Abstract
Plexiform angiomyxoid myofibroblast tumour (PAMT) is a rare mesenchymal tumour of the stomach. To date, about 45 cases of PAMT have been reported in the literature. This is an extremely rare mesenchymal gastric tumour with definite histological pattern and is a tumour typified by spindle cells with myofibroblast characteristics. A 70-year-old woman was admitted with vague upper abdominal pain and dyspepsia and on OGD was found to have a polypoidal lesion with ulceration on the posterior wall of the body of the stomach towards the greater curvature. The endoscopy biopsy suggested the above diagnosis. The patient was investigated with CT scan and CT showed a large nodular growth 10 × 8 cm with pancreatic tail involvement and splenic involvement. The patient was treated with multi-visceral resection and favourable outcome was achieved. This entity of PAMT was a histological rarity and a technically challenging case and hence was analysed and presented. PAMT is a rare mesenchymal tumour of the stomach and is characterised by spindle cells with myofibroblast characteristics with a potential to differentiate towards smooth muscle cells. These tumours have a benign course and rarely can have an infiltrative behaviour. PAMT of the stomach is a very rare mesenchymal tumour with a unique histological appearance, and it needs to be distinguished from GIST and other gastrointestinal mesenchymal tumours, although extra gastric extension and vascular invasion are sometimes observed. Here, we are reporting this case as a case of PAMT arising from the body of the stomach which required multi-visceral resection.
Keywords: Plexiform Angiomyxoid Myofibroblast Tumour (PAMT), Mesenchymal Tumour, Gastric Tumour
Introduction
Plexiform angiomyxoid myofibroblast tumour (PAMT) is a rare mesenchymal tumour of the stomach. To date, about 45 cases of PAMT have been reported in the literature. This is an extremely rare mesenchymal gastric tumour. This tumour is not specific in clinical manifestations but has a definite histological pattern and is a tumour typified by spindle cells with myofibroblast characteristics [1] with a potential to differentiate towards smooth muscle cells. These tumours have a benign course and rarely can have an infiltrative behaviour [2].
This case is presented due to the rarity of the issue and rare occasion of multi-visceral resection in a case of plexiform angiomyxoid myofibroblast tumour.
Case Presentation
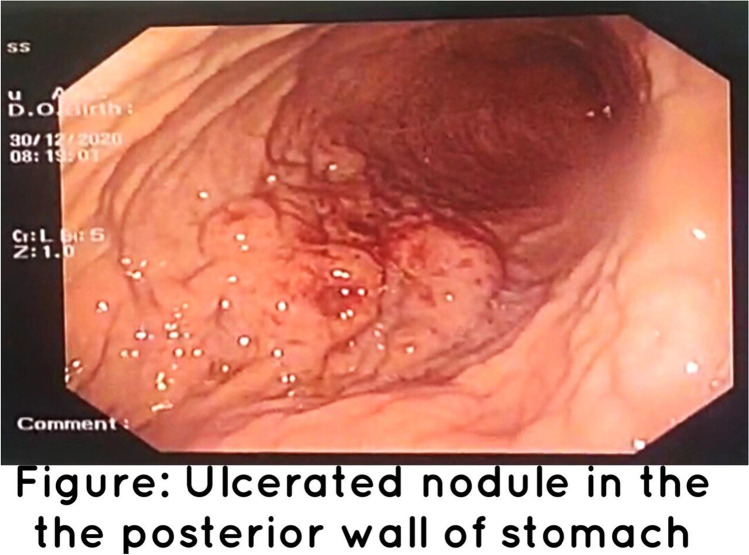
A 70-year-old woman was admitted with vague upper abdominal pain and dyspepsia and on endoscopy was found to have a polypoidal lesion with ulceration on the posterior wall of the body of the stomach towards the greater curvature (Fig. 1).
Fig. 1.
Nodular ulcerated lesion: posterior wall of the stomach and the greater curvature
The patient was investigated with CT scan and CT showed a large nodular growth 10 × 8 cm with pancreatic tail involvement and splenic involvement with infiltration to the Gerota’s fascia on the left side (Fig. 2).
Fig. 2.
Large nodular growth (10 × 8 cm) in close relation to the pancreatic body and the tail, the spleen, and the greater curvature of the stomach
The patient underwent a laparotomy and the tumour was 12 × 8 cm arising from the greater curvature of the stomach infiltrating the tail of the pancreas, splenic hilum, and Gerota’s fascia. The tumour was resected en-bloc (Fig. 3) with a sleeve gastrectomy, distal pancreatectomy, splenectomy, and resection of Gerota’s fascia.
Fig. 3.

Sleeve gastrectomy + distal pancreatectomy + splenectomy specimen. Specimen shows a nodular mass measuring 13 × 7 × 5.5 cm arising from the wall of the stomach. Growth is seen infiltrating the pancreatic parenchyma. The surface of the spleen unremarkable
Histopathological examination showed infiltrating neoplasm composed of cells arranged in fascicles and diffusely in background of collagenous and fibromyxoid matrix. Individual cells are plump spindle-shaped cells with a moderate amount of eosinophilic cytoplasm (Fig. 4). There was vascular proliferation and lymphocytic infiltration (Fig. 5).
Fig. 4.
Histopathology of infiltrating neoplasm composed of cells arranged in fascicles and diffusely in background of collagenous and fibromyxoid matrix. Individual cells are plump spindle-shaped cells with a moderate amount of eosinophilic cytoplasm. There was vascular proliferation and lymphocytic infiltration
Fig. 5.
IHC showed SMA positive, Desmin positive, EMA, synaptophysin, S-100, HMB, CD3, CD117, CD34, CD 31 all negative. DOG 1 negative
IHC showed SMA positive, desmin positive, EMA, synaptophysin negative, S-100, HMB, CD3, CD117, CD34, CD 31, and DOG1 negative. The same tumour clumps were infiltrating the Gerota’s fascia.
IHC also showed a low MIB (Ki67) index (1%), thus ruling out leiomyosarcoma as a possibility (Fig. 6).
Fig. 6.
IHC showed a low MIB (Ki67) index (1%)
This case is presented because of the rarity of the condition and its infiltrative behaviour.
Discussion and Conclusion
This entity of PAMT was a histological rarity and technically challenging case and hence was analysed and presented. PAMT is a tumour that usually arises from the gastric antrum and rarely from the fundus, body, or oesophagus. Our case was mainly arising from the body of the stomach making it an unusual location [3].
PAMT is a rare mesenchymal tumour of the stomach and is characterised by spindle cells with myofibroblast characteristics with a potential to differentiate towards smooth muscle cells. They have a whitish or reddish colour and form a lobulated submucosal or transmural mass. The mucosa is usually intact but can be ulcerated as in our case. It is not encapsulated and, in many cases, it protrudes outside the serosa, which often has a granular or nodular appearance like in our case. Very unusually the tumour infiltrates surrounding organs and that’s a sign of borderline type of tumour [4].
The typical diagnostic features are plexiform architecture, an abundant myxoid stroma rich in small blood vessels, and absence of plexiform pattern that is typical to exclude myxoid variant of GIST, inflammatory fibroid polyp, plexiform neurofibromas, and solitary fibrous tumour. They are differentiated by IHC and classical histological findings [5] (Table 1).
Table 1.
IHC differentiation
| IHC | PAMT | GIST | Plexiform neurofibromas |
|---|---|---|---|
| Positive | SMA positive |
CD117 DOG 1 KIT PDGFRA gene |
SMA Desmin H-caldesmon S-100 protein |
| Negative |
CD 117 CD 34 |
SMA S-100 protein EMA Desmin |
CD 117 CD 34 |
PAMT has an excellent prognosis with no recurrence or metastasis reported so far. PAMT can be categorized as a benign lesion based on favourable prognoses, absence of nuclear atypia, and low mitotic index [6]. However, vascular invasion was reported in one case by Reu et al.; thus, the possibility of metastasis cannot be completely excluded for PAMT cases and it needs more follow-up to comment on the outcome [7].
Conclusion
PAMT of the stomach is an extremely rare mesenchymal tumour with a unique histological appearance, and it needs to be distinguished from GIST and other gastrointestinal mesenchymal tumours. The tumour usually behaves as a benign lesion even though extra gastric extension has been reported and so operative resection with a margin is the best available treatment option as executed in our case. However, a continued follow-up of similar cases will be essential to finally predict the clinic pathological behaviour, pathogenesis, and outcome.
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sharath K. Krishnan, Email: sharathkkrishnan@yahoo.co.in
Ravindran Chirukandath, Email: ravimen@gmail.com.
Togy Zachariah, Email: ttzach13@gmail.com.
Rajiv Sajan Thomas, Email: dr.rajivsthomas@gmail.com.
References
- 1.Takahashi Y, Shimizu S, Ishida T, et al. Plexiform angiomyxoid myofibroblastic tumor of the stomach. Am J Surg Pathol. 2007;31:724–728. doi: 10.1097/01.pas.0000213448.54643.2f. [DOI] [PubMed] [Google Scholar]
- 2.Miettinen M, Fletcher CD, Kindblom LG, Tsui WM, editors (2010) Mesenchymal tumors of the stomach. In: WHO Classification of Tumours of the Digestive System. Lyon: IARC 74–79
- 3.Duckworth LV, Gonzalez RS, Martelli M, et al. Plexiform fibromyxoma: report of two pediatric cases and review of the literature. Pediatr Dev Pathol. 2014;17:21–27. doi: 10.2350/13-09-1373-OA.1. [DOI] [PubMed] [Google Scholar]
- 4.Ikemura M, Maeda E, Hatao F, et al. Plexiform angiomyxoid myofibroblastic tumor (PAMT) of the stomach A case report focusing on its characteristic growth pattern. Int J Clin Exp Pathol. 2014;7:685–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Kim A, Bae YK, Shin HC, Choi JH. Plexiform angiomyxoid myofibroblastic tumor of the stomach: a case report. J Korean Med Sci. 2011;26:1508–1511. doi: 10.3346/jkms.2011.26.11.1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kang Y, Jung W, Do IG, et al. Plexiform angiomyxoid myofibroblastic tumor of the stomach: report of two cases and review of the literature. Korean J Pathol. 2012;46:292–296. doi: 10.4132/KoreanJPathol.2012.46.3.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rau TT, Hartmann A, Dietmaier W. Plexiform angio myxoid myofibroblastic tumour: differential diagnosis of gastrointestinal stromal tumour in the stomach. J Clin Pathol. 2008;61:1136–1137. doi: 10.1136/jcp.2008.059162. [DOI] [PubMed] [Google Scholar]