Abstract
Infection by pneumococci causes an acute inflammatory response associated with neutrophil influx, increased vascular permeability, and edema. Vascular endothelial growth factor (VEGF) is one of the most potent regulators of endothelial permeability. In vitro stimulation of neutrophils showed that pneumococci and purified pneumococcal cell wall induce VEGF secretion, independent of the presence of pneumolysin or polysaccharide capsule. The results of this study indicate VEGF is secreted in pneumococcal disease, suggesting a role as a mediator of increased vascular permeability.
Streptococcus pneumoniae is a major cause of pneumonia, septicemia, and meningitis. Pneumococcal infection induces host responses associated with acute inflammation. One of the key characteristics of acute inflammation is edema caused by increased vascular permeability. During pneumococcal infection, increased vascular permeability may result in vasogenic brain edema in meningitis, as well as empyema, pleural effusion, and pulmonary consolidation in pneumonia.
One of the most potent regulators of endothelial permeability is vascular endothelial growth factor (VEGF), also called vascular permeability factor. Only minutes after administration of VEGF, small capillaries and venules display endothelial fenestration and opening of tight junctions (12). VEGF has been involved in several disease states characterized by edema and increased vascular permeability, including rheumatoid arthritis, brain edema following trauma or tumor growth, allergic diseases, and parainfectious pleural effusions (1, 2, 5, 9, 13, 19). VEGF is also an endothelial mitogen which promotes embryonal vascular development and neovascularization in tumor growth (3, 6). VEGF is produced by a broad range of cell types, including macrophages, platelets, and neutrophils (4). The expression of VEGF is regulated by various stimuli, such as inflammatory cytokines (interleukin-1, tumor necrosis factor alpha, gamma interferon), hypoxia, and lipopolysaccharide (11, 18). The first line of defense against pneumococci consists predominantly of neutrophils. Since neutrophils are associated with the initial inflammatory response and can produce VEGF, we hypothesized that the increase in vascular permeability observed in pneumococcal disease may be mediated by VEGF. In this study, we assessed whether pneumococci and pneumococcal components induce secretion of VEGF by human neutrophils.
Bacterial strains, growth conditions, and pneumococcal components.
The strains of S. pneumoniae tested were S3 (serotype 3; American Type Culture Collection), D39 (serotype 2), and two isogenic mutants: the pneumolysin-negative mutant PLN-A and the unencapsulated derivative R6 (a kind gift from E. Tuomanen). Bacteria were grown in Todd-Hewitt broth to mid-logarithmic phase (optical density at 660 nm of 0.5). Alternatively, bacteria were grown on tryptic soy agar containing 5% sheep blood for 16 to 18 h at 37°C in 5% CO2. Mutant strain PLN-A was grown in the presence of erythromycin (1 μg ml−1) to maintain an environment selective for the mutant. For some experiments, bacteria were killed by heating for 10 min at 60°C. Purified cell wall was prepared from strain S3 as described previously (15). Briefly, logarithmically growing pneumococci were heat killed. Crude cell wall was extracted in 5% sodium dodecyl sulfate at 100°C for 15 min. The pellet was washed to remove detergent and then vortexed with glass beads to mechanically break any remaining intact cells. After treatment with DNase, RNase, and finally trypsin to remove associated proteins, the cell wall was reprecipitated in sodium dodecyl sulfate, washed, vacuum dried, and stored at room temperature. The cellular equivalent of 0.02 μg of cell wall approximates 105 cells (17). The pneumococcal polysaccharide vaccine Pneumovax 23 was purchased from Pasteur Mérieux MSD (Brussels, Belgium). The cellular equivalent of 0.2 μg of capsular polysaccharide approximates 105 cells (10).
Isolation and stimulation of neutrophils and VEGF measurement.
Neutrophils were isolated by a Ficoll-Histopaque gradient from peripheral blood of healthy volunteers as described previously (14). Neutrophils were resuspended in RPMI 1640 containing 1% heat-inactivated fetal calf serum. The viability of cells exceeded 95% as determined by trypan blue exclusion. Purity was checked by optical and impedance analysis (Abbott Cell Dyn 3500) and was >98%; in the purified neutrophil fraction, platelets represented one-fifth of the cells. Neutrophils (1.25 × 106 cells; 0.5 ml) were stimulated with live or heat-killed pneumococci or pneumococcal components at 37°C for 0 to 4 h in a water bath shaker. As a positive control, cells were incubated with cytochalasin B (10 μg ml−1) for 30 min, followed by addition of formylmethionylleucylphenylalanine (fMLP) at 1 μM for 30 min. As a negative control, cells were incubated with medium alone. Experiments were carried out aseptically to avoid endotoxin contamination. In addition, polymyxin B (Sigma Chemical Co., St. Louis, Mo.) was added to all test mixtures at a final concentration of 10 μg ml−1 to abolish the stimulatory effects of endotoxin (8). After incubation, the samples were centrifuged at 350 × g, and the supernatants were collected and stored at −70°C prior to VEGF assays. A commercially available human VEGF enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems Europe, Abingdon, United Kingdom) was used to measure VEGF in culture supernatants. Measurements were done according to the manufacturer's protocol. All data are expressed as means ± standard deviations (SD).
Pneumococci induce dose- and time-dependent VEGF secretion.
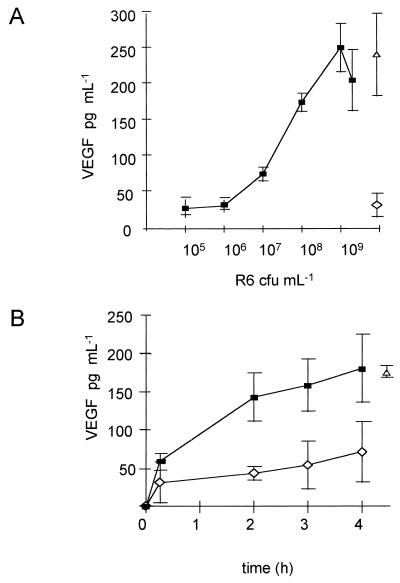
To determine the dose effects and kinetics of pneumococcus-induced VEGF secretion, freshly isolated neutrophils were incubated with heat-killed S. pneumoniae (R6) suspensions of several concentrations for 0 to 4 h. Heat-killed pneumococci were used to avoid differences in pneumococcal concentration during the stimulation assay due to bacterial growth and lysis. Pneumococcal suspensions at a concentration of ≥∼107 CFU ml−1 (multiplicity of infection of ≥4) induced VEGF secretion (Fig. 1A). Release of VEGF reached a plateau at a concentration of ∼108 to 109 CFU ml−1 (multiplicity of infection of ∼40 to 400). Though relatively high numbers of pneumococci were needed, these concentrations are not unlike those encountered in clinical disease: during meningitis, bacterial concentrations in the cerebrospinal fluid as high as 4 × 109 CFU ml−1 may be reached, and in >50% of patients concentrations of ∼107 CFU ml−1 are found (7). Kinetics studies showed that the VEGF concentration in the supernatant was increased at 2 h and accumulated to a plateau at 4 h (Fig. 1B).
FIG. 1.
(A) Dose-effect curve of VEGF secretion by human neutrophils (2.5 × 106 neutrophils ml−1) following stimulation with different doses of heat-killed S. pneumoniae R6 at 37°C for 4 h. (B) Kinetics of VEGF secretion by human neutrophils (2.5 × 106 neutrophils ml−1) following stimulation with heat-killed S. pneumoniae R6 at a concentration of 109 CFU ml−1 at 37°C for 0 to 4 h. Results are means ± SD of ≥2 independent experiments with blood from different donors and ELISA performed in duplicate. Symbols for stimuli: ■, R6; ◊, medium alone; ▵, cytochalasin B (10 μg ml−1) plus fMLP (10 μM).
The possibility that hematogenous cells other than neutrophils accounted for the VEGF production is unlikely: VEGF levels did not increase above background values when samples of monocytes, lymphocytes, or platelets (10-fold greater in number than in the purified neutrophil fraction) were stimulated with pneumococci using the same protocol (data not shown).
Characterization of pneumococcal stimulus.
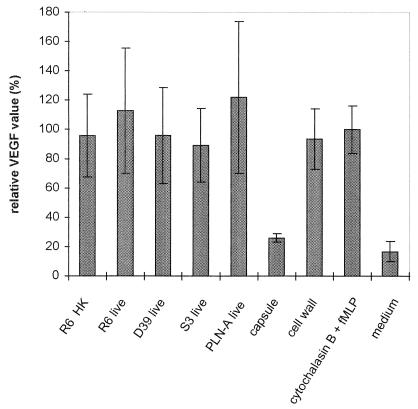
Based on the dose and kinetics experiments, for all subsequent experiments 4-h incubations with bacterial suspensions of ∼108 to 109 CFU ml−1 were used. As shown in Fig. 2, no difference was found between live and heat-killed S. pneumoniae R6. In addition, both encapsulated pneumococci (D39 and S3) and unencapsulated pneumococci (R6) induced VEGF secretion, though the unencapsulated pneumococcal strain was slightly more effective.
FIG. 2.
VEGF secretion by neutrophils following incubation with different stimuli at 37°C for 4 h. Live pneumococci were tested at 109 CFU ml−1. Polysaccharide capsule and pneumococcal cell wall were tested at a cell equivalent of 108 CFU ml−1. Incubation with cytochalasin B (10 μg ml−1) for 30 min followed by fMLP (10 μM) for 30 min served as a positive control; medium alone served as negative control. Data are percentages of the positive control (means ± SD [error bars]) and represent two independent experiments with blood from different donors and ELISA performed in duplicate.
Next we studied the intracellular pneumococcal toxin pneumolysin, purified capsular polysaccharide, and cell wall for the ability to trigger VEGF secretion. The pneumolysin-negative mutant PLN-A was compared for its capacity to induce VEGF secretion to its parent strain D39. PLN-A showed no reduced response, suggesting a pneumolysin-independent mechanism of neutrophil stimulation (Fig. 2). This is consistent with the finding that heat-killed pneumococci, which cannot actively secrete pneumolysin, induce VEGF secretion from neutrophils. Pneumococcal polysaccharide at a concentration of 230 μg ml−1 (cell equivalent, ∼108 ml−1) induced no VEGF secretion above background values of the negative control. However, purified pneumococcal cell wall at a concentration of 20 μg ml−1 (cell equivalent, 108 ml−1) induced similar VEGF release as heat-killed pneumococcus strain R6 at ∼108 CFU ml−1 (Fig. 2). Our finding that the pneumococcal cell wall is capable of effective induction of VEGF secretion is consistent with previous findings in animal models: when injected intracisternally in rabbits, pneumococcal cell wall causes neutrophil influx and disruption of the blood-brain barrier, with brain edema as a result (15); similarly, pneumococcal cell wall induces pulmonary inflammation, with accumulation of protein in the bronchoalveolar lavage fluid (16). The increased vascular permeability found in the animal studies may be mediated by VEGF. Pneumococcal capsular polysaccharide failed to induce VEGF secretion in our assay, consistent with the absence of inflammatory changes in the above-mentioned animal models.
The simultaneous influx of neutrophils and increase in vascular permeability during acute inflammation in pneumococcal disease and the ability of neutrophils to secrete VEGF, when stimulated with whole pneumococci or pneumococcal cell wall as shown in this study, suggest that VEGF is a mediator of vascular permeability and formation of edema in pneumococcal disease. This observation may have significance for future research on therapeutic inhibitory drugs aimed at blocking excessive vascular leak and edema in infectious diseases.
Acknowledgments
M. van der Flier was supported by a stipend from the Medical Branch of the Dutch Sciences Organization (MW-NWO AGIKO no. 920-03-077).
REFERENCES
- 1.Boesiger J, Tsai M, Yamaguchi M, Brown L F, Claffey K P, Dvorak H F, Galli S J. Mast cells can secrete vascular permeability factor/vascular endothelial growth factor and exhibit enhanced release after immunoglobulin E-dependent upregulation of fc epsilon receptor I expression. J Exp Med. 1998;188:1135–1145. doi: 10.1084/jem.188.6.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fava R A, Olsen N J, Spencer-Green G, Yeo K, Berse B, Jackman R W, Senger D R, Dvorak H F, Brown L F. Vascular permeability factor/endothelial growth factor (VPF/VEGF): accumulation and expression in human synovial fluids and rheumatoid synovial tissue. J Exp Med. 1994;180:341–346. doi: 10.1084/jem.180.1.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferrara N, Carver-Moore K, Chen H, Dowd M, Lu L, O'Shea K S, Powell-Braxton L, Hillan K J, Moore M W. Heterozygous embryonic lethality induced by targeted inactivation of the VEGF gene. Nature. 1996;380:439–442. doi: 10.1038/380439a0. [DOI] [PubMed] [Google Scholar]
- 4.Gaudry M, Bregerie O, Andrieu V, El Benna J, Pocidalo M A, Hakim J. Intracellular pool of vascular endothelial growth factor in human neutrophils. Blood. 1997;90:4153–4161. [PubMed] [Google Scholar]
- 5.Heiss J D, Papavassiliou E, Merrill M J, Nieman L, Knightly J J, Walbridge S, Edwards N A. Mechanism of dexamethasone suppression of brain tumor-associated vascular permeability in rats: involvement of the glucocorticoid receptor and vascular permeability factor. J Clin Investig. 1996;98:1400–1408. doi: 10.1172/JCI118927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kolch W, Martiny-Baron G, Kieser A, Marme D. Regulation of the expression of the VEGF/VPS and its receptors: role in tumor angiogenesis. Breast Cancer Res Treat. 1995;36:139–155. doi: 10.1007/BF00666036. [DOI] [PubMed] [Google Scholar]
- 7.Mariani-Kurkdjian P, Doit C, Le Thomas I, Aujard Y, Bourrillon A, Bingen E. Bacterial concentration in the cerebrospinal fluid in childhood meningitis. Presse Med. 1999;28:1227–1230. [PubMed] [Google Scholar]
- 8.Mattson E, Rollof J, Verhoef J, van Dijk H, Fleer A. Serum-induced potentiation of tumor necrosis factor alpha production by human leukocytes in response to staphylococcal peptidoglycan: involvement of different serum factors. Infect Immun. 1994;62:3837–3843. doi: 10.1128/iai.62.9.3837-3843.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nag S, Takahashi J L, Kilty D W. Role of vascular endothelial growth factor in blood-brain barrier breakdown and angiogenesis in brain trauma. J Neuropathol Exp Neur. 1997;56:912–921. doi: 10.1097/00005072-199708000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Nolan C M, Ulmer W C. Enzyme immunoassay of the capsular polysaccharide of Streptococcus pneumoniae type III in cerebrospinal fluid in experimental meningitis. J Med Microb. 1980;13:551–560. doi: 10.1099/00222615-13-4-551. [DOI] [PubMed] [Google Scholar]
- 11.Perez-Ruiz M, Ros J, Morales-Ruiz M, Navasa M, Colmenero J, Ruiz-Del-Arbol L, Cejudo P, Claria J, Rivera F, Arrovo V, Rodes J, Jimenez W. Vascular endothelial growth factor production in peritoneal macrophages of cirrhotic patients: regulation by cytokines and bacterial lipopolysaccharide. Hepatology. 1999;29:1057–1063. doi: 10.1002/hep.510290416. [DOI] [PubMed] [Google Scholar]
- 12.Roberts W G, Palade G E. Increased microvascular permeability and endothelial fenestration induced by vascular endothelial growth factor. J Cell Sci. 1995;108:2369–2379. doi: 10.1242/jcs.108.6.2369. [DOI] [PubMed] [Google Scholar]
- 13.Thickett D R, Armstrong L, Millar A B. Vascular endothelial growth factor (VEGF) in inflammatory and malignant pleural effusions. Thorax. 1999;54:707–710. doi: 10.1136/thx.54.8.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Troelstra A, de Graaf-Miltenburg L A, van Bommel T, Verhoef J, van Kessel K P, van Strijp J A. Lipopolysaccharide-coated erythrocytes activate human neutrophils via CD14 while subsequent binding is through CD11b/CD18. J Immunol. 1999;162:4220–4225. [PubMed] [Google Scholar]
- 15.Tuomanen E, Liu H, Hengstler B, Zak O, Tomasz A. The induction of meningeal inflammation by components of the pneumococcal cell wall. J Infect Dis. 1985;151:859–868. doi: 10.1093/infdis/151.5.859. [DOI] [PubMed] [Google Scholar]
- 16.Tuomanen E, Rich R, Zak O. Induction of pulmonary inflammation by components of the pneumococcal cell surface. Am Rev Respir Dis. 1987;135:869–874. doi: 10.1164/arrd.1987.135.4.869. [DOI] [PubMed] [Google Scholar]
- 17.Tuomanen E, Tomasz A, Hengstler B, Zak O. The relative role of bacterial cell wall and capsule in the induction of inflammation in pneumococcal meningitis. J Infect Dis. 1985;151:535–540. doi: 10.1093/infdis/151.3.535. [DOI] [PubMed] [Google Scholar]
- 18.Xiong M, Elson G, Legarda D, Leibovich S J. Production of vascular endothelial growth factor by murine macrophages. Am J Pathol. 1998;153:587–598. doi: 10.1016/S0002-9440(10)65601-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yeo K, Wang H H, Nagy J A, Sioussat T M, Ledbetter S R, Hoogewerf A J, Zhou Y, Masse E M, Senger D R, Dvorak H F, Yeo T. Vascular permeability factor (vascular endothelial growth factor) in guinea pig and human tumor effusions. Cancer Res. 1993;53:2912–2918. [PubMed] [Google Scholar]