 2.7), range 3–15; internalized stigma 6 (SD: 2.6), range 3–15, perceived community stigma 5 (SD: 2.4), range 2–10, disclosure concerns 7 (SD: 2.0), range 2–10. Of 890 AYWHIV with an overall stigma score (all stigma questions answered), 817 (92%) had any stigma; 350 (36%) had experienced stigma, 241 (24%) had internalized stigma, 478 (48%) had perceived community stigma, and 871 (88%) had disclosure concerns. Of the 871 with disclosure concerns, 819 (94%) reported being careful about who they tell their HIV status, while 489 (56%) reported worrying about those who know their status telling others. Only 83 (9%) had all four stigma types. There was high co-occurrence of all stigma types with the lowest being the proportion of AYWHIV with disclosure concerns who also had internalized stigma (25%), and the highest being the proportion of AYWHIV with experienced stigma who also had disclosure concerns (97%). Female and older youth (20–24 years) had higher prevalence of all four HIV stigma types (Fig. 2).
Fig. 2.
Co-occurrence of HIV stigma types and the prevalence by age and gender
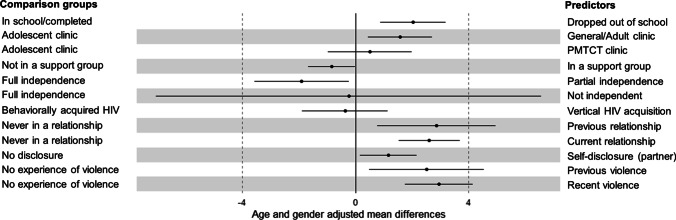
Predictors of Overall HIV Stigma (Fig. 3)
Fig. 3.
Predictors of HIV stigma among adolescents and youth with HIV
Institutional-level factors associated with overall HIV stigma were the clinic type and school enrollment status. Compared to AYWHIV attending adolescent/pediatric clinics, those in general/adult clinics had a higher mean stigma level (aMD: 1.58 [0.13–3.04], p = 0.042). Only 4% of the mean difference in stigma levels between those in adolescent and general/adult clinics was explained by being in a support group. AYWHIV who had dropped out of school reported higher stigma levels compared to those who had completed or were still in school (aMD: 2.04 [0.44–3.64], 0.027) (Table 2).
Table 2.
Correlates of HIV stigma from multivariate analysis (adjusted for age and gender)
| Factor | Age and gender adjusted mean difference (95% confidence interval), p value | ||||
|---|---|---|---|---|---|
| Overall stigma | Experienced stigma | Internalized stigma | Perceived community stigma | Disclosure concerns | |
| School enrollment | |||||
| In school/completed | Reference | Reference | Reference | Reference | Reference |
| Dropped out | 2.04 (0.44 to 3.64), 0.027 | 0.23 (− 0.25 to 0.71), 0.226 | 0.76 (0.02 to 1.50), 0.049 | 0.51 (− 0.11 to 1.13), 0.094 | 0.31 (− 0.19 to 0.82), 0.196 |
| Point of care | |||||
| Adolescent clinic | Reference | Reference | Reference | Reference | Reference |
| General/adult clinic | 1.58 (0.13 to 3.04), 0.042 | 0.21 (− 0.22 to 0.64), 0.286 | 0.78 (0.09 to 1.47), 0.033 | 0.17 (− 0.25 to 0.60), 0.328 | 0.25 (− 0.35 to 0.85), 0.253 |
| Maternal and child health clinic | 0.51 (− 1.86 to 2.88), 0.513 | − 0.10 (− 0.51 to 0.32), 0.610 | 0.53 (− 0.11 to 1.16), 0.080 | − 0.26 (− 1.58 to 1.05), 0.669 | 0.18 (− 1.06 to 0.21), 0.759 |
| In a peer support group | |||||
| No | Reference | Reference | Reference | Reference | Reference |
| Yes | − 0.84 (− 2.06 to 0.39), 0.126 | 0.04 (− 0.32 to 0.39), 0.797 | − 0.58 (− 1.29 to 0.11), 0.071 | − 0.16 (− 0.33 to 0.01), 0.059 | 0.03 (− 0.35 to 0.41), 0.812 |
| Independence in care | |||||
| Full | Reference | Reference | Reference | Reference | Reference |
| Partial | − 1.90 (− 4.10 to 0.31), 0.07 | − 0.04 (− 0.99 to 0.90), 0.920 | − 0.82 (− 1.55-[− 0.10]), 0.029 | − 0.52 (− 1.52 to 0.47), 0.112 | − 0.39 (− 1.29 to 0.51), 0.340 |
| Not independent | − 0.24 (− 18.82 to 18.34), 0.950 | 1.16 (− 4.83 to 7.15), 0.462 | 0.06 (− 2.16 to 2.27), 0.949 | − 0.14 (− 4.01 to 3.72), 0.869 | − 1.09 (− 8.39 to 6.21), 0.469 |
| Mode of HIV infection | |||||
| Vertical | Reference | Reference | Reference | Reference | Reference |
| Behavioral | 0.37 (− 2.94 to 3.67), 0.642 | 0.04 (− 0.76 to 0.84), 0.883 | 0.21 (− 0.76 to 1.18), 0.515 | − 0.02 (− 0.42 to 0.367), 0.901 | 0.11 (− 0.92 to 1.14), 0.644 |
| Sexual relationships | |||||
| None | Reference | Reference | Reference | Reference | Reference |
| Yes but not currently | 2.87 (0.10 to 5.65), 0.048 | 1.14 (0.39 to 1.90), 0.005 | 0.42 (− 0.39 to 1.23), 0.275 | 0.47 (− 0.41 to 1.34), 0.200 | 0.31 (− 0.51 to 1.14), 0.321 |
| Currently in a relationship | 2.61 (1.28 to 3.93), 0.001 | 1.02 (0.44 to 1.61), 0.009 | 0.28 (− 0.32 to 0.87), 0.295 | 0.38 (− 0.25 to 1.02), 0.129 | 0.50 (0.06 to 0.94), 0.034 |
| Self-disclosed to sexual partner | |||||
| No | Reference | Reference | Reference | Reference | Reference |
| Yes | 1.16 (− 0.27 to 2.59), 0.070 | 0.40 (− 0.13 to 0.93), 0.124 | 0.23 (− 0.35 to 0.81), 0.397 | 0.22 (− 0.21 to 0.66), 0.176 | 0.23 (− 0.30 to 0.76), 0.293 |
| Ever experienced violence (physical/emotional/sexual) | |||||
| No | Reference | Reference | Reference | Reference | Reference |
| Yes (but not in last 6 months) | 2.51 (− 0.12 − 5.13), 0.058 | 0.89 (0.04 to 1.75), 0.046 | 0.60 (0 to 1.21), 0.056 | 0.66 (0.24 to 1.08), 0.008 | 0.43 (− 0.24 to 1.09), 0.177 |
| Yes (including last 6 months) | 2.91 (1.38 to 4.44), 0.002 | 0.81 (0.26 to 1.36), 0.013 | 0.65 (0.26 to 1.05), 0.014 | 1.13 (0.49 to 1.77), 0.010 | 0.46 (− 0.05 to 0.97), 0.073 |
Bolded and black font color: Significant association between factor and overall HIV stigma/stigma type
Bolded and gray font color: Association between factor and overall HIV stigma/stigma type has a trend towards significance (0.1 < p > 0.05)
A positive mean difference means that the participants reporting the specified factor had a higher mean stigma score compared to the participants in the reference group
Interpersonal-level factors associated with overall HIV stigma were being in a sexual relationship, self-disclosure to a sexual partner, experiencing violence, and independence in care. Those who had a past sexual relationship (aMD: 2.87 [0.10–5.65], p = 0.048) or were in a current relationship (aMD: 2.61 [1.28–3.93], p = 0.001) had higher stigma levels compared to those who have never been in one. AYWHIV who had ever self-disclosed to a sexual partner tended to have higher stigma levels (aMD: 1.16 [− 0.27 to 2.59], p = 0.07). Those who had experienced past violence (aMD: 2.51 [− 0.12 to 5.13], p = 0.058) and recent violence (aMD: 2.91 [1.38–4.44], p = 0.002) also had higher stigma levels compared to those with no experience of violence. There was a trend towards significance in the analysis for independence in care. Compared to AYWHIV without any caregiver involvement in their HIV care (fully independent), those with some involvement (partial independence) had lower mean stigma levels (aMD: − 1.90 [− 4.10 to 0.31], p = 0.07) (Table 2). Social support was not associated with HIV stigma (Supplementary Table 1).
Individual-level factors assessed included mode of HIV acquisition, process of learning ones HIV status, age of knowing their HIV status and resilience. Unlike resilience, the first three had an association with HIV stigma on bivariate analysis but not after adjusting for age and gender (Supplementary table 1).
In the age-stratified analysis, the factors that were associated with overall stigma for those ages 20–24 years were being in the adult/general clinic (aMD: 3.05 [1.01–5.10], p = 0.012), dropping out of school (aMD: 2.00 [0.20–3.81], 0.043), having partial independence (aMD: − 3.49 [− 6.78 to (− 0.20)], p = 0.041), and experiencing recent violence (aMD: 3.45 [1.27–5.62], p = 0.008). For those 15–19 years, cofactors were being in a sexual relationship in the past (aMD: 2.64 [0.02–5.26], p = 0.048) and currently (aMD: 2.71 [1.20–4.22], p = 0.005). There was a trend towards significance for those who experienced recent violence (aMD: 2.42 [− 0.53 to 5.62], p = 0.083) and dropping out of school (aMD: 2.33 [− 0.20 to 4.85], 0.060). While not significant, those receiving care at PMTCT (aMD: 2.05 [− 1.94 to 6.04], p = 0.265) and those who had self-disclosed to a sexual partner (aMD: 1.93 [− 0.64 to 4.51], p = 0.104) had higher stigma levels (Supplementary Table 1).
Predictors of Stigma Types
Factors that were associated with experienced stigma were being in a sexual relationship in the past (aMD: 1.14 [0.39–1.90], p = 0.005) and currently (aMD: 1.02 [0.44–1.61], p = 0.009), and experiencing violence in the past (aMD: 0.89 [0.04–1.75], p = 0.046) and recently (aMD: 0.81 [0.26–1.36], p = 0.013). Dropping out of school (aMD: 0.76 [0.02–1.50], 0.049), being served in the adult/general clinic (aMD: 0.78 [0.09–1.47], p = 0.033), partial independence (aMD: − 0.82 [− 1.55 to (− 0.10)], p = 0.029), and experiencing violence recently (aMD: 0.65 [0.26–1.05], p = 0.014) were associated with internalized stigma. There was a trend towards significance for the association between internalized stigma and experiencing violence in the past (aMD: 0.60 [0–1.21], p = 0.056) and being in a support group (aMD: − 0.58 [− 1.29 to 0.11], p = 0.071). Experiencing violence in the past (aMD: 0.66 [0.24–1.08], p = 0.008), and recently (aMD: 1.13 [0.49–1.77], p = 0.010) were associated with perceived community stigma. The association between being in a support group and perceived community stigma trended towards significance (aMD: − 0.16 [− 0.33 to 0.01], p = 0.059). Factors associated with disclosure concerns were being in a current sexual relationship (aMD: 0.50 [0.06–0.94], p = 0.034), with a trend to significance for recent experience of violence (aMD: 0.46 [− 0.05 to 0.97], p = 0.073) (Table 2). Results of the bivariate analysis for all factors and the four stigma types are in supplementary Table 2.
Discussion
Nearly all youth included in this study reported at least one form of stigma. Disclosure concerns were the most prevalent while a quarter of the youth reported internalized stigma, and about 10% reported experience of all four stigma types. School attendance and clinic type were institutional level factors associated with HIV stigma, while interpersonal level factors included independence in care (involvement of a caregiver in care), sexual relationships, self-disclosure to a sexual partner, and experiencing violence. The health stigma and discrimination framework proposes relationships between HIV stigma types and health/behavioral/interpersonal outcomes. In this study, we shift the focus more proximally to identify modifiable multilevel factors that either cause or co-occur with specific HIV stigma types, and therefore are important to include in the anti-stigma interventions.
A variety of stigma scales and approaches to computation of scores have been used in the literature, making comparisons of prevalence or levels of HIV stigma across studies and populations challenging [49, 56–60]. Previous studies in settings similar to ours have reported higher prevalence of internalized stigma and experienced stigma, with a mixed picture for anticipated stigma among AYWHIV [39, 60, 61]. While a few other studies reported lower prevalence of internalized and experienced stigma [62], it is clear that there is a significant stigma burden among youth with HIV. In our study, older age was associated with higher stigma levels, consistent with higher levels of stigma observed in adult studies [59, 63, 64]. The marginalizing experiences by PLHIV likely stack up across the life span. Except for the much higher prevalence of anticipated stigma or more broadly associated disclosure concerns, as we have described in details in this paper, previous studieswith adults too reported higher prevalence of experienced and internalized stigma levels [58, 65–68]. Overall, our data suggest a need to incorporate interventions to reduce stigma in multiple setting especially clinics and communities.
The multi-level manifestation of HIV stigma where structural, institutional, community, interpersonal and intrapersonal factors contribute to its propagation is fairly well understood [27]. However, to develop effective interventions and policies that reduce stigma and mitigate its effects, we need to contextualize these factors across the different population groups and regions. In our study, we highlight the influence of clinic type. While some clinics serve their youth in separate spaces or days, others serve them together with adults [69]. We found significantly lower stigma levels among youth attending adolescent clinics. Youth have previously reported their discomfort with attending HIV clinics with adults. The reactions include shame of being seen by older members of their communities in the HIV clinics, expectation of being looked down upon, ambivalence and complex emotions around the chronicity of the illness seen as one sees older unwell/disease afflicted individuals, expectation not to be understood by providers in the adult clinics among others [70, 71]. From this study, we could infer that these activate pathways for HIV stigma, especially internalized stigma. These challenges informed the roll-out of youth responsive clinics in region [72–74]. Providers in these clinics were also trained on provision of youth friendly services [75, 76].
On the other hand, pregnant or parenting adolescent girls and young women with HIV served in PMTCT clinics reported high stigma levels. Though we did not have power to detect statistically significant differences with those in the adolescent clinics, it is possible that the associations are from a combination of the entrenched stigmatization, unmet socioemotional needs around unplanned, early pregnancy, their HIV status, how and what services are offered or not in these PMTCT clinics. Unlike youth who were served in general/adult and PMTCT clinics, majority of those in adolescent clinics had joined support groups. Though being in a support group only marginally explained the differences in HIV stigma between those in adolescent and general/adult clinics, the support groups by themselves could be important interventions to reduce stigma. Being in a support group was associated with lower internalized stigma and disclosure concerns. The support groups likely prepare the adolescents and youth to counter some stigmatizing situations and bolster their confidence and sense of self-worth leveraging peer support. Expanding the reach of youth responsive clinics and peer support groups, which are highly advocated for to enhance HIV treatment outcomes [77–79], could be effective ways to mitigate internalized stigma for youth.
HIV stigma manifests in the interpersonal relationships youth are involved in. We found that youth who had ever been in sexual relationships, and especially if they were currently in one, reported higher experienced stigma. Likely due to their lived experiences, including the need for disclosure to their partners, they also had higher levels of disclosure concerns. Development of relationships is a key part of development during adolescence and young adulthood [80, 81]. Ensuring that these relationships are healthy is a challenge especially for adolescents [82], which is worsened by mixed messaging around the need for partnerships for support and the equally important message for them to delay sexual debut [6, 83, 84]. For AYWHIV, the complexity is heightened by disclosure of their HIV status, which may lead to emotional and physical intimate partner violence and rejection [8–10]. Violence however does not only affect those in sexual relationships. Youth with HIV in general are disproportionately affected by physical, emotional and sexual violence, which negatively affects their mental health and treatment adherence [85–89]. We found a relationship between lived experience of interpersonal violence and HIV stigma through all types. It is highly likely that HIV stigma is one of the main pathways through which violence impacts treatment outcomes for AYWHIV. Interventions focused on mitigating the impact of HIV stigma and eventually improving treatment outcomes would be strengthened by the inclusion of measures to address violence against AYWHIV.
We assessed the role of caregivers in the HIV care for AYWHIV. We found that youth whose caregivers were involved in their care- especially in clinic attendance (partially or not independent), had lower levels of internalized stigma independent of their age. Interestingly, the association was stronger for the older age group (20–24 years), which counter-intuitively may support the continued involvement of caregivers into early adulthood of their youth with HIV. It was also worth noting that self-disclosure to family was not associated with higher stigma levels unlike disclosure to partners, a trend highlighted in previous literature [11]. In summary, these results support increased involvement of caregivers in the HIV care for adolescents and youth, including into their early adulthood, which has been shown to improve their treatment outcomes [90].
It is plausible that dropping out of school may heighten internalization of stigma by cutting these youth from sources of support, information and oversight of key individuals like teachers, social workers and peers. In this case, supporting AYWHIV to remain in school could be an important structural and institutional anti-stigma intervention. The reverse interpretation, that HIV stigma may result in AYWHIV dropping out of school suggests that the support for the AYWHIV to remain in school should include measures that mitigate the impact of HIV stigma in the school environment. Measures already tested in our setting include increasing HIV literacy among school staff, specific HIV treatment support measures in school like confidential treatment storage, linkages between schools and health facilities and psychosocial support [47].
A strength of this analysis is that the study population resembled the population of youth with HIV in care in Kenya with majority being female, having acquired HIV vertically, being in school, and already debuted sexual relationships. The large sample size, collection of a wide range of variables, basing the analysis on an established theoretical framework, and using validated scales for key measures including the HIV stigma scale validated for AYWHIV are strengths of this study. Understanding of stigma and risk factors associated with HIV disclosure in AYWHIV can easily be neglected in rural contexts and our study contributes to evidence in that regard. However, all the participants are from Western Kenya, a region with a high HIV prevalence, largely rural, and a relatively homogenous cultural context, which limits generalizability of the results. The data was also collected only at the individual level, and with very few ecological units (9 clinics) missing key institutional and structural factors that would have facilitated an improved multilevel analysis. The cross-sectional design of this study is a key limitation that makes it challenging to explain the direction of associations. The interpretation of results for disclosure concerns which in part represent anticipated stigma is also limited due to the very low internal consistency of the measurements (α = 0.44). More work is required to develop a more reliable scale assessing anticipated stigma.
Conclusion
This exploratory analysis leverages the health stigma and discrimination framework to demonstrate relationships between HIV stigma and potential predictors. This study added proximal factors to the existing framework and assessed their relationships with the stigma types. The identified institutional, interpersonal and individual level assessed influence the experience, internalization, anticipation of stigma and perception of their communities differently. While violence towards adolescents and youth with HIV had an effect on all four HIV stigma types, being in sexual relationships largely influenced their experience and anticipation of stigma. On the other hand, school enrollment, caregiver involvement, being in a support group and clinic type influenced their internalization of HIV stigma. These factors could be considered among other structural factors when developing anti-stigma interventions.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We wish to thank the study participants and clinic staff from the nine facilities in Western Kenya we conducted this study. We also appreciate the study staff who worked to meticulously complete data collection despite the challenges of the COVID-19 pandemic.
Author Contributions
PK, GJ-S and KO contributed to the study conception and design, and obtained funding; Cyrus Mugo conducted the analyses and drafted the manuscript; All authors reviewed and revised drafts of the manuscript, read and approved the final manuscript.
Funding
The Data-Informed Stepped Care (DiSC) was funded by the National Institutes of Health (UG3 HD096906). Cyrus Mugo was supported by D43TW009783 and D43TW009345 (Fogarty International Center). This publication was also supported by the UW Global Center for Integrated Health of Women, Adolescents and Children (Global WACh). The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The funding sources were not involved in the analyses or interpretation of data. None of the authors was paid to write this article by a pharmaceutical company or other agency.
Data Availability
The data that support the findings of this study are available from the Principal Investigators of the DiSC study upon a reasonable request to the corresponding author.
Declarations
Competing Interests
The authors declare that they have no conflicts of interest.
Ethical Approval
The DiSC study was approved by the Maseno University Ethics Review Committee (MUERC/00642/18), and the University of Washington Institutional Review Board (#STUDY00005767). The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent to Participate
Participants ≥ 18 years and emancipated minors (< 18 years) provided informed written consent at the time of recruitment. We received a waiver allowing AYWHIV ages 15–17 attending clinic alone to self-consent. Caregivers for the other minors provided parental consent with the minors providing assent.
Consent for Publication
We do not include any individual identifying information in this manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Kawango Agot and Grace C. John-Stewart are joint last author.
References
- 1.Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. Am J Public Health. 2017;107(6):863–869. doi: 10.2105/AJPH.2017.303744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Placek CD, Nishimura H, Hudanick N, Stephens D, Madhivanan P. Reframing HIV stigma and fear: considerations from social-ecological and evolutionary theories of reproduction. Hum Nat. 2019;30(1):1–22. doi: 10.1007/s12110-018-09335-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Turan B, Budhwani H, Fazeli PL, Browning WR, Raper JL, Mugavero MJ, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav. 2017;21(1):283–291. doi: 10.1007/s10461-016-1451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16:18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Desta AA, Woldearegay TW, Futwi N, Gebrehiwot GT, Gebru GG, Berhe AA, et al. HIV virological non-suppression and factors associated with non-suppression among adolescents and adults on antiretroviral therapy in northern Ethiopia: a retrospective study. BMC Infect Dis. 2020;20(1):4. doi: 10.1186/s12879-019-4732-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.La Greca AM, Harrison HM. Adolescent peer relations, friendships, and romantic relationships: do they predict social anxiety and depression? J Clin Child Adolesc Psychol. 2005;34(1):49–61. doi: 10.1207/s15374424jccp3401_5. [DOI] [PubMed] [Google Scholar]
- 7.Roach A. Supportive peer relationships and mental health in adolescence: an integrative review. Issues Ment Health Nurs. 2018;39(9):723–737. doi: 10.1080/01612840.2018.1496498. [DOI] [PubMed] [Google Scholar]
- 8.Madiba S, Mokgatle M. Perceptions and experiences about self-disclosure of HIV status among adolescents with perinatal acquired HIV in poor-resourced communities in South Africa. AIDS Res Treat. 2016;2016:1–10. doi: 10.1155/2016/2607249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nostlinger C, Bakeera-Kitaka S, Buyze J, Loos J, Buve A. Factors influencing social self-disclosure among adolescents living with HIV in Eastern Africa. AIDS Care. 2015;27(Suppl 1):36–46. doi: 10.1080/09540121.2015.1051501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hogwood J, Campbell T, Butler S. I wish I could tell you but I can’t: adolescents with perinatally acquired HIV and their dilemmas around self-disclosure. Clin Child Psychol Psychiatry. 2013;18(1):44–60. doi: 10.1177/1359104511433195. [DOI] [PubMed] [Google Scholar]
- 11.Gabbidon K, Chenneville T, Peless T, Sheared-Evans S. Self-disclosure of HIV status among youth living with HIV: a global systematic review. AIDS Behav. 2019;24:1–28. doi: 10.1007/s10461-019-02478-9. [DOI] [PubMed] [Google Scholar]
- 12.Li L, Lin C, Feng N, Nguyen DB, Cao W, Le AT, et al. Stigma related to HIV and drug use: layers, types, and relations to mental health. AIDS Behav. 2020;24(8):2347–2354. doi: 10.1007/s10461-020-02794-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am Psychol. 2013;68(4):225–236. doi: 10.1037/a0032705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsang EY, Qiao S, Wilkinson JS, Fung AL, Lipeleke F, Li X. Multilayered stigma and vulnerabilities for HIV infection and transmission: a qualitative study on male sex workers in Zimbabwe. Am J Mens Health. 2019;13(1):1557988318823883. doi: 10.1177/1557988318823883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jackson-Best F, Edwards N. Stigma and intersectionality: a systematic review of systematic reviews across HIV/AIDS, mental illness, and physical disability. BMC Public Health. 2018;18(1):919. doi: 10.1186/s12889-018-5861-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nobre N, Pereira M, Roine RP, Sutinen J, Sintonen H. HIV-related self-stigma and health-related quality of life of people living with HIV in Finland. J Assoc Nurses AIDS Care. 2018;29(2):254–265. doi: 10.1016/j.jana.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 17.Crockett KB, Kalichman SC, Kalichman MO, Cruess DG, Katner HP. Experiences of HIV-related discrimination and consequences for internalised stigma, depression and alcohol use. Psychol Health. 2019;34(7):796–810. doi: 10.1080/08870446.2019.1572143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stangl AL, Earnshaw VA, Logie CH, van Brakel W, Barré I, et al. The Health Stigma and Discrimination Framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17:31. doi: 10.1186/s12916-019-1271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chambers LA, Rueda S, Baker DN, Wilson MG, Deutsch R, Raeifar E, et al. Stigma, HIV and health: a qualitative synthesis. BMC Public Health. 2015;15:848. doi: 10.1186/s12889-015-2197-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Breet E, Kagee A, Seedat S. HIV-related stigma and symptoms of post-traumatic stress disorder and depression in HIV-infected individuals: does social support play a mediating or moderating role? AIDS Care. 2014;26(8):947–951. doi: 10.1080/09540121.2014.901486. [DOI] [PubMed] [Google Scholar]
- 21.Li J, Mo PK, Wu AM, Lau JT. Roles of self-stigma, social support, and positive and negative affects as determinants of depressive symptoms among HIV infected men who have sex with men in China. AIDS Behav. 2017;21(1):261–273. doi: 10.1007/s10461-016-1321-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Logie CH, Wang Y, Lacombe-Duncan A, Wagner AC, Kaida A, Conway T, et al. HIV-related stigma, racial discrimination, and gender discrimination: pathways to physical and mental health-related quality of life among a national cohort of women living with HIV. Prev Med. 2018;107:36–44. doi: 10.1016/j.ypmed.2017.12.018. [DOI] [PubMed] [Google Scholar]
- 23.Earnshaw VA, Kidman RC, Violari A. Stigma, depression, and substance use problems among perinatally HIV-infected youth in South Africa. AIDS Behav. 2018;22(12):3892–3896. doi: 10.1007/s10461-018-2201-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kemp CG, Lipira L, Huh D, Nevin PE, Turan JM, Simoni JM, et al. HIV stigma and viral load among African-American women receiving treatment for HIV. AIDS. 2019;33(9):1511–1519. doi: 10.1097/QAD.0000000000002212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van der Kooij YL, Kupková A, den Daas C, van den Berk GEL, Kleene MJT, Jansen HSE, et al. Role of self-stigma in pathways from HIV-related stigma to quality of life among people living with HIV. AIDS Patient Care STDS. 2021;35(6):231–238. doi: 10.1089/apc.2020.0236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andersson GZ, Reinius M, Eriksson LE, Svedhem V, Esfahani FM, Deuba K, et al. Stigma reduction interventions in people living with HIV to improve health-related quality of life. Lancet HIV. 2020;7(2):e129–e140. doi: 10.1016/S2352-3018(19)30343-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rao D, Elshafei A, Nguyen M, Hatzenbuehler ML, Frey S, Go VF. A systematic review of multi-level stigma interventions: state of the science and future directions. BMC Med. 2019;17(1):41. doi: 10.1186/s12916-018-1244-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pantelic M, Steinert JI, Park J, Mellors S, Murau F. 'Management of a spoiled identity': systematic review of interventions to address self-stigma among people living with and affected by HIV. BMJ Glob Health. 2019;4:e001285. doi: 10.1136/bmjgh-2018-001285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sengupta S, Banks B, Jonas D, Miles MS, Smith GC. HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav. 2011;15(6):1075–1087. doi: 10.1007/s10461-010-9847-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: what have we learned? AIDS Educ Prev. 2003;15(1):49–69. doi: 10.1521/aeap.15.1.49.23844. [DOI] [PubMed] [Google Scholar]
- 31.Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11(3):353–363. doi: 10.1080/13548500600595327. [DOI] [PubMed] [Google Scholar]
- 32.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. 2013;16(3 Suppl 2):18734. doi: 10.7448/IAS.16.3.18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mak WWS, Mo PKH, Ma GYK, Lam MYY. Meta-analysis and systematic review of studies on the effectiveness of HIV stigma reduction programs. Soc Sci Med. 2017;188:30–40. doi: 10.1016/j.socscimed.2017.06.045. [DOI] [PubMed] [Google Scholar]
- 34.Bhana A, Mellins CA, Petersen I, Alicea S, Myeza N, Holst H, et al. The VUKA family program: piloting a family-based psychosocial intervention to promote health and mental health among HIV infected early adolescents in South Africa. AIDS Care. 2014;26(1):1–11. doi: 10.1080/09540121.2013.806770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chidrawi HC, Greeff M, Doak CM, Temane QM. HIV stigma experiences and stigmatisation before and after an intervention. Health SA. 2016;21(1):196–205. [Google Scholar]
- 36.Joint United Nations Programme on HIV/AIDS. HIV-related stigma, discrimination and human rights violations: Case studies of successful programmes. UNAIDS best practice collection) Geneva Switzerland. https://data.unaids.org/publications/irc-pub06/jc999-humrightsviol_en.pdf (2005). accessed 20 Apr 2012
- 37.Harper GW, Lemos D, Hosek SG. Stigma reduction in adolescents and young adults newly diagnosed with HIV: findings from the Project ACCEPT intervention. AIDS Patient Care STDS. 2014;28(10):543–554. doi: 10.1089/apc.2013.0331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wagner AC, Hart TA, Mohammed S, Ivanova E, Wong J, Loutfy MR. Correlates of HIV stigma in HIV-positive women. Arch Womens Ment Health. 2010;13(3):207–214. doi: 10.1007/s00737-010-0158-2. [DOI] [PubMed] [Google Scholar]
- 39.Mugo C, Seeh D, Guthrie B, Moreno M, Kumar M, John-Stewart G, et al. Association of experienced and internalized stigma with self-disclosure of HIV status by youth living with HIV. AIDS Behav. 2021;25:2084–2093. doi: 10.1007/s10461-020-03137-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pantelic M, Shenderovich Y, Cluver L, Boyes M. Predictors of internalised HIV-related stigma: a systematic review of studies in sub-Saharan Africa. Health Psychol Rev. 2015;9(4):469–490. doi: 10.1080/17437199.2014.996243. [DOI] [PubMed] [Google Scholar]
- 41.Deering KN, Logie C, Krüsi A, Ranville F, Braschel M, Duff P, et al. Prevalence and correlates of HIV stigma among women living with HIV in metro Vancouver, Canada. AIDS Behav. 2021;25(6):1688–1698. doi: 10.1007/s10461-020-03084-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dyer J, Wilson K, Badia J, Agot K, Neary J, Njuguna I, et al. The psychosocial effects of the COVID-19 pandemic on youth living with HIV in Western Kenya. AIDS Behav. 2021;25(1):68–72. doi: 10.1007/s10461-020-03005-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kenya National AIDS Control Council. Kenya HIV Estimates Report 2018 Nairobi2018 [cited 2019 November 09]. https://nacc.or.ke/wp-content/uploads/2018/11/HIV-estimates-report-Kenya-20182.pdf.
- 44.Nyandiko WM, Mwangi A, Ayaya SO, Nabakwe EC, Tenge CN, Gisore PM, et al. Characteristics of HIV-infected children seen in Western Kenya. East Afr Med J. 2009;86(8):364–373. doi: 10.4314/eamj.v86i8.54156. [DOI] [PubMed] [Google Scholar]
- 45.Perry B, Oluoch L, Agot K, Taylor J, Onyango J, Ouma L, et al. Widow cleansing and inheritance among the Luo in Kenya: the need for additional women-centred HIV prevention options. J Int AIDS Soc. 2014;17(1):19010. doi: 10.7448/IAS.17.1.19010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Akullian A, Onyango M, Klein D, Odhiambo J, Bershteyn A. Geographic coverage of male circumcision in western Kenya. Medicine (Baltimore) 2017;96(2):e5885. doi: 10.1097/MD.0000000000005885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kose J, Lenz C, Akuno J, Kiiru F, Jelagat Odionyi J, Otieno-Masaba R, et al. Supporting adolescents living with HIV within boarding schools in Kenya. PLoS ONE. 2021;16(12):e0260278. doi: 10.1371/journal.pone.0260278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wright K, Naar-King S, Lam P, Templin T, Frey M. Stigma scale revised: reliability and validity of a brief measure of stigma for HIV+ youth. J Adolesc Health. 2007;40(1):96–98. doi: 10.1016/j.jadohealth.2006.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 51.Tavakol M, Dennick R. Making sense of Cronbach's alpha. Int J Med Educ. 2011;2:53. doi: 10.5116/ijme.4dfb.8dfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ogunbajo A, Iwuagwu S, Williams R, Biello KB, Kahler CW, Sandfort TGM, et al. Validation of depressive symptoms, social support, and minority stress scales among gay, bisexual, and other men who have with men (GBMSM) in Nigeria, Africa: a mixed methods approach. BMC Public Health. 2020;20(1):1023. doi: 10.1186/s12889-020-09127-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kuiper H, van Leeuwen CCM, Stolwijk-Swüste JM, Post MWM. Measuring resilience with the Connor-Davidson Resilience Scale (CD-RISC): which version to choose? Spinal Cord. 2019;57(5):360–366. doi: 10.1038/s41393-019-0240-1. [DOI] [PubMed] [Google Scholar]
- 54.Nybergh L, Taft C, Krantz G. Psychometric properties of the WHO Violence Against Women instrument in a female population-based sample in Sweden: a cross-sectional survey. BMJ Open. 2013;3(5):e002053. doi: 10.1136/bmjopen-2012-002053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Teasdale CA, Brittain K, Zerbe A, Mellins CA, Falcao J, Couto A, et al. Characteristics of adolescents aged 15–19 years living with vertically and horizontally acquired HIV in Nampula, Mozambique. PLoS ONE. 2021;16(4):e0250218. doi: 10.1371/journal.pone.0250218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tanney MR, Naar-King S, MacDonnel K. Depression and stigma in high-risk youth living with HIV: a multi-site study. J Pediatr Health Care. 2012;26(4):300–305. doi: 10.1016/j.pedhc.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rongkavilit C, Wright K, Chen X, Naar-King S, Chuenyam T, Phanuphak P. HIV stigma, disclosure and psychosocial distress among Thai youth living with HIV. Int J STD AIDS. 2010;21(2):126–132. doi: 10.1258/ijsa.2009.008488. [DOI] [PubMed] [Google Scholar]
- 58.Onono M, Odwar T, Abuogi L, Owuor K, Helova A, Bukusi E, et al. Effects of depression, stigma and intimate partner violence on postpartum women's adherence and engagement in HIV care in Kenya. AIDS Behav. 2020;24(6):1807–1815. doi: 10.1007/s10461-019-02750-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wanjala SW, Nyongesa MK, Mwangi P, Mutua AM, Luchters S, Newton C, et al. Measurement characteristics and correlates of HIV-related stigma among adults living with HIV: a cross-sectional study from coastal Kenya. BMJ Open. 2022;12(2):e050709. doi: 10.1136/bmjopen-2021-050709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.MacLean JR, Wetherall K. The association between HIV-stigma and depressive symptoms among people living with HIV/AIDS: a systematic review of studies conducted in South Africa. J Affect Disord. 2021;287:125–137. doi: 10.1016/j.jad.2021.03.027. [DOI] [PubMed] [Google Scholar]
- 61.Denison JA, Burke VM, Miti S, Nonyane BAS, Frimpong C, Merrill KG, et al. Project YES! Youth Engaging for Success: a randomized controlled trial assessing the impact of a clinic-based peer mentoring program on viral suppression, adherence and internalized stigma among HIV-positive youth (15–24 years) in Ndola, Zambia. PLoS ONE. 2020;15(4):e0230703. doi: 10.1371/journal.pone.0230703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Perez A, Brittain K, Phillips N, Stein DJ, Zar HJ, Myer L, et al. HIV-related stigma and psychological adjustment among perinatally HIV-infected youth in Cape Town, South Africa. AIDS Behav. 2022;26(2):434–442. doi: 10.1007/s10461-021-03398-3. [DOI] [PubMed] [Google Scholar]
- 63.Moradzadeh R, Zamanian M. HIV-related stigma among people living with HIV in Iran: a cross-sectional study. J Assoc Nurses AIDS Care. 2021;32(5):610–618. doi: 10.1097/JNC.0000000000000251. [DOI] [PubMed] [Google Scholar]
- 64.Yator O, Mathai M, Albert T, Kumar M. Burden of HIV-related stigma and post-partum depression: a cross-sectional study of patients attending prevention of mother-to-child transmission clinic at Kenyatta National Hospital in Nairobi. Front Psychiatry. 2020;11:532557. doi: 10.3389/fpsyt.2020.532557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chace Dwyer S, Jain A, Liambila W, Warren CE. The role of unintended pregnancy in internalized stigma among women living with HIV in Kenya. BMC Womens Health. 2021;21(1):106. doi: 10.1186/s12905-021-01224-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Parcesepe AM, Nash D, Tymejczyk O, Reidy W, Kulkarni SG, Elul B. Gender, HIV-related stigma, and health-related quality of life among adults enrolling in HIV care in Tanzania. AIDS Behav. 2020;24(1):142–150. doi: 10.1007/s10461-019-02480-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Arinaitwe I, Amutuhaire H, Atwongyeire D, Tusingwire E, Kawungezi PC, Rukundo GZ, et al. Social support, food insecurity, and HIV stigma among men living with HIV in rural Southwestern Uganda: a cross-sectional analysis. HIV AIDS (Auckl) 2021;13:657–666. doi: 10.2147/HIV.S316174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Earnshaw VA, Bogart LM, Laurenceau JP, Chan BT, Maughan-Brown BG, Dietrich JJ, et al. Internalized HIV stigma, ART initiation and HIV-1 RNA suppression in South Africa: exploring avoidant coping as a longitudinal mediator. J Int AIDS Soc. 2018;21(10):e25198. doi: 10.1002/jia2.25198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Njuguna I, Beima-Sofie K, Mburu C, Black D, Evans Y, Guthrie B, et al. What happens at adolescent and young adult HIV clinics? A national survey of models of care, transition and disclosure practices in Kenya. Trop Med Int Health. 2020;25(5):558–565. doi: 10.1111/tmi.13374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mesic A, Halim N, MacLeod W, Haker C, Mwansa M, Biemba G. Facilitators and barriers to adherence to antiretroviral therapy and retention in care among adolescents living with HIV/AIDS in Zambia: a mixed methods study. AIDS Behav. 2019;23(9):2618–2628. doi: 10.1007/s10461-019-02533-5. [DOI] [PubMed] [Google Scholar]
- 71.Kimani D, Karanja S, Ngure K, Mwalili S. Multi-level challenges and opportunities in providing antiretroviral treatment to adolescents in Kenya. AIDS Care. 2021;33(3):364–367. doi: 10.1080/09540121.2020.1717422. [DOI] [PubMed] [Google Scholar]
- 72.Zanoni BC, Sibaya T, Cairns C, Lammert S, Haberer JE. Higher retention and viral suppression with adolescent-focused HIV clinic in South Africa. PLoS ONE. 2017 doi: 10.1371/journal.pone.0190260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Murray KR, Dulli LS, Ridgeway K, Dal Santo L, Darrow de Mora D, Olsen P, et al. Improving retention in HIV care among adolescents and adults in low- and middle-income countries: a systematic review of the literature. PLoS ONE. 2017;12(9):e0184879. doi: 10.1371/journal.pone.0184879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zanoni BC, Sibaya T, Cairns C, Haberer JE. Barriers to retention in care are overcome by adolescent-friendly services for adolescents living with HIV in South Africa: a qualitative analysis. AIDS Behav. 2019;23(4):957–965. doi: 10.1007/s10461-018-2352-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mburu M, Guze MA, Ong'wen P, Okoko N, Moghadassi M, Cohen CR, et al. Evaluating the effectiveness of the HIV adolescent package of care (APOC) training on viral load suppression in Kenya. Public Health. 2019;173:146–149. doi: 10.1016/j.puhe.2019.05.026. [DOI] [PubMed] [Google Scholar]
- 76.Okinyi HM, Wachira CM, Wilson KS, Nduati MN, Onyango AD, Mburu CW, et al. “I have actually not lost any adolescent since i started engaging them one on one:” training satisfaction and subsequent practice among health providers participating in a standardized patient actor training to improve adolescent engagement in HIV care. J Int Assoc Provid AIDS Care (JIAPAC) 2022;21:23259582221075133. doi: 10.1177/23259582221075133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Settergren SK, Philippe R, St Louis J, Segaren N, Boisson S, Lewis T, et al. Importance of support groups to the health and well-being of vulnerable children and young people living with HIV: a case study of the Kids Clubs program in Haiti. BMC Health Serv Res. 2021;21(1):236. doi: 10.1186/s12913-021-06242-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Stangl AL, Mwale M, Sebany M, Mackworth-Young CR, Chiiya C, Chonta M, et al. Feasibility, acceptability and preliminary efficacy of Tikambisane ('Let's Talk to Each Other'): a pilot support group intervention for adolescent girls living With HIV in Zambia. J Int Assoc Provid AIDS Care. 2021;20:23259582211024772. doi: 10.1177/23259582211024772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Armstrong A, Nagata JM, Vicari M, Irvine C, Cluver L, Sohn AH, et al. A global research agenda for adolescents living with HIV. J Acquir Immune Defic Syndr. 2018;78(1):S16–s21. doi: 10.1097/QAI.0000000000001744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ali MM, Merdad L, Bellizzi S. Socioeconomic variations in risky sexual behavior among adolescents in 14 sub-Saharan Africa countries who report ever having had sex. Int J Equity Health. 2021;20(1):11. doi: 10.1186/s12939-020-01352-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fortenberry JD. Puberty and adolescent sexuality. Horm Behav. 2013;64(2):280–287. doi: 10.1016/j.yhbeh.2013.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Anderson RM. Positive sexuality and its impact on overall well-being. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56(2):208–214. doi: 10.1007/s00103-012-1607-z. [DOI] [PubMed] [Google Scholar]
- 83.Konkor I, Mkandawire P, Antabe R, Luginaah I, Husbands W, Wong J, et al. Sexual debut among heterosexual men of African and Caribbean descent: are the youth initiating sex earlier than the older generation? Arch Sex Behav. 2021;50(6):2359–2369. doi: 10.1007/s10508-020-01855-z. [DOI] [PubMed] [Google Scholar]
- 84.Alabi TA, Adejoh SO, Oyefara JL. Predictors and consequences of early sexual debut among students in tertiary institutions in Lagos metropolis, Nigeria. Afr J Reprod Health. 2020;24(3):78–87. doi: 10.29063/ajrh2020/v24i3.9. [DOI] [PubMed] [Google Scholar]
- 85.Kidman R, Violari A. Dating violence against HIV-infected youth in South Africa: associations with sexual risk behavior, medication adherence, and mental health. J Acquir Immune Defic Syndr. 2018;77(1):64–71. doi: 10.1097/QAI.0000000000001569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Merrill KG, Campbell JC, Decker MR, McGready J, Burke VM, Mwansa JK, et al. Prevalence of physical and sexual violence and psychological abuse among adolescents and young adults living with HIV in Zambia. PLoS ONE. 2020;15(6):e0235203. doi: 10.1371/journal.pone.0235203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Biomndo BC, Bergmann A, Lahmann N, Atwoli L. Intimate partner violence is a barrier to antiretroviral therapy adherence among HIV-positive women: evidence from government facilities in Kenya. PLoS ONE. 2021;16(4):e0249813. doi: 10.1371/journal.pone.0249813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Merrill KG, Campbell JC, Decker MR, McGready J, Burke VM, Mwansa JK, et al. Past-year violence victimization is associated with viral load failure among HIV-positive adolescents and young adults. AIDS Behav. 2021;25(5):1373–1383. doi: 10.1007/s10461-020-02958-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kacanek D, Malee K, Mellins CA, Tassiopoulos K, Smith R, Grant M, et al. Exposure to violence and virologic and immunological outcomes among youth with perinatal HIV in the pediatric HIV/AIDS Cohort Study. J Adolesc Health. 2016;59(1):30–37. doi: 10.1016/j.jadohealth.2016.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shenderovich Y, Boyes M, Esposti MD, Casale M, Toska E, Roberts KJ, et al. Relationships with caregivers and mental health outcomes among adolescents living with HIV: a prospective cohort study in South Africa. BMC Public Health. 2021;21(1):172. doi: 10.1186/s12889-020-10147-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the Principal Investigators of the DiSC study upon a reasonable request to the corresponding author.