Pediatricians' conviction is that pediatric chronic pain is mainly psychological; however, when talking to patients and families, they stress biological factors as main cause.
Keywords: Pain concepts, Pediatricians, Chronic pain, Qualitative analysis, Children and adolescents, Biopsychosocial framework
Abstract
Introduction:
Chronic pain is a prevalent, yet underrecognized, condition in children and adolescents. A biopsychosocial framework has been widely adopted over the past decades and resulted in a new pain classification in the International Classification of Diseases, 11th revision (ICD-11). Nevertheless, little is known about pediatricians' pain concepts.
Objectives:
We explored pain concepts of Swiss pediatricians by means of a qualitative analysis.
Method:
A cross-sectional online survey was sent to clinically active Swiss pediatricians registered with the Swiss Society for Pediatrics. A case vignette of a girl with chronic musculoskeletal pain was presented and pediatricians were asked (1) what they think caused the pain, and (2) how they would explain the pain to the patient and their family. Structuring content analysis was applied to describe major themes within the answers.
Results:
The following main categories emerged: psychological factors, biological factors, unclear etiology, social context, disorder specific, and multifactorial. Most pediatricians reported the belief that psychological factors explained the pain. However, when explaining the pain to the patient, biological factors were reported most often.
Conclusion:
There is a discrepancy between pediatricians' conviction that chronic pain is mostly explained by psychological factors and their exploratory model towards patients that focuses on biological factors. Promoting the biopsychosocial framework of chronic pain is key to ensure timely and effective treatment. The new pain classification in the ICD-11 has the potential to increase the use of the biopsychosocial model.
1. Introduction
Pediatric chronic pain is a prevalent condition, with varying international prevalence rates ranging between 20% and 44%.2,13,17,38,40 In a recent survey among Swiss pediatricians, their estimated prevalence of patients with chronic pain seen in their practices was approximately 3%, which is considerably lower.19 This might in part be due to an underrecognition of chronic pain problems,37 associated with a lack of a clear diagnostic classification. According to the established and evidence-based biopsychosocial framework, chronic pain is considered to be explained by biological (eg, genetic disposition, peripheral or central sensitization), social (eg, socioeconomic status, family dynamics), and psychological (eg, emotions, trauma) factors.12,29 Based on this understanding, pediatric chronic pain is best treated with interdisciplinary care, including for example physiotherapy, medication if needed, and psychotherapy.6,15 Historically, however, pain has been understood as a biomedical problem, and, as a consequence, it has been treated with biomedical solutions.25,54
For patients, successful reconceptualization of chronic pain as multifactorial can produce positive effects such as improving pain and pain-related disability, and normalizing pain beliefs.11,20,31,32 Similarly, progressively increasing attention has been paid to the dimension of patients' experiences of the pain condition and their subjective illness narratives. According to the well-established illness paradigm, patients create cognitive models of their illness, which constitute 5 core dimensions: identity, cause, control, timeline, and consequences.18 Some studies revealed that the patient's perspective is linked to symptom relief and the healing process in general.44,45,50 Along similar lines, it has been suggested that pediatricians' beliefs about chronic pain are important for the course of treatment, including how they educate patients and families about pain.14,20 It has been hypothesized that perception of physicians of an illness consists of the same dimensions as the one for patients, yet it is based on academic knowledge and clinical experience.1 Nevertheless, qualitative studies that explore physicians' personal pain concepts are scarce, especially for the treatment of children and adolescents with chronic pain. One study reported that physicians have 3 diverging perspectives about pain, ie, biological, professional, and personal perspectives. However, these perspectives were all examined within the physicians' representation of the doctor–patient relationship.52 A very recent study also focused on the link between physicians' illness perceptions and their relationship with their patients.1 Due to the lack of relevant studies in the field of pediatric pain, we set out to explore current pain concepts of Swiss pediatricians by means of qualitative survey. For doing so, we used a case vignette of a girl with chronic musculoskeletal pain. The pediatricians were asked 2 questions, ie, what they think caused the pain and how they would explain the pain to the patient and their family.
2. Methods
This study is part of a larger survey that also intended to estimate the prevalence rate of pediatric chronic pain as seen in private pediatric practices and to assess pediatricians' professional experience with and care provision for patients with pediatric chronic pain (reported elsewhere, see Ref. 19).
2.1. Study design and study sample
All Swiss pediatricians registered with the Swiss Society of Pediatricians (SSP), the largest national, professional organization for pediatricians, were asked whether they would consent to participate in the cross-sectional online survey. At the time of the survey, approximately 2,500 pediatricians were registered with the SSP, the final mailing list of clinically active pediatricians included 1,595 addresses. The study was exempted from a full ethical review by the Ethics Committee Zurich, Switzerland (Project ID: 2019-00111). Data collection took place between March and April 2019, using Questback's UniPark tool for the online questionnaire.39 Two reminder emails were sent to potential participants after the initial inquiry.
2.2. Questionnaire
Data collection was anonymous and participation was voluntary. The first part of the questionnaire included questions about prevalence estimates and are reported elsewhere.19 The second part of the questionnaire is the focus of this study and consisted of questions on sociodemographic background and professional characteristics. Specifically, we used a case vignette to qualitatively assess pain concepts of participants. The case vignette was designed by a group of pain experts with backgrounds in pediatrics, psychology, and public health, with the goal to present participants with a patient they might see in their own practice: a 14-year-old girl reports musculoskeletal pain in the upper and lower extremities with no specific triggers that can be identified. The girl has been referred to an orthopedic surgeon and a pediatric rheumatologist, neither of whom found evidence of a cause from their area of expertise (Table 1).
Table 1.
Case vignette.
| Present complaint: A 14-year-old girl who comes to your office. She reports musculoskeletal pain in the lower and upper extremities. These occur symmetrically with movement, are distributed throughout the day with a duration of a few seconds to a few hours and improve with rest. Specific triggers of the complaints cannot be elicited. There is no morning stiffness and no nocturnal pain. At the girl's initial presentation 3 mo ago, these complaints had been present for 3 mo. After your evaluation in the office, the girl had been referred to an orthopedic surgeon and a pediatric rheumatologist, neither of whom found evidence of a cause from their specialty. The pain had resulted in 4 school absences of 1 and 2 d each in the previous 6 wk |
| Personal history: Until 5 mo ago, hip hop dancing 1x/wk for 1 h each; then suspended. Approximately 7 mo ago, general health had sustained a left upper ankle distortion trauma at a school function. At that time, there was a local hematoma; a lesion of the ligamentous apparatus or a fracture had been ruled out. The further personal history was unremarkable. Vaccinations up to date according to the Federal Office of Public Health (FOPH) recommendations, no allergies, no other traumas |
| Family history: 12-year-old brother, healthy. Parents without known diseases |
| Clinical findings: 14-year-old girl in good general health and nutritional status. Weight 51 kg (P50), body length 160.1 cm (P50). Gait symmetrical, muscular trophism unremarkable. All joints are freely mobile without redness, swelling, or hyperthermia. On passive movement of wrist left, shoulder elevation left, and knee joint right: Alternating indication of pain, no limitation of mobility. The further pediatric status is unremarkable |
Two open-ended questions were asked in relation to the case vignette: “What do you think is the etiology of the pain?” and “Please describe how you explain the cause of the pain to the parent and child.” Since Switzerland is multilingual, the German questionnaire was translated to Italian and French by a professional translation agency.
2.3. Qualitative analyses
We applied structuring content analysis.28 Data were coded and analyzed by 2 independent raters (ie, J.S. and K.M.G.) using the program MAXQDA.53 Structuring content analysis is suitable to summarize, structure, evaluate, and analyze large data sets. We conducted a multistage analytic process23,28: First, we defined our 2 research questions (ie, “What narratives for the etiology of pain do pediatricians use?”; “How do pediatricians explain the cause of the pain to the parent and the child?”). Second, based on theoretical considerations, we decided to define the level of abstraction a priori. Third, the 2 raters worked through the text material line by line. As soon as a text passage fitted the overall theme, a category was constructed. Fourth, after working through a substantial amount of the material (ie, 15%) and in a consensual process between the 2 raters, we adapted the whole category system. Fifth, the 2 raters worked through the whole material with the same rules (ie, category definition and level of abstraction). Sixth, we classified the final list of categories into main categories. Seventh, we conducted the intercoder agreement. The 2 raters compared the 2 coding schemes, discussed disagreements, and reached consensus on one scheme. Disagreements were resolved with a third rater (ie, H.K. or C.L.). Finally, we performed frequency analyses of the category occurrences in the text material.
3. Results
3.1. Sample characteristics
A total of 233 pediatricians answered the open questions and were included for this study. In our sample, 70.6% identified as female, 29.4% identified as male, and most participants ranged between 36 and 55 years of age (Table 2).
Table 2.
Sociodemographic and work-related characteristics of the sample (N = 337).
| N | % | |
|---|---|---|
| Gender | ||
| Female | 238 | 70.6 |
| Male | 99 | 29.4 |
| Age category | ||
| ≤35 y | 21 | 6.2 |
| 36–45 y | 144 | 42.7 |
| 46–55 y | 109 | 32.2 |
| 56–65 y | 59 | 17.5 |
| >65 y | 4 | 1.2 |
| Year of specialization | ||
| 1980–1989 | 22 | 6.5 |
| 1990–1999 | 78 | 23.1 |
| 2000–2009 | 119 | 32.3 |
| 2010–2019 | 118 | 35 |
| Language region of workplace* | ||
| German speaking | 211 | 62.6 |
| French speaking | 113 | 33.5 |
| Italian speaking | 19 | 5.3 |
| Workplace* | ||
| Single practice | 54 | 16 |
| Group practice | 171 | 50.7 |
| University hospital | 70 | 20.8 |
| Cantonal hospital | 64 | 19 |
| Regional hospital | 23 | 6.8 |
| Other | 19 | 5.6 |
| No. of patients seen quarterly (N = 209) | ||
| <205 patients | 27 | 12.9 |
| 250–500 patients | 51 | 24.4 |
| 500–750 patients | 48 | 23.0 |
| 750–1000 patients | 42 | 10.1 |
| 1000–1500 patients | 35 | 16.7 |
| >1500 patients | 6 | 2.9 |
| Other professionals in practice (N = 214) | ||
| Pediatrician | 145 | 67.8 |
| Psychologist | 33 | 15.4 |
| Physiotherapist | 15 | 7.0 |
| Occupational therapist | 5 | 2.3 |
| Medical specialist (other area) | 37 | 17.3 |
| Not applicable | 45 | 21.0 |
Multiple answers possible.
3.2. General description of responses and main categories
Participants' responses varied in form and length: some provided one-word responses, whereas others answered in whole sentences. In total, 726 quotations were given. The first research question (ie, “What narratives for the etiology of pain do pediatricians use?”) led to a total of 387 quotations with 6 main categories: psychological factors, biological factors, unclear etiology, disorder specific, social context, and multifactorial (in descending frequency). The second research question (ie, “How do pediatricians explain the cause of the pain to the parent and the child?”) was associated with a total of 341 quotations with 6 main categories: biological factors, psychological factors, unclear etiology, validating attitude towards the patient, multifactorial, and social (in descending frequency). Figure 1 shows a visual comparison of main categories across the 2 questions.
Figure 1.
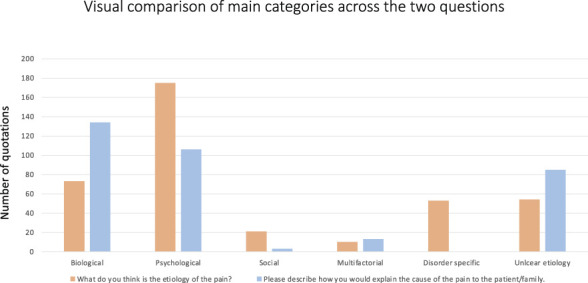
Visual comparison of main categories across the 2 questions.
In the following section, more details about the statements that pediatricians gave in relation to the 2 research questions are provided. For each main category, the number of quotations is displayed in parentheses.
3.3. First research question: “what narratives for the etiology of pain do pediatricians use?”
3.3.1. Psychological factors (total number of quotations: 175)
Most pediatricians highlighted that the origin of pain was psychosomatic (135 quotations), by which they meant that to a large extent, the pain is caused by psychological factors. Examples: “Pain may be the manifestation of a yet unknown psychopathology” or “Psychosomatic is obvious.” Several statements (18) saw the pain as a symptom of depression. Examples: “Sounds like depressed mood to me,” “Physical symptom of depression.”
Other statements concluded that the pain had psychogenic components (19). Examples: “Probably psychogenic,” or “especially psychogenic component.”
The remaining quotations revealed pediatricians' perception of the pain as due to other psychological factors, such as fear of pain or pain as a result of an adolescence crisis.
3.3.2. Biological factors (total number of quotations: 73)
Most quotations within this theme explained the pain as the result of trauma to the ankle (30). Examples: “Chronic pain experience, which may be triggered by the minor trauma,” “Posttraumatic condition,” or “Triggering factor was the ankle sprain.”
Other quotations suggested that pain was caused by pain sensitization (20). Examples: “Increased pain sensation” or “Increased body perception.” A small number of quotations (12) indicated that the pain may be the result of poor posture due to growing pains, cessation of sports, or muscular tension. Examples: “Terminating regular active sports,” “Muscular tension,” or “Growing pains.”
The remaining statements included lack of physical activity and other somatic issues.
3.3.3. Unclear etiology (total number of quotations: 54)
Numerous quotations (17) revealed that pediatricians were unsure about the etiology of the pain. Examples: “Unable to elicit from previous medical history,” “Unclear—as is unfortunately very common with these patients and female patients,” or “I cannot disentangle what is due to the main cause and what is in the realm of anxious anticipation of pain or the effects of avoidance behavior.”
Several quotations (37) described the pain as functional, indicating a lack of somatic correlates. Example: “If no organic cause, then functional,” or “Functional complaints.”
3.3.4. Disorder specific (total number of quotations: 53)
Several quotations specifically named a disorder as the cause of the pain: somatic symptom disorder (16), fibromyalgia (13), and complex regional pain syndrome (11). In addition, and less often, chronic pain syndrome or rheumatism were named.
3.3.5. Social context (total number of quotations: 21)
A number of quotations suggested that pain was caused by social circumstances, such as family or school problems. Examples: “Identify stressors and tension in the family, at school and with peers,” or “I would try to learn more about the environment, how are things at school?”
3.3.6. Multifactorial (total number of quotations: 10)
Few quotations mentioned that the pain may be caused by multiple factors, even fewer pointed to the biopsychosocial model. Examples: “The pain may have a multifactorial cause,” or “I assume an interaction of somatic, psychological, and social factors.”
3.4. Second research question: “how do pediatricians explain the cause of the pain to the parent and the child?”
3.4.1. Biological factors (total number of quotations: 134)
Most quotations indicated that pediatricians would explain the cause of the pain to be (purely) somatic. Respondents suggested that they would state that the pain was caused by altered nociception, leading to pain sensitization (89). Examples: “Hypersensitivity of the pain sensors,” or “Lowered tolerance threshold for multiple reasons.”
The second most common explanation (23) was trauma as the main cause for the pain. Examples: “Symptom expansion after minor trauma,” “Pain triggered by accident/trauma,” or “Due to the trauma 7 months ago, a pain process was triggered.”
Furthermore, pain was explained by the loss of the nociceptive warning function (20). Examples: “Normally, there is a mechanism that tells us when the pain has healed, and we no longer need to feel pain. Somehow this information has been lost and chronic pain occurs,” “([…] That pain can get a momentum of its own and become chronic,” or “The pain is actually felt but has lost its warning function).”
Pain as a result of poor posture, due to growing pains, cessation of sports or muscular tension were other common explanations (17). Examples: “Pain could be due to tension,” or “After stopping active sports, the metabolism in the muscles changes and the splitting of certain substances causes pain.”
Closely related to the idea that sensitization caused the pain was the view that pain occurred due to pain memory or a response to past pain (16). Examples: “She must have felt that pain in the beginning and her ‘brain’ maintains that pain as if the memory of the pain persists,” or “Memory of the previous trauma […], the body remembers and wants to express something.”
A final explanation was that a vicious continuous cycle caused the pain (11). Example: “A vicious cycle often develops: tension, pain, even more tension, avoidance, deconditioning.”
3.4.2. Psychological factors (total number of quotations: 106)
Most pediatricians would explain the etiology of pain to be psychosomatic (88). Examples: “Pain is the language of the soul,” or “There are situations where the body reacts to certain feelings with various reactions. […], or you have diarrhea before an exam.” Among those, a number of quotations indicate that the connection between body and mind have an influence on perceived pain (20). Examples: “Body and mind are connected. When the mind hurts, the body hurts, and vice versa,” or “Body and psyche are mutually influencing parts of every human being.”
Stress was also mentioned as a possible explanation for the pain (18). Examples: “There are cases where mental stress affects the body and causes pain, as a kind of cry for help,” or “At the moment, due to various stresses, pain cannot be properly allocated by the body, and that is why it is alarmed.”
In the remaining quotations, pediatricians stated that they would explain to the patient and their family that the pain was caused by psychological factors such as fear of pain.
3.4.3. Unclear etiology (total number of quotations: 85)
Several pediatricians stated that they would discuss with the patient and the family that it is difficult to find a cause of the pain. Examples: “The cause is not clear, but it is necessary to find a way to relieve the present pain,” or “I could not find an answer.” Among them, some pediatricians highlighted that the pain was unlikely to be associated with a serious disease (45). Examples: “A broad workup ruled out various serious diseases,” “The tests performed are reassuring to rule out a serious cause of the pain,” or “Nothing is broken.”
3.4.4. Validating attitude towards the patient (total number of quotations: 61)
One additional topic was frequently mentioned in pediatricians' answers and pointed to a general validating attitude towards their patient. Several statements emphasized the importance of validating and acknowledging the child's pain, regardless of its origin. Example: “Pain is really present even if the correlate is missing, meaning it's not imaginary.”
3.4.5. Multifactorial (total number of quotations: 13)
Some quotations indicated that pediatricians would explain that the pain could be caused by multiple factors. Examples: “I would try to explain the pain as multimodal, in the sense of an interaction of biology, psychology, and social environment,” or “May be due to several factors, which may be multifactorial.”
3.4.6. Social context (total number of quotations: 3)
Three quotations from pediatricians suggested that pain was caused by social circumstances, such as family or school problems. Example: “Search for personal or social anxiety difficulties.”
4. Discussion
The aim of this study was to qualitatively explore pediatricians' personal pain concepts and evaluate how they would explain the etiology of chronic pain to a patient and the family. Two open questions about a case vignette of a 14-year-old girl with chronic pain of unknown origin were asked. Our results show that pediatricians in our sample rarely referred to the biopsychosocial model, a widely accepted explanatory model for chronic pain,3,8,12,20 when explaining the pain to the family. We also found an interesting difference between what pediatricians think the cause of the pain is and their explanation to the patient and their family, supporting the notion that pediatricians' own pain concept is primarily shaped by their understanding that psychological factors largely contribute to chronic pain. This is in line with the fact that many physicians refer patients to a mental health professional once no organic lesion is identified.41 This can lead to patients' feeling of being misunderstood and hence noncompliance with medical advice because patients naturally strive for an explanation for their pain.21
Indeed, the concept of diagnostic uncertainty, ie, the perception that an explanation for a patient's health problem is missing or inaccurate,33 is highly prevalent in parents of children with chronic pain: almost 40% of parents indicate that they do not accept or “buy” their child's diagnosis.36 In pediatric patients with chronic pain, 31% of adolescents reported experiencing diagnostic uncertainty33 and 48% believed that something else was going on with their pain that doctors had not found out about yet.47 This is in line with our recent survey among Swiss pediatricians: We found that only 20% of pediatricians reported feeling confident in treating pediatric chronic pain.19 This might in part be due to the fact that pain courses are still rare in medical schools worldwide, with a median of 12 hours of compulsory pain medicine classes across Europe.43 A recent study in the United States showed that if pediatric residents are provided with a multidisciplinary pain education curriculum, their management and conceptualization of chronic pain changes.27
Notably, the experience of diagnostic uncertainty by patients and their families can negatively influence their communication with their pediatrician and the health care system.4,9 In our results, a number of pediatricians stated that the etiology of the pain remains unclear—both when asked about their own pain concept and when describing how they would explain the etiology to the family. This might indicate the presence of diagnostic uncertainty of pediatricians in our sample. Importantly, the introduction of the International Classification of Diseases, 11th edition (ICD-11) has the potential to offer a solution for pediatricians' presumptive diagnostic uncertainty. According to the ICD-11, chronic pain can now be a “disease in its own right”35: This means that the diagnosis of Chronic Primary Pain (CPP) is appropriate if a patient experiences chronic or recurrent pain for 3 or more months, associated with significant emotional distress and/or functional disability, and the pain is not better explained by another condition.34,51 Notably, however, the ICD-11 classification for chronic pain (ie, chronic primary and chronic secondary pain) has yet to be validated in large samples of children and adolescents.26
According to the new chronic pain classification of the ICD-11 and supported by the biopsychosocial understanding of pain, a change of view regarding care for pain is desirable, as Taylor and colleagues stated, “(…) the philosophy of care may change from a biomedical model that views chronic pain as a symptom to that of a biopsychosocial one that views chronic pain as a disease or long-term condition” (p. 1948).48 Without clinicians' biopsychosocial understanding of chronic pain, implementation of interdisciplinary care is at risk because a biopsychosocial framework enables health care professionals to advertise and administer interdisciplinary care that includes psychological support.6 The International Association for the Study of Pain defines interdisciplinary care as a “multimodal treatment provided by a multidisciplinary team collaborating in assessment and treatment using a shared biopsychosocial model and goals”49 (accessed on April 14, 2022). By contrast, in clinical practice, the first approach to manage pain is often purely pharmacological, despite a lack of high-quality evidence to support any pharmacological intervention to pediatric patients with chronic pain.7,22
Based on our findings, we propose that pediatricians might use the following steps as a guide when planning and implementing pain management. First, it is important to consider the primary pain disorders as part of the differential diagnosis, although a thorough validation is still outstanding.26 Second, a specific emphasis should be placed on pediatric chronic pain education and communication. This includes asking patients and their families about their own understanding of pain as well as possible biomedical causes. Pain education of patients itself includes (yet is not restricted to) statements such as “pain is a protector” and “the pain system can become overly protective” (for more details see Ref. 20). Third, treatment planning should always be in line with the biopsychosocial framework. Providing patients and their families with a biopsychosocial framework from the very beginning might help to reduce the threatening nature of pain, enable behavior changes if necessary,20 and mitigate the degree of diagnostic uncertainty.47 Notably, for all of these steps, a good patient-health care provider relationship builds the foundation for a successful communication.5,20 Studies highlight the need for both physicians' competence (composed of aspects such as efficiency, knowledge, and skills) and patients' perceptions of physicians' warmth (including personal aspects such as engagement, connection, and care for the patient).16
To the best of our knowledge, this is the first study that aimed to explore current pain concepts of pediatricians. It is of great importance to not only gain insights about patients' subjective illness narratives but also highlight pediatricians' point of view to guarantee a shared understanding and narrative.24 Nevertheless, our study has several limitations. First, we had a low response rate of approximately 20%. Considering the pediatrician workload, no reimbursement for study participation, and the nonpersonal invitation, the low response rate was expected (for details see Ref. 19). Second, all our data are based on self-report and might therefore be associated with bias. We did, for example, not observe the physicians' communication in clinical practice to gain a more nuanced impression of how they educate their patients about pain. Third, our survey focused on Swiss pediatricians, and thus it remains unclear whether the findings are transferrable to other countries. Finally, the choice to conduct a structuring content analysis according to Mayring28 has the limitation that only thematic descriptions are examined, which is contrary to other approaches that enable to generate explanatory theories (eg, grounded theory).46 Nevertheless, we think that for the aim of our study (ie, to explore current pain themes of pediatricians), a content analysis was most suitable.
Our findings indicate that the biopsychosocial model of chronic pain may not yet have been incorporated in pediatricians' personal understanding of chronic pain. We also found an interesting discrepancy between what pediatricians think is the cause of the pain (ie, mostly referring to psychological factors) and the way they explain pain to the patients and their families (ie, mostly mentioning biological factors). Thus, we conclude that the new ICD-11 classification for chronic pain may help pediatricians to better conceptualize pain diagnosis for themselves and their patients. Similarly, our findings support the notion that pain education of physicians should be incorporated into medical training as a dedicated, stand-alone module or course.27,30 This would ensure timely and accurate dissemination of pain research that clearly indicates that pain is not an exclusively biomedical phenomenon.10 Pediatricians are usually the first and main address for chronic pain complaints, and estimates from a large children's hospital in Switzerland indicate that it takes an average of 2 years before patients are finally referred to a specialized clinic.42 Thus, raising awareness amongst pediatricians and general practitioners that the biopsychosocial framework of pain is well suited to educate patients about pain is crucial to reduce the burden caused by chronic pain in children and adolescents.
Disclosures
The authors have no conflict of interest to declare.
Acknowledgements
The authors thank Jorinde Straub and Kimberly McGowan for their support in the coding of the text passages.
H. Koechlin receives funding from the Swiss National Science Foundation (P5R5PS_203064/1), as does C. Locher (PZ00P1_201972).
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Cosima Locher, Email: cosimaantoinette.locher@uzh.ch.
Andreas Wörner, Email: Andreas.Woerner@ukbb.ch.
Maria Carlander, Email: mj.carlander@gmail.com.
Joe Kossowsky, Email: Joe.Kossowsky@childrens.harvard.edu.
Julia Dratva, Email: drat@zhaw.ch.
References
- [1].Aloush V, Niv D, Ablin JN, Yaish I, Elkayam O, Elkana O. Good pain, bad pain: illness perception and physician attitudes towards rheumatoid arthritis and fibromyalgia patients. Clin Exp Rheumatol 2021;39:54–60. [DOI] [PubMed] [Google Scholar]
- [2].Ambord S, Eichenberger Y, Delgrande Jordan M. Gesundheit und Wohlbefinden der 11-15-jährigen Jugendlichen in der Schweiz im Jahr 2018 und zeitliche Entwicklung. Lausanne: Addiction Suisse, 2020. [Google Scholar]
- [3].Bevers K, Watts L, Kishino ND, Gatchel RJ. The Biopsychosocial model of the assessment, prevention, and treatment of chronic pain. US Neurol 2016;12:98–104. [Google Scholar]
- [4].Bhise V, Rajan SS, Sittig DF, Morgan RO, Chaudhary P, Singh H. Defining and measuring diagnostic uncertainty in medicine: a systematic review. J Gen Intern Med 2018;33:103–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Birkhäuer J, Gaab J, Kossowsky J, Hasler S, Krummenacher P, Werner C, Gerger H. Trust in the health care professional and health outcome: a meta-analysis. PLoS One 2017;12:e0170988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Coakley R, Wihak T. Evidence-based psychological interventions for the management of pediatric chronic pain: new directions in research and clinical practice. Children (Basel) 2017;4:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Eccleston C, Fisher E, Cooper TE, Grégoire M-C, Heathcote LC, Krane E, Lord SM, Sethna NF, Anderson A-K, Anderson B, Clinch J, Gray AL, Gold JI, Howard RF, Ljungman G, Moore RA, Schechter N, Wiffen PJ, Wilkinson NMR, Williams DG, Wood C, van Tilburg MAL, Zernikow B. Pharmacological interventions for chronic pain in children: an overview of systematic reviews. PAIN 2019;160:1698–707. [DOI] [PubMed] [Google Scholar]
- [8].Engel GL. From biomedical to biopsychosocial: being scientific in the human domain. Psychosomatics 1997;38:521–8. [DOI] [PubMed] [Google Scholar]
- [9].Fishbain DA, Bruns D, Disorbio JM, Lewis JE, Gao J. Exploration of the illness uncertainty concept in acute and chronic pain patients vs community patients. Pain Med 2010;11:658–69. [DOI] [PubMed] [Google Scholar]
- [10].Friedrichsdorf SJ, Giordano J, Desai Dakoji K, Warmuth A, Daughtry C, Schulz CA. Chronic pain in children and adolescents: diagnosis and treatment of primary pain disorders in head, abdomen, muscles and joints. Children (Basel) 2016;3:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Gallagher L, McAuley J, Moseley GL. A randomized-controlled trial of using a book of metaphors to reconceptualize pain and decrease catastrophizing in people with chronic pain. Clin J Pain 2013;29:20–5. [DOI] [PubMed] [Google Scholar]
- [12].Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull 2007;133:581–624. [DOI] [PubMed] [Google Scholar]
- [13].Gobina I, Villberg J, Välimaa R, Tynjälä J, Whitehead R, Cosma A, Brooks F, Cavallo F, Ng K, de Matos MG, Villerusa A. Prevalence of self-reported chronic pain among adolescents: evidence from 42 countries and regions. Eur J Pain 2019;23:316–26. [DOI] [PubMed] [Google Scholar]
- [14].Harrison LE, Pate JW, Richardson PA, Ickmans K, Wicksell RK, Simons LE. Best-evidence for the rehabilitation of chronic pain part 1: pediatric pain. J Clin Med 2019;8:1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Hechler T, Dobe M, Zernikow B. Commentary: a worldwide call for multimodal inpatient treatment for children and adolescents suffering from chronic pain and pain-related disability. J Pediatr Psychol 2010;35:138–40. [DOI] [PubMed] [Google Scholar]
- [16].Howe LC, Leibowitz KA, Crum AJ. When your doctor “gets it” and “gets you”: the critical role of competence and warmth in the patient-provider interaction. Front Psychiatry 2019;10:475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, MacDonald AJ. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. PAIN 2011;152:2729–38. [DOI] [PubMed] [Google Scholar]
- [18].Kleinman A. The illness narratives: Suffering, healing, and the human condition. New York, NY: Basic Books, 1988. [Google Scholar]
- [19].Koechlin H, Locher C, Carlander M, Kossowsky J, Woerner A, Dratva J. Estimating the prevalence of paediatric chronic pain in Switzerland: an online survey among paediatricians. Swiss Med Wkly 2022;152:w30194. [DOI] [PubMed] [Google Scholar]
- [20].Koechlin H, Locher C, Prchal A. Talking to children and families about chronic pain: the importance of pain education-an introduction for pediatricians and other health care providers. Children (Basel) 2020;7:179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Locher C, Koechlin H, Gaab J, Gerger H. The other side of the coin: nocebo effects and psychotherapy. Front Psychiatry 2019;10:555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Locher C, Kossowsky J, Koechlin H, Lam TL, Barthel J, Berde CB, Gaab J, Schwarzer G, Linde K, Meissner K. Efficacy, safety, and acceptability of pharmacologic treatments for pediatric migraine prophylaxis: a systematic review and network meta-analysis. JAMA Pediatr 2020;174:341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Locher C, Mansour R, Koechlin H, Büchi S. Patient-appraised beneficial moments during inpatient psychiatric treatment. BMC Health Serv Res 2020;20:734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Locher C, Meier S, Gaab J. Psychotherapy: a world of meanings. Front Psychol 2019;10:460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Martin SR, Zeltzer LK. Prioritizing pediatric chronic pain and comprehensive pain treatment in the context of the opioid epidemic. Pain Manag 2018;8:67–70. [DOI] [PubMed] [Google Scholar]
- [26].Matthews E, Murray G, McCarthy K. ICD-11 classification of pediatric chronic pain referrals in Ireland, with secondary analysis of primary vs secondary pain conditions. Pain Med 2021;22:2533–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Matthews J, Zoffness R, Becker D. Integrative pediatric pain management: impact & implications of a novel interdisciplinary curriculum. Complement Ther Med 2021;59:102721. [DOI] [PubMed] [Google Scholar]
- [28].Mayring P. Qualitative content analysis: theoretical foundation, basic procedures and software solution. Klagenfurt, 2014. Available at: http://nbn-resolving.de/urn:nbn:de:0168-ssoar-395173. [Google Scholar]
- [29].Melzack R, Wall PD. Pain mechanisms: a new theory. Pain Forum 1996;5:3–11. [Google Scholar]
- [30].Mezei L, Murinson BB. Pain education in north American medical schools. J Pain 2011;12:1199–208. [DOI] [PubMed] [Google Scholar]
- [31].Moseley GL. Reconceptualising pain according to modern pain science. Phys Ther Rev 2007;12:169–78. [Google Scholar]
- [32].Moseley GL, Nicholas MK, Hodges PW. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain 2004;20:324–30. [DOI] [PubMed] [Google Scholar]
- [33].Neville A, Jordan A, Pincus T, Nania C, Schulte F, Yeates KO, Noel M. Diagnostic uncertainty in pediatric chronic pain: nature, prevalence, and consequences. Pain Rep 2020;5:e871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Nicholas M, Vlaeyen JWS, Rief W, Barke A, Aziz Q, Benoliel R, Cohen M, Evers S, Giamberardino MA, Goebel A, Korwisi B, Perrot S, Svensson P, Wang S-J, Treede R-D; IASP Taskforce for the Classification of Chronic Pain. The IASP classification of chronic pain for ICD-11: chronic primary pain. PAIN 2019;160:28. [DOI] [PubMed] [Google Scholar]
- [35].Niv D, Devor M. Chronic pain as a disease in its own right. Pain Pract 2004;4:179–81. [DOI] [PubMed] [Google Scholar]
- [36].Noel M, Beals-Erickson SE, Law EF, Alberts NM, Palermo TM. Characterizing the pain narratives of parents of youth with chronic pain. Clin J Pain 2016;32:849–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Palermo TM. Impact of recurrent and chronic pain on child and family daily functioning: a critical review of the literature. J Develop Behav Pediatr 2000;21:58–69. [DOI] [PubMed] [Google Scholar]
- [38].Perquin CW, Hazebroek-Kampschreur AAJM, Hunfeld JAM, Bohnen AM, van Suijlekom-Smit LWA, Passchier J, van der Wouden JC. Pain in children and adolescents: a common experience. PAIN 2000;87:51–8. [DOI] [PubMed] [Google Scholar]
- [39].Questback GmbH. EFS survey; 2019. [Google Scholar]
- [40].Roth-Isigkeit A, Thyen U, Raspe HH, Stöven H, Schmucker P. Reports of pain among German children and adolescents: an epidemiological study. Acta Paediatr 2007;93:258–63. [PubMed] [Google Scholar]
- [41].Schechter NL. Functional pain: time for a new name. JAMA Pediatr 2014;168:693–4. [DOI] [PubMed] [Google Scholar]
- [42].Schneider T, Pfister D, Wörner A, Ruppen W. Characteristics of children and adolescents at the Switzerland-wide first ambulatory interdisciplinary pain clinic at the University Children's Hospital Basel—a retrospective study. Swiss Med Wkly 2019;149:w20073. [DOI] [PubMed] [Google Scholar]
- [43].Shipton EE, Bate F, Garrick R, Steketee C, Shipton EA, Visser EJ. Systematic review of pain medicine content, teaching, and assessment in medical school curricula internationally. Pain Ther 2018;7:139–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Sim J, Madden S. Illness experience in fibromyalgia syndrome: a metasynthesis of qualitative studies. Soc Sci Med 2008;67:57–67. [DOI] [PubMed] [Google Scholar]
- [45].Snelgrove S, Liossi C. Living with chronic low back pain: a metasynthesis of qualitative research. Chronic Illn 2013;9:283–301. [DOI] [PubMed] [Google Scholar]
- [46].Starks H, Brown Trinidad S. Choose your method: a comparison of phenomenology, discourse analysis, and grounded theory. Qual Health Res 2007;17:1372–80. [DOI] [PubMed] [Google Scholar]
- [47].Tanna V, Heathcote LC, Heirich MS, Rush G, Neville A, Noel M, Pate JW, Simons LE. Something else going on? Diagnostic uncertainty in children with chronic pain and their parents. Children 2020;7:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Taylor AM, Phillips K, Taylor JO, Singh JA, Conaghan PG, Choy EH, Tugwell PS, Kaiser U, Strand V, Simon LS, Mease PJ. Is chronic pain a disease in its own right? Discussions from a pre-OMERACT 2014 workshop on chronic pain. J Rheumatol 2015;42:1947–53. [DOI] [PubMed] [Google Scholar]
- [49].Terminology|International Association for the Study of Pain. International Association for the Study of Pain (IASP). Available at: https://www.iasp-pain.org/resources/terminology/. Accessed April 14, 2022. [Google Scholar]
- [50].Toye F, Seers K, Allcock N, Briggs M, Carr E, Andrews J, Barker K. Patients' experiences of chronic non-malignant musculoskeletal pain: a qualitative systematic review. Br J Gen Pract 2013;63:e829–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Treede R-D, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, Cohen M, Evers S, Finnerup NB, First MB, Giamberardino MA, Kaasa S, Kosek E, Lavand’homme P, Nicholas M, Perrot S, Scholz J, Schug S, Smith BH, Svensson P, Vlaeyen JWS, Wang S-J. A classification of chronic pain for ICD-11. PAIN 2015;156:1003–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Vegni E, Mauri E, Moja EA. Stories from doctors of patients with pain. A qualitative research on the physicians' perspective. Support Care Cancer 2005;13:18–25. [DOI] [PubMed] [Google Scholar]
- [53].MAXQDA 2022, [software], Berlin, VERBI Software, 2021. Available at: maxqda.com. [Google Scholar]
- [54].Zoffness R. Pediatric pain, CBT, and the internet: modern tools for pain management. Pediatric Pain Letter 2019;21:34–9. [Google Scholar]


