Abstract
Vaccination is one of the most effective strategies to control the spread of COVID-19 and reduce morbidity and mortality; however, rapid and equitable vaccine distribution is required to achieve such outcomes. We conducted a basic interrupted time-series analysis to examine the short-term impacts of a citywide vaccine equity plan, the Protect Chicago Plus (PCP) plan. We compared vaccine coverage in zip codes in Chicago with high COVID-19 vulnerability, as identified from the Chicago COVID-19 Community Vulnerability Index, with coverage in all other zip codes in Chicago. From our analysis, we observed that implementation of PCP coincided with reduced vaccination disparities between Chicago communities with low and high vulnerability indexes over time. In our analysis of vaccination coverage before program implementation, vaccination coverage climbed nearly twice as fast among non-PCP zip codes (0.19% per day) than among PCP zip codes (0.10% per day) or by 0.09 percentage points (P < .001). In model analysis after program implementation, zip codes prioritized for the program had 0.42% additional coverage per day as compared with 0.27% per day for non-PCP zip codes. Our findings suggest that such programs may improve vaccine equity, but additional research is needed to better understand the longer-term effects of citywide vaccination strategies on vaccine uptake.
Keywords: COVID-19, vaccination, interrupted time series, health equity, community vulnerability
The illness caused by SARS-CoV-2 (COVID-19) was declared a pandemic in March 2020; by May 2022, >1 million people in the United States had died of COVID-19.1,2 The disease has not affected population groups uniformly; rather, COVID-19 has disproportionately affected Black or African American people, Indigenous people, and people from other racial and ethnic minority groups, demonstrating the effects of long-standing inequities in social determinants of health, neighborhood traits, and underlying comorbidities. 3 For example, people from racial and ethnic minority groups in urban settings are often employed in service occupations that prevent work-from-home opportunities and social distancing.4,5 Identifying characteristics that are associated with increased risk of COVID-19, even if the risks are not causally related, can assist in prioritizing communities for vaccination.
Chicago recorded 244 230 positive COVID-19 cases from March 13, 2020, through May 1, 2021, resulting in 4984 deaths. 6 Despite representing 28.5% and 28.8% of the city’s total population, Black and Latinx populations represented 38.5% and 33.4% of deaths from COVID-19, respectively. 6 Two highly effective COVID-19 vaccines received Emergency Use Authorization in the United States in December 2020, and a third vaccine received Emergency Use Authorization in February 2021. 7 Because COVID-19 vaccination is one of the most effective strategies to control spread and reduce morbidity and mortality, rapid and equitable dissemination of the vaccine is necessary. 8
The Chicago COVID-19 Community Vulnerability Index (CCVI) identified communities that are uniquely vulnerable to the adverse effects of COVID-19 by ranking 10 components across 4 broader categories—sociodemographic (3 components), epidemiologic (2 components), occupational (2 components), and cumulative COVID-19 burden (3 components)—and by synthesizing results into a composite score.9,10 Chicago zip codes that received high CCVI scores had low socioeconomic status, high rates of COVID-19 hospital admission, and high rates of COVID-19 mortality. 11 The top quintile of CCVI scores comprises 13 zip codes, 6 of which have a majority of Latinx residents and 7 of which have a majority of Black residents, as shown by the 2015-2019 American Community Survey 5-year estimates. 12
To reduce further inequities in COVID-19–related outcomes, on January 25, 2021, Chicago announced Protect Chicago Plus (PCP), a citywide plan for equitable vaccine distribution. 13 For the PCP program, the city of Chicago used 3 strategies to increase vaccine uptake in the top quintile of CCVI zip codes (prioritized communities). First, the city worked with each prioritized community to create a neighborhood task force composed of diverse representatives to design vaccine outreach and distribution strategies. Second, the city worked with these groups to implement agreed-on strategies, which included door-to-door vaccination outreach, call-in lines, mobile clinics, distribution to homebound residents, and other community-led vaccination events.14,15 As part of the program, the city of Chicago also expanded vaccine eligibility in PCP communities beyond what was outlined in the city’s phased distribution plan, which included all residents aged ≥18 years. 16 Implementation of the program began February 5, 2021, and eligibility was expanded on March 29, 2021, and was ongoing as of July 2022.
We provide an overview of Chicago’s COVID-19 vaccine coverage during a 4-month period, from December 29, 2020, through May 1, 2021. We focused on evaluating whether the number of first-dose vaccinations improved in areas of Chicago with high CCVI after implementation of the PCP program. Specifically, we aimed to determine to what extent PCP improved the uptake of COVID-19 vaccines among communities with high CCVI as compared with all other communities in Chicago.
Methods
The Ann & Robert H. Children’s Hospital Institutional Review Board (2021-4755) reviewed the study, determined that the research did not constitute human participant research, and waived formal ethical review. We used publicly available deidentified data, which included population characteristics (age, race and ethnicity, socioeconomic status, and worker occupation) 12 ; weekly COVID-19 case, death, and testing counts by zip code 17 ; and daily first-dose COVID-19 vaccination counts by zip code. 18 The Chicago zip code–level data used in our analysis are the most granular COVID-19 information and are made publicly available by the city. Press releases from the city of Chicago, related media reports, and personal communication with municipal public health personnel concerning the geographic scope, rollout, and overall implementation of the city’s PCP vaccination program also informed the periods evaluated in our study.16,19
We first aggregated socioeconomic and zip code–level COVID-19 vaccination data by PCP status of the zip code, designating zip codes that were prioritized and not prioritized through the PCP program as PCP and non-PCP, respectively. We then used these data to create a series of 2-way contingency tables representing cumulative daily percentages of first-dose COVID-19 vaccination coverage by PCP status for residents aged ≥16 years. Altogether, we created 124 contingency tables that compared vaccination coverage between PCP and non-PCP zip codes for each day from December 29, 2020, through May 1, 2021. We then evaluated differences in cumulative vaccination uptake between PCP and non-PCP zip codes using rate ratios (ie, vaccination coverage in PCP zip codes divided by a similar rate for non-PCP zip codes) and a series of Pearson χ2 tests of independence. We made comparisons of the χ2 statistics with the corresponding critical values using a df of 1 at the level of P < .05.
We then implemented 2 quasi-experimental basic interrupted time series (ITS) models to assess the effects of the PCP program before and after its implementation. We used ITS as our statistical approach because it requires fewer controls in the regression equation as compared with more conventional multivariate regression models, allowing for general inferences to be made about the program’s efficacy with respect to 2 independent variables (time and program start date).20-22 ITS models use linear regression to estimate coefficients that represent changes in slope between periods before and after implementation of the PCP program, including the shorter- and longer-term effects.
For our analyses, we used the modeled slope coefficient to quantify the difference between the pre– and the post–PCP implementation period with regard to vaccine distribution. We made our analyses with some qualifications attributed to the city’s COVID-19 vaccine distribution. Phase 1A of Chicago’s vaccine distribution plan began December 15, 2020, with vaccine eligibility to all Chicago health care workers; phase 1B began January 25, 2021, expanding vaccine eligibility to all Chicago residents aged ≥65 years, essential frontline workers, and residential workers (which included caregivers and people working in non–health care residential settings, such as homeless shelters and correctional facilities). On February 5, 2021, the city of Chicago began implementing the PCP program in selected communities and expanding vaccine eligibility to all residents aged ≥18 years in prioritized zip codes. Phase 1C began March 29, 2021, expanding vaccine eligibility to all Chicago residents aged 16-64 years with underlying health conditions and all other essential workers, and phase 2 began April 19, 2021, expanding eligibility to all Chicago residents aged ≥16 years.
We used R statistical program version 4.0.5 (R Foundation for Statistical Computing) with associated code made publicly available on GitHub (https://github.com/justenvirons/vaccine-equity) for data transformation and statistical analyses.
Results
Among the 13 Chicago zip codes prioritized in the PCP program (808 387 people aged ≥16 y), we found the distribution of Black residents (44.1%) and Latinx residents (45.2%) to be nearly equal. Within the PCP zip codes, 24.3% of households had an annual household income below the federal poverty level, and 13.4% of residents had no health insurance (Table). From January 15, 2020, through May 1, 2021, the numbers of COVID-19 cases (118.1) and COVID-19 deaths (2.4) per 100 000 population in PCP zip codes were higher than the corresponding estimates (89.9 and 1.7) for residents in non-PCP zip codes. Furthermore, the total population receiving ≥1 dose of COVID-19 vaccine per 100 000 population was 48.0 in PCP zip codes and 58.2 in non-PCP zip codes, despite PCP zip codes having a higher number of essential workers (59.7% vs 36.1%) and a higher percentage of residents aged ≥65 years (12.9% vs 12.3%).
Table.
Demographic characteristics, cumulative COVID-19 outcomes, and vaccination activity of Chicago residents by PCP status, January 15, 2020, through May 1, 2021 a
| PCP status | |||
|---|---|---|---|
| Characteristics and COVID-19 data | In non-PCP zip codes | In PCP zip codes | City of Chicago |
| Total zip codes, no. | 47 | 13 | 58 |
| Total population | 1 955 851 (70.8) | 808 387 (29.2) | 2 764 238 (100.0) |
| Demographic characteristics b | |||
| Age group, y | |||
| ≥16 | 1 651 595 (82.0) | 564 061 (75.2) | 2 215 656 (80.2) |
| ≥18 | 1 589 133 (81.3) | 596 254 (73.8) | 2 185 387 (79.1) |
| ≥65 | 240 686 (12.3) | 103 991 (12.9) | 344 677 (12.5) |
| Essential workers | 381 144 (36.1) | 193 836 (59.7) | 574 980 (41.7) |
| Race and ethnicity | |||
| Asian, not Latinx | 164 040 (8.4) | 14 241 (1.8) | 178 281 (6.5) |
| Black, not Latinx | 455 820 (23.3) | 356 834 (44.1) | 812 654 (29.4) |
| Latinx | 427 528 (21.9) | 365 082 (45.2) | 792 610 (28.7) |
| White, not Latinx | 856 503 (43.8) | 63 723 (7.9) | 920 226 (33.3) |
| Earning below poverty-level income | 300 723 (15.8) | 195 271 (24.3) | 495 994 (18.3) |
| No health insurance | 156 004 (8.1) | 108 182 (13.4) | 264 186 (9.7) |
| COVID-19 data c | |||
| Cases | 175 903 (89.9) | 95 462 (118.1) | 271 365 (98.2) |
| Deaths | 3308 (1.7) | 1945 (2.4) | 5253 (1.9) |
| Tests | 2 925 814 (149.6) | 861 002 (106.5) | 3 786 816 (137.0) |
| Test positivity rate (cases/tests c × 100), % | 6.0 | 11.1 | 7.2 |
| Mean CCVI score d | 28.8 | 52.6 | 35.7 |
| First COVID-19 vaccine dose e | 924 146 (58.2) | 286 275 (48.0) | 1 210 421 (55.4) |
| Completed COVID-19 vaccine series e | 650 283 (40.9) | 199 258 (33.4) | 849 541 (38.9) |
Abbreviations: CCVI, Chicago COVID-19 Community Vulnerability Index; PCP, Protect Chicago Plus.
Included residents were those aged ≥16 years. Data sources: US Census Bureau 12 and City of Chicago Data Portal.11,17,18
All values are no. (%) unless otherwise indicated.
COVID-19 data are reported as counts (counts/100 000 population) from January 15, 2020, through May 1, 2021, unless otherwise indicated.
CCVI ranked zip codes based on a composite score derived from a series of 10 components across 4 broader categories of vulnerability: sociodemographic (3 components), epidemiologic (2 components), occupational (2 components), and cumulative COVID-19 burden (3 components).
First COVID-19 vaccine dose and completed COVID-19 vaccine counts are reported as cases (cases per 100 000 population) by zip code from December 15, 2020, through May 1, 2021.
We found significant associations between PCP status and first-dose vaccine coverage for Chicago residents aged ≥16 years across each of the 124 days examined (P < .05), although variations in the magnitude of these associations changed over time. When evaluated collectively, PCP zip codes underperformed as compared with non-PCP zip codes in first-dose vaccination coverage, with an average rate ratio of 0.70. That is, vaccination coverage among residents in PCP zip codes was, on average, 70% of the coverage estimated for residents in non-PCP zip codes. A rate ratio of 1.0 would indicate equal vaccination coverage in the 2 groups. We observed that the gap in vaccination coverage steadily narrowed from a rate ratio of 0.58 on February 5, 2021, to 0.92 on March 29, 2021, before it remained steady at a daily average of 0.87 through April 19, 2021.
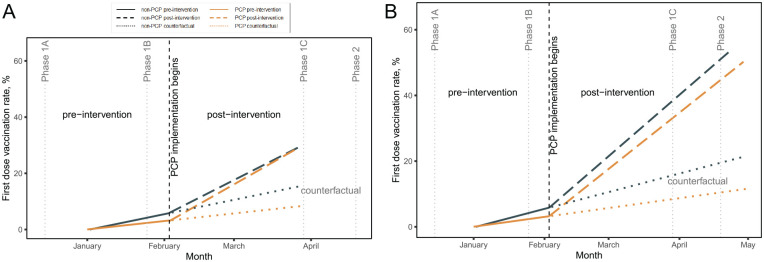
The ITS results (Figure) suggested that the PCP program reduced inequities between communities with low and high CCVI scores over time. Before implementation of the PCP program, cumulative rates of first-dose vaccination increased nearly twice as fast in non-PCP zip codes (0.19% per day; P < .001) as in PCP zip codes (0.10% per day; P < .001). Model results showed that from February 5 through March 29, 2021, PCP zip codes had an additional coverage per day of 0.42% as compared with 0.27% for non-PCP zip codes (Figure A). In an assessment of the longer-term sustained effect of PCP from February 5 through May 1, 2021, which included the gradual expansion of vaccine eligibility to include all Chicago residents aged ≥16 years, residents of PCP and non-PCP zip codes were vaccinated at similar rates of 0.47% and 0.43% per day, respectively (P < .001) (Figure B).
Figure.
Interrupted time-series analysis of short-term (A) and sustained (B) effects of cumulative first-dose COVID-19 vaccination coverage, before and after and implementation of the Protect Chicago Plus (PCP) program in Chicago zip codes, December 29, 2020, through May 1, 2021. Short-term effects analyzed PCP implementation from February 5 through March 29, 2021. Sustained effects analyzed PCP implementation from February 5 through May 1, 2021. Data sources: US Census Bureau12 and City of Chicago Data Portal.11,17,18
Discussion
Our findings showed that PCP may have reduced vaccine inequities between communities with low and high CCVI scores, suggesting that community-led vaccination efforts may have had a positive effect on uptake. We note that barriers to vaccination may be mitigated by not only increasing access but also addressing vaccine hesitancy and medical mistrust . In a 2022 analysis of strategies to promote COVID-19 vaccine equity, authors asserted 3 main strategies: addressing mistrust, combatting misinformation, and improving access. 23 Equity efforts must engage key members of the community to ensure that strategies are salient to community residents. The PCP program included walk-in and scheduled appointments, as well as centralized and community-based vaccine opportunities. If found effective in the long term, the PCP program can serve as a model to improve national equity in vaccine distribution.
Limitations
This study had several limitations. First, because of limitations in data availability and accuracy, we used data on first dose as an indicator of vaccine status. Future analyses should consider using data on fully vaccinated individuals (ie, people who have either completed an initial series of vaccinations or are up to date with the federally recommended COVID-19 vaccination program, including booster doses). Second, the study period may be too short and variable (eg, overlap with vaccine eligibility changes and expanded access) to detect impact. Because of the brief study period, we were only able to obtain insights into the early effects of PCP and not able to make determinations about the longer-term effects of the program. The evaluation should be repeated as additional data become available. Furthermore, we did not disaggregate the vaccine counts made available by the city by age group, making it impossible to stratify by age group and evaluate the sensitivity of the ITS model results. Finally, our analysis focused only on Chicago. Although Chicago may be demographically similar to other large urban jurisdictions, our findings may not be generalizable to other settings.
Citywide implementation strategies may improve vaccine equity and address health inequities. It is important to monitor the impact of vaccine equity strategies to rapidly identify and address any needed modifications and to inform future program scale-up.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Amy K. Johnson, PhD, MSW  https://orcid.org/0000-0002-4247-455X
https://orcid.org/0000-0002-4247-455X
Bijou Hunt, MA  https://orcid.org/0000-0002-6787-295X
https://orcid.org/0000-0002-6787-295X
Jacquelyn Jacobs, MPH  https://orcid.org/0000-0003-1584-3521
https://orcid.org/0000-0003-1584-3521
References
- 1. Scannell Bryan M, Sun J, Jagai J, et al. Coronavirus disease 2019 (COVID-19) mortality and neighborhood characteristics in Chicago. Ann Epidemiol. 2021;56:47-54.e5. doi: 10.1016/j.annepidem.2020.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention. COVID data tracker. March 28, 2020. Accessed March 15, 2021. https://covid.cdc.gov/covid-data-tracker/#datatracker-home
- 3. Maroko AR, Nash D, Pavilonis BT. COVID-19 and inequity: a comparative spatial analysis of New York City and Chicago hot spots. J Urban Health. 2020;97(4):461-470. doi: 10.1007/s11524-020-00468-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466-2467. doi: 10.1001/jama.2020.8598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ruprecht MM, Wang X, Johnson AK, et al. Evidence of social and structural COVID-19 disparities by sexual orientation, gender identity, and race/ethnicity in an urban environment. J Urban Health. 2021;98(1):27-40. doi: 10.1007/s11524-020-00497-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. City of Chicago. COVID-19 dashboard. 2021. Accessed May 2, 2021. https://www.chicago.gov/content/city/en/sites/covid-19/home/covid-dashboard.html
- 7. Gee J, Marquez P, Su J, et al. First month of COVID-19 vaccine safety monitoring—United States, December 14, 2020–January 13, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(8):283-288. doi: 10.15585/mmwr.mm7008e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Salmon D, Opel DJ, Dudley MZ, Brewer J, Breiman R. Reflections on governance, communication, and equity: challenges and opportunities in COVID-19 vaccination. Health Aff (Millwood). 2021;40(3):419-425. doi: 10.1377/hlthaff.2020.02254 [DOI] [PubMed] [Google Scholar]
- 9. Centers for Disease Control and Prevention, Agency for Toxic Substances and Disease Registry. CDC/ATSDR Social Vulnerability Index. April 28, 2021. Accessed May 2, 2021. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
- 10. City of Chicago Data Portal. Chicago COVID-19 Community Vulnerability Index (CCVI). 2020. Accessed December 15, 2020. https://data.cityofchicago.org/Health-Human-Services/Chicago-COVID-19-Community-Vulnerability-Index-CCV/xhc6-88s9
- 11. City of Chicago Data Portal. Chicago COVID-19 Community Vulnerability Index (CCVI)—zip code only. 2021. Accessed May 11, 2021. https://data.cityofchicago.org/Health-Human-Services/Chicago-COVID-19-Community-Vulnerability-Index-CCV/2ns9-phjk
- 12. US Census Bureau. American Community Survey: 2015-2019 ACS 5-year estimates. December 2020. Accessed June 2, 2021. https://www.census.gov/programs-surveys/acs/technical-documentation/table-and-geography-changes/2019/5-year.html
- 13. City of Chicago, Mayor’s Press Office. City of Chicago launches “Protect Chicago” strategy to mitigate further spread of COVID-19. November 12, 2020. Accessed April 13, 2021. https://www.chicago.gov/content/city/en/depts/mayor/press_room/press_releases/2020/november/ProtectChicagoStrategy.html
- 14. Block Club Chicago. Protect Chicago Plus archives. 2021. Accessed May 12, 2021. https://blockclubchicago.org/tag/protect-chicago-plus
- 15. City of Chicago. Protect Chicago Plus in Belmont Cragin. February 6, 2021. Accessed April 13, 2021. https://www.chicago.gov/content/city/en/sites/covid19-vaccine/home/blog/vaccination-event-in-belmont-cragin.html
- 16. City of Chicago. Vaccine distribution phases. 2021. Accessed April 15, 2021. https://www.chicago.gov/content/city/en/sites/covid19-vaccine/home/vaccine-distribution-phases.html
- 17. City of Chicago Data Portal. COVID-19 daily cases, deaths, and hospitalizations. 2021. Accessed February 11, 2021. https://data.cityofchicago.org/Health-Human-Services/COVID-19-Daily-Cases-Deaths-and-Hospitalizations/naz8-j4nc
- 18. City of Chicago Data Portal. COVID-19 vaccine doses by zip code—at least one dose. 2021. Accessed May 11, 2021. https://data.cityofchicago.org/Health-Human-Services/COVID-19-Vaccine-Doses-by-ZIP-Code-At-Least-One-Do/c28u-q29v
- 19. City of Chicago. Mayor’s press releases. 2021. Accessed April 5, 2021. https://www.chicago.gov/content/city/en/depts/mayor/press_room/press_releases.html
- 20. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348-355. doi: 10.1093/ije/dyw098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Biglan A, Ary D, Wagenaar AC. The value of interrupted time-series experiments for community intervention research. Prev Sci. 2000;1(1):31-49. doi: 10.1023/A:1010024016308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kontopantelis E, Doran T, Springate DA, Buchan I, Reeves D. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ. 2015;350:h2750. doi: 10.1136/bmj.h2750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dada D, Djiometio JN, McFadden SM, et al. Strategies that promote equity in COVID-19 vaccine uptake for Black communities: a review. J Urban Health. 2022;99(1):15-27. doi: 10.1007/s11524-021-00594-3 [DOI] [PMC free article] [PubMed] [Google Scholar]