Abstract
Purpose
Rosacea is a common facial dermatosis, with flares induced by exposome factors. M89PF containing Vichy mineralizing water, probiotic fractions, hyaluronic acid, niacinamide and tocopherol repairs the skin barrier and reinforces skin defences against exposome factors. This study assessed the benefit of M89PF in subjects with rosacea associated with erythema and sensitive skin during the Covid-19 pandemic using protective face masks.
Methods
M89PF was compared to usual skin care in a randomized, split-face study, for 30 days in subjects with rosacea associated with erythema and sensitive skin. Clinical evaluations included erythema, desquamation, skin tightness, dryness, burning sensation, itching, stinging, stinging test, and local tolerability. Instrument evaluations included erythema, skin hydration and TEWL. Subject satisfaction was also assessed.
Results
Erythema significantly improved with M89PF at both time points (p<0.01 at D15, and p<0.001 at D30). Skin sensitivity assessed by the skin stinging test improved significantly (p<0.01) with M89PF at D30, compared to baseline and usual skin care. Skin erythema, tightness, dryness, hydration and TEWL significantly improved (p≤0.05) with M89PF at D15 and D30, versus baseline and the untreated side. Subjects were highly satisfied with M89PF at D15 and D30. Tolerance was very good in all subjects.
Conclusion
In subjects with rosacea, M89PF significantly reduces erythema, skin tightness, dryness and TEWL, and improves skin hydration and skin sensitivity, even when using protective masks. M89PF is well tolerated and received high satisfaction ratings.
ClinicalTrials.gov. No
Keywords: rosacea, skin barrier, exposome, erythema, sensitive skin
Introduction
Rosacea is a common chronic inflammatory skin disease characterized by persistent erythema associated with periodical intensification or “flares”. Other clinical features, such as flushing, papules, pustules and telangiectasia may also be observed.1 Its course is irregular, with periods of flares and remission.2 In rosacea, immune-mediated inflammatory pathways involve mast cells and macrophages, as well as the release of proinflammatory mediators.3,4 Moreover, TLR-2 is overexpressed on keratinocytes and on infiltrating dermis cells.5,6 This enhances skin sensitivity to exposome factors and the production of proinflammatory mediators by keratinocytes.7,8 TLR-2 activates the NLRP3 inflammasome and causes cell death.9,10 Components of the inflammasome worsen or activate other proinflammatory factors, such as IL-8, TNF-α and MMPs leading to further worsening of the condition.7,11
Rosacea patients frequently report skin sensitivity symptoms such as skin burning, itching, stinging/tingling and often feel embarrassed and stigmatized, adding psychosocial burden to the visible features.12,13 Some of these symptoms have been described as secondary features of rosacea in the recently published phenotype classification.1
Exposome factors, which may be environmental such as friction when wearing protective masks, can lead to alterations in the skin barrier and skin defence functions.14–17 As a results skin sensitivity may be exacerbated and rosacea worsen leading to further discomfort.18–20
Recently, two investigations confirmed the benefit of M89PF in the management of acute stressed skin.21,22
M89PF (Mineral 89 Probiotic Fractions, Laboratoires Vichy International, France) contains Vichy volcanic mineralizing water (VVMW), probiotic fractions of Vitreoscilla filiformis (VfeV), hyaluronic acid (HA), niacinamide and tocopherol. M89PF has been developed to repair the skin barrier and to reinforce skin defences impacted by exposome factors, thus reducing stress on the skin. It is hypoallergenic and contains no perfume, thus being suitable for subjects with rosacea.
The objective of this study was to assess the efficacy and tolerability of M89PF in subjects with rosacea associated with erythema and sensitive skin in the context of the Covid-19 pandemic and wearing protective masks.
Materials and Methods
This single-centre, split-face, randomized, controlled clinical trial was conducted within the context of the Covid-19 pandemic, with subjects wearing face masks between January and March 2021, and adhered to the principles of Good Clinical Practices and the declaration of Helsinki. According to Italian regulatory guidelines, this type of trial testing marketed cosmetics does not require approval from local ethics committees. However, the local ethics committee of Milan/Italy was informed about this study and subjects provided written informed consent prior to participation. The study is registered in the ClinicalTrials.gov database (NCT05562661).
Adult subjects with rosacea associated with erythema and less than 3 papules or pustules and having sensitive skin (positive 15% lactic acid sting test) received randomly either M89PF or continued the use of their non-medical cosmetic standard skin care on one of the half-face sides. Products were to be applied twice daily for 30 days.
Instrumental evaluations included a Chromameter (Chromameter CR400®, Konica Minolta, Tokyo, Japan) for erythema, a corneometer (Corneometer CM825®, Courage & Khazaka, Cologne, Germany) for evaluating skin hydration, and a tewameter (Tewameter TM 300® MDD 4, Cologne, Germany) for assessing transepidermal water loss (TEWL).
Subjects assessed skin tightness, dryness, burning sensation, itching and stinging on a scale of 0 = none to 10 = very severe. Subject satisfaction was assessed at D15 and D30.
Clinical evaluations at baseline, Day 15 and Day 30 included a visual assessment of erythema and desquamation on a scale from 0 = none to 10 = very severe. Lactic acid skin stinging tests were performed on Day 15 and Day 30. Demodex density was assessed at baseline and D30, using the SSSB method.23
Local tolerability was assessed throughout the study.
Mean values, standard deviations and variations were calculated. Instrumental data at baseline, Day 15 and Day 30 were compared using the ANOVA and the Bonferroni Tests. Variations at Day 15-baseline and Day 30-baseline in the M89PF-treated areas and in those having received the usual skin care were compared using the t-test. Scores of the clinical evaluation and the stinging test at baseline, Day 15 and Day 30 were compared using the Friedman ANOVA and Kendall’s Concordance Coefficient. Variations at Day 15-baseline, Day 30-baseline and the Demodex density on both half-face sides were compared using the Wilcoxon test for non-parametric and dependent data. The significance level was set at 5%. For each subject satisfaction question, the number of answers given for each level of intensity was given as a percentage.
Results
Twenty adult subjects aged between 20 and 60 years with a phototype I to III were included. Subjects wore a face mask for a mean time of 4.4 hours/day (1–8 hours).
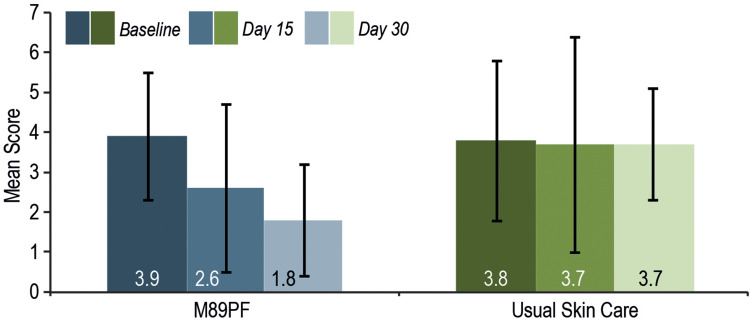
Skin sensitivity significantly improved with M89PF compared to baseline, Day 15 (−1.3%, p<0.01) and at Day 30 (−2.1%, p<0.0001) and was significantly improved versus usual skin care side at Day 30 (Figure 1).
Figure 1.
Skin sensitivity at baseline, Day 15 and Day 30. M89PF significantly (p<0.0001) reduced skin sensitivity as early as Day 15.
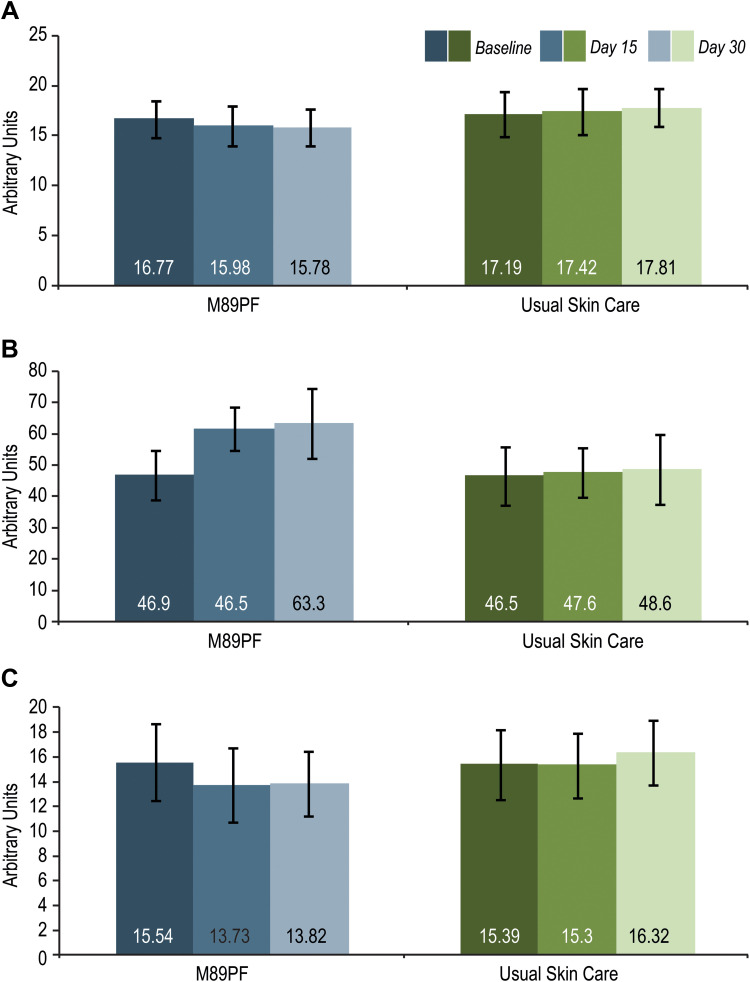
On the M89PF-treated side, erythema measured by chromameter (Figure 2A) had significantly improved compared to baseline at Day 15 (−4.7%, p<0.05) and Day 30 (−5.9%, p<0.01). The difference between M89PF and the usual skin care side was statistically significant in favour of M89PF at Day 15 (p<0.01) and Day 30 (p<0.001).
Figure 2.
Instrumental assessments at baseline, Day 15 and Day 30. M89PF significantly (p<0.0001) improved erythema, skin hydration and transepidermal water loss as early as Day 15 compared to the standard skin care. (A) Erythema. (B) Skin hydration. (C) Transepidermal water loss.
Skin hydration measured (Figure 2B), and TEWL (Figure 2C) significantly improved versus baseline with M89PF at Day 15 (+31.3%, −11.6%, for skin hydration and TEWL, respectively, both p≤0.05) and Day 30 (+35.0% and −11.1%, respectively, both p≤0.01) and were significantly better on the M89PF side as early as Day 15 (Day 15: p≤0.05, Day 30: p<0.01). No significant change over time was observed on the usual skin care side.
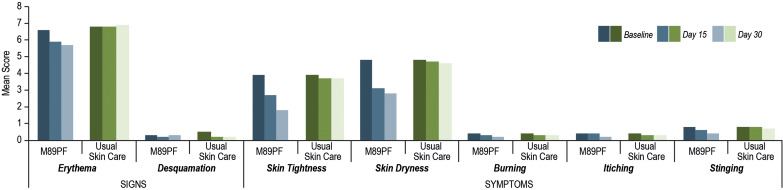
When assessed clinically by the dermatologist or self-evaluated by patients, skin erythema, skin tightness and skin dryness significantly (all p≤0.05) improved from Day 15 until Day 30 on the M89PF side, compared to the usual skin care side (Figure 3). No difference over time was observed with the usual skin care.
Figure 3.
Clinical signs and symptom scores at baseline, Day 15 and Day 30. M89Pf significantly (p<0.0001) reduced clinical signs and symptoms as early as Day 15.
A significantly (p<0.01) lower mean Demodex density was observed on the M89PF side (0.6±0.8 Demodex/cm²) compared to the usual care side (1.2±0.9 Demodex/cm²) after 30 days of daily use.
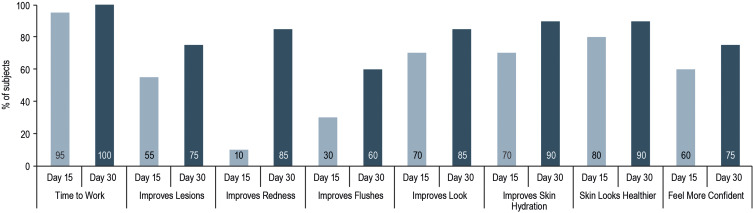
Patient satisfaction increased between Day 15 and Day 30 for all items questioned. After 30 days of daily use, 80% of the subjects were satisfied or very satisfied with M89PF, 90% would consider using the product again, 75% would recommend it, 90% would continue using it, all would integrate M89PF in their daily routine and no subject was bothered by eventual side effects. Detailed results per item are provided in Figure 4.
Figure 4.
Subject satisfaction after 15 and 30 days of use of M89PF.
The local tolerance of M89PF was excellent.
Discussion and Conclusion
This half-face randomized study shows that in subjects with rosacea, the daily use of M89PF significantly improves skin sensitivity, erythema, skin tightness and skin dryness sensations after 15 and 30 days of treatment, compared to usual skin care products. Subjects were highly satisfied with M89PF and all would reuse it.
M89PF significantly reduced TEWL and correspondingly improved skin hydration, confirming the restoration of the natural skin barrier. Moreover, it improved patient-reported symptoms including stinging, erythema, tightness and dryness of the skin as early as after 15 days of use, with a continued benefit up to 30 days, when compared to standard skin care regimens. Besides, the mean Demodex density was significantly (p<0.01) reduced on the M89PF side compared to the usual care side after 30 days of daily use. This may be of particular interest as it confirms that in rosacea the natural skin barrier is damaged leading to an overgrowth of Demodex, considered to be a trigger of rosacea and that a specifically developed dermocosmetic such as M89PF may help to decrease the density of Demodex.24
VVMW originates from a French volcanic region and contains 15 minerals with a total mineral concentration of 5.2g/l. These minerals reinforce the natural defences of the skin by restoring the natural skin barrier, stimulating antioxidant activity and reducing inflammation, commonly observed in subjects with rosacea.22,25,26 Probiotic fractions have been reported to play a potential role in the management of inflammatory skin diseases.27,28 M89PF contains VfeV in a medium containing VVMW and cultured by a fermentation process to obtain an extract. Topically applied VfeV extract regulated immunity by optimising the regulatory cell function, protecting against infection, and helped skin barrier function for improved recovery and resistance and thus potentially reduces the density of Demodex.20,29 In vitro studies showed that in normal human epidermal keratinocyte cultures, the combination of 10% VVMW and 0.002% VfeV significantly increased transglutaminase, filaggrin, involucrin, claudin-1, and zonula occludens-1 in comparison with the controls.21 Tocopherol or vitamin E is a well-known antioxidant.30 Niacinamide has anti-oxidant and anti-inflammatory properties and reduces oedema. It also improves skin barrier function by stimulating skin differentiation markers and reduces transepidermal water loss (TEWL) to improve skin hydration.28,31 Hyaluronic acid is the predominant component of the extracellular matrix with viscoelastic and hygroscopic properties, a unique capacity to retain skin moisture, and is involved in skin repair mechanisms.32
In rosacea, the natural skin barrier is impaired. The use of dermocosmetics before and during treatment, and as part of a maintenance regimen helps to improve clinical signs and symptoms of rosacea.33 In this study of subjects with rosacea associated with erythema and skin sensitivity, the dermocosmetic M89PF improves signs and symptoms and reduces the Demodex density.
In conclusion, in subjects with rosacea, M89PF significantly reduces erythema, skin tightness, dryness and TEWL, and improves skin hydration within 15 days, as well as skin sensitivity after 30 days. M89PF is well tolerated and received high satisfaction ratings.
Acknowledgments
The authors acknowledge the editorial assistance of Karl Patrick Göritz, Scientific and Medical Writing Services, France.
Funding Statement
This study was funded by Laboratories Vichy International, a L’Oreal company.
Data Sharing Statement
Enzo Berardesca, the corresponding author will share upon reasonable request for 1 year after publication of this manuscript the study protocol and all data collected and statistically analysed and in relationship with this study, except deidentified participant data.
Disclosure
Adriana Bonfigli and Claudia Cartigliani are affiliated with ISPE. Delphine Kerob is an employee of Cosmetic Active International, France (a L’Oreal company). Jerry Tan is an advisor, consultant and speaker for Cosmetic Active International, France (a L’Oreal company). He also reports personal fees from Vichy, during the conduct of the study; personal fees from La Roche Posay, Vichy, and Galderma, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- 1.Thiboutot D, Anderson R, Cook-Bolden F, et al. Standard management options for rosacea: the 2019 update by the National Rosacea Society Expert Committee. J Am Acad Dermatol. 2020;82(6):1501–1510. doi: 10.1016/j.jaad.2020.01.077 [DOI] [PubMed] [Google Scholar]
- 2.Powell FC. The histopathology of rosacea: “where’s the beef?”. Dermatology. 2004;209:173–174. doi: 10.1159/000079884 [DOI] [PubMed] [Google Scholar]
- 3.Salamon M, Sysa-Jedrzejowska A, Lukamowicz J, Lukamowicz M, Swiatkowska E, Wozniacka A. Stężenie wybranych cytokin w surowicy pacjentów z trądzikiem różowatym [Concentration of selected cytokines in serum of patients with acne rosacea]. Przegl Lek. 2008;65(9):371–374. Polish. [PubMed] [Google Scholar]
- 4.Holmes AD, Spoendlin J, Chien AL, Baldwin H, Chang ALS. Evidence-based update on rosacea comorbidities and their common physiologic pathways. J Am Acad Dermatol. 2018;78(1):156–166. doi: 10.1016/j.jaad.2017.07.055 [DOI] [PubMed] [Google Scholar]
- 5.Yamasaki K, Kanada K, Macleod DT, et al. TLR2 expression is increased in rosacea and stimulates enhanced serine protease production by keratinocytes. J Invest Dermatol. 2011;131(3):688–697. doi: 10.1038/jid.2010.351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moura AKA, Guedes F, Rivitti-Machado MC, Sotto MN. Innate immunity in rosacea. Langerhans cells, plasmacytoid dendritic cells, Toll-like receptors and inducible oxide nitric synthase (iNOS) expression in skin specimens: case-control study. Arch Dermatol Res. 2018;310(2):139–146. doi: 10.1007/s00403-018-1806-z [DOI] [PubMed] [Google Scholar]
- 7.Holmes AD, Steinhoff M. Integrative concepts of rosacea pathophysiology, clinical presentation and new therapeutics. Exp Dermatol. 2017;26(8):659–667. doi: 10.1111/exd.13143 [DOI] [PubMed] [Google Scholar]
- 8.Hari A, Flach TL, Shi Y, Mydlarski PR. Toll-like receptors: role in dermatological disease. Mediators Inflamm. 2010;2010:437246. doi: 10.1155/2010/437246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harijith A, Ebenezer DL, Natarajan V. Reactive oxygen species at the crossroads of inflammasome and inflammation. Front Physiol. 2014;5:352. doi: 10.3389/fphys.2014.00352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tschopp J, Schroder K. NLRP3 inflammasome activation: the convergence of multiple signalling pathways on ROS production? Nat Rev Immunol. 2010;10:210–215. doi: 10.1038/nri2725 [DOI] [PubMed] [Google Scholar]
- 11.Casas C, Paul C, Lahfa M, et al. Quantification of Demodex folliculorum by PCR in rosacea and its relationship to skin innate immune activation. Exp Dermatol. 2012;21(12):906–910. doi: 10.1111/exd.12030 [DOI] [PubMed] [Google Scholar]
- 12.Cardwell LA, Nyckowski T, Uwakwe LN, Feldman SR. Coping mechanisms and resources for patients suffering from rosacea. Dermatol Clin. 2018;36(2):171–174. doi: 10.1016/j.det.2017.11.013 [DOI] [PubMed] [Google Scholar]
- 13.Halioua B, Cribier B, Frey M, Tan J. Feelings of stigmatization in patients with rosacea. J Eur Acad Dermatol Venereol. 2017;31(1):163–168. doi: 10.1111/jdv.13748 [DOI] [PubMed] [Google Scholar]
- 14.Dreno B, Bettoli V, Araviiskaia E, Sanchez Viera M, Bouloc A. The influence of exposome on acne. J Eur Acad Dermatol Venereol. 2018;32(5):812–819. doi: 10.1111/jdv.14820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Passeron T, Krutmann J, Andersen ML, Katta R, Zouboulis CC. Clinical and biological impact of the exposome on the skin. J Eur Acad Dermatol Venereol. 2020;34(Suppl 4):4–25. doi: 10.1111/jdv.16614 [DOI] [PubMed] [Google Scholar]
- 16.Stefanovic N, Flohr C, Irvine AD. The exposome in atopic dermatitis. Allergy. 2020;75(1):63–74. doi: 10.1111/all.13946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Passeron T, Zouboulis CC, Tan J, et al. Adult skin acute stress responses to short-term environmental and internal aggression from exposome factors. J Eur Acad Dermatol Venereol. 2021;35(10):1963–1975. doi: 10.1111/jdv.17432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Damiani G, Gironi LC, Grada A, et al. COVID-19 related masks increase severity of both acne (maskne) and rosacea (mask rosacea): multi-center, real-life, telemedical, and observational prospective study. Dermatol Ther. 2021;34(2):e14848. doi: 10.1111/dth.14848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chiriac AE, Wollina U, Azoicai D. Flare-up of rosacea due to face mask in healthcare workers during COVID-19. Maedica. 2020;15(3):416–417. doi: 10.26574/maedica.2020.15.3.416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gueniche A, Nielsen M. Introduction to probiotic fractions and Vichy volcanic mineralizing water: two key ingredients for stressed skin. J Eur Acad Dermatol Venereol. 2022;36(Suppl 2):3–4. doi: 10.1111/jdv.17783 [DOI] [PubMed] [Google Scholar]
- 21.Gueniche A, Valois A, Kerob D, Rasmont V, Nielsen M. A combination of Vitreoscilla filiformis extract and Vichy volcanic mineralizing water strengthens the skin defenses and skin barrier. J Eur Acad Dermatol Venereol. 2022;36(Suppl 2):16–25. doi: 10.1111/jdv.17786 [DOI] [PubMed] [Google Scholar]
- 22.Rasmont V, Valois A, Gueniche A, et al. Vichy volcanic mineralizing water has unique properties to strengthen the skin barrier and skin defenses against exposome aggressions. J Eur Acad Dermatol Venereol. 2022;36(Suppl 2):5–15. doi: 10.1111/jdv.17784 [DOI] [PubMed] [Google Scholar]
- 23.Forton F, Seys B. Density of Demodex folliculorum in rosacea: a case-control study using standardized skin-surface biopsy. Br J Dermatol. 1993;128(6):650–659. doi: 10.1111/j.1365-2133.1993.tb00261.x [DOI] [PubMed] [Google Scholar]
- 24.Chang YS, Huang YC. Role of Demodex mite infestation in rosacea: a systematic review and meta-analysis. J Am Acad Dermatol. 2017;77(3):441–7.e6. doi: 10.1016/j.jaad.2017.03.040 [DOI] [PubMed] [Google Scholar]
- 25.Tacheau C, Weisgerber F, Fagot D, et al. Vichy Thermal Spring Water (VTSW), a cosmetic ingredient of potential interest in the frame of skin ageing exposome: an in vitro study. Int J Cosmet Sci. 2018;40(4):377–387. doi: 10.1111/ics.12470 [DOI] [PubMed] [Google Scholar]
- 26.Salsberg J, Andriessen A, Abdulla S, et al. A review of protection against exposome factors impacting facial skin barrier function with 89% mineralizing thermal water. J Cosmet Dermatol. 2019;18(3):815–820. doi: 10.1111/jocd.12927 [DOI] [PubMed] [Google Scholar]
- 27.Knackstedt R, Knackstedt T, Gatherwright J. The role of topical probiotics in skin conditions: a systematic review of animal and human studies and implications for future therapies. Exp Dermatol. 2020;29(1):15–21. doi: 10.1111/exd.14032 [DOI] [PubMed] [Google Scholar]
- 28.Gueniche A, Valois A, Salomao Calixto L, et al. A dermocosmetic formulation containing Vichy volcanic mineralizing water, Vitreoscilla filiformis extract, niacinamide, hyaluronic acid, and vitamin E regenerates and repairs acutely stressed skin. J Eur Acad Dermatol Venereol. 2022;36(Suppl 2):26–34. doi: 10.1111/jdv.17785 [DOI] [PubMed] [Google Scholar]
- 29.Gueniche A, Liboutet M, Cheilian S, Fagot D, Juchaux F, Breton L. Vitreoscilla filiformis Extract for Topical Skin Care: a Review. Front Cell Infect Microbiol. 2021;11:747663. doi: 10.3389/fcimb.2021.747663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nachbar F, Korting HC. The role of vitamin E in normal and damaged skin. J Mol Med. 1995;73(1):7–17. doi: 10.1007/BF00203614 [DOI] [PubMed] [Google Scholar]
- 31.Bissett DL, Oblong JE, Berge CA. Niacinamide: a B vitamin that improves aging facial skin appearance. Dermatol Surg. 2005;31(7 Pt 2):860–5; discussion 5. doi: 10.1111/j.1524-4725.2005.31732 [DOI] [PubMed] [Google Scholar]
- 32.Abatangelo G, Vindigni V, Avruscio G, Pandis L, Brun P. Hyaluronic acid: redefining its role. Cells. 2020;9(7):1743. doi: 10.3390/cells9071743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baldwin H, Alexis AF, Andriessen A, et al. Evidence of barrier deficiency in rosacea and the importance of integrating OTC skincare products into treatment regimens. J Drugs Dermatol. 2021;20(4):384–392. doi: 10.36849/JDD.5861 [DOI] [PubMed] [Google Scholar]