Abstract
Introduction
Both collateral flow via the internal carotid artery (ICA) terminus (ICT) and initial mild symptoms might be associated with favorable outcomes in patients with acute ICA occlusion (ICAO). This study aimed to address the association between early clinical outcomes and patency of the ICT and middle cerebral artery (MCA) in patients with acute ICAO with mild symptoms.
Methods
Of 1,214 consecutive patients with acute ischemic stroke or transient ischemic attack due to large vessel occlusion, patients with ipsilateral ICAO and initial National Institutes of Health Stroke Scale (NIHSS) score ≤5 were retrospectively enrolled. We examined the associations between clinical factors including patency of the ICT and MCA and recurrence of stroke or early neurological deterioration (REND). Significant early neurological deterioration was defined as increment in NIHSS score ≥1 during hospital stay.
Results
Thirteen of the 35 patients who were finally enrolled had REND (37%), and median modified Rankin scale (mRS) score at discharge was 1 (interquartile range, 0–4). Initial NIHSS score (4 vs. 1, p < 0.001) and rates of diabetes mellitus (61.5% vs. 13.6%, p = 0.007), intravenous thrombolysis (IVT) (30.9% vs. 0%, p = 0.014), and mechanical thrombectomy (MT) (23.1% vs. 0%, p = 0.044) were significantly higher in patients with REND rather than in those without. The rate of patent ICT and MCA was comparable between groups. Except for 1 patient who underwent MT promptly after IVT immediately after REND, 3 patients initially treated with IVT deteriorated after the procedure. One patient without patent ICT and MCA did not meet the indications for MT. In 2 other patients with patent ICT and MCA, MT was not initially performed, but was eventually performed because of REND due to thrombus migration, and both were discharged with an mRS score of 5.
Conclusion
The overall clinical outcomes of patients with acute ICAO with mild symptoms were not depending on the patency of the ICT and MCA, but initial treatment with IVT alone might risk unfavorable outcomes due to thrombus migration in patients with patent ICT and MCA.
Keywords: Internal carotid artery terminus, Stroke, Low NIHSS, Large vessel occlusion
Introduction
Mechanical thrombectomy (MT) is an established and effective treatment for patients with acute large vessel occlusion (LVO) including internal carotid artery (ICA) occlusion (ICAO) [1]. However, the indications for MT in patients with LVO showing mild symptoms remain contentious because of uncertainty regarding treatment effectiveness [2]. On the other hand, various patterns of ICAO could affect the rate of revascularization success and subsequent clinical outcome [3]. ICAO with patent ICA terminus (ICT), which would be also called carotid-I occlusion [3] or isolated ICAO [4], shows reconstitution from the contralateral ICA via the proximal anterior cerebral artery and anterior communicating artery, or ipsilateral posterior cerebral artery via the posterior communicating artery. Although both collateral flow via patent ICT and initial mild symptoms might be associated with more favorable outcomes in the acute stage [5], early neurological deterioration was reported to be relatively common in patients with isolated ICAO [4]. Furthermore, it was also reported that early neurological deterioration after intravenous thrombolysis (IVT) was a frequent and highly deleterious in patients with isolated ICAO [6]. Although these past studies focus on the early clinical course in acute ICAO patients with both collateral flow via the ICT and initial mild symptoms, optimal indication of acute revascularization including IVT or MT for these patients has not been fully addressed. The present study aimed to clarify the effect of the patency of the ICA and the status of collateral flow to the ipsilateral middle cerebral artery (MCA) via the ICT on early clinical outcomes in patients with acute ICAO with mild symptoms, particularly in terms of the effectiveness of IVT, MT, or surgery, using data from the stroke registry of a single center.
Methods
Study Population
Subjects in the present study were retrospectively selected from 1,214 consecutive patients with acute ischemic stroke or transient ischemic attack (TIA) with LVO who were admitted to Kohnan Hospital (Sendai, Miyagi, Japan) within 24 h after onset between April 2006 and March 2018. Based on clinical and brain imaging findings, board-certified stroke neurologists specializing in the care of stroke patients made a diagnosis of ischemic stroke or TIA. The severity of neurological deficits was evaluated using the National Institutes of Health Stroke Scale (NIHSS) score on admission [7], and activities of daily living for patients before or after the onset of stroke were measured using the modified Rankin Scale (mRS) [8]. Clinical and investigative data were prospectively entered in a standardized fashion by stroke neurologists into the Kohnan Hospital Stroke Registry. Inclusion criteria for this study were as follows: (1) acute ischemic stroke or TIA due to ipsilateral ICAO; (2) NIHSS score ≤5 on admission; (3) mRS score ≤2 before stroke onset. We excluded patients based on the following criteria: (1) previous identification of occlusive disease in the ipsilateral ICA; (2) contraindications for performing magnetic resonance angiography (MRA); or (3) other circumstances considered as inappropriate by the investigators.
Data Collection and Definitions
In addition to general patient characteristics, including age, sex, cardiovascular risk factors, mRS score before onset, and initial NIHSS score, stroke classification according to the “Trial of ORG 10172 in Acute Stroke Treatment” (TOAST) [9], patency of the ICT and MCA on initial intracranial vascular imaging, and use of IVT or MT were also collected. We evaluated patency of the ICT and MCA according to signal intensity of the ICT and ipsilateral MCA on MRA. In our center, MRA was employed as the standard vascular imaging and could be performed immediately, 24 h a day, 7 days a week. MRA was usually performed just before or during IVT. Signal intensity of the MCA on MRA was qualitatively classified by a single investigator (R.I.) into 4 grades of “excellent,” “good,” “fair,” or “poor” [10]. In this study, patients with excellent or good signal intensity of the ipsilateral MCA and visualization of the ICT were defined as having patent ICT and MCA. Onset-to-door time was defined as the time from the last known time when the patient appeared well and free of index stroke symptoms to the time at which the patient arrived at the emergency room. The primary outcome was recurrence of stroke or early neurological deterioration (REND). Significant early neurological deterioration was defined as increment in NIHSS score ≥1 during hospital stay.
Statistical Analysis
We conducted univariate analysis to compare clinical and radiological characteristics between patients with and without REND. Categorical variables are presented as numbers and percentages and were analyzed using the χ2 test and Fisher's exact test, as appropriate. Continuous variables are expressed as median and interquartile range (IQR) and were analyzed using the Wilcoxon rank-sum test because of their non-normal distribution. All statistical analyses were performed using EZR software (Saitama Medical Center, Jichi Medical University, Saitama, Japan; http://www.jichi.ac.jp/saitama-sct/SaitamaHP.files/manual.html) [11], a graphical user interface for R (the R Foundation for Statistical Computing, Vienna, Austria). More precisely, EZR is a modified version of R Commander designed to add statistical functions frequently used in biostatistics. All reported p values are two-tailed, and values of p < 0.05 were considered statistically significant.
Results
Among the 1,214 patients who were initially screened, we selected all 49 patients with an initial NIHSS score of 0–5, ipsilateral ICAO, and premorbid mRS score 0–2. We then excluded 13 patients with known occlusive ICA disease before admission and 1 patient in whom MRA was obtained at the referring hospital. Finally, 35 patients (median age, 73 years [IQR, 55–79 years]; 24 males; median NIHSS score, 2 [IQR, 1–4]) were studied. As the primary outcome, 13 of the 35 patients (37%) had REND. Median mRS score at discharge was 1 (IQR, 0–4). We compared clinical and radiological characteristics and outcomes between patients with and without REND using univariate analyses (Table 1). Age, onset-to-door time, and rate of patent ICT and MCA were comparable between groups. Initial NIHSS score (4 vs. 1, p < 0.001) and rate of diabetes mellitus (61.5% vs. 13.6%, p = 0.007) were significantly higher in patients with REND than in those without. Moreover, the rate of IVT (30.9% vs. 0%, p = 0.014) and the rate of MT (23.1% vs. 0%, p = 0.044) were significantly higher in patients with REND than in those without. In patients with REND, mRS at discharge was significantly poorer than in those without (5 vs. 0, p < 0.001).
Table 1.
Univariate analysis comparing characteristics between patients with and without REND
| Characteristics | With REND (n = 13) | Without REND (n = 22) | p value |
|---|---|---|---|
| Age, years | 75 (65–858) | 63.5 (54–75.8) | 0.054 |
| Male | 8 (57.1) | 16 (76.2) | 0.28 |
| Hypertension | 11 (84.6) | 20 (90.9) | 0.62 |
| Dyslipidemia | 5 (38.5) | 11 (61.5) | 0.73 |
| Diabetes mellitus | 8 (61.5) | 3 (13.6) | 0.007 |
| Smoking | 9 (69.2) | 16 (76.2) | 0.70 |
| Heart disease as embolic source | 1 (11.1) | 5 (35.7) | 0.34 |
| Subtype classification | 0.15 | ||
| LAD | 8 (61.5) | 13 (59.1) | |
| CES | 3 (23.1) | 1 (4.5) | |
| Others | 2 (15.4) | 3 (13.6) | |
| TIA | 0 (0) | 5 (22.7) | |
| Initial NIHSS score | 4 (3–5) | 1 (0–2.8) | <0.001 |
| Onset-to-door time, min | 169 (80–420) | 340 (157.5–627.5) | 0.23 |
| Patent ICT and MCA | 8 (61.5) | 14 (63.6) | 1.00 |
| Systolic blood pressure on arrival, mm Hg | 155 (150–181) | 135 (130–170) | 0.16 |
| Diastolic blood pressure on arrival, mm Hg | 86 (78–101) | 75 (66–109) | 0.17 |
| IVT | 4 (30.9) | 0 (0) | 0.014 |
| MT | 3 (23.1) | 0 (0) | 0.044 |
| Bypass surgery | 2 (15.4) | 0 (0) | 0.13 |
| sICH | 0 (0) | 0 (0) | 1.00 |
| mRS at discharge | 5 (4–5) | 0 (0–1) | <0.001 |
Data are presented as number (%) or median (IQR). REND, recurrence of stroke or early neurological deterioration with increment in NIHSS score ≥1 during hospital stay; IQR, interquartile range; TOAST, Trial of ORG 10172 in Acute Stroke Treatment; LAD, large artery disease; CES, cardioembolic stroke; TIA, transient ischemic attack; NIHSS, National Institutes of Health Stroke Scale; ICT, internal carotid artery terminus; MCA, middle cerebral artery; IVT, intravenous thrombolysis; MT, mechanical thrombectomy; sICH, symptomatic intracranial hemorrhage; mRS, modified Rankin Scale.
Clinical characteristics and the clinical course of 13 patients with REND are shown in Table 2. All of 3 patients initially treated with IVT alone deteriorated within 24 h after IVT. On the other hand, in Case 11 with patent ICT and MCA, REND occurred just before initiating IVT and was promptly followed by MT 55 min after arrival (152 min from onset). One patient without patent ICT and MCA (Case 2) was not indicated for MT because of advanced age and insufficient evidence at the time, in 2008. In other 2 patients with patent ICT and MCA (Cases 7 and 13), MT was not initially performed because of low NIHSS on admission and good visualization of the ipsilateral MCA on MRA. Eventually, both patients were treated with MT because of REND suggesting thrombus migration several hours after IVT (599 and 470 min, respectively) and both were discharged with an mRS score of 5 (Fig. 1, 2).
Table 2.
Clinical characteristics and courses of patients treated with revascularization therapy including IVT, MT, or bypass surgery
| No. | Age | Sex | OTD | Stroke subtype | ICT and MCA | Initial NIHSS | Initial therapy (IVT time from onset | REND time from) onset | Rescue revascularization | mRS at discharge |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 48 | M | 280 min | LAD | Not patent | 5 | AT | Several days | None | 4 |
| 2 | 87 | F | 90 min | CES | Not patent | 5 | IVT (117 min) | 165 min | None | 6 |
| 3 | 45 | M | 50 min | Arterial dissection | Patent | 2 | AT | 250 min | None | 2 |
| 4 | 85 | M | 711 min | LAD | Patent | 5 | AT | Several days | None | 5 |
| 5 | 88 | F | 810 min | LAD | Not patent | 3 | AT | Several days | None | 5 |
| 6 | 84 | M | 80 min | LAD | Patent | 5 | AT | 1 day | None | 5 |
| 7 | 75 | M | 169 min | Aortogenic emboli | Patent | 4 | IVT (200 min) | 545 min | MT | 5 |
| 8 | 79 | M | 420 min | LAD | Patent | 5 | AT | 3 days | None | 4 |
| 9 | 61 | F | 60 min | LAD | Not patent | 0 | AT | 215 min | None | 5 |
| 10 | 65 | F | 980 min | LAD | Not patent | 4 | AT | 1 day | Bypass surgery | 5 |
| 11 | 85 | F | 100 min | CES | Patent | 4 | Not yet initiated | 110 min | IVT + MT | 0 |
| 12 | 74 | M | 270 min | LAD | Patent | 1 | AT | 1 day | Bypass surgery | 2 |
| 13 | 75 | M | 48 min | CES | Patent | 5 | IVT (135 min) | 435 min | MT | 5 |
IVT, intravenous thrombolysis; MT, mechanical thrombectomy; OTD, onset-to-door time; ICT, internal carotid artery terminus; MCA, middle cerebral artery; CES, cardioembolic stroke; LAD, large artery disease; NIHSS, National Institutes of Health Stroke Scale; AT, antithrombotic therapy; REND, recurrence of stroke or early neurological deterioration with increment in NIHSS score ≥1 during hospital stay; mRS, modified Rankin Scale.
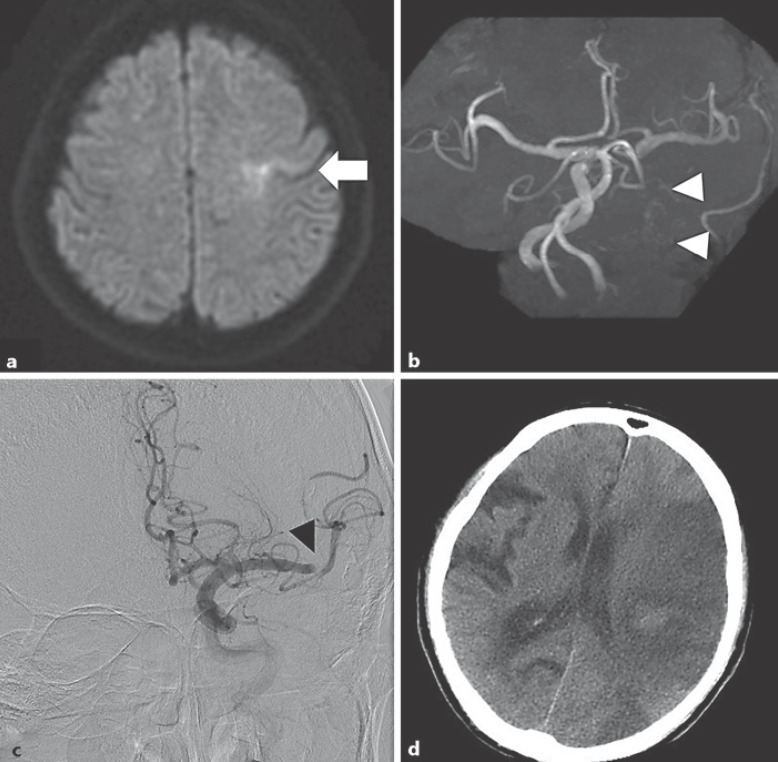
Fig. 1.
Case 7, a 75-year-old-man. He was initially treated with IVT alone 31 min after arrival (200 min from onset). a DWI shows acute infarct on the left precentral gyrus on the territory of the MCA (white arrow). b MRA shows ICAO with a patent ICT and MCA (white arrowheads). MT was withheld because of mild symptoms (NIHSS score 4) and patent ICT. Five hours after IVT, left visual acuity was completely lost, suggesting occlusion of the left ophthalmic artery due to thrombus migration. At 5 h 45 min after IVT (545 min after onset), he presented with global aphasia and right hemiplegia (NIHSS score 19). c Although emergent DSA initially showed occlusion of the intracranial ICA, subsequent imaging reveals occlusion of the left distal M1 MCA segment (black arrowhead). Immediate MT was performed using a Merci retriever, but significant recanalization was not obtained. d After MT, a large infarct in the MCA territory was confirmed. The patient was finally diagnosed with aortogenic brain embolism. IVT, intravenous thrombolysis; DWI, diffusion-weighted imaging; MCA, middle cerebral artery; ICAO, internal carotid artery occlusion; ICT, internal carotid artery terminus; MRA, magnetic resonance angiography; MT, mechanical thrombectomy; NIHSS, National Institutes of Health Stroke Scale; ICA, internal carotid artery; DSA, digital subtraction angiography.
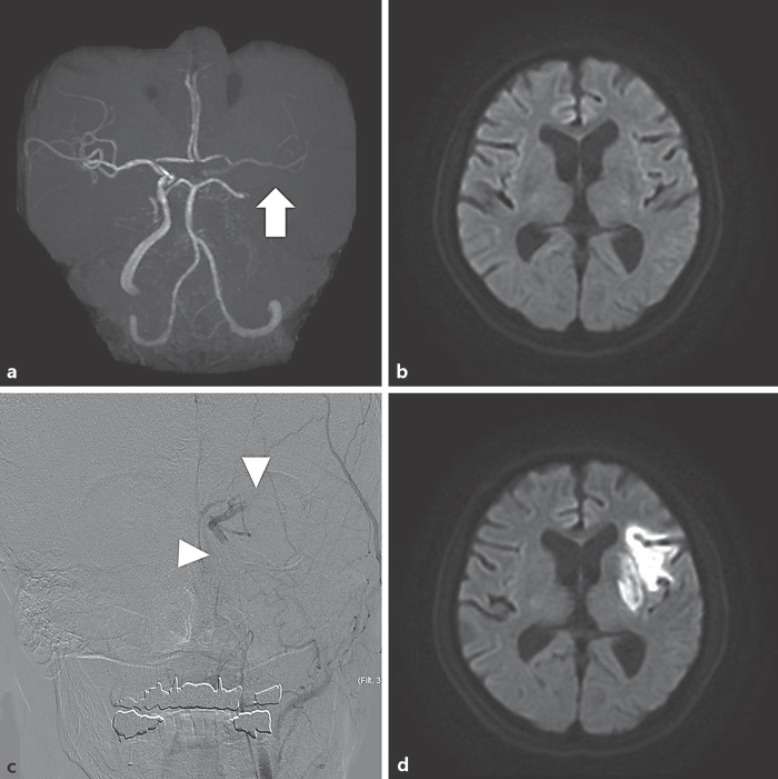
Fig. 2.
Case 13, a 75-year-old man. He was initially treated with IVT alone 27 min after arrival (135 min from onset). a Initial DWI shows no acute infarct. b MRA shows ICAO with a patent ICT and MCA. The signal from the ipsilateral MCA is weak but visible (white arrow). MT was withheld because of mild symptoms (NIHSS score 5) and patent ICT. At 300 min after IVT, he presented with global aphasia, conjugate deviation, and right hemiplegia (NIHSS score 22). c Emergent DSA shows left tandem ICAO (ICA and proximal M1 MCA segment) (white arrowheads). He was immediately treated with MT with a stent retriever, obtaining complete recanalization. d After MT, infarcts on the upper MCA territory are confirmed. Symptoms gradually improved, but clinical outcome at discharge was unfavorable because of aspiration pneumonia. IVT, intravenous thrombolysis; DWI, diffusion-weighted imaging; MRA, magnetic resonance angiography; ICAO, internal carotid artery occlusion; ICT, internal carotid artery terminus; MCA, middle cerebral artery; MT, mechanical thrombectomy; NIHSS, National Institutes of Health Stroke Scale; ICA, internal carotid artery; DSA, digital subtraction angiography.
Conclusion
In patients with acute ICAO and mild symptoms, we demonstrated that initial NIHSS score and rates of diabetes mellitus, IVT, and MT were significantly higher among patients with REND than among those without. Patency of the ICT and MCA was not associated with REND. The reason for the results might be that only patients with mild symptoms were enrolled. The initial symptoms might have more impact on early outcome rather than the status of collateral flow in patients with mild symptoms. However, all of 3 patients initially treated using IVT alone showed deterioration several hours after IVT. In 1 patient who was not indicated for MT, neurological deterioration might have been attributable to poor collaterals due to nonpatency of the ICT and MCA. In another 2 patients with patent ICT and MCA, neurological deterioration would have been caused by thrombus migration after IVT, and clinical outcomes were unfavorable despite rescue MT. In patients with acute ICAO with patent ICT and MCA and mild symptoms, initial treatment with IVT alone might lead to neurological deterioration and unfavorable outcomes due to thrombus migration.
The efficacy and safety of MT in patients with acute LVO and low NIHSS scores have not been established [2]. However, a sub-analysis of a large Japanese stroke registry reported that IVT, but not MT, was associated with favorable outcomes among acute LVO patients with low NIHSS scores [12]. On the other hand, it was reported that thrombus migration has been associated with prior IVT in patients with LVO [13]. Thrombus migration occurred spontaneously or during MT in 26% of patients with acute ICAO and patent MCA collateral flow, and was associated with worsened outcomes [14]. Furthermore, Boulenoir et al. [6] reported that early neurological deterioration after IVT occurred in 30% of isolated ICAO patients with mild symptoms and argued that thrombus fragmentation rather than collateral failure or extension of thrombus might be responsible for early neurological deterioration after IVT in these patients. Immediate MT for LVO in patients with low NIHSS scores has been suggested as potentially effective, as MT would prevent neurological deterioration [15]. Moreover, some studies have suggested that MT after the worsening of neurological symptoms in patients with initial mild symptoms could not be associated with favorable outcomes [16]. Although there was a patient treated by IVT and MT after REND who had a good outcome in our series (No. 11), REND occurred immediately after admission in this case. Immediate MT as well as IVT could be reasonable for patients with acute ICAO, even in patients with mild symptoms and patent ICT and MCA; however, there were no cases who underwent prompt MT irrespective of initial neurological symptoms in our series.
Thrombus migration or fragmentation after IVT could be more likely to occur in patients with embolic stroke, in which an embolus lodged in the extracranial ICA, than those with large artery disease (LAD) [6]; however, all patients who underwent IVT in this study were embolic stroke (3 cardioembolic stroke (CES) and 1 aortogenic brain embolism) (Table 2). On the other hand, in our series, 2 patients with REND (Cases 10 and 12, both with LAD, not treated by IVT) were treated using bypass surgery during the acute stage. As the first case occurred in 2011 and the second in 2015, sufficient evidence for the use of MT for acute LVO was lacking at the time both cases were treated. Other nonelderly patients in whom symptoms were also presumed to have been caused by atherosclerosis (Cases 1 and 9) might have met the indications for bypass surgery, but the efficacy of bypass surgery for patients with acute LVO due to intracranial atherosclerosis has not been established [17]. Consensus remains lacking on the optimal endovascular strategy for such cases [18].
We also showed that hyperglycemia was associated with REND in the present cohort. This result was compatible with our latest studies in patients with LVO and mild symptoms using a large Japanese stroke registry [12]. Moreover, hyperglycemia on admission is reportedly independently associated with increased incidence of symptomatic intracerebral hemorrhage and a decreased frequency of favorable outcomes at 90 days in patient with LVO, regardless of initial neurological symptoms [19].
Some limitations should be kept in mind when interpreting the results of this investigation. First, this study used data from a single center. It would be desirable to conduct a multicenter collaborative study. Second, we employed MRA as standard vascular imaging in this study, but this modality might underestimate the vascular patency of intracranial vessels compared to computed tomography angiography because MRA does not have as good spatial resolution as computed tomography angiography due to the strong association between signal intensity and blood flow. Therefore, it would be difficult to accurately evaluate by MRA cases in which the ICT was patent but horizontal segment of MCA was occluded, and such cases would be classified as “not patent ICT and MCA” in this study. Third, we could not enroll a sufficient number of participants in this study. The number of patients was thus too small to clarify associations between the effectiveness of vessel revascularization and patency of the ICT and MCA. The number of patients in a previous observational study on the outcome of isolated ICAO patients who underwent IVT was 74 [6]. Fourth, we could not obtain data on clinical outcomes at 90 days after symptom onset.
In conclusion, we have demonstrated that the overall clinical outcomes of patients with acute ICAO with mild symptoms were not depending on the patency of the ICT and MCA, but initial treatment with IVT alone might risk unfavorable outcomes due to thrombus migration in patients with patent ICT and MCA. Prospective studies using larger sample sizes are warranted to clarify the impact of the status of the ICT and MCA on clinical outcomes among patients with acute ICAO.
Statement of Ethics
The Kohnan Hospital Ethics Committee approved the study protocol in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan (280926). Due to the retrospective nature of the study, the need for written informed consent was waived based on the approval of the Kohnan Hospital Ethics Committee.
Conflict of Interest Statement
Ryo Itabashi received honoraria from Bayer, Bristol Myers Squibb, Amgen, Takeda, Tanabe Mitsubishi Parma, Daiichi Sankyo, Boehringer Ingelheim, Eisai, Pfizer, Kyowa Kirin, Stryker, GE Healthcare, Nestle, Otsuka Pharmaceutical, Boston Scientific, and Medtronic, and received research support not attributed in the manuscript from Boehringer Ingelheim. Yukako Yazawa received honoraria for lecture fees from Bayer, Bristol Myers Squibb, Daiichi Sankyo, Stryker, and Medtronic. Takuya Saito, Yuichi Kawabata, and Yuya Kobayashi report no disclosure.
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author Contributions
Ryo Itabashi: data acquisition, data analysis, and writing of the manuscript. Takuya Saito, Yuichi Kawabata, Yuya Kobayashi, and Yukako Yazawa: data acquisition and critical revision of the manuscript.
Data Availability Statement
The data that support the findings of this study are not publicly available due to legal regulation in Japan regarding the privacy of research participants but are available from the corresponding author (R. I.) on reasonable request and with approval from the co-authors and the Kohnan Hospital Ethics Committee. Further inquiries can be directed to the corresponding author.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Goyal M, Menon BK, van Zwam WH, Dippel DWJ, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016 Apr 23;387((10029)):1723–1731. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 2.McCarthy DJ, Tonetti DA, Stone J, Starke RM, Narayanan S, Lang MJ, et al. More expansive horizons: a review of endovascular therapy for patients with low NIHSS scores. J Neurointerv Surg. 2021 Feb;13((2)):146–151. doi: 10.1136/neurintsurg-2020-016583. [DOI] [PubMed] [Google Scholar]
- 3.Liebeskind DS, Flint AC, Budzik RF, Xiang B, Smith WS, Duckwiler GR, et al. Carotid I's, L's and T's: collaterals shape the outcome of intracranial carotid occlusion in acute ischemic stroke. J Neurointervent Surg. 2015 Jun;7((6)):402–407. doi: 10.1136/neurintsurg-2014-011231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khazaal O, Natalie N, Acton EK, Husain MR, Kung D, Cucchiara B, et al. Early neurologic deterioration with symptomatic Isolated internal carotid artery occlusion: a cohort study, systematic review, and meta-analysis. Stroke Vasc Interv Neurol. 2022;0:e000219. doi: 10.1161/svin.121.000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim JT, Park MS, Choi KH, Nam TS, Choi SM, Cho KH. Clinical implications of collateral middle cerebral artery flow in acute ischaemic stroke with internal carotid artery occlusion. Eur J Neurol. 2011 Dec;18((12)):1384–1390. doi: 10.1111/j.1468-1331.2011.03415.x. [DOI] [PubMed] [Google Scholar]
- 6.Boulenoir N, Turc G, Henon H, Laksiri N, Mounier-Véhier F, Girard Buttaz I, et al. Early neurological deterioration following thrombolysis for minor stroke with isolated internal carotid artery occlusion. Eur J Neurol. 2021 Feb;28((2)):479–490. doi: 10.1111/ene.14541. [DOI] [PubMed] [Google Scholar]
- 7.Lyden P, Brott T, Tilley B, Welch KM, Mascha EJ, Levine S, et al. Improved reliability of the NIH stroke Scale using video training. NINDS TPA stroke study group. Stroke. 1994 Nov;25((11)):2220–2226. doi: 10.1161/01.str.25.11.2220. [DOI] [PubMed] [Google Scholar]
- 8.van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988 May;19((5)):604–607. doi: 10.1161/01.str.19.5.604. [DOI] [PubMed] [Google Scholar]
- 9.Adams HP, Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993 Jan;24((1)):35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 10.Hirooka R, Ogasawara K, Inoue T, Fujiwara S, Sasaki M, Chida K, et al. Simple assessment of cerebral hemodynamics using single-slab 3D time-of-flight MR angiography in patients with cervical internal carotid artery steno-occlusive diseases: comparison with quantitative perfusion single-photon emission CT. AJNR Am J Neuroradiol. 2009 Mar;30((3)):559–563. doi: 10.3174/ajnr.A1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transpl. 2013 Mar;48((3)):452–458. doi: 10.1038/bmt.2012.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saito T, Itabashi R, Yazawa Y, Uchida K, Yamagami H, Sakai N, et al. Clinical outcome of patients with large vessel occlusion and low National Institutes of Health Stroke Scale scores. Stroke. 2020 May;51((5)):1458–1463. doi: 10.1161/STROKEAHA.119.028562. [DOI] [PubMed] [Google Scholar]
- 13.Alves HC, Treurniet KM, Jansen IGH, Yoo AJ, Dutra BG, Zhang G, et al. Thrombus migration paradox in patients with acute ischemic stroke. Stroke. 2019 Nov;50((11)):3156–3163. doi: 10.1161/STROKEAHA.119.026107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koge J, Matsumoto S, Nakahara I, Ishii A, Hatano T, Tanaka Y, et al. Impact of thrombus migration on clinical outcomes in patients with internal carotid artery occlusions and patent middle cerebral artery. J Neurol Sci. 2020 May 15;412:116737. doi: 10.1016/j.jns.2020.116737. [DOI] [PubMed] [Google Scholar]
- 15.Haussen DC, Bouslama M, Grossberg JA, Anderson A, Belagage S, Frankel MR, et al. Too good to intervene? Thrombectomy for large vessel occlusion strokes with minimal symptoms: an intention-to-treat analysis. J Neurointerv Surg. 2017 Oct;9((10)):917–921. doi: 10.1136/neurintsurg-2016-012633. [DOI] [PubMed] [Google Scholar]
- 16.Messer MP, Schonenberger S, Mohlenbruch MA, Pfaff J, Herweh C, Ringleb PA, et al. Minor stroke syndromes in large-vessel occlusions: mechanical thrombectomy or thrombolysis only? AJNR Am J Neuroradiol. 2017 Jun;38((6)):1177–1179. doi: 10.3174/ajnr.A5164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kanematsu R, Kimura T, Ichikawa Y, Inoue T. Safety of urgent STA-MCA anastomosis after intravenous rt-PA treatment: a report of five cases and literature review. Acta Neurochir. 2018 Sep;160((9)):1721–1727. doi: 10.1007/s00701-018-3576-y. [DOI] [PubMed] [Google Scholar]
- 18.Chang Y, Kim BM, Bang OY, Baek JH, Heo JH, Nam HS, et al. Rescue stenting for failed mechanical thrombectomy in acute ischemic stroke: a multicenter experience. Stroke. 2018 Apr;49((4)):958–964. doi: 10.1161/STROKEAHA.117.020072. [DOI] [PubMed] [Google Scholar]
- 19.Yazawa Y, Ohira T, Itabashi R, Uchida K, Sakai N, Yamagami H, et al. Association of admission hyperglycemia with clinical outcomes in Japanese patients with acute large vessel occlusion stroke: a post hoc analysis of the recovery by endovascular salvage for cerebral ultra-acute embolism Japan registry 2. Cerebrovasc Dis. 2021;50((1)):12–19. doi: 10.1159/000511679. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are not publicly available due to legal regulation in Japan regarding the privacy of research participants but are available from the corresponding author (R. I.) on reasonable request and with approval from the co-authors and the Kohnan Hospital Ethics Committee. Further inquiries can be directed to the corresponding author.