Abstract
BACKGROUND
Transorbital penetrating head injuries (PHIs) are uncommon but can lead to substantial deficits, depending on intracranial involvement and the neuroanatomical structures affected. Complete recovery after such injuries is rare.
OBSERVATIONS
A 7-year-old boy sustained a PHI when he fell onto a garden spike while climbing a fence. Initial imaging showed an orbital roof fracture, focal subarachnoid hemorrhage, and an intraparenchymal hemorrhage in the right frontal lobe with associated linear tract extending to the contralateral superior temporal gyrus. Relevant neuroanatomical structures, including the anterior cerebral arteries (ACAs) and the basal ganglia, were spared. This is in keeping with superior transorbital PHI caused by a garden spike, which had transgressed the skull entering from the right superior orbit. Clinically, he experienced some transient right-sided weakness and mild speech disturbance. Some questionable vasospasm of the ACAs observed on interim magnetic resonance imaging was absent in a repeat imaging study, followed by an unremarkable radiographic follow-up at 6 months after injury. At 18 months after injury, he is neurologically intact without deficit.
LESSONS
Most PHIs bear serious lifelong consequences, but here was a case of a deep, penetrating object that managed to avoid all significant neuroanatomical pathways, leading to complete recovery in follow-up.
Keywords: transorbital, penetrating, head injury, child, outcome, favorable
ABBREVIATIONS: ACA = anterior cerebral artery, CT = computed tomography, CTA = computed tomography angiography, MRI = magnetic resonance imaging, PHI = penetrating head injury, SAH = subarachnoid hemorrhage
Transorbital penetrating head injury (PHI) represents a small percentage of all head injuries (0.4%)1 but accounts for up to 24% of PHIs in adults and 45% in children.2,3 Several cases with various objects penetrating different intracranial compartments have been described.4–7 Depending on the type of object, mechanism of injury, and neuroanatomical structures affected, most of these injuries result in significant morbidity and mortality.8–10 We present a case of transorbital PHI in a child with a highly favorable outcome and discuss it in the context of previously reported injuries with relevant implications for diagnosis and treatment.
Illustrative Case
A 7-year-old boy sustained a PHI when he fell onto a garden spike while climbing a fence. Immediately after the fall and after extricating himself from the spike, he was reported by his mother with slurred speech but no loss of consciousness. He presented with right eye contusion, periorbital swelling, and abrasion below the right eyebrow (Fig. 1). The finding of his neurological examination was unremarkable except for mild dysarthria and some minor right-sided weakness. Initial imaging with computed tomography (CT) followed by CT angiography (CTA) showed an intraparenchymal hemorrhage in the right frontal basal lobe with associated linear tract extending from the posterior aspect of the hematoma to the left parietal lobe through the genu of the corpus callosum, left globus pallidus, anterior limb of the internal capsule, and left posterior insula, as well as a right orbital roof fracture and focal subarachnoid hemorrhage (SAH) (Figs. 2 and 3). This is in keeping with a PHI caused by the garden spike, which had transgressed his right orbit on top of his globe, pierced the bony superior orbital roof, bypassed the anterior cerebral arteries (ACAs), narrowly missed the posterior limb of the internal capsule, and ended up on the contralateral side in the left superior temporal gyrus (Figs. 4 and 5). Ophthalmological examination did not reveal any visual impairment but disclosed minor subconjunctival hemorrhage. He was admitted for observation and treated with a prophylactic 5-day course of antibiotics (meropenem and amphotericin), given the contact of the foreign body with plants and potentially soil. His vaccinations were up to date, including tetanus. He underwent follow-up CT/CTA 8 hours after the first imaging, which showed a stable focus of intraparenchymal hemorrhage in the right basal frontal lobe. Magnetic resonance imaging (MRI) revealed some questionable vasospasm of the ACAs, but this was absent on a repeat MRI study, which was obtained before discharge. His clinical and radiographic follow-up at 6 months after injury with CT/CTA was unremarkable. At his last follow-up 18 months after injury, he was doing well, reporting very occasional headaches but otherwise denying any concerns with learning capabilities in school. The neurological examination was uneventful, with his speech back to baseline before the accident. He was discharged from clinical follow-up at that time.
FIG. 1.

Photographs illustrating the traumatizing object, a garden spike (arrowheads, A), which penetrated the right orbit of the patient, who presented with bruising, periorbital swelling, and a right-sided abrasion below the eyebrow (arrows), indicating the entry point of the garden spike (B).
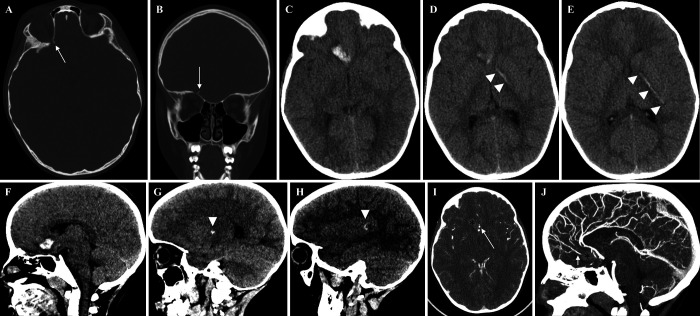
FIG. 2.
CT bone window showing a displaced fracture of the roof of the right orbit, with the fracture fragment (arrows) angulated superiorly toward the right basal frontal lobe (A and B). Axial (C–E) and sagittal (F–H) CT scans showing intraparenchymal hemorrhage in the right basal frontal lobe with linear extension (arrowheads) to the anterior limb of left internal capsule and left posterior insula. Findings suggest penetrating injury through the roof of the right orbit, extending across the right basal frontal lobe to the left internal capsule. In the contrast-supported CTA (I and J), the intraparenchymal hemorrhage (asterisks) is close to the ACAs (arrows). The intracranial branches of the internal carotid, basilar, and vertebral arteries are patent without signs of significant narrowing or intracranial dissection.
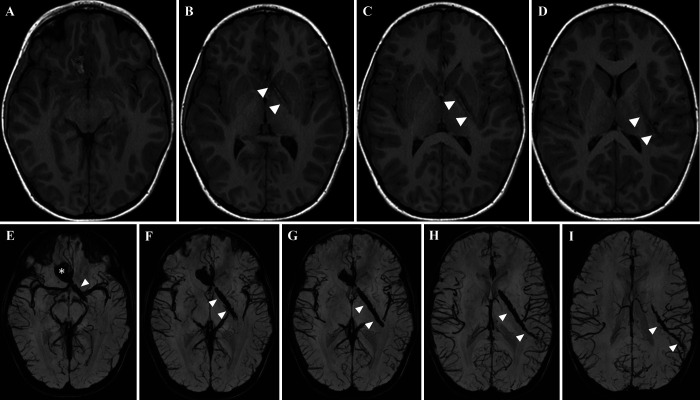
FIG. 3.
Axial T1-weighted MRI (A–D) and susceptibility-weighted imaging (E–I) showing the intraparenchymal hemorrhage (asterisks) in the right basal frontal lobe with associated linear tract (arrowheads) extending from the posterior aspect of the hematoma to the left temporal lobe through the genu of the corpus callosum, left pallidum, anterior limb of internal capsule, and left posterior insula. This is in keeping with a penetrating injury through the right orbit.
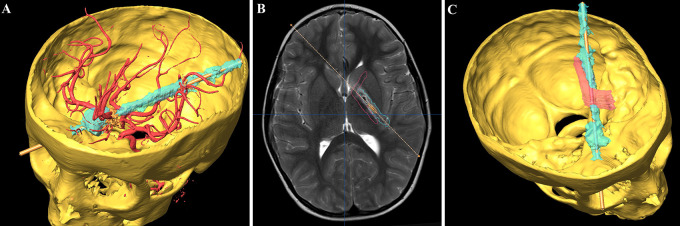
FIG. 4.
Three-dimensional (3D) reconstruction of the patients’ skull and injury tract using the BrainLAB planning software. Rotatory image revealing the 3D anatomical association among the trajectory of the penetrating object, the orbit with its entry point, and the bypassed intracerebral vasculature (A). Axial T2-weighted MRI with visualization of the left internal capsule (red outline, B), indicating the relative localization of the trajectory of penetrating trauma to its posterior limb. Blood products involve the genu and anterior part of the posterior limb and also can be seen adjacent to the posterior limb of the internal capsule (B) with additional 3D reconstruction (C).
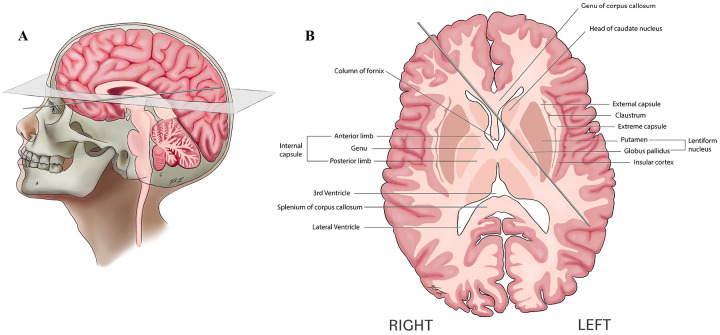
FIG. 5.
Graphic illustration of the spike’s trajectory entering the skull via the right orbit (A) and its anatomical relationship to functional structures within the brain parenchyma (B, adapted to the MRI-typical orientation from caudal to cranial).
Discussion
Observations
Transorbital PHIs are rare; however, they have been reported repeatedly in the literature, predominantly in children.7,11,12 Different mechanisms of injury as well as various types of penetrating objects have been associated with variable outcomes and implications.2,13–16 The direction and velocity of the penetrating foreign body will determine its trajectory and subsequently the extent and severity of injury, based on the neuroanatomical structures passed.5 However, the most significant complications and long-term consequences result from primary neurovascular damage followed by related secondary neurological injury, including hemorrhage and ischemia. These latter ones are the major determinants of clinical deterioration and death in patients with PHI.17 Bodanapally et al.18 investigated the risk factors for an intracranial arterial injury in PHI and identified a trajectory in proximity to the circle of Willis as the best predictor of injury (odds ratio 6.8; and p = 0.005) besides an entry wound over the frontobasal-temporal region, a bihemispheric wound trajectory, and presence of SAH. On the basis of these predictors, our patient was at highest risk for vascular injury and underwent early CTA followed by magnetic resonance angiography. Luckily, his ACAs were missed by the garden spike and remained intact. Also, other delayed complications, such as vasospasm, traumatic intracranial aneurysms, or dissections, were eventually excluded during his follow-up. Given the high complication, morbidity, and mortality rates from neurovascular injuries, a precise and thorough vascular work-up is mandatory in PHI, especially after transorbital penetration due to the proximity of the internal carotid artery and the ACA.
Another outcome-determining factor of PHI is the risk of infection. Many case reports have described PHIs complicated by cerebral infections in the form of meningitis or abscess formation caused by retained or missed foreign bodies.1,19–22 Sometimes injuries may appear trivial and are not accompanied by neurological signs initially. Especially in these cases, a thorough search using accurate imaging modalities with exploration for orbital fractures or retained foreign bodies is crucial.19 A recommendation for the use of antibiotics in PHI, suggesting preventive antibiotics for 5 days as soon as possible after the injury along with human antitetanus immunoglobulin (250–500 IU intramuscularly) for patients whose vaccination status is not updated, has been reported.23 Treatment for manifest cerebral infections should follow the standards as per infectious disease guidelines and should be initiated immediately in addition to appropriate surgical exploration.23 Accordingly, our patient underwent a 5-day course of meropenem and amphotericin. Given that the foreign object was a garden spike, antifungal treatment was briefly discussed but was not considered indicated. His vaccination status was up to date.
Overall, we describe a most fortuitous case of a child with transorbital PHI, which remained uncomplicated and in which full recovery was achieved. The uniqueness of our case refers to the type of penetrating object, as well as to its exceptional intracerebral trajectory, bypassing all neurofunctional and vascular structures and leaving the patient unharmed. It would be hard to imagine creating a similar trajectory of a penetrating object even with the aid of frameless stereotaxy or robotic guidance at the same angle and to the same intracranial depth that would similarly leave a patient neurologically intact as in the case presented. The use of three-dimensional neuroimaging by CT and advanced MRI sequences enabled us to carefully reconstruct the pathway of the penetrating object and the neuroanatomical structures that were potentially at risk. Despite a few other cases being reported with a similarly good outcome,12,24,25 we consider this case illustration an important reminder for comprehensive diagnostics during admission and close follow-up for vascular or infectious complications.
Lessons
Most penetrating injuries such as this will have serious lifelong consequences, but here was a case of the passage of a penetrating object that traversed the midline and managed to avoid all significant neuroanatomical pathways, leading to complete recovery in follow-up. Relevant outcome-determining factors are early adequate vascular imaging to rule out vascular injury as well as foreign body retrieval along with antibiotic prevention of early and delayed infections.
Acknowledgments
We express special thanks to Viola Yu for the professional anatomical illustrations and her significant contribution to this article.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Rutka. Acquisition of data: Lohkamp, Holowka, Manicat-Emo. Analysis and interpretation of data: Lohkamp, Holowka, Widjaja, Manicat-Emo. Drafting the article: Lohkamp, Widjaja, Manicat-Emo. Critically revising the article: Widjaja, Manicat-Emo, Rutka. Reviewed submitted version of manuscript: Lohkamp, Holowka, Widjaja. Approved the final version of the manuscript on behalf of all authors: Lohkamp. Administrative/technical/material support: Widjaja, Rutka. Study supervision: Rutka. Fusion and 3D reconstruction of CT/MRI images: Holowka.
References
- 1. Paiva WS, Monaco B, Prudente M, et al. Surgical treatment of a transorbital penetrating brain injury. Clin Ophthalmol. 2010;4:1103–1105. doi: 10.2147/OPTH.S9638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Arslan M, Eseoğlu M, Güdü BO, Demir I. Transorbital orbitocranial penetrating injury caused by a metal bar. J Neurosci Rural Pract. 2012;3(2):178–181. doi: 10.4103/0976-3147.98228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kasamo S, Asakura T, Kusumoto K, et al. Transorbital penetrating brain injury. Article in Japanese. No Shinkei Geka. 1992;20(4):433–438. [PubMed] [Google Scholar]
- 4. Hoffman JR, Neuhaus RW, Baylis HI. Penetrating orbital trauma. Am J Emerg Med. 1983;1(1):22–27. doi: 10.1016/0735-6757(83)90033-5. [DOI] [PubMed] [Google Scholar]
- 5. Schreckinger M, Orringer D, Thompson BG, La Marca F, Sagher O. Transorbital penetrating injury: case series, review of the literature, and proposed management algorithm. J Neurosurg. 2011;114(1):53–61. doi: 10.3171/2010.8.JNS10301. [DOI] [PubMed] [Google Scholar]
- 6. Quinn LM, Egan RA, Shults WT. Transorbital penetrating brainstem injuries. Arch Ophthalmol. 2006;124(6):915–916. doi: 10.1001/archopht.124.6.915. [DOI] [PubMed] [Google Scholar]
- 7. Tabibkhooei A, Aslaninia A, Anousha K. Childhood transorbital skull base penetrating injury: report of 2 cases and review of literature. World Neurosurg. 2019;131:213–216. doi: 10.1016/j.wneu.2019.06.234. [DOI] [PubMed] [Google Scholar]
- 8. Alamri AA, Algethami AR, Alghamdi F. Transorbital craniocerebral penetration by a sharp object with an intact globe. Case Rep Emerg Med. 2018;2018:3575897. doi: 10.1155/2018/3575897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sheikh NA, Ateriya N, Khan G, Singh A, Raj K. Fatal transorbital- intracranial penetrating injury – a case report. J Forensic Leg Med. 2022;85:102288. doi: 10.1016/j.jflm.2021.102288. [DOI] [PubMed] [Google Scholar]
- 10. Harrington BM, Gretschel A, Lombard C, Lonser RR, Vlok AJ. Complications, outcomes, and management strategies of non- missile penetrating head injuries. J Neurosurg. 2020;134(5):1658–1666. doi: 10.3171/2020.4.JNS20122. [DOI] [PubMed] [Google Scholar]
- 11. Mzimbiri JM, Li J, Bajawi MA, Lan S, Chen F, Liu J. Orbitocranial low-velocity penetrating injury: a personal experience, case series, review of the literature, and proposed management plan. World Neurosurg. 2016;87:26–34. doi: 10.1016/j.wneu.2015.12.063. [DOI] [PubMed] [Google Scholar]
- 12. Jacob JT, Cohen-Gadol AA, Maher CO, Meyer FB. Transorbital penetrating brainstem injury in a child: case report. J Neurosurg. 2005;102(3 suppl):350–352. doi: 10.3171/ped.2005.102.3.0350. [DOI] [PubMed] [Google Scholar]
- 13. Mahalangikar R, Kumar A, Sharma BS. Transorbital penetrating intracranial injury with an umbrella wire causing cavernous internal carotid artery injury and thrombosis. World Neurosurg. 2016;86:513.e15–513.e18. doi: 10.1016/j.wneu.2015.09.033. [DOI] [PubMed] [Google Scholar]
- 14. Muthe MM, Joshi AR, Kulsange A, Firke VP. Imaging findings in transorbital intracranial penetrating injury with an ice pick. BMJ Case Rep. 2021;14(8):e245705. doi: 10.1136/bcr-2021-245705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Satyarthee GD, Borkar SA, Tripathi AK, Sharma BS. Transorbital penetrating cerebral injury with a ceramic stone: report of an interesting case. Neurol India. 2009;57(3):331–333. doi: 10.4103/0028-3886.53285. [DOI] [PubMed] [Google Scholar]
- 16. Ghadersohi S, Ference EH, Detwiller K, Kern RC. Presentation, workup, and management of penetrating transorbital and transnasal injuries: a case report and systematic review. Am J Rhinol Allergy. 2017;31(2):29–34. doi: 10.2500/ajra.2017.31.4421. [DOI] [PubMed] [Google Scholar]
- 17. Bell RS, Vo AH, Roberts R, Wanebo J, Armonda RA. Wartime traumatic aneurysms: acute presentation, diagnosis, and multimodal treatment of 64 craniocervical arterial injuries. Neurosurgery. 2010;66(1):66–79. doi: 10.1227/01.NEU.0000361285.50218.A8. [DOI] [PubMed] [Google Scholar]
- 18. Bodanapally UK, Saksobhavivat N, Shanmuganathan K, Aarabi B, Roy AK. Arterial injuries after penetrating brain injury in civilians: risk factors on admission head computed tomography. J Neurosurg. 2015;122(1):219–226. doi: 10.3171/2014.9.JNS14679. [DOI] [PubMed] [Google Scholar]
- 19. Abdulbaki A, Al-Otaibi F, Almalki A, Alohaly N, Baeesa S. Transorbital craniocerebral occult penetrating injury with cerebral abscess complication. Case Rep Ophthalmol Med. 2012;2012:742186. doi: 10.1155/2012/742186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Di Roio C, Jourdan C, Mottolese C, Convert J, Artru F. Craniocerebral injury resulting from transorbital stick penetration in children. Childs Nerv Syst. 2000;16(8):503–507. doi: 10.1007/s003810000291. [DOI] [PubMed] [Google Scholar]
- 21. Maruya J, Yamamoto K, Wakai M, Kaneko U. Brain abscess following transorbital penetrating injury due to bamboo fragments – case report. Neurol Med Chir (Tokyo) 2002;42(3):143–146. doi: 10.2176/nmc.42.143. [DOI] [PubMed] [Google Scholar]
- 22. Seider N, Gilboa M, Lautman E, Miller B. Delayed presentation of orbito-cerebral abscess caused by pencil-tip injury. Ophthal Plast Reconstr Surg. 2006;22(4):316–317. doi: 10.1097/01/iop.0000226920.54294.0c. [DOI] [PubMed] [Google Scholar]
- 23. Bayston R, de Louvois J, Brown EM, Johnston RA, Lees P, Pople IK. Use of antibiotics in penetrating craniocerebral injuries. “Infection in Neurosurgery” Working Party of British Society for Antimicrobial Chemotherapy. Lancet. 2000;355(9217):1813–1817. doi: 10.1016/s0140-6736(00)02275-3. [DOI] [PubMed] [Google Scholar]
- 24. Ramos R, Antunes C, Machado MJO, Almeida R. Penetrating head trauma injury with an excellent outcome. BMJ Case Rep. 2017;2017 doi: 10.1136/bcr-2017-219746. bcr-2017-219746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kawai N, Yabuno S, Hirashita K, Yoshino K. A case of transpetrosal penetrating head injury near the sigmoid sinus. Surg Neurol Int. 2021;12:468. doi: 10.25259/SNI_503_2020. [DOI] [PMC free article] [PubMed] [Google Scholar]