Abstract
Many adults with diabetes do not reach optimal glycemic targets, and, despite advances in diabetes management, diabetes technology use remains significantly lower in racial/ethnic minority groups. This study aimed to identify factors associated with achieving the recommended A1C target of <7% using data on 12,035 adults with type 1 diabetes from 15 centers participating in the T1D Exchange Quality Improvement Collaborative. Individuals attaining the target A1C were more likely to be older, White, have private health insurance, and use diabetes technology and less likely to report depressive symptoms or episodes of severe hypoglycemia or diabetic ketoacidosis than those with higher A1C levels. These findings highlight the importance of overcoming inequities in diabetes care.
Achieving and maintaining the recommended glycemic target (i.e., an A1C <7%) reduces risks for developing micro- and macrovascular complications of type 1 diabetes; however, many people with type 1 diabetes do not achieve this goal (1,2). A previous T1D Exchange clinic registry study showed that many adults (79%) did not achieve this A1C target (3). Use of diabetes technology, especially continuous glucose monitoring (CGM), is associated with better glycemic outcomes, including decreased severe hypoglycemia (SH) and diabetic ketoacidosis (DKA) and increased time in the target glucose range (70–180 mg/dL) (1–7). Unfortunately, racial/ethnic disparities exist in diabetes technology use, with lower use and higher A1C levels in Non-Hispanic Blacks and Hispanics compared with Non-Hispanic Whites (8–11).
It is important to understand the factors contributing to achieving and maintaining the recommended glycemic target to improve diabetes care and to decrease inequities among people with type 1 diabetes, not just in well-controlled clinical trials but also in real-world settings. This study from the T1D Exchange Quality Improvement Collaborative (T1DX-QI) used a dataset from a large cohort of adults with type 1 diabetes in a real-world setting in the United States to evaluate the factors associated with attaining the recommended A1C target.
Research Design and Methods
The T1DX-QI was established in 2016 and includes 15 U.S. adult diabetes clinics engaged in data-sharing and quality improvement (QI) methods to drive system changes. The collaborative aims to accelerate QI interventions through shared learning and continuous review of best practices. It is the first learning health system in the United States dedicated to the care of people with type 1 diabetes. Additional information about the T1DX-QI has been published (12).
We collected electronic health record (EHR) data from 15 centers for 12,035 adults (≥18 years of age) with type 1 diabetes in the T1D Exchange EHR database who had an encounter between January 2017 and January 2022 and at least one A1C measurement. The most recent A1C result during this period was used. We compared sociodemographic attributes, self-reported depressive symptoms, episodes of DKA, episodes of SH, and diabetes device use (CGM systems and insulin pumps) by A1C level (most recent A1C <7, 7–9, or >9%). The presence of depressive symptoms was defined as having a most recent nine-item Patient Health Questionnaire (PHQ-9) score ≥5 or a seven-item General Anxiety Disorder (GAD-7) score ≥5 or a two-item PHQ-2 score >0.
These categorical data are represented as the percentage of adults with either depressive symptoms or anxiety. Means (SDs) are reported for continuous variables. P values were calculated using χ2 tests to examine the associations between the categorical variables. A logistic regression analysis was performed, and odds ratios (ORs) are reported for factors associated with achieving the A1C target. The model was adjusted for age, race/ethnicity, insurance type, device use, and positive depression screening record. All analyses were performed using R, v. 3.6, statistical software (R Foundation, Vienna, Austria).
This project was deemed nonhuman subject research by the Western Institutional Review Board, and all participating centers received local institutional review board approval to share aggregate data and participate in this QI project. No protected health information was transmitted outside of each clinic for this project.
Results
Of the 12,035 adults with type 1 diabetes in the T1D Exchange EHR database, 23% had an A1C <7%, 44.5% had an A1C of 7–9%, and 32.5% had an A1C >9%. Characteristics of these adults by A1C are shown in Table 1. Those with an A1C >9% were significantly younger and more likely to be Non-Hispanic Blacks, experienced more DKA and SH events, and had more depressive symptoms (P <0.001 for all). They also had lower BMIs, were less likely to have private health insurance, and were less likely to use CGM and insulin pump therapy compared with individuals with an A1C <7% (P <0.001 for all).
TABLE 1.
Characteristics of Adults With Type 1 Diabetes (N = 12,035) Grouped by A1C
| Characteristic | Patients With A1C <7% (n = 2,774 [23%]) | Patients With A1C 7–9% (n = 5,363 [44.5%]) | Patients With A1C >9% (n = 3,898 [32.5%]) | P |
|---|---|---|---|---|
| Age, years | 33.4 ± 15.8 | 31.8 ± 16 | 26.6 ± 12.2 | <0.001 |
| Age-group, years 19–25 26–49 ≥50 |
1,215 (44) 1,034 (37) 495 (18) |
2,976 (55) 1,448 (27) 939 (18) |
2,778 (71) 801 (21) 319 (8) |
<0.001 |
| Female sex | 1,366 (49) | 2,694 (50) | 1,884 (48) | 0.1 |
| Race/ethnicity NH White NH Black Hispanic Other |
2,170 (78) 125 (5) 140 (5) 339 (12) |
4,054 (76) 364 (7) 367 (7) 578 (11) |
2,303 (59) 787 (20) 335 (9) 473 (12) |
<0.001 |
| Health insurance type Public Private Other |
498 (18) 1,650 (59) 626 (23) |
1,157 (22) 2,693 (50) 1,513 (28) |
1,144 (29) 1,479 (38) 1,275 (33) |
<0.001 |
| CGM used | 1,827 (66) | 2,944 (55) | 1,425 (37) | <0.001 |
| Insulin pump use | 1,380 (50) | 2,464 (46) | 1,030 (26) | <0.001 |
| CGM and insulin pump use | 1,132 (41) | 1,766 (33) | 612 (16) | <0.001 |
| Patients with DKA event | 148 (5) | 515 (10) | 860 (22) | <0.001 |
| Patients with SH event | 100 (4) | 270 (5) | 291 (7) | <0.001 |
| BMI, kg/m2 | 27 ± 5.8 | 27.7 ± 5.9 | 26.6 ± 6.2 | <0.001 |
| Overweight or obesity | 583 (21) | 1,309 (24) | 678 (17) | <0.001 |
Data are mean ± SD or n (%). NH, non-Hispanic.
Table 2 shows the factors associated with attainment of an A1C <7% in adults with type 1 diabetes. Use of diabetes technology (CGM and/or insulin pump therapy) and having private health insurance were associated with greater achievement of A1C <7% (ORs 1.28 and 1.47, respectively), while Non-Hispanic Black and Hispanic race/ethnicity (ORs 0.46 and 0.52, respectively) and screening positive for depressive symptoms (OR 0.60) had negative correlations with an A1C <7%.
TABLE 2.
Factors Associated With A1C <7% in Adults With Type 1 Diabetes (N = 12,035)
| Characteristic | OR (95% CI) | P * |
|---|---|---|
| Race/ethnicity NH White (ref) NH Black Hispanic |
— 0.46 (0.34–0.61) 0.52 (0.37–0.72) |
<0.001 <0.001 |
| Health insurance Public (ref) Private |
— 1.47 (1.19–1.80) |
<0.001 |
| CGM or insulin pump use | 1.28 (1.09–1.49) | <0.001 |
| Screened positive for depression | 0.60 (0.49–0.72) | <0.001 |
Adjusted for age, race/ethnicity, insurance type, technology use, and positive depression screening record. NH, non-Hispanic; ref, reference category.
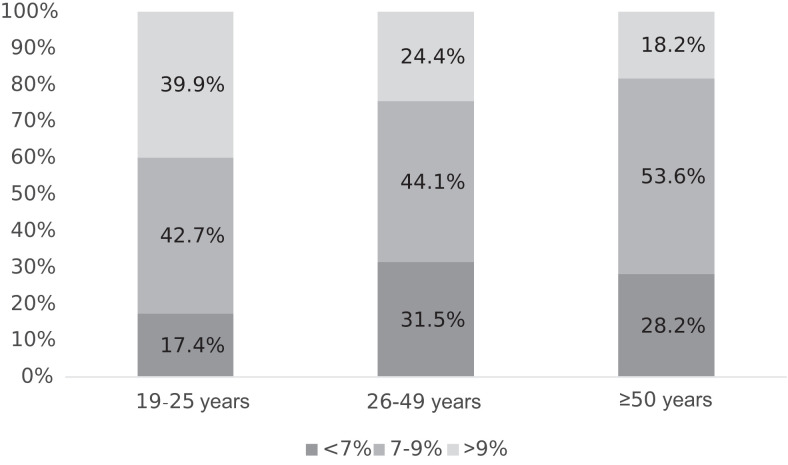
Figure 1 shows A1C achievement by age-group. In all age-groups (19–25, 26–49 and ≥50 years), most of the patients had A1C of 7–9%. In the 19- to 25-year-old age-group, 17.4% had an A1C <7%; among those 26–49 years of age, that proportion was 31.5%, and among those ≥50 years of age, it was 28.2%. Younger adults were much more likely than older adults to have an A1C >9%, a pattern that has been observed in earlier studies as well (3).
FIGURE 1.
A1C distribution by age.
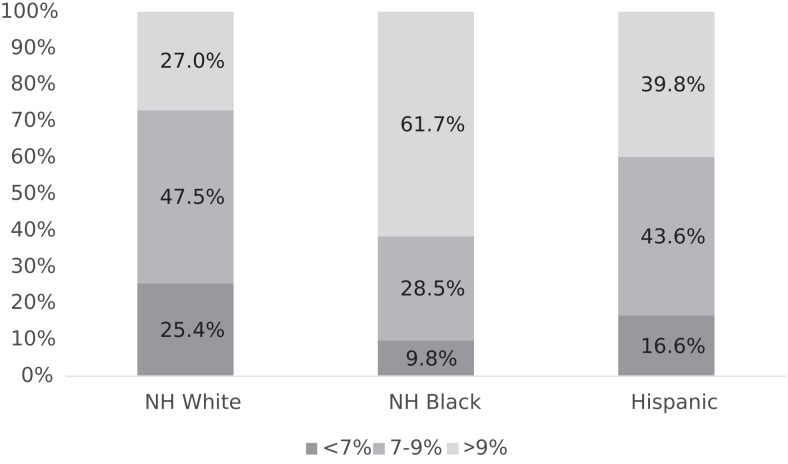
Figure 2 shows A1C achievement by race/ethnicity. Most non-Hispanic Whites (47.5%) and Hispanics (43.6%) had an A1C of 7–9%, whereas most non-Hispanic Blacks (61.7%) had an A1C >9%. The percentage of people not attaining the A1C target of <7% was highest among non-Hispanic Blacks (90.2%), followed by Hispanics (83.4%) and non-Hispanic Whites (74.6%).
FIGURE 2.
A1C by race/ethnicity. NH, non-Hispanic.
Discussion
The findings from these analyses of real-world data collected by the T1DX-QI demonstrate associations between the achievement of the recommended A1C target and race/ethnicity, health insurance coverage, DKA and SH events, depression, and diabetes technology use.
In our study, having private health insurance was associated with achieving an A1C <7% (OR 1.47). Previous studies have shown that patients with public health insurance were more likely to be hospitalized with DKA (13,14). Health insurance coverage for diabetes technology, medications, and supplies varies among both public and private plans. High copayments, high- deductible plans, and limited formularies may act as barriers to the adoption and use of CGM and insulin pump therapy.
Previous T1D Exchange data showed that CGM use was strongly associated with lower A1C levels (10,15). Several studies have shown a correlation between lower diabetes technology use and negative diabetes outcomes among non-Hispanic Blacks and Hispanics (8–10). Despite an increase in prevalence of type 1 diabetes among racial/ethnic minorities (16), inequity persists in racial/ethnic representation in randomized clinical trials of diabetes technology use in type 1 diabetes (17). Our work, and that of others, support the notion that there is a need to enroll more people from racial/ethnic minority groups in diabetes technology clinical trials. Most importantly, CGM and hybrid closed-loop insulin delivery systems should be made accessible to everyone in routine diabetes care. The incorporation of special programs that are sensitive to the cultural attitudes and lived experiences of adults living with type 1 diabetes should help more individuals use these devices and improve their glycemic profiles.
Another important finding of our study was that screening positive for depressive symptoms was negatively correlated with achievement of an A1C <7% (OR 0.6, 95% CI 0.49–0.72). The prevalence of depression among people with type 1 diabetes is two to three times higher than in the general population (18). Studies have shown that adults with comorbid depression and type 1 diabetes are less likely to achieve and maintain glycemic targets, have less interest in diabetes self- management, and are at increased risk for diabetes- related complications (19–21). It is important to both screen patients with diabetes for depression and treat depression among those affected to achieve recommended glycemic outcomes (22).
The strengths of this study include the use of a large database of racially/ethnically diverse adults from multiple centers to assess factors associated with attaining glycemic targets and the verification of diabetes technology use by EHR data rather than self-report. Limitations of this study include using academic-based diabetes centers, thus revealing findings that may not be generalizable outside of this setting, and using EHR data that are subject to documentation errors. We have incomplete glucose metrics (i.e., percentage of time in hypoglycemia and time in the target glycemic range) documented and do not know the percentage of individuals using hybrid closed-loop insulin delivery systems. Finally, data on social determinants of health were not available but are being collected for future analyses.
In summary, our results suggest that inequities in diabetes care still exist. Greater proportions of people from racial/ethnic minority groups did not reach glycemic targets when compared with non-Hispanic Whites. Having private health insurance and using advanced diabetes technology (i.e., CGM and insulin pumps) correlated with achieving an A1C <7%. Interventions are necessary to decrease racial/ethnic inequities in diabetes care among adults with type 1 diabetes.
Article Information
Acknowledgments
The authors thank the Leona M. and Harry B. Helmsley Charitable Trust for funding the T1DX-QI. The authors acknowledge the contributions of patients, families, diabetes care teams, and collaborators within the T1DX-QI who continually seek to improve care and outcomes for people with diabetes.
Duality of Interest
H.K.A., R.S.W., S.A., and S.P. have received research funding from multiple manufacturers of CGM systems and insulin pumps. O.E. is an advisory board member for the Medtronic Diabetes Health Equity Council. No other potential conflicts of interest relevant to this article were reported.
Author Contributions
H.K.A. wrote the manuscript. S.R. analyzed the data. O.E. conceptualized the manuscript. All of the authors reviewed/edited and approved the final version of the manuscript. S.R. and O.E. are the guarantors of this work and, as such, had access to all of the data and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation
Some of the data reported in this article were presented at the American Diabetes Association’s virtual 81st Scientific Sessions, 25–29 June 2021.
Footnotes
This article is part of a special article collection available at https://diabetesjournals.org/collection/1507/Leveraging-Real-World-Data-for-Quality-Improvement.
References
- 1. Akturk HK, Garg S. Technological advances shaping diabetes care. Curr Opin Endocrinol Diabetes Obes 2019;26:84–89 [DOI] [PubMed] [Google Scholar]
- 2. Slattery D, Choudhary P. Clinical use of continuous glucose monitoring in adults with type 1 diabetes. Diabetes Technol Ther 2017;19(Suppl. 2):S55–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Foster NC, Beck RW, Miller KM, et al. State of type 1 diabetes management and outcomes from the T1D exchange in 2016–2018. Diabetes Technol Ther 2019;21:66–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Beck RW, Riddlesworth T, Ruedy K, et al.; DIAMOND Study Group . Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections: the DIAMOND randomized clinical trial. JAMA 2017;317:371–378 [DOI] [PubMed] [Google Scholar]
- 5. Beck RW, Riddlesworth TD, Ruedy KJ, et al.; DIAMOND Study Group . Effect of initiating use of an insulin pump in adults with type 1 diabetes using multiple daily insulin injections and continuous glucose monitoring (DIAMOND): a multicentre, randomised controlled trial. Lancet Diabetes Endocrinol 2017;5:700–708 [DOI] [PubMed] [Google Scholar]
- 6. Pratley RE, Kanapka LG, Rickels MR, et al.; Wireless Innovation for Seniors With Diabetes Mellitus (WISDM) Study Group . Effect of continuous glucose monitoring on hypoglycemia in older adults with type 1 diabetes: a randomized clinical trial. JAMA 2020;323:2397–2406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lind M, Polonsky W, Hirsch IB, et al. Continuous glucose monitoring vs conventional therapy for glycemic control in adults with type 1 diabetes treated with multiple daily insulin injections: the GOLD randomized clinical trial. JAMA 2017;317:379–387 [DOI] [PubMed] [Google Scholar]
- 8. Agarwal S, Schechter C, Gonzalez J, Long JA. Racial-ethnic disparities in diabetes technology use among young adults with type 1 diabetes. Diabetes Technol Ther 2021;23:306–313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lyons SK, Ebekozien O, Garrity A, et al. Increasing insulin pump use among 12- to 26-year-olds with type 1 diabetes: results from the T1D Exchange Quality Improvement Collaborative. Clin Diabetes 2021;39:272–277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. DeSalvo DJ, Noor N, Xie C, et al. Patient demographics and clinical outcomes among type 1 diabetes patients using continuous glucose monitors: data from T1D Exchange real-world observational study. J Diabetes Sci Technol. Online ahead of print on 9 October 2021 (doi: 10.1177/19322968211049783) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Majidi S, Ebekozien O, Noor N, et al. Inequities in health outcomes in children and adults with type 1 diabetes: data from the T1D Exchange Quality Improvement Collaborative. Clin Diabetes 2021;39:278–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Alonso GT, Corathers S, Shah A, et al. Establishment of the T1D Exchange Quality Improvement Collaborative (T1DX-QI). Clin Diabetes 2020;38:141–151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. O’Malley G, Ebekozien O, Desimone M, et al. COVID-19 hospitalization in adults with type 1 diabetes: results from the T1D Exchange Multicenter Surveillance Study. J Clin Endocrinol Metab 2021;106:e936–e942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ebekozien O, Agarwal S, Noor N, et al. Inequities in diabetic ketoacidosis among patients with type 1 diabetes and COVID-19: data from 52 US clinical centers. J Clin Endocrinol Metab 2021;106:e1755–e1762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. DeSalvo DJ, Miller KM, Hermann JM, et al.; T1D Exchange and DPV Registries . Continuous glucose monitoring and glycemic control among youth with type 1 diabetes: international comparison from the T1D Exchange and DPV Initiative. Pediatr Diabetes 2018;19:1271–1275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dabelea D, Mayer-Davis EJ, Saydah S, et al.; SEARCH for Diabetes in Youth Study . Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA 2014;311:1778–1786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Akturk HK, Agarwal S, Hoffecker L, Shah VN. Inequity in racial-ethnic representation in randomized controlled trials of diabetes technologies in type 1 diabetes: critical need for new standards. Diabetes Care 2021;44:e121–e123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Garey CJ, Clements MA, McAuliffe-Fogarty AH, et al. The association between depression symptom endorsement and glycemic outcomes in adolescents with type 1 diabetes. Pediatr Diabetes 2022;23:248–257 [DOI] [PubMed] [Google Scholar]
- 19. Ludman EJ, Katon W, Russo J, et al. Depression and diabetes symptom burden. Gen Hosp Psychiatry 2004;26:430–436 [DOI] [PubMed] [Google Scholar]
- 20. Egede LE. Effects of depression on work loss and disability bed days in individuals with diabetes. Diabetes Care 2004;27:1751–1753 [DOI] [PubMed] [Google Scholar]
- 21. Bogner HR, McClintock HF. Costs of coexisting depression and diabetes. J Gen Intern Med 2016;31:594–595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord 2012;142(Suppl.):S8–S21 [DOI] [PubMed] [Google Scholar]