Key Teaching Points.
-
•
Solia S60 lead (Biotronik) conductor fractures can occur after 6 months despite constant parameters at pacemaker interrogation.
-
•
An implantation depth of at least 12 mm covering the ring electrode might be advisable to reduce mechanical strain on the lead.
-
•
Early lead conductor fracture can suddenly occur despite uncomplicated implantation procedure.
Introduction
Left bundle branch area pacing (LBBAP) is an emerging technique of physiological pacing. It promises to improve clinical outcomes by sparing the detrimental effects of right ventricular (RV) pacing1,2 and to overcome the limitations of His bundle pacing (HBP) like poor pacing thresholds and low RV sensing amplitudes.3 Recently, the Biotronik Solia S60 stylet-driven, extendable-helix lead delivered via a Biotronik Selectra 3D sheath was described in a case series. In this small comparative study as an alternative to lumenless fixed helix leads, the stylet-driven lead yielded comparable implant success.4,5 Adverse events observed with stylet-driven leads for LBBAP are scarce. Here, we report a case of a delayed conductor fracture of the stylet-driven extendable-helix lead Solia S60 (Biotronik, Berlin, Germany) encountered 6 months after LBBAP implant.
Case report
A 79-year-old man presented to his cardiologist with new onset of dizziness and fainting in July 2021. Six months before, the patient had a pacemaker placed in the setting of third-degree atrioventricular block after transcatheter aortic valve replacement with preexisting right bundle branch block. For physiological pacing, LBBAP was established using the stylet-driven, active-helix Biotronik Solia S60 lead delivered via the Biotronik Selectra 3D 55-39 sheath. Implantation was performed as previously described by Huang and colleagues,2,6 resulting in stable and good pacing thresholds, pacing impedance, and sensing amplitudes (0.5 V @ 0.4 ms; 351 Ω unipolar, 526 Ω bipolar, 13.5 mV; Figure 1A) after a third positioning attempt. The sheath was carefully peeled after retraction of the stylet, and pacing values remained stable. No special occurrences were noted. The procedure duration was 125 minutes (fluoroscopy time 15.3 minutes, 10 mL contrast dye). Pacemaker interrogation 3 months after implantation revealed constant lead parameters (0.6 V @ 0.4 ms; 351 Ω unipolar, 565 Ω bipolar, 12.8 mV).
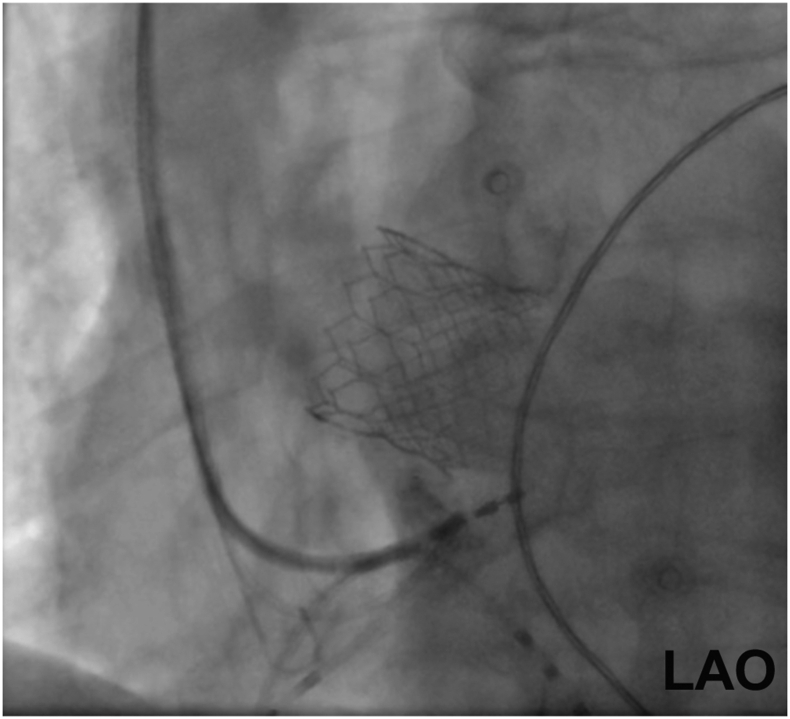
Figure 1.
Left anterior oblique (LAO) projection demonstrating implantation depth during contrast dye injection at primary implantation.
At presentation at the cardiologist’s office, the electrocardiogram showed an intermittent higher-degree atrioventricular block. Pacemaker interrogation revealed loss of capture and a lead impedance >2000 Ω. At maximum pacing output, intermittent capture was achieved. Chest radiography revealed no obvious lead anomaly or fracture. The patient was promptly admitted for pacing lead revision.
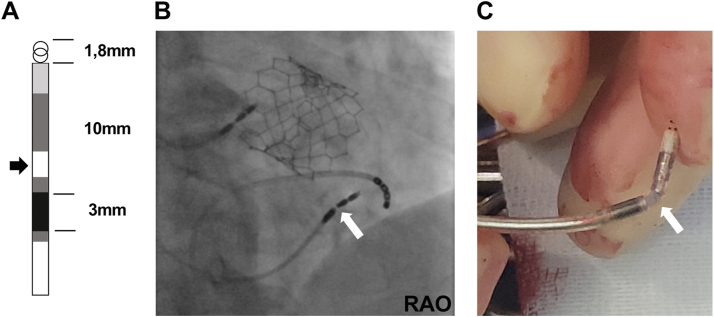
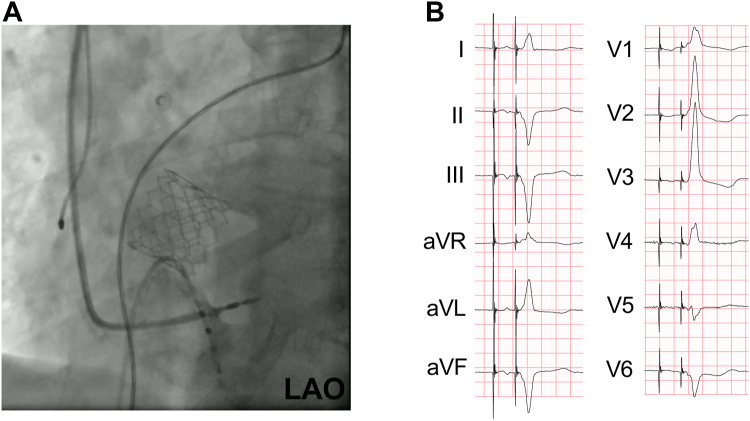
By fluoroscopy, the lead was in place in the ventricular septum, but a possible conductor fracture was visualized by a suggestive lead movement just before the ring electrode at the entry point into the septum (Figure 2A–2C and Supplemental Video). RV capture could be restored by reinserting a stylet in the pacing lead. The lead was subsequently extracted using the inserted stylet, unscrewing, and slight traction. A new LBBAP lead (Biotronik Solia S60) was inserted as described above in a slightly more apical direction with a deeper penetration into the RV septum using a Biotronik Selectra 3D 40-42 sheath, resulting in physiological pacing (Figure 3A and 3B). A detailed investigation of the extracted lead by the manufacturer confirmed the conductor fracture at the described site, possibly provoked mechanically by the septal contractions with every heartbeat. No further damage or lead anomalies were revealed.
Figure 2.
A: Schematic structure of the Solia S lead (Biotronik) highlighting the conductor breaking point (black arrow). B: Right anterior oblique (RAO) projection demonstrating lead fracture distal to ring electrode (white arrow). C: Image of the explanted lead breaking point marked with white arrow.
Figure 3.
A: Left anterior oblique (LAO) projection demonstrating implantation depth during contrast dye injection at lead revision. B: Left bundle branch area pacing in 12-lead electrocardiogram after lead revision (50 mm/s).
Discussion
We present a case of delayed distal Solia S60 conductor fracture 6 months after implant for LBBAP. According to the manufacturer’s performance report in 2021, the rate of conductor fractures in Solia leads is low (0.01%). However, the need for lead revision in physiological pacing is a known disadvantage of this technique, especially for HBP (about 4%, compared to 0.5% for RV pacing). In most instances, pacing capture loss has been described either as occurring within the first 30 days after implant or as being accompanied by progressive increases in pacing thresholds.7
Implantation of a stylet-driven lead via curved delivery sheaths for LBBAP is an attractive alternative to the wider spread use of lumenless leads. Owing to the additional stylet support, high implant success rates have been reported for LBBAP and HBP.4,5 Yet, the Solia S60 lead as used in the presented case comes with a more complex design and has a larger diameter of 5.9F, compared to 4.1F in lumenless leads. To date, only limited experience is available informing the performance of the Solia stylet system for LBBAP. In the presented case, the pacing lead was implanted at a depth of less than 12 mm, resulting in constant movement of the part between the ring and tip electrodes. Such mechanical stress may have provoked the observed conductor fracture (Figures 1 and 2). Also, the more basal implantation site close to the tricuspid valve, as in the presented case, might have resulted in a higher degree of motion stress on the lead.
According to published data, the mean LBBAP implantation depth, measured by echocardiography, was described as about 14 mm.8 It may thus be speculated that a deeper implantation depth, covering the ring electrode with myocardial tissue, might protect the interelectrode space and might help avoid mechanical stress–mediated lead fracture. Careful clinical observation is warranted to identify an excess rate of lead fractures at the culprit location in patients who underwent LBBAP. Whether this could be a specific problem of stylet-driven leads or might also apply to lumenless leads needs further surveillance. As a perspective, it might be advisable to ensure implantation at an oblique angle for sufficient implantation depth or select patients in whom at least some degree of septal hypertrophy is present to allow for the required implantation depth for stylet-driven LBBAP.
Footnotes
Funding Sources: There are no funding sources.
Disclosures: None; all authors declare no conflict of interest.
Supplementary data associated with this article can be found in the online version at https://doi.org/10.1016/j.hrcr.2022.10.004
Supplementary data
Fluoroscopy movie in RAO projection of lead fracture.
References
- 1.Sharma P.S., Patel N.R., Ravi V., et al. Clinical outcomes of left bundle branch area pacing compared to right ventricular pacing: results from the Geisinger-Rush Conduction System Pacing Registry. Heart Rhythm. 2022;19:3–11. doi: 10.1016/j.hrthm.2021.08.033. [DOI] [PubMed] [Google Scholar]
- 2.Huang W., Su L., Wu S., et al. A novel pacing strategy with low and stable output: pacing the left bundle branch immediately beyond the conduction block. Can J Cardiol. 2017;33:1736 e1–1736 e3. doi: 10.1016/j.cjca.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 3.Vijayaraman P., Ponnusamy S., Cano O., et al. Left bundle branch area pacing for cardiac resynchronization therapy: results from the International LBBAP Collaborative Study Group. JACC Clin Electrophysiol. 2021;7:135–147. doi: 10.1016/j.jacep.2020.08.015. [DOI] [PubMed] [Google Scholar]
- 4.Zanon F., Marcantoni L., Pastore G., Baracca E. Left bundle branch pacing by standard stylet-driven lead: preliminary experience of two case reports. HeartRhythm Case Rep. 2020;6:614–617. doi: 10.1016/j.hrcr.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Pooter J., Calle S., Timmermans F., Van Heuverswyn F. Left bundle branch area pacing using stylet-driven pacing leads with a new delivery sheath: a comparison with lumen-less leads. J Cardiovasc Electrophysiol. 2021;32:439–448. doi: 10.1111/jce.14851. [DOI] [PubMed] [Google Scholar]
- 6.Huang W., Chen X., Su L., Wu S., Xia X., Vijayaraman P. A beginner's guide to permanent left bundle branch pacing. Heart Rhythm. 2019;16:1791–1796. doi: 10.1016/j.hrthm.2019.06.016. [DOI] [PubMed] [Google Scholar]
- 7.Abdelrahman M., Subzposh F.A., Beer D., et al. Clinical outcomes of His bundle pacing compared to right ventricular pacing. J Am Coll Cardiol. 2018;71:2319–2330. doi: 10.1016/j.jacc.2018.02.048. [DOI] [PubMed] [Google Scholar]
- 8.Vijayaraman P., Subzposh F.A., Naperkowski A., et al. Prospective evaluation of feasibility and electrophysiologic and echocardiographic characteristics of left bundle branch area pacing. Heart Rhythm. 2019;16:1774–1782. doi: 10.1016/j.hrthm.2019.05.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fluoroscopy movie in RAO projection of lead fracture.