Abstract
Introduction:
The association between e-cigarette use and chronic bronchitis, emphysema, and chronic obstructive pulmonary disease (COPD) has not been studied thoroughly, particularly in populations defined by concomitant combustible smoking status.
Methods:
Using pooled 2016 and 2017 data from the Behavioral Risk Factor Surveillance System, investigators studied 705,159 participants with complete self-reported information on e-cigarette use, combustible cigarette use, key covariates, and chronic bronchitis/emphysema/COPD. Current e-cigarette use was the main exposure, with current use further classified as daily or occasional use. The main outcome was defined as reported ever having a diagnosis of chronic bronchitis/emphysema/COPD. For all analyses, multivariable adjusted logistic regression was used, with the study population stratified by combustible cigarette use status (never, former, or current). All analyses were conducted in 2019.
Results:
Of 705,159 participants, 25,175 (3.6%) were current e-cigarette users, 64,792 (9.2%) current combustible cigarette smokers, 207,905 (29.5%) former combustible cigarette smokers, 432,462 (61.3%) never combustible cigarette smokers, and 14,036 (2.0%) dual users of e-cigarettes and combustible cigarettes. A total of 53,702 (7.6%) participants self-reported chronic bronchitis/emphysema/COPD. Among never combustible cigarette smokers, current e-cigarette use was associated with 75% higher odds of chronic bronchitis/emphysema/COPD compared with never e-cigarette users (OR=1.75, 95% CI=1.25, 2.45), with daily users of e-cigarettes having the highest odds (OR=2.64, 95% CI=1.43, 4.89). Similar associations between e-cigarette use and chronic bronchitis/emphysema/COPD were noted among both former and current combustible cigarette smokers.
Conclusions:
Results suggest possible e-cigarette-related pulmonary toxicity across all categories of combustible cigarette smoking status, including those who had never smoked combustible cigarettes.
INTRODUCTION
More than a decade ago, e-cigarettes were introduced in the U.S. market; since then, their prevalence has grown rapidly.1,2 In 2016, an estimated 10.8 million U.S. adults used e-cigarettes. Of these, about 1.9 million were sole e-cigarette users.1,3 Although there are many varieties of e-cigarettes, most devices contain a nicotine cartridge, a vaporization chamber, and a rechargeable lithium battery that delivers an aerosolized product containing flavored liquids and nicotine to the lungs of the user when inhaled.4,5 Currently, these products are being marketed as less harmful substitutes for combustible cigarettes as well as smoking-cessation devices.1 However, neither the acute nor the chronic health effects of e-cigarettes have been well studied. As most e-cigarettes contain nicotine and flavoring chemicals, generating a variety of harmful or potentially harmful substances,2 they theoretically could affect a variety of different organ systems and their function. However, of these potential health effects, pulmonary toxicity is perhaps most immediate, given that the lung is the primary site of exposure to e-cigarette aerosols. The theoretical basis for e-cigarette aerosols exerting potential pulmonary toxicity is supported by a range of in vitro and in vivo studies as well as data from human e-cigarette users.6,7
For example, data from several acute exposure studies in animals and human epithelial cells suggest that exposure to e-cigarette liquids or aerosol extracts could potentially lead to increased airway reactivity, impaired anti-microbial defenses, and destruction of lung tissue.8–12 In animal models, inhalation of e-cigarettes has also been found to change the mechanical properties of the lung and increase pulmonary oxidative stress and inflammatory responses, leading to increased expression of cytokines such as monocyte chemoattractant protein-1 (MCP-1) and interleukin 1B.8–12 Despite this, there is scant evidence linking pulmonary toxicity to e-cigarette use in humans.13,14 In one study, current e-cigarette use in adolescents was found to be associated with a twofold increased risk of bronchitic symptoms compared with never users.15 A large, cross-sectional, population-based study performed within the Obstructive Lung Disease in Northern Sweden study and West Sweden Asthma Study found that respiratory symptoms were generally more common among e-cigarette users. E-cigarette use was significantly associated with respiratory symptoms among dual users (OR=4.03, 95% CI=3.23, 5.02).16
In addition, results from the large, nationally representative Population Assessment of Tobacco and Health study showed that e-cigarette use was associated with an increased odds of chronic obstructive pulmonary disease (COPD).17 Despite these suggestive data, the long-term health effects of e-cigarettes require additional investigation, not only to develop a robust evidence base related to their relative harm/benefit, but also to develop effective regulatory and advisory approaches to minimize their potential health burden.1 Therefore, this study examines the association between e-cigarette use and self-reported chronic bronchitis/emphysema/COPD across differing combustible cigarette smoking use patterns in the Behavioral Risk Factor Surveillance System (BRFSS), the largest U.S. survey of e-cigarette use to date.
METHODS
Study Sample
For this study, data were pooled from the 2016 and 2017 BRFSS annual surveys. The BRFSS is the largest, representative, annual, cross-sectional, telephone-based survey that obtains data on health-related risk behaviors and chronic medical conditions from U.S. adult participants aged ≥18 years.18 The BRFSS is a public data set and therefore did not require IRB review. The median survey response rate for all states, territories, and Washington DC in 2016 was 47.0%, ranging from 30.7% to 65.0%. In 2017, the response rate was 45.1%, ranging from 30.6% to 64.1%.19,20 Of 936,319 participants in the BRFSS, 705,159 participants with complete information on all key variables were included in this study.
Measures
In the survey, the participants were asked: Have you ever used an e-cigarette or other electronic “vaping” product, even just one time, in your entire life? Participants who answered yes were then asked: Do you now use e-cigarettes or other electronic “vaping” products every day, some days, or not at all? Participants who responded no to the first question were categorized as never e-cigarette users. Current e-cigarette users who used e-cigarettes every day and some days were categorized as daily or occasional e-cigarette users, respectively.
Participants who responded yes to Have you smoked at least 100 cigarettes in your entire life? were categorized as ever smokers, and participants who responded no were classified as never cigarette smokers. Among ever smokers, participants who answered every day or some days to the question: Do you now smoke cigarettes every day, some days, or not at all? were classified as current cigarette smokers. Participants who answered not at all were classified as former cigarette smokers.
The income variable from BRFSS was adjusted using the federal poverty levels in the U.S. for 2016 and 2017.21 Age, sex, race, and level of education were self-reported.
Participants who responded yes to Has a doctor, nurse, or other health professional ever told you that you have chronic obstructive pulmonary disease or COPD, emphysema, or chronic bronchitis were categorized as having the outcome of interest.13
Statistical Analysis
The authors used the BRFSS weighting methodology according to Centers for Disease Control and Prevention guidelines to maintain national representativeness of the data.22 Baseline characteristics were summarized across never and current e-cigarette use categories.
Multivariable logistic regression models stratified by combustible cigarette smoking status were used to assess the association between e-cigarette use and COPD. The models were adjusted for age, sex, race, federal poverty line–adjusted income level, and educational status. The reference group in each stratum of combustible cigarette smoking status was never e-cigarette users. Additional interactive analysis was conducted by using never combustible cigarette smokers who never used e-cigarette as the sole reference group with which different combinations of e-cigarette and combustible cigarette use was compared. Additional models exploring effect modification by sex were explored. All analyses were conducted in 2019.
RESULTS
Of the 705,159 participants, 25,175 (3.6%) were current e-cigarette users, 64,792 (9.2%) current combustible cigarette smokers, and 207,905 (29.5%) former combustible cigarette smokers. A total of 432,462 (61.3%) never smoked combustible cigarettes, 14,036 (2.0%) were dual users of e-cigarettes and combustible cigarettes; 53,702 (7.6%) participants self-reported COPD. The median age group of current e-cigarette users was 30–34 years (Table 1). Compared with never e-cigarette users, current e-cigarette users were more likely to be men, white, and current combustible cigarette users.
Table 1.
Baseline Characteristics of the Study Population According to E-cigarette Use, BRFSS 2016 and 2017, N=705,159
| Variables | E-cigarette use status | |
|---|---|---|
| Current (N=25,175) |
Never (N=679,984) |
|
| Median age group, years | 30–34 | 50–54 |
| Women, % | 40.6 | 53.9 |
| Race | ||
| White, % | 71.7 | 63.1 |
| Black, % | 8.2 | 11.3 |
| Asian, % | 3.5 | 5.5 |
| Hispanic, % | 11.4 | 17.4 |
| Others, % | 5.2 | 2.7 |
| Education | ||
| Less than high school diploma, % | 14.3 | 13.6 |
| High school diploma, % | 35.5 | 26.5 |
| Some college, % | 50.2 | 59.9 |
| Federal poverty line | ||
| <100%, % | 17.5 | 13.4 |
| 100%−200%, % | 23.5 | 19.7 |
| >200%, % | 59.0 | 66.9 |
| Combustible cigarette use | ||
| Never smoker, % | 18.5 | 67.7 |
| Former smoker, % | 29.5 | 24.5 |
| Current smoker, % | 52.0 | 7.8 |
| Chronic bronchitis/emphysema/c ônic obstructive pulmonary disease, % | 11.1 | 5.6 |
BRFSS, Behavioral Risk Factor Surveillance System.
Across all categories of combustible cigarette smoking status, there was a significant association between e-cigarette use and COPD (Table 2). In comparison with never e-cigarette users, current e-cigarette use was associated with 75% higher odds of COPD (OR=1.75, 95% CI=1.25, 2.45). Among never combustible cigarette smokers, daily use of e-cigarettes was associated with the highest odds of COPD (OR=2.64, 95% CI=1.43, 4.89) compared with never e-cigarette users. Among former combustible cigarette smokers, current e-cigarette users had higher odds of COPD compared with never e-cigarette users (OR=2.13, 95% CI=1.82, 2.50). In the additional analysis with never combustible cigarette smokers who never used e-cigarette as the sole reference group (Figure 1), dual users of combustible cigarette and e-cigarettes had the highest odds of the outcome of interest (OR=6.89, 95% CI=6.29, 7.55). The association between e-cigarette use and COPD was modified by sex (p<0.001), with stronger associations observed in women. Stratified analysis by sex are available in the supplements (Appendix Tables 1 and 2).
Table 2.
Association Between E-cigarette Use and COPD According to Combustible Cigarette Smoking Among U.S. Adults, Pooled BRFSS 2016 and 2017a
| Combustible cigarette smoking status | |||
|---|---|---|---|
| E-cigarette use status | Never smoker (N=432,462) |
Former smoker (N=207,905) |
Current smoker (N=64,792) |
| OR (95%CI) | OR (95%CI) | OR (95%CI) | |
| Never e-cigarette users | ref | ref | ref |
| Current e-cigarette users | 1.75 (1.25, 2.45) | 2.13 (1.82, 2.50) | 1.66 (1.50, 1.84) |
| Occasional use | 1.51 (1.03, 2.23) | 2.30 (1.71, 3.08) | 1.67 (1.50, 1.86) |
| Daily use | 2.64 (1.43, 4.89) | 2.05 (1.72, 2.44) | 1.64 (1.34, 2.00) |
Adjusted for age, sex, race, educational status, and income.
BRFSS, Behavioral Risk Factor Surveillance System; COPD, chronic obstructive pulmonary disease.
Figure 1.
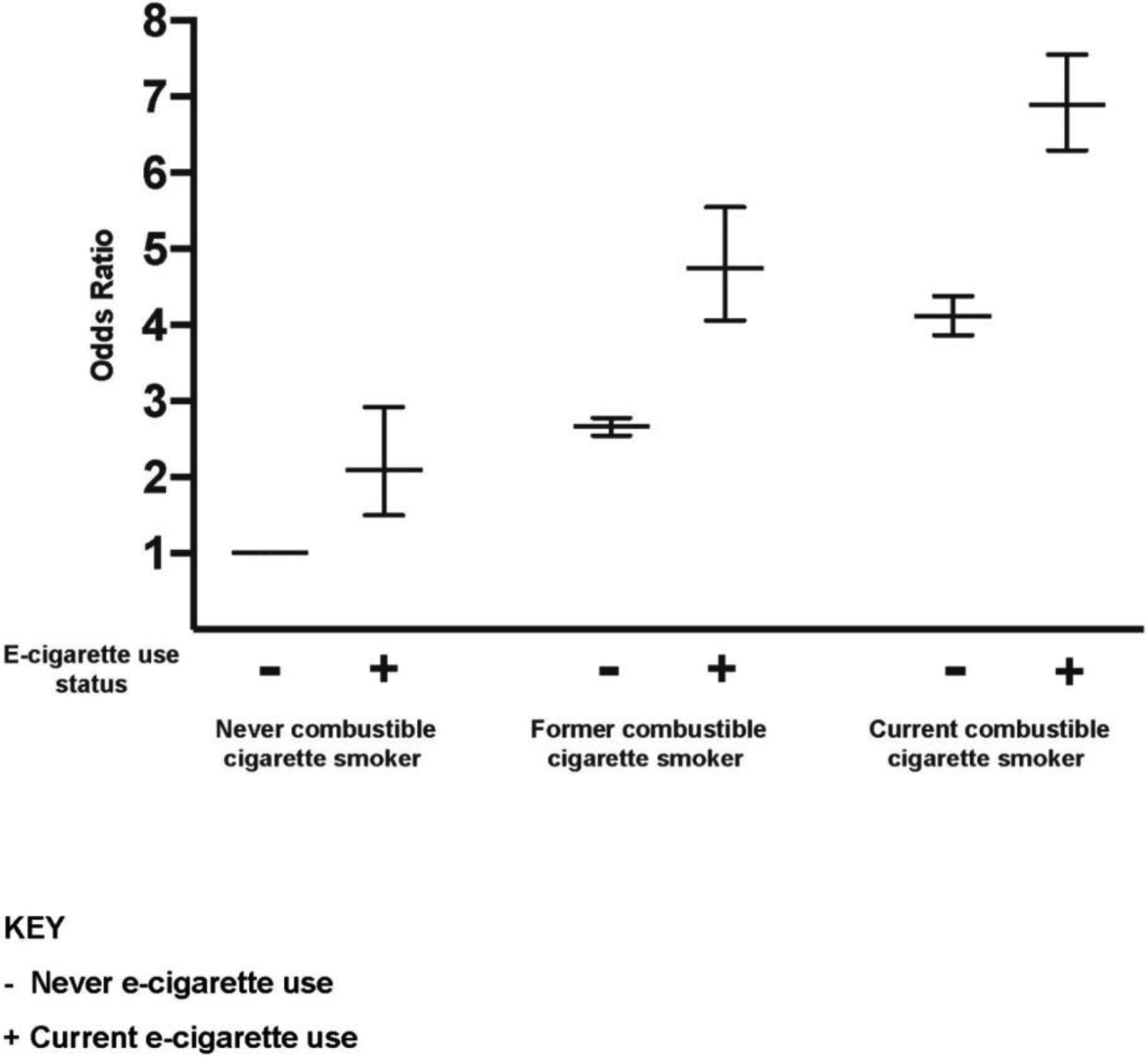
Association between e-cigarette use and COPD according to combustible cigarette smoking among U.S. adults with never e-cigarette and never combustible cigarette use as the reference group.
Notes: Adjusted for age, sex, race, educational status, and income.
COPD, chronic obstructive pulmonary disease.
DISCUSSION
The major finding from this cross-sectional study is that there is a significant association between e-cigarette use and COPD across all categories of combustible cigarette smoking status. Perhaps most importantly, the authors found a stepped increase in odds of the outcome with increasing frequency of e-cigarette use among never combustible cigarette smokers. This stepped relationship is intriguing, and should be explored in future studies where more fine-grained analysis of e-cigarette intensity is available. Additionally, the association between e-cigarette use and COPD was modified by sex.
Previous work has shown that e-cigarettes alter innate defense proteins in respiratory secretions in a manner similar to combustible cigarettes. Using induced sputum samples, Reidel et al.23 demonstrated that levels of innate defense proteins associated with COPD, such as elastase and matrix mellatoproteinase-9, were significantly increased in e-cigarette users. Potential e-cigarette-related impact on lung physiology is also supported by a range of evidence showing that in vitro exposure of lung cells to either e-cigarette aerosol extract or e-cigarette liquids alters membrane ion conductance and impedance, ciliary beat frequency, and induces oxidative stress and inflammation. For instance, using an air–liquid interface, Lerner and colleagues10 found that exposure of human airway epithelial cells to ENDS resulted in elevated secretion of inflammatory cytokines, such as interleukins 6 and 8, denoting inflammatory changes that could lead to undesirable health effects. Similar inflammatory responses have been documented in animal models exposed to e-cigarette aerosols via inhalation.8,9
Although there are only limited data related to pulmonary responses in human e-cigarette use, some studies have found that individuals using e-cigarettes report chronic bronchitis, and that the use of e-cigarettes is associated with an increase in airway resistance. Previous analysis of the Population Assessment of Tobacco and Health study by Perez et al.17 showed that in e-cigarette users who were nonsmokers, the prevalence of COPD was 3.0% (95% CI=2.7, 3.4). Using propensity-matched groups composed of e-cigarette and non-e-cigarette users, they showed that e-cigarette users had 1.43 higher odds (95% CI=1.12, 1.85) of having COPD than non-users. The present study extended these observations by exploring this association among differing combustible cigarette smoking groups, demonstrating similar strengths of association across all categories. In addition, this analysis shows that the use of e-cigarettes is associated with pulmonary toxicity even among never combustible cigarette smokers.
The notion that the use of e-cigarettes could compromise lung physiology and function is further supported by the analysis of the 2016 Hawaii BRFSS, which showed that e-cigarette use is significantly associated with chronic pulmonary disorder (OR=2.58, 95% CI=1.36, 4.89), with stronger associations among adult nonsmokers.13 This is significant, for even though smoking combustible cigarettes is robustly associated with COPD,24 these emergent data may also implicate sole e-cigarette use with COPD risk. In addition, the present analysis also shows that dual users of e-cigarettes and combustible cigarettes, the most common e-cigarette use pattern,1 had the highest odds of COPD when compared with individuals who have never used either of these products. These observations suggest that the use of e-cigarettes may actually act additively with smoking combustible cigarettes to promote the pathophysiology of COPD.
In a previous analysis of the BRFSS data set, the authors found that 60% of e-cigarette users without a history of combustible cigarette smoking are younger than age 25 years.3 Therefore, sole e-cigarette users may represent a new category of users who may have a unique risk profile. The analysis in this specific category of users who had never smoked combustible cigarettes showed that there was a significant association between e-cigarette use and COPD. Moreover, the frequency of e-cigarette in this population was associated with a graded increase in odds of the outcome.
That there is significant risk of pulmonary injury in sole e-cigarette users is further supported by a study among adolescents, which demonstrated twofold odds of bronchitic symptoms among current e-cigarette users compared with never e-cigarette users (OR=2.02, 95% CI=1.42, 2.88).15 Wang and colleagues25 reported a strong association of respiratory symptoms with e-cigarettes observed among never smokers (OR=2.06, 95% CI=1.24, 3.42). A cross-sectional study among high school students showed an association between e-cigarette use and asthma among even among never smokers (OR=2.74, 95% CI=1.30, 5.78), reporting more absences from school because of asthma.26
Taken together, this evidence suggests that sole e-cigarette use may play a significant role in the development of pulmonary injury or dysfunction. If further confirmed, these findings are significant because e-cigarette use is popular among never combustible cigarette smokers as it is viewed as a less harmful substitute for combustible cigarettes.1 Therefore, this study strengthens the rationale for conducting comprehensive longitudinal studies to assess the safety of e-cigarettes. The study also demonstrates that the association between e-cigarette use and COPD is modified by sex, consistent with previous studies that showed sex-specific differences in the manifestation of COPD.27 Some studies have suggested potential reasons for sex differences in COPD manifestation, which may include differential susceptibility to tobacco, behavioral, anatomic, and hormonal factors. However, these findings should be explored in longitudinal studies.28
These results should be considered cautiously as they are derived from national survey data without direct evaluation of lung function. However, they do represent important hypothesis-generating evidence that, when placed in context, constitutes a strong rationale for the future study of potential e-cigarette-related pulmonary toxicity at the population level. Importantly, these data have important potential public health and regulatory implications. In 2016, the U.S. Food and Drug Administration issued the “Deeming Rule” extending its regulatory authority to e-cigarettes.29 The findings from this study, therefore, provide useful and up-to-date data to the Food and Drug Administration that may provide rationale for future regulatory science and actions in the field of pulmonary health effects.
Limitations
Despite the many strengths related to the analysis of a large nationally representative data set with sufficient statistical power to permit stratification by smoking status, this study has several limitations. In BRFSS, the exposures and outcomes were self-reported and may both be misclassified in a nonrandom fashion, with participants with self-reported COPD potentially being more likely to classify themselves as former combustible cigarette smokers or current e-cigarette users. The cross-sectional data used in this analysis also limit causal inferences. It is difficult to establish if the outcome of interest occurs before or after e-cigarette exposure. Additionally, data on combustible cigarette smoking intensity or burden (pack years) were not systematically available in BRFSS; however, these confounding variables would only be relevant to analysis of former and current combustible cigarette smokers. BRFSS also lacks detailed data on burden, duration, and intensity of e-cigarette use.
In addition, the authors cannot exclude the possibility that reverse causation may have contributed to the finding of the highest odds of COPD among dual users when compared with never combustible cigarette smokers who never use e-cigarettes. For example, current and former combustible cigarette smokers with the outcome of interest are potentially more likely to report using e-cigarette as a smoking-cessation strategy. However, the findings of a significant association between e-cigarette use and COPD among never combustible cigarette smokers makes reverse causation as the sole explanation of these findings unlikely. Finally, the e-cigarette device type and flavorings used were not available in this study, which could significantly impact both the dose and the nature of the potential relationship between lung physiology and e-cigarette use.
CONCLUSIONS
Data from the largest nationally representative survey on health-related risk factors and chronic medical conditions show potential e-cigarette-related pulmonary toxicity regardless of combustible cigarette use status, with graded increase in odds of COPD with increasing frequency of e-cigarette use among never combustible cigarette smokers. These findings provide a robust rationale and a strong scientific premise for conducting longitudinal studies to explore pulmonary risk associated with the use of e-cigarette use, particularly in those individuals who have never smoked combustible tobacco products.
Supplementary Material
ACKNOWLEDGMENTS
American Heart Association Tobacco Regulation and Addiction Center, 2U54HL120163, which is funded by the U.S. Food and Drug Administration and National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, the Food and Drug Administration or the American Heart Association.
Dr. DeFilippis receives grant funding related to tobacco research from the NIH. He has unrelated research funding from NIH and Astra Zeneca and is a consultant on an unrelated topic for Radiometer America, Inc. No other financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Mirbolouk M, Charkhchi P, Kianoush S, et al. Prevalence and distribution of e-cigarette use among U.S. adults: Behavioral Risk Factor Surveillance System, 2016. Ann Intern Med. 2018;169(7):429‒438. 10.7326/m17-3440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhatnagar A, Whitsel LP, Ribisl KM, et al. Electronic cigarettes: a policy statement from the American Heart Association. Circulation. 2014;130(16):1418‒1436. 10.1161/CIR.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mirbolouk M, Charkhchi P, Orimoloye OA, et al. E-cigarette use without a history of combustible cigarette smoking among U.S. adults: Behavioral Risk Factor Surveillance System, 2016. Ann Intern Med. 2019;170(1):76‒79. 10.7326/m18-1826. [DOI] [PubMed] [Google Scholar]
- 4.Qasim H, Karim ZA, Rivera JO, Khasawneh FT, Alshbool FZ. Impact of electronic cigarettes on the cardiovascular system. J Am Heart Assoc. 2017;6(9):e006353. 10.1161/jaha.117.006353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129(19):1972‒1986. 10.1161/circulationaha.114.007667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chun LF, Moazed F, Calfee CS, Matthay MA, Gotts JE. Pulmonary toxicity of e-cigarettes. Am J Physiol Cell Mol Physiol. 2017;313(2):L193‒L206. 10.1152/ajplung.00071.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glantz SA, Bareham DW. E-cigarettes: use, effects on smoking, risks, and policy implications. Annu Rev Public Health. 2018;39:215‒235. 10.1146/annurev-publhealth-040617-013757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garcia-Arcos I, Geraghty P, Baumlin N, et al. Chronic electronic cigarette exposure in mice induces features of COPD in a nicotine-dependent manner. Thorax. 2016;71(12):1119‒1129. 10.1136/thoraxjnl-2015-208039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sussan TE, Gajghate S, Thimmulappa RK, et al. Exposure to electronic cigarettes impairs pulmonary anti-bacterial and anti-viral defenses in a mouse model. PLoS One. 2015;10(2):e0116861. 10.1371/journal.pone.0116861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lerner CA, Sundar IK, Yao H, et al. Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. PLoS One. 2015;10(2):e0116732. 10.1371/journal.pone.0116732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martin EM, Clapp PW, Rebuli ME, et al. E-cigarette use results in suppression of immune and inflammatory-response genes in nasal epithelial cells similar to cigarette smoke. Am J Physiol Cell Mol Physiol. 2016;311(1):L135‒L144. 10.1152/ajplung.00170.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hwang JH, Lyes M, Sladewski K, et al. Electronic cigarette inhalation alters innate immunity and airway cytokines while increasing the virulence of colonizing bacteria. J Mol Med. 2016;94(6):667‒679. 10.1007/s00109-016-1378-3. [DOI] [PubMed] [Google Scholar]
- 13.Wills TA, Pagano I, Williams RJ, Tam EK. E-cigarette use and respiratory disorder in an adult sample. Drug Alcohol Depend. 2019;194:363‒370. 10.1016/j.drugalcdep.2018.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Academies of Sciences, Engineering, and Medicine, Stratton KR, Kwan LY, Eaton DL. Public Health Consequences of E-Cigarettes. Washington, DC: The National Academies Press; 2018. 10.17226/24952. [DOI] [PubMed] [Google Scholar]
- 15.McConnell R, Barrington-Trimis JL, Wang K, et al. Electronic cigarette use and respiratory symptoms in adolescents. Am J Respir Crit Care Med. 2017;195(8):1043‒1049. 10.1164/rccm.201604-0804oc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hedman L, Backman H, Stridsman C, et al. Association of electronic cigarette use with smoking habits, demographic factors, and respiratory symptoms. JAMA Netw Open. 2018;1(3):e180789. 10.1001/jamanetworkopen.2018.0789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perez MF, Atuegwu NC, Mead EL, Oncken C, Mortensen EM. Adult e-cigarettes use associated with a self-reported diagnosis of COPD. Int J Environ Res Public Health. 2019;16(20):3938. 10.3390/ijerph16203938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.CDC. About BRFSS. www.cdc.gov/brfss/about/index.htm. Accessed August 22, 2018.
- 19.CDC. Behavioral Risk Factor Surveillance Ssystem 2016 Summary Data Quality Report. www.cdc.gov/brfss/annual_data/2016/pdf/2016-sdqr.pdf. Published 2017. Accessed September 26, 2018.
- 20.CDC. The Behavioral Risk Factor Surveillance System 2017 Summary Data Quality Report. www.cdc.gov/brfss/annual_data/2017/pdf/2017-sdqr-508.pdf. Published 2018. Accessed September 26, 2018.
- 21.Federal Register. Annual Update of the HHS Poverty Guidelines. www.federalregister.gov/documents/2017/01/31/2017-02076/annual-update-of-the-hhs-poverty-guidelines. Published 2017. Accessed October 1, 2018.
- 22.CDC. Behavioral Risk Factor Surveillance System: Weighting BRFSS Data, BRFSS 2016. www.cdc.gov/brfss/annual_data/2016/pdf/weighting_the-data_webpage_content.pdf. Published 2016. Accessed August 30, 2018.
- 23.Reidel B, Radicioni G, Clapp PW, et al. E-cigarette use causes a unique innate immune response in the lung, involving increased neutrophilic activation and altered mucin secretion. Am J Respir Crit Care Med. 2018;197(4):492‒501. 10.1164/rccm.201708-1590oc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lundbäck B, Lindberg A, Lindström M, et al. Not 15 but 50% of smokers develop COPD?—Report from the Obstructive Lung Disease in Northern Sweden Studies. Respir Med. 2003;97(2):115‒122. 10.1053/rmed.2003.1446. [DOI] [PubMed] [Google Scholar]
- 25.Wang MP, Ho SY, Leung LT, Lam TH. Electronic cigarette use and respiratory symptoms in Chinese adolescents in Hong Kong. JAMA Pediatr. 2016;170(1):89. 10.1001/jamapediatrics.2015.3024. [DOI] [PubMed] [Google Scholar]
- 26.Cho JH, Paik SY. Association between electronic cigarette use and asthma among high school students in South Korea. PLoS One. 2016;11(3):e0151022. 10.1371/journal.pone.0151022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kamil F, Pinzon I, Foreman MG. Sex and race factors in early-onset COPD. Curr Opin Pulm Med. 2013;19(2):140‒144. 10.1097/mcp.0b013e32835d903b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aryal S, Diaz-Guzman E, Mannino DM. COPD and gender differences: an update. Transl Res. 2013;162(4):208‒218. 10.1016/j.trsl.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 29.Restrictions on the Sale and Distribution of Tobacco Products and Required Warning Statements for Tobacco Products; Final Rule. Fed Regist. 2016;90(81). www.gpo.gov/fdsys/pkg/FR-2016-05-10/pdf/2016-10685.pdf. Accessed October 31, 2018. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


