Abstract
Acupuncture is part of a complex medical approach used in China for about 2000 years, known as Traditional Chinese Medicine, whose central assumption is that health occurs when the patterned energy flow throughout the body is balanced. Within this paradigm, acute illness occurs when a major state of imbalance or disruption arises, and the use of acupuncture may help in correcting these imbalances.
While the Chinese hospital system often offers the integration of traditional and western medicine, in Europe and the United States this combined approach is infrequently practiced. However, several investigations have consistently shown the effectiveness of acupuncture for different aspects of critical illness.
The aim of this systematic review is to increase the clinician's awareness of the current evidence regarding the use of acupuncture for the management of critically ill patients, both alone or as a complement to western medicine. The effects of acupuncture on critical illness, with a particular focus on respiratory function, pain and delirium treatment and prevention, circulatory function, nutritional support, and recovery after acute illness are explored and summarized, and evidence is provided that acupuncture is an acceptable and feasible option for the management of several aspects of critical illness. In addition, we suggest a practical selection of potentially useful acupuncture points in the critical care setting, with indications for simple localization and the correct puncture method.
Keywords: Acupuncture, Critical care, Traditional Chinese medicine, Systematic review
Graphical abstract
1. Introduction
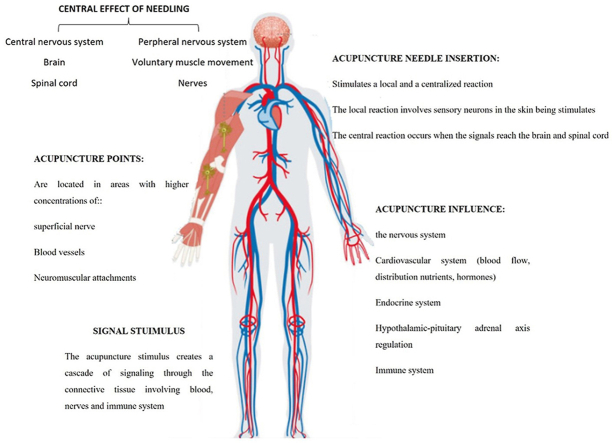
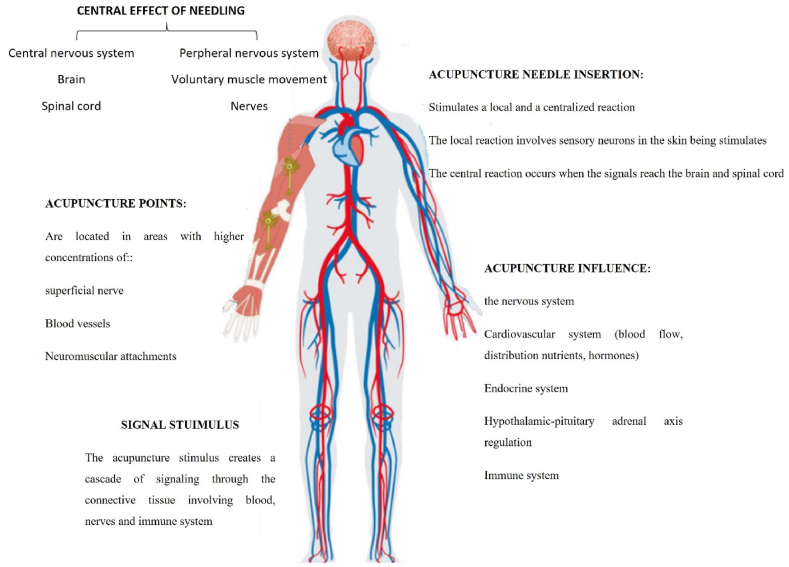
Acupuncture is part of a complex medical approach used in China since at least 2000 years ago and known as Traditional Chinese Medicine (TCM).1 TCM medical theory holds that health occurs when the patterned energy flow throughout the body is balanced.2 The central assumption in TCM is that health is achieved by maintaining the body in a ‘balanced state' and that disease results from an internal imbalance of Yin and Yang. This imbalance leads to blockage Qi (vital energy) flow along meridians. It is believed that there are 12 main meridians and 8 secondary meridians and that there are more than 400 acupuncture points on the human body that connect with them. The channel system includes blood vessels, lymphatic vessels, and nerves, and the microscopic tissue spaces or network structures throughout a living organism3 (Fig. 1). The exact mechanism by which acupuncture works is not clear. It has been suggested that acupoints are located at sites where their stimulation can affect the activity of multiple sensory neurons.4 These sites are also known as receptive fields. The physical stimulation of needle insertion at these sites may affect pain processing in the central nervous system and muscles and increase blood flow to certain parts of the body. Therefore, acute illness may be defined when a significant state of imbalance or disruption arises, and acupuncture may help correct these imbalances. While Chinese hospital system often integrates traditional and western medicine, this combined approach is infrequently practiced in Europe and the United States.5 However, several studies from peer-reviewed, indexed journals have extensively shown the effectiveness of acupuncture in different kinds of critical and non-critical illnesses, and acupuncture was repeatedly shown to be more effective than a placebo. Acupuncture is used to treat knee pain and gastroesophageal reflux and has proved effective for patients with low back pain, headache, and depression.6 Moreover, acupuncture is safe and potentially effective in treating bronchial asthma and chronic obstructive pulmonary disease.7 In addition, it improves the respiratory status and promotes successful weaning from prolonged mechanical ventilation in intensive care unit (ICU) patients.8 The use of adjunctive acupuncture has been shown to reduce pain, nausea, and vomiting and decrease the need for narcotic use in the perioperative and in the intensive care setting.9, 10, 11 Furthermore, its use demonstrated a significant reduction in the incidence of postoperative opioid-related adverse effects, including nausea, pruritus, dizziness, sedation, and urinary retention, as well as an effective treatment for delayed gastric emptying.12 The extent to which TCM is used among ICU patients is less investigated. This systematic review aims to explore and summarize the effects of acupuncture on critical illness. We focused on its effectiveness on respiratory function, pain and delirium treatment and prevention, circulatory function, nutritional support, and recovery after acute illness.
Fig. 1.
Whole-body effects of acupuncture.
The figure depicts the main effects on central and peripheral nervous system, the effects of acupoint stimulation and needling insertions, the signal stimulus and its influence on cardiovascular, endocrine, and immune systems.
2. Methods
This review adheres to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for the identification, screening, and inclusion of relevant articles. The PICO (Patient/Intervention/Comparison/Outcome) model was used as the strategy for formulating the research question. The review protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO, CRD42022321901).
2.1. Study population
We conducted a systematic review of published randomized, controlled studies of critically ill, adult patients in a medical or surgical ICU, treated with acupuncture.
2.2. Intervention
All studies in which an acupuncture intervention was administered to critically ill patients with the aim of supporting respiratory and circulatory function, treating or preventing pain and delirium, improving nutritional support and recovery after acute illness were included in the present review.
2.3. Comparator
Our comparators were the group of patients in the studies included who did not receive the intervention.
2.4. Study identification
A comprehensive bibliographic search strategy was developed. The search accessed PubMed, from inception to the cutoff date of March 30th, 2022. We restricted our search to publications in English. To supplement our search, we also manually screened the reference list of every paper to identify additional potentially eligible studies.
2.5. Search strategy
The following key-words were used, alone or combined with appropriate boolean operators, to search the different databases: acupuncture, “traditional Chinese medicine”, “intensive care unit”, “non-pharmacological interventions”, “critical care” “critically ill patients”, “critical illness”, “respiratory function”, “circulatory function” shock, pain, delirium, “nutritional support”, recovery. A similar search was also performed using the PubMed MeSH thesaurus. The detailed retrieval strategy for PubMed is reported in Table 1.
Table 1.
Detailed retrieval strategy for Pubmed.
| Query | Search term |
|---|---|
| #1 | Acupuncture [mesh] |
| #2 | Acupuncture [Title/Abstract] OR pharmacoacupuncture[Title/Abstract] OR acupotomy[Title/Abstract] OR acupressure[Title/Abstract] OR pharmacopuncture[Title/Abstract] OR needle[Title/Abstract] OR needling[Title/Abstract] OR dry-needling[Title/Abstract] OR body-acupuncture[Title/Abstract] OR electroacupuncture[Title/Abstract] OR electro-acupuncture[Title/Abstract] |
| #3 | Traditional chinese medicine [mesh] |
| #4 | #1 OR #2 OR #3 |
| #5 | "intensive care unit∗" [Title/Abstract] OR "Critical care" [Title/Abstract] OR "Critically ill patient∗" [Title/Abstract] OR "critical illness" [Title/Abstract] |
| #6 | #4 AND #5 |
| #7 | Respiratory function[Mesh] |
| #8 | Circulatory function [Mesh] |
| #9 | Nutritional support [Mesh] |
| #10 | Pain [Mesh] |
| #11 | Delirium [Mesh] |
| #12 | Recovery [Mesh] |
| #13 | Respiratory function∗[Title/Abstract] OR Circulatory function∗ [Title/Abstract] OR Shock∗ [Title/Abstract] OR pain∗ [Title/Abstract] OR delirium∗ [Title/Abstract] OR nutrition∗ [Title/Abstract] OR recovery∗ [Title/Abstract] |
| #14 | #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 |
| #15 | adult[mh] |
| #16 | English [la] |
| #17 | #15 AND #16 |
| #18 | Case Reports [pt] OR Clinical study [pt] OR Clinical trial [pt] OR Controlled Clinical Trial [pt] OR Observational Study [pt] OR Randomized Controlled Trial [pt] |
| #19 | Case report [Title/Abstract] OR Case series [Title/Abstract] OR randomized controlled trial [Title/Abstract] OR case-control [Title/Abstract] OR Observational∗ [Title/Abstract] |
| #20 | #18 OR #19 |
| #21 | #6 AND #14 AND #17 AND #20 |
2.6. Study selection and quality assessment
Two authors independently screened the studies selected from the search strategy to identify potentially eligible studies. Studies considered to be potentially eligible then underwent full-text review. In case of disagreement the authors reviewed the article in question together until they reached a consensus. The Physiotherapy Evidence Database (PEDro) scale was used to assess the methodological quality of the studies included.
Types of study to be included.
The following inclusion criteria will be used to select the eligible studies:
-
1.
Case series, retrospective or prospective observational cohort studies;
-
2.
Randomized controlled studies;
-
3.
Case reports;
-
4.
Studies concerning acupuncture in critically ill adult patients, i.e. hospitalized in ICU or invasively ventilated;
-
5.
Studies in the English language.
Exclusion criteria:
-
1.
Studies on children;
-
2.
Studies not reporting relevant data;
-
3.
Systematic reviews and meta-analyses
-
4.
Articles lacking a full text.
2.7. Data extraction and synthesis
Two authors independently extracted data from all the included studies. A specific data sheet was created to record the following information: author, year, design of the study, inclusion and exclusion criteria, population, intervention, outcomes, potential sources of bias, adverse effects of the intervention.
3. Findings
3.1. Literature screening
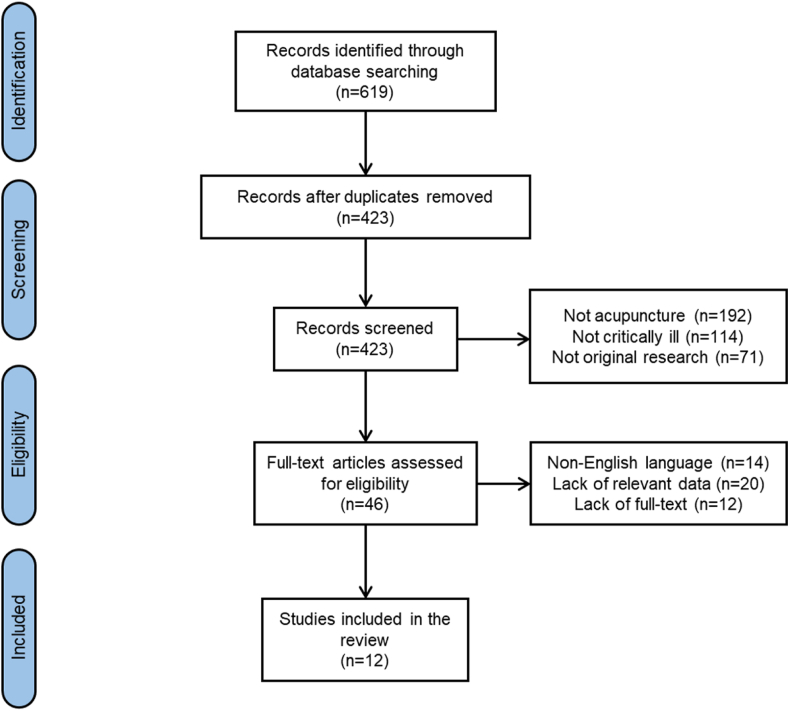
The literature search yielded 619 citations, of which 196 duplicates were removed. After screening the title and abstract, 423 citations were excluded and the remaining 46 eligible studies were further evaluated through full-text reading. After independent screening and full-text review, 12 studies were eventually identified: two case-control and one observational studies, one case report, eight randomized-controlled studies, for a total of 682 patients. Fig. 2 shows the literature screening flowchart.
Fig. 2.
Literature screening flowchart.
3.2. Methodological quality
According to the PEDro scale, only 5 studies (41.6%) presented an excellent level of methodological quality, 3 studies (25%) presented a good quality, 3 studies (25%) had a fair quality while one (8.4%) had a low level of methodological quality. Lack of blinded therapist (10/12 studies) of blind assessors (9/12 studies), and of blinded participants (7/12 studies) were the main limitations of the included studies. Table 3 shows the quality assessment of the included studies using the PEDro scale.
Table 3.
– Quality assessment of the included studies using the PEDro scale.
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Matsumoto-Miyazaki, 2018 | ✓ | x | x | x | x | x | x | ✓ | x | ✓ | ✓ | 4 | Fair |
| Yuan, 2021 | ✓ | ✓ | ✓ | ✓ | x | x | x | ✓ | x | ✓ | ✓ | 7 | Good |
| Suzuki, 2012 | ✓ | ✓ | ✓ | ✓ | ✓ | x | ✓ | ✓ | ✓ | ✓ | ✓ | 10 | Excellent |
| Tsay, 2005 | ✓ | ✓ | ✓ | ✓ | x | x | x | ✓ | ✓ | ✓ | ✓ | 8 | Good |
| Maa, 2013 | ✓ | ✓ | ✓ | ✓ | ✓ | x | x | ✓ | ✓ | ✓ | ✓ | 9 | Excellent |
| AminiSaman, 2018 | ✓ | ✓ | x | ✓ | ✓ | ✓ | ✓ | x | ✓ | ✓ | ✓ | 9 | Excellent |
| Zheng, 2012 | ✓ | ✓ | ✓ | ✓ | ✓ | x | x | ✓ | ✓ | ✓ | ✓ | 9 | Excellent |
| Matsumoto-Miyazaki, 2017 | ✓ | ✓ | x | x | x | x | x | ✓ | x | ✓ | ✓ | 5 | Fair |
| Hsu, 2006 | ✓ | x | x | x | x | x | x | x | x | x | ✓ | 2 | Low |
| Pfab, 2011 | ✓ | ✓ | ✓ | ✓ | x | x | x | ✓ | ✓ | ✓ | ✓ | 8 | Good |
| Kao, 2017 | ✓ | ✓ | x | ✓ | x | x | x | ✓ | x | ✓ | ✓ | 6 | Fair |
| Ben-arie, 2019 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 11 | Excellent |
1: eligibility criteria and source of participants; 2: random allocation; 3: concealed allocation; 4: baseline comparability; 5: blinded participants; 6: blinded therapists; 7: blind assessors; 8: adequate follow-up; 9: intention-to-treat analysis; 10: between-group comparisons; 11: point estimates and variability.
3.3. Characteristics of the included studies
In this systematic review, 12 studies published from 2005 to 2021 were included. The interventions applied to the experimental groups were acupuncture alone or in combination with conventional therapy, while those administered to the control groups were conventional treatment or sham acupuncture. Table 2 summarizes relevant studies regarding acupuncture in a critical care setting. We chose not to perform a formal meta-analysis of the finding of the studies included, as they differed widely in terms of the features of the acupuncture intervention, the time during the course of ICU stay in which it was administered, its duration, as did the outcomes considered and the tools used to assess the effects. Indeed, the lack of a meta-analytic approach is also the main limitation of the current review, which can impact the validity of the findings. Most of the studies included in the final review were performed in mechanically ventilated patients, and were focused not only on respiratory function, but also on the treatment of anxiety and pain, circulatory shock, and nutritional support. Most of the RCT investigated the effects of acupuncture as compared with traditional treatment, few of them used sham acupuncture as control, only one paper compared the effects of electroacupuncture. The detailed description of these results will be discussed below.
Table 2.
- Relevant studies regarding acupuncture in the critical care setting.
| Author | Design | Setting of the study | Main remarks |
|---|---|---|---|
| Matsumoto-Miyazaki et al.7 | Observational. 16 ventilated ICU patients | Tidal volume (VT), respiratory rate, heart rate, oxygen saturation (SpO2), dynamic lung compliance (Cdyn), rapid shallow breath index values before and immediately after acupuncture were extracted from the medical records. | VT and Cdyn were significantly increased immediately after acupuncture. In the weaning success group, VT and Cdyn were significantly increased. The increase in Cdyn after acupuncture was larger in the weaning success than in the weaning failure group. |
| Cheng yuan et al.11 | RCT. 188 ventilated, elderly ICU patients | Two groups; the observation group was treated with acupuncture at Neiguan (PC 6), Hegu (LI 4), Yintang (GV 29) and Baihui (GV 20), twice a day until the mechanical ventilation was offline. | Acupuncture has analgesic and sedative effect in elderly patients with severe pneumonia during invasive mechanical ventilation, which could reduce the dosage of sedative and analgesic drugs and the occurrence of complications, improve blood oxygen. It showed good safety. |
| Suzuki et al.13 | RCT. 68 COPD patients | Randomized, controlled study of traditional acupuncture (n = 34) or placebo needling (n = 34); outcome: improvement of dyspnea in COPD patients receiving standard medication. | Borg scale score after a 6-min walk test was significantly higher in the real acupuncture group compared with the placebo needling group |
| COPD patients who received real acupuncture experienced improvement in the 6-min walk distance during exercise, indicating better exercise tolerance and reduced dyspnea | |||
| Tsay et al.14 | RCT. 52 COPD, ventilated ICU patients | Effects of acupressure on dyspnea, anxiety and physiological indicators of distress (heart and respiratory rate) in COPD patients undergoing mechanical ventilation support, randomized to acupressure vs. control. | Dyspnea, anxiety and physiological indicators in the acupressure group improved over time when compared with those of the comparison group |
| Maa et al.15 | RCT. 94 ventilated, comatose ICU patients | Randomized investigation (standard care with adjunctive acupressure for one or two days and standard care alone) of the effects of acupressure on weaning indices in stable coma patients receiving mechanical ventilation. | Statistically significant improvement in tidal volume and indices of rapid shallow breathing in the one-day and two-day adjunctive acupressure study arms compared to the standard care arm immediately after acupressure and persisting until 2 h |
| 10' of bilateral stimulation at five acupoints was administered per treatment session. | |||
| AminiSaman et al.16 | RCT. 50 ventilated ICU patients | Randomized double-blind clinical trial (Intervention: TENS electrodes placed on Hegu and Zusanli; control group). Pain was measured using the Critical Care Pain Observation Tool, and dosages of narcotics and sedation intake were recorded. | Pain level decreased in the intervention in comparison with the control group. The amount of analgesic and sedative drugs used was lower in the intervention group. |
| Zheng et al.17 | RCT. 45 ventilated ICU patients | Randomized double-blind clinical trial (group A no additional treatment; group B acupuncture without electrical stimulation at GV24 and EX–HN3 for 6 h; group C electroacupuncture to the same points as in group B). All patients were sedated with midazolam with a BIS-targeted protocol (BIS 60–80). | The hourly mean dose of midazolam within the first 6 h after sedation in group C was significantly lower than both group A and B. The doses in groups A and B showed no significant difference. Between-group comparison analysis of hepatic and renal function and severe adverse reactions all showed no significant difference between the three groups. |
| Matsumoto-Miyazaki18 | Case-control: 30 ventilated ICU patients vs. 29 historical controls | Combination therapy: acupuncture and traditional herbal medicine (Kamikihito) for reducing the incidence of delirium in patients with cardiovascular disease. Acupuncture points were GV20, Ex-HN3, HT7, LI4, LR3, and KI3. | The incidence of delirium was significantly lower in the treatment group than in the control period. Sedative drugs and non-pharmacological approaches against aggressive behavior of patients who were delirious were used less in the treatment than in the control period. |
| Hsu et al.19 | Case report | Emergency acupuncture to resuscitate patients during cardiac arrest. Acupuncture points: DU-26 on the face, bilateral LI-, PC6 and Shixuan on both hands, bilateral ST36 on both lower legs, and REN22 on the suprasternal notch area. |
Ten minutes after acupuncture, ROSC occurred. |
| Pfab et el.20 | RCT. 30 ventilated neurosurgical patients | Acupoint stimulation group (ASG; bilateral transcutaneous electrical stimulation at PC6) vs. conventional promotility drug treatment group (DTG, metoclopramide, cisapride, erythromycin). | After 5 days, 80% ASG patients group successfully developed feeding tolerance versus 60% in the DTG group. On day 1, the mean feeding balance was higher in the ASG than in the DTG group. Overall, the feeding balance improved significantly on all days of treatment in comparison with the DTG group. |
| Ben-Arie E et al.21 | RCT. 28 Post-Operative Oral and Hypopharyngeal Cancer Patients | Single-blind randomized control trial. In addition to routine ICU treatments, daily bilateral acupuncture on ST36, ST37, ST39, PC6, and LI4 for 3 days | Intervention group reached 70% and 80% of target energy intake significantly earlier than the control group, as well as higher total calorie intake within the first postoperative week and a reduced need for prokinetic drugs |
| Kao ML et al.22 | Case-control. 16 neurosurgical ventilated ICU patients | Prospective case-control pilot study. Electroacupuncture combined with prokinetics (bilateral electrical stimulation on PC6, TE8, ST36 and SP3. ST37 and ST39 were needled without electrical stimulation. | Gastric residual volume in patients treated with electroacupuncture combined with intravenous metoclopramide reduced gradually until day four and was <200 ml per day on the fifth day. |
ICU: Intensive care unit; COPD: Chronic obstructive lung disease; PONV: Postoperative nausea and vomiting; QoL: Quality of life; RCT: randomized, controlled trial.
4. Discussion
-
1.
Acupuncture and respiratory function in critically ill patients
Patients with acute respiratory failure in critical care settings often require mechanical ventilation (MV) and may present difficulties in the weaning process.23 Establishing strategies for promoting successful weaning from MV and improving the respiratory status is essential in managing ICU patients, as prolonged MV involves risks of several ventilator-associated events, ICU-acquired weakness, and ventilator-associated pneumonia, which are all closely associated with increased morbidity and mortality.24
Acupuncture treatment and acupuncture-point stimulation therapy have been reported to improve respiratory status in chronic obstructive pulmonary disease.13, 14, 25 These effects seem to be clinically associated with a reduction in dyspnea, increased respiratory muscle strength functional respiratory indices, improved chest wall mobility, and increased b-endorphin levels. Indeed, few papers explored the effects of acupuncture in mechanically ventilated, critically ill patients in the ICU. Some authors explored the acupressure (which is the massage of acupuncture points performed with the fingertip or knuckle) effects on dyspnea and respiratory rate, and some reported improving the indices related to weaning (i.e. tidal volume and rapid shallow breath index) in patients receiving MV.15,26 Matsumoto-Miyazaki and coworkers investigated the effects of acupuncture for improving the respiratory status in ICU patients receiving prolonged MV through a retrospective chart review.8 The authors showed how tidal volume and dynamic respiratory system compliance were significantly increased immediately after acupuncture, whereas respiratory rate, heart rate and rapid shallow breathing index were significantly decreased; moreover, the increase in dynamic compliance was greater in the weaning success group than in the weaning failure group. Two studies compared the effect of acupuncture associated with conventional therapy in the treatment of pneumonia. One study showed that acupuncture plus the classic herbal formula Da Cheng Qi decoction (Da Huang 12 g, Mang Xiao 8 g, Hou Pu 24 g, Zhi Shi 5 g) were effective for improving clinical symptom scores, shortening mechanical ventilation times, and reducing antibiotic use. Patients were randomly divided into an acupuncture treatment group and a control group. In this investigation, ST36 (Zusanli) was selected bilaterally for the treatment group patients. The needles were manipulated with the Ping Bu Ping Xie (mild tonifying and attenuating) technique. Another study showed how administering conventional drug therapy with acupuncture and herbs increases the rate of favourable patient outcomes.27 The treatment group received acupuncture at CV10 (Xiawan), ST25 (Tianshu), RN4 (Guanyuan), ST36 (Zusanli). The investigation found that patients receiving acupuncture plus drug therapy scored significantly better than patients in the drug monotherapy control group.
In summary, addition of acupuncture to standard therapy seems beneficial at least in the short-term of acute disease and during the weaning phase; additional controlled trials with no or sham acupuncture groups should still be conducted to investigate the incidence of ventilator-associated events, including ICU-acquired weakness, ventilator-associated pneumonia, and mortality.
-
2.
Acupuncture and pain/sedation in the critically ill
Current approaches to pain management include pharmacological agents and nonpharmacological agents. Among these, the application of electrical current through electrodes placed on the skin for pain control is effective.16 On the other hand, transcutaneous electrical acupoint stimulation (TEAS) has been suggested to improve the acupuncture stimulation effects.28 Acupuncture effectively reduces anxiety as well as acute, procedural, post-operative and chronic pain9. Different mechanisms have been advocated to explain the apparent analgesic effects of acupuncture, such as the gate control theory, the central endorphin activation, the supraspinal serotonergic and noradrenergic descending projection systems, and opioid neurotransmitters increases.29 It has been showed how TEAS lowers the intraoperative consumption of anesthetics and general anesthesia–related side effects,30 reduces low back pain31 and may prove effective in reducing abdominal pain.17 With specific regard to patients undergoing MV, Zheng et al.32 showed how electroacupuncture can reduce the midazolam dosage required for the sedation of critically ill patients, while Feeny et al.33 reported a benefit from acupuncture on pain and anxiety with a significant decrease in morphine use after treatment. A recent randomized, double-blind, clinical trial showed the effects of TEAS on the acupoints of pain in patients undergoing MV. The pain level in patients decreased in the intervention compared to the sham group, and the amount of analgesic and sedation drugs used was significantly lower in the intervention than in the sham group.28 A scoping review showed a reduction in pain intensity among general ICU patients from pretreatment to the last post-treatment time-point with acupuncture.34
Delirium is a common and severe problem in the ICU since its occurrence is strongly associated with mortality, length of stay and organ dysfunction.35 Although there is no definitive mechanism for delirium insurgency, inflammation, neurotransmitter, chronic stress, metabolic disorders, electrolyte disorders, and sleep-wake disturbance have all been suggested as cofactors.36 Although nonpharmacological strategies for delirium treatment and prevention has failed so far to provide sufficient evidence to support their routine use, acupuncture has been reported as an alternative intervention for preventing delirium.37 A recent study showed a shorter time-to-first remission of delirium in the acupuncture vs. the standard care arm among hospitalized patients, as well as a significantly higher number of delirium-free days in the acupuncture arm.18 In a study in the ICU setting which evaluated the use of once-daily acupuncture treatment, associated to the administration of a TCM herbal formula administered orally three times a day during the first week of the ICU stay, the incidence rates of delirium, assessed using the confusion assessment method for ICU, in the treatment and control period were significantly lower in the treatment group than in the control group.38 In summary, acupuncture seems an effective part of a non-pharmacological strategy to manage agitation, pain and delirium in the ICU.
-
3.
Acupuncture and circulatory shock
Even if shock resuscitation and critical care medicine are continuously updating with complementary approaches, no one has yet suggested acupuncture as a standard of care for cardiocirculatory failure.39 Indeed, some recent pieces of evidence suggest that hypertension and other chronic cardiovascular diseases can be improved by treatment with acupuncture. However, few studies of acupuncture efficacy have been based on the results of animal experiments with anesthesia. Li et al. showed how the stimulation of the median nerve to mimic electroacupuncture diminishes regional myocardial ischemia triggered by a sympathetically mediated increase in cardiac oxygen demand.19 This (and other studies) indicates that acupuncture works through physiological interactions with the autonomic nervous system, but how emergency acupuncture stimulation may benefit shock resuscitation still remains unclear. The initial results of a case report in which the authors hypothesized that LR3 (Taichong) stimulation would affect hemodynamics in the peripheral arteries and ST36 (Zusanli) stimulation would affect macrocirculatory parameters suggest possible beneficial effects of emergency acupuncture stimulation for shock resuscitation.40
The clinical management of sepsis aims to reduce inflammation and support organ dysfunction using different pharmacological and non-pharmacological approaches. Few studies suggested acupuncture as a promising alternative for its clinical anti-inflammatory effects.41 Its potential mechanisms of action might include reducing oxidative stress and inflammation, improving microcirculatory disturbance, and maintaining the immune balance mediated by dopamine.42 Experimental studies showed how the electrical stimulation of ST36 (Zusanli) upregulated the function of natural killer cells and macrophages,43, 44, 45, 46 increased lymphocyte number and T-cells function.47 To summarize these results, the effects of acupuncture on immunity might benefit the prevention of sepsis.
The most noteworthy aspect of acupuncture is a bidirectional regulation effect on the body's homeostasis.48 Clinical reports suggest that the effect of adding acupuncture intervention in conjunction with conventional treatment seems to be superior to the conventional treatment group alone. For instance, in a prospective randomized controlled trial, 60 patients with sepsis were randomly assigned to a standard care control group or to an intervention group receiving electroacupuncture at bilateral ST36 (Zusanli) and RN4 (Guanyuan) in addition to routine treatment.49 The authors showed a reduction in sepsis scores and increased lymphocyte count, however without differences in mortality. Similarly, another randomized controlled trial in 50 patients treated by daily electrical stimulation of ST36 (Zusanli) showed a significant reduction in sepsis severity scores and interleukin concentrations at day seven.50 For more conclusive results, we are waiting for the results of a systematic review planned in 2019 with the aim to assess the efficacy and safety of acupuncture as a complementary therapy for sepsis.41
-
4.
Acupuncture and nutritional support in critical illness
Acupuncture is only one of the cardines of TCM, which also includes a nutritional approach very different as compared to Western medicine, as its primary goal is to use food to achieve balance and harmony within the body. Early enteral nutrition remains the preferred way of feeding in a critical care setting to reduce the catabolic state induced by severe illness.51 This approach could be complicated by delayed gastric emptying due to several factors. This is a relatively common condition, involving up to almost half of mechanically-ventilated, critically-ill patients.52 Few studies suggested how acupuncture might modulate important components involved in the pathogenesis of delayed gastric emptying, such as relaxation of the lower esophageal sphincter and gastric myoelectrical activity, both related to autonomic nervous system activity. For instance, in a healthy subject, Zou et al. showed how electrical acupoint stimulation (EAS) at PC6 (Neiguan) inhibits the frequency of transient lower esophageal sphincter relaxations.53 Similarly, Chang et al. reported how EAS of acupuncture points might improve gastric myoelectrical regularity.54 Consistently, experimental animal studies showed modulating acupuncture stimulation effects on gastric motility.55,56 These effects may be mediated via vagal innervations, which are in turn modulated by higher cortical and subcortical circuitries. The latter have been postulated to be a possible cause of delayed gastric emptying in critically-ill, mechanically-ventilated patients.57 Curiously, this effect can be activated specifically by stimulation of PC6 (Neiguan).58 This point became well known in Western medicine as its stimulation has proven highly effective not only in the treatment but also in the prevention of Postoperative Nausea and Vomiting (PONV) in the anesthetic setting.11,20 Despite these observations, much less is known regarding acupuncture effects on delayed gastric emptying in the ICU setting. A recent study by Pfab et al. introduced a new protocol which was shown to be effective in treating delayed gastric emptying in critically ill patients.22 The authors showed that bilateral transcutaneous electrical acupoint stimulation at PC6 (Neiguan) increased gastric emptying as compared with conventional promotility drug treatment. Electroacupuncture combined with prokinetic drugs has also proved an effective treatment for improvement of gastric emptying in adult critically ill neurosurgical patients. Gastric residual volume in patients treated with electroacupuncture combined with intravenous metoclopramide reduced gradually until day four after treatment and was less than 200 ml per day on the fifth day. The authors provided electrical stimulation bilaterally on PC6 (Neiguan), TE8 (Sanyanglou), ST36 (Zusanli) and SP3 (Taibai). In addition, ST37 (Shangjuxu) and ST39 (Xiajuxu) were also needled without electrical stimulation.21 Acupuncture reduced postoperative feeding intolerance in critically ill postoperative oral and hypopharyngeal cancer patients in a double-blind, randomized control trial: patients in the treatment group underwent daily bilateral acupuncture on the acupoints ST36 (Zusanli), ST37 (Shangjuxu), ST39 (Xiajuxu), PC6 (Neiguan), and LI4 (Hegu) for the first three postoperative days, on top of routine ICU treatments. The intervention group reached 80% of target energy intake significantly earlier than the control group, and this was associated to a higher total calorie intake within the first postoperative week. Furthermore, the intervention group needed fewer prokinetic drugs.59,60
-
5.
Acupuncture and functional recovery after critical illness
A new pathological entity related to patients recovering from critical illness recovered has recently been defined as Intensive Care Unit Acquired Weakness (ICUAW).61 This includes critical illness myopathy and polyneuropathy, or a mixture of both (where myopathy is typically predominant). This condition is very common in patients who were previously mechanically ventilated (with a prevalence of 25–60% in those undergoing MV for >7 days),62 and can be investigated at bed side.63 Despite the relevance, no specific treatments have yet been found, and efforts should be put to prevent its appearance. From this perspective, acupuncture therapy has already effectively shown to increase nerve function and restore muscle atrophy and muscle mass.64, 65, 66 A recent study found that acupuncture counteracts skeletal muscle atrophy by increasing IGF-1 levels and stimulating muscle regeneration.65 Acupoints such as LI15 (Jianyu), LI11 (Quchi), ST36 (Zusanli), GB34 (Yanglingquan), and ST31 (Biguan) has been suggested. These promising, preliminary findings will be enriched and complemented by the results from a single-blinded, randomized, sham-procedure-controlled clinical trial with a 3-month follow-up to assess the efficacy of acupuncture combined with rehabilitation training in patients with ICUAW.67
4.1. Practical suggestions
We finally summarized practical suggestions for using a selection of potentially useful acupuncture points in the critical care setting including indications for simple localization and the correct puncture method (Table 4).
Table 4.
– Practical suggestions: name, location and needling of the main acupoints useful in the critical care setting.
| Name | Location | Needling | Therapeutic applications | |
|---|---|---|---|---|
| PC6 (Neiguan) | On the flexor aspect of the forearm between the tendons of the palmaris longus and the flexor carpi radialis two cun proximal to the wrist joint. |  |
Perpendicular insertion 0.5 to 1 cun. Caution: the median nerve lies directly under this point and needling commonly induces a significant electric sensation. This symptom is an acceptable manifestation of correct needling, but further manipulation is inappropriate and may damage the nerve. | PC6 stimulation significantly reduced the incidence of nausea, vomiting and the need for rescue. There was no difference between PC6 acupoint stimulation and antiemetic drugs in the incidence of PONV. The combination of PC6 stimulation and antiemetic therapy reduced the incidence of PONV. PC6 stimulation reduced postoperative feeding intolerance in oral and hypopharyngeal cancer patients. Electrostimulation of PC6, combined with prokinetics drugs, is an effective treatment for gastric emptying in adult critically ill neurosurgical patients. |
| ST36 (Zusanli) | Below the knee, three cun inferior to the lateral hollow formed when the knee is flexed, one finger-breadth lateral to the anterior crest of the tibia. |  |
Perpendicular insertion 1 to 1.5 cun | Tidal volume and dynamic respiratory system compliance are significantly increased immediately after ST36 stimulation, whereas respiratory rate, heart rate and rapid shallow breathing index were significantly decreased. In the treatment of pneumonia, ST36 stimulation, alone and in combination with traditional fitoterapic drugs, is effective for improving clinical symptom scores, shortening mechanical ventilation times, and reducing antibiotic use. In the treatment of sepsis, electrical stimulation of ST36 upregulated the function of natural killer cells and macrophages, increased lymphocytes number and function of T cells. Daily electrical stimulation of ST36 showed a significant reduction in sepsis gravity scores and interleukin concentrations after seven days. Electrostimulation of ST36, combined with prokinetics drugs, is an effective treatment for gastric emptying in adult critically ill neurosurgical patients. ST36 stimulation reduced postoperative feeding intolerance in oral and hypopharyngeal cancer patients. ST36, alone and in combination with other acupoints, could counteract skeletal muscle atrophy by increasing IGF-1 levels and stimulating muscle regeneration that opens some possibility to use acupuncture combined with rehabilitation training in patients with ICUAW. |
| LI4 (Hegu) | On the dorsum of the hand, between the first and second metacarpal bones, at the midpoint of the second metacarpal bone. |  |
Perpendicular insertion 0.5 to 1 cun | LI4, alone and in combination with other acupoints, reduced the incidence rate of delirium with minor needing of sedative drugs and non-pharmacological approaches against aggressive behavior of delirious patients. LI4 stimulation reduced postoperative feeding intolerance in oral and hypopharyngeal cancer patients. |
| LR3 (Taichong) | On the dorsum of the foot, in the hollow distal to the junction of the first and the second metatarsal bones. |  |
Perpendicular insertion 0.5 to 1.5 cun | LR3 stimulation affected hemodynamics in the peripheral arteries. LR3, alone and in combination with other acupoints, reduces the incidence rate of delirium with minor needing of sedative drugs and non-pharmacological approaches against aggressive behavior of delirious patients. |
| GB34 (Guanyuan) | Below the lateral aspect of the knee, in the depression found approximately one cun anterior and inferior to the head of the fibula |  |
Perpendicular or slightly oblique posterior insertion 1 to 1.5 cun | GB34, alone and in combination with other acupoints, could counteract skeletal muscle atrophy by increasing IGF-1 levels and stimulating muscle regeneration that opens some possibility to use acupuncture combined with rehabilitation training in patients with ICUAW. |
| CV4 (Guan Yuan) | On the midline of the lower abdomen, three cun inferior to the umbilicus and two cun superior to the pubic symphysis. |  |
Perpendicular insertion 0.5 to 1 cun or oblique insertion directed inferiorly 1 to 1.5 cun. | In the treatment of pneumonia, RN4 stimulation, alone and in combination with traditional fitoterapic drugs, is effective for improving clinical symptom scores, shortening mechanical ventilation times, and reducing antibiotic use. |
| Caution: deep insertion may penetrate a full bladder which should therefore be emptied before treatment. | ||||
The cun is a traditional Chinese unit of length. Its traditional measure is the width of a person's thumb at the knuckle, whereas the width of the two patient's forefingers denotes 1.5 cun, and the width of all subject's fingers side-by-side is three cun.
5. Conclusions
This systematic review shows that acupuncture therapy in the ICU is an acceptable and feasible treatment modality for the management of several aspects of critical illness. A relatively high patient acceptance rate of acupuncture when offered may be considered for clinical trial purposes in the ICU. Further randomized controlled studies are warranted to investigate the efficacy of acupuncture therapy as an adjunct to standard care in critically ill patients.
Funding statement
This work was not supported by any grant
Declaration of competing interest
No author has to disclose any potential conflict of interest.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
References
- 1.Lu A.-P., Jia H.-W., Xiao C., Lu Q.-P. Theory of traditional Chinese medicine and therapeutic method of diseases. World J Gastroenterol : WJG. 2004;10:1854. doi: 10.3748/wjg.v10.i13.1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu A., Jiang M., Zhang C., Chan K. An integrative approach of linking traditional Chinese medicine pattern classification and biomedicine diagnosis. J Ethnopharmacol. 2012;141:549–556. doi: 10.1016/j.jep.2011.08.045. [DOI] [PubMed] [Google Scholar]
- 3.Xutian S., Zhang J., Louise W. New exploration and understanding of traditional Chinese medicine. Am J Chin Med. 2009;37:411–426. doi: 10.1142/S0192415X09006941. [DOI] [PubMed] [Google Scholar]
- 4.Quiroz-González S., Torres-Castillo S., López-Gómez R.E., Jiménez Estrada I. Acupuncture points and their relationship with multireceptive fields of neurons. J Acupuncture Meridian Stud. 2017;10:81–89. doi: 10.1016/j.jams.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 5.Xue C.C.L., Zhang A.L., Greenwood K.M., Lin V., Story D.F. Traditional Chinese medicine: an update on clinical evidence. J Alternative Compl Med. 2010;16:301–312. doi: 10.1089/acm.2009.0293. [DOI] [PubMed] [Google Scholar]
- 6.Carlos L., Cruz LAP da, Leopoldo V.C., Campos FR de, Almeida AM de, RC de CP Silveira. Effectiveness of traditional Chinese acupuncture versus sham acupuncture: a systematic review. Rev Lat Am Enfermagem. 2016;24 doi: 10.1590/1518-8345.0647.2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gy Y R.H. vol. 101. The Medical Clinics of North America; 2017. (Integrative Medicine for Respiratory Conditions: Asthma and Chronic Obstructive Pulmonary Disease). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matsumoto-Miyazaki J., Ushikoshi H., Suzuki K., et al. Efficacy of acupuncture treatment for improving the respiratory status in patients receiving prolonged mechanical ventilation in intensive care units: a retrospective observational study. J Alternative Compl Med. 2018;24:1076–1084. doi: 10.1089/acm.2017.0365. [DOI] [PubMed] [Google Scholar]
- 9.Patil S., Sen S., Bral M., et al. The role of acupuncture in pain management. Curr Pain Headache Rep. 2016;20:22. doi: 10.1007/s11916-016-0552-1. [DOI] [PubMed] [Google Scholar]
- 10.Yuan S.-C., Cao W.-J., Huang Y., Hua S.-Y., Zhou Y.-H., Cai R. [Effect of acupuncture on analgesia and sedation in elderly patients with severe pneumonia during invasive mechanical ventilation] Zhongguo Zhen Jiu. 2021;41:971–978. doi: 10.13703/j.0255-2930.20200903-k0004. [DOI] [PubMed] [Google Scholar]
- 11.Lee A., Done M.L. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2004:CD003281. doi: 10.1002/14651858.CD003281.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Acupuncture and related techniques during perioperative period. Lit Rev. 2021 https://pubmed.ncbi.nlm.nih.gov/27912957/ PubMed n.d. [Google Scholar]
- 13.Coyle M.E., Shergis J.L., Huang E.T.-Y., et al. Acupuncture therapies for chronic obstructive pulmonary disease: a systematic review of randomized, controlled trials. Alternative Ther Health Med. 2014;20:10–23. [PubMed] [Google Scholar]
- 14.Liu X., Fan T., Lan Y., Dong S., Fu J., Mao B. Effects of transcutaneous electrical acupoint stimulation on patients with stable chronic obstructive pulmonary disease: a prospective, single-blind, randomized, placebo-controlled study. J Alternative Compl Med. 2015;21:610–616. doi: 10.1089/acm.2014.0284. [DOI] [PubMed] [Google Scholar]
- 15.Tsay S.-L., Wang J.-C., Lin K.-C., Chung U.-L. Effects of acupressure therapy for patients having prolonged mechanical ventilation support. J Adv Nurs. 2005;52:142–150. doi: 10.1111/j.1365-2648.2005.03576.x. [DOI] [PubMed] [Google Scholar]
- 16.Vance C.G., Dailey D.L., Rakel B.A., Sluka K.A. Using TENS for pain control: the state of the evidence. Pain Manag. 2014;4:197–209. doi: 10.2217/pmt.14.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen Y., Wu W., Yao Y., Yang Y., Zhao Q., Qiu L. Transcutaneous electric acupoint stimulation at Jiaji points reduce abdominal pain after colonoscopy: a randomized controlled trial. Int J Clin Exp Med. 2015;8:5972–5977. [PMC free article] [PubMed] [Google Scholar]
- 18.Levy I., Gavrieli S., Hefer T., et al. Acupuncture treatment of delirium in older adults hospitalized in internal medicine departments: an open-label pragmatic randomized-controlled trial. J Geriatr Psychiatr Neurol. 2021 doi: 10.1177/0891988721996804. [DOI] [PubMed] [Google Scholar]
- 19.Li P., Pitsillides K.F., Rendig S.V., Pan H.L., Longhurst J.C. Reversal of reflex-induced myocardial ischemia by median nerve stimulation: a feline model of electroacupuncture. Circulation. 1998;97:1186–1194. doi: 10.1161/01.cir.97.12.1186. [DOI] [PubMed] [Google Scholar]
- 20.Jin Z., Gan T.J., Bergese S.D. Prevention and treatment of postoperative nausea and vomiting (PONV): a review of current recommendations and emerging therapies. Therapeut Clin Risk Manag. 2020;16:1305–1317. doi: 10.2147/TCRM.S256234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kao M.-L., Chen Y.-L., Lee S.-C., Huang S.-Y., Lin P.-Y. Electroacupuncture improves gastric emptying in critically ill neurosurgical patients: a pilot study. Evid Based Complement Alternat Med. 2017;2017 doi: 10.1155/2017/1892161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pfab F., Winhard M., Nowak-Machen M., et al. Acupuncture in critically ill patients improves delayed gastric emptying: a randomized controlled trial. Anesth Analg. 2011;112:150–155. doi: 10.1213/ANE.0b013e3181fdfac8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Funk G.-C., Anders S., Breyer M.-K., et al. Incidence and outcome of weaning from mechanical ventilation according to new categories. Eur Respir J. 2010;35:88–94. doi: 10.1183/09031936.00056909. [DOI] [PubMed] [Google Scholar]
- 24.Jia X., Malhotra A., Saeed M., Mark R.G., Talmor D. Risk factors for ARDS in patients receiving mechanical ventilation for > 48 h. Chest. 2008;133:853–861. doi: 10.1378/chest.07-1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Suzuki M., Muro S., Ando Y., et al. A randomized, placebo-controlled trial of acupuncture in patients with chronic obstructive pulmonary disease (COPD): the COPD-acupuncture trial (CAT) Arch Intern Med. 2012;172:878–886. doi: 10.1001/archinternmed.2012.1233. [DOI] [PubMed] [Google Scholar]
- 26.Maa S.-H., Wang C.-H., Hsu K.-H., et al. Acupressure improves the weaning indices of tidal volumes and rapid shallow breathing index in stable coma patients receiving mechanical ventilation: randomized controlled trial. Evid base Compl Alternative Med. 2013;2013 doi: 10.1155/2013/723128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Therapeutic observation of acupuncture for gastrointestinal dysfunction in severe pneumonia. Shanghai J Acupuncture Moxibustion. 2017;(12):287–290. https://pesquisa.bvsalud.org/portal/resource/pt/wpr-510491 | WPRIM n.d. [Google Scholar]
- 28.AminiSaman J., Mohammadi S., Karimpour H., Hemmatpour B., Sharifi H., Kawyannejad R. Transcutaneous electrical nerve stimulation at the acupuncture points to relieve pain of patients under mechanical ventilation: a randomized controlled study. J Acupunct Meridian Stud. 2018;11:290–295. doi: 10.1016/j.jams.2018.06.008. [DOI] [PubMed] [Google Scholar]
- 29.Andersson S., Lundeberg T. Acupuncture — from empiricism to science: functional background to acupuncture effects in pain and disease Pain and disease. Med Hypotheses. 1995;45:271–281. doi: 10.1016/0306-9877(95)90117-5. [DOI] [PubMed] [Google Scholar]
- 30.Wang H., Xie Y., Zhang Q., et al. Transcutaneous electric acupoint stimulation reduces intra-operative remifentanil consumption and alleviates postoperative side-effects in patients undergoing sinusotomy: a prospective, randomized, placebo-controlled trial. Br J Anaesth. 2014;112:1075–1082. doi: 10.1093/bja/aeu001. [DOI] [PubMed] [Google Scholar]
- 31.Melzack R., Vetere P., Finch L. Transcutaneous electrical nerve stimulation for low back pain - a comparison of TENS for pain and range of motion. Phys Ther. 1983;63:489–493. doi: 10.1093/ptj/63.4.489. [DOI] [PubMed] [Google Scholar]
- 32.Zheng X., Meng J.-B., Fang Q. Electroacupuncture reduces the dose of midazolam monitored by the bispectral index in critically ill patients with mechanical ventilation: an exploratory study. Acupuncture in medicine. J British Med Acupuncture Spc. 2012 doi: 10.1136/acupmed-2011-010095. [DOI] [PubMed] [Google Scholar]
- 33.Feeney C., Bruns E., LeCompte G., Forati A., Chen T., Matecki A. Acupuncture for pain and nausea in the intensive care unit: a feasibility study in a public safety net hospital. J Alternative Compl Med. 2017;23:996–1004. doi: 10.1089/acm.2016.0323. [DOI] [PubMed] [Google Scholar]
- 34.Sandvik R.K., Olsen B.F., Rygh L.-J., Moi A.L. Pain relief from nonpharmacological interventions in the intensive care unit: a scoping review. J Clin Nurs. 2020;29:1488–1498. doi: 10.1111/jocn.15194. [DOI] [PubMed] [Google Scholar]
- 35.Frontera J.A. Delirium and sedation in the ICU. Neurocritical Care. 2011;14:463–474. doi: 10.1007/s12028-011-9520-0. [DOI] [PubMed] [Google Scholar]
- 36.Cavallazzi R., Saad M., Marik P.E. Delirium in the ICU: an overview. Ann Intensive Care. 2012;2:49. doi: 10.1186/2110-5820-2-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Joo C., Lee S., Kang J.W., Lee J.-D. Acupuncture for postoperative delirium (POD): a systematic review and meta-analysis protocol. Medicine. 2021;100 doi: 10.1097/MD.0000000000023822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Matsumoto-Miyazaki J., Ushikoshi H., Miyata S., et al. Acupuncture and traditional herbal medicine therapy prevent deliriumin patients with cardiovascular disease in intensive care units. Am J Chin Med. 2017;45:255–268. doi: 10.1142/S0192415X17500161. [DOI] [PubMed] [Google Scholar]
- 39.Moore F.A., McKinley B.A., Moore E.E. The next generation in shock resuscitation. Lancet. 2004;363:1988–1996. doi: 10.1016/S0140-6736(04)16415-5. [DOI] [PubMed] [Google Scholar]
- 40.Hsu C., Hua Y., Jong G., et al. Shock resuscitation with acupuncture: case report. Emerg Med J. 2006;23:e18. doi: 10.1136/emj.2004.023218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xian J., Wang L., Zhang C., et al. Efficacy and safety of acupuncture as a complementary therapy for sepsis. Medicine (Baltim) 2019;98 doi: 10.1097/MD.0000000000018025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lai F., Ren Y., Lai C., et al. Acupuncture at Zusanli (ST36) for experimental sepsis: a systematic review. Evid Based Complement Alternat Med. 2020;2020 doi: 10.1155/2020/3620741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Choi G.S., Oha S.D., Han J.B., et al. Modulation of natural killer cell activity affected by electroacupuncture through lateral hypothalamic area in rats. Neurosci Lett. 2002;329:1–4. doi: 10.1016/s0304-3940(02)00551-7. [DOI] [PubMed] [Google Scholar]
- 44.Sato T., Yu Y., Guo S.Y., Kasahara T., Hisamitsu T. Acupuncture stimulation enhances splenic natural killer cell cytotoxicity in rats. Jpn J Physiol. 1996;46:131–136. doi: 10.2170/jjphysiol.46.131. [DOI] [PubMed] [Google Scholar]
- 45.Rho S.-W., Choi G.-S., Ko E.-J., et al. Molecular changes in remote tissues induced by electro-acupuncture stimulation at acupoint ST36. Mol Cell. 2008;25:178–183. [PubMed] [Google Scholar]
- 46.Kim S.K., Lee Y., Cho H., et al. A parametric study on the immunomodulatory effects of electroacupuncture in DNP-KLH immunized mice. Evid Based Complement Alternat Med. 2011;2011 doi: 10.1093/ecam/nep166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen L., Xu A., Yin N., et al. Enhancement of immune cytokines and splenic CD4+ T cells by electroacupuncture at ST36 acupoint of SD rats. PLoS One. 2017;12 doi: 10.1371/journal.pone.0175568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pan W.-X., Fan A.Y., Chen S., Alemi S.F. Acupuncture modulates immunity in sepsis: toward a science-based protocol. Auton Neurosci. 2021;232 doi: 10.1016/j.autneu.2021.102793. [DOI] [PubMed] [Google Scholar]
- 49.Yang G., Hu R., Deng A., Huang Y., Li J. Effects of electro-acupuncture at Zusanli, Guanyuan for sepsis patients and its mechanism through immune regulation. Chin J Integr Med. 2016;22:219–224. doi: 10.1007/s11655-016-2462-9. [DOI] [PubMed] [Google Scholar]
- 50.Wu F.W. Effect of electro-acupuncture upon Zusanli on inflammatory response and immune function in the patients of sepsis. J Emerg Tradit Chin Med. 2016;9:1794–1797. [Google Scholar]
- 51.Braunschweig C.L., Levy P., Sheean P.M., Wang X. Enteral compared with parenteral nutrition: a meta-analysis. Am J Clin Nutr. 2001;74:534–542. doi: 10.1093/ajcn/74.4.534. [DOI] [PubMed] [Google Scholar]
- 52.Montejo J.C., Miñambres E., Bordejé L., et al. Gastric residual volume during enteral nutrition in ICU patients: the REGANE study. Intensive Care Med. 2010;36:1386–1393. doi: 10.1007/s00134-010-1856-y. [DOI] [PubMed] [Google Scholar]
- 53.Zou D., Chen W.H., Iwakiri K., Rigda R., Tippett M., Holloway R.H. Inhibition of transient lower esophageal sphincter relaxations by electrical acupoint stimulation. Am J Physiol Gastrointest Liver Physiol. 2005;289:G197–G201. doi: 10.1152/ajpgi.00023.2005. [DOI] [PubMed] [Google Scholar]
- 54.Chang C.-S., Chou J.-W., Ko C.-W., Wu C.-Y., Chen G.-H. Cutaneous electrical stimulation of acupuncture points may enhance gastric myoelectrical regularity. Digestion. 2002;66:106–111. doi: 10.1159/000065596. [DOI] [PubMed] [Google Scholar]
- 55.Tabosa A., Yamamura Y., Forno E.R., Mello L.E.A.M. A comparative study of the effects of electroacupuncture and moxibustion in the gastrointestinal motility of the rat. Dig Dis Sci. 2004;49:602–610. doi: 10.1023/b:ddas.0000026305.20852.41. [DOI] [PubMed] [Google Scholar]
- 56.Jin H.O., Zhou L., Lee K.Y., Chang T.M., Chey W.Y. Inhibition of acid secretion by electrical acupuncture is mediated via beta-endorphin and somatostatin. Am J Physiol. 1996;271:G524–G530. doi: 10.1152/ajpgi.1996.271.3.G524. [DOI] [PubMed] [Google Scholar]
- 57.Nind G., Chen W.-H., Protheroe R., et al. Mechanisms of gastroesophageal reflux in critically ill mechanically ventilated patients. Gastroenterology. 2005;128:600–606. doi: 10.1053/j.gastro.2004.12.034. [DOI] [PubMed] [Google Scholar]
- 58.Huang S.-T., Chen G.-Y., Lo H.-M., Lin J.-G., Lee Y.-S., Kuo C.-D. Increase in the vagal modulation by acupuncture at neiguan point in the healthy subjects. Am J Chin Med. 2005;33:157–164. doi: 10.1142/S0192415X0500276X. [DOI] [PubMed] [Google Scholar]
- 59.Ben-Arie E., Kao P.-Y., Ho W.-C., Lee Y.C. Acupuncture effect on digestion in critically ill postoperative oral and hypopharyngeal cancer patients. Medicine (Baltim) 2019;98 doi: 10.1097/MD.0000000000016944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ben-Arie E., Wei T.-H., Chen H.-C., et al. Digestion-specific acupuncture effect on feeding intolerance in critically ill post-operative oral and hypopharyngeal cancer patients: a single-blind randomized control trial. Nutrients. 2021;13:2110. doi: 10.3390/nu13062110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schefold J.C., Bierbrauer J., Weber-Carstens S. Intensive care unit-acquired weakness (ICUAW) and muscle wasting in critically ill patients with severe sepsis and septic shock. J Cachexia Sarcopenia Muscle. 2010;1:147–157. doi: 10.1007/s13539-010-0010-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Babb T., Levine B., Philley J. ICU-acquired weakness: an extension of the effects of bed rest. Am J Respir Crit Care Med. 2012;185:230–231. doi: 10.1164/ajrccm.185.2.230. [DOI] [PubMed] [Google Scholar]
- 63.Formenti P., Umbrello M., Coppola S., Froio S., Chiumello D. Clinical review: peripheral muscular ultrasound in the ICU. Ann Intensive Care. 2019;9:57. doi: 10.1186/s13613-019-0531-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Song J., Li H., Cao Y., et al. Electroacupuncture improves survival in rats with lethal endotoxemia via the autonomic nervous system. Anesthesiology. 2012;116:406–414. doi: 10.1097/ALN.0b013e3182426ebd. [DOI] [PubMed] [Google Scholar]
- 65.Su Z., Hu L., Cheng J., et al. Acupuncture plus low-frequency electrical stimulation (Acu-LFES) attenuates denervation-induced muscle atrophy. J Appl Physiol. 2016;120:426–436. doi: 10.1152/japplphysiol.00175.2015. 1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhou X., Xing B., He G., Lyu X., Zeng Y. The effects of electrical acupuncture and essential amino acid supplementation on sarcopenic obesity in male older adults: a randomized control study. Obes Facts. 2018;11:327–334. doi: 10.1159/000491797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shou Y., Jin W., Zhuang L., et al. Efficacy of acupuncture combined with rehabilitation training for intensive care unit-acquired muscle weakness: a protocol for a randomized, sham-procedure-controlled clinical trial. Evid base Compl Alternative Med. 2021;2021 doi: 10.1155/2021/3539651. [DOI] [PMC free article] [PubMed] [Google Scholar]
Further reading
- 68.Tonner P.H., Weiler N., Paris A., Scholz J. Sedation and analgesia in the intensive care unit. Curr Opin Anaesthesiol. 2003;16:113–121. doi: 10.1097/00001503-200304000-00003. [DOI] [PubMed] [Google Scholar]
- 69.Hughes C.G., McGrane S., Pandharipande P.P. Sedation in the intensive care setting. Clin Pharmacol. 2012;4:53–63. doi: 10.2147/CPAA.S26582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bolton C., Thilges S., Lane C., Lowe J., Mumby P. Post-traumatic stress disorder following acute delirium. J Clin Psychol Med Settings. 2021;28:31–39. doi: 10.1007/s10880-019-09689-1. [DOI] [PubMed] [Google Scholar]
- 71.Jacobi J., Fraser G.L., Coursin D.B., et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002;30:119–141. doi: 10.1097/00003246-200201000-00020. [DOI] [PubMed] [Google Scholar]
- 72.Pandharipande P.P., Pun B.T., Herr D.L., et al. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA. 2007;298:2644–2653. doi: 10.1001/jama.298.22.2644. [DOI] [PubMed] [Google Scholar]