Learning objectives.
By reading this article, you should be able to:
-
•
Describe the anatomy of the cervical plexus.
-
•
Discuss the potential indications for cervical plexus block.
-
•
Describe the techniques for performing superficial, intermediate and deep cervical plexus block.
Key points.
-
•
The cervical plexus provides sensory innervation to the whole neck and upper anterior torso and motor innervation to most muscles in the neck.
-
•
Indications for cervical plexus block include procedures to the neck, clavicle or shoulder.
-
•
The cervical plexus may be divided into superficial (sensory) and deep (mostly motor) parts.
-
•
The cervical plexus can be identified and blocked using surface anatomical landmarks or ultrasound for guidance.
Cervical plexus block was traditionally used for awake carotid endarterectomy, but the potential uses of this block extend across many specialties, either as a sole technique, in combination with other regional anaesthetic techniques or as an adjunct to general anaesthesia.
Anatomy of the cervical fascia
The neck contains many important structures passing between the head and torso, including the trachea, oesophagus, blood vessels and nerves. Several layers of fascia surround the various musculoskeletal and visceral structures in the neck. These layers can be broadly divided into superficial and deep cervical fascia, although much debate exists around the detailed anatomy.1
The superficial cervical fascia is a loose layer of connective tissue containing platysma muscle, subcutaneous fat, cutaneous nerves, superficial veins (including the external jugular vein) and superficial lymph nodes.2
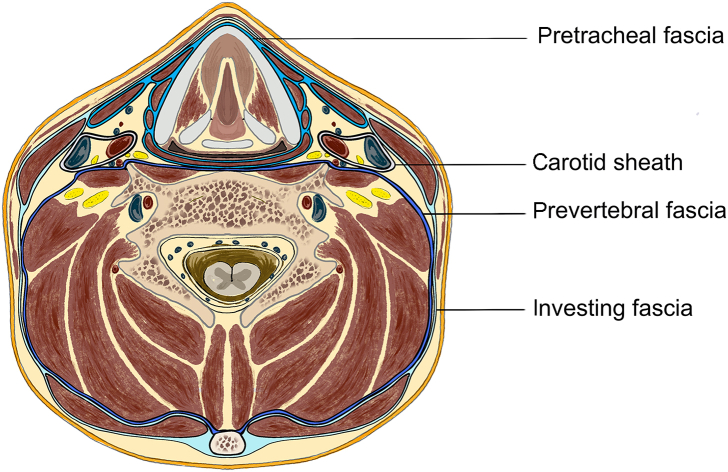
The deep cervical fascia is organised into several layers, packaging up different structures in the neck: the investing, pretracheal and prevertebral layers and the carotid sheath. The layers of the deep cervical fascia are demonstrated in Fig. 1. The most superficial layer of deep cervical fascia is the investing layer. It encircles the neck and is attached from the inferior border of the mandible, zygomatic arch, mastoid process, superior nuchal line and external occipital protuberance superiorly to the acromion and spine of scapula, clavicle and manubrium inferiorly. It completely ensheathes the sternocleidomastoid and trapezius muscles.3,4 The pretracheal, or middle, layer of deep cervical fascia extends from the skull base and hyoid bone and thyroid cartilage superiorly to the mediastinum inferiorly, where it fuses with the fibrous pericardium. It is usually described as possessing two divisions: a muscular layer and a visceral layer. The muscular layer encloses the infrahyoid (strap) muscles: sternohyoid, sternothyroid, omohyoid and thyrohyoid. The visceral layer wraps around the larynx, pharynx, trachea, oesophagus, recurrent laryngeal nerves and thyroid and parathyroid glands.3 The prevertebral layer, or deep layer of deep cervical fascia, extends from the skull base to the mediastinum and surrounds the vertebral column and associated paravertebral muscles. It also covers the scalene muscles, deep cervical muscles and parts of the sympathetic trunk. Inferolaterally, this layer encompasses the subclavian artery and vein and parts of the brachial plexus, continuing as the axillary sheath.3
Fig. 1.
Axial cross section of the neck at C5 level demonstrating the layers of deep cervical fascia. The investing fascia is the most superficial, the pretracheal fascia is divided into muscular and visceral components and the prevertebral layer is the deepest.
The carotid sheath is a distinct condensation of deep fascia containing the common carotid artery (and the internal and external carotid above its bifurcation), internal jugular vein, ansa cervicalis, vagus nerve and some deep cervical lymph nodes. It runs from the skull base above into the superior mediastinum below.
Anatomy of the cervical plexus
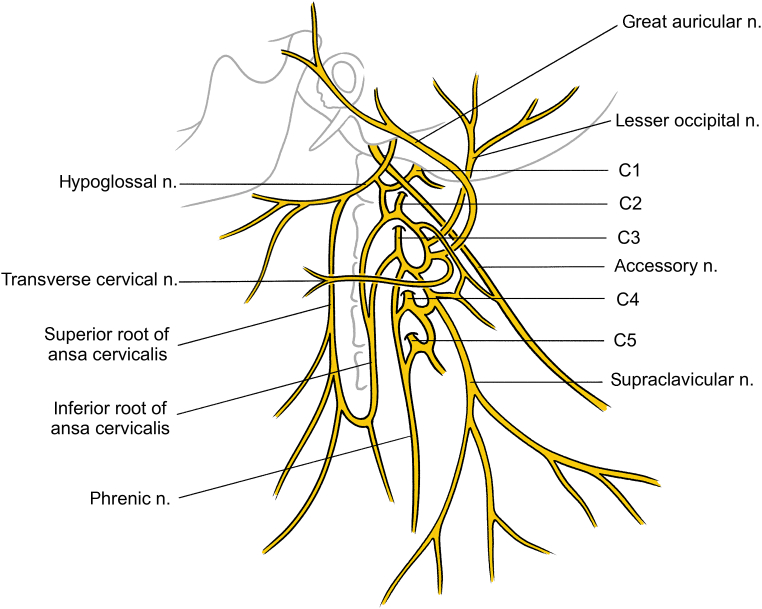
The cervical plexus comprises a superficial and deep set of branches. The superficial branches are sensory to skin, and the deep branches are mostly motor to muscles. The plexus is formed from the anterior (ventral) rami of C1–4. Each ramus receives input from the superior cervical sympathetic ganglion via a grey ramus communicans. Each of the cervical nerves (except C1) forms ascending and descending branches, which join in loops forming the plexus. The branches of the cervical plexus are demonstrated in Fig. 2.
Fig. 2.
Branches of the cervical plexus. C5 does not contribute to the cervical plexus, but it is included to demonstrate the contribution to the phrenic nerve, and the accessory nerve is included to demonstrate its association to the plexus. n., nerve.
The ventral ramus of C1 emerges above the posterior arch of atlas, then runs forward to lie anterior to the transverse process, where it receives an ascending branch from C2. The ventral (anterior) ramus of C2 emerges between the atlas and axis, runs upwards between longus colli and levator scapulae and then divides into its ascending and descending branches. The ventral ramus of C3 emerges between longus capitis and scalenus medius, and the ventral ramus of C4 passes between scalenus medius and scalenus anterior. The looping connections of the plexus lie level with the upper cervical vertebrae, deep to the sternocleidomastoid and the internal jugular vein, lateral to the transverse processes of the vertebrae and anterior to the scalenus medius and levator scapulae.
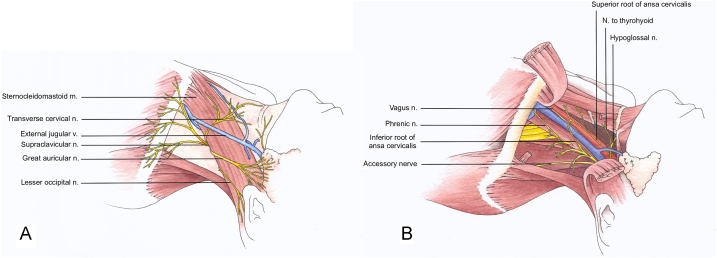
The deep branches of the cervical plexus (Fig. 3) supply most of the muscles in the neck, anterior to the vertebral column. Branches pass directly from the ventral rami of C1 to C4 to the prevertebral muscles (rectus capitis anterior, rectus capitis lateralis, longus capitis and longus colli muscles). A branch from C1 passes to the vagus nerve, and then C1 runs anteriorly to join the hypoglossal nerve, looping under the angle of the mandible. The hitchhiking C1 fibres leave the hypoglossal nerve as the nerves to thyrohyoid and geniohyoid and the superior root of the ansa cervicalis (also called the nervus descendens hypoglossi); these branches may also contain some hypoglossal fibres.5,6 The inferior root of the ansa cervicalis (nervus descendens cervicalis) derives from C2 and C3 in 75% of cases (variations include various contributions from C1 to C4 and the hypoglossal and vagus nerves).7 The two roots join to form the ansa cervicalis, looping around the internal jugular vein (ansa means ‘loop’ or ‘handle’). The ansa cervicalis provides branches to all the infrahyoid muscles except thyrohyoid. The phrenic nerve derives from C3 to C5 but mainly from C4. It forms at the lateral border of scalenus anterior then runs down on this muscle, deep to the prevertebral fascia, posterior to the sternocleidomastoid and the internal jugular vein, down through the thoracic inlet. Here, it is often joined (in some 75% of cases) by the accessory phrenic nerve, deriving from C5, and usually branching off the nerve to subclavius.7 Eventually, the phrenic nerve passes all the way down to the diaphragm—as the sole motor supply to this important muscle, on each side. Other deep branches of the cervical plexus supply the sternocleidomastoid, trapezius, levator scapulae and scalene muscles.
Fig. 3.
(A) The nerves of the superficial branches of the cervical plexus as they emerge from the posterior border of the sternocleidomastoid muscle. (B) The deep branches of the cervical plexus. The sternocleidomastoid is lifted in this illustration to allow visualisation of the deep branches of the plexus and demonstrate the close association to the hypoglossal, phrenic, vagus and spinal accessory nerves. First published in The Abbott Pocket Guide to Practical Peripheral Nerve Blockade. m., muscle; n., nerve; v., vein.
The superficial branches of the cervical plexus supply skin over the anterior and lateral regions of the neck. They are formed by the connections between C2, C3 and C4, generating four branches: the lesser occipital, great auricular, transverse cervical and supraclavicular nerves. Initially lying anterior to the middle scalene and levator scapulae and deep to the internal jugular vein, these branches pierce the investing layer of deep cervical fascia along the posterior border of the sternocleidomastoid muscle, as demonstrated in Fig. 3(A).
The lesser occipital nerve (C2) curves around the spinal accessory nerve to lie anterior to it, ascends along the posterior border of the sternocleidomastoid and close to the mastoid process, pierces the deep investing fascia to supply the upper third of the medial side of the auricle and the skin under the ear. The lesser occipital nerve is occasionally present as a branch of the greater occipital nerve (branching from the dorsal ramus of C2).7 The great auricular nerve (C2 and C3) pierces the investing deep fascia near the midpoint of the posterior border of the sternocleidomastoid and then runs superomedially on this muscle, deep to platysma. An anterior branch supplies the lateral side of the auricle, the skin over the parotid gland and the angle of the jaw; a posterior branch supplies skin of the medial aspect of the auricle. The transverse cervical nerve (C2 and C3, although occasionally C3 and C4) also pierces the investing fascia near the midpoint of the posterior border of the sternocleidomastoid then runs medially on the muscle, deep to the external jugular vein, fanning out into branches that supply the anterior neck. The supraclavicular nerve (C3 and C4) divides into three branches before piercing the investing fascia a little lower down the posterior border of the sternocleidomastoid; the medial supraclavicular nerve supplies skin over the manubrium sterni, down to the level of the second rib; the intermediate supraclavicular nerves run over the clavicle (occasionally piercing it) to supply skin over the upper part of pectoralis major; and the lateral supraclavicular nerves supply skin over the shoulder.8 The nerves originating from the branches of the superficial cervical plexus are demonstrated in Fig. 3(A).
Regional anaesthesia techniques
Superficial cervical plexus block
The superficial branches of the cervical plexus can be blocked using anatomical landmarks or using ultrasound guidance. Taking care to avoid the external jugular vein, local anaesthetic is deposited subcutaneously along the posterior border of the middle third of the sternocleidomastoid muscle to form a sausage of local anaesthetic. Ultrasound may be used to identify the veins in the neck and layers of neck fascia and guide injection superficial to the superficial cervical fascia. In experienced hands, modern ultrasound may allow branches of the plexus to be visualised, allowing selective blockade of individual nerves.
Deep cervical plexus block
The deep cervical plexus block (DCPB) was traditionally performed by landmark technique. Two approaches have been described. The posterior approach, described by Kappis in 1912, aimed to block each of the nerves as they emerged from the vertebral column.9 This technique involved needle passage through the extensor muscles of the neck; it was painful but avoided the vertebral artery and vein, which lie anterior to the plexus. Because of patient discomfort and long needle path, this technique has been superseded by the lateral approach.
In 1914, a multiple-injection lateral approach was described.10 In 1975, this approach was simplified to a single-injection approach at the level of C3 or C4.11 A modified approach to the multiple-injection block is described by the New York School of Regional Anesthesia.12 In brief, this approach involves:
(i) Skin preparation with antiseptic solution
(ii) The patient is positioned, as shown in Fig. 4, with the head turned away from the side of the block.
(iii) A line is drawn from the mastoid process to the anterior tubercle of the transverse process of C6, known as Chassaignac's tubercle (or the carotid tubercle).
(iv) Next, C2, C3 and C4 are marked along this line at 2, 4 and 6 cm from the mastoid process.
(v) Local anaesthetic is administered subcutaneously at each injection point.
(vi) A needle is inserted, angulated slightly caudad, to contact the transverse process. The needle is withdrawn 1–2 mm, and after excluding intravascular placement, 3–4 ml local anaesthetic is injected at each level.
Fig. 4.
(A) Patient positioned for cervical plexus block. Note that the head is turned away and is resting on a surface so that the sternocleidomastoid muscle is relaxed. (B) Transverse processes of C4–7 with the position of the corresponding nerve root as visualised using ultrasound.
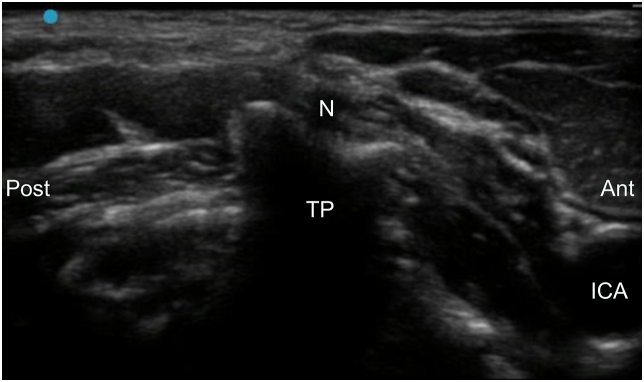
Deep cervical plexus block may be performed with ultrasound to lessen risks of complications. The patient should be positioned as described previously. A high-frequency linear probe is used to identify the transverse process of the first thoracic vertebra with corresponding rib or the distinctive appearances of the C6 or C7 transverse processes, as illustrated in Fig. 4. The ultrasound probe is translated in a caudad direction to identify the transverse process of C4. The cervical nerve should be observed in the shallow U-shaped tip of the transverse process of C4 vertebra (Fig. 5). The needle is introduced using an in-plane or out-of-plane approach to contact the transverse process at this level. Negative aspiration excludes subarachnoid or intravascular needle placement. Injection of 2–4 ml of local anaesthetic should be observed to spread around the nerve root.
Fig. 5.
Ultrasound image of the C4 transverse process demonstrating C4 nerve root at the tip of the transverse process. ant, anterior; ICA, internal carotid artery; N, nerve; post, posterior; TP, transverse process.
Intermediate cervical plexus block
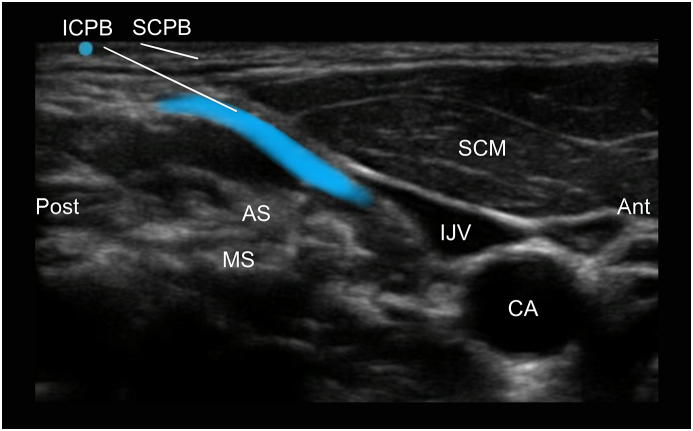
First described in 2007, ultrasound-guided intermediate cervical plexus block (ICPB) involves injection into the fascial plane between the sternocleidomastoid and prevertebral muscles at the C4 level.13,14 Anterior and posterior approaches have since been described, but the posterior approach is recommended to avoid the large vascular structures on the anterior side. First, the C4 level is identified, as described previously. The probe is then translated forward to identify the sternocleidomastoid muscle. Taking care to avoid the external jugular vein, the needle tip is advanced in-plane between the sternocleidomastoid muscle and the anterior scalene muscle. Separation of the two distinct fascial layers should be observed with correct needle placement. Fig. 6 demonstrates the ultrasonographic anatomy of superficial cervical plexus block (SCPB) and ICPB.
Fig. 6.
Ultrasound image of the anatomy relevant to the superficial (SCPB) and intermediate cervical plexus blocks (ICPB) at the C4 vertebral level. The intended spread of local anaesthetic within the ICPB plane is indicated by the blue area. Note that the external jugular vein is easily compressed by light pressure from the ultrasound probe as is not visible in this image. ant, anterior; AS, anterior scalene; CA, carotid artery; IJV, internal jugular vein; MS, middle scalene; post, posterior; SCM, sternocleidomastoid.
Complications
Complications of the SCPB are similar to those of most other peripheral nerve blocks. Local infection can be limited with strict aseptic technique and careful preparation. Haematoma formation may be observed in those with underlying coagulation abnormalities. The external jugular vein overlies the sternocleidomastoid muscle close to the point of injection; it should be identified and avoided to prevent intravascular injection and limit haematoma formation. Nerve injury may be minimised by ensuring low-pressure injections throughout and avoidance of vasoconstrictors, such as adrenaline (epinephrine) in peripheral nerve blocks.
In addition to the risks described previously, the DCPB carries the additional risks of phrenic, recurrent laryngeal, vagus and hypoglossal nerve palsies. Because of the vascular nature of the deep structures within the neck and proximity to the carotid artery and internal jugular vein, haematoma formation is more likely with the DCPB. Care must be taken to avoid subarachnoid injection by a meticulous technique, including avoiding cephalad needle direction when performing the block and a ‘negative’ aspiration before injection of local anaesthetic. Horner's syndrome is common and occurs because of blockade of the sympathetic chain in the upper cervical region.
The ICPB theoretically minimises the risks associated with deep blockade.
Communication with the surgical team and careful calculation of local anaesthetic doses are vital during surgery under regional anaesthesia. Carotid surgery may require additional top-ups around the carotid artery and along the mandible, or at the time of closing the skin if surgery has been prolonged. Care must be taken to avoid local anaesthetic toxicity.
Indications
Awake carotid endarterectomy was traditionally considered to reduce complication rates by enabling early detection of cerebral ischaemia during carotid cross-clamping. The General Anaesthesia versus Local Anaesthesia for carotid surgery trial demonstrated no difference in quality of life, length of hospital stay or incidence of stroke, myocardial infarction or death within 30 days of surgery between general and local anaesthesia.15 In 2021, 26.7% of carotid endarterectomies were performed under local or regional anaesthesia.16 The techniques and considerations for anaesthesia for carotid endarterectomy have been covered in depth previously in this journal.17
Several small studies have demonstrated that bilateral superficial or combined (superficial and deep) cervical plexus blocks reduce pain scores at rest and on swallowing, after thyroidectomy under general anaesthesia, with reduced intra- and postoperative opioid requirements.18,19 Reduction in severe postoperative nausea and vomiting has also been recorded.20 Cervical plexus block with conscious sedation has been reported for several surgeries in the neck, including thyroidectomy.21
Clavicle fractures placing tension on the overlying skin can be particularly painful, and cervical plexus block may be used as an analgesic option in the emergency department.
The clavicle and clavicular joints receive innervation from the supraclavicular, lateral pectoral and subclavian nerves, although the functional importance of each contributing nerve remains to be elucidated.22 Awake open reduction and internal fixation of the clavicle have been described using either interscalene or supraclavicular brachial plexus block combined with cervical plexus block.23, 24, 25 Cervical plexus block has been demonstrated to reduce pain scores and postoperative analgesic requirements in a variety of surgical procedures, including cervical discectomy and fusion and modified radical mastoidectomy.26,27
An important but often underused use of the SCPB is for internal jugular vein central venous catheter insertion. Compared with local anaesthetic infiltration, performance of this technique reduces the number of individual injections per insertion and reduces patient verbal pain scores, including 5 min after the procedure.28
Conclusions
The cervical plexus provides sensory innervation to the neck and upper chest wall and motor innervation to many muscles in the neck. Superficial cervical plexus block, ICPB and DCPB may be performed using anatomical landmarks, but complications may be reduced with the use of ultrasound. Cervical plexus block is clinically useful for a number of procedures in the neck: as a sole technique for awake surgery, as an adjunct to other regional techniques or general anaesthesia, to provide perioperative analgesia, or outside of the operating theatre setting.
Declaration of interest
The authors declare that they have no conflicts of interest.
Biographies
Michael JarvisBMBS BSc (Hons) FRCA is a specialty trainee in anaesthesia working at University Hospitals of North Midlands NHS Trust. His interests include regional anaesthesia and anaesthesia for vascular surgery.
Rajinikanth Sundara Rajan MD FRCA EDRA FFPMRCA is a consultant anaesthetist and pain physician at University Hospitals of North Midlands NHS Trust. His major clinical interests are regional anaesthesia and acute pain. He regularly performs regional anaesthetic techniques for vascular surgery and has several publications in regional pain techniques.
Alice Roberts BScPhD Hon FBAASc is a clinical anatomist, author, broadcaster and professor of public engagement in science atthe University of Birmingham. She authored Human Anatomy and The Complete Human Body and co-authored The Abbott Pocket Guide to Practical Peripheral Nerve Blockade.
Matrix codes: 1A01, 1D02, 2G01, 2G02, 2G03, 3A05, 3A09
MCQs
The associated MCQs (to support CME/CPD activity) will be accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
References
- 1.Natale G., Condino S., Stecco A., et al. Is the cervical fascia an anatomical proteus? Surg Radiol Anat. 2015;37:1119–1127. doi: 10.1007/s00276-015-1480-1. [DOI] [PubMed] [Google Scholar]
- 2.Kohan E.J., Wirth G.A. Anatomy of the neck. Clin Plast Surg. 2014;41:1–6. doi: 10.1016/j.cps.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 3.Warshafsky D., Goldenberg D., Kanekar S.G. Imaging anatomy of deep neck spaces. Otolaryngol Clin North Am. 2012;45:1203–1221. doi: 10.1016/j.otc.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Guidera A.K., Dawes P.J., Fong A., Stringer M.D. Head and neck fascia and compartments: no space for spaces. Head Neck. 2014;36:1058–1068. doi: 10.1002/hed.23442. [DOI] [PubMed] [Google Scholar]
- 5.Caliot P., Dumont D., Bousquet V., Midy D. A note on the anastomoses between the hypoglossal nerve and the cervical plexus. Surg Radiol Anat. 1986;8:75–79. doi: 10.1007/BF02539711. [DOI] [PubMed] [Google Scholar]
- 6.Sakamoto Y. Morphological features of the branching pattern of the hypoglossal nerve. Anat Rec (Hoboken) 2018;302:558–567. doi: 10.1002/ar.23819. [DOI] [PubMed] [Google Scholar]
- 7.Warner T., Tubbs R.S. In: Surgical Anatomy of the cervical Plexus and its branches. Tubbs R.S., Loukas M., Martinez-Pereira M.A., et al., editors. Elsevier; London: 2022. Anatomical variations of the cervical plexus; pp. 81–91. [Google Scholar]
- 8.Standring S. 42nd Edn. Elsevier; London: 2021. Gray’s anatomy: the anatomical basis of clinical practice; pp. 573–578. [Google Scholar]
- 9.Kappis H. Über Leitunganaesthesie am Bauch, Brust, Arm, und Hals durch injection aus Foramen intervertebrale. München Med Wschr. 1912;59:794–796. [Google Scholar]
- 10.Heidenhein L. In: Local Anesthesia, its scientific basis and practical use. Braun H., editor. Lea & Febiger; Philadelphia, PA: 1914. Operations on the neck; pp. 268–269. [Google Scholar]
- 11.Winnie A.P., Ramamurthy S., Durrani Z., Radonjic R. Interscalene cervical plexus block: a single-injection technique. Anesth Analg. 1975;54:370–375. doi: 10.1213/00000539-197505000-00030. [DOI] [PubMed] [Google Scholar]
- 12.Vloka JD, Smeets AS, Tsai T, Bouts C. New York School of Regional Anaesthesia (NYSORA). Cervical plexus block—landmarks and nerve stimulator technique. Available from: https://www.nysora.com/techniques/head-and-neck-blocks/cervical/cervical-plexus-block/ (accessed 17 May 2022).
- 13.Pandit J.J., Satya-Krishna R., Gration P. Superficial or deep cervical plexus block for carotid endarterectomy: a systematic review of complications. Br J Anaesth. 2007;99:159–169. doi: 10.1093/bja/aem160. [DOI] [PubMed] [Google Scholar]
- 14.Choquet O., Dadure C., Capdevila X. Ultrasound-guided deep or intermediate cervical plexus block: the target should be the posterior cervical space. Anesth Analg. 2010;111:1563–1564. doi: 10.1213/ANE.0b013e3181f1d48f. [DOI] [PubMed] [Google Scholar]
- 15.GALA trial Collaborative Group General Anaesthesia versus Local Anaesthesia for carotid surgery (GALA): a multicentre, randomised controlled trial. Lancet. 2008;372:2132–2142. doi: 10.1016/S0140-6736(08)61699-2. [DOI] [PubMed] [Google Scholar]
- 16.Waton S., Johal A., Birmpili P., et al. The Royal College of Surgeons of England; London: 2021. National vascular registry. 2021 reportAnnual report. [Google Scholar]
- 17.Ladak N., Thompson J.P. General or local anaesthesia for carotid endarterectomy? Cont Educ Anaesth Crit Care Pain. 2012;12:92–96. [Google Scholar]
- 18.Aunac S., Carlier M., Singelyn F., De Kock M. The analgesic efficacy of bilateral combined superficial and deep cervical plexus block administered before thyroid surgery under general anesthesia. Anesth Analg. 2002;95:746–750. doi: 10.1097/00000539-200209000-00039. [DOI] [PubMed] [Google Scholar]
- 19.Dieudonne N., Gomola A., Bonnichon P., Ozier Y.M. Prevention of postoperative pain after thyroid surgery: a double-blind randomized study of bilateral superficial cervical plexus blocks. Anesth Analg. 2001;92:1538–1542. doi: 10.1097/00000539-200106000-00038. [DOI] [PubMed] [Google Scholar]
- 20.Shih M.L., Duh Q.Y., Hsieh C.B., et al. Bilateral superficial cervical plexus block combined with general anesthesia administered in thyroid operations. World J Surg. 2010;34:2338–2343. doi: 10.1007/s00268-010-0698-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inabnet W.B., Shifrin A., Ahmed L., Sinha P. Safety of same day discharge in patients undergoing sutureless thyroidectomy: a comparison of local and general anesthesia. Thyroid. 2008;18:57–61. doi: 10.1089/thy.2007.0148. [DOI] [PubMed] [Google Scholar]
- 22.Leurcharusmee P., Maikong N., Kantakam P., Navic P., Mahakkanukrauh P., Tran D. Innervation of the clavicle: a cadaveric investigation. Reg Anesth Pain Med. 2021;46:1076–1079. doi: 10.1136/rapm-2021-103197. [DOI] [PubMed] [Google Scholar]
- 23.Balaban O., Dülgeroğlu T.C., Aydın T. Ultrasound-guided combined interscalene-cervical plexus block for surgical anesthesia in clavicular fractures: a retrospective observational study. Anesthesiol Res Pract. 2018;2018 doi: 10.1155/2018/7842128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Banerjee S., Acharya R., Sriramka B. Ultrasound-guided inter-scalene brachial plexus block with superficial cervical plexus block compared with general anesthesia in patients undergoing clavicular surgery: a comparative analysis. Anesth Essays Res. 2019;13:149–154. doi: 10.4103/aer.AER_185_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baran O., Kır B., Ateş İ., Şahin A., Üztürk A. Combined supraclavicular and superficial cervical plexus block for clavicle surgery. Korean J Anesthesiol. 2020;73:67–70. doi: 10.4097/kja.d.18.00296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mariappan R., Mehta J., Massicotte E., Nagappa M., Manninen P., Venkatraghavan L. Effect of superficial cervical plexus block on postoperative quality of recovery after anterior cervical discectomy and fusion: a randomized controlled trial. Can J Anaesth. 2015;62:883–890. doi: 10.1007/s12630-015-0382-3. [DOI] [PubMed] [Google Scholar]
- 27.Deepika V., Ahuja V., Thapa D., Gombar S., Gupta N. Evaluation of analgesic efficacy of superficial cervical plexus block in patients undergoing modified radical mastoidectomy: a randomised controlled trial. Indian J Anaesth. 2021;65:S115–S120. doi: 10.4103/ija.ija_339_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tikle H.A., Patil B.M. Comparison of superficial cervical plexus block versus local infiltration for pain relief during internal jugular vein cannulation. Int J Contemp Med Res. 2018;5:I6–I12. [Google Scholar]