Abstract
Introduction: Mass burn casualty disasters present with a big challenge due to the complex multidisciplinary management of severely burned patients and the limited capacity of the specialized centers. Literature is scarce, and so is the management of these disasters with enzymatic debridement (ED). Methods: Retrospective observational analysis of nine patients admitted to the Vall d’Hebron University Hospital Burn Center (Barcelona, Spain), as a consequence of a bell tower explosion on December 30, 2019. The patients with intermediate-deep second-degree burns, either in circumferential or affecting highly functional areas as hands, feet or face, were included in the ED group. Continuous variables are expressed as mode and standard deviation and quantitative ones as percentages. Results: Fourteen people were injured after the explosion of gunpowder-containing bags in a bell tower during a cultural celebration. Nine casualties (6 men and 3 women) suffered burn injuries that required assessment and admission in our Burn Center. The mean age was 44.33 years (range 19-61 years), with burns covering a mean total body surface area (TBSA) of 15% (range 5-48% TBSA). One patient required invasive mechanical ventilation and intensive care management. Seven patients required ED, with an average debrided TBSA of 6.1% (range 3-10% TBSA). Seven out of 9 patients required at least one surgery. The average hospital stay was 23.33 days (range 2-53 days). No escharotomy was required and no patient died. Conclusions: This experience brought out the weak and strong features of our center when facing a situation that implies an important care stress. It can be useful for other Burn Centers in similar situations in the future. We found that new tools, such as ED, can be advantageous in such situations.
Keywords: Burn, multiple burn victims, mass casualty disaster, fire disasters, burn center, enzymatic debridement
Introduction
A mass casualty event is an emergency that can push the boundaries of the regional emergency services and hospital centers and they may even exceed the available resources [1]. There are some publications that analyse the responses to some major catastrophes, both from a global point of view [2-4] and others with a specific center perspective [5,6]. These evaluations contribute to a better understanding and management of those events [7]. Nevertheless, we have found no references of accidents that, despite having a lower number of casualties, all of them are assisted in a single Burn Center.
In the last years, our region faced some situations that required an important effort from our center, such as the terrorist bombing of the department store Hipercor in Barcelona in June 1987, with 21 deaths and 45 injured [8], the explosion in Gavà in 2008, with 7 deaths and 21 injured [9], and the explosion of a gas carrying tanker truck in a road located next to the Los Alfaques campground in 1978, where 215 people died and 175 were injured [10].
Our center has been using ED since 2015, so the familiarity with this treatment let us use it in a mass burn casualty event. It allowed us to treat a large number of patients in the first 24 hours without the need of an operating room.
The objective of this research is to show the characteristics of the accident occurred in Centelles (Spain) on December 30, 2019, the response of our Burn Center and the lessons learned from this event.
Methods
A retrospective descriptive analysis was carried out from digitalized clinical database of nine patients admitted to the Vall d’Hebron University Hospital Burn Center (Barcelona, Spain) on December 30, 2019, as a consequence of the explosion in a bell tower in Centelles (Barcelona, Spain). We included only the victims transferred and admitted to our Burn Center; casualties attended at the scene and not transferred were not considered. Moreover, the patients with intermediate-deep second-degree burns, either in circumferential areas or affecting highly functional areas as hands, feet or face, were included in the ED group. The following variables were collected: gender, age, length of hospital stay, TBSA for second and third-degree burns and affected areas, need of ED, local infection and need of surgery. The continuous variables are expressed as mode and standard deviation and the quantitative ones as percentage.
This study was approved by the ethics and clinical research committee of our center: PR(ATR)486/2020. Some press reports were added to complete the chronicle of the event.
Results
The accident
Centelles is a small town located 50 km north from Vall d’Hebron University Hospital in Barcelona. This town celebrates annually the “Festa del Pi”, a cultural festivity in which a pine tree is carried from the forest to the town’s church, while the “galejadors” fire their weapons charged with gunpowder [11]. Apparently, on December 30th, 2019, while some of these “galejadors” were in the bell tower, one of the bags containing gunpowder exploded and it spread to the bags of the people around. This chain explosion resulted in a big deflagration in a demi-closed space that caused wounds in 14 people among “galejadors” and photographers. Figure 1 shows the location of the accident few seconds after the explosion.
Figure 1.

The bell tower seconds after the explosion (retrieved from Twitter with permission from the author).
Notification and patient transfer
Our center received the first notification approximately at 2 pm. The first call reported 14 casualties: one severely burned patient and more patients with milder lesions that could require derivation to our center. There were 2 plastic surgeons (one of them a trainee) and 3 intensive care specialists on call. Two plastic surgery trainees reinforced the on-call team because of the potential huge number of patients expected. Of note, the accident occurred during the Christmas Holiday peak season with part of team on leave. Subsequently, the emergency services confirmed the transfer of 2 severely injured casualties and the on-call team agreed to transfer and assess the patients with milder lesions gradually (in that moment 10 patients were reported). Following the Mass Disaster Protocol of our hospital, the clinical head of our Burn Center joined the team to offer his support.
The first patient arrived transferred by helicopter at our center at approximately 3 pm. Few minutes later 2 other patients arrived by ambulance and one hour later, the last 6 patients arrived by ambulance too, all of them at the same time.
Patients and hospitalization
Nine patients (3 women and 6 men), with a mean age of 44.33 years (range 19-61 years) were assessed in the emergency room of our Burn Center, all of them requiring admission. The average burn extension was 15% TBSA (range 5-48% TBSA). Data is summarized in Table 1 and Figure 2 shows the distribution of the burned areas.
Table 1.
Patient data and summary of hospitalization
| Patients | TBSA (%) | Burned areas | ED | Hospital stay (days) | Surgeries |
|---|---|---|---|---|---|
| 1 | 48 | Face, upper limbs, lower limbs, gluteus, trunk | Yes | 53 | 3 |
| 2 | 18 | Face, upper limbs, thighs, abdomen | Yes | 25 | 1 |
| 3 | 15 | Face, right upper limb, hands, trunk, lower limbs, right flank | Yes | 32 | 2 |
| 4 | 12 | Face-neck, upper limbs, lower limbs | Yes | 17 | 0 |
| 5 | 12 | Face-neck, hands, legs, right thigh | Yes | 25 | 1 |
| 6 | 12 | Face, thigh, right upper limb | Yes | 28 | 1 |
| 7 | 8 | Face-neck, hands, lower limbs | Yes | 24 | 1 |
| 8 | 5 | Face, trunk, forearms, left hand | No | 4 | 1 |
| 9 | 5 | Face, right upper limb | No | 2 | 0 |
M: Male; F: female; TBSA: Total Body Surface Area; ED: Enzymatic debridement.
Figure 2.

Most burns were intermediate-deep second and third degree burns and were located in face and upper and lower limbs.
One patient required invasive mechanical ventilation because of the deep burns in the facial area. Five patients had circumferential burn injuries on their limbs (12 limbs in total, 8 upper and 4 lower limbs) with potential risk of compartment syndrome; no escharotomy was required. In contrast, ED (NexoBrid®, Mediwound, Germany) was carried out in all of them. ED was applied also in the facial area of the patient that required mechanical ventilation and in no circumferential burns affecting hands. In overall, seven patients were treated with ED in any body surface.
The two patients that were not candidates for ED had superficial second degree burns in facial areas and hands (approximately 5% TBSA) and were admitted to our hospital to assess facial edema and rule out any potential airway complications. Both were discharged two days afterwards. One of them required elective surgery few days later to cover the non-healing wounds in hands with skin grafts.
Seven patients required one or more surgical interventions, with an average of 1.11 surgeries per patient (range 0-3 surgeries). Surgery consisted in tangential excision and autologous skin grafts in all of them, except for the most severely burned patient, who required tangential excision and homografts before the definitive coverage with autologous skin grafts.
The mean hospitalization stay was 23.33 days (range 2-53 days). No patient died.
Enzymatic debridement (ED)
According to our center protocol, all intermediate-deep second-degree burns, either in circumferential areas or affecting highly functional areas as hands, feet or face, are tributary for early/immediate ED with NexoBrid® [12-16].
Seven patients (78%) met the criteria. Due to the logistic impossibility of applying the product to all of them in the same afternoon, we prioritized the patient with deep burn injuries to the face and those who had deeper and/or circumferential lesions with a higher risk of developing complications as compartment syndrome. ED was performed in 4 patients during the first afternoon, all of them in upper limbs and two of them also in facial area and circumferential wounds on their knees. The other 3 patients were treated with ED the next morning. The average debrided TBSA was 6.1% (range 3-10% TBSA). We followed the ED protocol of our Burn Center in every patient. Data is summarized in Table 2.
Table 2.
Enzymatic debridement (ED) summary
| Patients | Days since accident | Areas | Local infection | Surgery NEED after ED |
|---|---|---|---|---|
| 1 | 0 | Face | No | Hands |
| Hands | ||||
| 2 | 0 | Hands | No | No |
| Forearms | ||||
| 3 | +1 | Hands | No | Right hand |
| Right upper limb | Right upper limb | |||
| 4 | 0 | Hands | No | No |
| Knees | ||||
| 5 | 0 | Hands | Yes (S. aureus) | Hands |
| 6 | +1 | Right hand | No | Right upper limb |
| Right upper limb | ||||
| 7 | +1 | Hands | Yes (E. coli, S. aureus, K. pneumoniae) | No |
| Right upper limb |
Fourteen out of 21 (66.7%) areas treated with ED, which we initially considered that would need surgery, healed spontaneously without surgery in 35.07 days on average (range 16-59 days). Moreover, we observed a reduction of the extension in grafted areas in all the areas that required surgery after ED. Two patients developed local infections in areas treated with ED (hands in both cases), S. aureus was identified in one of them and S. aureus, E. coli and K. pneumoniae in the other one. One of the patients required surgery for coverage as soon as the infection was controlled and cleared.
After the post-ED assessment, all the wounds were considered to have spontaneous healing potential without surgery. Therefore, according to our protocol that is shown in Table 3, the elective dressing applied was Suprathel® (Polymedics Inc., Germany). Unfortunately, due to the Christmas Holidays there was a shortage of product (limited resource by the company) and only some of the patients could be treated with Suprathel®. Therefore, we prioritized this dressing for the superficial wounds after ED and the rest of the wounds were treated with nitrofurazone based ointments. These dressings were discontinued and replaced with Suprathel® as soon as it became available. The facial area was covered with Medihoney® (Medihoney Pty Ltd., Queensland, Australia).
Table 3.
ED application protocol in Vall d’Hebron University Hospital Burn Center
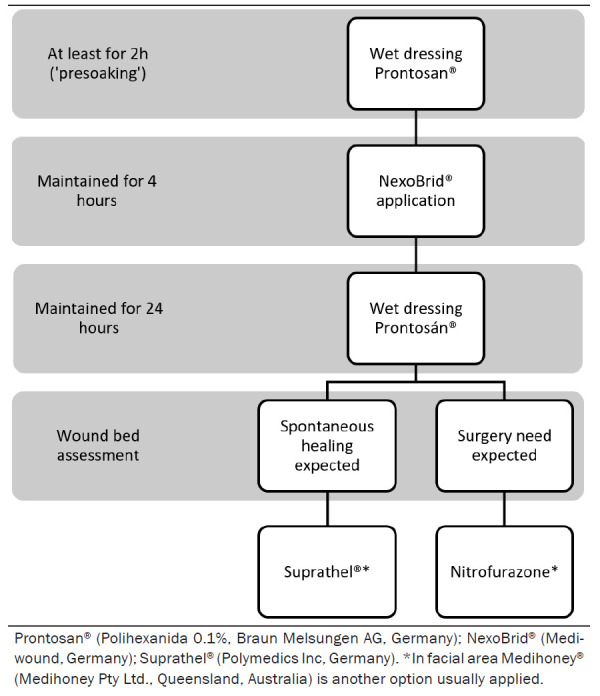
|
Discussion
A mass burn casualty disaster is defined as an event in which the number of victims exceeds the capacity of the local burn center to provide optimal burn care. It poses an extreme stress to the emergency and health system of the region [17]. It is not defined by the absolute number of casualties, but by the capacity of the event to disrupt local resources [5,18]. Some authors suggest that the acute treatment of 2-3 severely burned patients require to increase the capacity of facilities, and accidents with 20 or more victims can produce a collapse even in the most modern and equipped centers [7]. Our center has 20 regular hospitalization and 6 intensive care beds. Therefore, the admission of 9 acute patients that required specialized techniques in a unit that, like most Burn Centers, is usually in its high occupancy limit [1,19], produced an important stress that was managed with an extra effort of the hospital staff.
We consider that every hospital or sanitary area with a Burn Center should have a protocol to guide the assistance in mass casualty events, with the aim of optimizing the patient’s triage, transfer, derivation and, finally, the treatment that they receive. Nowadays, we have a protocol agreed with emergency services and firefighters and some preliminary contacts are in place to renew the protocol of MCI (Multiple Casualty Incidents) for burn victims in the area of Barcelona. Similarly, the EBA (European Burns Association) has started an international plan to face catastrophes through the collaboration among Burn Centers from different countries, including our center [20,21]. These strategies enable to have clear guidelines, avoid improvisation and facilitate a more efficient use of the resources in such complex situations.
A key objective in these situations is to avoid overwhelming specialized centers with minor casualties in order to focus all resources in the most complex patients and distribute the patients to prevent the simultaneous arrival of cases not requiring immediate attention [2,22]. In our case, as per our Mass Casualty Protocol we agreed to assist all the patients after the confirmation of the total number of victims, but only on condition that the transfer was staggered. However, after the arrival of the first 3 most severely injured patients, 6 other patients arrived at the same time at our emergency room. It seems to be a consensus that severe patients (>20% TBSA) should be transferred to a burn unit for evaluation and treatment [2]; although, burn injuries in functional or cosmetic important areas, that in other circumstances should be evaluated in a specialized center, would not be derived, at least initially, to a burn unit [1]. This situation could have been avoided attending the patients in non-specialized hospitals close to the accident location, coordinating later, if necessary, the transfer to our center once we had attended the most severe patients [17,19,23].
Before the arrival of the first patients, we redistributed the milder patients of our unit in other units of our hospital with the aim of having available beds for the expected patients. When 6 patients arrived at the same time, we had to prepare the room where ambulatory patients are normally treated as an emergency room. This was possible because we have a multidisciplinary unit that has an emergency room, wound-dressing room, hospitalization rooms and an operating room in the same unit. The fact that two plastic surgeon trainees stayed in the hospital and the coordination with the nursery team and other services like anesthesiology (who performed the nerve blocks before ED) allowed to speed up the evaluations, decision making and interventions. However, in a posterior discussion and audit, we concluded that we faced a stressing situation that could have been prevented with a better planning.
The use of ED in these patients contributed some advantages. In one hand, as there is no need of an operation room to apply the product (it is carried out in the emergency or wound-dressing room) and the procedure is performed by the nursery staff after a first evaluation by a plastic surgeon, we could perform an early debridement of an important number of patients; without ED, this would have not been possible. ED was performed in all cases within the first 24 hours of hospital admission. It also allowed us to maintain the surgical planning of the unit during the next days. In the other hand, it was very useful to prevent compartment syndrome in circumferential burn injuries in extremities [15,16,24,25]; we did not have to perform any escharotomy, as shown in Figure 3. In these cases, ED is conducted as soon as possible and must not be delayed for the eschar presoaking [15,16]. Finally, we consider that the number of surgical interventions was lower than previously estimated in the first clinical exploration. 67% of treated areas did not require any surgery, despite all of them seemed to be intermediate second degree or deeper initially. Figure 4 shows the evolution of the facial area treated with ED.
Figure 3.
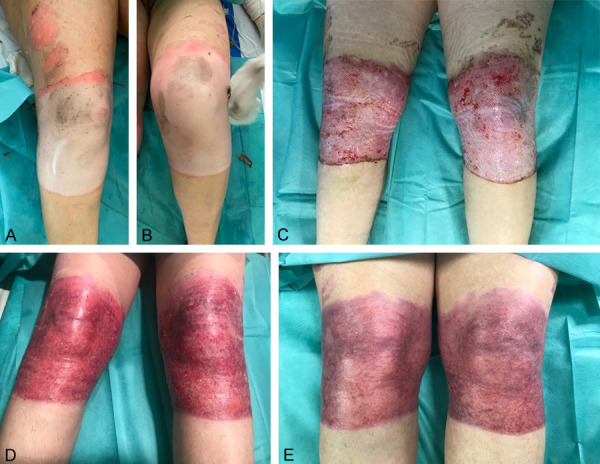
Patient with deep second - third degree circumferential burns in both knees. ED was applied some hours after the accident and posterior dressings consisted in nitrofurazone ointments. Initially, surgery was scheduled, but due to the good evolution of the wound, it was suspending and complete healing was achieved without skin grafting. A, B. Pictures taken during the first assessment in the emergency room. C. Day 12, big areas with deep appearance. D. Day 30, almost complete healing with residual wounds. E. Day 44, uniform epithelialization waiting for scar maturation.
Figure 4.

Deep burns in facial area treated with enzymatic debridement and posterior application of Medihoney®. Complete healing was achieved without need of surgery, with a good cosmetic result. A. Pictures taken in the emergency room. B. Just after removing the enzymatic product (it was maintained for 4 hours). C. 24 hours after ED. D. Day 30, complete epithelialization, good cosmetic result.
Conclusions
After revising our response to the event, we consider all patients received a correct attention, even though the coordination of the patient transfer was not well conducted. We highlight the importance of the pre-established protocols to improve the actuation in this kind of accidents and all the actors in the incident to follow them; in our case, we could manage the situation with an extra effort from the health personnel, but this could not be enough in future events with more casualties or more severely injured ones unless all emergency systems active and do follow the protocol. Regarding the lack of materials, we decided to have a stricter control of the warehouse, especially before periods in which getting new supplies could be difficult (peak holiday seasons). ED enabled us to treat a large number of patients in the early stages of medical care. We could prevent potential complications as compartment syndrome, and, afterwards, reduce the number of surgeries needed and the total surface area requiring surgical intervention. We consider it a useful tool in similar situations when used by an experienced burn care team.
Disclosure of conflict of interest
None.
References
- 1.Haller LH, Wurzer P, Peterlik C, Gabriel C, Cancio LC. Burn management in disasters and humanitarian crises. In: Herndon DN, editor. Total Burn Care. 5th edition. China: Elsevier; 2018. pp. 36–49.pp. e2 [Google Scholar]
- 2.Seifman M, Ek EW, Menezes H, Rozen WM, Whitaker IS, Cleland HJ. Bushfire disaster burn casualty management: the Australian “black saturday” bushfire experience. Ann Plast Surg. 2011;67:460–3. doi: 10.1097/SAP.0b013e3182111021. [DOI] [PubMed] [Google Scholar]
- 3.Cassuto J, Tarnow P. The discotheque fire in Gothenburg 1998. A tragedy among teenagers. Burns. 2003;19:405–416. doi: 10.1016/s0305-4179(03)00074-3. [DOI] [PubMed] [Google Scholar]
- 4.Yang CC, Shih CL. A coordinated emergency response: a color dust explosion at a 2015 concert in Taiwan. Am J Public Health. 2016;106:1582–1585. doi: 10.2105/AJPH.2016.303261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yeong EK, O’Boyle CP, Huang HF, Tai HC, Hsu YC, Chuang SY, Wu YF, Chang CW, Liu TJ, Lai HS. Response of a local hospital to a burn disaster: contributory factors leading to zero mortality outcomes. Burns. 2018;44:1083–1090. doi: 10.1016/j.burns.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 6.Ng CJ, You SH, Wu IL, Weng YM, Chaou CH, Chien CY, Seak CJ. Introduction of a mass burn casualty triage system in a hospital during a powder explosion disaster: a retrospective cohort study. World J Emerg Surg. 2018;13:38. doi: 10.1186/s13017-018-0199-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wachtel TL, Kelly McQueen KA. Tratamiento de las quemaduras en desastres y crisis humanitarias. In: Herndon DN, editor. Tratamiento Integral de las Quemaduras. 3rd edition. Barcelona: Elsevier España; 2009. pp. 26–48. [Google Scholar]
- 8.Gomez Morell PA, Escudero Naif F, Palao Domenech R, Sospedra Carol E, Bañuelos Roda JA. Burns caused by the terrorist bombing of the department store Hipercor in Barcelona. Part I. Burns. 1990;16:423–425. doi: 10.1016/0305-4179(90)90070-d. [DOI] [PubMed] [Google Scholar]
- 9. https://cadenaser.com/ser/2008/12/03/espana/1228265411_850215.html.
- 10.Baux S, Saizy R, Porte A, Zumer L, Mayer G, Mole B, Monsaingeon I. The los alfaques disaster. Ann Chir Plast. 1981;26:185–187. [PubMed] [Google Scholar]
- 11. https://www.centelles.cat/coneixer/festes-i-tradicions/festa-del-pi.
- 12.Krieger Y, Bogdanov-Berezovsky A, Gurfinkel R, Silberstein E, Sagi A, Rosenberg L. Efficacy of enzymatic debridement of deeply burned hands. Burns. 2012;38:108–112. doi: 10.1016/j.burns.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Krieger Y, Rubin G, Schulz A, Rosenberg N, Levi A, Singer AJ, Rosenberg L, Shoham Y. Bromelain-based enzymatic debridement and minimal invasive modality (MIM) care of deeply burned hands. Ann Burns Fire Disasters. 2017;30:198–204. [PMC free article] [PubMed] [Google Scholar]
- 14.Martínez-Méndez JR, Serracanta-Domènech J, Monclús-Fuertes E, Pérez-del-Caz D, López-Suso E, García-Contreras JD, Piqueras-Perez Guía clínica de consenso en el uso de desbridamiento enzimático en quemaduras con NexoBrid® . C Plást Iberolatinoam. 2017;43:193–202. [Google Scholar]
- 15.Hirche C, Kreken Almeland S, Dheansa B, Fuchs P, Governa M, Hoeksema H, Korzeniowski T, Lumenta DB, Marinescu S, Martinez-Mendez R, Plock JA, Sander F, Ziegler B, Kneser U. Eschar removal by bromelain based enzymatic debridement (Nexobrid®) in burns: European consensus guidelines update. Burns. 2020;46:782–796. doi: 10.1016/j.burns.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Hirche C, Citterio A, Hoeksema H, Koller J, Lehner M, Martinez JR, Monstrey S, Murray A, Plock JA, Sander F, Schulz A, Ziegler B, Kneser U. Eschar removal by bromelain based enzymatic debridement (Nexobrid®) in burns: an European consensus. Burns. 2017;43:1640–1653. doi: 10.1016/j.burns.2017.07.025. [DOI] [PubMed] [Google Scholar]
- 17.Kuo LW, Yen CI, Fu CY, Pan CH, Hsu CP, Hsiao YC, Hsieh CH, Hsu YP. The role of preliminary hospitals in the management of a mass burn casualty disaster. Burns. 2018;44:800–806. doi: 10.1016/j.burns.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 18.McElroy JA, Steinberg S, Keller J, Falcone RE. Operation continued care: a large mass-casualty, full-scale exercise as a test of regional preparedness. Surgery. 2019;166:587–592. doi: 10.1016/j.surg.2019.05.045. [DOI] [PubMed] [Google Scholar]
- 19.Kearns RD, Holmes JH 4th, Alson RL, Cairns BA. Disaster planning: the past, present, and future concepts and principles of managing a surge of burn injured patients for those involved in hospital facility planning and preparedness. J Burn Care Res. 2014;35:e33–e42. doi: 10.1097/BCR.0b013e318283b7d2. [DOI] [PubMed] [Google Scholar]
- 20. https://ec.europa.eu/echo/sites/echo-site/files/swd_preparing_for_mass_burn_casualty_incidents.pdf.
- 21. http://euroburn.org/documents/
- 22.Atiyeh B, Gunn SW, Dibo S. Primary triage of mass burn casualties with associated severe traumatic injuries. Ann Burns Fire Disasters. 2013;26:48–52. [PMC free article] [PubMed] [Google Scholar]
- 23.Lancet EA, Zhang WW, Roblin P, Arquilla B, Zeig-Owens R, Asaeda G, Kaufman B, Alexandrou NA, Gallagher JJ, Cooper ML, Styles T, Prezant DJ, Quinn C. Factors influencing the prioritization of injured patients for transfer to a burn or trauma center following a mass casualty event. Disaster Med Public Health Prep. 2021;15:78–85. doi: 10.1017/dmp.2019.144. [DOI] [PubMed] [Google Scholar]
- 24.Fischer S, Haug V, Diehm Y, Rhodius P, Cordts T, Schmidt VJ, Kotsougiani D, Horter J, Kneser U, Hirche C. Feasibility and safety of enzymatic debridement for the prevention of operative escharotomy in circumferential deep burns of the distal upper extremity. Surgery. 2019;165:1100–1105. doi: 10.1016/j.surg.2018.11.019. [DOI] [PubMed] [Google Scholar]
- 25.Mataro I, Lanza A, Di Franco S, Di Franco L, Sangiuolo M, Notaro M, d’Alessio R, Villani R. Releasing burn induced compartment syndrome (BICS) by enzymatic escharotomy-debridement: a case series. J Burn Care Res. 2020;41:1097–1103. doi: 10.1093/jbcr/iraa055. [DOI] [PubMed] [Google Scholar]


