Abstract
Background:
Frailty is increasingly being recognized as a public health issue, straining healthcare resources and increasing costs to care for these patients. Frailty is the decline in physical and cognitive reserves leading to increased vulnerability to stressors such as surgery or disease states. The goal of this pilot diagnostic accuracy study was to identify whether point-of-care ultrasound measurements of the quadriceps and rectus femoris muscles can be used to discriminate between frail and not-frail patients and predict postoperative outcomes. This study hypothesized that ultrasound could discriminate between frail and not-frail patients before surgery.
Methods:
Preoperative ultrasound measurements of the quadriceps and rectus femoris were obtained in patients with previous computed tomography scans. Using the computed tomography scans, psoas muscle area was measured in all patients for comparative purposes. Frailty was identified using the Fried phenotype assessment. Postoperative outcomes included unplanned intensive care unit admission, delirium, intensive care unit length of stay, hospital length of stay, unplanned skilled nursing facility admission, rehospitalization, falls within 30 days, and all-cause 30-day and 1-yr mortality.
Results:
A total of 32 patients and 20 healthy volunteers were included. Frailty was identified in 18 of the 32 patients. Receiver operating characteristic curve analysis showed that quadriceps depth and psoas muscle area are able to identify frailty (area under the curve–receiver operating characteristic, 0.80 [95% CI, 0.64 to 0.97] and 0.88 [95% CI, 0.76 to 1.00], respectively), whereas the cross-sectional area of the rectus femoris is less promising (area under the curve–receiver operating characteristic, 0.70 [95% CI, 0.49 to 0.91]). Quadriceps depth was also associated with unplanned postoperative skilled nursing facility discharge disposition (area under the curve 0.81 [95% CI, 0.61 to 1.00]) and delirium (area under the curve 0.89 [95% CI, 0.77 to 1.00]).
Conclusions:
Similar to computed tomography measurements of psoas muscle area, preoperative ultrasound measurements of quadriceps depth shows promise in discriminating between frail and not-frail patients before surgery. It was also associated with skilled nursing facility admission and postoperative delirium.
Every year, millions of Americans undergo surgical procedures to improve health and reduce disease burden. However, for frail patients, undergoing surgery carries increased risk of adverse outcomes including loss of independence and increased risk of mortality. Frailty is the decline in physical and cognitive reserves leading to increased vulnerability to stressors such as surgery or disease states.1 The frail phenotype has been well described to include decreased status in mobility, muscle mass, nutritional status, strength, and endurance1–5 and is associated with increased symptom burden and adverse clinical outcomes.6 Although frailty is often characterized as a syndrome of physiologic decline later in life with age being a strong correlate of frailty, frailty alone, despite age, is an independent predictor of adverse outcomes including falls, hospitalization, delirium, and death.4,7–10 More and more younger adults with deficit accumulations are at increased risk of frailty and having worse postsurgical outcomes than their fit or resilient counterparts.11
Although the frail phenotype is well understood to lead to worse outcomes, and many frailty assessment tools have been created to help us identify these at-risk patients, there is still no gold standard for identifying frailty preoperatively.12 The Fried frailty phenotype13 characterizes frailty in five different domains (weight loss, exhaustion, weakness, slowness, and physical activity levels). Although extensively validated in skilled nursing facilities, concerns are raised that the assessment may be too time-consuming and was not created as a way to risk-stratify preoperative patients.8,9 In the perioperative setting, a frailty tool that can be applied when a patient is not able to walk due to an acute or chronic disease process or unable to provide a comprehensive medical history due to altered mental status is necessary. Sarcopenia, or skeletal muscle loss, is a biologic and functional marker of frailty that can be objectively quantified.14 The mainstay for many surgical specialties is to measure psoas muscle area via computed tomography as a way to identify frailty in their surgical populations.15 However, computed tomography is expensive and resource-intensive and exposes patients to radiation. Therefore, unless the patient needs a preoperative computed tomography scan as part of standard of care for their diagnostic work-up, it is not an optimal diagnostic tool of frailty.
Recently, bedside ultrasound has been used in intensive care unit (ICU) patients to track the development of sarcopenia and was shown to correlate well with frailty in this patient population by measuring the quantity and quality of quadriceps muscles.16 We hypothesized that point-of-care ultrasound could discriminate between frail and not-frail patients before surgery. We also assessed whether frailty as defined by ultrasound measurements predicted adverse discharge disposition (i.e. loss of independence) and other postoperative outcomes.
Materials and Methods
After institutional review board approval (approval no. 18–000857) and in accordance to the items on the Standards for the Reporting of Diagnostic Accuracy Studies (STARD) statement and checklist,17 we prospectively enrolled adults who presented to the preoperative clinic and provided written informed consent. Patients who present to the preoperative clinic are referred by the surgical team for preoperative evaluation and are assessed by a resident and attending anesthesiologist as part of their routine care.
Study Population
Adult patients scheduled for major abdominal, gynecological, vascular, or spine/orthopedic surgery who had an abdominal/pelvis computed tomography scan within 90 days of their preoperative clinic as part of their routine work-up were recruited for this study. Those who lacked the capacity to consent and those who had any extremity amputation, paraplegia, or diseases affecting the muscles were excluded from the study. The study population is comprised of a consecutive consenting sample.
Measurements
Frailty Assessments.
All patients were assessed for frailty based on the Fried frailty phenotype assessment, which was used as the reference standard. The original definition of frailty as reported by Fried et al.13 consists of five criteria: unintentional weight loss, self-reported exhaustion, physical weakness (grip strength), slow walking speed, and low physical activity. Frailty was defined when three or more of the above criteria were present. For the purposes of this study, patients either self-reported unintentional weight loss (more than 4.5 kg in previous year) or the information was extracted by medical record review. Self-reported exhaustion was measured using two questions from the Center for Epidemiologic Studies Depression Scale (CES-D).13 The exhaustion criterion was considered present if a participant answered “often” or “most of the time” to the following two statements: “In the last week I felt that everything I did was an effort” and “In the last week I could not get going.” Grip strength was used to measure physical weakness. A Camry digital hand dynamometer with 90-kg grip strength was used to calculate the grip strength adjusting for sex and body mass index. The nondominant hand of the patient was used, and three continuous measurements were taken. The average value of these measurements constituted the final value. The cutoffs values for men were 20.5 kg (body mass index less than 24), 21.5 kg (body mass index of 24 to 26), and 23 kg (body mass index greater than 26) and for women, 11.5 kg (body mass index less than 23) and 13 kg (body mass index greater than 23).18 Slow walking speed was measured using the timed up and go test.18,19 The patient was observed and timed on their ability to rise from an armchair, walk 3 m, turn, walk back, and sit down again. The cutoff for a positive timed up and go test was 10 s.18 Physical activity was assessed using the LASA Physical Activity Questionnaire.20 Low physical activity was defined by the lowest quintile of average time spent on physical activities per day during 2 weeks before the interview.
Ultrasound Image Acquisition and Measurements.
The two-dimensional ultrasound images of the quadriceps and rectus femoris were collected on supine patients at 30° upper body elevation with legs extended. The measurements were obtained at 60% length mark measured from the anterior superior iliac spine to the superior border of the patella. Three consecutive images on the right leg were acquired for each patient with a Vivid S6 ultrasound system (GE Healthcare, USA) using a curved-array transducer (4C-RS) with 1.8- to 6-MHz bandwidth. Two-dimensional images were acquired at a frame rate of 22 to 60 frames/s for optimizing gray scale. The studies were transferred and stored as raw data images in a General Electric EchoPAC system version 113 (GE Healthcare) for measurement and analysis. The quadriceps depth, rectus femoris cross-sectional area, and rectus femoris circumference were measured for each of the three images acquired and averaged. In an effort to standardize across various muscle mass composition to body habitus (i.e., muscle ratio differences between men and women, or obese patients with high versus low muscle quantity), values were indexed by dividing by the body surface area and body mass index for normalization. All images were acquired and all measurements were performed by the same trained and certified sonographer, who was blinded to the patient’s frailty status.
Computed Tomography Scan Images and Measurements.
The cross-sectional axial area (cm2) of bilateral psoas muscle was assessed computed tomography at the level of the fourth lumbar vertebra (L4) on one axial slice with visible vertebral spine and averaged. The psoas muscle area values were again indexed by dividing by the body surface area and body mass index for normalization. Images were obtained using OsiriX version 9.0 (Pixmeo, Switzerland) using a range of −30 to +110 Hounsfield units to distinguish skeletal muscle tissue. Abdominal/pelvic computed tomography scans were obtained as part of the patient’s routine medical work-up as ordered by their surgeon, specialist, or primary care physician before being considered for this study. Computed tomography scans had to be completed within 90 days of the preoperative clinic visit to meet the inclusion criteria. A trained radiologist blinded to the patient’s frailty status completed the measurements.
Postsurgical Outcome Data
Unplanned skilled nursing facility admission was the primary postoperative outcome measured. Other outcomes measures included unplanned ICU admission, delirium, ICU length of stay, hospital length of stay, rehospitalization and falls within 30 days, all-cause 30-day mortality, and 1-yr mortality were all recorded. Outcome data and complications were obtained from review of the medical record.
Normal Controls
Adult healthy volunteers who responded to a posted ad and met the inclusion and exclusion criteria were considered normal controls for this study. Recruitment of healthy volunteers was approved by the institutional review board, and written consent was obtained from each participant. Volunteers received no payment for their participation. Healthy volunteers were eligible to participate if they were adults with the capacity to consent and denied having a history of diabetes, coronary artery disease, myocardial infarct, renal disease, cerebral vascular accident, neurocognitive deficits, or reduced mobility. Healthy volunteers completed the Fried frailty phenotype assessments as noted previously, and ultrasound images of the quadriceps depth, rectus femoris cross-sectional area, and rectus femoris circumference were acquired using the same technique and by the same sonographer as noted previously.
Power Analysis
A sample size of 32 gives a precision on a 95% CI of the area under the curve to be approximately ±0.18 if we assume a discrimination magnitude of approximately 0.70. We felt this level of discrimination between frail/not-frail was adequate for what we were expecting with our ultrasound parameters because this would yield a statistically significant result.
Statistical Analysis
The results are presented as frequency of patients (percentage) or means (SD) where applicable unless otherwise noted. Differences among the frail and not-frail groups were tested using independent sample t tests or chi-square tests as appropriate. Receiver operating characteristic curve analysis was used to determine the ability of psoas muscle area, rectus femoris, and quadriceps ultrasound measurements to discriminate between frail and not-frail patients (as well as secondary outcomes). The data are presented as unadjusted and indexed area under the curve with 95% CI. Standard mean differences were computed using methods described by Yang and Dalton.21 We also computed exploratory cutoffs for each measure using Youden’s index with respective sensitivity, specificity, negative predictive value, and positive predictive value. Box plots were constructed to visualize the different ultrasound parameters between groups (frail, not frail, and controls). Rectus femoris and quadriceps ultrasound measurements were taken three times for each patient, and the interclass correlation coefficient was determined for each test. Because table 1 presents results from 40 statistical tests without adjustment, we computed the false discovery rate.22 All tests were two-tailed. All statistical analyses were performed using SPSS V25 (IBM, USA).
Table 1.
Postoperative Outcomes
| Area under the Curve (95% CI) | |||||
|---|---|---|---|---|---|
| Outcome | Fried Phenotype | Quadriceps Depth | Rectus Femoris Cross-sectional Area | Psoas Muscle Area | Rectus Femoris Circumference |
| Unplanned skilled nursing facility admission | 0.75 (0.56, 0.94) | 0.81 (0.61, 1.00) | 0.77 (0.60, 0.94) | 0.68 (0.48, 0.88) | 0.79 (0.61, 0.96) |
| Unplanned ICU admission | 0.61 (0.32, 0.89) | 0.70 (0.48, 0.92) | 0.72 (0.52, 0.92) | 0.80 (0.62, 0.98) | 0.70 (0.46, 0.93) |
| Delirium | 0.75 (0.56, 0.94) | 0.89 (0.77, 1.00) | 0.79 (0.63, 0.95) | 0.76 (0.58, 0.95) | 0.63 (0.38, 0.87) |
| ICU length of stay | 0.54 (0.31, 0.77) | 0.69 (0.51, 0.87) | 0.78 (0.62, 0.93) | 0.66 (0.43, 0.90) | 0.76 (0.59, 0.92) |
| Hospital length of stay | 0.65 (0.45, 0.85) | 0.53 (0.32, 0.73) | 0.58 (0.38, 0.79) | 0.59 (0.37, 0.80) | 0.60 (0.40, 0.81) |
| Falls | 0.73 (0.48, 0.99) | 0.63 (0.39, 0.88) | 0.77 (0.62, 0.92) | 0.72 (0.39, 1.00) | 0.65 (0.43, 0.88) |
| Rehospitalization | 0.52 (0.24, 0.80) | 0.51 (0.25, 0.77) | 0.55 (0.28, 0.82) | 0.63 (0.32, 0.94) | 0.52 (0.27, 0.77) |
| 30-day mortality | No deaths | No deaths | No deaths | No deaths | No deaths |
| 1-yr mortality | 0.77 (0.60, 0.94) | 0.70 (0.50, 0.90) | 0.64 (0.42, 0.85) | 0.79 (0.60, 0.97) | 0.65 (0.45, 0.86) |
ICU, intensive care unit.
Results
From February 2019 to March 2020, 34 patients and 20 healthy volunteers consented to participate in this study. Of the 34 patients recruited, we excluded two patients whose surgery was cancelled (fig. 1). Participants were characterized as “frail” or “not frail” based on the Fried frailty phenotype criteria. Frailty was defined when three or more of the Fried frailty phenotype measures (described previously) were present. Frailty was identified in 18 of the 32 patients or 56% of our study population. The median age was 66 yr (49 to 95) in frail patients, 57 yr (33 to 72) in not-frail patients, and 36 yr (28 to 61) in the control group. Women represented 61% of the frail group, 71% of the not-frail group, and 60% of the control group. The demographic data and baseline characteristics (table 2) showed no statistical differences between the groups. Fried frailty assessments were used as the reference standard. Point-of-care ultrasound and computed tomography scans were used as index tests. Point-of-care ultrasound images were captured on the same day as the Fried frailty assessments. Computed tomography scan images were captured within 90 days (mean interval of 39 days) of the Fried frailty assessments. Two patients in the frail group had interventions (one colonoscopy and one inferior vena cava filter placement, both under monitored anesthesia care) and three patients in the not-frail group had interventions (three colonoscopies under monitored anesthesia care) between computed tomography scans and frailty assessments. There were no missing data in the analysis.
Fig. 1.
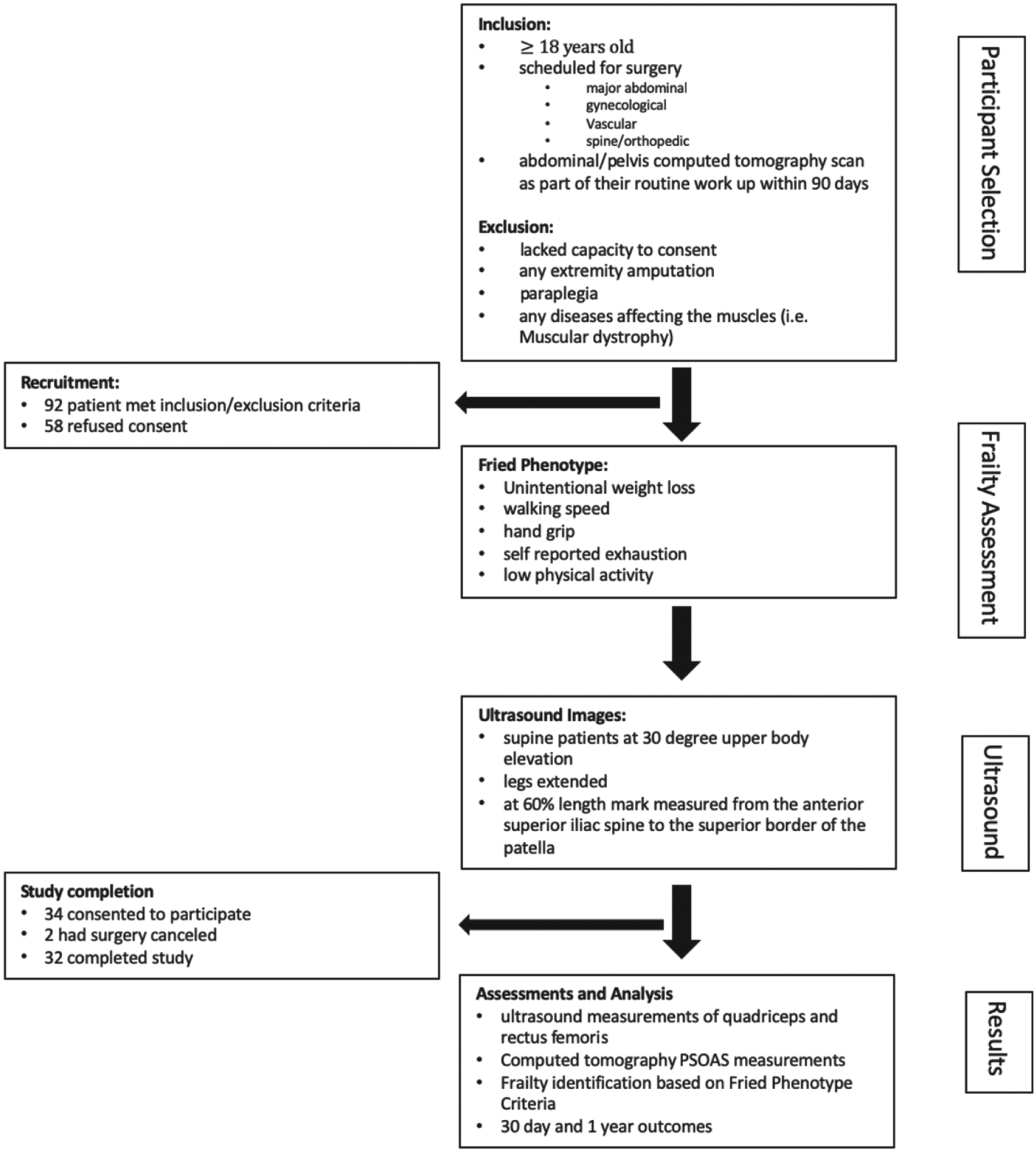
Study flow diagram.
Table 2.
Demographic and Baseline Characteristics of Participants
| Participant Characteristics | Not Frail (N = 14) | Frail (N = 18) | Standard Mean Difference |
|---|---|---|---|
| At-risk patients | |||
| Age, mean in yr | 57 ± 12 | 66 ± 13 | 0.74 |
| Female | 10 (71%) | 11 (61%) | 0.22 |
| Body mass index, kg/m2 | 28.8 ± 5.0 | 26.7 ± 7.2 | 0.34 |
| Body surface area, m2 | 1.91 ± 0.19 | 1.83 ± 0.27 | 0.36 |
| Ethnicity | |||
| Caucasian | 11 (79%) | 10 (55%) | 1.25 |
| Hispanic | 0 (0%) | 5 (28%) | |
| Asian | 1 (7%) | 1 (6%) | |
| African American/Black | 2 (14%) | 0 (0%) | |
| Other | 0 (0%) | 2 (11%) | |
| ASA status | 0.33 | ||
| I | 2 (14%) | 1 (6%) | |
| II | 2 (14%) | 3 (17%) | |
| III | 8 (57%) | 12 (67%) | |
| IV | 2 (14%) | 2 (11%) | |
| Type of surgery | 1.03 | ||
| General (major abdominal) | 1 (7%) | 6 (33%) | |
| Orthopedic/spine | 2 (14%) | 5 (28%) | |
| Gynecologic oncology | 6 (43%) | 3 (17%) | |
| Urologic oncology | 4 (28%) | 2 (11%) | |
| Vascular | 1 (7%) | 2 (11%) | |
| Healthy volunteers | |||
| Age, mean in yr | 36 ± 10 | ||
| Female | 12 (60%) | ||
| Body mass index, kg/m2 | 24.7 ± 4.57 | ||
| Body surface area, m2 | 1.8 ± 0.23 | ||
| Ethnicity | |||
| Caucasian | 7 (35%) | ||
| Hispanic | 5 (25%) | ||
| Asian | 6 (30%) | ||
| African American/Black | 0 (0%) | ||
| Other | 2 (10%) |
The values are expressed as n (%) or means ± SD. “Frail” was defined using the Fried phenotype criteria.
ASA, American Society of Anesthesiologists.
Primary Outcome
The primary aim was to estimate the discriminatory value of ultrasound measurement of the quadriceps and rectus femoris to identify frail patients. Receiver operating characteristic analysis showed the following area under the curve values: psoas muscle area, 0.88 (95% CI, 0.76 to 1.00); quadriceps depth, 0.80 (95% CI, 0.64 to 0.97); rectus femoris cross-sectional area, 0.70 (95% CI, 0.49 to 0.91); and rectus femoris circumference, 0.67 (95% CI, 0.46 to 0.88). When normalized by body mass index, the area under the curve values were as follows: psoas muscle area, 0.80 (95% CI, 0.65 to 0.91); quadriceps depth, 0.76 (95% CI, 0.57 to 0.95); rectus femoris cross-sectional area, 0.71 (95% CI, 0.50 to 0.92); and rectus femoris circumference, 0.61 (95% CI, 0.41 to 0.82). When normalized by body surface area, the area under the curve values were as follows: psoas muscle area, 0.95 (95% CI, 0.89 to 1.00); quadriceps depth, 0.77 (95% CI, 0.58 to 0.97); rectus femoris cross-sectional area, 0.71 (95% CI, 0.51 to 0.92); and rectus femoris circumference, 0.63 (95% CI, 0.43 to 0.84). Table 3 shows the Youden’s score cutoff points for the different measurements. Figures 2 and 3 visualize the relative muscle mass differences as measured by ultrasound and computed tomography imaging for the frail and not frail groups. Measurements of healthy controls are included for comparison purposes. Ultrasound measurement of quadriceps depth, rectus femoris cross-sectional area, and rectus femoris circumference were taken three times for each patient to determine the reliability of assessments. The intraclass correlation coefficient were as follows: quadriceps depth, 0.97; rectus femoris cross-sectional area, 0.95; and rectus femoris circumference, 0.94.
Table 3.
Cutoff Points of Frail and Not-Frail Patients Based on Fried Phenotype Frailty Assessment
| Direct Measurements | ||||||
|---|---|---|---|---|---|---|
| Characteristic | Cutoff | Sensitivity (95% CI) | Specificity (95% CI) | Negative Predictive value (95% CI) | Positive Predictive Value (95% CI) | Area under the Curve (95% CI) |
| Healthy controls | ||||||
| Quadriceps depth, cm | 2.3 | 0.94 (0.74, 0.99) | 0.64 (0.39, 0.84) | 0.90 (0.60, 0.98) | 0.77 (0.57, 0.90) | 0.80 (0.64, 0.97) |
| Rectus femoris cross-sectional area, cm2 | 6.2 | 1.00 (0.82, 1.00) | 0.57 (0.33, 0.79) | 1.00 (0.68, 1.00) | 0.75 (0.55, 0.88) | 0.70 (0.49, 0.91) |
| Psoas muscle area, cm2 | 18.5 | 0.78 (0.55, 0.91) | 0.93 (0.69, 0.99) | 0.76 (0.53, 0.90) | 0.93 (0.70, 0.99) | 0.88 (0.76, 1.00) |
| Rectus femoris circumference, cm | 12.9 | 0.89 (0.67, 0.97) | 0.57 (0.33, 0.79) | 0.80 (0.49, 0.94) | 0.73 (0.52, 0.87) | 0.67 (0.46, 0.88) |
| Normalized body mass index | ||||||
| Quadriceps depth, cm | 0.09 | 0.89 (0.67, 0.97) | 0.71 (0.45, 0.88) | 0.83 (0.55, 0.95) | 0.80 (0.58, 0.92) | 0.76 (0.57, 0.95) |
| Rectus femoris cross-sectional area, cm2 | 0.21 | 0.94 (0.74, 0.99) | 0.64 (0.39, 0.84) | 0.90 (0.60, 0.98) | 0.77 (0.57, 0.90) | 0.71 (0.50, 0.92) |
| Psoas muscle area | 0.55 | 0.50 (0.29, 0.71) | 1.00 (0.78, 1.00) | 0.61 (0.41, 0.78) | 1.00 (0.70, 1.00) | 0.80 (0.65, 0.95) |
| Rectus femoris circumference, cm | 0.44 | 0.67 (0.44, 0.84) | 0.64 (0.39, 0.84) | 0.60 (0.36, 0.80) | 0.71 (0.47, 0.87) | 0.61 (0.41, 0.82) |
| Normalized body surface area | ||||||
| Quadriceps depth, cm | 1.1 | 0.89 (0.67, 0.97) | 0.79 (0.52, 0.92) | 0.85 (0.58, 0.96) | 0.84 (0.62, 0.94) | 0.77 (0.58, 0.97) |
| Rectus femoris cross-sectional area, cm2 | 3.1 | 0.94 (0.74, 0.99) | 0.57 (0.33, 0.79) | 0.89 (0.57, 0.98) | 0.74 (0.54, 0.87) | 0.71 (0.51, 0.92) |
| Psoas muscle area | 9.7 | 0.89 (0.67, 0.97) | 0.93 (0.69, 0.99) | 0.87 (0.62, 0.96) | 0.94 (0.73, 0.99) | 0.95 (0.89, 1.00) |
| Rectus femoris circumference, cm | 6.7 | 0.78 (0.55, 0.91) | 0.57 (0.33, 0.79) | 0.67 (0.39, 0.86) | 0.70 (0.48, 0.85) | 0.63 (0.43, 0.84) |
Positive and negative predictive values were computed based on our sample frailty prevalence, which is likely not generalizable to the larger population. Our sample size was 32. The negative likelihood ratio is the ratio between the odds of a negative test result given the presence of frailty and the odds of a negative test result given the absence of frailty. The positive likelihood ratio is the ratio between the odds of a positive test result given the presence of frailty and the odds of a positive test result given the absence of frailty.
Fig. 2.
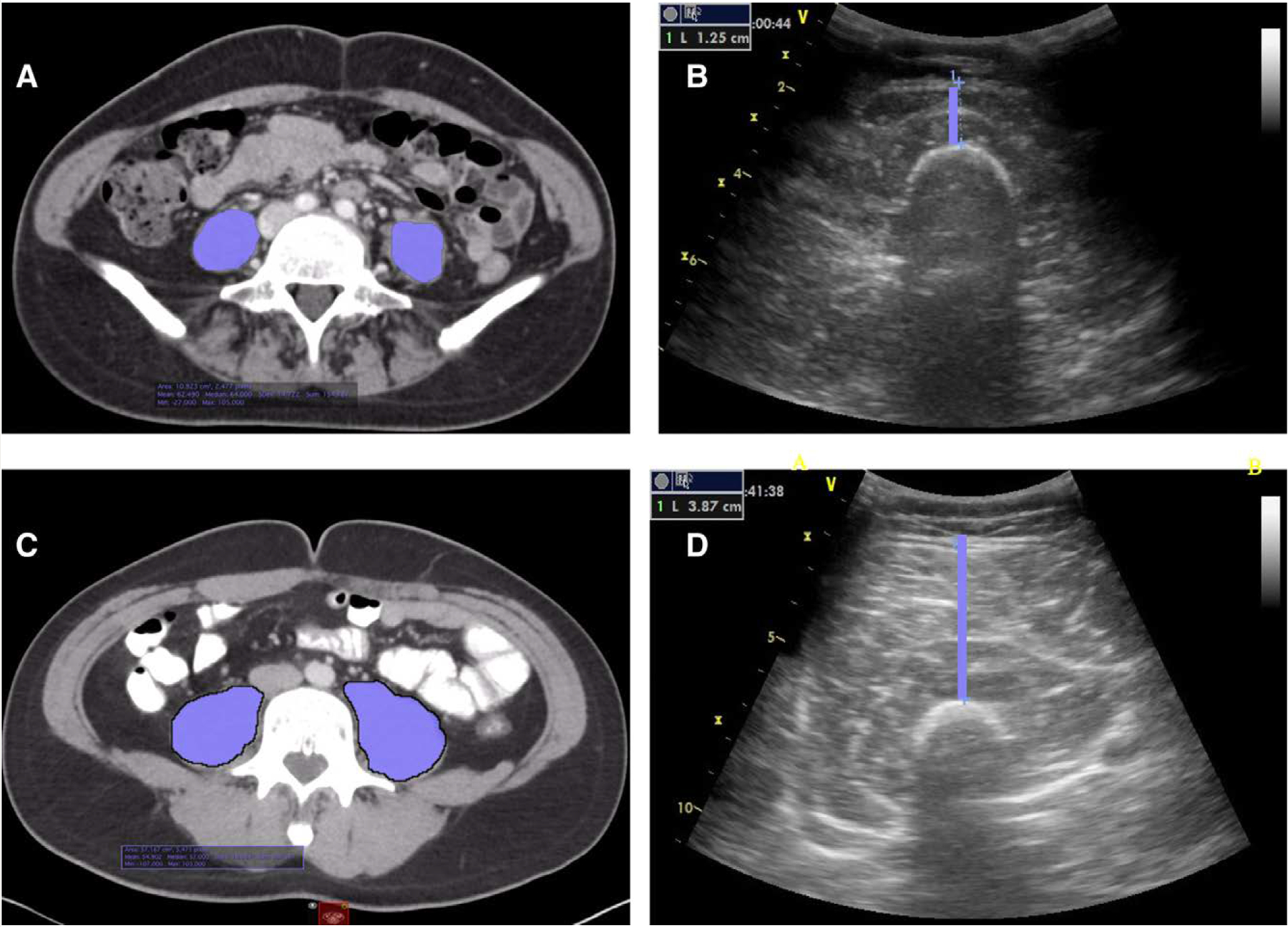
Computed tomography and ultrasound imaging of frail and not-frail patients. (A) Cross-sections of psoas muscles on computed tomography of a patient who is frail. (B) Corresponding quadriceps depth on ultrasound of the same frail patient. (C) Cross-sections of psoas muscles on computed tomography of a patient who is not frail. (D) Corresponding quadriceps depth on ultrasound of the same not-frail patient.
Fig. 3.
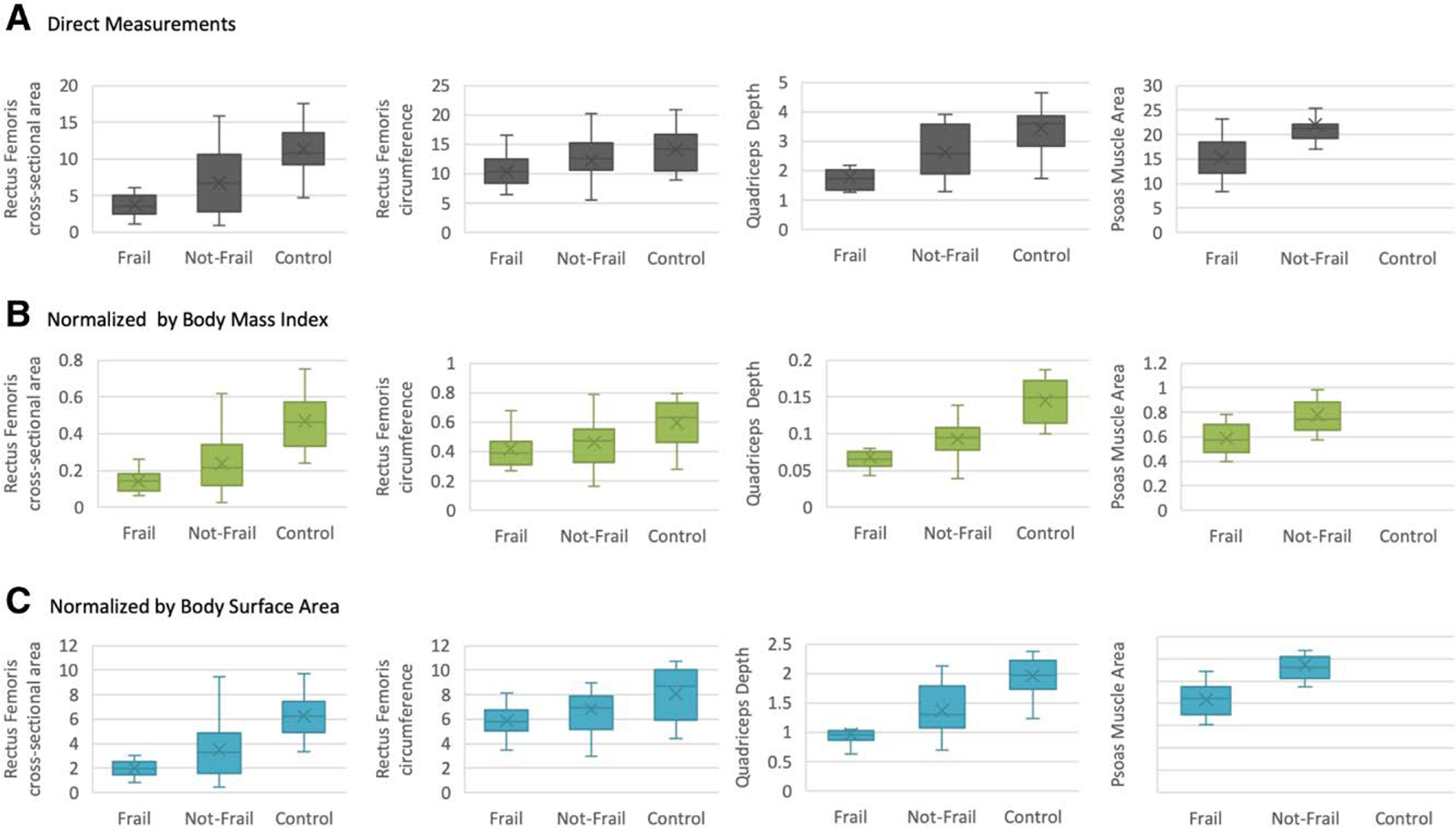
Box and whisker plot showing relative muscle mass differences in frail, not-frail, and control study subjects.
Secondary Outcomes
We also examined the ability of the various frailty measurements to predict postoperative outcomes. We collected data on unplanned skilled nursing facility admission, unplanned ICU admission, delirium, ICU length of stay, hospital length of stay, rehospitalization and falls within 30 days, and all-cause 30-day and 1-yr mortality. As shown in table 1, quadriceps depth was associated with unplanned skilled nursing facility admission (i.e., adverse discharge disposition; area under the curve, 0.81 [95% CI, 0.61 to 1.00]) and delirium (area under the curve, 0.89 [95% CI, 0.77 to 1.00]). Fried phenotype frailty assessment (area under the curve, 0.77 [95% CI, 0.60 to 0.94]) and psoas muscle area (area under the curve, 0.79 [95% CI, 0.60 to 0.970]) were associated with all-cause 1-yr mortality.
Discussion
Similar to computed tomography measurements of psoas muscle area, preoperative ultrasound measurement of quadriceps depth is able to discriminate between frail and not-frail patients before surgery. It was also able to predict skilled nursing facility admission and postoperative delirium. As the United States healthcare system population continues to age, older patients are more commonly undergoing surgery, and these patients are increasingly frail, which has a significant impact on resource utilization with increasing costs of healthcare delivery.23 Beyond resources and cost, the need to provide anesthetic care to increasingly frail patients requires an understanding of how to best manage and treat this vulnerable and aging surgical population. Frailty is not a disease we learned about in school, but a constellation of multisystem dysregulation that leads to declining physical reserve. It is important to identify frail patients because they are at greater risk of adverse outcomes, such as functional decline, hospitalization, and death in a variety of surgical settings, including cardiac, thoracic, orthopedic, general, otolaryngology, urology, and surgical oncology.4,7–10
As our knowledge of frailty evolves, understanding when and how to optimize the care for those at risk is essential. By measuring quadriceps depth, we were identifying sarcopenia, or muscle wasting, using ultrasound, a tool that has become ubiquitous with perioperative healthcare providers. Although sarcopenia and frailty are distinct entities, sarcopenia is a major component in the frailty syndrome.24 In critically ill patients, sarcopenia has long been tied to poor outcomes, poor nutrition status, and decreased ability to perform activities of daily living.25 Sarcopenia may be a viable therapeutic target for frailty intervention to improve patient outcomes and reduce healthcare expenditure.26 Specifically, nutrition and exercise programs adapted to the patient’s underlying pathology and functional status can yield improved resilience and postoperative outcomes.26 For those who present as urgent or emergent cases and cannot be optimized, the identification of frail status is still important. Knowing the frailty status before surgery can help guide anesthetic management. For example, avoidance of medications that are associated with delirium may be necessary, because frail patients are more likely to experience delirium and postoperative cognitive dysfunction.27
Although different measures exist for identifying frailty, in perioperative medicine it is important to have an easy and reproducible modality that can be used at the bedside. For example, although the frailty index is comprehensive and comprises 70 domains including mobility, mood, function, cognitive impairment, and disease states, the time requirements in applying this comprehensive measure makes it less likely to be applied in a preoperative setting. The goal of our pilot study was to identify a simple and objective measure that could be used in the bedside perioperatively whether in the preoperative clinic, trauma bay, or ICU. We found that ultrasound assessment took less than 5 min to make three consecutive measurements. In perioperative medicine, we have adopted point-of-care ultrasound in a variety of settings,28 which provides an accessible tool to quickly and easily identify frail patients. A large proportion of surgical patients do not present to a preoperative clinic, meeting their anesthetic provider minutes to hours before their surgical procedure. Further, some surgical patients, like those with hip fractures, may be unable to participate in timed walking tests to identify frailty. Therefore, although the Fried phenotype assessment is relatively quick (also 5 min or less) and easy to administer, not every patient is able to walk because of safety concerns, preexisting medical conditions, injury, or pain preoperatively, and therefore the Fried assessment cannot be applied broadly in the perioperative setting. Computed tomography imaging of psoas muscle is able to discriminate frailty in this patient population, but computed tomography imaging poses the additional risk of radiation exposure, and scheduling of scans may not be available in ambulatory settings or may be inaccessible due to demand in tertiary care centers. Ultrasound is able to be performed at the bedside, making it an important prognostic tool for frailty.
We also assessed whether frailty as defined by ultrasound measurements predicted adverse discharge disposition. Quadriceps depth was associated with unplanned skilled nursing facility admission and delirium with good discriminatory values. This is important for our surgical patients because adverse discharge disposition or unplanned skilled nursing facility admission indicates a decline in activities of daily living or independence. Delirium may be closely associated with postoperative neurocognitive dysfunction.29 Most patients seek planned surgical intervention to improve quality of life and reduce disease burden. Faced with increased likelihood of declining activities of daily living, short- or long-term skilled nursing facility care, or postoperative cognitive dysfunction, patients may elect to postpone elective surgery until they are optimized. In our study, 100% of not-frail patients went home after surgery where only 55% of frail patients went home. Knowing frailty status provides useful information regarding the risk of worse outcomes and gives perioperative health providers the ability to have meaningful discussions regarding risk.
Previously, Salim et al.30 found that postoperative ultrasound measurements of thigh muscles correlated with total lumbar skeletal muscle cross-sectional area on patient computed tomography scan to identify sarcopenia and that the inverse relationship between thigh muscle thickness and frailty existed in a group of older adults undergoing abdominal surgery. In the surgical ICU, Mueller et al.16 found that serial ultrasound measurements of the rectus femoris tracked well with sarcopenia and correlated with frailty. Our study adds to the scientific body of work by showing broader applicability of ultrasound-based frailty assessments in a heterogenous patient population that can be used preoperatively to identify those at risk for frailty and worse postoperative outcomes. Together, all three studies suggest that ultrasound-based frailty assessments can be used by perioperative physicians for preoperative surgical risk stratification, in critical care patients, and postoperatively to identify risk of postoperative complications.
Although frailty is well understood to lead to worse postoperative outcomes, how to reverse frailty and when to intervene is not well understood. Sarcopenia may be a viable therapeutic target for frailty intervention to improve patient outcomes and reduce healthcare expenditure. Future studies should focus on prehabilitation, rehabilitation, and other interventions to improve resilience and improve outcomes in frail patients. More studies are also needed to elucidate the specific impact and best practices of anesthetic management, because frailty may warrant more invasive monitoring, different mean arterial pressure goals, or lower anesthetic requirements.
Limitations
There were several limitations in our study. Our study population was limited by requiring computed tomography scans to be completed within 90 days of the preoperative clinic visit. Further, our patient population represented a heterogenous surgical population that likely indicated various degrees of functional status and outcomes from the disease burden and surgical approach, confounding the direct impact of frailty on outcomes. However, the goal of this pilot study was to identify whether ultrasound could be used reliably in a preoperative setting to identify frailty. For purposes of this study, all ultrasound and frailty assessments were performed by a trained ultrasound technician outside of the treating anesthesiology attending/resident team. Integrating ultrasound assessments without disrupting clinic workflow will require buy-in from key stakeholders in the preoperative clinic. Further work is required to establish whether ultrasound studies performed by the treating anesthesiology team have similar diagnostic and predictive performance and adequate interrater reliability. In our study, we measured quadriceps muscles via ultrasound as a measure of frailty, although psoas muscles seem to have a better discriminatory value. We specifically chose quadriceps, given the technical expertise needed to accurately and reliably measure the psoas muscle at the same anatomical level with the various body habitus and mobility limitations of many surgical patients. Our goal was to identify a simple, objective, and reproducible measure of frailty. Further, we did not have the ability to adequately control/adjust for surgery type and other patient characteristics, which likely confounded the results. Finally, it is important to keep in mind the contextual nature of discrimination testing. This study recruited individuals with suitable variability in the predictors and outcomes. Further studies will need to examine the finer discrimination in individuals who are all at high risk. We stress the exploratory nature of the study. The next phase of the study will be a more rigorous validation in which surgery type and other characteristics are considered. A more definitive study will also include interreliability to measure the ability for broad implementation.
Conclusions
In this prospective prognostic study of frailty, we found that preoperative ultrasound measurements of quadriceps depth shows promise in discriminating between frail and not-frail patients and was associated with skilled nursing facility admission and postoperative delirium.
EDITOR’S PERSPECTIVE.
What We Already Know about This Topic
Frailty is associated with a range of adverse postoperative outcomes
Screening preoperatively for frailty using traditional instruments may be challenging in some circumstances
What This Article Tells Us That Is New
Quadriceps depth defined using point-of-care ultrasound was able to predict frailty (defined using the Fried phenotype assessment) with good discrimination
Quadriceps depth was also a predictor of certain adverse postoperative outcomes including discharge to a skilled nursing facility and delirium
Additional studies with larger samples of patients are needed to confirm the clinical utility of this approach and determine whether these associations are independent of potential confounders such as surgery type
Research Support
Support was provided solely from institutional and/or departmental sources.
Competing Interests
Dr. Cannesson has funding from Masimo (Irvine, California), Edwards Lifesciences (Irvine, California), and the National Institutes of Health (Bethesda, Maryland) for unrelated work and is a shareholder of Sironis (Newport Beach, California) and Perceptive Medical (Newport Beach, California). Dr. Duval has funding from the National Institutes of Health (Bethesda, Maryland) for unrelated work. The other authors declare no competing interests.
Footnotes
This article has been selected for the Anesthesiology CME Program. Learning objectives and disclosure and ordering information can be found in the CME section at the front of this issue. This article is featured in “This Month in Anesthesiology,” page A1. This article is accompanied by an editorial on p. 255. This article has a related Infographic on p. A15. This article has a video abstract. This article has an audio podcast. This article has a visual abstract available in the online version. Part of the work presented in this article has been presented at the Anesthesiology Annual Meeting in Orlando, Florida, October 19 to 23, 2019, as part of “What’s New with the Old” Journal Symposium (JS04).
References
- 1.Xue QL: The frailty syndrome: Definition and natural history. Clin Geriatr Med 2011; 27:1–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Op het Veld LP, van Rossum E, Kempen GI, de Vet HC, Hajema K, Beurskens AJ: Fried phenotype of frailty: Cross-sectional comparison of three frailty stages on various health domains. BMC Geriatr 2015; 15:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ritt M, Schwarz C, Kronawitter V, Delinic A, Bollheimer LC, Gassmann KG, Sieber CC: Analysis of Rockwood et al.’s clinical frailty scale and Fried et al.’s frailty phenotype as predictors of mortality and other clinical outcomes in older patients who were admitted to a geriatric ward. J Nutr Health Aging 2015; 19:1043–8 [DOI] [PubMed] [Google Scholar]
- 4.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A: A global clinical measure of fitness and frailty in elderly people. CMAJ 2005; 173:489–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zylberglait Lisigurski M, Bueno YA, Karanam C, Andrade AD, Akkineni S, Cevallos V, Ruiz JG: Healthcare utilization by frail, community-dwelling older veterans: A 1-year follow-up study. South Med J 2017; 110:699–704 [DOI] [PubMed] [Google Scholar]
- 6.Eamer G, Gibson JA, Gillis C, Hsu AT, Krawczyk M, MacDonald E, Whitlock R, Khadaroo RG: Surgical frailty assessment: A missed opportunity. BMC Anesthesiol 2017; 17:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hastings SN, Purser JL, Johnson KS, Sloane RJ, Whitson HE: Frailty predicts some but not all adverse outcomes in older adults discharged from the emergency department. J Am Geriatr Soc 2008; 56:1651–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin H, Peel NM, Scott IA, Vardesh DL, Sivalingam P, McBride RL, Morong JJ, Nelson MJ, Hubbard RE: Perioperative assessment of older surgical patients using a frailty index-feasibility and association with adverse post-operative outcomes. Anaesth Intensive Care 2017; 45:676–82 [DOI] [PubMed] [Google Scholar]
- 9.Lin HS, Watts JN, Peel NM, Hubbard RE: Frailty and post-operative outcomes in older surgical patients: A systematic review. BMC Geriatr 2016; 16:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robinson TN, Wu DS, Pointer L, Dunn CL, Cleveland JC Jr, Moss M: Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg 2013; 206:544–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smart R, Carter B, McGovern J, Luckman S, Connelly A, Hewitt J, Quasim T, Moug S: Frailty exists in younger adults admitted as surgical emergency leading to adverse outcomes. J Frailty Aging 2017; 6:219–23 [DOI] [PubMed] [Google Scholar]
- 12.Pritchard JM, Kennedy CC, Karampatos S, Ioannidis G, Misiaszek B, Marr S, Patterson C, Woo T, Papaioannou A: Measuring frailty in clinical practice: A comparison of physical frailty assessment methods in a geriatric out-patient clinic. BMC Geriatr 2017; 17:264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA; Cardiovascular Health Study Collaborative Research Group: Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56:M146–56 [DOI] [PubMed] [Google Scholar]
- 14.Gruther W, Benesch T, Zorn C, Paternostro-Sluga T, Quittan M, Fialka-Moser V, Spiss C, Kainberger F, Crevenna R: Muscle wasting in intensive care patients: Ultrasound observation of the M. quadriceps femoris muscle layer. J Rehabil Med 2008; 40:185–9 [DOI] [PubMed] [Google Scholar]
- 15.Balsam LB: Psoas muscle area: A new standard for frailty assessment in cardiac surgery? J Thorac Dis 2018; 10:3846–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mueller N, Murthy S, Tainter CR, Lee J, Riddell K, Fintelmann FJ, Grabitz SD, Timm FP, Levi B, Kurth T, Eikermann M: Can sarcopenia quantified by ultrasound of the rectus femoris muscle predict adverse outcome of surgical intensive care unit patients as well as frailty?: A prospective, observational cohort study. Ann Surg 2016; 264:1116–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen JF, Korevaar DA, Altman DG, Bruns DE, Gatsonis CA, Hooft L, Irwig L, Levine D, Reitsma JB, de Vet HC, Bossuyt PM: STARD 2015 guidelines for reporting diagnostic accuracy studies: Explanation and elaboration. BMJ Open 2016; 6:e012799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Savva GM, Donoghue OA, Horgan F, O’Regan C, Cronin H, Kenny RA: Using timed up-and-go to identify frail members of the older population. J Gerontol A Biol Sci Med Sci 2013; 68:441–6 [DOI] [PubMed] [Google Scholar]
- 19.Podsiadlo D, Richardson S: The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991; 39:142–8 [DOI] [PubMed] [Google Scholar]
- 20.Stel VS, Smit JH, Pluijm SM, Visser M, Deeg DJ, Lips P: Comparison of the LASA Physical Activity Questionnaire with a 7-day diary and pedometer. J Clin Epidemiol 2004; 57:252–8 [DOI] [PubMed] [Google Scholar]
- 21.Yang D, Dalton JE: A unified approach to measuring the effect size between two groups using SAS®, SAS Global Forum, 2012, p 335 [Google Scholar]
- 22.Storey JD: A direct approach to false discovery rates. J R Stat Soc Series B Stat Methodol 2002; 64: 479–98 [Google Scholar]
- 23.Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP: Frailty: Implications for clinical practice and public health. Lancet 2019; 394:1365–75 [DOI] [PubMed] [Google Scholar]
- 24.Nascimento CM, Ingles M, Salvador-Pascual A, Cominetti MR, Gomez-Cabrera MC, Viña J: Sarcopenia, frailty and their prevention by exercise. Free Radic Biol Med 2019; 132:42–9 [DOI] [PubMed] [Google Scholar]
- 25.Canales C, Elsayes A, Yeh DD, Belcher D, Nakayama A, McCarthy CM, Chokengarmwong N, Quraishi SA: Nutrition Risk in Critically Ill versus the Nutritional Risk Screening 2002: Are they comparable for assessing risk of malnutrition in critically ill patients? JPEN J Parenter Enteral Nutr 2019; 43:81–7 [DOI] [PubMed] [Google Scholar]
- 26.Whittle J, Wischmeyer PE, Grocott MPW, Miller TE: Surgical prehabilitation: Nutrition and exercise. Anesthesiol Clin 2018; 36:567–80 [DOI] [PubMed] [Google Scholar]
- 27.Susano MJ, Grasfield RH, Friese M, Rosner B, Crosby G, Bader AM, Kang JD, Smith TR, Lu Y, Groff MW, Chi JH, Grodstein F, Culley DJ: Brief preoperative screening for frailty and cognitive impairment predicts delirium after spine surgery. Anesthesiology 2020; 133:1184–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ramsingh D, Rinehart J, Kain Z, Strom S, Canales C, Alexander B, Capatina A, Ma M, Le KV, Cannesson M: Impact assessment of perioperative point-of-care ultrasound training on anesthesiology residents. Anesthesiology 2015; 123:670–82 [DOI] [PubMed] [Google Scholar]
- 29.Daiello LA, Racine AM, Yun Gou R, Marcantonio ER, Xie Z, Kunze LJ, Vlassakov KV, Inouye SK, Jones RN, Alsop D, Travison T, Arnold S, Cooper Z, Dickerson B, Fong T, Metzger E, Pascual-Leone A, Schmitt EM, Shafi M, Cavallari M, Dai W, Dillon ST, McElhaney J, Guttmann C, Hshieh T, Kuchel G, Libermann T, Ngo L, Press D, Saczynski J, Vasunilashorn S, O’Connor M, Kimchi E, Strauss J, Wong B, Belkin M, Ayres D, Callery M, Pomposelli F, Wright J, Schermerhorn M, Abrantes T, Albuquerque A, Bertrand S, Brown A, Callahan A, D’Aquila M, Dowal S, Fox M, Gallagher J, Anna Gersten R, Hodara A, Helfand B, Inloes J, Kettell J, Kuczmarska A, Nee J, Nemeth E, Ochsner L, Palihnich K, Parisi K, Puelle M, Rastegar S, Vella M, Xu G, Bryan M, Guess J, Enghorn D, Gross A, Gou Y, Habtemariam D, Isaza I, Kosar C, Rockett C, Tommet D, Gruen T, Ross M, Tasker K, Gee J, Kolanowski A, Pisani M, de Rooij S, Rogers S, Studenski S, Stern Y, Whittemore A, Gottlieb G, Orav J, Sperling R; SAGES Study Group: Postoperative delirium and postoperative cognitive dysfunction: Overlap and divergence. Anesthesiology 2019; 131:477–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Salim SY, Al-Khathiri O, Tandon P, Baracos VE, Churchill TA, Warkentin LM, Khadaroo RG: Thigh ultrasound used to identify frail elderly patients with sarcopenia undergoing surgery: A pilot study. J Surg Res 2020; 256:422–32 [DOI] [PubMed] [Google Scholar]


