Abstract
Background/Aim: People who are undergoing cancer treatment often ask themselves what they can do in addition to conventional medical therapy with regard to nutrition, activity, and complementary methods. However, we know little about the motivation why people opt for one or the other measure. The aim of this study was therefore to examine the extent of physical activity (PA), healthy nutrition, and the use of complementary methods in relation to both demographic and psychological data.
Materials and Methods: A questionnaire was used to collect data on demographic data, resilience, coherence, self-efficacy, spirituality, satisfaction, and complementary and alternative medicine (CAM) behavior, PA, and diet. Between March and July 2021, data from 446 patients were collected. Regression models and correlation analyzes were used to examine the associations between CAM use, diet and PA with the other variables surveyed.
Results: CAM usage could only be predicted based on the patient’s spirituality. Women used CAM more often and ate more healthily. Healthy eating was also related to younger age, shorter medical history, resilience, satisfaction, and coherence. In addition, the results showed that daily PA was related to the level of resilience, spirituality, and self-efficacy.
Conclusion: Which people or why patients use CAM remains a question to be further investigated. Our data suggest that CAM seeks to address similar needs that others find in spirituality. In order to promote a healthy diet and PA in cancer patients in the future, various psychological variables seem conceivable. Resilience stands out, which is related to an overall healthier lifestyle.
Keywords: Cancer, complementary medicine, lifestyle, resilience, self-efficacy, spirituality
Many patients with cancer have a high interest in complementary and alternative medicine (CAM) (1,2), diets (3,4), physical and other activities, which allow them to get active and to contribute to the therapy (5). Aims are heterogenous ranging from fighting cancer, improving prognosis to increasing quality of life, and reducing side effects (6-8).
While evidence on physical activity (PA) is level 1A (9,10), and healthy nutrition is also recommended to all patients (11), evidence on most complementary methods are low and controversial (11). As former studies have shown, despite high evidence, patient information on and motivation to sports by physicians is low (12). Moreover, even today, many cancer centers do not use regular screening on malnutrition (3,13,14) and do not offer dietary counselling to all patients who have difficulties with nutrition or questions on nutrition. In fact, this number is much higher than those which are at risk of malnutrition. Loss or change of appetite or taste are a burden to many patients who do not talk about it to their oncologist (3,14). In several surveys on information needs, patients reported high needs on information on all these topics (15-17).
One way to improve patient information besides installing screenings and improving physicians’ awareness on these topics could be to train patients to actively ask questions. Talking to the physician on questions of lifestyle and complementary medicine might be easier for patients with higher self-efficacy (18). Actually, taking an active part, turning to healthy diet and PA, might also be associated to higher self-efficacy (19). In contrast, in our own studies, we have shown that patients who use complementary medicine have a lower self-efficacy than those who do not, which at first glance seemed quite contradictory (20). Nevertheless, we have reproduced this result in several surveys (21). One explanation might be that many types of complementary medicine in fact are not realized by any active part from the patient but resemble either conventional treatments (taking another pill for example containing vitamins) or aim at connecting the individual to a spiritual being or world. Accordingly, spirituality might be another characteristic of the individual patient and his inclination to supplemental and complementary methods.
Last but not least, for cancer patients, learning to live with a life-threatening diagnosis is a question of resilience with patients with higher resilience being able to cope with cancer more easily (22). Another concept in this context is coherence. People with a high sense of coherence show better coping in critical illness (23). They may also rely more on their own capacities to undergo the treatment and endure difficult times due to side effects or a progression of the cancer. So far, to our knowledge, there are no data on lifestyle, complementary medicine and resilience or sense of coherence.
The aim of our study was to learn more regarding the association of usage of complementary medicine, interest in nutrition and diets, adherence to PA on the one side and resilience, coherence, self-efficacy, spirituality, and satisfaction on the other side.
Materials and Methods
Questionnaire. We put together our own questionnaire consisting of 10 parts. In the first part, we collected the demographic data (sex, age, cancer and time of diagnosis, education, religion, marital and financial status) and the following parts related to psychological constructs like resilience, coherence, self-efficacy, spirituality, satisfaction, and lifestyle aspects, such as CAM behavior, PA, and diet. The last part included patient-explanations regarding their disease (etiology). However, this aspect will be the focus of another study and for this reason will not be discussed further here.
Dependent variables. In order to measure the dependent variables, a questionnaire that was originally developed by the working group Prevention and Integrative Oncology of the German Cancer Society (5) was used. We shortened the questionnaire from 17 to 10 available CAM methods (vitamin C, D, selenium, zinc, curcumin, mistletoe, acupuncture, Chinese herbs/tea, homeopathy, vitamin B17/apricot kernels) and asked the patients whether they had ever used and whether they were currently using these methods.
To further investigate the participants´ PA in their everyday life, before the cancer diagnosis and current, we used a short questionnaire in which the patients could give information on the duration of daily PA by going shopping or going to work, for example (“less than 10 minutes”-“more than 60 minutes”) and sporting activities, such as for example biking or swimming (“0-2 hours”-“more than 4 hours”) (12). The answer choices relate to current recommendations from the guideline “Komplementärmedizin in der Behandlung von onkologischen PatientInnen“ (11).
Finally, a few questions were asked about dietary habits. Therefore, a shortened and translated version of the Adolescent Food Habits Checklist was used. Instead of 23 items, we used 12 items and excluded duplication. The questions included eating habits and the consumed amount of sugar, fats, fruits, and vegetables.
Independent variables. Spirituality was measured with the FACIT-Sp12 (Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being) (24). Each of the 12 items is assessed according to a 5-point Likert response scale from 0 to 4 (0=”not at all” to 4=”very much”). The questionnaire is composed of the subscales meaning, peace, and faith and can be used to measure spiritual well-being not only within people with religious beliefs but also in populations that identify as spiritual but not religious. Both the internal consistency for the entire scale, as well as for the three subscales meaning, peace, and faith were good (α=0.81-0.88) (25).
Information on self-efficacy of the patients was collected with the help of the ASKU questionnaire (Allgemeine Selbstwirksamkeit Kurzskala, English: Short scale for measuring general self-efficacy beliefs). It is a three item scale by Beierlein, et al. (26) measuring subjectively perceived personal competences on a 5-point Likert scale (1=“doesn’t apply at all” to 5=“fully applies”). Reliability (ω=0.81 to ω=0.86) and validity are assessed as sufficient (26).
We used the resilience scale (RS-13) by Leppert, et al. (27), a reliable short version of the RS-25 (28). Patients can answer the items concerning belief in their own abilities on a 7-point Likert-scale (1=“I don`t agree at all” to 7=“I fully agree”). The internal consistency of the scale can be considered excellent (Chronbach’s α=0.9). In case of only one missing item, we substituted the value by the row mean of the patient. People with more than one missing item were excluded.
Coherence was measured with the SOC-L9 – sense of coherence questionnaire in a short version from Leipzig (29). The format of the questionnaire consists again of a 7-point Likert-scale with changing answer options concerning the topics meaning, manageability, and comprehensibility of aspects of life. The SOC-L9 presents an excellent intercorrelation with the longform and has a high internal consistency (Chronbach’s α=0.87). For missing values, the same procedure as for the RS-13 was used.
The L-1 (Lebenszufriedenheit-1, English: Life satisfaction) asks patients in one single item on a 10-point Likert scale about their actual satisfaction. Re-test-reliability of this scale after six weeks is r=0.67 (30).
Participants. The questionnaire was distributed to outpatient cancer patients in 10 different cancer centers in Germany (6 oncological departments of hospitals, one rehabilitation clinic and 3 oncological offices), between March and July 2021. They got a printed version of the questionnaire that they answered anonymously. Inclusion criteria were an active cancer treatment and current cancer diagnosis. Knowledge of the German language was also relevant in order to answer the questions. In addition, the patients had to be over 18 years old.
Statistical analyses. Analyses were conducted using the open-source software R Studio (version 1.4.1106). To get information about CAM users we first created a new dichotomous variable, which describes whether patients are actually using at least one CAM method or not. For more detailed analyses, we then divided the dependent variable once again into two, one for biological based CAM methods (vitamin C, D, B17, selenium, zinc, curcumin, and mistletoe) and one for holistic methods like homeopathy, acupuncture, and Chinese herbs/tea. With the help of binary logistic regressions, we tested whether CAM use could be predicted from the demographic data or the constructs resilience, coherence, self-efficacy, spirituality, and satisfaction. Therefore, odds ratios (OR) were calculated in three regression models – one for CAM usage in general, one for biological-based CAM methods and one for holistic methods. A positive relationship between predictor and dependent variables is indicated by an OR greater than one, a negative one by an OR less than one. To compare the two groups of users and non-users of CAM, t tests for independent samples were carried out. For the assessment of differences in CAM use between more than two groups (e.g., for the different cancer types or religion affiliations) we performed variance analyses.
Concerning daily PA and diet, we conducted correlation analyses to look for associations to the demographic data and psychological constructs. One-sample t-tests were used to compare activity levels before the disease and the current situation. For all statistical tests, a level of p≤0.05 was considered significant.
Results
Demographics. A total of 446 patients took part in the survey; 65% of them were women and 35% men. Their age range was between 33 and 93 (M=63, SD=11). The most common cancer diagnoses were breast cancer (34.6%), followed by head and neck (11.3%) and colorectal cancer (11.1%). For half of the patients, the time of their first diagnosis was less than a year ago (50%), for 29% it was one to three years ago, for 10% three to six years, and for 11% more than six years.
With regard to further demographic data, the sample was composed of the following: When asked how long patients could manage financially if suddenly, they had no more income, 40% answered that they would manage for more than a year. On the other hand, 36% stated that it was only for one to six months. 68% of the respondents were currently living in a partnership. More than half of the patients assigned their religion to Christianity (57%), followed by 42% who did not feel they belonged to any religion. The majority of the sample had attended school for eight to ten years (66%). Further details on the demographics of the patients are shown in Table I.
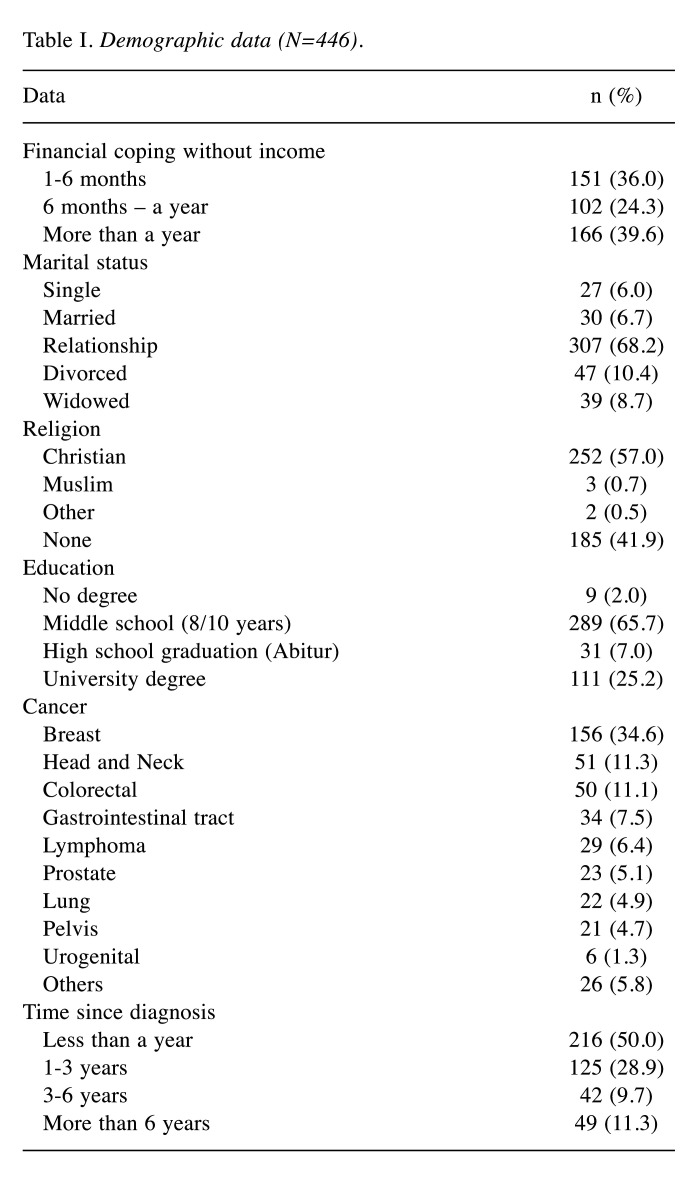
Table I. Demographic data (N=446).
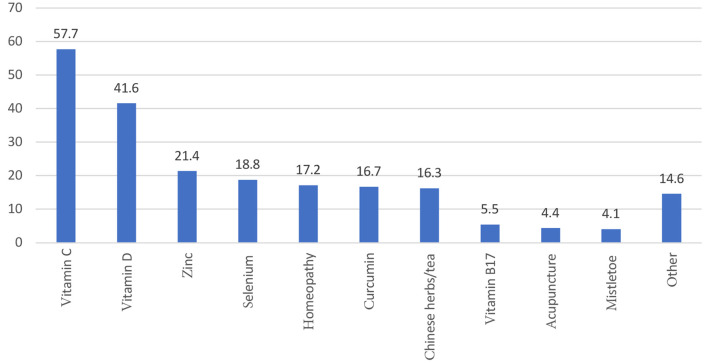
Usage of CAM. Of the patients surveyed, 138 (31%) stated that they were currently using one or more CAM methods compared to 72 who did not use anything. Patients used between one and 13 CAM methods at the same time. The most commonly used CAM substance was vitamin D (58%), followed by vitamin C (42%), and zinc (21%). An overview of all the CAM methods used can be seen in Figure 1.
Figure 1. Frequencies of used complementary and alternative medicine (CAM) methods.
Diet. The responses from the AFHC on the diet of the patients showed that the average was eating rather healthily. The mean value of the sample (M=7.8, SD=2.2) was above the mean value of the scale (M=6). In this context, eating healthily means eating low-fat, without too much sugar and meat, but with enough fruit and vegetables.
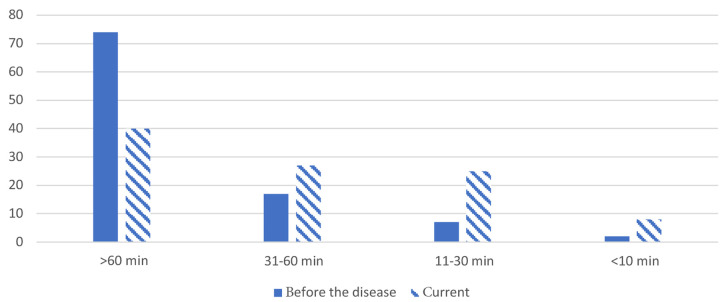
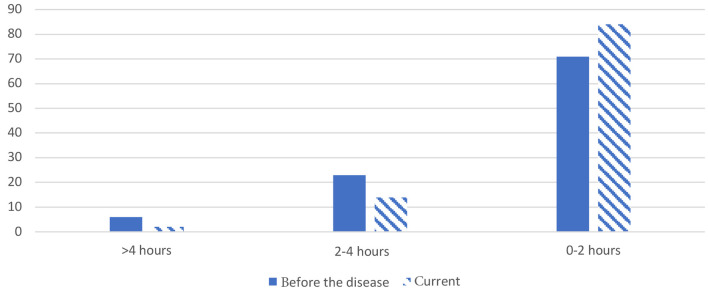
Daily physical activity. In most of the patients, the PA in everyday life was more than 60 minutes on average per day. both before the disease and current (Figure 2); however, group comparisons showed a significant decrease in average daily PA [t(379)=12.56, p<0.001]. Those who had been more active before the illness were also more active during that time (r=0.31, p<0.001). Related to sporting activities, the majority of patients averaged zero to two hours per day (Figure 3). Here, too, there was a significant difference between before the diagnosis and the current situation [t(347)=5.574, p<0.001] but at the same time an association (r=0.25, p<0.001).
Figure 2. Average daily physical activity before the disease and current (%).
Figure 3. Average sporting activity per day before the disease and current (%).
Predictors for CAM use. The demographic data could not predict the general use of CAM except for sex. It turned out, that women were more likely to use CAM than men (OR=0.38, 95%CI=0.20-0.69, p=0.002). With one exception, the other variables could also not be identified as predictors for general CAM use. Only spirituality showed a significant negative association (OR=0.97, 95%CI=0.95-1.00, p=0.05). The group comparison made it clear that the value of spirituality in the group of patients using CAM was significantly lower than that of those who did not use CAM [Muser=27 vs. Mnon-user=30, t(204)=1.97, p=0.05]. In relation to the subscales, this tendency only persisted for the meaning scale (OR=0.82, 95%CI=0.70-0.95, p=0.01) but not for peace and faith.
No predictors for only biological-based CAM methods or holistic CAM methods were found. Only the fact that sex predicts CAM use remained in the subgroup of biological-based substances (OR=0.53, 95%CI=0.3-0.96, p=0.04).
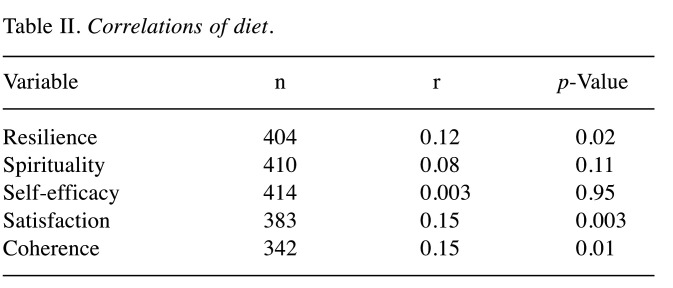
Healthy diet. Concerning diet, the analyses showed that female and older patients eat healthier than male and younger patients (rgender=-0.26, rage=0.15, p´s<0.01). They also made it clear that the diet became unhealthier with time after the diagnosis (r=-0.16, p<0.01). A significant difference after alpha error adjustment was seen between the groups of patients with breast cancer and those with head and neck cancer. The former ate healthier than the latter (Mbreast=8.2, Mhead and neck=6.9, p=0.05). The other demographic variables showed no significant correlations (p>0.05). Diet was further positively correlated with resilience, satisfaction, and coherence (0.11>r<0.15, p≤0.02). No association to self-efficacy and spirituality emerged (Table II).
Table II. Correlations of diet.
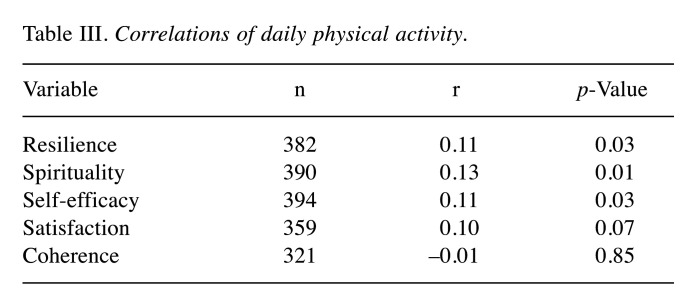
Daily physical activity. The current amount of daily PA was not associated with the demographic data and also not with coherence and satisfaction (p>0.05). Instead, PA showed positive correlations with resilience, spirituality, and self-efficacy (p<0.05). The correlations were all in a small range (0.11>r<0.13, Table III). In regard to sporting activities, we found no correlations at all – neither with demographic nor with psychological variables (p>0.05).
Table III. Correlations of daily physical activity.
Discussion
CAM use. There are heterogeneous data on the extent to which a person’s age and education can predict the use of CAM. We found no association in our work, but other publications disagree (31). However, the authors compared the extreme groups with one another and note that no effects become apparent when, for example, middle educated, and higher educated participants are compared (31). This could be an explanation for our results, in which the majority of included patients were middle educated. Other studies confirm our results, in which age (32) and education were also irrelevant (20,33). In line with the latter result, the financial situation was also not able to predict CAM usage. If we assume that educational status and income are linked, that makes sense and was also found in the study by Sohl, et al. (34), for example. The only demographic factor that predicted the use of CAM was sex. The result that women use CAM more often than men is in accordance with previous studies (1,31,32).
Resilience and life satisfaction were just as unable to predict whether patients were using CAM, as was coherence and self-efficacy. In a former study, we have reported similar data (20,35). As usage of CAM often is discussed as means to activate patients and further patient empowerment, one would expect patients with higher self-efficacy more often using CAM. One reason might be that mostly biological-based CAM for some patients is just another type of substance intake which add to the conventional drugs but do not rely on a strong internal locus of control. Accordingly, our results would support the statement that the use of CAM is not necessarily based on the desire for autonomy and becoming active, but rather the need to hand over responsibility to external forces (20). This is also supported by the result that in the data presented here, patients who were less spiritual were more likely to use CAM. This finding persisted above all for the subscale meaning, which stands for the cognitive aspect of spiritual well-being (36) – that life has a meaning, a purpose (25). The results could be interpreted in such a way that people who can cognitively transfer parts of the process of their healing to an external source through their spirituality, seldom demand CAM methods to meet this need.
Healthy diet. In our study, women, the elderly, and patients who were recently diagnosed were paying more attention to a healthy diet. The fact that the diet worsens with time after the first diagnosis could be a motivation phenomenon. It is easy to imagine that shortly after such a profound diagnosis the will to adapt one’s lifestyle in order to have better chances of recovery is greatest and that it decreases again over time.
Along with our data, also other studies report that patients with breast cancer are more engaged in a healthy lifestyle and stand out with very conscientious behavior (37). Head and neck cancer patients, on the other hand, often have more problems with nutrition due to their therapy, since the radiation in the head and neck area often leads to side effects, such as swallowing difficulties, pain, changes in the sense of taste, and reduced saliva production, which restricts or complicates eating.
Regarding the psychological variables, resilience, satisfaction, and coherence correlated weakly with healthy diet. Other studies are very unanimous: Greater resilience is associated with a healthier or more balanced diet (38,39). The notion that patients who are autonomously motivated to follow a healthy diet are more likely to feel more satisfied with their lives is supported by the authors Castillo-Mayen, et al. (40) in patients with cardiovascular disease. Coherence and diet have only been assessed in few studies (41). They suggest that people with a higher sense of coherence eat healthier.
To our astonishment, we were not able to show an association between self-efficacy and healthy diet. This is in accordance with the results on the use of CAM. Self-efficacy did not seem to be a motive for action here either. Rather, one explanation for the results could be that there is an external rather than an internal locus of control behind the behavior. That means that patients believe that external factors have a stronger influence on the future course of the disease than her or himself.
Daily physical activity. In other studies, engagement in PA after a cardiovascular event was correlated to coherence (42). In a recent study from 2020 on patients with multiple sclerosis, as in our survey, no associations were visible (43). This and our study are among a few who so far speak against the hypothesis that coherence predicts a healthier lifestyle. The situation is similar with life satisfaction and PA where a positive association has so far been assumed in different samples. Other studies that have already been carried out have also shown that PA and resilience were positively correlated in oncological patients (44). It is believed that resilience acts as a protective factor. Also, self-efficacy and PA are positively associated, which has already been proven in various studies (45). Self-efficacy thus appears to help establish or maintain behavior. On the other hand, less is known about the association between spirituality and PA, which according to our data is positive. Studies on healthy volunteers confirm these results (46).
Most importantly, PA in our study was not associated with demographic data. This means that the positive effects of daily PA may be accessible for all patients and do not reflect social or economic resources.
The points described all relate to PA, i.e., to activities of everyday life. We could not find any correlations in this study for sporting activities. This could be related to the fact that we collected our data in mid-2021, when the coronavirus pandemic had a major impact on free time activities. Vulnerable people in particular, including patients with cancer, probably behaved rather cautiously for fear of infection.
Study limitations included that all variables were only measured at one point of time. As a result, no statements can be made about changes in psychological variables or diet since diagnosis. Even though our questionnaire was long and extensive, there is information that would have been additionally important, such as a more precise medical history to see how many treatments the patient had already undergone or the degree of current involvement in a religious community to better assess the importance of faith. Another point is that all statements were based on self-assessments. Studies on this problem have already made it clear that subjective and objective measures can deviate from one another (47). Lastly, an even larger sample would have been necessary for usable subgroup analyses - both for the individual types of cancer and for the CAM methods.
Conclusion
With regard to the use of CAM, it still remains difficult to say which variables could help predict whether patients will use methods or not. It seems to be important to pay attention to the spiritual well-being of the person and to take the need for orientation and finding meaning seriously and to strengthen it. At the same time, one should continue to educate well about what CAM can and cannot actually do in order to make realistic hopes and goals possible and to avoid interactions or side effects.
Diet appears to be linked to many positive psychological variables. At the moment, we cannot say whether the diet strengthens the psychological constitution or whether people who are more psychologically stable eat better. Previous studies have only found these relationships for other samples. From the data presented here, one can draw the conclusion that they can also be transferred to patients with cancer.
Regarding PA, some questions remain unanswered and only a few associations with the data we collected could be discovered. Paying attention to cancer patients with low resilience, self-efficacy, or spirituality could help to focus more on those individuals who need more external support to be physically active in everyday life. In particular, promoting resilience seems to support a healthy lifestyle in the form of healthy eating and frequent PA.
Conflicts of Interest
The Authors have no relevant financial or non-financial interests to disclose in relation to this study.
Authors’ Contributions
Material preparation and analysis were performed by Catalina Hoppe and Jutta Hübner. Data collection was carried out by Jens Büntzel, Ludwig Fischer von Weikersthal, Constanze Junghans, Bijan Zomorodbakhsch, Christoph Stoll, Franz-Josef Prott, Stefan Fuxius, Oliver Micke and Achim Richter. The first draft of the manuscript was written by Catalina Hoppe and Jutta Hübner and Jens Büntzel commented on previous versions of the manuscript. All Authors read and approved the final manuscript.
References
- 1.Micke O, Bruns F, Glatzel M, Schönekaes K, Micke P, Mücke R, Büntzel J. Predictive factors for the use of complementary and alternative medicine (CAM) in radiation oncology. Eur J Integr Med. 2009;1(1):19–25. doi: 10.1016/j.eujim.2009.02.001. [DOI] [Google Scholar]
- 2.Molassiotis A, Fernández-Ortega P, Pud D, Ozden G, Scott JA, Panteli V, Margulies A, Browall M, Magri M, Selvekerova S, Madsen E, Milovics L, Bruyns I, Gudmundsdottir G, Hummerston S, Ahmad AM, Platin N, Kearney N, Patiraki E. Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol. 2005;16(4):655–663. doi: 10.1093/annonc/mdi110. [DOI] [PubMed] [Google Scholar]
- 3.Maschke J, Kruk U, Kastrati K, Kleeberg J, Buchholz D, Erickson N, Huebner J. Nutritional care of cancer patients: a survey on patients’ needs and medical care in reality. Int J Clin Oncol. 2017;22(1):200–206. doi: 10.1007/s10147-016-1025-6. [DOI] [PubMed] [Google Scholar]
- 4.Pieper D, Jülich F, Antoine SL, Bächle C, Chernyak N, Genz J, Eikermann M, Icks A. Studies analysing the need for health-related information in Germany - a systematic review. BMC Health Serv Res. 2015;15:407. doi: 10.1186/s12913-015-1076-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huebner J, Micke O, Muecke R, Buentzel J, Prott FJ, Kleeberg U, Senf B, Muenstedt K, PRIO (Working Group Prevention and Integrative Oncology of the German Cancer Society) User rate of complementary and alternative medicine (CAM) of patients visiting a counseling facility for CAM of a German comprehensive cancer center. Anticancer Res. 2014;34(2):943–948. [PubMed] [Google Scholar]
- 6.Bauer F, Schmidt T, Eisfeld H, Dubois C, Kastrati K, Hochhaus A, Huebner J. Information needs and usage of complementary and alternative medicine in members of a German self-help group for gastrointestinal stroma tumours, sarcoma, and renal cancer. Complement Ther Med. 2018;41:105–110. doi: 10.1016/j.ctim.2018.09.008. [DOI] [PubMed] [Google Scholar]
- 7.Elsner T, Muecke R, Micke O, Prott FJ, Muenstedt K, Waldmann A, Geissler J, Huebner J. Survey on the worldwide Chronic Myeloid Leukemia Advocates Network regarding complementary and alternative medicine. J Cancer Res Clin Oncol. 2013;139(6):1025–1031. doi: 10.1007/s00432-013-1414-4. [DOI] [PubMed] [Google Scholar]
- 8.Huebner J, Prott FJ, Micke O, Muecke R, Senf B, Dennert G, Muenstedt K, PRIO (Working Group Prevention and Integrative Oncology - German Cancer Society) Online survey of cancer patients on complementary and alternative medicine. Oncol Res Treat. 2014;37(6):304–308. doi: 10.1159/000362616. [DOI] [PubMed] [Google Scholar]
- 9.Campbell KL, Winters-Stone KM, Wiskemann J, May AM, Schwartz AL, Courneya KS, Zucker DS, Matthews CE, Ligibel JA, Gerber LH, Morris GS, Patel AV, Hue TF, Perna FM, Schmitz KH. Exercise guidelines for cancer survivors: Consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc. 2019;51(11):2375–2390. doi: 10.1249/MSS.0000000000002116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Friedenreich CM, Stone CR, Cheung WY, Hayes SC. Physical activity and mortality in cancer survivors: a systematic review and meta-analysis. JNCI Cancer Spectr. 2019;4(1):pkz080. doi: 10.1093/jncics/pkz080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft DK and AWMF): Komplementärmedizin in der behandlung v on onkologischen patientinnen, langversion 1.1, awmf registernummer: 032/055ol, 2021. Available at: https://www.Leitlinienprogramm-onkologie.De/leitlinien/komplementaermedizin. [Last accessed on October 31, 2022]
- 12.Höh JC, Schmidt T, Hübner J. Physical activity among cancer survivors-what is their perception and experience. Support Care Cancer. 2018;26(5):1471–1478. doi: 10.1007/s00520-017-3977-0. [DOI] [PubMed] [Google Scholar]
- 13.Erickson N, Paradies K, Buchholz D, Huebner J. Nutrition care of cancer patients-A survey among physicians and nurses. Eur J Cancer Care (Engl) 2018;27(4):e12855. doi: 10.1111/ecc.12855. [DOI] [PubMed] [Google Scholar]
- 14.Sonneborn-Papakostopoulos M, Dubois C, Mathies V, Heß M, Erickson N, Ernst T, Huebner J. Quality of life, symptoms and dietary habits in oncology outpatients with malnutrition: A cross-sectional study. Med Oncol. 2021;38(2):20. doi: 10.1007/s12032-021-01460-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ciarlo G, Ahmadi E, Welter S, Hübner J. Factors influencing the usage of complementary and alternative medicine by patients with cancer. Complement Ther Clin Pract. 2021;44:101389. doi: 10.1016/j.ctcp.2021.101389. [DOI] [PubMed] [Google Scholar]
- 16.Muusses LD, van Weert JC, van Dulmen S, Jansen J. Chemotherapy and information-seeking behaviour: characteristics of patients using mass-media information sources. Psychooncology. 2012;21(9):993–1002. doi: 10.1002/pon.1997. [DOI] [PubMed] [Google Scholar]
- 17.Elsner T, Muecke R, Micke O, Prott FJ, Muenstedt K, Waldmann A, Geissler J, Huebner J. Survey on the worldwide Chronic Myeloid Leukemia Advocates Network regarding complementary and alternative medicine. J Cancer Res Clin Oncol. 2013;139(6):1025–1031. doi: 10.1007/s00432-013-1414-4. [DOI] [PubMed] [Google Scholar]
- 18.Zimmaro LA, Lepore SJ, Beach MC, Reese JB. Patients’ perceived barriers to discussing sexual health with breast cancer healthcare providers. Psychooncology. 2020;29(7):1123–1131. doi: 10.1002/pon.5386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Imai H, Furukawa TA, Hayashi SU, Goto A, Izumi K, Hayashino Y, Noda M, J-DOIT2 Study Group Risk perception, self-efficacy, trust for physician, depression, and behavior modification in diabetic patients. J Health Psychol. 2020;25(3):350–360. doi: 10.1177/1359105317718057. [DOI] [PubMed] [Google Scholar]
- 20.Ebel MD, Rudolph I, Keinki C, Hoppe A, Muecke R, Micke O, Muenstedt K, Huebner J. Perception of cancer patients of their disease, self-efficacy and locus of control and usage of complementary and alternative medicine. J Cancer Res Clin Oncol. 2015;141(8):1449–1455. doi: 10.1007/s00432-015-1940-3. [DOI] [PubMed] [Google Scholar]
- 21.Welter S, Keinki C, Ahmadi E, Huebner J. Lay etiology, self-efficacy and patient activation among cancer patients. Cancer Invest. 2021;39(3):219–228. doi: 10.1080/07357907.2021.1878528. [DOI] [PubMed] [Google Scholar]
- 22.Macía P, Barranco M, Gorbeña S, Iraurgi I. Expression of resilience, coping and quality of life in people with cancer. PLoS One. 2020;15(7):e0236572. doi: 10.1371/journal.pone.0236572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fok SK, Chair SY, Lopez V. Sense of coherence, coping and quality of life following a critical illness. J Adv Nurs. 2005;49(2):173–181. doi: 10.1111/j.1365-2648.2004.03277.x. [DOI] [PubMed] [Google Scholar]
- 24.Fitchett G. World Congress of Psycho-Oncology. 1996. Spiritual beliefs and quality of life in cancer and HIV patients. [Google Scholar]
- 25.Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy—Spiritual Well-being Scale (FACIT-Sp) Ann Behav Med. 2002;24(1):49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 26.Beierlein C, Kovaleva A, Kemper CJ, Rammstedt B. Mannheim, GESIS - Leibniz-Institut für Sozialwissenschaften. 2012. Ein messinstrument zur erfassung subjektiver kompetenzerwartungen: Allgemeine selbstwirksamkeit kurzskala (ASKU) p. pp. 24. [Google Scholar]
- 27.Leppert K, Koch B, Brähler E, Strauß B. Die resilienzskala (rs)–überprüfung der langform rs-25 und einer kurzform rs-13. Klin Diagn Eval. 2008;1(2):226–243. [Google Scholar]
- 28.Schumacher J, Leppert K, Gunzelmann T, Strauß B, Brähler E. Die resilienzskala–ein fragebogen zur erfassung der psychischen widerstandsfähigkeit als personmerkmal. Z Klin Psychol Psychiatr Psychother. 2005;53(1):16–39. [Google Scholar]
- 29.Schumacher J, Wilz G, Gunzelmann T, Brähler E. [The Antonovsky Sense of Coherence Scale. Test statistical evaluation of a representative population sample and construction of a brief scale] Psychother Psychosom Med Psychol. 2000;50(12):472–482. doi: 10.1055/s-2000-9207. [DOI] [PubMed] [Google Scholar]
- 30.Beierlein C, Kovaleva A, László Z, Kemper CJ, Rammstedt B. Eine single-item-skala zur erfassung der allgemeinen lebenszufriedenheit: Die kurzskala lebenszufriedenheit-1 (l-1), 2014. Available at: https://www.gesis.org/fileadmin/kurzskalen/working_papers/L1_WorkingPapers_2014-33.pdf. [Last accessed on November 1, 2022]
- 31.Dufter SA, Hübner J, Ahmadi E, Zomorodbakhsch B. Traits of cancer patients and CAM usage. J Cancer Res Clin Oncol. 2021;147(12):3685–3692. doi: 10.1007/s00432-021-03605-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dubois C, Eisfeld H, Bauer F, Schmidt T, Kastrati K, Hochhaus A, Hübner J. Not all cancer patients with an interest in CAM are the same. Differences between patients with a CAM interest prior to the cancer diagnosis and those with first-time interest since diagnosis. Complement Ther Med. 2019;45:167–171. doi: 10.1016/j.ctim.2019.06.009. [DOI] [PubMed] [Google Scholar]
- 33.Keinki C, Ahmadi E, Kastrati K, Zomorodbakhsch B, Hübner J, Working Group Prevention and Integrative Oncology of the German Cancer Society (PRIO) Cancer patient motives and expectations on non-medical practitioners. In Vivo. 2022;36(5):2505–2513. doi: 10.21873/invivo.12986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sohl SJ, Weaver KE, Birdee G, Kent EE, Danhauer SC, Hamilton AS. Characteristics associated with the use of complementary health approaches among long-term cancer survivors. Support Care Cancer. 2014;22(4):927–936. doi: 10.1007/s00520-013-2040-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Josfeld L, Krüger L, Büntzel J, Zomorodbakhsch B, Hübner J. Self-efficacy in relation to the use of complementary and alternative medicine, lifestyle choices and cancer aetiology. J Cancer Res Clin Oncol. 2022;148(10):2707–2715. doi: 10.1007/s00432-021-03857-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bredle JM, Salsman JM, Debb SM, Arnold BJ, Cella D. Spiritual well-being as a component of health-related quality of life: the functional assessment of chronic illness therapy-spiritual well-being scale (FACIT-Sp) Religions. 2018;2(1):77–94. doi: 10.3390/rel2010077. [DOI] [Google Scholar]
- 37.Büntzel J, Kusterer I, Rudolph Y, Kubin T, Micke O, Hübner J. Cancer patients’ knowledge and acceptance of physical activities for rehabilitation. In Vivo. 2017;31(6):1187–1192. doi: 10.21873/invivo.11188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bonaccio M, Di Castelnuovo A, Costanzo S, Pounis G, Persichillo M, Cerletti C, Donati MB, de Gaetano G, Iacoviello L. Mediterranean-type diet is associated with higher psychological resilience in a general adult population: findings from the Moli-sani study. Eur J Clin Nutr. 2018;72(1):154–160. doi: 10.1038/ejcn.2017.150. [DOI] [PubMed] [Google Scholar]
- 39.Ozdemir C, Akbas Gunes N. The effect of diet and regular exercise on psychological resilience in obese or overweight women. Int J Clin Pract. 2021;75(8):e14320. doi: 10.1111/ijcp.14320. [DOI] [PubMed] [Google Scholar]
- 40.Castillo-Mayén R, Cano-Espejo C, Luque B, Cuadrado E, Gutiérrez-Domingo T, Arenas A, Rubio SJ, Delgado-Lista J, Pérez-Martínez P, Tabernero C. Influence of self-efficacy and motivation to follow a healthy diet on life satisfaction of patients with cardiovascular disease: a longitudinal study. Nutrients. 2020;12(7):1903. doi: 10.3390/nu12071903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.da-Silva-Domingues H, Del-Pino-Casado R, Palomino-Moral PÁ, López Martínez C, Moreno-Cámara S, Frías-Osuna A. Relationship between sense of coherence and health-related behaviours in adolescents and young adults: a systematic review. BMC Public Health. 2022;22(1):477. doi: 10.1186/s12889-022-12816-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Adorni R, Greco A, D’Addario M, Zanatta F, Fattirolli F, Franzelli C, Maloberti A, Giannattasio C, Steca P. Sense of coherence predicts physical activity maintenance and health-related quality of life: a 3-year longitudinal study on cardiovascular patients. Int J Environ Res Public Health. 2022;19(8):4700. doi: 10.3390/ijerph19084700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Reguera-García MM, Liébana-Presa C, Álvarez-Barrio L, Alves Gomes L, Fernández-Martínez E. Physical activity, resilience, sense of coherence and coping in people with multiple sclerosis in the situation derived from COVID-19. Int J Environ Res Public Health. 2020;17(21):8202. doi: 10.3390/ijerph17218202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Matzka M, Mayer H, Köck-Hódi S, Moses-Passini C, Dubey C, Jahn P, Schneeweiss S, Eicher M. Relationship between resilience, psychological distress and physical activity in cancer patients: a cross-sectional observation study. PLoS One. 2016;11(4):e0154496. doi: 10.1371/journal.pone.0154496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kindred MM, Pinto BM, Dunsiger SI. Mediators of physical activity adoption and maintenance among breast cancer survivors. J Behav Med. 2020;43(4):605–613. doi: 10.1007/s10865-019-00085-6. [DOI] [PubMed] [Google Scholar]
- 46.Silfee VJ, Haughton CF, Lemon SC, Lora V, Rosal MC. Spirituality and physical activity and sedentary behavior among Latino men and women in Massachusetts. Ethn Dis. 2017;27(1):3–10. doi: 10.18865/ed.27.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Douma JAJ, de Beaufort MB, Kampshoff CS, Persoon S, Vermaire JA, Chinapaw MJ, van Mechelen W, Nollet F, Kersten MJ, Smit JH, Verdonck-de Leeuw IM, Altenburg TM, Buffart LM. Physical activity in patients with cancer: self-report versus accelerometer assessments. Support Care Cancer. 2020;28(8):3701–3709. doi: 10.1007/s00520-019-05203-3. [DOI] [PMC free article] [PubMed] [Google Scholar]