Abstract
PURPOSE:
We examined how longitudinal changes and inter-community differences of food insecurity rates were associated with child maltreatment report (CMR) rates at the zip code level. We assessed these associations overall, by urbanicity, and within subgroups of age and maltreatment type.
METHODS:
We used Illinois statewide zip code-level data from 2011-2018. We measured CMR rates based on Illinois child protective services records and food insecurity rates from Feeding America’s Map the Meal Gap. We used linear spatial-temporal autoregressive models with controls for various socioeconomic, demographic, care burden, and instability conditions of communities.
RESULTS:
Both longitudinal changes and inter-community differences of food insecurity rates were significantly associated with increased CMR rates overall and within all subgroups. These associations were significant among all large urban, small urban, and rural areas, while longitudinal changes of food insecurity rates had significantly stronger associations among small urban and rural areas than among large urban areas.
CONCLUSIONS:
Communities experiencing higher food insecurity had higher CMR rates. Increases in food insecurity over time were also associated with increases in CMR rates. These associations were reproduced within subgroups of child age, maltreatment type, and urbanicity. Attention and collaborative efforts are warranted for high food-insecure communities.
Introduction
Food insecurity (FI) and child maltreatment (CM) are major public health problems. In 2020, 14.8% of U.S. children lived in food-insecure households [1], and in 2019, 4.7% of U.S. children were reported to child protective services for CM [2]. Emerging evidence documents a strong FI-CM association [3–8]. This is concerning because both problems increase the risk of a wide range of negative outcomes for children, including developmental, cognitive, psychological, behavioral, and health problems [9–16].
Existing research focuses on individual-level pathways from FI to CM. For example, stress theory suggests that FI provokes parental distress, which creates conflicts and violence between family members and eventually increases CM risk [5,17]. While research is scant, community-level pathways from FI to CM are also possible. A sociological perspective suggests that concentrated disadvantages, such as FI, may weaken protective neighborhood processes (e.g., collective efficacy) that can alleviate community problems, including CM [18]. A psychological perspective proposes that concentrated disadvantages may function as environmental stressors, and when families have few social supports to mitigate environmental stressors, CM risk may escalate [19].
Prior FI-CM studies are limited to individual-level relationships, high-risk samples, and local and mostly urban data [3–8]. These limitations hinder our ability to shape good interventions in several important ways. First, understanding community-level relationships has important practical implications given the emphasis on community-based interventions in both public health and social work [20,21]. It also has strong implications for shaping policy measures, identifying high-risk communities and geographically allocating services and resources. Second, from a public health perspective, understanding impacts of risk factors in a general population can inform programs and policies seeking population-level impacts [22,23]. Finally, emerging research suggests that CM contexts may differ by urbanicity [24,25]. This requires using data across all urban-rural areas and examining impacts of risk/protective factors by urbanicity to develop tailored responses to local contexts and needs.
This study examines community-level associations between FI and CM report (CMR) rates, using Illinois statewide zip code-level data from 2011-2018. This is built upon the unique opportunity to access 2011-2018 Illinois CMR records, including residential zip code information, which is confidential and unavailable in national and most other states’ data. Both longitudinal changes (i.e., within-effects) and inter-community differences (i.e., between-effects) of FI rates were considered for their associations with CMR rates. Additional analysis tested whether these associations differed by urbanicity. Compared with large urban areas, small urban and rural areas have fewer social service providers, including physical/behavioral health professionals [26–28]. Although these professionals make over one-fourth of CMRs in the U.S. [2], a recent national study identifies no systematic underreporting of CM incidents in small urban or rural areas in spite of the shortages [25]. Rather, CMR rates are higher in these areas, both overall and from these professionals [25]. We expect that the impacts of community FI may be greater in small urban and rural areas than large urban areas because the shortage of social service providers in small urban and rural areas may aggravate community FI and its consequences. We estimated these associations overall, as well as within subgroups of age and CM type. Younger children have substantially higher CMR risks than older children [2]. Some research suggests that the lower physical and cognitive capabilities and the greater care needs of younger children may interact with CM risk factors [29]. Regarding CM type, prior research suggests that impacts of community economic conditions may differ by type, with neglect showing the largest impacts, followed by physical abuse and sexual abuse [30].
Methods
Data/Sample
We constructed zip code-level data based on Illinois statewide administrative/archival data from 2011-2018. We used all official CMRs, investigated by the Illinois Department of Children and Family Services (DCFS) in 2011-2018. This study included both substantiated CMRs (about 20% of CMRs that DCFS identified as having enough evidence to legally substantiate CM allegations) and unsubstantiated CMRs (about 80% of CMRs) because of strong evidence suggesting substantiation decisions are unreliable [31–35]. Substantiated and unsubstantiated cases are practically indistinguishable across a broad range of negative outcomes (e.g., recidivism, developmental, academic, behavioral, mental health, and health problems) [31–35]. Including only substantiated CMRs would therefore greatly underestimate CM rates.
CMRs were made about 70% of the time by professionals (e.g., education, legal/law enforcement, medical, social service, and mental health professionals) and about 30% by non-professionals (e.g., family, friends, and neighbors). Many CM incidents go unreported and were not included in our data, raising reporting bias concerns. For example, report rates can be erroneously inflated among low-income families due to class bias (straightforward classism) or visibility bias (high visibility due to frequent contacts with social service professionals). The shortage of professionals in small urban and rural communities [26–28] can lower visibility of their residents, which can falsely diminish report rates in these communities. There can be also racial bias (straightforward racism) in CMRs. However, best available evidence suggests class bias, income/urbanicity-based visibility bias, and racial bias in CMRs are all minimal [25,36–40].
In 2011-2018, 1,073,168 children were reported to and investigated by DCFS in Illinois (annual unique counts). Among these children, we excluded children with (1) missing/out-of-range ages (1.35%) or (2) missing/outside-Illinois zip codes (1.86%). We aggregated the remaining 1,038,772 reported children (96.79% of the DCFS data) into zip code-years to compute annual CMR rates per zip code from 2011-2018.
We traced all 1,383 Illinois zip codes from 2011-2018. The initial data had 11,064 zip code-years (1,383 zip codes×8 years). The analyses excluded 188 zip code-years with no resident children (1.7%) and 156 zip code-years with missing controls (1.4%). For each age-specific analysis, we further excluded 175 zip code-years with no resident children aged 0-5 (1.6%), 173 zip code-years with no resident children aged 6-11 (1.6%), and 145 zip code-years with no resident children aged 12-17 (1.3%). Altogether, the analyses included 96.9% (overall and type-specific) and 95.3%-95.6% (age-specific) of Illinois zip code-years.
We used the DCFS data with permission from the DCFS IRB and the University of Illinois at Urbana-Champaign IRB. Other data were publicly available and linked with the DCFS data at the zip code level.
Measures
We created seven dependent variables: one variable measuring overall CMR rates and six variables measuring age- and type-specific CMR rates per zip code each year from 2011-2018 (Table 1). We estimated separate models for each dependent variable.
Table 1.
Descriptive Statistics, Illinois Zip Codes, 2011-2018.
| Variable | M (SD) or % |
|---|---|
| Dependent variables: child maltreatment report rate | |
| Total | |
| Total: # reported children per 1k children (N1=10,720; N2=1,358) | 43.6 (31.1) |
| By child age | |
| Young: # reported children per 1k children aged 0-5 years (N1=10,545; N2=1,347) | 51.6 (42.3) |
| Middle: # reported children per 1k children aged 6-11 years (N1=10,547; N2=1,350) | 45.2 (33.7) |
| Adolescent: # reported children per 1k children aged 12-17 years (N1=10,575; N2=1,348) | 34.9 (24.5) |
| By maltreatment type | |
| Neglect: # reported children for neglect per 1k children (N1=10,720; N2=1,358) | 21.5 (18.1) |
| Physical abuse: # reported children for physical abuse per 1k children (N1=10,720; N2=1,358) | 10.3 (7.2) |
| Sexual abuse: # reported children for sexual abuse per 1k children (N1=10,720; N2=1,358) | 5.2 (4.9) |
| Independent variables (based on data for total report rates) | |
| % persons in a food-insecure household | 12.7 (5.7) |
| Control variables (based on data for total report rates) | |
| % children in poverty | 18.9 (13.9) |
| % single-parent households | 33.7 (17.0) |
| % persons aged ≥ 25 years with no high school diploma | 12.6 (9.5) |
| Median owner-occupied house value per 10k | 21.3 (12.2) |
| % vacant housing units | 9.1 (5.3) |
| % Black among children | 15.8 (24.2) |
| % Latino among children | 24.2 (24.6) |
| % foreign-born among persons | 14.2 (12.1) |
| % children (aged 17 years and younger) among persons | 24.2 (4.4) |
| % male among adults aged 20-64 years | 49.4 (3.0) |
| % elderly persons (aged 65 years and older) | 13.9 (4.6) |
| % moved in one year among persons | 12.3 (5.2) |
| % children with disabilities | 3.4 (2.0) |
| Urbanicity | |
| Large urban: zip code in metro area with ≥ 1 million population (USDA RUC code 1) | 31.7% |
| Small urban: zip code in metro area with < 1 million population (USDA RUC code 2 to 3) | 24.3% |
| Rural: zip code in nonmetro area (USDA RUC code 4 to 9) | 44.0% |
| Year | |
| 2011 | 12.6% |
| 2012 | 12.6% |
| 2013 | 12.5% |
| 2014 | 12.5% |
| 2015 | 12.5% |
| 2016 | 12.4% |
| 2017 | 12.4% |
| 2018 | 12.4% |
M = mean. SD = standard deviation. All means and standard deviations were weighted by the child population in each zip code. N1 = number of zip code-year observations. N2 = number of zip codes. USDA RUC = U.S. Department of Agriculture Rural-Urban Continuum Codes (1 = counties in metro areas of 1 million population or more; 2 = counties in metro areas of 250,000 to 1 million population; 3 = counties in metro areas of fewer than 250,000 population; 4 to 9 = nonmetropolitan counties).
We obtained zip code-level FI rates (i.e., percentages of residents in a food-insecure household) from Feeding America’s Map the Meal Gap (MMG) [41,42]. MMG first estimated state-level FI models based on the official FI measure and the FI determinants (i.e., poverty rates, unemployment rates, median income, homeowner rates, disability rates, % Black, and % Latino) from the Current Population Survey. Then, MMG estimated zip code-level FI rates by applying the state-level FI models to zip code-level FI determinants from the American Community Survey (ACS). Many studies have used MMG estimates as predictors of outcomes [43–48], and research shows they are consistent with available direct measures of FI rates of metropolitan areas [42]. We used MMG-estimated zip code-level FI rates in Illinois from 2011-2018.
We measured zip code-level urbanicity based on the rural-urban code of a county in which a zip code was located. For zip codes crossing multiple counties, we assigned the closest integer of the population-weighted average of the rural-urban codes. We used the 2013 U.S. Department of Agriculture Rural-Urban Continuum Codes [49]. We combined the original nine-category codes into three for parsimony (Table 1).
We considered a range of controls in analyses guided by the existing literature (Table 1). Research has identified myriad community conditions that elevate CMR risks, including low socioeconomic conditions (e.g., high rates of child poverty, single-parent, no high school, and vacant housing and low house values), high care burdens (e.g., high percentages of children and elders, low percentages of female adults, and high rates of children with disabilities), and high instability (e.g., high rates of residential moves) [50–52]. Emerging evidence suggests that racial/ethnic minority (e.g., Black, Latino, and foreign-born) populations have lower CMR risks than White populations while controlling for socioeconomic conditions [53–55] and that higher percentages of these minority populations may reduce CMR rates in communities [56,57]. The cited papers provide more theoretical explanations on these community factors. We obtained control variables from the ACS 5-year estimates and linked them with 1-year CMR rates by mid-year (e.g., ACS 2009-2013 estimates were linked to 2011 CMR rates). No predictors showed high and non-tolerable correlations with other predictors (VIF>10) (Table S1 in the Supplement).
Statistical Analysis
We estimated linear spatial-temporal autoregressive models, using the R package spaMM (version 3.11.14). All models considered a first-order temporal autoregressive random effect, as well as a spatially conditional autoregressive random effect based on a first-order queen contiguity matrix. We entered both with-effect of FI (; here, xti is the FI rate for the tth year in the ith zip code, and is the mean of the FI rates from 2011-2018 for the ith zip code) and between-effect of FI () together in the models. This was to examine both the longitudinal changes (i.e., within-effects) and the inter-community differences (i.e., between-effects) simultaneously. Methodologically, within-effects corresponded to fixed effects eliminating time-invariant confounding, and between-effects were equivalent to time-invariant variables in random effects modeling [58,59]. We additionally entered year fixed effects (year dummies), urbanicity (time-invariant), and other controls (time-varying) in the models. The distributions of residuals were fairly normal for most models but positively skewed for some less frequent outcomes (i.e., physical abuse and sexual abuse) (skewness>1). Given the large sample sizes (>10,000), the estimates would be robust to minor normality violations. All estimates were weighted by zip code child populations.
Results
Table 1 presents the descriptive statistics. Annually, 43.6 per 1,000 children in a zip code had a CMR on average. The mean CMR rate was higher for younger children. The mean neglect report rate was the highest, followed by physical abuse and sexual abuse. Each year, on average, 12.7% of zip code residents were in a food-insecure household.
Both WFI and BFI were significantly associated with increased CMR rates in all models (Table 2). A 10-percentage-point increase in WFI increased CMR rates by 13.8 per 1,000 without controls (coefficient=13.8; 95% confidence interval=[11.9, 15.7]) and 10.3 per 1,000 with controls (10.3 [8.4, 12.1]). Every 10-percentage-point increase in BFI increased CMR rates by 43.9 per 1,000 without controls (43.9 [34.7, 53.1]) and 16.5 per 1,000 with controls (16.5 [8.9, 24.3]). Adding the WFI-urbanicity interaction significantly improved the model fit according to the likelihood ratio test (χ2=20.2, df=2, p<.0001). Compared with large urban areas, the WFI-CMR relationship was significantly stronger for small urban areas (8.1 [4.6, 11.7]) but was not significantly different for rural areas (0.9 [−2.7, 4.6]). Specifically, a 10-percentage-point increase in WFI significantly increased CMR rates by 8.5 per 1,000 for large urban (8.5 [6.3, 10.7]), 16.6 per 1,000 for small urban (8.5+8.1 [13.4, 19.9]), and 9.4 per 1,000 for rural areas (8.5+0.9 [6.3, 12.6]). The BFI-urbanicity interaction was not significant (results not shown).
Table 2.
Spatial Linear Models of Child Maltreatment Report Rates (per 1,000 children), Illinois Zip Codes, 2011-2018.
| Coefficient (95% confidence interval) | |||
|---|---|---|---|
|
| |||
| Fixed effect | Model 1: Unadjusted model N1=10,720; N2=1,358 |
Model 2: Adjusted model N1=10,720; N2=1,358 |
Model 3: Adjusted interaction model N1=10,720; N2=1,358 |
| Food insecurity rate (1 unit = 10-percentage-point) |
|||
| Within-effect | 13.8 (11.9, 15.7) | 10.3 (8.4, 12.1) | 8.5 (6.3, 10.7) |
| Within-effect × Small urban | - | - | 8.1 (4.6, 11.7) |
| Within-effect × Rural | - | - | 0.9 (−2.7, 4.6) |
| Between-effect | 43.9 (34.7, 53.1) | 16.5 (8.9, 24.3) | 16.1 (8.6, 23.8) |
| Model fit | |||
|
| |||
| Likelihood Ratio Test | - | Model 2 vs 1: χ2=1344.6, df=22, p<.0001 | Model 3 vs 2: χ2=20.2, df=2, p<.0001 |
Note. N1 = number of zip code-year observations. N2 = number of zip codes. The unadjusted model included a first-order temporal autoregressive random effect and a spatially conditional autoregressive random effect based on a first-order queen contiguity matrix. The adjusted model additionally included all control variables (i.e., year-fixed effects, urbanicity, % children in poverty, % single-parent households, % persons aged ≥25 years with no high school diploma, median owner-occupied house values, % vacant housing units, % Black among children, % Latino among children, % foreign-born among persons, % children aged ≤17 years among persons, % male among adults aged 20-64 years, % elderly persons aged ≥65 years, % moved within one year among persons, and % children with disabilities). The adjusted interaction model further included the interaction between the within-effect of food insecurity rate and urbanicity (large urban, small urban, and rural). All estimates were weighted by the child population in each zip code. Boldface indicates statistical significance (p<.05). A likelihood ratio test is a significance test for model fit improvement from a simpler model to a more complex one.
Table 3 reports the model results of subgroup-specific CMR rates. We additionally present coefficients relative to the mean of the outcome (e.g., a 10-percentage-point increase in WFI increased CMR rates for aged 12-17 by 26.3%). The subgroup-specific results were mostly consistent with the overall results. Yet, a few exceptions were found. First, for age 0-5, age 6-11, physical abuse, and sexual abuse CMR rates, the WFI-CMR association among rural areas was also significantly stronger than among large urban areas. Second, for sexual abuse, WFI was not significant among large urban areas, while WFI was stronger and significant among small urban and rural areas.
Table 3.
Spatial Linear Models of Child Maltreatment Report Rates (per 1,000 children) by Age and Maltreatment Type, Illinois Zip Codes, 2011-2018.
| Coefficient (95% confidence interval) |
Coefficient relative to mean Y (95% confidence interval) |
|||||
|---|---|---|---|---|---|---|
| Age-specific report rate | Age 0-5 N1=10,545; N2=1,347 |
Age 6-11 N1=10,547; N2=1,350 |
Age 12-17 N1=10,575; N2=1,348 |
Age 0-5 Mean Y=51.6 |
Age 6-11 Mean Y=45.2 |
Age 12-17 Mean Y=34.9 |
| Food insecurity rate (1 unit=10-percentage-point) |
||||||
| Within-effect | 6.8 (3.2, 10.3) | 10.8 (7.7, 13.8) | 9.2 (6.7, 11.6) | 13.1% (6.2, 20.0) | 23.8% (16.9, 30.6) | 26.3% (19.3, 33.2) |
| Within-effect×Small urban | 12.3 (6.8, 17.8) | 13.3 (8.6, 18.0) | 9.8 (6.2, 13.3) | 23.9% (13.2, 34.6) | 29.4% (18.9, 39.9) | 28.0% (17.8, 38.2) |
| Within-effect×Rural | 8.5 (2.6, 14.4) | 6.7 (1.7, 11.7) | −0.8 (−4.7, 3.2) | 16.5% (5.1, 27.9) | 14.8% (3.7, 25.9) | −2.2% (−13.4, 9.1) |
| Between-effect | 16.0 (5.7, 26.4) | 15.8 (7.5, 24.2) | 12.3 (6.6, 18.0) | 30.9% (11.1, 51.1) | 34.9% (16.6, 53.5) | 35.2% (18.9, 51.7) |
| Type-specific report rate | Neglect N1=10,720; N2=1,358 |
Physical abuse N1=10,720; N2=1,358 |
Sexual abuse N1=10,720; N2=1,358 |
Neglect Mean Y=21.5 |
Physical abuse Mean Y=10.3 |
Sexual abuse Mean Y=5.2 |
|
| ||||||
| Food insecurity rate (1 unit=10-percentage-point) |
||||||
| Within-effect | 6.2 (4.8, 7.6) | 1.5 (0.8, 2.2) | 0.4 (−0.2, 0.9) | 28.8% (22.2, 35.4) | 14.6% (7.9, 21.2) | 7.2% (−3.2, 17.6) |
| Within-effect×Small urban | 4.5 (2.2, 6.7) | 3.8 (2.9, 4.8) | 2.9 (2.2, 3.5) | 20.7% (10.4, 31.0) | 37.1% (27.7, 46.8) | 55.0% (42.1, 67.8) |
| Within-effect×Rural | −0.7 (−3.0, 1.6) | 1.8 (0.7, 2.9) | 2.4 (1.5, 3.2) | −3.3% (−14.1, 7.4) | 17.0% (6.5, 27.7) | 45.5% (28.9, 61.9) |
| Between-effect | 10.0 (5.7, 14.4) | 3.3 (1.6, 5.0) | 2.3 (1.3, 3.5) | 46.5% (26.5, 66.7) | 32.0% (15.6, 48.1) | 44.9% (24.0, 66.0) |
Note. N1 = number of zip code-year observations. N2 = number of zip codes. Each model included a first-order temporal autoregressive random effect, a spatially conditional autoregressive random effect based on a first-order queen contiguity matrix, and all control variables (i.e., year-fixed effects, urbanicity, % children in poverty, % single-parent households, % persons aged ≥ 25 years with no high school diploma, median owner-occupied house values, % vacant housing units, % Black among children, % Latino among children, % foreign-born among persons, % children aged ≤ 17 years among persons, % male among adults aged 20-64 years, % elderly persons aged ≥ 65 years, % moved within one year among persons, and % children with disabilities). All estimates were weighted by the child population in each zip code. Boldface indicates statistical significance (p < .05).
To further assess the WFI×urbanicity interaction, Figures 1 and 2 depict the estimated longitudinal changes in overall and subgroup-specific CMR rates by the longitudinal changes in FI rates and urbanicity. Compared with large urban zip codes, small urban zip codes showed a significantly steeper slope (i.e., a steeper increase in CMR rates along with an increase in FI rates) for overall and all subgroup-specific CMR rates. Rural zip codes also showed a significantly steeper slope for age 0-5, age 6-11, physical abuse, and sexual abuse CMR rates than large urban zip codes.
Figure 1.
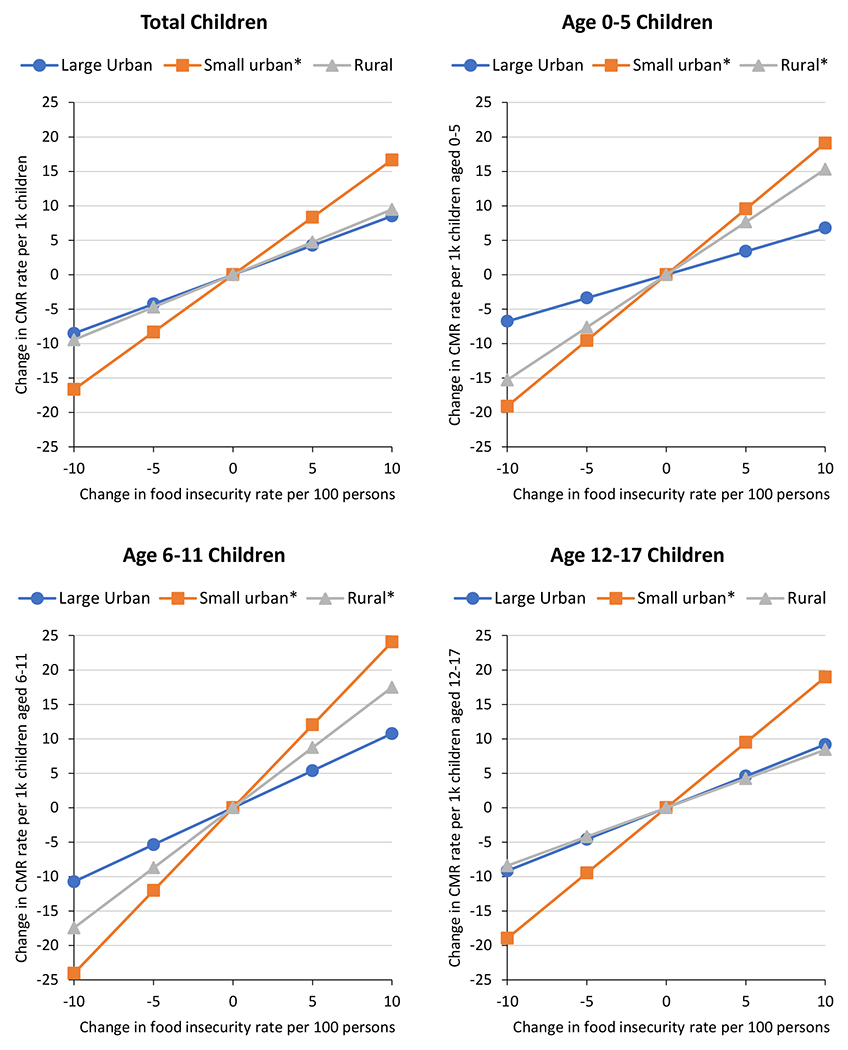
Estimated longitudinal changes in total and age-specific child maltreatment report (CMR) rates by longitudinal changes in food insecurity rates and urban-rural areas, Illinois zip codes, 2011-2018.
Note. Estimated longitudinal changes in total CMR rates are based on Model 3 in Table 2. Estimated longitudinal changes in age-specific CMR rates are based on the age-specific models in Table 3.
*The given slope is significantly different from the large urban slope at p < .05.
Figure 2.
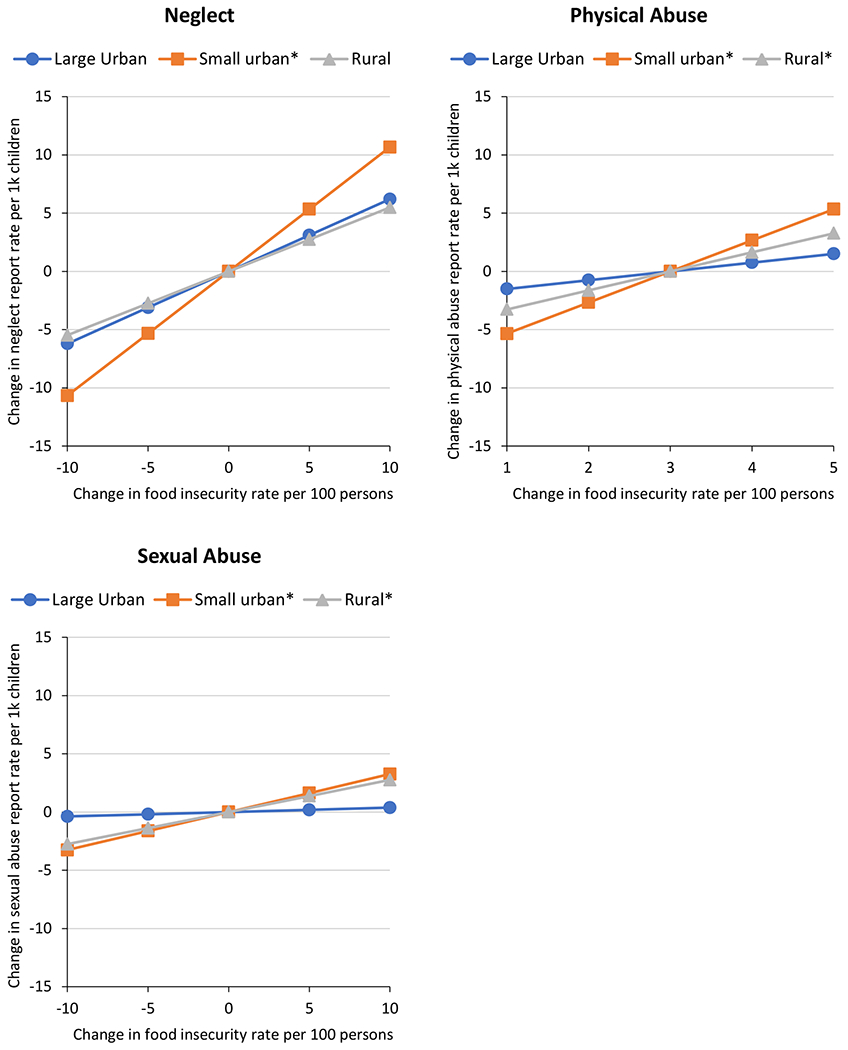
Estimated longitudinal changes in type-specific report rates by longitudinal changes in food insecurity rates and urban-rural areas, Illinois zip codes, 2011-2018.
Note. Estimated longitudinal changes in type-specific report rates are based on the type-specific models in Table 3.
*The given slope is significantly different from the large urban slope at p < .05.
Discussion
This study reports the first findings on the zip code-level associations between FI rates and CMR rates in Illinois from 2011-2018. While controlling for potential confounders, we found that both the longitudinal change and the inter-community difference in FI rates were significantly associated with CMR rates, overall and within all age/type subgroups. This suggests that community FI raises risk of CMR in the general child population, as well as all specific age groups and CM subtypes. We found that the effect sizes of BFI were generally larger than those of WFI. This is because within-effects are closer to the net effects in that time-invariant confounding is eliminated. However, between-effects allow for assessing relationships in a wide social context and can be useful for locating high-risk communities. Methodologically, the community-level approach allowed us to use statewide population-level data and helped us expand on prior individual-level findings within high-risk populations [3–8] to address community-level associations in general populations, including all urban-rural areas. This study also extended existing evidence to specific age groups and CM subtypes.
The present study also extended insights mostly drawn from large urban populations to small urban and rural populations. Findings indicate that the BFI-CMR relationship was significant and did not differ by urbanicity. That is, in inter-community comparisons, higher FI rates consistently increased CMR rates in all urban-rural communities. For WFI, longitudinal increases of FI rates were found to increase CMR rates in all urban-rural communities, but this relationship was significantly stronger among small urban and rural communities. This suggests that small urban and rural communities may be more vulnerable to longitudinal worsening of FI. We speculate that the shortages of social service providers in small urban and rural communities [26–28] may limit the availability of social services to alleviate FI directly or buffer its impacts on CMR risk. This may eventually worsen impacts of community FI on CMRs in small urban and rural communities. Further research is needed to confirm, generalize, and better understand the FI-CM relationship by urban-rural context.
The robust community-level FI-CMR associations point to the need for interdisciplinary efforts. Policies and programs for FI may need to be trauma-informed [60,61], and those for CM may need to reinforce material supports [4,5,62]. Screening FI and CM and referring to community resources as a part of routine public health and medical practices may help early identification and intervention [63,64]. Building a database of these screening results can help agencies monitor community-level adversities directly, while indirect MMG estimates and CMR data are readily available for this monitoring to date.
Although correlational rather than experimental, accumulating evidence, including ours, suggests that addressing FI can be a viable approach for CM prevention efforts. A few CM prevention programs that provide services for food hardships do exist, such as Child First, Healthy Beginnings, Minding the Baby Home Visiting, and Safe Environment for Every Kid [65,66]. These programs provide FI screenings, referral services to promote access to eligible food assistance programs, intensive case management to coordinate community services and resources for food hardships, and education and training about FI. Expanding these services in a community may help prevent CM. Policy-wise, the Supplemental Nutrition Assistance Program (SNAP) is the largest federal program providing nutrition benefits and the key policy tool to address FI [67]. Expanding SNAP benefits and eligibility can reduce FI rates substantially [67,68]. Increasing the number of stores that accept SNAP benefits in communities, especially those with high FI rates, may enhance access to food and reduce FI [69]. These in turn may help reduce CM incidents and reports.
Limitations
This study drew upon Illinois statewide data, which allowed us to cover almost all Illinois populations and conduct analyses overall and within important subgroups. This was only possible by using the MMG estimates and the DCFS records and linking them at the zip code level. Examining both WFI and BFI simultaneously was also a strength for a comprehensive understanding of a phenomenon while considering both dynamic changes and wider social contexts [58,59].
Several limitations call for caution when interpreting the findings. First, the generalizability of the findings is limited to zip code-level relationships in Illinois. Although they are in line with prior individual-level findings [3–8], multilevel studies are needed to examine unique contributions of individual-level and community-level FI. Second, this study is observational, not experimental. Even though the within-effects controlled for time-invariant confounders, this study could not adjust for unobserved time-varying confounders. Third, we used indirect MMG estimates, which are currently the most comprehensive and best available data for community FI. However, direct measurement of community FI might improve on the MMG estimates. Fourth, we used FI rates among all persons, reflecting overall community contexts. Future studies might use child FI rates as a potential driver of CMR rates. Finally, our findings are about CMRs, which are a subset of all incidents [70]. Although much evidence denies any existence of substantial reporting bias in CMRs by poverty, urbanicity, or race/ethnicity [25,36–40], it is also the case that many incidents of abuse go unreported.
Conclusions
This study found that FI rates were significantly associated with CMR rates at the zip code level in Illinois from 2011-2018, while adjusting for potential confounders. Both longitudinal changes and inter-community differences of FI rates had significant associations with CMR rates overall and within subgroups of urbanicity, age, and CM type. We further found that small urban and rural communities generally showed larger increases in CMR rates when their FI rates increased longitudinally, compared with large urban communities. Although further research is required to understand interactions and causal mechanisms, our findings suggest the need for increased attention to communities with high FI rates and for interdisciplinary efforts to address comorbid FI and CMR within communities.
Supplementary Material
Acknowledgements/Funding:
This work was supported by the Centers for Disease Control and Prevention (CDC) [K01CE003229]. The analyses presented in this publication were based on the administrative records of the Illinois Department of Children and Family Services (DCFS). These records were provided by the Children and Family Research Center (CFRC) and have been used with permission of the University of Illinois at Urbana-Champaign IRB (21212) and the DCFS IRB. The CDC, DCFS, CFRC, and the agents or employees of these institutions bear no responsibility for the analyses or interpretations presented here. The information and opinions expressed reflect solely the opinions of the authors.
Abbreviations and Acronyms
- CM
child maltreatment
- CMR
child maltreatment report
- DCFS
Department of Children and Family Services
- MMG
Map the Meal Gap
- FI
food insecurity
- WFI
within-effect of food insecurity
- BFI
between-effect of food insecurity
- SNAP
Supplemental Nutrition Assistance Program
Contributor Information
Hyunil Kim, School of Social work, University of Illinois at Urbana-Champaign, 1010 W Nevada St, Urbana, Illinois 61801, United States
Craig Gundersen, Department of Economics, Baylor University, One Bear Place, Waco, Texas 76798, United States
Liliane Windsor, School of Social work, University of Illinois at Urbana-Champaign, 1010 W Nevada St, Urbana, Illinois 61801, United States
References
- [1].Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2020, ERR-298. U.S. Department of Agriculture, Economic Research Service; 2021. [Google Scholar]
- [2].U.S. Department of Health and Human Services. Child maltreatment 2019. 2021. [Google Scholar]
- [3].Epstein MR. Predicting abuse and neglect in the first two years of life from risk assessment during the prenatal and perinatal period. University of California, Davis, 2001. [Google Scholar]
- [4].Garg A, Tripodis Y, Dworsky ZD, Sege RD. Do basic unmet maternal needs influence infant maltreatment risk? A nested case-control study. Clin Pediatr (Phila) 2019;58:461–5. 10.1177/0009922818821879. [DOI] [PubMed] [Google Scholar]
- [5].Helton JJ, Jackson DB, Boutwell BB, Vaughn MG. Household food insecurity and parent-to-child aggression. Child Maltreat 2019;24:213–21. 10.1177/1077559518819141. [DOI] [PubMed] [Google Scholar]
- [6].Mersky JP, Janczewski CE. Racial and ethnic differences in the prevalence of adverse childhood experiences: Findings from a low-income sample of U.S. women. Child Abuse Negl 2018;76:480–7. 10.1016/j.chiabu.2017.12.012. [DOI] [PubMed] [Google Scholar]
- [7].Slack KS, Berger LM, DuMont K, Yang M-Y, Kim B, Ehrhard-Dietzel S, et al. Risk and protective factors for child neglect during early childhood: A cross-study comparison. Child Youth Serv Rev 2011;33:1354–63. 10.1016/j.childyouth.2011.04.024. [DOI] [Google Scholar]
- [8].Yang M-Y. The effect of material hardship on child protective service involvement. Child Abuse Negl 2015;41:113–25. 10.1016/j.chiabu.2014.05.009. [DOI] [PubMed] [Google Scholar]
- [9].Oliveira KHD, Almeida GM, Gubert MB, Moura AS, Spaniol AM, Hernandez DC, et al. Household food insecurity and early childhood development: Systematic review and meta-analysis. Matern Child Nutr 2020;16. 10.1111/mcn.12967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Shankar P, Chung R, Frank DA. Association of food insecurity with children’s behavioral, emotional, and academic outcomes: A systematic review. J Dev Behav Pediatr 2017;38:135–50. 10.1097/DBP.0000000000000383. [DOI] [PubMed] [Google Scholar]
- [11].Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff 2015;34:1830–9. 10.1377/hlthaff.2015.0645. [DOI] [PubMed] [Google Scholar]
- [12].Thomas MMC, Miller DP, Morrissey TW. Food insecurity and child health. Pediatrics 2019;144:e20190397. 10.1542/peds.2019-0397. [DOI] [PubMed] [Google Scholar]
- [13].Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci 2006;256:174–86. 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bellis MA, Hughes K, Ford K, Ramos Rodriguez G, Sethi D, Passmore J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Heal 2019;4:e517–28. 10.1016/S2468-2667(19)30145-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].McCrory E, De Brito SA, Viding E. The impact of childhood maltreatment: A review of neurobiological and genetic factors. Front Psychiatry 2011;2:1–14. 10.3389/fpsyt.2011.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Lansford JE, Dodge KA, Pettit GS, Bates JE, Crozier J, Kaplow J. A 12-year prospective study of the long-term effects of early child physical maltreatment on psychological, behavioral, and academic problems in adolescence. Arch Pediatr Adolesc Med 2002;156:824–30. 10.1001/archpedi.156.8.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Conrad-Hiebner A, Byram E. The temporal impact of economic insecurity on child maltreatment: A systematic review. Trauma, Violence, Abus 2020;21:157–78. 10.1177/1524838018756122. [DOI] [PubMed] [Google Scholar]
- [18].Sampson RJ, Morenoff JD, Earls F. Beyond social capital: Spatial dynamics of collective efficacy for children. Am Sociol Rev 1999;64:633. 10.2307/2657367. [DOI] [Google Scholar]
- [19].Belsky J Etiology of child maltreatment: A developmental-ecological analysis. Psychol Bull 1993;114:413–34. 10.1037/0033-2909.114.3.413. [DOI] [PubMed] [Google Scholar]
- [20].Merzel C, D’Afflitti J. Reconsidering community-based health promotion: Promise, performance, and potential. Am J Public Health 2003;93:557–74. 10.2105/AJPH.93.4.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Graaf G, Ratliff GA. Preparing social workers for evidence-informed community-based practice: An integrative framework. J Soc Work Educ 2018;54:S5–19. 10.1080/10437797.2018.1434437. [DOI] [Google Scholar]
- [22].Covington T The public health approach for understanding and preventing child maltreatment: A brief review of the literature and a call to action. Child Welfare 2013;92:21–39. [PubMed] [Google Scholar]
- [23].Putnam-Hornstein E, Webster D, Needell B, Magruder J. A public health approach to child maltreatment surveillance: Evidence from a data linkage project in the United States. Child Abus Rev 2011;20:256–73. 10.1002/car.1191. [DOI] [Google Scholar]
- [24].Maguire-Jack K, Jespersen B, Korbin JE, Spilsbury JC. Rural child maltreatment: A scoping literature review. Trauma, Violence, Abus 2020:1–10. 10.1177/1524838020915592. [DOI] [PubMed] [Google Scholar]
- [25].Maguire-Jack K, Kim H. Rural differences in child maltreatment reports, reporters, and service responses. Child Youth Serv Rev 2021;120:105792. 10.1016/j.childyouth.2020.105792. [DOI] [Google Scholar]
- [26].Andrilla CHA, Patterson DG, Garberson LA, Coulthard C, Larson EH. Geographic variation in the supply of selected behavioral health providers. Am J Prev Med 2018;54:S199–207. 10.1016/j.amepre.2018.01.004. [DOI] [PubMed] [Google Scholar]
- [27].Zhang D, Son H, Shen Y, Chen Z, Rajbhandari-Thapa J, Li Y, et al. Assessment of changes in rural and urban primary care workforce in the United States from 2009 to 2017. JAMA Netw Open 2020;3:e2022914. 10.1001/jamanetworkopen.2020.22914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-level estimates of mental health professional shortage in the United States. Psychiatr Serv 2009;60:1323–8. 10.1176/ps.2009.60.10.1323. [DOI] [PubMed] [Google Scholar]
- [29].Kim H, Drake B, Jonson-Reid M. Longitudinal understanding of child maltreatment report risks. Child Abuse Negl 2020;104:104467. 10.1016/j.chiabu.2020.104467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Drake B, Pandey S. Understanding the relationship between neighborhood poverty and specific types of child maltreatment. Child Abuse Negl 1996;20:1003–18. 10.1016/0145-2134(96)00091-9. [DOI] [PubMed] [Google Scholar]
- [31].Cross TP, Casanueva C. Caseworker judgments and substantiation. Child Maltreat 2009;14:38–52. 10.1177/1077559508318400. [DOI] [PubMed] [Google Scholar]
- [32].Drake B Unraveling “unsubstantiated.” Child Maltreat 1996;1:261–71. 10.1177/1077559596001003008. [DOI] [Google Scholar]
- [33].Hussey JM, Marshall JM, English DJ, Knight ED, Lau AS, Dubowitz H, et al. Defining maltreatment according to substantiation: Distinction without a difference? Child Abus Negl 2005;29:479–92. 10.1016/j.chiabu.2003.12.005. [DOI] [PubMed] [Google Scholar]
- [34].Kohl PL, Jonson-Reid M, Drake B. Time to leave substantiation behind: Findings from a national probability study. Child Maltreat 2009;14:17–26. 10.1177/1077559508326030. [DOI] [PubMed] [Google Scholar]
- [35].Leiter J, Myers KA, Zingraff MT. Substantiated and unsubstantiated cases of child maltreatment: Do their consequences differ? Soc Work Res 1994;18:67–82. 10.1093/swr/18.2.67. [DOI] [Google Scholar]
- [36].Jonson-Reid M, Drake B, Kohl PL. Is the overrepresentation of the poor in child welfare caseloads due to bias or need? Child Youth Serv Rev 2009;31:422–7. 10.1016/j.childyouth.2008.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Kim H, Drake B, Jonson-Reid M. An examination of class-based visibility bias in national child maltreatment reporting. Child Youth Serv Rev 2018;85:165–73. 10.1016/j.childyouth.2017.12.019. [DOI] [Google Scholar]
- [38].Drake B, Jolley JM, Lanier P, Fluke J, Barth RP, Jonson-Reid M. Racial bias in child protection? A comparison of competing explanations using national data. Pediatrics 2011;127:peds.2010–1710. 10.1542/peds.2010-1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Drake B, Jonson-Reid M, Dvalishvili D. Poverty and child maltreatment. In: Krugman RD, Korbin JE, editors. Handb. child maltreatment, Cham: Springer; 2022, p. 239–57. 10.1007/978-3-030-82479-2_11. [DOI] [Google Scholar]
- [40].Drake B, Jonson-Reid M, Kim H, Chiang C-J, Davalishvili D. Disproportionate need as a factor explaining racial disproportionality in the CW system. In: Dettlaff AJ, editor. Racial Disproportionality Disparities Child Welf. Syst, Cham: Springer; 2021, p. 159–76. 10.1007/978-3-030-54314-3_9. [DOI] [Google Scholar]
- [41].Feeding America. Food insecurity in the United States n.d. https://map.feedingamerica.org/.
- [42].Gundersen C, Engelhard E, Waxman E. Map the Meal Gap: Exploring food insecurity at the local level. Appl Econ Perspect Policy 2014;36:373–86. 10.1093/aepp/ppu018. [DOI] [Google Scholar]
- [43].Ali A, Broome J, Tatum D, Fleckman J, Theall K, Chaparro MP, et al. The association between food insecurity and gun violence in a major metropolitan city. J Trauma Acute Care Surg 2022;Publish Ah. 10.1097/TA.0000000000003578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Berkowitz SA, Basu S, Gundersen C, Seligman HK. State-level and county-level estimates of health care costs associated with food insecurity. Prev Chronic Dis 2019;16:180549. 10.5888/pcd16.180549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Gundersen C, Dewey A, Hake M, Engelhard E, Crumbaugh AS. Food insecurity across the rural-urban divide: Are counties in need being reached by charitable food assistance? Ann Am Acad Pol Soc Sci 2017;672:217–37. 10.1177/0002716217710172. [DOI] [Google Scholar]
- [46].Mensah R The impact of food insecurity on diabetes prevalence in the US: A look at the Northeast and the Midwest. Wright State University. Dayton, Ohio, 2020. [Google Scholar]
- [47].Rosenberg BL, Kellar JA, Labno A, Matheson DHM, Ringel M, VonAchen P, et al. Quantifying geographic variation in health care outcomes in the United States before and after risk-adjustment. PLoS One 2016;11:e0166762. 10.1371/journal.pone.0166762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Wang SY, Eberly LA, Roberto CA, Venkataramani AS, Groeneveld PW, Khatana SAM. Food insecurity and cardiovascular mortality for nonelderly adults in the United States from 2011 to 2017. Circ Cardiovasc Qual Outcomes 2021;14. 10.1161/CIRCOUTCOMES.120.007473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].USDA Economic Research Service. Rural-Urban Continuum Codes n.d. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/.
- [50].Coulton CJ, Crampton DS, Irwin M, Spilsbury JC, Korbin JE. How neighborhoods influence child maltreatment: A review of the literature and alternative pathways. Child Abuse Negl 2007;31:1117–42. 10.1016/j.chiabu.2007.03.023. [DOI] [PubMed] [Google Scholar]
- [51].Freisthler B, Merritt DH, LaScala EA. Understanding the ecology of child maltreatment: A review of the literature and directions for future research. Child Maltreat 2006;11:263–80. 10.1177/1077559506289524. [DOI] [PubMed] [Google Scholar]
- [52].Maguire-Jack K Multilevel investigation into the community context of child maltreatment. J Aggress Maltreat Trauma 2014;23:229–48. 10.1080/10926771.2014.881950. [DOI] [Google Scholar]
- [53].Kim H, Drake B. Child maltreatment risk as a function of poverty and race/ethnicity in the USA. Int J Epidemiol 2018;47:780–7. 10.1093/ije/dyx280. [DOI] [PubMed] [Google Scholar]
- [54].Putnam-Hornstein E, Needell B, King B, Johnson-Motoyama M. Racial and ethnic disparities: A population-based examination of risk factors for involvement with child protective services. Child Abuse Negl 2013;37:33–46. 10.1016/j.chiabu.2012.08.005. [DOI] [PubMed] [Google Scholar]
- [55].Drake B, Lee SM, Jonson-Reid M. Race and child maltreatment reporting: Are Blacks overrepresented? Child Youth Serv Rev 2009;31:309–16. 10.1016/j.childyouth.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Freisthler B, Maguire-Jack K. Understanding the interplay between neighborhood structural factors, social processes, and alcohol outlets on child physical abuse. Child Maltreat 2015;20:268–77. 10.1177/1077559515598000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Smith BD, Li Q, Wang K, Smith AM. A national study of child maltreatment reporting at the county level: Interactions among race/ethnicity, rurality and poverty. Child Youth Serv Rev 2021;122:105925. 10.1016/j.childyouth.2021.105925. [DOI] [Google Scholar]
- [58].Schunck R Within and between estimates in random-effects models: Advantages and drawbacks of correlated random effects and hybrid models. Stata J Promot Commun Stat Stata 2013;13:65–76. 10.1177/1536867X1301300105. [DOI] [Google Scholar]
- [59].Bell A, Fairbrother M, Jones K. Fixed and random effects models: Making an informed choice. Qual Quant 2019;53:1051–74. 10.1007/s11135-018-0802-x. [DOI] [Google Scholar]
- [60].Sun J, Knowles M, Patel F, Frank DA, Heeren TC, Chilton M. Childhood adversity and adult reports of food insecurity among households with children. Am J Prev Med 2016;50:561–72. 10.1016/j.amepre.2015.09.024. [DOI] [PubMed] [Google Scholar]
- [61].Phojanakong P, Welles S, Dugan J, Booshehri L, Brown Weida E, Chilton M. Trauma-informed financial empowerment programming improves food security among families with young children. J Nutr Educ Behav 2020;52:465–73. 10.1016/j.jneb.2020.02.008. [DOI] [PubMed] [Google Scholar]
- [62].Helton JJ, Moore AR, Henrichsen C. Food security status of mothers at-risk for child maltreatment. Child Youth Serv Rev 2018;93:263–9. 10.1016/j.childyouth.2018.07.031. [DOI] [Google Scholar]
- [63].Council on Community Pediatrics, Committee on Nutrition. Promoting food security for all children. Pediatrics 2015;136:e1431–8. 10.1542/peds.2015-3301. [DOI] [PubMed] [Google Scholar]
- [64].Flaherty EG, Stirling J. The pediatrician’s role in child maltreatment prevention. Pediatrics 2010;126:833–41. 10.1542/peds.2010-2087. [DOI] [PubMed] [Google Scholar]
- [65].CEBC. Safe Environment for Every Kid n.d. https://www.cebc4cw.org/program/safe-environment-for-every-kid-seek-model/.
- [66].HomeVEE. Model implementation summary reports n.d. https://homvee.acf.hhs.gov/implementation.
- [67].Gundersen C Food insecurity is an ongoing national concern. Adv Nutr 2013;4:36–41. 10.3945/an.112.003244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Gundersen C, Waxman E, Crumbaugh AS. An examination of the adequacy of Supplemental Nutrition Assistance Program (SNAP) benefit levels: Impacts on food insecurity. Agric Resour Econ Rev 2019;48:433–47. 10.1017/age.2019.30. [DOI] [Google Scholar]
- [69].Bullinger LR, Fleckman JM, Fong K. Proximity to SNAP-authorized retailers and child maltreatment reports. Econ Hum Biol 2021;42:101015. 10.1016/j.ehb.2021.101015. [DOI] [PubMed] [Google Scholar]
- [70].Sedlak AJ, Mettenburg J, Basena M, Petta I, McPherson K, Green A, et al. Fourth national incidence study of child abuse and neglect (NIS-4): Report to congress. Washington, DC: US Department of Health and Human Services; 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


