Abstract
Background
Telehealth delivery of preventive health services may improve access to care; however, its effectiveness and adverse effects are unknown. We conducted a comparative effectiveness review on the effectiveness and harms of telehealth interventions for women’s reproductive health and intimate partner violence (IPV) services.
Methods
We searched MEDLINE, Cochrane Library, CINAHL, and Scopus for English-language studies (July 2016 to May 2022) for randomized controlled trials (RCTs) and observational studies of telehealth strategies for women’s reproductive health and IPV versus usual care. Two investigators identified studies and abstracted data using a predefined protocol. Study quality was assessed using study design-specific standardized methods; disagreements were resolved through consensus.
Results
Eight RCTs, 1 nonrandomized trial, and 7 observational studies (n=10 731) were included (7 studies of contraceptive care and 9 of IPV services). Telehealth interventions to supplement contraceptive care demonstrated similar rates as usual care for contraceptive use, sexually transmitted infections, and pregnancy (low strength of evidence [SOE]); evidence on abortion was insufficient. Outcomes were also similar between telehealth interventions to replace or supplement IPV services and comparators for repeat IPV, depression, posttraumatic stress disorder, fear of partner, coercive control, self-efficacy, and safety behaviors (low SOE). In these studies, telehealth barriers included limited internet access, digital literacy, technical challenges, and confidentiality concerns. Strategies to ensure safety increased telehealth use for IPV services. Evidence on access, health equity, or harms was lacking.
Discussion
Telehealth interventions for contraceptive care and IPV services demonstrate equivalent clinical and patient-reported outcomes versus in-person care, although few studies are available. Effective approaches for delivering these services and how to best mobilize telehealth, particularly for women facing barriers to care remain uncertain.
Trial Registration
PROSPERO CRD42021282298.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-023-08033-6.
INTRODUCTION
Telehealth may improve access to health care for underserved populations and those facing barriers to care,1 but may widen disparities due to differences in internet access and digital literacy; age and language limitations1–3; availability of clinicians providing telehealth services; and social determinants of health. Recent research suggests telehealth may improve some obstetric and gynecologic outcomes4 and may be effective for contraceptive care,5–7 but has not definitively addressed whether telehealth increases access to care nor whether it results in similar or better outcomes compared with in-person care for women’s reproductive health and intimate partner violence (IPV) services.
We conducted a comparative effectiveness review in response to the increased use of telehealth during the COVID-19 pandemic.8–11 We focused on current research evaluating telehealth strategies for a specific subset of preventive health services included in the Women’s Preventive Services Initiative guidelines to inform HRSA program planning and identify research gaps, particularly for populations adversely affected by disparities.12 Reproductive health (family planning, contraception, and sexually transmitted infection [STI] counseling) and IPV services were selected because they are particularly amenable to telehealth interventions and may have been affected by limited in-person care early in the pandemic. This article is a condensed version of the full report.13
METHODS
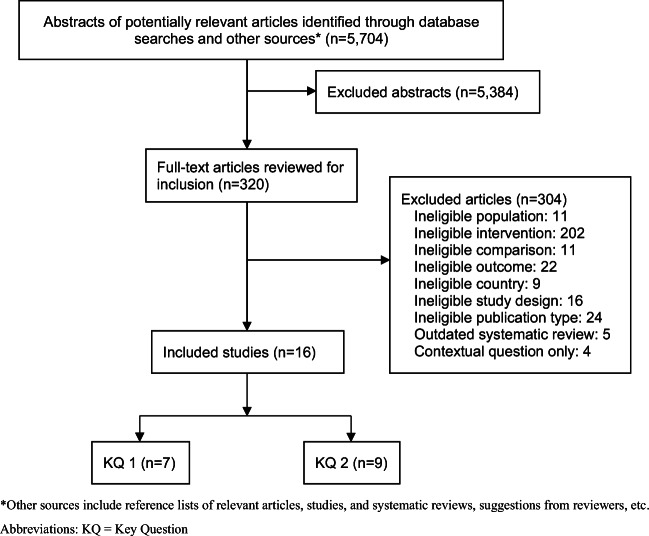
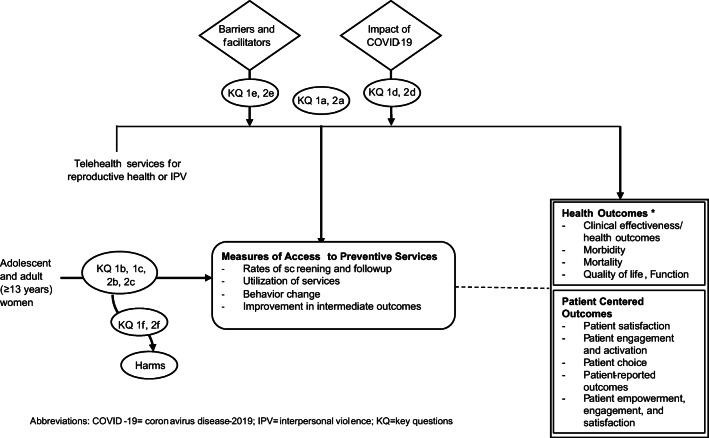
This review adhered to international Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines14 and was registered in PROSPERO on 6 June 2021 (CRD42021282298)15 (Fig. 1). An analytic framework and two key questions guided the review (Fig. 2) to address evidence on the comparative effectiveness, harms, patient experiences, barriers and facilitators, and utilization of telehealth during the COVID-19 pandemic for telehealth strategies aimed to supplement or replace in-person care. The first question focused on telehealth interventions for women’s reproductive health and the second on IPV. All methods were established a priori, after collaboration with an expert panel and followed AHRQ Methods.16 Detailed methods and findings are available the full report (https://effectivehealthcare.ahrq.gov/products/telehealth-women/research).13
Figure 1.
PRISMA flow diagram. *Other sources include reference lists of relevant articles, studies, and systematic reviews, suggestions from reviewers, etc. Abbreviations: KQ, key question.
Figure 2.
Analytic framework. Abbreviations: COVID-19, coronavirus disease-2019; IPV, interpersonal violence; KQ, key questions. The analytic framework illustrates how the populations, interventions, and outcomes relate to the KQ in the review. *Outcomes vary by preventive service and are specified in Appendix Table B-2.
Data Source and Searches
We searched Ovid MEDLINE, CINAHL, EMBASE, and Cochrane Central Register of Controlled Trials (July 1, 2016, to March 4, 2022) (Appendix Table A) and reviewed bibliographies of included studies. Searches began in 2016, following a recent review and evidence map of telehealth services for women,17 used to inform the scope of this review. Additional citations were identified from references lists, database searches, and expert consultation. Complete search strategies are in Appendix A.
Study Selection
Two investigators dual reviewed abstracts and full text articles using DistillerSR software to optimize efficiency. There was a high level of agreement and disagreements were resolved by consensus. Using a priori criteria, a hierarchy-of-evidence approach helped determine eligible studies. We included English-language randomized controlled trials (RCTs) and observational studies enrolling adolescent and adult women (≥13 years old), including those who are pregnant, and eligible for screening, counseling, or treatment for reproductive health (family planning, contraception, and STI counseling) and IPV services compared with in-person care. For this review, the term women is used inclusively and applies broadly to individuals with biological and other types of associations with the term. We considered controlled cohort studies conducted prior to the pandemic (beginning March 2020), and cohort, pre-post, and cross-sectional studies described as conducted during the pandemic or compared outcomes before and after March 2020 (Fig. 1, Appendix Table D-2).
We considered telehealth interventions that used technology to facilitate interactions at a distance between specific patients and clinicians and were bidirectional (e.g., a two-way telehealth interaction between a clinician and patient) or linked to clinical care. Reproductive health services included family planning, contraception, and STI counseling. Family planning was defined based on Title X guidelines18 and included preconception counseling and birth spacing. Contraceptive care (screening, counseling, provision, and follow-up care) was considered under reproductive health services, separate from family planning, and could be delivered via telehealth by a broad range of health care workers (e.g., physicians, nurses, pharmacists, counselors). Telehealth services for IPV included screening, diagnosis, and treatment for IPV and domestic violence. Details regarding study eligibility criteria are summarized in Appendix Tables B-1 and B-2.13
Data Extraction and Quality Assessment
A single investigator extracted detailed study characteristics, with dual review by a second reviewer for accuracy. Using predefined criteria, two reviewers independently applied study design–specific risk of bias (ROB) criteria to evaluate aspects most likely to affect critical biases13 (Appendix tables C1-4). Disagreements were resolved through consensus. Data were qualitatively synthesized and narratively summarized based on the direction of effect, statistical significance, and ROB and were grouped by clinical area, intervention details, and outcome. Strength of the body of evidence was assessed independently by two investigators following guidance established for AHRQ Evidence-based Practice Centers.16 Four key domains resulted in evidence graded as high, moderate, low, or insufficient based on the number, quality, and size of studies; the consistency of results between studies; and the directness of the evidence (Appendix Table D-4).16 Disagreements were resolved by consensus with a third reviewer. Cross-sectional and pre-post studies conducted during the COVID-19 pandemic were considered primarily to inform utilization or patient satisfaction outcomes. Meta-analysis was not conducted due to study heterogeneity. The full report describes additional methods (https://effectivehealthcare.ahrq.gov/products/telehealth-women/research)
RESULTS
Of 5704 eligible, unique citations, 8 RCTs,19–26 one nonrandomized trial,27 and 7 observational studies28–34 with 10,731 participants evaluated the effectiveness of telehealth interventions for contraceptive care and IPV (Fig. 1, Table 1, Appendix Tables D-1). Cross-sectional studies used survey data from clinicians and patients to evaluate the impact of telehealth interventions during the COVID-19 pandemic (Appendix table D-2). No studies evaluated telehealth interventions for family planning or STI counseling. Risk of bias was low in one study,31 moderate in nine trials19–27 and five observational studies,28,29,32–34 and high in one study.30 Telehealth interventions replaced usual care in 14 studies20–24,26–34 and supplemented care in two studies.19,25 Delivery modes included telephone (4 studies),19,25–27 online modules (6 studies),20–24,30 and mobile applications (1 study),29 and was unclear or undefined in five studies.28,31–34 Outcomes related to access, health equity, or health disparities were not addressed; data on harms was extremely limited. Main findings are summarized by preventive service (Table 2). Evidence tables of study and patient characteristics, results, and risk of bias assessments for individual studies are available in Appendix C and D and in the full report.13
Table 1.
Key Characteristics and Main Outcomes of Telehealth Trials by Clinical Condition
| Study, year | Study design RoB |
Population (N) | Intervention purpose; details | Comparison | Main outcomes (effect of telehealth) |
|---|---|---|---|---|---|
| Contraception | |||||
| Berenson, 2020 (41) |
RCT Moderate |
Low-income women 16 to 24 years (N=1155) | Supplement; telephone support | In-person counseling plus contraceptive supplies | Similar contraceptive use; similar STI and pregnancy rates |
| Kumar, 2019 (42) |
RCT Moderate |
Women seeking abortion care (N=569) | Supplement; structured telephone support | General advice to follow-up | Similar contraceptive use; similar abortion rates |
| Interpersonal Violence | |||||
| Ford-Gilboe, 202027 |
RCT Moderate |
Women >19 years with a history of IPV (N=531) | Replace; tailored, online tool | Static online tool | Similar depression scores (CES-D); similar coercive control (WEB) and PTSD rates; similar anxiety ratings (harms) |
| Gilbert, 201528 |
RCT Moderate |
Women >18 years undergoing supervision for substance use, with a history of IPV (N=191) | Replace; personalized, computerized program | Case manager (in-person) program | No difference in self-efficacy scores or safety behaviors |
| Glass, 201729 |
RCT Moderate |
Adult women with a history of IPV (N=720) | Replace; tailored, online tool | Static online tool | Similar rates of IPV; similar depression scores (CESD-R); similar coercive control (WEB) and PTSD scores |
| Hegarty, 201930 |
RCT Low |
Women 16-50 years who screen positive for IPV (N=422) | Replace; tailored, online tool | Static website | Similar depression scores (CESD-R); similar self-efficacy, coercive control |
| Koziol-McLain, 201932 |
RCT Moderate |
Women >16 years, experiencing IPV (N=412) | Replace; tailored, online tool | Static online tool | Similar rates of IPV and depression (CESD-R) |
| McFarlane, 200434 |
Nonrandomized trial Moderate |
Women receiving protection orders for IPV (N=150) | Replace; telephone-based support (6 additional calls) | In person counseling, 4 follow up calls | More safety behaviors in intervention group |
| Saftlas, 201436 |
RCT Moderate |
Women >18 years who screen positive for IPV (N=306) | Replace; telephone-based support | In person meeting, written materials | Improved (adjusted) depression scores (CES-D) in intervention group vs controls; similar self-efficacy scores |
Abbreviations: CES-D Center for Epidemiologic Studies Depression Scale, CESD-R Center for Epidemiologic Studies Depression Scale-Revised, IPV interpersonal violence, N total sample size, PTSD posttraumatic stress disorder, RCT randomized controlled trial, RoB risk of bias, STI sexually transmitted infection, WEB women’s experience with battering
Table 2.
Summary of Evidence and Strength of Findings
| Preventive service | Outcome | Intervention | Comparison | Studies (n) | Findings |
|---|---|---|---|---|---|
| Family planning† | NA | NA | NA | No studies | NA |
| Contraception | Contraceptive use | Supplemental telephone counseling; structured telephone support | Contraceptive supplies and in-person counseling; general advice for follow-up as needed | 2 RCTs (1724) | Low strength of evidence for similar contraceptive use |
| STI rates | Supplemental telephone counseling | Contraceptive supplies and in-person counseling | 1 RCT (1155) | Low strength of evidence for similar STI rates | |
| Pregnancy rates | Supplemental telephone counseling | Contraceptive supplies and in-person counseling | 1 RCT (1155) | Low strength of evidence for similar pregnancy rates | |
| Abortion rates | Structured telephone support | General advice for follow-up as needed | 1 RCT (569) | Insufficient strength of evidence for similar rates of abortion | |
| STI counseling | NA | NA | NA | No studies | NA |
| IPV | IPV rates | Interactive online tools | Noninteractive online tools | 2 RCTs (1132) | Low strength of evidence for no difference in IPV rates |
| Depression scores | In-person interviews followed by phone calls; interactive online tools | Referral; noninteractive online tools | 5 RCTs (2322) | Low strength of evidence for similar depression scores | |
| PTSD scores | Interactive online tools | Noninteractive online tools | 2 RCTs (1182) | Low strength of evidence for no difference in PTSD symptoms | |
| Fear, coercive control | Interactive online tools | Noninteractive online tools | 2 RCTs (884) | Low strength of evidence for no difference in coercive control | |
| Self-efficacy | Interactive online tools; computerized encounters; in-person interviews followed by phone calls | Noninteractive online tools; in-person encounters; referral | 3 RCTs (919) | Low strength of evidence for no difference in self-efficacy scores | |
| Safety behaviors | Telephone calls; computerized encounters; in-person interviews followed by phone calls | Usual care; in-person encounters; referral | 4 RCTs (1175) | Low strength of evidence for no difference in safety behaviors | |
| Harms | Interactive online tool | Noninteractive online tool | 1 RCT (231) | Insufficient evidence for no difference in reported anxiety |
*Outcomes reported separately; the same study may report different outcomes
†Family Planning was defined based on Title X guidelines2 and included preconception counseling and birth spacing; contraceptive care (screening, counseling, provision, and follow-up care) was considered separately under reproductive health services.
IPV interpersonal violence, LARC long-acting reversible contraception, NA not applicable, OCPs oral contraceptive pills, PTSD posttraumatic stress disorder, STI sexually transmitted infection, RCT randomized controlled trial
Reproductive Health Services
Effectiveness of Telehealth on Clinical Outcomes
Two RCTs of 1724 women and adolescents comparing supplemental telephone counseling with usual care found no differences between groups in rates of contraceptive use,19,25 STIs,19 pregnancy,19 and abortion25 (Table 2, Appendix Table D-1). Both RCTs met criteria for moderate risk of bias (Appendix Table C-1).19,25 Populations ranged from 569 to 1155 participants in reproductive health clinics in the USA19 or abortion clinics in the UK.25 Studies examined predominantly populations of Black, Hispanic, Asian, or other race (62 to 75%); lower income; and women ages 16 to 27 years. Neither study was conducted in a rural setting. Telephone counseling for contraceptive care was used to supplement clinic visits19 or provide structured telephone support25 for postabortion care. Telephone interventions in these studies were compared to standard care that included limited supplies of contraception plus in-person counseling19 or general advice for follow-up care.25 Limitations included high loss to follow-up, lack of blinding, and high attrition. Applicability was low due to the limited populations and narrow clinical settings.
Patient Engagement
Five cross-sectional studies from the USA described the impact of the COVID-19 pandemic on patient engagement for contraceptive care; studies did not evaluate STI counseling or family planning (Appendix Table D-2).28,31–34 Surveys ranged in sample size from 86 to 3142 participants and included primary care and family planning clinicians, and women seeking reproductive care. Studies evaluated the types of contraceptive services provided and examined patients’ use and acceptability of telehealth services for contraception during the pandemic. Risk of bias was low31 to moderate28,32–34 (Appendix Table C-4).
Two cross-sectional studies assessed either patient preferences33 or telehealth utilization for contraceptive care during the COVID pandemic.28 A US telephone survey from patients at a family planning clinic revealed high patient satisfaction (86%) and acceptability for the continued use of telehealth after the pandemic (72%); half preferred telehealth over in-person care (50%). Patients represented different demographic groups (12% White, 33% Black, 56% Hispanic), levels of education, marital, employment, and the majority (76%) reported never having prior difficulty accessing contraceptive care in the past 5 years.
Racial and ethnic differences in utilization of telehealth services were examined in a cross-sectional study from April to July 2020.28 Of 3142 sexual and reproductive health visits, 40% were conducted using telehealth. Black and multiracial patients had fewer telehealth visits versus in person care, while White and Asian/Native American/Hawaiian patients attended more telehealth visits versus in person care. There was no significant difference for patients identifying as Latinx. Reasons for between-racial group differences were not explored. Limitations included narrow selection of clinics in a single geographic region and did not describe the scope of services; however, the majority of visits (64%) were for contraception.
The remaining surveys34–37 described high overall levels of satisfaction and acceptability among patients and clinicians. Reported barriers to the use of telehealth included technical challenges, confidentiality concerns, billing concerns, and patient discomfort.36 Limitations of surveys include low overall response rates and potential recall bias regarding timing and delivery of services. Studies also lacked precision defining contraceptive and STI services and timeframes for the pre- and during-pandemic periods (Appendix Table D-3).
Intimate Partner Violence
Effectiveness of Telehealth on Clinical Outcomes
Six RCTs20–24,26 and a nonrandomized trial27 of 2,663 women indicated no differences between women randomized to telehealth interventions versus comparison for repeat IPV,22,24 depressive symptoms,20,22–24,26 posttraumatic stress disorder (PTSD) scores,20,22,24 fear of partner,23 coercive control,20,22 measures of self-efficacy,21,23,26 and safety behaviors,21–23,27 while only one RCT described harms.20 One RCT met criteria for low risk of bias23; five RCTs and one non randomized trial27 had moderate risk of bias20–22,24,26 (Appendix Tables C-1 and C-2). No trials evaluated patient preferences, choices, or patient engagement strategies of telehealth interventions for IPV. Trials were conducted in the USA,21,22,26,27 Australia or New Zealand,23,24 and Canada,20 and enrolled women with positive responses to IPV screening questions or recent IPV experiences. Trials enrolled between 150 and 720 women from academic medical centers,20,22 family planning clinics,26 a district attorney’s office,27 probation programs,21 and through online recruitment.23,24
Two RCTs evaluated repeat IPV, measured by the severity of violence against women scale (SVAWS).22,24 Both trials evaluated similar versions of a tailored, interactive online safety tool versus a static version, adapted for different populations from the USA (N=720)22 or New Zealand (N=412).24 In the US study, nearly 40% of the study population self-identified as Black, Asian, Native American, Hawaiian Pacific Islander, or multiracial, and 10% reported female partners.22 Both intervention and control groups reported a significant decrease in SVAWS subscales for psychological abuse, physical abuse, and sexual abuse. Less abuse occurred over time for both groups, with no differences between groups. In the New Zealand study, 27% of the study population identified as indigenous (Maori).24 Both groups demonstrated reduced IPV exposure over time, measured by the SVAWS, with no difference between groups at 12 months. A sub-analysis of indigenous women demonstrated a statistically significant effect of the intervention on IPV based on the SVAWS at 6 and 12 months compared with non-indigenous women.
Five RCTs20,22–24,26 evaluated depressive symptoms in 2322 participants using versions of the Center for Epidemiologic Studies Depression Scale (CES-D). One trial used telephone encounters to supplement in-person interviews compared with a control intervention involving referrals to community-based resources26; four trials evaluated similar versions of tailored, interactive online safety tools versus a static version, adapted for different populations of women with a history of IPV.20,22–24 One trial of a telephone intervention to supplement in-person interviews and reported improved CES-D scores (reduced depression) for both groups from baseline to 6 months. In the four trials of an interactive online safety tool, depression scores improved for both groups over time with no difference between groups.20,22–24
Two RCTs of depression also evaluated PTSD symptoms in 1182 participants20,22,24 using a tailored, interactive online safety tool versus a static version. Both studies used the PTSD checklist, Civilian Version (PCL-C), to measure PTSD symptoms and demonstrated similar or slightly improved measures for both groups from baseline to 12 months, with no difference between groups.
Two RCTs measured experiences of coercive control using the Women’s Experiences with Battering scale in 884 participants. One RCT randomized women to a tailored, interactive online safety intervention compared with a static version. Both studies reported improvements (scores declined) in IPV-related measures for both interactive online tools and control groups without significant differences between groups.20,22
Three RCTs21,23,26 used the Generalized Self-Efficacy Scale or the Domestic Violence Self-Efficacy Scale to evaluate self-efficacy scores in 919 participants and found no differences between groups. Scores improved (increased) from baseline to 12 months for both groups in one RCT23 favoring the control group. A RCT of women receiving community supervision for prior substance use in the US randomized women to computerized versus in-person services (comparison) and found self-efficacy scores improved for both groups, with no difference between groups.21 No differences in self-efficacy were reported in a RCT comparing in-person motivational interviews plus telephone sessions to community referrals.26
Four trials evaluated safety behaviors in 1175 participants with a history of IPV.21–23,27 Populations included women with protective orders against an intimate partner,27 women receiving community supervision for substance use in the USA,21 and women with a history IPV in Australia23 and the USA.22 Interventions included telephone calls versus usual care,27 computerized IPV services,21 and interactive computer modules versus a static website.22,23 Outcomes were measured using the Safety-Promoting Behavior Checklist that included 15 behaviors,27 or measurements of the number of safety behaviors adopted.21–23 There was no difference between groups in safety behavior scores in 4 RCTs reporting similar21–23 or slightly improved measures.27
Adverse events associated with telehealth interventions for IPV were reported in one trial of an online IPV intervention.20 Intervention and control groups reported similar rates of feeling “anxious or upset” when using the online tool, with no difference between groups.
Impact of COVID on IPV Interventions
One before-after study29 and one cross-sectional study30 described the impact of telehealth strategies for IPV during the COVID-19 pandemic in 995 participants in the USA (Appendix Table D-2). Studies evaluated IPV screening frequency or access to services during the COVID-19 pandemic using a mobile app, phone, or video conference in an academic health center or domestic violence organizations. Based on modified criteria, one study was rated moderate risk of bias29 and the other high risk of bias.30 The before-after study29 demonstrated increased use of the IPV self-screening tool in a prenatal care app in pregnant women during the COVID-19 stay-at-home order (March 23 to May 15, 2020) compared with pre-pandemic use, but similar outcomes for levels of physical violence, sexual violence, and psychological abuse.
The other cross-sectional study30 used phone or video conference interviews to identify barriers in English-speaking immigrant IPV survivors from several US regions and care providers to evaluate the effect of the COVID-19 pandemic on their relationship, accessibility of IPV services, and identification of pertinent needs or safety concerns. Participant-reported challenges included access issues (i.e., lack of internet access, digital illiteracy) and preference for face-to-face interactions, as it allowed survivors to leave their homes. Providers reported strengthening their web-based platforms to tailor safety plans using code words and hand signals during video conferences to mitigate risk during telehealth visits. Major study limitations include low power to detect change in IPV incidence.29,30
DISCUSSION
The findings of this comparative effectiveness review are generally consistent with other studies of telehealth that show telehealth interventions for other women’s health services (e.g., smoking cessation, breastfeeding, medication abortion, and high-risk obstetric scheduling) are associated with improved clinical outcomes.4 In this review, few studies were available to determine the comparative effectiveness of telehealth interventions for contraceptive care (screening, counseling, provision, follow-up care) or screening, evaluation, or treatment of IPV for women (Table 2). Two studies demonstrated that telehealth was either better or worse than usual care for outcomes related to contraceptive care or IPV services; the remaining 14 studies showed no differences in effectiveness. No studies evaluated telehealth services for family planning or STI counseling. Compared with usual care alone, telephone interventions to supplement in-person contraceptive care resulted in similar rates of contraceptive use (oral contraception, condoms, or long-acting reversible contraception) at 6 months, STI, and pregnancy (low strength of evidence [SOE]), while the impact on abortion rates was unclear (insufficient SOE). Compared with usual care, telehealth interventions for IPV services resulted in similar rates of repeat IPV, depression, fear of partner, coercive control, self-efficacy, post-traumatic stress disorder, and safety behaviors (low SOE), and unclear evidence on harms (insufficient SOE). Three studies indicated the COVID-19 pandemic increased telehealth utilization. Studies did not adequately evaluate factors related to access, health equity, or potential harms of telehealth.
Telehealth interventions in this review included video, interactive websites, mobile app, or telephone to supplement or replace in-person care to provide access to contraceptive care or IPV services. Findings suggest that several of these strategies could facilitate the uptake of telehealth for these preventive services and result in mostly similar outcomes. Remote provision of contraceptive care and reproductive health services using telehealth strategies is not a new practice, and is becoming more common due to emerging limitations on reproductive access.35 Prior to the COVID-19 pandemic, a wide range of reproductive health services were already being offered via telehealth.36 Telehealth utilization for contraceptive care is increasingly more common36 and is associated with high satisfaction and acceptability among patients and clinicians.37
Cross-sectional studies conducted during the COVID-19 pandemic offer a snapshot of utilization patterns or patient perspectives but provide a low level of evidence. While some studies report on service acceptability,32,33 measures of effectiveness are notably absent. Barriers to telehealth implementation include limitations in internet access, lack of comfort with technology, and lack of resources for engaging in telehealth services. Surveys reflect that strategies to ensure safety when using virtual platforms for IPV interventions are critical. The impact of telehealth on patient engagement, access to care, health equity, and harms is uncertain.
Limitations of the evidence included lack of relevant telehealth studies for these specific preventive services, the relative weakness of study designs used, the rigor with which the studies were executed, and the completeness of reporting key outcomes. Cross-sectional studies lacked comparison groups and did not isolate the effect of telehealth from historical trends or temporal changes resulting from the pandemic. Future studies should more clearly evaluate effectiveness of telehealth interventions and include studies that assess whether telehealth platforms can increase the reach of services and improve effectiveness for communities.
This review was limited in scope and included a defined subset of preventive services for a specific population. Studies of contraceptive care were limited to supplemental telephone delivered contraceptive counseling and offer a limited view of effectiveness. Patients in surveys may represent a self-selected group willing to receive telehealth services, limiting applicability. The focused timeframe for this review is characterized by a sudden acceleration in the telehealth adoption and concurrent rapid policy changes for telehealth reimbursement in response to the COVID-19 pandemic. Most studies were conducted when in-person care was considered unsafe.
Future studies should more clearly evaluate effectiveness of telehealth interventions, including the benefits or potential harms, in addition to research to identify the disadvantages telehealth may pose in delivering preventive services to specific underserved populations. Further well-designed studies, such as RCTs with clearly defined comparison groups and health outcomes, would improve understanding of effective telehealth interventions to address women’s preventive health care needs.
Limited evidence suggests that telehealth interventions for contraceptive care and IPV services result in equivalent clinical and patient-reported outcomes as in-person care. Uncertainty remains regarding the most effective approaches for delivering these services and how to best mobilize telehealth, particularly for women facing barriers to health care.
Supplementary Information
(DOCX 209 kb)
Funding
This manuscript is based on research conducted by the Pacific Northwest Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. 75Q80120D00006). This work received financial support from the Agency for Healthcare Research and Quality (AHRQ), Contract No. 75Q80120D00006.
Declarations
Disclaimer
The findings and conclusions in this document are those of the authors, who are responsible for its content and do not necessarily represent the views of AHRQ. Therefore, no statement in this review should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. None of the investigators have any affiliations or financial involvement that conflicts with the material presented in this report.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nouri S, Khoong EC, Lyles CR, Karliner L Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catal Innov Care Deliv. 2020.
- 2.Lyles CR, Sarkar U. Health literacy, vulnerable patients, and health information technology use: where do we go from here? J Gen Intern Med. 2015;30(3):271–2. doi: 10.1007/s11606-014-3166-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schifeling C, Shanbhag P, Johnson A, et al. Disparities in video and telephone visits among older adults during the COVID-19 pandemic: cross-sectional analysis. JMIR Aging. 2020;3(2):e23176. doi: 10.2196/23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DeNicola N, Grossman D, Marko K, Sonalkar S, Butler Tobah YS, Ganju N, et al. Telehealth Interventions to Improve Obstetric and Gynecologic Health Outcomes: A Systematic Review. Obstet Gynecol. 2020;135(2):371–82. doi: 10.1097/AOG.0000000000003646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chernick LS, Stockwell MS, Wu M, Castaño PM, Schnall R, Westhoff CL, et al. Texting to increase contraceptive initiation among adolescents in the emergency department. J Adolesc Health. 2017;61(6):786–90. doi: 10.1016/j.jadohealth.2017.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thiel de Bocanegra H, Bradsberry M, Lewis C, Maguire F. Do bedsider family planning mobile text message and e-mail reminders increase kept appointments and contraceptive coverage? Womens Health Issues. 2017;27(4):420–5. doi: 10.1016/j.whi.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Bull S, Devine S, Schmiege SJ, Pickard L, Campbell J, Shlay JC. Text messaging, teen outreach program, and sexual health behavior: a cluster randomized trial. Am J Public Health. 2016;106(S1):S117–S24. doi: 10.2105/AJPH.2016.303363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Betancourt JA, Rosenberg MA, Zevallos A, Brown JR, Mileski M. The impact of COVID-19 on telemedicine utilization across multiple service lines in the United States. Healthcare (Basel). 2020;8(4):380. doi: 10.3390/healthcare8040380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehrotra A, Ray K, Brockmeyer DM, Barnett ML, Bender JA. Rapidly converting to “virtual practices”: outpatient care in the era of Covid-19. NEJM catalyst innovations in care delivery. 2020.
- 10.Rockwell K, Gilroy A. Incorporating telemedicine as part of COVID-19 outbreak response systems. Am J Manag Care. 2020;26(4):147–8. doi: 10.37765/ajmc.2020.42784. [DOI] [PubMed] [Google Scholar]
- 11.Hong YR, Lawrence J, Williams D, Jr, Mainous IA. Population-level interest and telehealth capacity of US hospitals in response to COVID-19: cross-sectional analysis of Google search and National Hospital Survey data. JMIR Public Health Surveill. 2020;6(2):e18961. doi: 10.2196/18961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O'Neill J, Tabish H, Welch V, Petticrew M, Pottie K, Clarke M, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol. 2014;67(1):56–64. doi: 10.1016/j.jclinepi.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Cantor A, Nelson HD, Pappas M, Atchison C, Hatch B, Huguet N, et al. Effectiveness of Telehealth for Women’s Preventive Services. Comparative Effectiveness Review. No. #. (Prepared by the Pacific Northwest Evidence-based Practice Center under Contract No. 75Q80120D00006). Rockville, MD: Agency for Healthcare Research and Quality; April 2022.
- 14.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agency for Healthcare Research and Quality 2021; Accessed at https://effectivehealthcare.ahrq.gov/sites/default/files/pdf/telehealth-women-protocol.pdf on April 7, 2022.
- 16.Methods guide for effectiveness and comparative effectiveness reviews. Rockville, MD: Effective Health Care Program, Agency for Healthcare Research and Quality. Content last reviewed January 2020. https://effectivehealthcare.ahrq.gov/products/collections/cer-methods-guide.
- 17.Goldstein KM, Zullig LL, Dedert EA, Alishahi Tabriz A, Brearly TW, Raitz G, et al. Telehealth interventions designed for women: an evidence map. J Gen Intern Med. 2018;33(12):2191–200. doi: 10.1007/s11606-018-4655-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.U.S. Department of Health and Human Services Office of Population Affairs 2021; Accessed at https://opa.hhs.gov/grant-programs/title-x-service-grants/about-title-x-service-grants on December 10, 2021.
- 19.Berenson AB, Rahman M. A randomized controlled study of two educational interventions on adherence with oral contraceptives and condoms. Contraception. 2012;86(6):716–24. doi: 10.1016/j.contraception.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ford-Gilboe M, Varcoe C, Scott-Storey K, Perrin N, Wuest J, Wathen CN, et al. Longitudinal impacts of an online safety and health intervention for women experiencing intimate partner violence: randomized controlled trial. BMC Public Health. 2020;20(1):260. doi: 10.1186/s12889-020-8152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gilbert L, Shaw SA, Goddard-Eckrich D, Chang M, Rowe J, McCrimmon T, et al. Project WINGS (Women Initiating New Goals of Safety): a randomised controlled trial of a screening, brief intervention and referral to treatment (SBIRT) service to identify and address intimate partner violence victimisation among substance-using women receiving community supervision. Crim Behav Ment Health. 2015;25(4):314–29. doi: 10.1002/cbm.1979. [DOI] [PubMed] [Google Scholar]
- 22.Glass NE, Perrin NA, Hanson GC, Bloom TL, Messing JT, Clough AS, et al. The longitudinal impact of an internet safety decision aid for abused women. Am J Prev Med. 2017;52(5):606–15. doi: 10.1016/j.amepre.2016.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hegarty K, Tarzia L, Valpied J, Murray E, Humphreys C, Taft A, et al. An online healthy relationship tool and safety decision aid for women experiencing intimate partner violence (I-DECIDE): a randomised controlled trial. Lancet Public Health. 2019;4(6):e301–e10. doi: 10.1016/S2468-2667(19)30079-9. [DOI] [PubMed] [Google Scholar]
- 24.Koziol-McLain J, Vandal AC, Wilson D, Nada-Raja S, Dobbs T, McLean C, et al. Efficacy of a web-based safety decision aid for women experiencing intimate partner violence: randomized controlled trial. J Med Internet Res. 2018;19(12):e426. doi: 10.2196/jmir.8617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kumar U, Pollard L, Campbell L, Yurdakul S, Calvete CC, Coker B, et al. Specialist follow-up contraceptive support after abortion-Impact on effective contraceptive use at six months and subsequent abortions: A randomised controlled trial. PLoS ONE [Electronic Resource] 2019;14(6):e0217902. doi: 10.1371/journal.pone.0217902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saftlas AF, Harland KK, Wallis AB, Cavanaugh J, Dickey P, Peek-Asa C. Motivational interviewing and intimate partner violence: a randomized trial. Ann Epidemiol. 2014;24(2):144–50. doi: 10.1016/j.annepidem.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 27.McFarlane J, Malecha A, Gist J, Watson K, Batten E, Hall I, et al. Increasing the safety-promoting behaviors of abused women. Am J Nurs. 2004;104(3):40–50. doi: 10.1097/00000446-200403000-00019. [DOI] [PubMed] [Google Scholar]
- 28.Hill BJ, Lock L, Anderson B. Racial and ethnic differences in family planning telehealth use during the onset of the COVID-19 response in Arkansas, Kansas, Missouri, and Oklahoma. Contraception. 2021;104(3):262–4. doi: 10.1016/j.contraception.2021.05.016. [DOI] [PubMed] [Google Scholar]
- 29.Krishnamurti T, Davis AL, Quinn B, Castillo AF, Martin KL, Simhan HN. Mobile remote monitoring of intimate partner violence among pregnant patients during the COVID-19 shelter-in-place order: quality improvement pilot study. J Med Internet Res. 2021;23(2):e22790. doi: 10.2196/22790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sabri B, Hartley M, Saha J, Murray S, Glass N, Campbell JC. Effect of COVID-19 pandemic on women's health and safety: a study of immigrant survivors of intimate partner violence. Health Care Women Int. 2020;41(11-12):1294–312. doi: 10.1080/07399332.2020.1833012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Steiner RJ, Zapata LB, Curtis KM, Whiteman MK, Brittain AW, Tromble E, et al. COVID-19 and sexual and reproductive health care: findings from primary care providers who serve adolescents. J Adolesc Health. 2021;69(3):375–82. doi: 10.1016/j.jadohealth.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stifani BM, Avila K, Levi EE. Telemedicine for contraceptive counseling: an exploratory survey of US family planning providers following rapid adoption of services during the COVID-19 pandemic. Contraception. 2021;103(3):157–62. doi: 10.1016/j.contraception.2020.11.006. [DOI] [PubMed] [Google Scholar]
- 33.Stifani BM, Smith A, Avila K, Boos EW, Ng J, Levi EE, et al. Telemedicine for contraceptive counseling: patient experiences during the early phase of the COVID-19 pandemic in New York City. Contraception. 2021;104(3):254–61. doi: 10.1016/j.contraception.2021.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zapata LB, Curtis KM, Steiner RJ, Reeves JA, Nguyen AT, Miele K, et al. COVID-19 and family planning service delivery: findings from a survey of U.S. physicians. Prev Med. 2021;150:106664. doi: 10.1016/j.ypmed.2021.106664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aiken ARA, Starling JE, Scott JG, Gomperts R. Requests for Self-managed Medication Abortion Provided Using Online Telemedicine in 30 US States Before and After the Dobbs v Jackson Women’s Health Organization Decision. JAMA. 2022;328(17):1768–70. doi: 10.1001/jama.2022.18865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weigel G, Frederiksen BN, Ranji U, Salganicoff A 2019; Accessed at Kaiser Family Foundation at https://www.kff.org/womens-health-policy/issue-brief/telemedicine-in-sexual-and-reproductive-health/ on November 15, 2021.
- 37.Shin RJ, Yao M, Akesson C, Blazel M, Mei L, Brant AR. An exploratory study comparing the quality of contraceptive counseling provided via telemedicine versus in-person visits. Contraception. 2022;S0010-7824(22):00053-1. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 209 kb)