Abstract
Quality of life (QOL) and delay discounting (preference for smaller, immediate rewards) are significantly associated with substance use status, severity, and treatment outcomes. Associations between delay discounting and QOL among individuals in recovery from substance use have not been investigated. In this two-study investigation, using data collected from The International Quit & Recovery Registry, we examined the association between QOL, discounting rates, and remission status among individuals in recovery from SUD. Study 1 (N=166) investigated the relationship between delay discounting and QOL among individuals in recovery from SUD. Study 2 (N=282) aimed to validate and extend the results of Study 1 by assessing the association between the remission status, delay discounting, and QOL among individuals in recovery from alcohol use disorder (AUD). In both studies, delay discounting was a significant predictor of QOL domains of physical health, psychological, and environment even after controlling for age, gender, race, ethnicity, education, and days since last use. In Study 2, a mediation analysis using Hayes’ methods revealed that the association between the remission status and QOL domains of physical health, psychological and environment were partially mediated by the discounting rates. The current study expands the generality of delay discounting and indicates that discounting rates predict QOL and remission status among individuals in recovery from substance use disorders. This finding corroborates the recent characterizations of delay discounting as a candidate behavioral marker of addiction and may help identify sub-groups that require special treatment or unique interventions to overcome their addiction.
Keywords: Substance Use, Delay Discounting, Quality of Life, Recovery, Remission, WHOQOL-BREF
Public Significance Statement: In this investigation, delay discounting, which assesses the extent to which an individual chooses smaller, sooner rewards over larger, delayed ones, was significantly associated with quality of life domains of physical health, psychological, and environment among individuals in recovery from substance use. In addition, delay discounting was significantly associated with the remission status among those in recovery from alcohol. That is, those in remission (had no signs or symptoms -other than craving- of active addiction in the last 3 months) had lower rates of discounting (higher valuation of larger delayed rewards) compared to those not in remission. This information may serve as a base to better identify and target subgroups at higher risk of relapse and those that need special interventions to increase their likelihood of achieving better treatment outcomes.
Substance use disorders (SUDs) are chronically relapsing conditions that entail continuous support and management to prevent relapse and support long-term recovery (NIH, 2018; Volkow, 2010). Recovery is a multidimensional process not only involving abstinence, but also improving one’s wellness, health, and quality of life (Betty Ford Institute Consensus Panel, 2007; Kelly & Hoeppner, 2015; Laudet, 2007; McLellan, 2010; Rockville, 2010). Quality of life (QOL) refers generally to one’s perceived well-being and comprises multiple domains such as physical health (e.g., activities of daily living, energy, pain, and work capacity), psychological functioning (e.g., appearance, feelings, self-esteem, perceived cognition), social relationships (e.g., social support, personal relationships, and sexual activity) and environment (e.g., financial resources, freedom, health and social care, and home environment). Improving the quality of life is an especially important outcome when treating chronic conditions that cannot be cured. Similar to other chronic conditions (Mendlowicz, 2000; The World Health Organization, 1995), QOL measurement in SUDs aims to capture the impact and burden of addiction on individuals and societies and assesses psychosocial functioning during substance use or recovery (Laudet, 2011). This information is important for the development and evaluation of treatments.
While in 1990, QOL was called “the missing measurement in health” (Fallowfield, 1990), today almost all areas of medicine have published studies on QOL. Research and interest in understanding the association between changes in QOL, substance use, and the recovery process has been gaining ground (Bizzarri et al., 2005; Donovan et al., 2005; Havassy & Arns, 1998; Millson et al., 2006; Morgan et al., 2003; Puigdollers et al., 2004; Rudolf & Watts, 2002; Smith & Larson, 2003; Villeneuve et al., 2006). Addiction research examining the impact of substance use treatment is gradually shifting from the traditional paradigm of assessing drug use as the main outcome of treatment to a new paradigm that is complemented by QOL outcomes (Donovan et al., 2005; Institute of Medicine et al., 2006; Laudet, 2011; McLellan et al., 2000; White et al., 2003). Previous studies among individuals with alcohol and drug-dependencies have indicated a negative impact of SUD on domains of QOL such as physical functioning (Morgan et al., 2003; Stein et al., 1998), mental functioning (Préau et al., 2007; Smith & Larson, 2003; Volk et al., 1997), social relationships, employment and others (Hubbard et al., 2003; Smith & Larson, 2003). QOL is significantly associated with substance use status and severity. For example, current users and SUD treatment seekers have poorer QOL compared to non-users (Donovan et al., 2005; Gonzales et al., 2009; Rudolf & Watts, 2002; Smith & Larson, 2003). Moreover, the severity and number of alcohol or drug problems are negatively associated with functioning in almost all QOL domains (McKenna et al., 1996; Volk et al., 1997). Previous studies reported positive treatment-related changes in most QOL domains of functioning, including overall life satisfaction, psychosocial functioning, social relationships, environment, and employment (Donovan et al., 2005; Fassino et al., 2004; Foster et al., 2000; Hubbard et al., 2003; Kraemer et al., 2002; Morgan et al., 2003; Villeneuve et al., 2006). In addition, a study by Laudet and Stanick (2010) has indicated that the level of QOL satisfaction measured at the end of outpatient treatment is predictive of commitment to abstinence, which in turn is a strong predictor of actual abstinence.
Understanding the processes underlying decision-making in substance use (e.g., choosing short-term reinforcement from substance use or long-term reinforcement from abstinence) are important to the success of treatment. Behavioral economics, which integrates psychology and economics, has been widely utilized to understand the effects of psychological, cognitive, social, and emotional factors on decision-making (Bickel et al., 2014; Heather & Vuchinich, 2003). Delay discounting, the subjective decline in the value of a reward with the delay to its receipt (Madden & Bickel, 2010), is a candidate behavioral marker of addiction (Bickel et al., 2019; Bickel et al., 2014). Individuals with SUD have greater rates of discounting compared to healthy controls (Amlung et al., 2016; Bickel et al., 2014; MacKillop et al., 2011). This finding is consistent among most substances of abuse, including alcohol (Mitchell et al., 2005; Petry, 2001). Delay discounting is associated positively with the risk of substance use, substance consumption and dependence (Fernie et al., 2013; Khurana et al., 2013; MacKillop et al., 2011), and negatively with the likelihood of successful abstinence (Krishnan-Sarin et al., 2007; MacKillop & Kahler, 2009; Sheffer et al., 2012; Sheffer et al., 2014; Washio et al., 2011; Yoon et al., 2007). Moreover, previous studies comparing the ability of different neurocognitive measures to differentiate users from control or to predict treatment outcomes indicated that delay discounting is the best neurocognitive measure to predict substance dependence (Bickel et al., 2017) and treatment outcomes (correctly predicted treatment outcomes of 80% of the sample post-treatment and 81% at follow-up; Coughlin et al., 2018).
Based on a study conducted by Rubenis et al. (2018), discount rates may predict QOL improvement during early treatment for people with methamphetamine dependence. However, to our knowledge, the relationship between delay discounting and QOL among individuals in recovery from SUDs in general and from alcohol use disorders (AUDs) specifically has not been previously examined. The current investigation, in two separate cross-sectional studies, assessed the relationship between delay discounting and QOL among individuals in recovery from SUDs. Additionally, as an integral part of the recovery process, remission from SUDs and its association with delay discounting and QOL were examined. Remission is defined as freedom from substance use disorder criteria (except craving) for at least 3 months (Hasin et al., 2013). Study 1 investigated the relationship between delay discounting and QOL among 166 (104 females) individuals in recovery from SUDs. Study 2 sought to validate and extend the results of Study 1 by assessing the association between the remission status, delay discounting, and QOL among 282 (172 females) individuals in recovery from AUD. We hypothesized that higher rates of discounting would be associated with lower QOL among individuals in recovery from SUDs (studies 1 and 2). In addition, we hypothesized that individuals in remission from AUD would show lower discounting rates and greater QOL compared to those still meeting the AUD criteria (Study 2). Establishing the association between delay discounting, QOL, and remission status might help identify individuals in recovery who are at greater risk of relapse.
General Methodology
Participation in both studies was voluntary. Consent was implied through the completion and submission of the survey. This investigation was approved by the Institutional Review Board at Virginia Polytechnic and State University.
Participants
Both studies were conducted using data collected online through the International Quit and Recovery Registry (IQRR), an online community and registry launched in 2011 geared toward individuals in self-reported recovery from various substances. The aims of the IQRR include learning more about the different factors that allow people to overcome addiction, the association between addictions and decision-making, and identifying phenotypes of recovery (see also Athamneh et al., 2017, 2019). Individuals can register on the website (https://quitandrecovery.org), and may create profiles that enable them to complete monthly assessments aimed at advancing the aforementioned goals of the IQRR with no minimum commitment to stay in the registry. For each assessment completed, participants earn a badge (available on their profile) and a set number of points (400 to 1000 points), which can be exchanged at a rate of 100 points for $1.00. In addition, resources aimed at promoting recovery are available on the IQRR website for participants to access at any time and they are encouraged to utilize them.
Study 1
Methodology
A total of 172 participants completed the assessment. Inclusion criteria for Study 1 required that participants be 18 years or older and self-report recovery from one or more SUDs. Given the distinctive set of risks associated with SUDs compared to non-substance addictions such as the impact of substances on physical and mental health, participants were excluded if they reported a non-substance-related addiction (e.g. gambling, binge eating, excessive shopping, etc.; n = 6); thus, the final sample consisted of 166 participants.
Study Measures
Various demographic data including age, race, ethnicity, annual income, gender, marital status, and education level were collected using a standardized questionnaire. All participants self-reported being in recovery from at least one substance addiction. The primary addiction was determined using the question “What was your primary addiction?” for which the options were nicotine, alcohol, cannabis products, opioids, cocaine, stimulants, prescription pain relievers, hallucinogens, dissociative anesthetics, tranquilizers/depressants, inhalants, caffeine, gambling, overeating, binge eating or other eating disorders, excessive shopping, excessive sexual activity, excessive video gaming, excessive viewing of pornography, and excessive preoccupation with activities on the internet. Moreover, participants were asked “When was the last time you engaged in your primary addiction?” and days since last use was calculated by subtracting the response to that question from the date of completing the assessment.
Delay Discounting.
Delay discounting was measured using an adjusting-delay task (Koffarnus & Bickel, 2014). The adjusting-delay tasks determine the delay at which the larger reward loses about 50% of its value compared to the immediate reward. In this task, participants were asked to choose between $1000 in 3 weeks or $500 now. Depending on the response, the next question lengthens or shortens the delay of the $1000 reward (i.e. if the delayed $1000 is chosen, the next question lengthens the delay to 2 years; if the immediate $500 is chosen, the next question shortens the delay for the $1000 reward to 1 day). The delays continue to adjust for a total of five choice trials (Koffarnus & Bickel, 2014). The adjusting-delay task assumes that the value of the delayed reward is discounted hyperbolically based on Mazur’s equation (Mazur, 1987).
The indifference points (expressed in days) provided by the adjusting-delay task were used to calculate ED50 (i.e., the delay expected to reduce the value of the larger reward by 50%). Then, the inverse of this ED50 (1/ED50) was calculated to provide an estimate of the discounting rate (k) based on Mazur’s hyperbolic discounting equation (Koffarnus & Bickel, 2014; Yoon & Higgins, 2008). As the observed k values were positively skewed, the natural log transformation of k was used in analyses. The 5-trial adjusting-delay task was used in this study due to its flexibility and ability to quickly but accurately assess the discounting rate (Koffarnus and Bickel 2014). However, given that the task is relatively new and only assesses a single indifference point, an increased measurement error is possible.
World Health Organization Quality of Life Assessment (Brief).
The original World Health Organization Quality of Life Assessment (WHOQOL-100) was created as a 100-item assessment that would allow for cross-cultural indication of perceptions of quality of life (Group & The WHOQOL Group, 1994; Kim, 2014). The brief version (WHOQOL-BREF) is a 26-item assessment shortened from the original WHOQOL-100 (“Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group,” 1998). The assessments attempt to measure four main domains of QOL (multiple facets per domain): (1) physical health (e.g., activities of daily living, energy and fatigue, pain and discomfort); (2) psychological (e.g., negative and positive feelings, thinking, learning, and concentration); (3) social relationships (e.g., personal relationships, social support, sexual activity); and (4) environment (e.g., financial resources, freedom, physical safety, and physical environment). Each item in the WHOQOL-BREF is associated with one facet of one of the four larger domains, and two questions are meant to represent a more general perception of the quality of life and health. Each item in the WHOQOL-BREF was scored with a 5-point Likert scale (three items are reverse scored), and these scores were used to generate raw scores for each domain, which were then scaled 0–100 (the World Health Organization, 1998).
Statistical Analysis
Descriptive statistics were used to determine the means and distribution of sample characteristics. Bivariate linear regression analyses of delay discounting were carried out with each of the QOL domains, and results were presented as unadjusted coefficients with 95% confidence intervals (CI). In addition, to assess the ability of discounting rates to predict QOL, multivariate linear regression analysis was run with each of the QOL domains as dependent variables and discounting rates, demographics and substance use (i.e., age, gender, race, ethnicity, education level, and days since last use) as independent variables. All analyses were conducted in SPSS 26 (IBM Analytics, Armonk, NY) at a significance level of 0.05.
Results
A total of 166 participants completed the questionnaire and were included in the analysis. The distribution of the socio-demographic characteristics, substance use, discounting rates, and QOL domains for participants in Study 1 is shown in Table 1. The multivariate linear regression results indicated that all QOL domains (i.e., physical health, psychological, social relationships, and environment) were associated negatively with delay discounting rates even after controlling for age, gender, race, ethnicity, recent substance use, time since last use, and education level indicating that participants with lower degrees of delay discounting reported higher QOL (Table 2). Although the main findings are in agreement with our predictions, Study 1 did not assess the association and predictive utility of QOL or discounting rates of one’s remission status. In addition, given the possible distinctive effect associated with different SUDs on discounting rates and QOL, replicating the findings among each of the substances separately could enhance generalizability. Thus, before discussing the findings in Study 1, we aimed to replicate them in Study 2 among individuals in recovery from AUD while adding the Diagnostic and Statistical Manual (DSM-5) criteria for AUD dependence and remission.
Table 1.
Sample Characteristics for Study 1 (N = 166)
| Characteristics | Frequency (%) / Mean (SD) |
|---|---|
|
| |
| Female | 104 (62.7) |
| Marital Status* | |
| Single | 76 (46.1) |
| Married | 46 (27.9) |
| Other | 45 (27.3) |
| Education level* | 39 (23.6) |
| High school diploma/GED or less | 60 (36.4) |
| Some college or vocational training | |
| Completed a 4-year college degree or higher | 66 (40.0) |
| Income***** | |
| Less than $9,999 | 46 (28.6) |
| $10,000–$29,999 | 41 (25.5) |
| $30,000–$49,999 | 40 (24.8) |
| $50,000–$69,999 | 13 (8.1) |
| $70,000+ | 21 (13.0) |
| Race** | |
| Asian | 12 (7.3) |
| Black or African American | 8 (4.9) |
| White | 134 (81.7) |
| Other | 10 (6.1) |
| Non-Hispanic*** | 158 (96.9) |
| Primary addiction | |
| Alcohol | 98 (59.0) |
| Opioids | 22 (13.3) |
| Other | 46 (27.7) |
| Age | 46.77 (14.02) |
| Time since last use (days) | 3375.68 (3921.22) |
| Delay discounting rates (ln[k]) | −4.89 (2.56) |
| ED50 (years) | 2.21 (4.33) |
| WHOQOL-BREF Domain Scores | |
| Physical Health | 64.24 (23.06) |
| Psychological | 60.32 (20.83) |
| Social Relationships | 55.16 (26.06) |
| Environment | 68.45 (21.00) |
Note.
denotes one refusal to respond
Table 2.
Linear Regression Results for QOL and Delay Discounting Rates for Study 1
| Variable | Unadjusted coef. (95% CI) | P-value | Adjusted coef. (95% CI) a | P-Value b |
|---|---|---|---|---|
|
| ||||
| Physical Health | −2.901 (−4.211 −1.590) | <.001 | −2.052 (−3.465 −.639) | .005 |
| Psychological | −2.887 (−4.056 −1.717) | <.001 | −1.439 (−2.698 −.180) | .025 |
| Social Relationships | −3.751 (−5.205 −2.296) | <.001 | −2.621 (−4.276 −.966) | .002 |
| Environment | −3.551 (−4.687 −2.415) | <.001 | −1.975 (−3.132 −.818) | .001 |
Note. Cl= confidence interval
Adjusted to age, gender, years of education, race, ethnicity, and days since last use.
For the adjusted values
Study 2
Methodology
A total of 282 participants completed the assessment. Inclusion criteria for Study 2 required that participants be 18 years or older and meet the DSM-5 criteria for lifetime abuse and dependence of alcohol (report at least 2 DSM-5 criteria of AUD during lifetime).
Study Measures
We collected demographic data including age, income, gender, race, marital status, ethnicity, years of education, and days since last use. Similar to Study 1, the adjusting-delay discounting tasks and QOL measures were collected. All study measures were collected in the same assessment.
DSM-5 for abuse, dependence, and remission from AUD.
DSM-5 alcohol use disorders were assessed using the criteria of the DSM for alcohol abuse and dependence- 5th edition (American Psychiatric Association, 2013; Hasin et al., 2013). Alcohol-specific diagnoses were made for the life-time, last year, and last 3 months timeframes. The survey included 11 symptom questions from the DSM-5 criteria for a diagnosis of alcohol abuse and dependence (American Psychiatric Association, 2013; Hasin et al., 2013; Kuerbis et al., 2013; Sullivan et al., 2020). DSM-5 AUD lifetime diagnosis was established if participants indicated at least two of the 11 criteria in their life-time. Remission status included 2 groups: (1) early remission, defined as ≥3 to <12 months without meeting alcohol use disorders criteria (except craving); and (2) sustained remission as ≥12 months without meeting alcohol use disorders criteria (except craving). The test-retest reliability and validity of DSM-5 SUD diagnosis have been examined in psychometric studies, with fair to good test-retest reliability (κ = 0.4 – 0.6) and fair to excellent dimensional criteria scales (intraclass correlation coefficient [ICC] = 0.5 – 0.9, respectively; (Grant, Goldstein, Saha, et al., 2015; Grant, Goldstein, Smith, et al., 2015; Hasin et al., 2015)
Statistical Analysis
Descriptive statistics were used to determine the means and distribution of sample characteristics. Bivariate linear regression analyses of delay discounting were carried out with each of the QOL domains, and results were presented as unadjusted coefficients with 95% confidence intervals (CI). In addition, to assess the ability of discounting rates to predict QOL, multivariate linear regression analysis was run with each of the QOL domains as dependent variables and discounting rates and demographics (i.e., age, gender, race, ethnicity, marital status, education level, and days since last use) as independent variables.
One-way ANOVA analyses and chi-square analyses were used to compare the means and distribution of sample characteristics within groups (not in remission, in early remission, in sustained remission). As no significant difference in any of the demographics or outcome measures were found between those who were identified as in early remission (n=184) or sustained remission (n=22) based on DSM-5 remission criteria (data not shown), and given the small sample size for those in sustained remission, the two remission groups were reclassified into one group (i.e., in remission) to ease the analysis and interpretation of the results.
T-test and chi-square analyses were used to compare the means and distribution of sample characteristics between the “in remission” and “not in remission” groups. A separate multivariate binary logistic regression was performed to assess the relationship between the remission status (outcome variable) and each of the four QOL domains and delay discounting while controlling for the demographic variables (i.e., age, gender, years of education, marital status, race, and ethnicity).
Next, mediation analysis was conducted using Hayes’ (2017) methods to explore whether rates of discounting partially accounts for the association between QOL domains and the remission status. A bootstrapping technique (with 10,000 bootstrap samples) to estimate 95% confidence intervals (CI) was used. A 95% CI for the product of indirect path coefficient that does not include zero provides evidence of a significant indirect effect (Preacher et al., 2007). All analyses were conducted using IBM SPSS Statistics Version 26 (IBM Analytics, Armonk, NY; George & Mallery, 2019) and macro-program PROCESS 3.4 (Hayes 2009; Hayes 2017) at a significance level of 0.05.
Results
A total of 282 participants completed Study 2 and were included in the analysis. Means and distribution of the socio-demographic characteristics, discount rates, and QOL domains for participants in Study 2 are shown in Table 3. The multivariate linear regression results indicated that discounting is a significant predictor of three of the four QOL domains (i.e., physical health, psychological, and environment) even after controlling for age, gender, race, ethnicity, marital status, and education level (Table 4). Interestingly, the QOL domain of social relationships was not significantly associated with rates of discounting.
Table 3.
Sample Characteristics for Study 2 (N = 282)
| Characteristics | Total Frequency (%) / Mean (SD) |
|---|---|
|
| |
| Female | 172 (61) |
| Marital Status | |
| Single | 75 (26.6) |
| Married | 106 (37.6) |
| Divorced | 50 (17.7) |
| Other | 51 (18.1) |
| Income | |
| Less than $9,999 | 63 (22.3) |
| $10,000–$29,999 | 87 (30.9) |
| $30,000–$49,999 | 51 (18.1) |
| $50,000–$69,999 | 30 (10.6) |
| $70,000+ | 51 (18.1) |
| Race | |
| White | 252 (89.4) |
| Black or African American | 18 (6.4) |
| Other | 12 (4.2) |
| Non-Hispanic | 266 (94.3) |
| Age | 49.81 (14.06) |
| Years of education | 14.39 (4.57) |
| Time since last use (days) | 3962.60 (4310.59) |
| Delay discounting rates (ln[k]) | −5.37 (2.55) |
| ED50 (years) | 3.12 (5.22) |
| WHOQOL-BREF Domain Scores | |
| Physical Health | 66.74 (19.81) |
| Psychological | 61.66 (20.82) |
| Social Relationships | 57.62 (24.68) |
| Environment | 74.05 (19.26) |
Table 4.
Linear Regression Results for QOL and Delay Discounting Rates for Study 2
| Variable | Unadjusted coef. (95% CI) | P value | Adjusted coef. (95% CI) a | P Value b |
|---|---|---|---|---|
|
| ||||
| Physical Health | −1.824 (−2.712 −.936) | <.001 | −1.569 (−2.500 −.637) | .001 |
| Psychological | −1.719 (−2.657 −.780) | <.001 | −1.071 (−2.014 −.129) | .026 |
| Social Relationships | −.701 (−1.836 .434) | .225 | −.579 (−1.784 .626) | .345 |
| Environment | −2.696 (−3.526 −1.867) | <.001 | −2.361 (−3.243 −1.480) | <.001 |
Note. Cl= confidence interval
Adjusted to age, gender, years of education, race, ethnicity, and days since last use.
For the adjusted values
The t-test and pearson chi square analysis of the continuous and categorical demographic variables, respectively, indicated a significant difference in age; t(280) =−5.365, p <0.001], race; X2 (5, N=282) = 14.976, p =0.010, and marital status; X2 (5, N= 282) = 21.005, p =0.001 between the two groups (Table 5). We controlled for demographics (age, gender, race, ethnicity, marital status and education level) in our final multivariate logistic regression analysis (Table 6).
Table 5.
Chi- square and T-test Results for the Demographics Variables by Remission Status in Study 2 (N = 282)
| Total Frequency (within group %) / Mean (SD) | |||
|---|---|---|---|
| Characteristics | In remission n=206 | Not in remission n=76 | P value |
|
| |||
| Female | 128 (74.4) | 44 (57.9) | .517 |
| Marital Status | |||
| Single | 43 (20.9) | 32 (42.1) | .001 |
| Married | 86 (41.7) | 20 (26.6) | |
| Other | 77 (37.3) | 24 (31.6) | |
| Income***** | .160 | ||
| Less than $9,999 | 37 (18.0) | 26 (34.2) | |
| $10,000–$29,999 | 64 (31.1) | 23 (30.3) | |
| $30,000–$49,999 | 38 (18.4) | 13 (17.1) | |
| $50,000–$69,999 | 24 (11.7) | 6 (7.9) | |
| $70,000+ | 43 (20.9) | 8 (10.5) | |
| Race | .010 | ||
| White | 189 (91.7) | 63 (82.9) | |
| Black or African American | 8 (3.9) | 10 (13.2) | |
| Other | 9 (4.3) | 3 (3.9) | |
| Non-Hispanic | 196 (95.1) | 70 (92.1) | .327 |
| Age | 52.41 (13.59) | 42.75 (12.93) | <.001 |
| Years of education | 14.19 (4.386) | 14.93 (5.05) | .236 |
Table 6.
Summary of Multivariate Binary Logistic Regression Analysis of Discounting and QOL Predicting Remission Status in Study 2 (N = 282)
| Characteristics | B | S.E | Wald | P valuea | Exp (B) | 95% CI for Exp (B) | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Delay discounting rates | −.162 | .059 | 7.574 | .006 | .850 | .758 | .954 |
| WHOQOL-BREF | |||||||
| Physical Health | .023 | .008 | 8.629 | .003 | 1.023 | 1.008 | 1039 |
| Psychological | .021 | .008 | 8.098 | .004 | 1.022 | 1.007 | 1.037 |
| Social Relationships | .011 | .006 | 3.497 | .061 | 1.011 | .999 | 1.023 |
| Environment | .018 | .008 | 5.520 | .019 | 1.019 | 1.003 | 1.034 |
Note. Abbreviations: CI, confidence interval; OR, odds ratio; SE, standard error.
Variables entered in all models are age, gender, years of education, race, ethnicity, and marital status.
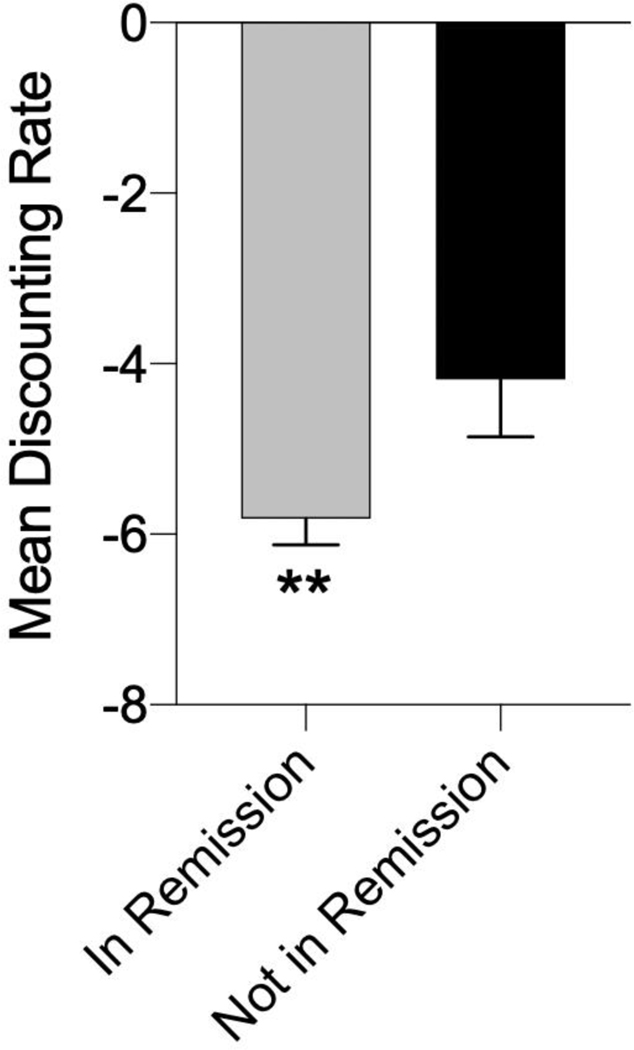
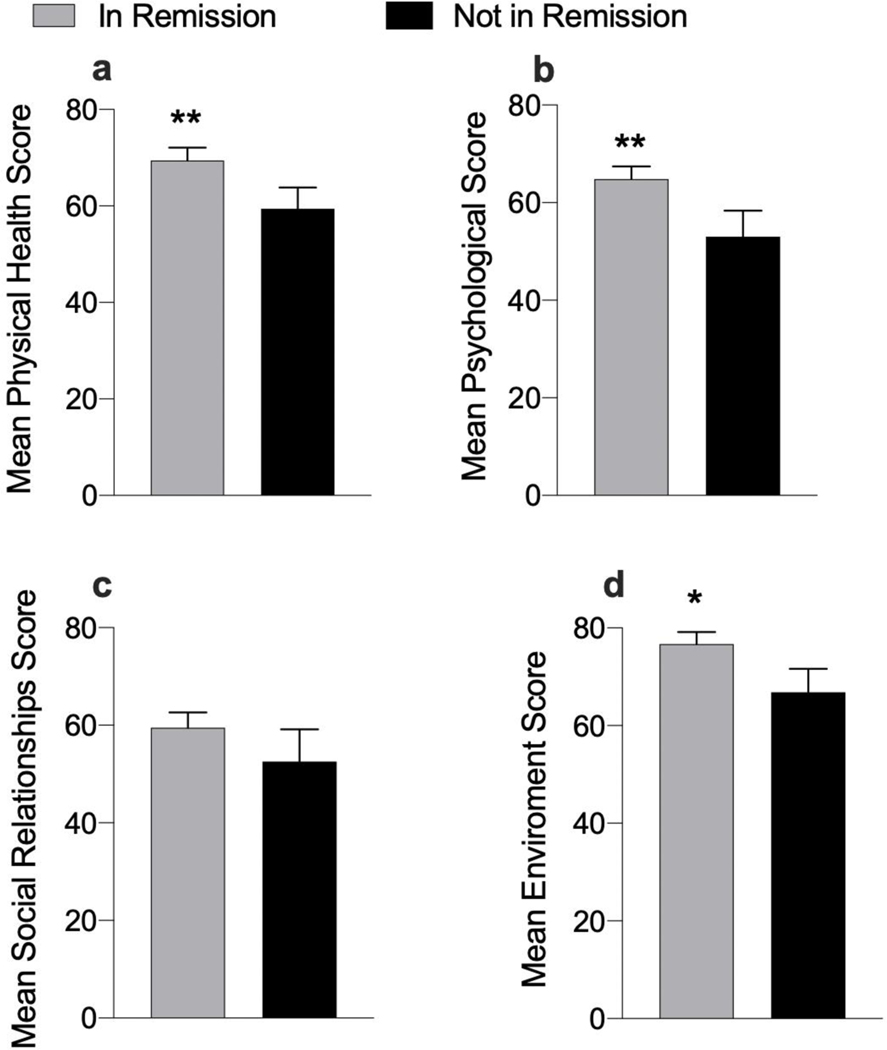
The multivariate binary logistic regression analysis indicated that discounting is a significant predictor of remission status with lower rates of discounting found among those in remission (M =−5.81, SD = 2.23, MED5= 3.81 years) compared to those not in remission (M =−4.18, SD = 2.96, MED50= 1.19 years, p= .006; Figure 1). In addition, those in remission had greater physical health (M =69.43, SD = 19.37) compared to those not in remission (M =59.43, SD = 19.24, p= .003), greater psychological status (M =64.86, SD = 18.87) compared to those not in remission (M =53.00, SD = 23.4, p= .004), and better environment (M =76.72, SD = 17.89) compared to those not in remission (M =66.80, SD = 21.04, p= .019; Figure 2). Interestingly, no significant difference in social relations was observed between those in remission (M =59.50, SD = 22.69) and those not in remission (M =52.54, SD = 28.95, p= .061; Figure 2). Therefore, this variable was not included in the subsequent mediation effect analysis.
Figure 1.
A Comparison from Study 2 of Discounting Rates (ln[k]) between Individuals in Remission and Not in Remission from AUDs.
Note. Error bars represent 95% confidence intervals.
Figure 2.
A Comparison from Study 2 of QOL Domains: (a) Physical Health, (b) Psychological, (c) Social Relationships, and (d) Environment between Individuals in Remission and Not in Remission from AUDs.
Note. Error bars represent 95% confidence intervals.
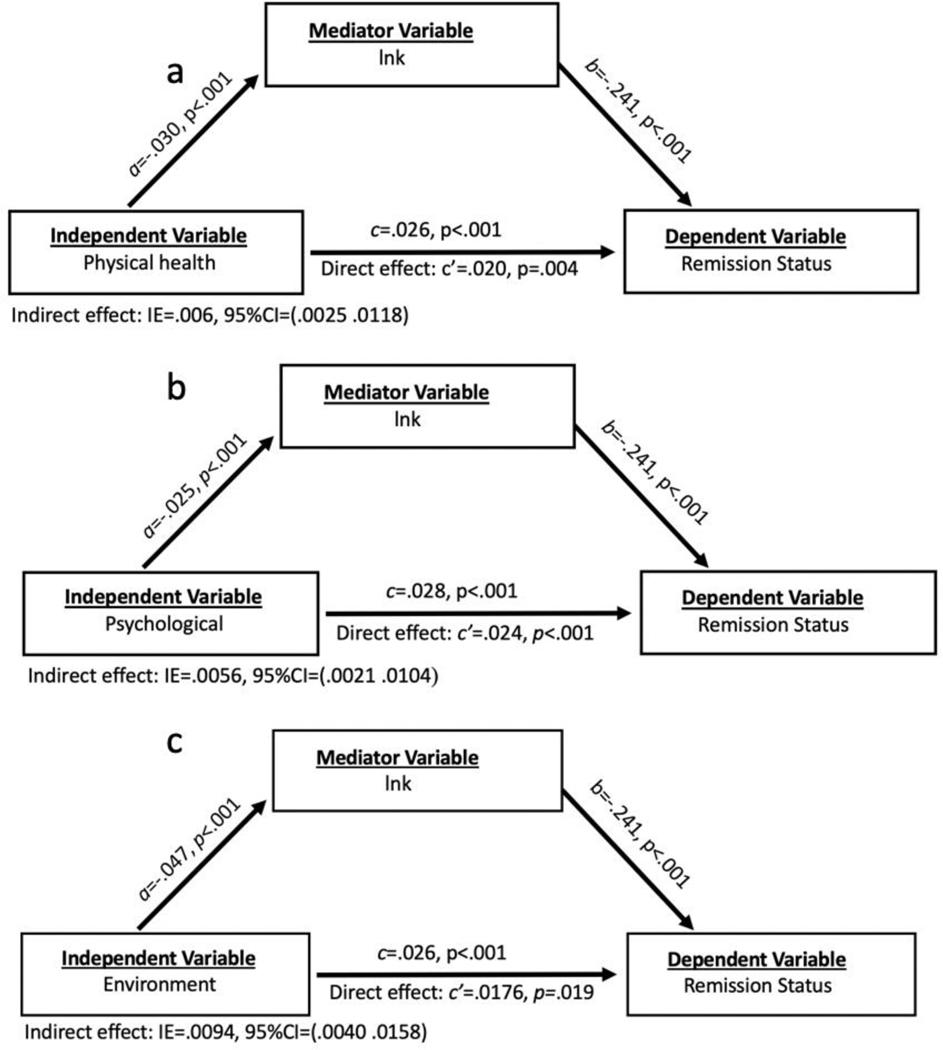
We next used the associated QOL domains (i.e., physical health, psychological, or environment) in mediation analysis. Results suggested significant indirect association between the scores of these domains and the remission status, through delay discounting (Figure 3). Overall, the discounting rates (lnk) represented 24% of the total effect between physical health score and the remission status, 19% of the total effect between psychological score and the remission status, and 35% of the total effect between environment score and the remission status.
Figure 3.
Mediation Analyses Using QOL Domains: (a) Physical Health, (b) Psychological, and (c) Environment
Note. Given that in all cases the indirect effect is statistically significant, they support partial mediation.
Discussion
The present study examined the association between discounting of delayed monetary rewards, assessments of QOL, and remission status in a sample of individuals in recovery from SUDs from the International Quit and Recovery Registry. The results indicate significant associations between physical health, psychological, and environment domains of QOL and discounting (both studies). Greater QOL was observed among those with lower discount rates. In addition, the current findings indicated lower discounting rates and greater physical health, psychological, and environment QOL scores (indicating higher satisfaction) among those in remission from AUDs compared to those not in remission (Study 2). Overall, the discounting rates accounted for 24%, 19%, and 35% of the total effect between the remission status and physical health, psychological, and the environment scores, respectively. These results extend the findings of previous research by reporting a significant association between QOL, rates of discounting and remission status among individuals in recovery from substance dependence. These findings further support delay discounting as a behavioral marker of addiction (Bickel et al., 2014) and support the evolving definition of recovery from substance use disorders as a multifaceted phenomenon (Betty Ford Institute Consensus Panel 2007; Kelly and Hoeppner 2015; Laudet 2007; McLellan 2010). Below, we discuss those findings in more detail.
The WHO-QOL BREF Physical Health domain assesses someone’s body condition to perform daily living activities, including questions on the dependence on medicinal substances and medical aids, level of energy and fatigue, mobility, pain, and discomfort, sleep and rest and work capacity. Previous studies have reported associations between different facets of physical functioning and lower future valuation, such as chronic pain (Tompkins et al., 2016; Wakaizumi et al., 2019), sleep deprivation (Curtis et al., 2018); or greater future valuation, such as physical activity (Tate et al., 2015) in different populations. Overall, the significant relationship between delay discounting and physical health with delay discounting rate accounting for 24% of the total effect between psychological score and remission status is consistent with those findings, suggesting that the capacity to perform daily tasks plays an important role in the subjective valuation of the future among individuals in recovery from substance use disorders.
Even though no previous study has examined the relationship between delay discounting and physical health in individuals in recovery from substance use disorders, the association between physical health-related indicators and treatment effectiveness has been established. Physical activity, for example, is often used as an adjunctive approach to substance use treatment to improve physical health amid other outcomes (see Wang et al., 2014 for a review). Interestingly, one study showed that differences in global functioning between adults submitted to a treatment program and population norms were initially verified but vanished three months after treatment commenced (Morgan et al., 2003). Similarly, detected differences in delay discounting and physical health between participants in remission (lower discount rates and higher physical health scores) and not in remission (higher discount rates and lower physical health scores) enhance the importance of the first months of recovery to leverage outcomes, improve physical health and increase the temporal window.
The WHO-QOL BREF psychological domain investigates several characteristics relating to mental health and cognitive functioning including enjoyment and meaningfulness of life, ability to concentrate, acceptance of bodily appearance, self-satisfaction, and negative feelings such as anxiety and depression. Psychiatric comorbidities, including anxiety and mood disorders, are common in individuals suffering from AUD specifically and in SUD generally (Walker & Druss, 2018). A bi-directional relationship between SUD and psychiatric disorders has been documented, such that the presence of one increases the risk for the other (Hunt et al., 2020). As previously noted, delay discounting has been well established as a determinant of substance use disorder severity (MacKillop et al., 2011), and recent meta-analysis identified discounting as a trans-diagnostic process undergirding several psychiatric conditions including depression (Amlung et al., 2019). Additionally, delay discounting has been shown to have a negative relationship with cognitive functions including working memory (Hinson et al., 2003; Wesley & Bickel, 2014) and educational attainment (Mischel et al., 1989; Kirby et al., 2005), and similar associations have been noted in SUD (Jaroni et al., 2004; Khurana et al., 2013). The relationship between remission status and psychological quality of life have been well documented. Reductions in alcohol use are associated with increased mental health and function status in early and longer-term remission (Donovan et al., 2005). Interestingly, some aspects related to psychological quality of life, including self-esteem and coping ability, have been shown to decrease in early recovery and are a risk factor for relapse (Dennis et al., 2007). The extant research coupled with the finding of this study provides further support for the importance of future valuation in the treatment of SUD. Further understanding of the relationships between psychological quality of life, SUD, and delay discounting seems likely to refine the therapeutic efficacy of current substance use treatment and improve the quality of life of individuals suffering from SUD.
The environment domain of the WHO-QOL BREF assesses a number of behaviors known to be associated with delay discounting and/or alcohol use, including financial resources (Snider et al., 2019; Hamilton & Potenza, 2012; Moos et al., 2010; Mishra & Lalumière, 2017; Ersner-Hershfield et al., 2009), freedom (Petry 2003), physical safety (Hayashi et al., 2015), health and social care (Mishra & Lalumière, 2017; Sheffer et al., 2018; Snider et al., 2019), home environment (Wang et al., 2016), participation in and opportunities for recreation/leisure activities (Snider et al., 2019; Moos & Moos, 2007), and physical environment (Grana et al., 2010; Snider et al., 2019; Gelino & Reed, 2020). The behaviors assessed in the environment domain have been shown to both influence delay discounting and be influenced by delay discounting. For example, demographic characteristics, like education or socioeconomic status, have been shown to influence delay discounting (Wilson et al. 2015; Stanger et al. 2012), and delay discounting rates have been shown to predict relapse rates in smokers (González-Roz et al. 2019; Sheffer et al. 2014). Although neither delay discounting nor the environment domain of quality of life were manipulated in this study, it is worth noting that these measures could influence one another. The current findings of significant association between discounting, the environment domain of QOL, and remission status further support previous literature as mentioned above.
Contrary to our initial hypothesis, social relations did not significantly differ between individuals in remission versus those not in remission. Previous work has shown that engagement in social relationships is imperative in the recovery process and predicts future abstinence (Brereton et al., 2014; Lookatch et al., 2019). Additionally, the larger the social network and the greater the percentage of abstinent individuals in this network, the greater the likelihood that the patient will remain abstinent (Zywiak et al., 2002). Some studies have even used relationship enhancement programs as interventions, showing that this treatment (compared to brief broad-spectrum or extended cognitive-behavioral treatments) is the most effective for individuals who have unsupportive social networks or low levels of investment in their previous social networks (Longabaugh et al., 1995). Collectively, this work shows that abstinence is most successful when individuals in recovery are able to embed themselves in supportive social networks, with the most beneficial being those that are homophilic (i.e., composed of individuals in similar recovery situations). Indeed, social relationships are considered an important part of the environmental enrichment that is now considered necessary for addiction treatment (Galaj et al., 2020).
The majority of the research to date examining the relationship between recovery and social networks has focused on recovery houses, such as Oxford House (OH), or 12-step recovery programs, such as Alcoholics or Narcotics Anonymous (AA/NA), whereby the social networks consist primarily of individuals in recovery (Doogan et al., 2019). Our research here focuses on a potentially more diverse population of individuals in recovery. One interpretation of our negative results is that social relationships may be the most resistant to change or most difficult to repair after the experience of addiction. Additionally, unlike the other QOL subscales, social relationships require the interaction of two people, which might make this area of life particularly challenging to repair. Individuals early in recovery may have social networks that consist largely of drug users, and as recovery progresses, shifting the social network to include others in recovery, and heal familial, romantic, and friend relationships may prove especially challenging. As the positive relationship between social functioning and quality of life in other psychiatric populations has been established (Trompenaars et al., 2007), future studies should investigate factors that promote the recovery of social relations in individuals in addiction recovery.
Finally, a small literature has investigated the phenomenon of social temporal discounting where individuals are required to make a choice between a smaller reward to be shared amongst a group of unknown individuals now or a larger reward to be shared amongst that same group sometime in the future (Charlton et al. 2013; Jones and Rachlin 2006). Interestingly, reports show that individuals are more willing to wait for shared rewards than for individual rewards (Charlton et al. 2013). That is, making monetary decisions in a social context makes individuals more future oriented. Additionally, social discounting rates increase as the perceived social distance between self and other increases (Jones and Rachlin 2006). Consistent with the delay discounting literature, we have shown that individuals with substance use disorders and obesity show steeper social discounting rates than healthy controls (Bickel et al. 2012; Bickel et al. 2014). To our knowledge, no studies to date have explicitly examined social discounting in individuals in addiction recovery. This is clearly an open area of inquiry, and we hypothesize that as recovery progresses, akin to delay discounting, social discounting rates would decrease. Other work has investigated the relationship between delay discounting and social relationships. For example, one prospective longitudinal study found that lower quality parent-adolescent relationships predict later risky sexual behavior, and this relationship is mediated through DD (Kahn et al., 2015). Future research is needed to establish how social relationship quality prior to recovery, engagement in social networks during recovery, and their relationship to DD predict success in addiction recovery and how these measures relate to social discounting.
A significant quality of the current study was the opportunity to use data from the IQRR, a unique online resource that permits the scientific study of recovery processes, depicts different groups of individuals in recovery, and provides an insight into the association between quality of life, delay discounting rates, and remission status in this specific population. The current study suggests several areas for future research. Further research examining the predictive utility of delay discounting of QOL for individuals in recovery from other types of substance and behavioral problems (e.g., cocaine, nicotine, gambling, overeating) may be beneficial. Moreover, additional research is needed to characterize the longer-term trajectory of the recovery process by understanding the relationships between changes in delay discounting over time and their related changes in substance use or remission status.
Despite the findings of the present study, several limitations are worth considering. First, although the IQRR is a valuable research tool to better understand the phenotype of recovery, the online-based assessments consist of self-report measures and limit our sample to include only those individuals in recovery who use technology, have an email address, and register in the IQRR. However, the use of online data collection has been validated by many studies reporting results similar to laboratory-based data collection (Birnbaum 2000; Buhrmester et al., 2011; Paolacci et al., 2010; Suri & Watts, 2011). Most relevant to the present study, online studies have replicated many discounting-related phenomena observed in laboratory studies, including cross-sectional differences in delay discounting related to cigarette smoking and alcohol use disorder (Jarmolowicz et al., 2012; Johnson et al., 2015; VanderBroek et al., 2016).
Second, although the present study assessed the relationship between delay discounting and QOL, several variables were not assessed and they may have affected the results. For example, the study did not collect data about other psychiatric comorbidities, living conditions, or stress levels. As those variables may alter rates of discounting and/or QOL, future research that includes assessments of these factors might be needed to better understand the relationship between QOL and delay discounting. Moreover, in Study 1 we asked participants to self-report being in recovery but did not provide a specific definition to this term. Hence, participants might have interpreted the meaning of recovery differently. In addition, in Study 1 participants were excluded if they reported a non-substance-related addiction. As previous studies have demonstrated that individuals with more than one impulsive disorder (e.g., alcohol use disorder and problem gambling) might exhibit greater discounting, investigating the effect of having multiple addictions on the association between discounting and quality of life would be beneficial to improve our understanding of the current findings. Furthermore, using the cross-sectional design in this study limited our ability to predict the temporal precedence and association between delay discounting and the multiple domains of quality of life. For example, while changes in delay discounting may alter one’s QOL, changes in the QOL and SUD status could feasibly alter self-reported delay discounting as well (e.g., relative improvements in those domains could reduce delay discounting). In addition, as we mentioned in the methods section, while the 5-trial adjusting-delay task is brief, flexible and can accurately assess the discounting rate (Koffarnus and Bickel 2014), the task is relatively new and only assesses a single indifference point increasing the possibility of measurement error. Finally, although all individuals in recovery from substance use are encouraged to join the IQRR, self-selection bias for those who volunteered to join might be present.
Conclusion
The current study expands previous research investigating the association between rates of discounting and substance use and indicates that discounting rates predict the remission status and physical health, psychological, and environment domains of quality of life among individuals in recovery from substance use disorders. This finding corroborates the recent characterizations of delay discounting as a candidate behavioral marker of addiction and may help identify sub-groups that require special treatment or unique interventions to overcome their addiction. Future research characterizing the longer-term trajectory of the recovery process by understanding the relationships between changes in delay discounting over time and their related changes in the substance use or remission status is needed. Moreover, examining the predictive utility of delay discounting of QOL for individuals in recovery from other types of substance and behavioral problems (e.g., cocaine, nicotine, gambling, overeating) may be beneficial.
Funding:
This work was supported by the Fralin Biomedical Research Institute at Virginia Tech Carilion and NIH/NIAAA [grant number R01AA027381]
Footnotes
Author Note
Liqa N. Athamneh, Addiction Recovery Research Center and Center for Transformative Research on Health Behaviors, Fralin Biomedical Research Institute at VTC; Roberta Freitas Lemos, Addiction Recovery Research Center and Center for Transformative Research on Health Behaviors, Fralin Biomedical Research Institute at VTC; Julia C. Basso, Addiction Recovery Research Center and Center for Transformative Research on Health Behaviors, Fralin Biomedical Research Institute at VTC; Devin C. Tomlinson, Addiction Recovery Research Center, Fralin Biomedical Research Institute at VTC and Graduate Program in Translational Biology, Medicine, and Health, Polytechnic Institute and State University; William H. Craft, Addiction Recovery Research Center, Fralin Biomedical Research Institute at VTC and Graduate Program in Translational Biology, Medicine, and Health, Polytechnic Institute and State University; Madison D. Stein, Center for Transformative Research on Health Behaviors, Fralin Biomedical Research Institute at VTC; Warren K. Bickel, Addiction Recovery Research Center and Center for Transformative Research on Health Behaviors, Fralin Biomedical Research Institute at VTC.
References
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). American Psychiatric Pub. [Google Scholar]
- Amlung M, Marsden E, Holshausen K, Morris V, Patel H, Vedelago L, Naish KR, Reed DD, & McCabe RE (2019). Delay Discounting as a Transdiagnostic Process in Psychiatric Disorders: A Meta-analysis. JAMA Psychiatry . 10.1001/jamapsychiatry.2019.2102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amlung M, Vedelago L, Acker J, Balodis I, & Mackillop J. (2016). Steep Delay Discounting and Addictive Behavior: A Meta-Analysis of Continuous Associations. Addiction . 10.1111/add.13535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athamneh LN, DeHart WB, Pope D, Mellis AM, Snider SE, Kaplan BA, & Bickel WK (2019). The phenotype of recovery III: Delay discounting predicts abstinence self-efficacy among individuals in recovery from substance use disorders. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors, 33(3), 310–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athamneh LN, Stein JS, Quisenberry AJ, Pope D, & Bickel WK (2017). The association between parental history and delay discounting among individuals in recovery from addiction. Drug and Alcohol Dependence, 179, 153–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betty Ford Institute Consensus Panel. (2007). What is recovery? A working definition from the Betty Ford Institute. Journal of Substance Abuse Treatment, 33(3), 221–228. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Athamneh LN, Basso JC, Mellis AM, DeHart WB, Craft WH, & Pope D. (2019). Excessive discounting of delayed reinforcers as a trans-disease process: Update on the state of the science. Current Opinion in Psychology, 30, 59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, George Wilson A, Franck CT, Terry Mueller E, Jarmolowicz DP, Koffarnus MN, & Fede SJ (2014). Using crowdsourcing to compare temporal, social temporal, and probability discounting among obese and non-obese individuals. Appetite, 75, 82–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Jarmolowicz DP, Mueller ET, Franck CT, Carrin C, & Gatchalian KM (2012). Altruism in time: social temporal discounting differentiates smokers from problem drinkers. Psychopharmacology, 224(1), 109–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, & Murphy JG (2014). The behavioral economics of substance use disorders: reinforcement pathologies and their repair. Annual Review of Clinical Psychology, 10, 641–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Koffarnus MN, Moody L, & Wilson AG (2014). The behavioral- and neuro-economic process of temporal discounting: A candidate behavioral marker of addiction. Neuropharmacology, 76 Pt B, 518–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Moody LN, Eddy CR, & Franck CT (2017). Neurocognitive dysfunction in addiction: Testing hypotheses of diffuse versus selective phenotypic dysfunction with a classification-based approach. Experimental and Clinical Psychopharmacology, 25(4), 322–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnbaum MH (2000). Introduction to psychological experiments on the internet. In Psychological Experiments on the Internet (pp. xv–xx). [Google Scholar]
- Bizzarri J, Rucci P, Vallotta A, Girelli M, Scandolari A, Zerbetto E, Sbrana A, Iagher C, & Dellantonio E. (2005). Dual diagnosis and quality of life in patients in treatment for opioid dependence. Substance Use & Misuse, 40(12), 1765–1776. [DOI] [PubMed] [Google Scholar]
- Brereton KL, Alvarez J, Jason LA, Stevens EB, Dyson VB, McNeilly C, & Ferrari JR (2014). RECIPROCAL RESPONSIBILITY AND SOCIAL SUPPORT AMONG WOMEN IN SUBSTANCE USE RECOVERY. International Journal of Self Help & Self Care, 8(2), 239–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, & Gosling SD (2011). Amazon’s Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science: A Journal of the Association for Psychological Science, 6(1), 3–5. [DOI] [PubMed] [Google Scholar]
- Charlton SR, Yi R, Porter C, Carter AE, Bickel W, & Rachlin H. (2013). Now for Me, Later for Us? Effects of Group Context on Temporal Discounting. Journal of Behavioral Decision Making, 26(2), 118–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coughlin LN, Tegge AN, Sheffer CE, & Bickel WK (2018). A machine-learning approach to predicting smoking cessation treatment outcomes. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco. 10.1093/ntr/nty259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis BJ, Williams PG, & Anderson JS (2018). Objective cognitive functioning in self-reported habitual short sleepers not reporting daytime dysfunction: examination of impulsivity via delay discounting. Sleep, 41(9). 10.1093/sleep/zsy115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Foss MA, & Scott CK (2007). An eight-year perspective on the relationship between the duration of abstinence and other aspects of recovery. Evaluation Review, 31(6), 585–612. [DOI] [PubMed] [Google Scholar]
- Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. (1998). Psychological Medicine, 28(3), 551–558. [DOI] [PubMed] [Google Scholar]
- Donovan D, Mattson ME, Cisler RA, Longabaugh R, & Zweben A. (2005). Quality of life as an outcome measure in alcoholism treatment research. In Journal of Studies on Alcohol, Supplement (Issue s15, pp. 119–139). 10.15288/jsas.2005.s15.119 [DOI] [PubMed] [Google Scholar]
- Doogan NJ, Light JM, Stevens EB, & Jason LA (2019). Quality of life as a predictor of social relationships in Oxford House. Journal of Substance Abuse Treatment, 101, 79–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ersner-Hershfield H, Garton MT, Ballard K, Samanez-Larkin GR, & Knutson B. (2009). Don’t stop thinking about tomorrow: Individual differences in future self-continuity account for saving. Judgment and Decision Making, 4(4), 280–286. [PMC free article] [PubMed] [Google Scholar]
- Fallowfield L. (1990). The quality of life: the missing measurement in health care. [Google Scholar]
- Fassino S, Daga GA, Delsedime N, Rogna L, & Boggio S. (2004). Quality of life and personality disorders in heroin abusers. Drug and Alcohol Dependence, 76(1), 73–80. [DOI] [PubMed] [Google Scholar]
- Fernie G, Peeters M, Gullo MJ, Christiansen P, Cole JC, Sumnall H, & Field M. (2013). Multiple behavioural impulsivity tasks predict prospective alcohol involvement in adolescents. Addiction , 108(11), 1916–1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster JH, Marshall EJ, & Peters TJ (2000). Application of a quality of life measure, the life situation survey (LSS), to alcohol-dependent subjects in relapse and remission. Alcoholism, Clinical and Experimental Research, 24(11), 1687–1692. [PubMed] [Google Scholar]
- Galaj E, Barrera ED, & Ranaldi R. (2020). Therapeutic efficacy of environmental enrichment for substance use disorders. Pharmacology, Biochemistry, and Behavior, 188, 172829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelino BW, & Reed DD (2020). Temporal discounting of tornado shelter-seeking intentions amidst standard and impact-based weather alerts: A crowdsourced experiment. Journal of Experimental Psychology. Applied, 26(1), 16–25. [DOI] [PubMed] [Google Scholar]
- George D, & Mallery P. (2019). IBM SPSS Statistics Processes for Mac. In IBM SPSS Statistics 26 Step by Step (pp. 26–42). 10.4324/9780429056765-3 [DOI] [Google Scholar]
- Gonzales R, Ang A, Marinelli-Casey P, Glik DC, Iguchi MY, & Rawson RA (2009). Health-related quality of life trajectories of methamphetamine-dependent individuals as a function of treatment completion and continued care over a 1-year period. In Journal of Substance Abuse Treatment (Vol. 37, Issue 4, pp. 353–361). 10.1016/j.jsat.2009.04.001 [DOI] [PubMed] [Google Scholar]
- González-Roz A, Secades-Villa R, Pericot-Valverde I, Weidberg S, & Alonso-Pérez F. (2019). Effects of Delay Discounting and Other Predictors on Smoking Relapse. The Spanish Journal of Psychology, 22, E9. [DOI] [PubMed] [Google Scholar]
- Grana RA, Black D, Sun P, Rohrbach LA, Gunning M, & Sussman S. (2010). School disrepair and substance use among regular and alternative high school students. The Journal of School Health, 80(8), 387–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, & Hasin DS (2015). Epidemiology of DSM-5 Alcohol Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry, 72(8), 757–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Smith SM, Jung J, Zhang H, Chou SP, Pickering RP, Ruan WJ, Huang B, Saha TD, Aivadyan C, Greenstein E, & Hasin DS (2015). The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): Reliability of substance use and psychiatric disorder modules in a general population sample. In Drug and Alcohol Dependence (Vol. 148, pp. 27–33). 10.1016/j.drugalcdep.2014.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Group TW, & The WHOQOL Group. (1994). The Development of the World Health Organization Quality of Life Assessment Instrument (the WHOQOL). In Quality of Life Assessment: International Perspectives (pp. 41–57). 10.1007/978-3-642-79123-9_4 [DOI] [Google Scholar]
- Hamilton KR, & Potenza MN (2012). Relations among delay discounting, addictions, and money mismanagement: implications and future directions. The American Journal of Drug and Alcohol Abuse, 38(1), 30–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Greenstein E, Aivadyan C, Stohl M, Aharonovich E, Saha T, Goldstein R, Nunes EV, Jung J, Zhang H, & Grant BF (2015). The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): Procedural validity of substance use disorders modules through clinical re-appraisal in a general population sample. In Drug and Alcohol Dependence (Vol. 148, pp. 40–46). 10.1016/j.drugalcdep.2014.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, Compton WM, Crowley T, Ling W, Petry NM, Schuckit M, & Grant BF (2013). DSM-5 Criteria for Substance Use Disorders: Recommendations and Rationale. In American Journal of Psychiatry (Vol. 170, Issue 8, pp. 834–851). 10.1176/appi.ajp.2013.12060782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havassy BE, & Arns PG (1998). Relationship of cocaine and other substance dependence to well-being of high-risk psychiatric patients. Psychiatric Services , 49(7), 935–940. [DOI] [PubMed] [Google Scholar]
- Hayashi Y, Russo CT, & Wirth O. (2015). Texting while driving as impulsive choice: A behavioral economic analysis. Accident; Analysis and Prevention, 83, 182–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2009). Beyond Baron and Kenny: Statistical Mediation Analysis in the New Millennium. Communication Monographs, 76(4), 408–420. [Google Scholar]
- Hayes AF (2017). Introduction to Mediation, Moderation, and Conditional Process Analysis, Second Edition: A Regression-Based Approach. Guilford Publications. [Google Scholar]
- Heather N, & Vuchinich RE (2003). Choice, Behavioural Economics and Addiction. Elsevier. [Google Scholar]
- Hinson JM, Jameson TL, & Whitney P. (2003). Impulsive decision making and working memory. Journal of Experimental Psychology. Learning, Memory, and Cognition, 29(2), 298–306. [DOI] [PubMed] [Google Scholar]
- Hubbard RL, Craddock SG, & Anderson J. (2003). Overview of 5-year followup outcomes in the drug abuse treatment outcome studies (DATOS). Journal of Substance Abuse Treatment, 25(3), 125–134. [DOI] [PubMed] [Google Scholar]
- Hunt GE, Malhi GS, Lai HMX, & Cleary M. (2020). Prevalence of comorbid substance use in major depressive disorder in community and clinical settings, 1990–2019: Systematic review and meta-analysis. Journal of Affective Disorders, 266, 288–304. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine, Board on Health Care Services, & Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. (2006). Improving the Quality of Health Care for Mental and Substance-Use Conditions. National Academies Press. [Google Scholar]
- Jarmolowicz DP, Bickel WK, Carter AE, Franck CT, & Mueller ET (2012). Using crowdsourcing to examine relations between delay and probability discounting. Behavioural Processes, 91(3), 308–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaroni JL, Wright SM, Lerman C, & Epstein LH (2004). Relationship between education and delay discounting in smokers. Addictive Behaviors, 29(6), 1171–1175. [DOI] [PubMed] [Google Scholar]
- Johnson PS, Herrmann ES, & Johnson MW (2015). Opportunity costs of reward delays and the discounting of hypothetical money and cigarettes. Journal of the Experimental Analysis of Behavior, 103(1), 87–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn RE, Holmes C, Farley JP, & Kim-Spoon J. (2015). Delay Discounting Mediates Parent-Adolescent Relationship Quality and Risky Sexual Behavior for Low Self-Control Adolescents. Journal of Youth and Adolescence, 44(9), 1674–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, & Hoeppner B. (2015). A biaxial formulation of the recovery construct. Addiction Research & Theory, 23(1), 5–9. [Google Scholar]
- Khurana A, Romer D, Betancourt LM, Brodsky NL, Giannetta JM, & Hurt H. (2013). Working memory ability predicts trajectories of early alcohol use in adolescents: the mediational role of impulsivity. Addiction, 108(3), 506–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. (2014). World Health Organization Quality of Life (WHOQOL) Assessment. In Encyclopedia of Quality of Life and Well-Being Research (pp. 7260–7261). 10.1007/978-94-007-0753-5_3282 [DOI]
- Kirby KN, Winston GC, & Santiesteban M. (2005). Impatience and grades: Delay-discount rates correlate negatively with college GPA. Learning and Individual Differences, 15(3), 213–222. [Google Scholar]
- Koffarnus MN, & Bickel WK (2014). A 5-trial adjusting delay discounting task: accurate discount rates in less than one minute. Experimental and Clinical Psychopharmacology, 22(3), 222–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer KL, Maisto SA, Conigliaro J, McNeil M, Gordon AJ, & Kelley ME (2002). Decreased alcohol consumption in outpatient drinkers is associated with improved quality of life and fewer alcohol-related consequences. In Journal of General Internal Medicine (Vol. 17, Issue 5, pp. 382–386). 10.1007/s11606-002-0045-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Suchitra K-S, Brady R, Duhig AM, Anne S, Thomas L, Amanda M, Cavallo DA, Carroll KM, & Potenza MN (2007). Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug and Alcohol Dependence, 88(1), 79–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuerbis AN, Hagman BT, & Sacco P. (2013). Functioning of alcohol use disorders criteria among middle-aged and older adults: implications for DSM-5. Substance Use & Misuse, 48(4), 309–322. [DOI] [PubMed] [Google Scholar]
- Laudet AB (2007). What does recovery mean to you? Lessons from the recovery experience for research and practice. Journal of Substance Abuse Treatment, 33(3), 243–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB (2011). The case for considering quality of life in addiction research and clinical practice. Addiction Science & Clinical Practice, 6(1), 44–55. [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, & Stanick V. (2010). Predictors of motivation for abstinence at the end of outpatient substance abuse treatment. Journal of Substance Abuse Treatment, 38(4), 317–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R, Wirtz PW, Beattie MC, Noel N, & Stout R. (1995). Matching treatment focus to patient social investment and support: 18-month follow-up results. Journal of Consulting and Clinical Psychology, 63(2), 296–307. [DOI] [PubMed] [Google Scholar]
- Lookatch SJ, Wimberly AS, & McKay JR (2019). Effects of Social Support and 12-Step Involvement on Recovery among People in Continuing Care for Cocaine Dependence. Substance Use & Misuse, 54(13), 2144–2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, & Munafò MR (2011). Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology, 216(3), 305–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, & Kahler CW (2009). Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug and Alcohol Dependence, 104(3), 197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden GJ, & Bickel WK (2010). Impulsivity: The Behavioral and Neurological Science of Discounting. Amer Psychological Assn. [Google Scholar]
- Mazur JE (1987). An adjusting procedure for studying delayed reinforcement. Commons ML ; Mazur JE ; Nevin JA, 55–73. [Google Scholar]
- McKenna M, Chick J, Buxton M, Howlett H, Patience D, & Ritson B. (1996). The SECCAT survey: I. The costs and consequences of alcoholism. Alcohol and Alcoholism, 31(6), 565–576. [DOI] [PubMed] [Google Scholar]
- McLellan AT (2010). What Is Recovery? Revisiting the Betty Ford Institute Consensus Panel Definition. Journal of Social Work Practice in the Addictions, 10(1), 109–113. [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, & Kleber HD (2000). Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA: The Journal of the American Medical Association, 284(13), 1689–1695. [DOI] [PubMed] [Google Scholar]
- Mendlowicz MV (2000). Quality of Life in Individuals With Anxiety Disorders. In American Journal of Psychiatry (Vol. 157, Issue 5, pp. 669–682). 10.1176/appi.ajp.157.5.669 [DOI] [PubMed] [Google Scholar]
- Millson P, Challacombe L, Villeneuve PJ, Strike CJ, Fischer B, Myers T, Shore R, & Hopkins S. (2006). Determinants of health-related quality of life of opiate users at entry to low-threshold methadone programs. European Addiction Research, 12(2), 74–82. [DOI] [PubMed] [Google Scholar]
- Mischel W, Shoda Y, & Rodriguez MI (1989). Delay of gratification in children. Science, 244(4907), 933–938. [DOI] [PubMed] [Google Scholar]
- Mishra S, & Lalumière ML (2017). Associations Between Delay Discounting and Risk-Related Behaviors, Traits, Attitudes, and Outcomes. In Journal of Behavioral Decision Making (Vol. 30, Issue 3, pp. 769–781). 10.1002/bdm.2000 [DOI] [Google Scholar]
- Mitchell JM, Fields HL, D’Esposito M, & Boettiger CA (2005). Impulsive responding in alcoholics. Alcoholism, Clinical and Experimental Research, 29(12), 2158–2169. [DOI] [PubMed] [Google Scholar]
- Moos RH, Brennan PL, Schutte KK, & Moos BS (2010). Social and financial resources and high-risk alcohol consumption among older adults. Alcoholism, Clinical and Experimental Research, 34(4), 646–654. [DOI] [PubMed] [Google Scholar]
- Moos RH, & Moos BS (2007). Protective resources and long-term recovery from alcohol use disorders. Drug and Alcohol Dependence, 86(1), 46–54. [DOI] [PubMed] [Google Scholar]
- Morgan TJ, Morgenstern J, Blanchard KA, Labouvie E, & Bux DA (2003). Health-related quality of life for adults participating in outpatient substance abuse treatment. The American Journal on Addictions / American Academy of Psychiatrists in Alcoholism and Addictions, 12(3), 198–210. [PubMed] [Google Scholar]
- NIH. (2018). Drugs, Brains, and Behavior: The Science of Addiction. https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/treatment-recovery
- Paolacci G, Chandler J, & Ipeirotis PG (2010). Running Experiments on Amazon Mechanical Turk. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=1626226 [Google Scholar]
- Petry NM (2001). Delay discounting of money and alcohol in actively using alcoholics, currently abstinent alcoholics, and controls. Psychopharmacology, 154(3), 243–250. [DOI] [PubMed] [Google Scholar]
- Petry NM (2003). Discounting of money, health, and freedom in substance abusers and controls. Drug and Alcohol Dependence, 71(2), 133–141. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, & Hayes AF (2007). Addressing Moderated Mediation Hypotheses: Theory, Methods, and Prescriptions. Multivariate Behavioral Research, 42(1), 185–227. [DOI] [PubMed] [Google Scholar]
- Préau M, Protopopescu C, Spire B, Sobel A, Dellamonica P, Moatti J-P, Carrieri MP, & MANIF-2000 Study Group. (2007). Health related quality of life among both current and former injection drug users who are HIV-infected. Drug and Alcohol Dependence, 86(2–3), 175–182. [DOI] [PubMed] [Google Scholar]
- Puigdollers E, Domingo-Salvany A, Brugal MT, Torrens M, Alvarós J, Castillo C, Magrí N, Martín S, & Vázquez JM (2004). Characteristics of heroin addicts entering methadone maintenance treatment: quality of life and gender. Substance Use & Misuse, 39(9), 1353–1368. [DOI] [PubMed] [Google Scholar]
- Rockville MD (2010). Substance Abuse and Mental Health Services Administration Center for Substance Abuse Treatment. Center for Substance Abuse Treatment National Advisory Council. https://www.samhsa.gov/sites/default/files/meeting/minutes/csat-april2013-minutes.pdf [Google Scholar]
- Rubenis AJ, Fitzpatrick RE, Lubman DI, & Verdejo-Garcia A. (2018). Impulsivity predicts poorer improvement in quality of life during early treatment for people with methamphetamine dependence. Addiction, 113(4), 668–676. [DOI] [PubMed] [Google Scholar]
- Rudolf H, & Watts J. (2002). Quality of life in substance abuse and dependency. In International Review of Psychiatry (Vol. 14, Issue 3, pp. 190–197). 10.1080/09540260220144975 [DOI] [Google Scholar]
- Sheffer C, Christine S, James M, John M, Reid L, Lawrence C, Richard Y, Bryan J, Darren C, Maxine S, Lisa J, & Warren B. (2012). Delay Discounting, Locus of Control, and Cognitive Impulsiveness Independently Predict Tobacco Dependence Treatment Outcomes in a Highly Dependent, Lower Socioeconomic Group of Smokers. The American Journal on Addictions / American Academy of Psychiatrists in Alcoholism and Addictions, 21(3), 221–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheffer CE, Christensen DR, Landes R, Carter LP, Jackson L, & Bickel WK (2014). Delay discounting rates: A strong prognostic indicator of smoking relapse. Addictive Behaviors, 39(11), 1682–1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheffer CE, Miller A, Bickel WK, Devonish JA, O’Connor RJ, Wang C, Rivard C, & Gage-Bouchard EA (2018). The treasure of now and an uncertain future: Delay discounting and health behaviors among cancer survivors. Cancer, 124(24), 4711–4719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KW, & Larson MJ (2003). Quality of life assessments by adult substance abusers receiving publicly funded treatment in Massachusetts. The American Journal of Drug and Alcohol Abuse, 29(2), 323–335. [DOI] [PubMed] [Google Scholar]
- Snider SE, DeHart WB, Epstein LH, & Bickel WK (2019). Does delay discounting predict maladaptive health and financial behaviors in smokers? Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 38(1), 21–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanger C, Ryan SR, Fu H, Landes RD, Jones BA, Bickel WK, & Budney AJ (2012). Delay discounting predicts adolescent substance abuse treatment outcome. Experimental and Clinical Psychopharmacology, 20(3), 205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MD, Mulvey KP, Plough A, & Samet JH (1998). The functioning and well being of persons who seek treatment for drug and alcohol use. Journal of Substance Abuse, 10(1), 75–84. [DOI] [PubMed] [Google Scholar]
- Sullivan MC, Strainge L, Blackmon JE, Cruess SE, Wheeler D, & Cruess DG (2020). Assessing an Epidemic: Utility of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition Level 2 Substance Use Screener in Adult Psychiatric Inpatients. Journal of Addictions Nursing, 31(1), 9–16. [DOI] [PubMed] [Google Scholar]
- Suri S, & Watts DJ (2011). Cooperation and contagion in web-based, networked public goods experiments. PloS One, 6(3), e16836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate LM, Tsai P-F, Landes RD, Rettiganti M, & Lefler LL (2015). Temporal discounting rates and their relation to exercise behavior in older adults. Physiology & Behavior, 152(Pt A), 295–299. [DOI] [PubMed] [Google Scholar]
- The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. (1995). In Social Science & Medicine (Vol. 41, Issue 10, pp. 1403–1409). 10.1016/0277-9536(95)00112-k [DOI] [PubMed] [Google Scholar]
- Tompkins DA, Johnson PS, Smith MT, Strain EC, Edwards RR, & Johnson MW (2016). Temporal preference in individuals reporting chronic pain: discounting of delayed pain-related and monetary outcomes. Pain, 157(8), 1724–1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trompenaars FJ, Masthoff ED, Van Heck GL, De Vries J, & Hodiamont PP (2007). Relationships between social functioning and quality of life in a population of Dutch adult psychiatric outpatients. The International Journal of Social Psychiatry, 53(1), 36–47. [DOI] [PubMed] [Google Scholar]
- VanderBroek L, Acker J, Palmer AA, de Wit H, & MacKillop J. (2016). Interrelationships among parental family history of substance misuse, delay discounting, and personal substance use. Psychopharmacology, 233(1), 39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villeneuve PJ, Challacombe L, Strike CJ, Myers T, Fischer B, Shore R, Hopkins S, & Millson PE (2006). Change in health-related quality of life of opiate users in low-threshold methadone programs. In Journal of Substance Use (Vol. 11, Issue 2, pp. 137–149). 10.1080/14659890500256945 [DOI] [PubMed] [Google Scholar]
- Volkow ND (2010). Drugs, brains, and behavior: The science of addiction. Retrieved on March, 23, 2011. [Google Scholar]
- Volk RJ, Cantor SB, Steinbauer JR, & Cass AR (1997). Alcohol use disorders, consumption patterns, and health-related quality of life of primary care patients. Alcoholism, Clinical and Experimental Research, 21(5), 899–905. [PubMed] [Google Scholar]
- Wakaizumi K, Jabakhanji R, Ihara N, Kosugi S, Terasawa Y, Morisaki H, Ogaki M, & Baliki MN (2019). Altered functional connectivity associated with time discounting in chronic pain. Scientific Reports, 9(1), 8154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker ER, & Druss BG (2018). Mental and Addictive Disorders and Medical Comorbidities. Current Psychiatry Reports, 20(10), 86. [DOI] [PubMed] [Google Scholar]
- Wang FL, Pandika D, Chassin L, Lee M, & King K. (2016). Testing the Relations Among Family Disorganization, Delay Discounting, and Adolescent Alcohol Use: A Genetically Informed Study. Alcoholism, Clinical and Experimental Research, 40(4), 846–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washio Y, Higgins ST, Heil SH, McKerchar TL, Badger GJ, Skelly JM, & Dantona RL (2011). Delay discounting is associated with treatment response among cocaine-dependent outpatients. Experimental and Clinical Psychopharmacology, 19(3), 243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesley MJ, & Bickel WK (2014). Remember the future II: meta-analyses and functional overlap of working memory and delay discounting. Biological Psychiatry, 75(6), 435–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White W, Boyle M, & Loveland D. (2003). Behavioral Health Recovery Management: Transcending the Limitations of Addiction Treatment. Health Management, 23(3), 38–44. [Google Scholar]
- Wilson AG, George Wilson A, Franck CT, Terry Mueller E, Landes RD, Kowal BP, Yi R, & Bickel WK (2015). Predictors of delay discounting among smokers: Education level and a Utility Measure of Cigarette Reinforcement Efficacy are better predictors than demographics, smoking characteristics, executive functioning, impulsivity, or time perception. In Addictive Behaviors (Vol. 45, pp. 124–133). 10.1016/j.addbeh.2015.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon JH, & Higgins ST (2008). Turning k on its head: comments on use of an ED50 in delay discounting research. Drug and Alcohol Dependence, 95(1–2), 169–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon JH, Higgins ST, Heil SH, Sugarbaker RJ, Thomas CS, & Badger GJ (2007). Delay discounting predicts postpartum relapse to cigarette smoking among pregnant women. Experimental and Clinical Psychopharmacology, 15(2), 176–186. [DOI] [PubMed] [Google Scholar]
- Zywiak WH, Longabaugh R, & Wirtz PW (2002). Decomposing the relationships between pretreatment social network characteristics and alcohol treatment outcome. Journal of Studies on Alcohol, 63(1), 114–121. [PubMed] [Google Scholar]