Abstract
Personalised and targeted interventions have revolutionised cancer treatment and dramatically improved survival rates in recent decades. Nonetheless, effective pain management remains a problem for patients diagnosed with cancer, who continue to suffer from the painful side effects of cancer itself, as well as treatments for the disease. This problem of cancer pain will continue to grow with an ageing population and the rapid advent of more effective therapeutics to treat the disease. Current pain management guidelines from the World Health Organisation are generalised for different pain severities, but fail to address the heterogeneity of mechanisms in patients with varying cancer types, stages of disease and treatment plans. Pain is the most common complaint leading to emergency unit visits by patients with cancer and over one-third of patients that have been diagnosed with cancer will experience under-treated pain. This review summarises preclinical models of cancer pain states, with a particular focus on cancer-induced bone pain and chemotherapy-associated pain. We provide an overview of how preclinical models can recapitulate aspects of pain and sensory dysfunction that is observed in patients with persistent cancer-induced bone pain or neuropathic pain following chemotherapy. Peripheral and central nervous system mechanisms of cancer pain are discussed, along with key cellular and molecular mediators that have been highlighted in animal models of cancer pain. These include interactions between neuronal cells, cancer cells and non-neuronal cells in the tumour microenvironment. Therapeutic targets beyond opioid-based management are reviewed for the treatment of cancer pain.
Keywords: pain, dorsal root ganglia, cancer-induced bone pain, chemotherapy associated pain, neuropathy, cancer, sensitisation
The problem of cancer pain
Cancer survival rates have dramatically increased since the turn of the century with the advent of targeted and improved treatment strategies. On the other hand, the annual number of cancer cases worldwide is estimated to rise from 14 million in 2012 to 22 million by 2032, leaving behind the growing problem of effective pain management for side effects of cancer and its treatments. Almost all patients diagnosed with cancer endure chronic pain because of surgery, treatments or side effects like a pathological fracture. Between 30% and 50% of patients receiving curative-intent therapy and 75%–90% of patients with advanced disease endure chronic pain that is strong enough to require opioid therapy (1, 2). More than one-third of patients in disease remission will continue to report pain after curative treatment (3). Cancer-related pain often consists of background pain with acute exacerbations, peaking several times a day that can be either spontaneous or evoked in areas of sensory abnormality. Spontaneous pain may be ongoing (either at a constant or fluctuating pain intensity), or it can be dominated by a juxtaposition of pain paroxysms of short duration interspersed by pain-free intervals or a less intense background pain. Paraesthesia and dysaesthesia are also frequently reported.
The World Health Organization (WHO) Analgesic Ladder is frequently the first step in a paradigm for guiding clinicians to manage pain in a systemic manner, where the selection of pharmacological analgesic treatments is based on the degree of pain. Over-the-counter analgesics comprise Step 1, “weak” opioids (such as codeine) are escalated in Step 2, followed by the use of “strong” opioids in Step 3 to treat moderate-to-severe pain. Clinical professionals are urged to take non-pharmacologic pain management methods in Step 4 into account (4). Non-opioid analgesics include acetaminophen (5) and non-steroidal anti-inflammatory drugs (NSAIDs) (6). The advantage of NSAID/opioid combination therapy is a reduction in overall opioid prescriptions, but data on its efficacy is conflicting (6–8). Adjuvant therapies include anti-depressants [like duloxetine (9) and anticonvulsants like gabapentin and pregabalin (10)], which are first or second-line analgesics for other chronic pain conditions, including painful neuropathies (11). Adjuvant analgesics, integrative therapeutic options [such as acupuncture (12)], as well as interventions [e.g., nerve block (13) and epidural or intrathecal analgesics (7)] can be considered at any stage of pain management even though they are not listed on the WHO ladder.
There remains a continuous debate regarding the suitability of these generalised WHO recommendations to adequately manage pain in a heterogeneous group of patients that have a cancer diagnosis. A meta-analysis of WHO Cancer Pain Relief guideline outcomes indicates that adequate analgesia is achieved in a range of as little as 20% but up to 100% of patients (14). A contentious point has been raised regarding the prescription of weak Step 2 opioids before starting morphine for managing moderate pain; patients with cancer suffering from moderate pain have a higher probability of responding to low-morphine doses than they are to codeine (15). Furthermore, new research indicates that potent analgesics may be more effective if given earlier in the course of the disease prior to a critical transition point when the plasticity of the nociceptive system may become resistant to conventional pharmacological treatment (16).
The need to modify current pain management protocols in patients with cancer is indicated by reports that pain is the most common complaint leading to emergency unit visits by patients with cancer (17–19). Despite well-established findings demonstrating that the experience of pain can impact long-term clinical outcomes, patients with cancer frequently receive insufficient pain management (20). Studies investigating the frequency and effectiveness of pain control suggest areas for improvement, e.g., a systematic analysis reported that despite a 25% drop in under-treated cancer pain between 2007 and 2013, over one-third of patients with cancer still experience under-treated pain (21). Pain has a demonstrable impact on the quality of life of patients with cancer, and the lack of adequate pain management among this growing population underlines the need for novel and targeted approaches to treat pain arising from cancer or its treatment. This review summarises the use of animal models of cancer pain, with a focus on cancer-induced bone pain (CIBP) and chemotherapy associated pain. Peripheral and central nervous system mechanisms involved in cancer pain are also discussed, followed by potential targets for pain relief.
Animal models of cancer pain
Here we describe animal models of cancer pain, including method of induction and pain related outcomes.
Animal models of cancer-induced bone pain (CIBP)
Early models of CIBP relied on the administration of cancer cells into the left ventricle of mice, followed by migration of cancer cells in the general circulation to develop metastases at different tissue sites, including bone marrow (22). The main advantage of models relying on systemic administration of cancer cells models is the replication of the clinical course of disease due to the fact that bone tumours usually develop as metastases rather than as primary tumours. However, significant disadvantages of such models include the poor predictability of metastatic sites and size, leading to insufficient reproducibility of disease progression across a cohort of animals. Another strategy is to directly administer cancer cells into the intramedullary space of a bone (e.g., the femur) in rodents (23). The site of the injection of the cancer cells into the bone is then sealed to restrict tumour growth in the intramedullary space. In comparison to systemic administration of cancer cells, CIBP models that involve direct injection in the bone facilitate the evaluation of tumour growth over time, radiological imaging, observation of bone degradation, examination of histopathologic changes, site-specific behavioural testing, as well as evaluation of neurochemical changes that take place at the tumour site, in the dorsal root ganglion (DRG) and the central nervous system (CNS) (24). Mouse models typically involve the implantation of tumour cells into the femur, and rat models are typically created via percutaneous injection of cancer cells into the tibia (25). The cell lines used will vary across species and studies, e.g., for B6C3-Fe-a/a and C3H/HeJ mice, fibrosarcoma cells have been reported to be administered in the femur (26, 27), humerus (28) and calcaneus bones (29). Lewis lung carcinoma cells are administered into the intramedullary space of the femur in C57BL/6 mice (30). In rats, MRMT1 mammary gland carcinoma cells are administered into the tibias of female Sprague–Dawley rats (31), and MDA-MB231 human breast cancer cells are injected into femoral arteries of nude rats (32) as well as R3327 prostate cancer cells (33). Cancer cells that have metastasised to the bone can be classified as either osteosclerotic or osteolytic based on x-ray images (34). Osteosclerotic cancers are distinguished by increased bone deposition through increased osteoblast activity. Prostate cancer is the protype for osteosclerotic bone metasases, whereas breast cancer is the protype for osteolytic bone metastases because breast cancer cells potentiate osteoclast-induced bone degradation (34, 35).
Rodents exhibit pain-like behaviours within 2–3 weeks of intrafemoral inoculation with cancer cells in a dose-dependent manner (30, 36, 37). Non-evoked pain behaviours include reduced use of the affected limb, which can be quantified using a limb score, as well as a reduction in weight borne on the affected limb when tested by an incapacitance tester (30, 36–38). Loss of bone mineral density or osteolysis can also be reliably detected with the progression of tumour growth (30). The ability to reproduce a chronic pain phenotype, as well as the cancer-induced bone remodelling, is critical to understanding the structural and neuronal mechanisms underlying CIBP (39, 40). One major shortcoming of animal models is the challenge in predicting breakthrough pain, which is an important clinical feature of CIBP. Assessment of breakthrough pain would require continuous monitoring of animals, e.g., with the use of ultrasound vocalisation techniques, but has yet to be an established feature of rodent CIBP models. See Table 1 for a summary of different animal models of CIBP.
Table 1.
Animal models used to study CIBP and targets for analgesia.
| Murine model and strain | Method of induction of cancer pain model | Assays to assess pain behaviour | Analgesics tested (and reference) |
|---|---|---|---|
| CIBP in C3H/HeNCrl mice | Injection of osteolytic NCTC 2472 fibrosarcoma cells into the femur | Spontaneous lifting Limb-use during forced ambulation on rotarod | Fentanyl (0.025–0.64 mg/kg, s.c) Sufentanil (0.005–0.04 mg/kg, s.c) Morphine (2.5–40 mg/kg, s.c) (41) |
| CIBP in athymic nude mice | Injection of Canine prostate carcinoma cells into the intramedullary space of the femur | Time spent in spontaneous guarding and flinching Thermal and mechanical sensitivity. | Antibodies against the nerve growth factor (NGF) (10 mg/kg, i.p.) Morphine sulfate (10 or 30 mg/kg, s.c) (42) |
| CIBP in C3H/HeJ mice | Injection of 2472 osteolytic sarcoma cells into the intramedullary space of the femur | Spontaneous flinching Flinching following normally non-noxious palpation Nocifensive behaviour scoring | Osteoprotegerin (daily s.c. injection of 50 μl containing 2.25 mg/ml Osteoprotegerin) (43) |
| CIBP in C3H/HeJ mice | Injection of 2472 osteolytic sarcoma cells into the intramedullary space of the femur | Mechanical hypersensitivity (von Frey) Spontaneous guarding | Morphine (15 mg/kg s.c.) (44) |
| CIBP in C3H/HeJ mice | Injection of NCTC 2472 tumour line into the intramedullary space of the femur | 52°C hot plate Guarding and flinching behaviours measurement Limb-use score Tactile hypersensitivity (von Frey) | Morphine (1, 3, 10, 20 mg/kg/day, s.c) (45) |
| CIBP in C3H/HeJ mice | Injection of NCTC 2472 tumour line into the intramedullary space of the femur | Spontaneous flinches Limb-use scoring Activity-related guarding | Osteoprotegerin (5 mg/kg s.c. daily from day 12 after sarcoma inoculation till day 21) (46) |
| CIBP in C3H/HeJ mice | Injection of NCTC 2472 tumour line into the intramedullary space of the femur | Guarding and flinching. Limb-use and rotarod tests. Touch-evoked pain (von Frey) Palpation-induced guarding Palpation-induced flinching. | Morphine sulfate (0.3–300 mg/kg i.p.) (47) |
| CIBP in C3H/HeJ mice | Injection of NCTC 2472 tumour line into the intramedullary space of the femur | Spontaneous flinching and guarding Palpation-evoked guarding and flinching Limb-use scoring | ABT-627 (a selective antagonist of endothelin receptor A) (10 mg/kg, i.p.) A-192621 (a selective antagonist of endothelin receptor B) (30 mg/kg, i.p.) (48) |
| CIBP in C3H/HeJ mice or B6C3-Fe-a/a mice | Injection of NCTC 2472 tumour line into the intramedullary space of the femur | Light palpation of the tumour followed by scoring of the nocifensive response | N/A (26) |
| CIBP in C3H/HeNCrl mice | Injection of NCTC 2472 tumour line into the intramedullary space of the femur | Spontaneous lifting behaviour Palpation-evoked lifting behaviour Limb-use during forced ambulation | Morphine sulphate (15 mg/kg, i.p.) (49) |
| CIBP in C3H/HeNCr mice | Injection of NCTC 2472 fibrosarcoma cells into and around the calcaneus | Mechanical hypersensitivity (von Frey) Heat hyperalgesia (Hargreaves’ test) | N/A (50) |
| CIBP in C3H/He mice | Injection of clone 2472 fibrosarcoma cells into the mouse calcaneus bone | Mechanical hyperalgesia (von Frey filaments) Cold hyperalgesia (3 ± 1°C cold plate) | N/A (29) |
| CIBP in C3H/He mice | Injection of clone 2472 fibrosarcoma cells into the mouse calcaneus bone | Mechanical sensitivity (von Frey test) | TNFR:Fc (i.pl. (0.001 pg to 1.0 ng/20 μl) or i.p. (100–500 μg/mouse) or intratumour (0 μg/20 μl/mouse) (51) |
| CIBP in C3H/HeJ mice | Injection of clone 2472 fibrosarcoma cells into and around the calcaneous bone | Mechanical sensitivity (von Frey) Cold hyperalgesia (2.5°C ± 1°C cold plate) | N/A (52) |
| CIBP in C3H/He mice | Injection of NCTC clone 2472 cells into the humerus | Measurement of forelimb grip force | WIN55,212-2 (1–30 mg/kg, i.p.) (53) |
| CIBP in C3H/HeJ mice | Injection of NCTC clone 2472 cells into the cavity of the humerus | Ambulation on a rotarod Assessing the grip force | Radiation Morphine-hydrochloride (5 mg/kg, i.p.) Ketorolac (30 mg/kg, i.p.) (54) |
| CIBP in C3H/He or B6C3/F1 mice | Implantation of NCTC 2472 sarcoma cells into the humeri (C3H/He) or melanoma cells (B6C3/F1 mice) | Grip force test Cutaneous hypersensitivity (von Frey) | Morphine (3–100 mg/kg, i.p.) (28) |
| CIBP in C3HHeJ mice | Injection of 2472 sarcoma cells into the intramedullary space of the femur | Palpation-induced flinches Limb-use score Limb-use while ambulating | Selective COX-2 inhibitor (chronic MF tricyclic, ∼30 mg/kg/day, p.o.) or (acute NS-398 (100 mg/kg, p.o) (55). |
| CIBP in immunocompromised C3H-SCID mice | Injecting 2472 sarcoma, B16 melanoma or C26 colon adenocarcinoma into the femur | Spontaneous guarding Guarding during forced ambulation on a Rotorod Guarding after innocuous palpation of tumour-bearing limb | N/A (38) |
| CIBP in Swiss CD1 mice | Injection of XC Rous sarcoma-virus-transformed rat fibroblast cells | Thermal hyperalgesia (55 ± 1°C hot plate) Mechanical hyperalgesia (Randall and Selitto) Capsaicin-Induced Licking | Morphine (1–10 mg/kg, i.p.) BQ-123 (10 nmol, i.pl.) BQ-788 (10 nmol, i.pl) (56) |
| CIBP in C3H/HeJ mice | Injection of NCTC 2472 cells intratibially | Thermal hyperalgesia (55 ± 1°C hot plate) Spontaneous pain [modified Dubuisson and Dennis method (57)] | Morphine (15 mg/kg, i.p) (58) |
| CIBP in C3H/HeJ mice | Injection of NCTC 2472 cells into the medullary cavity of the tibia | Thermal hyperalgesia (55 ± 1°C hot plate) | Morphine (10 nmol, s.c. over the tibial tumour mass) Loperamide (146 nmol, s.c. over the tibial tumour mass) (59) |
| CIBP in C3H/HeJ mice | Injection of SCC-7, squamous cell carcinoma cells into the thigh | Heat (radiant heat) Mechanical sensitivity (von Frey) Spontaneous pain (including lifting, licking, and flinching) | Capsazepine (10 or 30 mg/kg, i.p.) (60) |
| CIBP in C3H/HeJ mice | Injection of hepatocarcinoma cells, HCa-1 into the thigh or the dorsum of the foot | Mechanical sensitivity (von Frey test) Cold allodynia (acetone test) Heat hyperalgesia (radiant heat) | N/A (61) |
| CIBP in C3H/HeJ mice | Injection of hepatocarcinoma, hca-1 cells into the periosteal membrane of the foot dorsum | Mechanical sensitivity (von Frey) Cold sensitivity (acetone) Heat hyperalgesia (radiant heat) | Radiation (62) |
| CIBP in C3H/HeJ mice | Injection of hepatocellular carcinomahca-1 cells into the periosteal membrane of the foot dorsum | Mechanical sensitivity (von Frey test) Cold sensitivity (acetone) Heat hyperalgesia (radiant heat) | Radiation (63) |
| CIBP in C57BL/6 mice | The injection of Lewis lung carcinoma cells into the intramedullary space of the femur | Limb-use score Weight bearing | Nav1.7 knockout from DRG and sympathetic neurons. Ablation of Nav1.8-positive neurons (64) |
| CIBP in C57BL/6 mice | The injection of Lewis lung carcinoma cells into the intramedullary space of the femur | Limb-use scoring Weight-bearing Rotarod Mechanical sensitivity (von Frey) 50°C hot plate test Dry ice test | N/A (37) |
| CIBP in Sprague–Dawley rats | Injection of MRMT-1 rat mammary gland carcinoma cells into the medullary space of the proximal tibia | Cold bath test (4°C) Hot plate test (38°C for allodynia and 52°C for hyperalgesia) Mechanical hyperalgesia (Randall Selitto test) Thermal hyperalgesia (infrared beam) Tactile allodynia (von Frey test) Weight bearing test | Morphine (3 or 5 mg/kg, s.c.) Lacosamide (3, 10, 20, 30 or 40 mg/kg, i.p.) (65). |
| CIBP in Wistar rats | Implantation of Walker 256 carcinoma cells into the plantar surface of rat hind paw | Mechanical Hyperalgesia (Randall–Selitto Test) Mechanical sensitivity (von Frey) Spontaneous pain behaviour (lifting and licking of the affected paw) | Indomethacin (4 mg/kg, i.v.) Morphine (10 mg/kg, s.c.) (66) |
| CIBP in Sprague–Dawley rats | Injection of MRMT-1 tumour cells into the tibia | Weight-bearing Mechanical sensitivity (von Frey) | Lumiracoxib (10 and 30 mg/kg, p.o.) Valdecoxib (30 mg/kg, p.o.) (67) |
| CIBP in Wistar rats | Injection of 256 rat mammary gland carcinoma cells into the tibia | Limb-use score Mechanical sensitivity (von Frey) Hargreaves test Weight-bearing test | N/A (68) |
| CIBP in Sprague–Dawley rats | Injection of MRMT-1 rat mammary gland carcinoma cells into the tibia | Mechanical sensitivity (von Frey) Mechanical hyperalgesia (paw pressure) Overall daily activity | N/A (31) |
| CIBP in Sprague–Dawley rats | Injection of MRMT-1 rat mammary gland carcinoma cells into the tibia | Heat hyperalgesia (radiant heat) Grip force test Foot stamp test | Zoledronic acid (250 µg/kg/day, s.c.) (69) |
| CIBP in Sprague Dawley rats | Injection of MRMT-1 cell line into the tibia | Ambulatory-evoked pain (rotarod test) Mechanical sensitivity (von Frey) Cold allodynia (acetone) | Gabapentin (30 mg/kg, s.c. chronic) or (10, 30 or 100 mg/kg, s.c. acute) (70) |
| CIBP in Copenhagen rats | Injection of AT-3.1 prostate cancer cells in the tibia | Thermal hyperalgesia (radiant heat) Mechanical hyperalgesia (paw pressure) Mechanical sensitivity (von Frey) Spontaneous flinching | Morphine (5 mg/kg or 10 mg/kg, s.c.) (71) |
Animal models of non-bone cancer pain
Besides the models of cancer pain arising from bone, other animal models of primary cancers originating from different organs have been described, such as pancreatic cancer, squamous cell carcinoma and neuroma. One mouse model of pancreatic cancer involves the elastase 1 promoter-driven expression of the simian virus 40 large T antigen (72). In this model, pathological effects of these precancerous cells can be observed after 6 weeks, such as elevation in microvasculature density, the number of nerve growth factor (NGF) expressing macrophages and increased density of sensory and sympathetic fibers innervating the pancreas. Although these aforementioned changes would be expected to lead to severe pain in somatic structures like the skin, no apparent changes in pain-related behaviours, like morphine-reversible severe hunching and vocalisation, are observed in this model of pancreatic cancer until an advanced stage of disease after 16 weeks (72). These findings imply that a stereotypical series of pathological changes are present in both humans and mice as pancreatic cancer progresses. Although weight loss typically corresponds to disease progression, there is often a considerable delay from the onset of tumour growth to behaviours suggestive of pancreatic cancer pain (72). Clinical presentation of back and abdominal pain in pancreatic cancer is commonly reported at an advanced stage of disease in more than 80% of cases (73), but the underlying causes of the discrepancy between neuronal innervation and symptomatic pain in pancreatic cancer remain to be investigated.
Another preclinical model of pancreatic cancer that involves the implantation of SW 1990 cells into the pancreas of female BALB/c-nu mice carries several advantages, including reproducible transcriptional changes at the level of the dorsal horn in both mice and humans with pancreatic cancer (74). Pain-like behaviours in pancreatic cancer-bearing mice can be assessed by stimulating the abdomen mechanically (by von Frey hairs) to assess mechanical withdrawal thresholds and score hunching behaviours, as well as electrophysiologically record visceromotor responses from the rectus abdominis (74). An animal model of squamous cell carcinoma involves the injection of cancer cells into the subperiosteal tissue of the lower gingiva, which leads to elevated levels of calcitonin gene-related peptide, Substance P, P2X3 receptors and TRPV1 channels in the trigeminal ganglia, coinciding with the development of mechanical hypersensitivity and thermal hyperalgesia (75). Finally, the tibial neuroma transposition model involves the ligation of the tibial nerve and placement above the lateral malleolus—while not perfectly representative of the natural clinical course of disease progression, this model can be useful for mechanistic investigations of pain due to tumour-induced nerve injury (76, 77).
Patients with head and neck cancer experience pain early in the disease process, and orofacial pain is often the presenting symptom for oral squamous cell carcinoma (SCC). Schmidt and collleagues have pioneered the development of mouse models of oral cancer pain, either through orthotopic oral tissue injection of human SCC to produce operant nocifensive behaviours measured using the Dolognawmeter (to measure gnaw time) (78). Other work has used administration of SCC cells to the hindpaw to investigate mechanisms of mechanical allodynia (79). See Table 2 for a summary of different animal models of non-bone cancer pain.
Table 2.
Some of the animal models used to study pain in non-bone cancer and targets for analgesia.
| Murine model and strain | Method of induction of cancer pain model | Assays to assess pain behaviour | Analgesics tested (and reference) |
|---|---|---|---|
| A mouse model of pancreatic cancer (transgenic mouse) | Transgenic mouse expressing the simian virus 40 large T antigen under control of the rat elastase-1 promoter | Hunching behaviour Palpation-evoked vocalisation | Morphine sulfate (10 mg/kg, s.c) (72) |
| A rat model of Squamous cell carcinoma in Fisher rats | The inoculation of SCC-158 cells into the subperiosteal tissue of the rats on the lateral side of the lower gingiva | Mechanical sensitivity: von Frey (whisker-pad skin and submandibular skin) and dynamic plantar aesthesiometer (paw). Thermal sensitivity: 55 ± 0.5°C hotplate (whisker-pad skin and submandibular skin) and radiant heat (paw). | N/A (75) |
| A rat model of neuroma-induced pain in Sprague–Dawley rats | A neuroma is permitted to develop after the tibial nerve is ligated and positioned just superior to the lateral malleolus. | Neuroma tenderness (von Frey). Hindpaw mechanical hyperalgesia (von Frey). | Lidocaine injection (100 μl injection of 1% lidocaine with epinephrine, s.c.) Proximal tibial nerve transection (76) |
| Mouse models of pain in oral squamous cell carcinoma (SCC) in BALB/c nude mice | 50 μl of human SCC (cells for chronic pain, supernatant for acute pain) injected into the left lateral tongue. | Dolognawmeter (operant measure) | Soybean trypsin inhibitor (20 μg intratumour) (78) |
Animal models of cancer related neuropathic pain
Neuropathic pain is a key feature in some animal models of pain upon either cancer invasion or treatment with chemotherapy (80, 81). For the former, cancer cells are implanted in close proximity to nerves, e.g., sciatic nerve, and standardised behavioural assays measure changes in hindlimb sensitivity (81). Animal models of cancer invasion typically cause more profound neuronal damage than classic rodent models of neuropathic pain, such as the chronic constriction injury model, and the degree and effects of nerve compression after cancer appear mechanistically distinct (81).
Neurotoxicity is one of the key treatment-limiting side effects of chemotherapy, which can manifest as painful peripheral neuropathy or chemotherapy-induced neuropathic pain. Across classes of chemotherapeutic agents, the extent of polyneuropathy depends on the dose and length of treatment but is generally associated with an acute phase of allodynia and pricking dysaesthesia affecting the hands and feet in patients. Acute or persistent neuropathic pain can be reproduced by systemic administration of chemotherapeutic agents in rodents. Some studies also report the development of motor neuropathy, gait abnormalities and impaired rotarod performance (82), which mimic aspects of sensory impairment besides hypersensitivity that develops in chemotherapy-induced peripheral neuropathy (83). For example, daily intravenous administration of vincristine, a vinca alkaloid, elicits dose-dependent mechanical and cold (but not heat) hypersensitivity within 2 days (84–86) that is attenuated 2 weeks after cessation of treatment (84). Paclitaxel is a commonly used taxane in rodent models of chemotherapy-induced peripheral neuropathy to produce both thermal and mechanical hypersensitivity (87, 88). A recent study on the responses of 10 mouse strains to paclitaxel administration revealed that nearly all strains experienced mechanical allodynia and cold allodynia, including DBA/2J and C57BL/6J mice (89). Cisplatin is a platinum derivative that also results in numbness, tingling, as well as painful neuropathy in humans (90, 91). In rats, typically, three doses totaling 15 mg/kg are administered to produce mechanical allodynia and hyperalgesia lasting up to 15 days (92). The fast onset of neuropathic symptoms is a major benefit of this model (92). Additionally, while motor nerve conduction velocity is unaltered in electrophysiological studies, a considerable drop in sensory nerve conduction velocity can be detected (93). Lastly, preclinical studies using oxaliplatin-induced neuropathic pain have highlighted key mechanisms associated with cold allodynia that occur with chemotherapy administration. Mice administered 80 µg intraplantar oxaliplatin show a significant reduction in pain thresholds assessed using the cold plate test. Symptoms of cold allodynia become evident as early as 3 h after oxaliplatin administration (94). An important advantage of this model is its rapid onset resembling the rapid cold allodynia seen in patients with cancer treated using oxaliplatin (95). See Table 3 for a summary of different animal models of chemotherapy associated pain.
Table 3.
Some of the animal models used to study chemotherapy-associated pain and targets for analgesia.
| Murine model and strain | Method of induction of cancer pain model | Assays to assess pain behaviour | Analgesics tested (and reference) |
|---|---|---|---|
| Vincristine-induced neuropathy in Sprague-Dawley rats | Vincristine (100 μg/kg into a tail vein) administration on daily basis for 2 weeks. | Heat hyperalgesia (radiant heat) Mechanical hyperalgesia (Randall Selitto paw-withdrawal) Mechanical sensitivity (von Frey) Rotarod test for potential motor effects | DAMGO [(D-Ala2, N-MePhe4, Gly-ol)-enkephalin] (1 µg, i.d) (84) |
| Vincristine-induced neuropathy in Sprague-Dawley rats | Injection of Vincristine (50 or 75 μg/kg) into the tail vein of rats daily for 10 consecutive days. | Mechanical hyperalgesia (Randall-Selitto test) to measure vocalisation threshold Von Frey test. Heat hyperalgesia (radiant heat) Tail immersion test (42°C water bath) | N/A (96) |
| Vincristine-induced neuropathy in Sprague–Dawley rats | Injection of vincristine at a single dose of 50, 100 and 200 μg/kg, i.v) | Mechanical hyperalgesia [increasing mechanical force (20–160 g)] Mechanical sensitivity (von Frey) Rotarod test | Inhibitors of protein kinase Cε, A, G P42/p44-mitogen activated protein kinase inhibition Nitric oxide synthase inhibitors (all compounds i.d. 1 μg/paw) (97) |
| Vincristine-induced neuropathy in Sprague–Dawley rats | Vincristine is applied through jugular vein pump at a dose of 30 μg/kg/day | Thermal hyperalgesia (radiant heat) Mechanical hyperalgesia (Randall-Selitto test) Paw immersion in (4.5°C) water Mechanical sensitivity (von Frey test) | Dextromethorphan hydrobromide monohydrate (p.o.) Aspirin (p.o.) Ibuprofen (p.o.) Acetaminophen (p.o.) Carbamazepine (p.o.) Clonidine hydrochloride (i.p.) Morphine hemi[sulfate pentahydrate] (i.p.) Desipramine hydrochloride (i.p.) Gabapentin (p.o) Celecoxib (i.p.) Lamotrigine (p.o) (86) |
| Vincristine-induced neuropathic pain in | Vincristine was infused at a dose of 1–100 µg/kg/day for 14 days | Mechanical sensitivity (von Frey) Heat withdrawal threshold using lightbulb heat source | Morphine sulfate (5 mg/kg, i.p.) Lidocaine hydrochloride (45 mg/kg, i.p.) Mexiletine (30 mg/kg, i.p.) Tetrodotoxin (8 μg/kg, i.p.) Pregabalin (80 mg/kg, i.p.) (85) |
| Paclitaxel-induced neuropathy in CD1 mice | 21.6 mg/kg of paclitaxel (i.p.) for 6 consecutive days | Tail flick temperature | NGF (10 µg/gm, i.p., for 7 days) (98) |
| Paclitaxel-induced neuropathy in ddy mice | Paclitaxel injection (4 mg/kg, i.p.) | N/A | Gabapentin (3–30 mg/kg, i.p.) (99) |
| Paclitaxel-induced neuropathic pain in 129P3, A, AKR, C3H/He, C57BL/6, C57BL/10, CBA, DBA/2, RIIIS, and SM (all “J” substrains) mice | Several paclitaxel injections on days (1, 3, 5, and 7, i.p.). The total paclitaxel dose was 4 mg/kg | Mechanical sensitivity (von Frey test) Thermal hyperalgesia (Hargreaves’ test) Cold allodynia (acetone) | N/A (89) |
| Paclitaxel-induced neuropathy in Dark Agouti rats | Injection of paclitaxel at a dose of 9 mg/kg (i.p.) twice a week. Dosing continued until 20% weight loss is achieved. | Tail flick test Rotarod test Gait disturbance | Oral sodium glutamate (∼500 mg/kg/day, p.o.) (82) |
| Paclitaxel-induced peripheral neuropathy in Sprague–Dawley rats | 0.1, 0.5 or 1 mg/kg taxol (i.p, once a day for 2 weeks) | Mechanical hyperalgesia (Randall–Selitto test in the paw) Mechanical sensitivity (von Frey) Thermal sensitivity (Hargreaves’ test) | Pkcɛ-I inhibitor (1 μg/paw, i.d.) PKA inhibitor (1 μg/paw, i.d.) (100) |
| Cisplatin-induced neuropathy in Dark Agouti rats | Injection of cisplatin at a dose of 2 mg/kg (i.p.) twice a week. Dosing continued until 20% weight loss is achieved. | Tail flick test Rotarod test Gait disturbance | Oral sodium glutamate (∼500 mg/kg/day, p.o.) (82) |
| Cisplatin-induced neuropathy in Sprague-Dawley rats | Weekly injection of cisplatin (2 mg/kg, i.p.) for 10 weeks | Walking track | Decompressive surgery (101) |
| Cisplatin-induced neuropathy in Sprague-Dawley rats | Four to five cisplatin injections at 3 mg/kg at weekly intervals | Mechanical sensitivity (von Frey) Thermal sensitivity (Hargreaves’ test) | Morphine (0.3, 0.6 and 1 mg/kg s.c.) (102) Amitriptyline (30, 70 mg/kg i.p.) Meloxicam (5, 10 and 20 mg/kg i.p.) |
| Oxaliplatin-induced cold allodynia in albino Swiss mice | Singles injection of oxaliplatin (10 mg/kg, i.p.) | Cold plate test (1°C, 2.5°C and 4°C) | Amitriptyline (1, 2.5 and 10 mg/kg, i.p.) (103) |
| Oxaliplatin-induced cold allodynia in C57BL/6 background mice | Injection of 80 µg of oxaliplatin (i.pl.). | Cold plate test (5°C) | Deletion of Nav1.8 positive neurons (94) |
Mechanisms of cancer pain
Cancer-induced bone pain (CIBP)
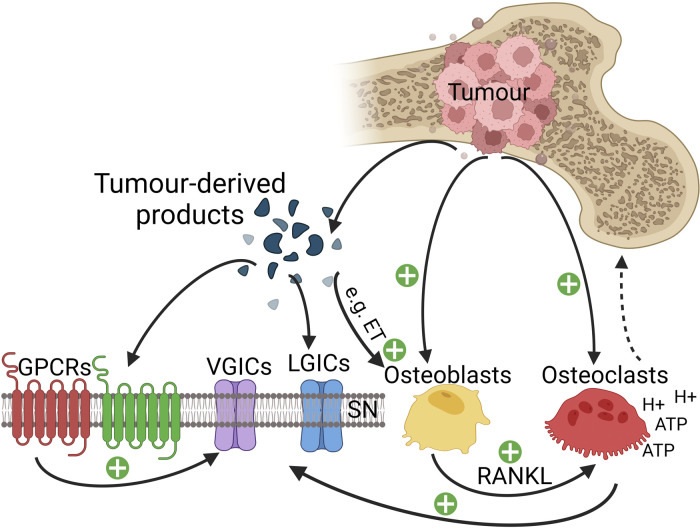
Paget's “seed and soil” hypothesis of the late 19th century was seminal to our current understanding that certain tumours exhibit a predilection for metastasis to specific organs (104). Bone is the optimal “soil” for metastatic cells of primary tumours, most commonly from breast, prostate myeloma, thyroid, lung and bladder cancer. Post-mortem examinations revealed that the incidence of bone metastases is around 70% for patients with breast or prostate cancer and 36% for patients with lung cancer (105). Bone metastases are the most common cause of cancer-related pain (105, 106) and are associated with poor prognosis and survival (107). Metastasis to bone disrupts skeletal homeostasis by disturbing the balance between osteoblastic bone formation and osteoclast-mediated bone destruction (108). Fenestrations in bone marrow sinusoids allow easy trafficking of hematopoietic cells but can also be permissive to metastatic invasion (109). Receptor activator of nuclear factor kappa-Β ligand (RANKL) is a chemotactic factor that promotes bone metastasis (110), and chemokine receptors such as CXCR4 (C-X chemokine receptor 4), which binds the survival chemokine stromal cell-derived factor 1 present on osteoblasts and bone lining cells, promote adhesion and metastasis within the bone microenvironment (111, 112). Within the bone, cancer cells directly compete with hematopoietic stem cells driving their terminal differentiation (113). In this microenvironment, bone-innervating neurons and cancer and tumour-associated stromal cells (including fibroblasts, endothelial cells, lymphocytes and bone marrow-derived cells, such as macrophages, neutrophils, mesenchymal stem cells and mast cells) can all contribute to CIBP through changes in bone homeostasis, structural and neurochemical reorganisation of sensory and sympathetic nerve fibres innervating bone, as well as the neurochemical reorganisation in the spinal cord. These processes highlight the importance of peripheral and central mechanisms driving the complex condition of CIBP that comprises inflammatory, neuropathic and cancer-specific mechanisms of nociceptive signalling. We discuss peripheral and central mechanisms below (see Figure 1).
Figure 1.
Cellular interactions in the bone microenvironment in CIBP. Tumour cells release endothelin (ET), which interacts with osteoblasts via their appropriate receptors to stimulate the proliferation of osteoblasts. Activated osteoblasts release receptor activator of nuclear factor-kappa-Β ligand (RANKL), which serves as a signal for osteoclast proliferation and maturation to enhance osteoclast-mediated bone matrix destruction. Osteoclasts generate adenosine triphosphate (ATP) and acidosis by releasing protons, resulting in the activation of various receptors and ligand-gated ion channels (LGICs) like P2X receptors, transient receptor potential V1 receptors and acid-sensing ion channels type 3 expressed on bone innervating sensory neurons. Tumour cells, stromal cells and activated immune cells release a variety of mediators (such as endothelin, the nerve growth factor, protons, and pro-inflammatory cytokines) that activate their respective receptors expressed on sensory neurons and thereby initiate the detection of noxious stimuli. GPCRs can sometimes indirectly sensitise various voltage-gated ion channels (VGICs) expressed on sensory neurons leading to a further potentiation of nociceptive signalling to the spinal cord. Osteolytic cancers (like breast cancer) activate osteoclasts, while osteosclerotic cancers (like prostate cancer) activate osteoblasts leading to a further potentiation of pain signal transmission.
Acidosis is thought to be a key mechanism driving CIBP and is largely driven by disseminated tumour cells that dysregulate bone remodelling through osteomimicry of osteoblast and osteoclasts (114–116). The disruption of skeletal homeostasis and acidic bone microenvironment can contribute to peripheral sensitisation through the activation of acid-sensing ion channels (ASICs) and transient receptor potential (TRP) channels. In the Warburg effect, cancer cells tend to undergo anaerobic respiration even in the abundance of oxygen, unlike normal cells that mainly undergo aerobic respiration in the abundance of oxygen and shift to anaerobic respiration when there is a shortage of oxygen supply (117). Among the products of anaerobic respiration is lactic acid (at physiological pH, lactic acid deprotonates to form lactate and protons), which causes acidosis. Cancer-induced acidosis is enhanced in bone cancers because the bone is a hypoxic tissue (118). In addition, tumour cells activate osteoclasts, which in turn cause bone degradation by releasing protons to solubilise the mineralised bone matrix (119). Upon the physiological activation of osteoclasts, the release of acids by osteoclasts during bone resorption is restricted to the bone matrix due to the tightly sealed sac called the resorption lacuna (120). Typically in bone cancer the number and activity of osteoclasts increase dramatically, thereby disrupting this tight regulation and resulting in the leakage of protons that can amplify acidity levels of the bone marrow. The bone marrow itself is richly innervated with nociceptors expressing ASICs and TRP channels—especially TRPV1—that are important sites of neuronal activation by protons (69, 121–124).
In addition to acidosis, several mediators released by cancer cells and their associated stromal cells contribute to CIBP. These include NGF and interleukin (IL)-1β (125), which can contribute to CIBP both directly and indirectly. For instance, IL-1β enhances the expression of cyclooxygenase (COX)-2 by macrophages, in turn amplifying prostaglandin synthesis. These prostaglandins can sensitise the primary afferent neurons by binding the prostanoid receptors expressed on terminals of bone innervating neurons (126, 127). Similarly, the production of NGF by cancer cells in the bone (e.g., derived from primary tumours of the breast and prostate) can lead to sensitisation of sensory neurons directly by increasing the expression ion channels linked to pain signal transduction and transmission. These include the TRPV1 channel, which is of particular interest in CIBP given the strong acidosis that characterises this painful condition (128). Moreover, in the spontaneous osteosarcoma canine model, TRPV1 blockade attenuates hypersensitivity suggesting it may be a potential analgesic target candidate in CIBP (122). NGF can also enhance the production and release of TNF-α, IL-6, IL-1β and prostaglandin (PG)E2 by macrophages (129). TNF-α is known to exert pro-nociceptive actions in animal models of chronic pain and can is targeted for pain relief in rheumatic disease (130). The peripheral pro-nociceptive actions of TNF-α are evident from the observation that intraplantar, intradermal, endoneurial or intramuscular administration of TNF-α induces thermal hyperalgesia and mechanical allodynia (131–135). In addition, TNF-α affects several ion channels like TRPV1, sodium and potassium channels (136–138) and results in the spontaneous firing of primary sensory neurons (139, 140). In preclinical models of CIBP, the administration of etanercept [a humanised soluble recombinant TNF receptor fusion protein (141)] was found to attenuate the thermal and mechanical allodynia in bone cancer-bearing mice (142). Additionally, blockade of the interaction between NGF and its receptor Tropomyosin receptor kinase A (TrkA) reduces pain-like behaviour in a mouse model of CIBP, with analgesic effects that are superior to morphine (143). Furthermore, several factors at the site of bone metastasis, such as reactive oxygen species (ROS), immune cell infiltration and activation, as well as tumour-induced cytotoxicity, result in the production of adenosine triphosphate (ATP) following the death of bone marrow cells. When ATP is released, it binds its receptor P2X3 on sensory neurons leading to their activation and subsequent sensitization (125). The blockade of P2X3 receptors can attenuate pain behaviours in a rat model of CIBP (144).
The neuropathic pain component of CIBP can be driven by increased intraosseous pressure, nerve sprouting and direct nerve injury. In humans, increased innervation density is also observed at sites of active bone remodelling, supporting the importance of neural regulation of skeletal remodelling and pain (145). Bone cancer pain, similar to intraosseous engorgement syndrome, produces intraosseous pressure within the bone microenvironment, which can sensitise primary afferents through activation of mechanoreceptors (146) and mechanotransducing osteocytes (147). Moreover, CIBP is characterised by the sprouting of sensory and sympathetic fibres, which has been shown to be driven by an NGF-dependent process. The requirement of NGF-TrkA signalling in bone innervating neurons for endochondral ossification and vascularisation, as well as bone formation upon mechanical loading, is well established (148, 149). In preclinical models of CIBP, prophylactic antibody-based blocking of NGF prevents ectopic sprouting and neuroma formation (150). The ablation of capsaicin-sensitive sensory neurons also results in loss of bone mineral density in adult rats (151). At the level of the peripheral somata, biomarkers that are indicative of nerve injury can also be detected, including cyclic activating transcription factor 3 (ATF3) expression. Spinal cord compression occurs in about 5% of patients with metastatic cancer, mainly presenting as back pain (152), and in animal models, spinal cord compression readily triggers mechanical hyperalgesia in the fore and hind limbs (153). Macrophage infiltration into peripheral sensory ganglia is also commonly observed in nerve injury models and studies highlight the importance of this neuro-immune interface in the development of CIBP (154).
At the level of the spinal cord, CIBP modulates synaptic plasticity between the peripheral neurons and second-order neurons, as observed through increased neuronal excitability measured with elevated expression of c-Fos, the internalisation of substance P, the rise in the expression of dynorphin (a pro-nociceptive opioid) and a significant activation and elevation in astrocytes and microglia (26, 155). In addition, CIBP has been shown to increase the proportion of the wide dynamic range to nociceptive-specific neurons in the superficial laminae of the dorsal horn in rats (156). It was reported that gabapentin can re-establish the typical ratio of wide dynamic range neurons to nociceptive-specific neurons, but long-term use of morphine maintains allodynia and fails to correct the pathophysiological phenotype of superficial dorsal horn neurons (157). Descending modulatory circuits also regulate spinal excitability in CIBP; 5-hydroxytryptamine type 3 (5-HT3) receptor antagonists can diminish the hyperexcitability of lamina I neurons in rodents with CIBP through the blockade of a descending serotonergic facilitatory drive (158). Other studies report an important role for amplified excitatory neurotransmission that may underlie enhanced spinal cord plasticity in CIBP; spinal glial cells secrete IL-1 that causes hyperalgesia by phosphorylating the NR1 subunit of N-methyl-D-aspartate receptor (NMDA) receptors (159). Moreover, spinal NR2B expression is increased in CIBP, and its specific inhibition prevents the induction of mechanical and thermal hypersensitivity (160). Due to hypertrophy of astrocytes and the subsequent decline in glutamate reuptake transporters, glutamate concentrations are also elevated in CIBP, which leads to excitotoxicity (161). Mice with CIBP also exhibit elevated amounts of dynorphin in the dorsal horn (26), which causes long-lasting pain through activation of NMDA receptors instead of opioid receptors (162).
Chemotherapy-induced neuropathic pain
Chemotherapy-induced neuropathic pain has a detrimental impact on the quality of life of patients during and after chemotherapy treatment (163). Because chemotherapeutic agents do not normally cross the blood-brain barrier, neuropathies are restricted to peripheral sensory and/or motor neurons, leading to a reduction in two-point discrimination and proprioception, as well as cold allodynia, myalgia and pain in extremities (164). The severity and duration of neuropathy are determined by the class of the chemotherapeutic agent used, the total duration of administration, as well as the cumulative dose administered. If the cell body is spared and a sufficient time-period for recovery is allowed before subsequent drug administration, the peripheral nervous system regenerates rapidly after the cessation of chemotherapy treatment. Still, up to one-third of patients experience damage lasting more than 6 months after cessation of a chemotherapy course (165). How do chemotherapeutic agents predominantly cause sensory neuropathy while leaving the motor neurons unaffected, even though motor neurons have axons that are as long as those of sensory counterparts and have extensive microtubule networks? And why are adult postmitotic sensory neurons preferentially harmed by chemotherapy drugs that are meant to target fast-dividing tumour cells? One explanation for this latter susceptibility with vinca alkaloids and taxanes is that these classes of chemotherapy drugs interfere with the stability of microtubules that are necessary for the axonal transport of chemicals and growth factors required for normal nerve function in sensory neurons. Unfortunately, this rationale does not apply to platinum-based chemotherapy drugs that generate DNA adducts in the nucleus but also injure sensory neurons to trigger chemotherapy-induced neuropathic pain (163, 166).
Chemotherapeutic agents with a high incidence of chemotherapy-induced neuropathic pain include paclitaxel, oxaliplatin and vincristine. Studies from animals and humans indicate that these agents build up in peripheral sensory ganglia and, to a lesser extent, in peripheral nerves (167–169). The neurotoxic effects of these classes of chemotherapeutic agents lead to cell death and neuronal degeneration. Expression of ATF3 in DRG neurons is significantly increased with administration of paclitaxel, and the same neurons also exhibit a deposition of neurofilaments and a translocation of their nuclei towards the periphery. Dorsal roots of rats receiving paclitaxel also show substantial axonal degradation and hypomyelination (170). Moreover, exposure to NGF attenuates some neurotoxic effects triggered by paclitaxel in CD1 mice, including the release of neuropeptides in DRG neurons (98). Apoptosis of DRG neurons is thought to be partially responsible for chemotherapy-induced neuropathy, and a high dose of NGF can prevent DRG apoptosis induced by cisplatin (171, 172). Chemotherapeutic agents have also been shown to increase the generation of ROS, which impairs mitochondrial electron transport chains, and disrupts ATP synthesis in the DRG neurons (173–177). These findings support the role of mitochondrial stress pathways in the neurotoxic effects of chemotherapeutic agents.
Ion channels have also been linked to mechanisms of chemotherapy-induced neuropathic pain. Rat studies demonstrate that paclitaxel and vincristine administration enhance the expression of the calcium channel alpha2delta-1 subunit in the dorsal horn of the spinal cord. Moreover, ensuing mechanical hypersensitivity is susceptible to attenuation by repeated gabapentin-dosing, which is also associated with a decrease in the expression of the spinal alpha2delta-1 subunit (176). Previous work has also shown an important role for tetrodotoxin (TTX)-sensitive sodium channels in chemotherapy-associated pain in mice. Acute subcutaneous administration of TTX at doses as low as 1 or 3 mg/kg diminished mechanical allodynia in paclitaxel-treated mice, while cold allodynia and heat hyperalgesia were attenuated with higher doses (3 or 6 mg/kg) (175). The antagonist of TRPA1 channels HC-030031 partially attenuated paclitaxel-evoked mechanical allodynia (174), whilst co-administration of HC-030031 and HC-067047 (TRPV4 antagonist) reversed paclitaxel-induced mechanical allodynia entirely (173) in rodents. Furthermore, a key mechanism of cold allodynia induced by oxaliplatin administration is the activation of “silent cold-sensing neurons” that express the voltage-gated sodium channel Nav1.8 (94, 178). Oxaliplatin treatment in mice with diphtheria toxin-ablated Nav1.8-positive neurons failed to exhibit cold allodynia compared to wild-type controls (94).
Distinct effects of different classes of chemotherapeutic agents are less studied. However, it is known that paclitaxel and vincristine-induced neuropathy trigger significant inflammatory processes which are less evident with oxaliplatin-induced neuropathy, mainly arising from the enhanced release of proalgesic mediators such as TNF and IL-1β by activated microglia, astrocytes and satellite glial cells within the dorsal horn of the spinal cord (179). The mechanism of action of vinca alkaloids that involves the prevention of microtubule formation by binding tubulin has also been shown to affect micro-tubuli, causing oedema of axons in the peripheral nervous system (163). Paclitaxel administration is also associated with a significant increase in macrophage activation and augmented staining for glial fibrillary acidic protein (GFAP). Following paclitaxel administration, satellite cells are reported to be tightly packed in “Nodules of Nagoette” that serve as a “tombstone” for the DRG neuron whose cell body they formerly encircled (180).
Mechanisms of pain in non-bone cancers
In pancreatic cancer, pain is the third most prevalent complaint among patients diagnosed with pancreatic cancer after weight reduction and jaundice (181). At the time of diagnosis, more than one-third of patients complain of abdominal discomfort and are already at an advanced stage of disease, but with disease progression, pain becomes severe in more than half of patients diagnosed with pancreatic cancer (182). Pain reports in recently diagnosed patients with pancreatic cancer can also predict survival and resectability, where preoperative pain is linked with a poor prognosis and a greater likelihood of recurrence (183). As a consequence of late diagnoses, the typical survival time of patients with pancreatic cancer ranges between 6 and 9 months, with the 5-year survival rate being less than 5% (184). Deciphering mechanisms that suppress nociceptive signalling in the early stages of pancreatic cancer and/or amplify nociceptive signalling in advanced disease is critical for improving the diagnosis, treatment and care of patients with pancreatic cancer.
Perineural invasion is a key feature of pancreatic cancer, which is enabled by the low resistance of the perineural space as well as the ideal milieu possessing chemoattractants and growth factors (such as transforming growth factor-alpha, epidermal growth factor receptor, and neural cell adhesion protein) to recruit cancer cells and promote their proliferation (185–187). A recent study showed that pancreatic cancer cells derived from patients had higher levels of TRPV1 gene expression with a downstream effect of the enhanced release of neuropeptides and augmented neurogenic inflammation (188). In mouse models of pancreatic cancer, extensive sprouting of sensory and sympathetic fibres is also detected (72) and partly attributed to the high levels of NGF released by the cancer cells and/or the inflammatory cells (187). Specifically, mice develop increased microvascular density, NGF-expressing macrophages and sensory and sympathetic innervation to the pancreas at 6 weeks following the induction of the pancreatic cancer model—all pathological events that are linked to precancerous cellular abnormalities (72, 189). Despite early changes in cell and tissue composition of the pancreatic microenvironment, pain-like behaviours are only detected after 16 weeks of age when pancreatic cancer is at an advanced stage, similar to clinical reports of pain in patients at advanced stages of the disease. Some studies suggest that regulation of nociceptive input by the descending opioidergic controls contributes to the slow evolution of tissue injury (190, 191) and that endogenous opioids may mask the full expression of pain at the early stages of disease (192). When naloxone or naltrexone were given subcutaneously to mice with early- and mid-stage pancreatic cancer, behaviours associated with pain were observed in these mice, while the healthy littermate controls failed to demonstrate pain behaviours (189). Unmasking of endogenous opioid regulation of pain behavior has also been observed in a rat model of prostate cancer induced bone pain, as well as a rat model of breast cancer induced bone pain (193, 194). A salient point is that this opioid-based un-masking of pain only occurs with opioid antagonists penetrating the blood-brain barrier, but not with peripherally-restricted opioid antagonists (192).
Visceral pain in pancreatic cancer can be caused by pancreatic neuropathy driven by cancer cells that infiltrate the perineurium of local intrapancreatic nerves (195). It is also thought that the initiation and maintenance of pain after pancreatic cancer is through neurogenic inflammation (187). In addition, several genes shown to be linked to pain are upregulated in the dorsal horn of the spinal cord in murine models of pancreatic cancer, such as Ccl12, Pin1 and Notum (74). The palmitoleoyl-protein carboxylesterase encoded by Notum is implicated in the Wnt signalling-mediated initiation and maintenance of neuropathic pain (196). Moreover, mRNA levels of Ccl12 increase by up to 35-fold in the prostate of mice with experimental autoimmune prostatitis (a model of chronic pelvic pain syndrome) (197).
In oral SCC, patients exhibit high levels of ET-1 in the cancer microenvironment, which has been shown to correlate with functional pain in response to mechanical stimulation (198, 199). Protein and mRNA levels of NGF are also significantly higher in patients with oral cancer and in oral SCC culture (200). Other studies have linked protease-activated receptor 2 (PAR2) to cancer pain (201). For instance, the supernatant of human oral SCC cells contains proteases that can activate and sensitise PAR2 expressing-sensory neurons (201). Injecting this supernatant (without cancer cells) in mice results in a severe and protracted mechanical allodynia. Analgesic approaches like serine protease blockade or mast cell depletion eliminate or lessen this nociceptive effect, respectively. Moreover, PAR2 knockout mice do not display nociceptive behaviours following exposure to SCC cell supernatant. Patients with oral cancer may develop mechanical allodynia due to the constant production of serine proteases from malignant as well as non-malignant cells within the tumour microenvironment. In addition, activating PAR2 sensitises TRPV1 and TRPV4 receptors on nociceptive afferents causing mechanical allodynia and thermal hyperalgesia, respectively (202).
Pharmacological interventions to treat cancer pain
The efficacy of pain management in cancer is limited by the multidimensional aspects of the pathophysiology of cancer, such as widespread localisation of metastases, skeletal-related events (SREs) or due to severe systemic side effects of chemotherapy treatment (203). Gabapentinoids and antidepressants are common first and second line treatments for treatment of neuropathic pain syndromes and indicated also for cancer pain (204), but drugs that act on peripheral tissues would be preferable due to mechanisms involved in the initiation of pain and primary afferent sensitisation. The added attractive benefit of targeting the peripheral nervous system in cancer pain states is the obvious circumvention of central side effects. Here we provide an overview of some conventional treatments and potential new targets for treating cancer pain states.
Opioids
Opioids remain the principal treatment option for intractable malignant pain by acting on peripheral and central nervous system sites, i.e., through inhibition of presynaptic release of neurotransmitters from primary afferent terminals to induce postsynaptic hyperpolarisation of interneurons in the dorsal horn, as well as engaging top down opioidergic controls from higher centres (205, 206). Strong immediate-release opioids are recommended as rescue medication for episodes of breakthrough pain. However, preclinical studies suggest that morphine is less effective in treating bone cancer pain compared to other painful conditions (41, 47), possibly due to decreased expression of μ-opioid receptors (MORs) in both DRG and superficial dorsal horn neurons with disease progression (207, 208). Moreover, opioid treatment in CIBP may also be linked to disease progression, as observed in mice administered morphine that demonstrated accelerated sarcoma-induced bone pain, bone loss and fractures (45). Altered expression of MORs in CIBP can also be reversed with anti-NGF in rats (209).
Agents targeting bone resorption
SREs such as pathological fractures, hypercalcemia of malignancy, and bone marrow failure/leukoerythroblastic anaemia, among others, are common complications of bone metastases. The occurrence of SREs in CIBP provides the rationale for bone targeting agents to manage CIBP and to reduce the occurrence of SREs by reducing bone resorption (210). Besides bone cancer, other painful syndromes such as osteoporosis and fracture repair are also associated with increased bone resorption (37). Bisphosphonates and Denosumab are osteoclast targeting molecules that inhibit bone resorption. Bisphosphonates have a phosphorus-carbon-phosphorus that enable resistance to hydrolysis; nitrogen-containing bisphosphonates prevent prenylation of small guanosine triphosphate binding proteins that are essential for osteoclast function and survival (211), and non-nitrogen containing bisphosphonates are metabolised as ATP analogues to induce osteoclast apoptosis (212). The human monoclonal antibody Denosumab targets RANKL to prevent the development, activation and survival of osteoclasts (213). Moreover, IL-6 and TNF-α can induce osteoclastogenesis and bone erosion through a non-canonical pathway, which is independent of the activation of RANK (214).
Anti-NGF
In animal models of CIBP, administration of anti-NGF neutralising antibodies dramatically reduces cutaneous and skeletal pain (215–217) by preventing ectopic sprouting (150) and reducing loss of bone integrity associated with CIBP (218). In non-cancer skeletal pain models, anti-NGF therapy has shown promising results, e.g., in mice with femoral fracture, anti-NGF therapy reduces pain behaviours without affecting bone healing (219). In a murine model of autoimmune arthritis, anti-NGF neutralising antibodies reduce hyperalgesia and cachexia with no effect on joint destruction and gross inflammation (220). Anti-NGF therapy may reduce hyperalgesia through the re-establishment of homeostatic MOR expression at the level of DRG and dorsal horn, where its anti-nociceptive effects can be reversed with naloxone pre-treatment (209). In humans, several monoclonal antibodies that bind NGF (including tanezumab, fulranumab, and fasinumab) have been used in clinical studies in a range of chronic pain conditions such as osteoarthritis [for a comprehensive review, see (221)]. A phase 2 trial investigating the analgesic efficacy of tanezumab as add-on therapy to opioid medication in patients with metastatic bone pain has recently been completed, and previous randomised control trials showed that tanezumab was shown to have greater analgesic efficacy in patients with lower baseline opioid use and/or higher baseline pain (222). Although tanezumab has been tested as a potential analgesic for patients with osteoarthritis, it did not secure FDA approval due to safety concerns linking use of NGF inhibitors to accelerated joint damage, and publication of NICE guidelines for the use of tanezumab to treat moderate-to-severe osteoarthritis pain is currently suspended.
Endothelins
The family of endothelins (ET) consists of ET-1, ET-2 and ET-3 peptides that act on ETA and ETB G-protein-coupled receptors (223, 224). ET-1 increases intracellular calcium in peripheral sensory neurons and activates PKC-ε, leading to phosphorylation and activation of TRPV1 channels expressed on nociceptive C-fibres (225). In addition to activating TRPV1 channels, ET-1 also modulates the activity of TTX-resistant sodium channels (226), likely through PKC (227). ET-1 increases the release of neuropeptides and glutamate from isolated sensory neurons through an ETA-dependent increase in intracellular calcium (228, 229). ET-1 also modulates N and L-type calcium channels in a biphasic manner; initially, ET-1 slows down the activity of these calcium channels and following that causes long-lasting facilitation (230). The effect of ET-1 on the membrane potential is also biphasic as ET-1 initially causes depolarisation along with non-selective inward cationic currents (mostly calcium-mediated) followed by hyperpolarisation (probably as a result of calcium-activated outward potassium currents) (231). Furthermore, the release of calcium ions from intracellular stores contributes to the ET-1-mediated increase of intra-neuronal calcium ions concentration (229, 232). ETB receptors are primarily expressed in DRG satellite cells and ensheathing Schwann cells (233), where it triggers the production and release of PGE2 (234). ETB receptors also enhance the release of β-endorphin from keratinocytes and accordingly generate a local analgesia (235). ETA receptor activation leads to excitation of small-to-medium diameter DRG neurons (233), partly through the ability of ET-1 to activate voltage-gated sodium channels (226). According to (226), ET-1 predominantly activates TTX-resistant sodium channels on nociceptors by enabling these channels to open at more negative membrane potential. In vivo injection of ET-1 close to nerves enhances their excitability. In contrast, TTX-sensitive sodium channels are not affected by ET-1 (226). In addition, ET-1 represses currents generated by the outward delayed rectifier potassium channels in the vast majority of sensory neurons (236). ET-1-mediated suppression of outward delayed rectifier potassium currents combined with the activation shift that ET-1 causes on TTX-resistant sodium current greatly enhances the excitability of neurons (236). Besides the mechanisms mentioned above, ET-1 is of particular interest in CIBP for its ability to activate osteoblasts. In turn, osteoblasts can release RANKL, which can cause the activation and differentiation of pre-osteoclasts into mature osteoclasts leading to substantial bone degradation and acidosis-mediated pain (237) (see Figure 1). Due to its strong involvement in CIBP, ET-1 was tested as a potential target in preclinical models of CIBP. Another study showed that mice injected with 2472 sarcoma cell lines possess an increased level of ET-1 in the plasma compared to the controls (48). In the same study, antagonising ETA receptors reduced pain-associated behaviour in cancer-bearing mice, including both spontaneous and movement-evoked pain; in contrast, antagonising ETB receptors exacerbated pain-like behaviour in the CIBP mice. Similar promising results were obtained when ETA receptors were targeted in further preclinical investigation CIBP mechanisms (56).
Other excitatory mediators
ATP is readily generated during inflammation and is abundantly expressed in malignant tissues (238). ATP receptors are known as purinergic receptors; P2Y receptors are members of the GPCR superfamily and P2X receptors are ligand-gated ion channels (239). Under physiological settings, it was discovered that cutaneous nerves have high concentrations of P2X3, but the periosteum and mineralised bone are nearly devoid of P2X3 (240). In line with these findings, it was demonstrated in a mouse model of CIBP (characterised by significant skin and skeletal hypersensitivity) that blocking P2X3 receptors with a monoclonal antibody reduces skin hypersensitivity (as measured by the von Frey test) while leaving skeletal pain-like behaviours largely unaffected (215). Another study reported a 5-fold increase in the expression of P2X3 in CGRP-positive epidermal nerve fibres in mice with osteolytic fibrosarcoma compared to control animals (241). Similarly, it was shown that the DRG neurons that innervate the rat tibia express P2X3 de novo in rat models of CIBP and systemic administration of the P2X2/3 antagonist AF-353 alleviates mechanical hypersensitivity without affecting cancer-induced bone deterioration. Not only does ATP contribute to pain peripherally, but it also has central effects demonstrated by in vivo recordings of dorsal horn neuronal excitability where intrathecal AF-353 decreases evoked action potential firing in significantly in a dose-dependent manner (144). For chemotherapy-induced neuropathy, preclinical studies suggest that glutamate can serve a protective function against neurotoxicity caused by cisplatin or paclitaxel, as measured by a reduction in proprioceptive loss and compromised performance in the rotarod test during dark cycles of rodents (82). Other protective strategies for cisplatin-induced neuropathy include ORG 2766 (93) and the recombinant human glial growth factor 2 (242).
Conclusion
Cancer pain arising from disease pathology and/or cancer treatments will increase in prevalence with increasing and prolonged survival rates. Preclinical rodent models of cancer-induced bone pain and of chemotherapy induced neuropathy address prevalent chronic pain syndromes that are experienced by patients with bone metastases or undergoing chemotherapy treatments. Cancer pain is a complex condition driven by inflammatory, neuropathic and cancer-specific mechanisms. Peripheral cross talk between tumour cells, non-neuronal cells and neurons is a key process for the induction and maintenance of cancer pain states. Changes in the tumour microenvironment, such as bone remodelling and acidosis also contribute to the sensitisation of peripheral sensory neurons. Conventional pain management still relies on opioids and standard conventional first- and second-line analgesics that are normally indicated for neuropathic pain states. Improved understanding of mechanisms specific to cancer pain states is necessary to highlight new targets for pain relief. Modelling the heterogeneity of sensory dysfunction across different types of cancer pain is one of the biggest challenges in preclinical investigations. Future studies that use animal models of distinct cancer pain states to investigate the peripheral crosstalk between neuronal and non-neuronal cells will provide valuable insight into pathophysiological mechanisms of cancer pain.
Acknowledgements
Figure 1 was created through BioRender.com.
Funding
Authors are supported by the European Commission’s Horizon 2020 Research and Innovation Programme, Marie Skłodowska-Curie grant (814244), the Wellcome Trust (200183/Z/15/Z), Versus Arthritis UK (21734) and Cancer Research UK (185341).
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Teunissen SC, Wesker W, Kruitwagen C, de Haes HC, Voest EE, de Graeff A. Symptom prevalence in patients with incurable cancer: a systematic review. J Pain Symptom Manage. (2007) 34(1):94–104. 10.1016/j.jpainsymman.2006.10.015 [DOI] [PubMed] [Google Scholar]
- 2.van den Beuken-van Everdingen MHJ, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. High prevalence of pain in patients with cancer in a large population-based study in The Netherlands. Pain. (2007) 132(3):312–20. 10.1016/j.pain.2007.08.022 [DOI] [PubMed] [Google Scholar]
- 3.van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol. (2007) 18(9):1437–49. 10.1093/annonc/mdm056 [DOI] [PubMed] [Google Scholar]
- 4.Organization WH. Cancer pain relief: With a guide to opioid availability. Geneva: World Health Organization; (1996). [Google Scholar]
- 5.Nabal M, Librada S, Redondo MJ, Pigni A, Brunelli C, Caraceni A. The role of paracetamol and nonsteroidal anti-inflammatory drugs in addition to WHO step III opioids in the control of pain in advanced cancer. A systematic review of the literature. Palliat Med. (2012) 26(4):305–12. 10.1177/0269216311428528 [DOI] [PubMed] [Google Scholar]
- 6.Caraceni A, Hanks G, Kaasa S, Bennett MI, Brunelli C, Cherny N, et al. Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC. Lancet Oncol. (2012) 13(2):e58–68. 10.1016/S1470-2045(12)70040-2 [DOI] [PubMed] [Google Scholar]
- 7.Goldstein NE, Morrison RS. Evidence-based practice of palliative medicine. Philadelphia: Elsevier Saunders; (2013). [Google Scholar]
- 8.McNicol E, Strassels S, Goudas L, Lau J, Carr D. Nonsteroidal anti-inflammatory drugs, alone or combined with opioids, for cancer pain: a systematic review. J Clin Oncol. (2004) 22(10):1975–92. 10.1200/JCO.2004.10.524 [DOI] [PubMed] [Google Scholar]
- 9.Smith EM, Pang H, Cirrincione C, Fleishman S, Paskett ED, Ahles T, et al. Effect of duloxetine on pain, function, and quality of life among patients with chemotherapy-induced painful peripheral neuropathy: a randomized clinical trial. J Am Med Assoc. (2013) 309(13):1359–67. 10.1001/jama.2013.2813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mishra S, Bhatnagar S, Goyal GN, Rana SP, Upadhya SP. A comparative efficacy of amitriptyline, gabapentin, and pregabalin in neuropathic cancer pain: a prospective randomized double-blind placebo-controlled study. Am J Hosp Palliat Care. (2012) 29(3):177–82. 10.1177/1049909111412539 [DOI] [PubMed] [Google Scholar]
- 11.Bates D, Schultheis BC, Hanes MC, Jolly SM, Chakravarthy KV, Deer TR, et al. A comprehensive algorithm for management of neuropathic pain. Pain Med. (2019) 20(Suppl 1):S2–s12. 10.1093/pm/pnz075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lu W, Dean-Clower E, Doherty-Gilman A, Rosenthal DS. The value of acupuncture in cancer care. Hematol Oncol Clin North Am. (2008) 22(4):631–48. 10.1016/j.hoc.2008.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amr YM, Makharita MY. Neurolytic sympathectomy in the management of cancer pain-time effect: a prospective, randomized multicenter study. J Pain Symptom Manage. (2014) 48(5):944–56.e2. 10.1016/j.jpainsymman.2014.01.015 [DOI] [PubMed] [Google Scholar]
- 14.Carlson CL. Effectiveness of the world health organization cancer pain relief guidelines: an integrative review. J Pain Res. (2016) 9:515–34. 10.2147/JPR.S97759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bandieri E, Romero M, Ripamonti CI, Artioli F, Sichetti D, Fanizza C, et al. Randomized trial of low-dose morphine versus weak opioids in moderate cancer pain. J Clin Oncol. (2016) 34(5):436–42. 10.1200/JCO.2015.61.0733 [DOI] [PubMed] [Google Scholar]
- 16.Scarborough BM, Smith CB. Optimal pain management for patients with cancer in the modern era. CA Cancer J Clin. (2018) 68(3):182–96. 10.3322/caac.21453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barbera L, Taylor C, Dudgeon D. Why do patients with cancer visit the emergency department near the end of life? Can Med Assoc J. (2010) 182(6):563–8. 10.1503/cmaj.091187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mayer DK, Travers D, Wyss A, Leak A, Waller A. Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol. (2011) 29(19):2683–8. 10.1200/JCO.2010.34.2816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Batalini F, Gomes M, Fábio I, Kuwae F, Macanhan G, Pereira JLB. Cancer complaints: the profile of patients from the emergency department of a Brazilian oncology teaching hospital. F1000Res. (2017) 6:1919. 10.12688/f1000research.12632.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Glare PA, Davies PS, Finlay E, Gulati A, Lemanne D, Moryl N, et al. Pain in cancer survivors. J Clin Oncol. (2014) 32(16):1739–47. 10.1200/JCO.2013.52.4629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greco MT, Roberto A, Corli O, Deandrea S, Bandieri E, Cavuto S, et al. Quality of cancer pain management: an update of a systematic review of undertreatment of patients with cancer. J Clin Oncol. (2014) 32(36):4149–54. 10.1200/JCO.2014.56.0383 [DOI] [PubMed] [Google Scholar]
- 22.Yoneda T, Sasaki A, Mundy GR. Osteolytic bone metastasis in breast cancer. Breast Cancer Res Treat. (1994) 32(1):73–84. 10.1007/BF00666208 [DOI] [PubMed] [Google Scholar]
- 23.Arguello F, Baggs RB, Frantz CN. A murine model of experimental metastasis to bone and bone marrow. Cancer Res. (1988) 48(23):6876–81. [PubMed] [Google Scholar]
- 24.Brown DC, Iadarola MJ, Perkowski SZ, Erin H, Shofer F, Laszlo KJ, et al. Physiologic and antinociceptive effects of intrathecal resiniferatoxin in a canine bone cancer model. Anesthesiology. (2005) 103(5):1052–9. 10.1097/00000542-200511000-00020 [DOI] [PubMed] [Google Scholar]
- 25.Goblirsch MJ, Zwolak P, Clohisy DR. Advances in understanding bone cancer pain. J Cell Biochem. (2005) 96(4):682–8. 10.1002/jcb.20589 [DOI] [PubMed] [Google Scholar]
- 26.Schwei MJ, Honore P, Rogers SD, Salak-Johnson JL, Finke MP, Ramnaraine ML, et al. Neurochemical and cellular reorganization of the spinal cord in a murine model of bone cancer pain. J Neurosci. (1999) 19(24):10886–97. 10.1523/JNEUROSCI.19-24-10886.1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Honoré P, Schwei J, Rogers SD, Salak-Johnson JL, Finke MP, Ramnaraine ML, et al. Cellular and neurochemical remodeling of the spinal cord in bone cancer pain. Prog Brain Res. (2000) 129:389–97. 10.1016/S0079-6123(00)29030-4 [DOI] [PubMed] [Google Scholar]
- 28.Wacnik PW, Kehl LJ, Trempe TM, Ramnaraine ML, Beitz AJ, Wilcox GL. Tumor implantation in mouse humerus evokes movement-related hyperalgesia exceeding that evoked by intramuscular carrageenan. Pain. (2003) 101(1-2):175–86. 10.1016/S0304-3959(02)00312-3 [DOI] [PubMed] [Google Scholar]
- 29.Wacnik PW, Eikmeier LJ, Ruggles TR, Ramnaraine ML, Walcheck BK, Beitz AJ, et al. Functional interactions between tumor and peripheral nerve: morphology, algogen identification, and behavioral characterization of a new murine model of cancer pain. J Neurosci. (2001) 21(23):9355–66. 10.1523/JNEUROSCI.21-23-09355.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.de Clauser L, Luiz AP, Santana-Varela S, Wood JN, Sikandar S. Sensitization of cutaneous primary afferents in bone cancer revealed by in vivo calcium imaging. Cancers (Basel). (2020) 12(12). 10.3390/cancers12123491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Medhurst SJ, Walker K, Bowes M, Kidd BL, Glatt M, Muller M, et al. A rat model of bone cancer pain. Pain. (2002) 96(1-2):129–40. 10.1016/S0304-3959(01)00437-7 [DOI] [PubMed] [Google Scholar]
- 32.Bäuerle T, Adwan H, Kiessling F, Hilbig H, Armbruster FP, Berger MR. Characterization of a rat model with site-specific bone metastasis induced by MDA-MB-231 breast cancer cells and its application to the effects of an antibody against bone sialoprotein. Int J Cancer. (2005) 115(2):177–86. 10.1002/ijc.20840 [DOI] [PubMed] [Google Scholar]
- 33.Liepe K, Geidel H, Haase M, Hakenberg OW, Runge R, Kotzerke J. New model for the induction of osteoblastic bone metastases in rat. Anticancer Res. (2005) 25(2a):1067–73. PMID: [PubMed] [Google Scholar]
- 34.Coleman RE. Bone cancer in 2011: prevention and treatment of bone metastases. Nat Rev Clin Oncol. (2011) 9(2):76–8. 10.1038/nrclinonc.2011.198 [DOI] [PubMed] [Google Scholar]
- 35.Rucci N, Teti A. Osteomimicry: how the seed grows in the soil. Calcif Tissue Int. (2018) 102(2):131–40. 10.1007/s00223-017-0365-1 [DOI] [PubMed] [Google Scholar]
- 36.Bangash MA, Alles SRA, Santana-Varela S, Millet Q, Sikandar S, de Clauser L, et al. Distinct transcriptional responses of mouse sensory neurons in models of human chronic pain conditions. Wellcome Open Res. (2018) 3:78. 10.12688/wellcomeopenres.14641.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.de Clauser L, Santana-Varela S, Wood JN, Sikandar S. Physiologic osteoclasts are not sufficient to induce skeletal pain in mice. Eur J Pain. (2021) 25(1):199–212. 10.1002/ejp.1662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sabino MA, Luger NM, Mach DB, Rogers SD, Schwei MJ, Mantyh PW. Different tumors in bone each give rise to a distinct pattern of skeletal destruction, bone cancer-related pain behaviors and neurochemical changes in the central nervous system. Int J Cancer. (2003) 104(5):550–8. 10.1002/ijc.10999 [DOI] [PubMed] [Google Scholar]
- 39.Coleman RE, Rubens RD. The clinical course of bone metastases from breast cancer. Br J Cancer. (1987) 55(1):61–6. 10.1038/bjc.1987.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mercadante S, Fulfaro F. Management of painful bone metastases. Curr Opin Oncol. (2007) 19(4):308–14. 10.1097/CCO.0b013e3281214400 [DOI] [PubMed] [Google Scholar]
- 41.El Mouedden M, Meert TF. Evaluation of pain-related behavior, bone destruction and effectiveness of fentanyl, sufentanil, and morphine in a murine model of cancer pain. Pharmacol Biochem Behav. (2005) 82(1):109–19. 10.1016/j.pbb.2005.07.016 [DOI] [PubMed] [Google Scholar]
- 42.Halvorson KG, Kubota K, Sevcik MA, Lindsay TH, Sotillo JE, Ghilardi JR, et al. A blocking antibody to nerve growth factor attenuates skeletal pain induced by prostate tumor cells growing in bone. Cancer Res. (2005) 65(20):9426. 10.1158/0008-5472.CAN-05-0826 [DOI] [PubMed] [Google Scholar]
- 43.Honore P, Luger NM, Sabino MAC, Schwei MJ, Rogers SD, Mach DB, et al. Osteoprotegerin blocks bone cancer-induced skeletal destruction, skeletal pain and pain-related neurochemical reorganization of the spinal cord. Nat Med. (2000) 6(5):521–8. 10.1038/74999 [DOI] [PubMed] [Google Scholar]
- 44.Honore P, Rogers SD, Schwei MJ, Salak-Johnson JL, Luger NM, Sabino MC, et al. Murine models of inflammatory, neuropathic and cancer pain each generates a unique set of neurochemical changes in the spinal cord and sensory neurons. Neuroscience. (2000) 98(3):585–98. 10.1016/S0306-4522(00)00110-X [DOI] [PubMed] [Google Scholar]
- 45.King T, Vardanyan A, Majuta L, Melemedjian O, Nagle R, Cress AE, et al. Morphine treatment accelerates sarcoma-induced bone pain, bone loss, and spontaneous fracture in a murine model of bone cancer. Pain. (2007) 132(1-2):154–68. 10.1016/j.pain.2007.06.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Luger NM, Honore P, Sabino MAC, Schwei MJ, Rogers SD, Mach DB, et al. Osteoprotegerin diminishes advanced bone cancer pain1. Cancer Res. (2001) 61(10):4038–47. PMID: [PubMed] [Google Scholar]
- 47.Luger NM, Sabino MAC, Schwei MJ, Mach DB, Pomonis JD, Keyser CP, et al. Efficacy of systemic morphine suggests a fundamental difference in the mechanisms that generate bone cancer vs. inflammatory pain. Pain. (2002) 99(3):397–406. 10.1016/S0304-3959(02)00102-1 [DOI] [PubMed] [Google Scholar]
- 48.Peters CM, Lindsay TH, Pomonis JD, Luger NM, Ghilardi JR, Sevcik MA, et al. Endothelin and the tumorigenic component of bone cancer pain. Neuroscience. (2004) 126(4):1043–52. 10.1016/j.neuroscience.2004.04.027 [DOI] [PubMed] [Google Scholar]
- 49.Vermeirsch H, Nuydens RM, Salmon PL, Meert TF. Bone cancer pain model in mice: evaluation of pain behavior, bone destruction and morphine sensitivity. Pharmacol Biochem Behav. (2004) 79(2):243–51. 10.1016/j.pbb.2004.07.011 [DOI] [PubMed] [Google Scholar]
- 50.Khasabov SG, Hamamoto DT, Harding-Rose C, Simone DA. Tumor-evoked hyperalgesia and sensitization of nociceptive dorsal horn neurons in a murine model of cancer pain. Brain Res. (2007) 1180:7–19. 10.1016/j.brainres.2007.08.075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wacnik PW, Eikmeier LJ, Simone DA, Wilcox GL, Beitz AJ. Nociceptive characteristics of tumor necrosis factor-α in naive and tumor-bearing mice. Neuroscience. (2005) 132(2):479–91. 10.1016/j.neuroscience.2004.12.035 [DOI] [PubMed] [Google Scholar]
- 52.Cain DM, Wacnik PW, Eikmeier L, Beitz A, Wilcox GL, Simone DA. Functional interactions between tumor and peripheral nerve in a model of cancer pain in the mouse. Pain Med. (2001) 2(1):15–23. 10.1046/j.1526-4637.2001.002001015.x [DOI] [PubMed] [Google Scholar]
- 53.Kehl LJ, Hamamoto DT, Wacnik PW, Croft DL, Norsted BD, Wilcox GL, et al. A cannabinoid agonist differentially attenuates deep tissue hyperalgesia in animal models of cancer and inflammatory muscle pain. Pain. (2003) 103(1):175–86. 10.1016/s0304-3959(02)00450-5 [DOI] [PubMed] [Google Scholar]
- 54.Vit J-P, Ohara PT, Tien DA, Fike JR, Eikmeier L, Beitz A, et al. The analgesic effect of low dose focal irradiation in a mouse model of bone cancer is associated with spinal changes in neuro-mediators of nociception. Pain. (2006) 120(1-2). [DOI] [PubMed] [Google Scholar]
- 55.Sabino MAC, Ghilardi JR, Jongen JLM, Keyser CP, Luger NM, Mach DB, et al. Simultaneous reduction in cancer pain, bone destruction, and tumor growth by selective inhibition of cyclooxygenase-21. Cancer Res. (2002) 62(24):7343–9. PMID: [PubMed] [Google Scholar]
- 56.Baamonde A, Lastra A, Fresno MF, Llames S, Meana Á, Hidalgo A, et al. Implantation of tumoral XC cells induces chronic, endothelin-dependent, thermal hyperalgesia in mice. Cell Mol Neurobiol. (2004) 24(2):269–81. 10.1023/B:CEMN.0000018621.58328.ea [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dubuisson D, Dennis SG. The formalin test: a quantitative study of the analgesic effects of morphine, meperidine, and brain stem stimulation in rats and cats. Pain. (1977) 4:161–74. 10.1016/0304-3959(77)90130-0 [DOI] [PubMed] [Google Scholar]
- 58.Menéndez L, Lastra A, Fresno MF, Llames S, Meana Á, Hidalgo A, et al. Initial thermal heat hypoalgesia and delayed hyperalgesia in a murine model of bone cancer pain. Brain Res. (2003) 969(1):102–9. 10.1016/S0006-8993(03)02284-4 [DOI] [PubMed] [Google Scholar]
- 59.Menéndez L, Lastra A, Hidalgo A, Meana Á, García E, Baamonde A. Peripheral opioids act as analgesics in bone cancer pain in mice. NeuroReport. (2003) 14(6):867–9. 10.1097/00001756-200305060-00018 [DOI] [PubMed] [Google Scholar]
- 60.Asai H, Ozaki N, Shinoda M, Nagamine K, Tohnai I, Ueda M, et al. Heat and mechanical hyperalgesia in mice model of cancer pain. Pain. (2005) 117(1):19–29. 10.1016/j.pain.2005.05.010 [DOI] [PubMed] [Google Scholar]
- 61.Lee BH, Seong J, Kim UJ, Won R, Kim J. Behavioral characteristics of a mouse model of cancer pain. Yonsei Med J. (2005) 46(2):252–9. 10.3349/ymj.2005.46.2.252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Park HC, Seong J, An JH, Kim J, Kim UJ, Lee BW. Alteration of cancer pain-related signals by radiation: proteomic analysis in an animal model with cancer bone invasion. Int J Radiat Oncol Biol Phys. (2005) 61(5):1523–34. 10.1016/j.ijrobp.2004.12.070 [DOI] [PubMed] [Google Scholar]
- 63.Seong J, Park HC, Kim J, Kim UJ, Lee BW. Radiation-induced alteration of pain-related signals in an animal model with bone invasion from cancer. Ann N Y Acad Sci. (2004) 1030(1):179–86. 10.1196/annals.1329.023 [DOI] [PubMed] [Google Scholar]
- 64.Minett MS, Falk S, Santana-Varela S, Bogdanov YD, Nassar MA, Heegaard AM, et al. Pain without nociceptors? Nav1.7-independent pain mechanisms. Cell Rep. (2014) 6(2):301–12. 10.1016/j.celrep.2013.12.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Beyreuther BK, Callizot N, Brot MD, Feldman R, Bain SC, Stöhr T. Antinociceptive efficacy of lacosamide in rat models for tumor- and chemotherapy-induced cancer pain. Eur J Pharmacol. (2007) 565(1):98–104. 10.1016/j.ejphar.2007.02.041 [DOI] [PubMed] [Google Scholar]
- 66.Brigatte P, Sampaio SC, Gutierrez VP, Guerra JL, Sinhorini IL, Curi R, et al. Walker 256 tumor-bearing rats as a model to study cancer pain. J Pain. (2007) 8(5):412–21. 10.1016/j.jpain.2006.11.006 [DOI] [PubMed] [Google Scholar]
- 67.Fox A, Medhurst S, Courade J-P, Glatt M, Dawson J, Urban L, et al. Anti-hyperalgesic activity of the cox-2 inhibitor lumiracoxib in a model of bone cancer pain in the rat. Pain. (2004) 107(1):33–40. 10.1016/j.pain.2003.09.003 [DOI] [PubMed] [Google Scholar]
- 68.Mao-Ying Q-L, Zhao J, Dong Z-Q, Wang J, Yu J, Yan M-F, et al. A rat model of bone cancer pain induced by intra-tibia inoculation of walker 256 mammary gland carcinoma cells. Biochem Biophys Res Commun. (2006) 345(4):1292–8. 10.1016/j.bbrc.2006.04.186 [DOI] [PubMed] [Google Scholar]
- 69.Nagae M, Hiraga T, Yoneda T. Acidic microenvironment created by osteoclasts causes bone pain associated with tumor colonization. J Bone Miner Metab. (2007) 25(2):99–104. 10.1007/s00774-006-0734-8 [DOI] [PubMed] [Google Scholar]
- 70.Donovan-Rodriguez T, Dickenson Anthony H, Urch Catherine E. Gabapentin normalizes spinal neuronal responses that correlate with behavior in a rat model of cancer-induced bone pain. Anesthesiology. (2005) 102(1):132–40. 10.1097/00000542-200501000-00022 [DOI] [PubMed] [Google Scholar]
- 71.Zhang R-X, Liu B, Wang L, Ren K, Qiao J-T, Berman BM, et al. Spinal glial activation in a new rat model of bone cancer pain produced by prostate cancer cell inoculation of the tibia. Pain. (2005) 118(1-2):125–36. 10.1016/j.pain.2005.08.001 [DOI] [PubMed] [Google Scholar]
- 72.Lindsay TH, Jonas BM, Sevcik MA, Kubota K, Halvorson KG, Ghilardi JR, et al. Pancreatic cancer pain and its correlation with changes in tumor vasculature, macrophage infiltration, neuronal innervation, body weight and disease progression. Pain. (2005) 119(1-3):233–46. 10.1016/j.pain.2005.10.019 [DOI] [PubMed] [Google Scholar]
- 73.Lahoud MJ, Kourie HR, Antoun J, El Osta L, Ghosn M. Road map for pain management in pancreatic cancer: a review. World J Gastrointest Oncol. (2016) 8(8):599–606. 10.4251/wjgo.v8.i8.599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wang L, Xu H, Ge Y, Zhu H, Yu D, Yu W, et al. Establishment of a murine pancreatic cancer pain model and microarray analysis of pain-associated genes in the spinal cord dorsal horn. Mol Med Rep. (2017) 16(4):4429–36. 10.3892/mmr.2017.7173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nagamine K, Ozaki N, Shinoda M, Asai H, Nishiguchi H, Mitsudo K, et al. Mechanical allodynia and thermal hyperalgesia induced by experimental squamous cell carcinoma of the lower gingiva in rats. J Pain. (2006) 7(9):659–70. 10.1016/j.jpain.2006.02.013 [DOI] [PubMed] [Google Scholar]
- 76.Dorsi MJ, Chen L, Murinson BB, Pogatzki-Zahn EM, Meyer RA, Belzberg AJ. The tibial neuroma transposition (TNT) model of neuroma pain and hyperalgesia. Pain. (2008) 134(3):320–34. 10.1016/j.pain.2007.06.030 [DOI] [PubMed] [Google Scholar]
- 77.Tyner TR, Parks N, Faria S, Simons M, Stapp B, Curtis B, et al. Effects of collagen nerve guide on neuroma formation and neuropathic pain in a rat model. Am J Surg. (2007) 193(1):e1–6. 10.1016/j.amjsurg.2006.08.026 [DOI] [PubMed] [Google Scholar]
- 78.Lam DK, Dang D, Zhang J, Dolan JC, Schmidt BL. Novel animal models of acute and chronic cancer pain: a pivotal role for PAR2. J Neurosci. (2012) 32(41):14178–83. 10.1523/JNEUROSCI.2399-12.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pickering V, Gupta RJ, Quang P, Jordan RC, Schmidt BL. Effect of peripheral endothelin-1 concentration on carcinoma-induced pain in mice. Eur J Pain. (2008) 12(3):293–300. 10.1016/j.ejpain.2007.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fallon MT. Neuropathic pain in cancer. Br J Anaesth. (2013) 111(1):105–11. 10.1093/bja/aet208 [DOI] [PubMed] [Google Scholar]
- 81.Shimoyama M, Tanaka K, Hasue F, Shimoyama N. A mouse model of neuropathic cancer pain. Pain. (2002) 99(1-2):167–74. 10.1016/S0304-3959(02)00073-8 [DOI] [PubMed] [Google Scholar]
- 82.Boyle FM, Wheeler HR, Shenfield GM. Amelioration of experimental cisplatin and paclitaxel neuropathy with glutamate. J Neurooncol. (1999) 41(2):107–16. 10.1023/A:1006124917643 [DOI] [PubMed] [Google Scholar]
- 83.Wang AB, Housley SN, Flores AM, Kircher SM, Perreault EJ, Cope TC. A review of movement disorders in chemotherapy-induced neurotoxicity. J Neuroeng Rehabil. (2021) 18(1):16. 10.1186/s12984-021-00818-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Aley KO, Reichling DB, Levine JD. Vincristine hyperalgesia in the rat: a model of painful vincristine neuropathy in humans. Neuroscience. (1996) 73(1):259–65. 10.1016/0306-4522(96)00020-6 [DOI] [PubMed] [Google Scholar]
- 85.Nozaki-Taguchi N, Chaplan SR, Higuera ES, Ajakwe RC, Yaksh TL. Vincristine-induced allodynia in the rat. Pain. (2001) 93(1):69–76. 10.1016/S0304-3959(01)00294-9 [DOI] [PubMed] [Google Scholar]
- 86.Lynch JJ, 3rd, Wade CL, Zhong CM, Mikusa JP, Honore P. Attenuation of mechanical allodynia by clinically utilized drugs in a rat chemotherapy-induced neuropathic pain model. Pain. (2004) 110(1-2):56–63. 10.1016/j.pain.2004.03.010 [DOI] [PubMed] [Google Scholar]
- 87.Polomano RC, Bennett GJ. Chemotherapy-evoked painful peripheral neuropathy. Pain Med. (2001) 2(1):8–14. 10.1046/j.1526-4637.2001.002001008.x [DOI] [PubMed] [Google Scholar]
- 88.Polomano RC, Mannes AJ, Clark US, Bennett GJ. A painful peripheral neuropathy in the rat produced by the chemotherapeutic drug, paclitaxel. Pain. (2001) 94(3):293–304. 10.1016/S0304-3959(01)00363-3 [DOI] [PubMed] [Google Scholar]
- 89.Smith SB, Crager SE, Mogil JS. Paclitaxel-induced neuropathic hypersensitivity in mice: responses in 10 inbred mouse strains. Life Sci. (2004) 74(21):2593–604. 10.1016/j.lfs.2004.01.002 [DOI] [PubMed] [Google Scholar]
- 90.Gispen WH, Hamers FP, Vecht CJ, Jennekens FG, Neyt JP. ACTH/MSH like peptides in the treatment of cisplatin neuropathy. J Steroid Biochem Mol Biol. (1992) 43(1-3):179–83. 10.1016/0960-0760(92)90205-W [DOI] [PubMed] [Google Scholar]
- 91.Strumberg D, Brügge S, Korn MW, Koeppen S, Ranft J, Scheiber G, et al. Evaluation of long-term toxicity in patients after cisplatin-based chemotherapy for non-seminomatous testicular cancer. Ann Oncol. (2002) 13(2):229–36. 10.1093/annonc/mdf058 [DOI] [PubMed] [Google Scholar]
- 92.Authier N, Fialip J, Eschalier A, Coudoré F. Assessment of allodynia and hyperalgesia after cisplatin administration to rats. Neurosci Lett. (2000) 291(2):73–6. 10.1016/S0304-3940(00)01373-2 [DOI] [PubMed] [Google Scholar]
- 93.de Koning P, Neijt JP, Jennekens FG, Gispen WH. Org.2766 protects from cisplatin-induced neurotoxicity in rats. Exp Neurol. (1987) 97(3):746–50. 10.1016/0014-4886(87)90132-4 [DOI] [PubMed] [Google Scholar]
- 94.MacDonald DI, Luiz AP, Iseppon F, Millet Q, Emery EC, Wood JN. Silent cold-sensing neurons contribute to cold allodynia in neuropathic pain. Brain. (2021) 144(6):1711–26. 10.1093/brain/awab086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Deuis JR, Zimmermann K, Romanovsky AA, Possani LD, Cabot PJ, Lewis RJ, et al. An animal model of oxaliplatin-induced cold allodynia reveals a crucial role for Nav1.6 in peripheral pain pathways. Pain. (2013) 154(9):1749–57. 10.1016/j.pain.2013.05.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Authier N, Coudore F, Eschalier A, Fialip J. Pain related behaviour during vincristine-induced neuropathy in rats. NeuroReport. (1999) 10(5):965–8. 10.1097/00001756-199904060-00013 [DOI] [PubMed] [Google Scholar]
- 97.Joseph EK, Levine JD. Sexual dimorphism for protein kinase c epsilon signaling in a rat model of vincristine-induced painful peripheral neuropathy. Neuroscience. (2003) 119(3):831–8. 10.1016/S0306-4522(03)00203-3 [DOI] [PubMed] [Google Scholar]
- 98.Apfel SC, Lipton RB, Arezzo JC, Kessler JA. Nerve growth factor prevents toxic neuropathy in mice. Ann Neurol. (1991) 29(1):87–90. 10.1002/ana.410290115 [DOI] [PubMed] [Google Scholar]
- 99.Matsumoto M, Inoue M, Hald A, Xie W, Ueda H. Inhibition of paclitaxel-induced A-fiber hypersensitization by gabapentin. J Pharmacol Exp Ther. (2006) 318(2):735–40. 10.1124/jpet.106.103614 [DOI] [PubMed] [Google Scholar]
- 100.Dina OA, Chen X, Reichling D, Levine JD. Role of protein kinase cepsilon and protein kinase A in a model of paclitaxel-induced painful peripheral neuropathy in the rat. Neuroscience. (2001) 108(3):507–15. 10.1016/S0306-4522(01)00425-0 [DOI] [PubMed] [Google Scholar]
- 101.Tassler P, Dellon AL, Lesser GJ, Grossman S. Utility of decompressive surgery in the prophylaxis and treatment of cisplatin neuropathy in adult rats. J Reconstr Microsurg. (2000) 16(6):457–63. 10.1055/s-2006-947153 [DOI] [PubMed] [Google Scholar]
- 102.Han FY, Wyse BD, Smith MT. Optimization and pharmacological characterization of a refined cisplatin-induced rat model of peripheral neuropathic pain. Behav Pharmacol. (2014) 25(8):732–40. 10.1097/FBP.0000000000000090 [DOI] [PubMed] [Google Scholar]
- 103.Furgała A, Sałat R, Sałat K. Acute cold allodynia induced by oxaliplatin is attenuated by amitriptyline. Acta Neurobiol Exp. (2018) 78(4):315–21. 10.21307/ane-2018-030 [DOI] [PubMed] [Google Scholar]
- 104.Paget S. The distribution of secondary growths in cancer of the breast. 1889. Cancer Metastasis Rev. (1989) 8(2):98–101. PMID: [PubMed] [Google Scholar]
- 105.Coleman RE. Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res. (2006) 12(20 Pt 2):6243s–9s. 10.1158/1078-0432.CCR-06-0931 [DOI] [PubMed] [Google Scholar]
- 106.Mercadante S. Malignant bone pain: pathophysiology and treatment. Pain. (1997) 69(1-2):1–18. 10.1016/S0304-3959(96)03267-8 [DOI] [PubMed] [Google Scholar]
- 107.Steeg PS. Tumor metastasis: mechanistic insights and clinical challenges. Nat Med. (2006) 12(8):895–904. 10.1038/nm1469 [DOI] [PubMed] [Google Scholar]
- 108.Lipton A. Pathophysiology of bone metastases: how this knowledge may lead to therapeutic intervention. J Support Oncol. (2004) 2(3):205–13; discussion 13–4, 16–7, 19–20. PMID: [PubMed] [Google Scholar]
- 109.Kopp HG, Avecilla ST, Hooper AT, Rafii S. The bone marrow vascular niche: home of HSC differentiation and mobilization. Physiology. (2005) 20:349–56. 10.1152/physiol.00025.2005 [DOI] [PubMed] [Google Scholar]
- 110.Jones DH, Nakashima T, Sanchez OH, Kozieradzki I, Komarova SV, Sarosi I, et al. Regulation of cancer cell migration and bone metastasis by RANKL. Nature. (2006) 440(7084):692–6. 10.1038/nature04524 [DOI] [PubMed] [Google Scholar]
- 111.Kang Y, Siegel PM, Shu W, Drobnjak M, Kakonen SM, Cordón-Cardo C, et al. A multigenic program mediating breast cancer metastasis to bone. Cancer Cell. (2003) 3(6):537–49. 10.1016/S1535-6108(03)00132-6 [DOI] [PubMed] [Google Scholar]
- 112.Sun YX, Schneider A, Jung Y, Wang J, Dai J, Wang J, et al. Skeletal localization and neutralization of the SDF-1(CXCL12)/CXCR4 axis blocks prostate cancer metastasis and growth in osseous sites in vivo. J Bone Miner Res. (2005) 20(2):318–29. 10.1359/JBMR.041109 [DOI] [PubMed] [Google Scholar]
- 113.Shiozawa Y, Pedersen EA, Havens AM, Jung Y, Mishra A, Joseph J, et al. Human prostate cancer metastases target the hematopoietic stem cell niche to establish footholds in mouse bone marrow. J Clin Invest. (2011) 121(4):1298–312. 10.1172/JCI43414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bellahcène A, Bachelier R, Detry C, Lidereau R, Clézardin P, Castronovo V. Transcriptome analysis reveals an osteoblast-like phenotype for human osteotropic breast cancer cells. Breast Cancer Res Treat. (2007) 101(2):135–48. 10.1007/s10549-006-9279-8 [DOI] [PubMed] [Google Scholar]
- 115.Akech J, Wixted JJ, Bedard K, van der Deen M, Hussain S, Guise TA, et al. Runx2 association with progression of prostate cancer in patients: mechanisms mediating bone osteolysis and osteoblastic metastatic lesions. Oncogene. (2010) 29(6):811–21. 10.1038/onc.2009.389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Andersen TL, Boissy P, Sondergaard TE, Kupisiewicz K, Plesner T, Rasmussen T, et al. Osteoclast nuclei of myeloma patients show chromosome translocations specific for the myeloma cell clone: a new type of cancer-host partnership? J Pathol. (2007) 211(1):10–7. 10.1002/path.2078 [DOI] [PubMed] [Google Scholar]
- 117.Liberti MV, Locasale JW. The warburg effect: how does it benefit cancer cells? Trends Biochem Sci. (2016) 41(3):211–8. 10.1016/j.tibs.2015.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Eliasson P, Jönsson J-I. The hematopoietic stem cell niche: low in oxygen but a nice place to be. J Cell Physiol. (2010) 222(1):17–22. 10.1002/jcp.21908 [DOI] [PubMed] [Google Scholar]
- 119.Zhang L, Wen C. Osteocyte dysfunction in joint homeostasis and osteoarthritis. Int J Mol Sci. (2021) 22(12):6522. 10.3390/ijms22126522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Cappariello A, Maurizi A, Veeriah V, Teti A. The great beauty of the osteoclast. Arch Biochem Biophys. (2014) 558:70–8. 10.1016/j.abb.2014.06.017 [DOI] [PubMed] [Google Scholar]
- 121.Pan HL, Zhang YQ, Zhao ZQ. Involvement of lysophosphatidic acid in bone cancer pain by potentiation of TRPV1 via PKCε pathway in dorsal root ganglion neurons. Mol Pain. (2010) 6:85. 10.1186/1744-8069-6-85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ghilardi JR, Röhrich H, Lindsay TH, Sevcik MA, Schwei MJ, Kubota K, et al. Selective blockade of the capsaicin receptor TRPV1 attenuates bone cancer pain. J Neurosci. (2005) 25(12):3126. 10.1523/JNEUROSCI.3815-04.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lautner MA, Ruparel SB, Patil MJ, Hargreaves KM. In vitro sarcoma cells release a lipophilic substance that activates the pain transduction system via TRPV1. Ann Surg Oncol. (2011) 18(3):866–71. 10.1245/s10434-010-1328-1 [DOI] [PubMed] [Google Scholar]
- 124.Qiu F, Wei X, Zhang S, Yuan W, Mi W. Increased expression of acid-sensing ion channel 3 within dorsal root ganglia in a rat model of bone cancer pain. NeuroReport. (2014) 25(12):887–93. 10.1097/WNR.0000000000000182 [DOI] [PubMed] [Google Scholar]
- 125.Aielli F, Ponzetti M, Rucci N. Bone metastasis pain, from the bench to the bedside. Int J Mol Sci. (2019) 20(2):280. 10.3390/ijms20020280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Barrios-Rodiles M, Chadee K. Novel regulation of cyclooxygenase-2 expression and prostaglandin E2 production by IFN-gamma in human macrophages. J Immunol. (1998) 161(5):2441–8. PMID: [PubMed] [Google Scholar]
- 127.Sabino MA, Ghilardi JR, Jongen JL, Keyser CP, Luger NM, Mach DB, et al. Simultaneous reduction in cancer pain, bone destruction, and tumor growth by selective inhibition of cyclooxygenase-2. Cancer Res. (2002) 62(24):7343–9. PMID: [PubMed] [Google Scholar]
- 128.Caterina MJ, Leffler A, Malmberg AB, Martin WJ, Trafton J, Petersen-Zeitz KR, et al. Impaired nociception and pain sensation in mice lacking the capsaicin receptor. Science. (2000) 288(5464):306–13. 10.1126/science.288.5464.306 [DOI] [PubMed] [Google Scholar]
- 129.Williams KS, Killebrew DA, Clary GP, Seawell JA, Meeker RB. Differential regulation of macrophage phenotype by mature and pro-nerve growth factor. J Neuroimmunol. (2015) 285:76–93. 10.1016/j.jneuroim.2015.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Klareskog L, van der Heijde D, de Jager JP, Gough A, Kalden J, Malaise M, et al. Therapeutic effect of the combination of etanercept and methotrexate compared with each treatment alone in patients with rheumatoid arthritis: double-blind randomised controlled trial. Lancet. (2004) 363(9410):675–81. 10.1016/S0140-6736(04)15640-7 [DOI] [PubMed] [Google Scholar]
- 131.Cunha FQ, Poole S, Lorenzetti BB, Ferreira SH. The pivotal role of tumour necrosis factor α in the development of inflammatory hyperalgesia. Br J Pharmacol. (1992) 107(3):660–4. 10.1111/j.1476-5381.1992.tb14503.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Schäfers M, Sorkin LS, Sommer C. Intramuscular injection of tumor necrosis factor-alpha induces muscle hyperalgesia in rats. Pain. (2003) 104(3):579–88. 10.1016/S0304-3959(03)00115-5 [DOI] [PubMed] [Google Scholar]
- 133.Wagner R, Myers RR. Endoneurial injection of TNF-α produces neuropathic pain behaviors. NeuroReport. (1996) 7(18):2897-901. 10.1097/00001756-199611250-00018 [DOI] [PubMed] [Google Scholar]
- 134.Woolf CJ, Allchorne A, Safieh-Garabedian B, Poole S. Cytokines, nerve growth factor and inflammatory hyperalgesia: the contribution of tumour necrosis factor alpha. Br J Pharmacol. (1997) 121(3):417–24. 10.1038/sj.bjp.0701148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zelenka M, Schäfers M, Sommer C. Intraneural injection of interleukin-1β and tumor necrosis factor-alpha into rat sciatic nerve at physiological doses induces signs of neuropathic pain. Pain. (2005) 116(3):257–63. 10.1016/j.pain.2005.04.018 [DOI] [PubMed] [Google Scholar]
- 136.Czeschik JC, Hagenacker T, Schäfers M, Büsselberg D. TNF-α differentially modulates ion channels of nociceptive neurons. Neurosci Lett. (2008) 434(3):293–8. 10.1016/j.neulet.2008.01.070 [DOI] [PubMed] [Google Scholar]
- 137.Liu BG, Dobretsov M, Stimers JR, Zhang JM. Tumor necrosis factor-α suppresses activation of sustained potassium currents in rat small diameter sensory neurons. Open Pain J. (2008) 1:1. 10.2174/1876386300902010001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Jin X, Gereau RW, 4th. Acute p38-mediated modulation of tetrodotoxin-resistant sodium channels in mouse sensory neurons by tumor necrosis factor-alpha. J Neurosci. (2006) 26(1):246–55. 10.1523/JNEUROSCI.3858-05.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Schäfers M, Lee DH, Brors D, Yaksh TL, Sorkin LS. Increased sensitivity of injured and adjacent uninjured rat primary sensory neurons to exogenous tumor necrosis factor-alpha after spinal nerve ligation. J Neurosci. (2003) 23(7):3028–38. 10.1523/JNEUROSCI.23-07-03028.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Sorkin LS, Xiao WH, Wagner R, Myers RR. Tumour necrosis factor-α induces ectopic activity in nociceptive primary afferent fibres. Neuroscience. (1997) 81(1):255–62. 10.1016/S0306-4522(97)00147-4 [DOI] [PubMed] [Google Scholar]
- 141.Tracey D, Klareskog L, Sasso EH, Salfeld JG, Tak PP. Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacol Ther. (2008) 117(2):244–79. 10.1016/j.pharmthera.2007.10.001 [DOI] [PubMed] [Google Scholar]
- 142.Yang Y, Zhang J, Gao Q, Bo J, Ma Z. Etanercept attenuates thermal and mechanical hyperalgesia induced by bone cancer. Exp Ther Med. (2017) 13(5):2565–9. 10.3892/etm.2017.4260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sevcik MA, Ghilardi JR, Peters CM, Lindsay TH, Halvorson KG, Jonas BM, et al. Anti-NGF therapy profoundly reduces bone cancer pain and the accompanying increase in markers of peripheral and central sensitization. Pain. (2005) 115(1-2):128–41. 10.1016/j.pain.2005.02.022 [DOI] [PubMed] [Google Scholar]
- 144.Kaan TKY, Yip PK, Patel S, Davies M, Marchand F, Cockayne DA, et al. Systemic blockade of P2X3 and P2X2/3 receptors attenuates bone cancer pain behaviour in rats. Brain. (2010) 133(9):2549–64. 10.1093/brain/awq194 [DOI] [PubMed] [Google Scholar]
- 145.Sayilekshmy M, Hansen RB, Delaissé JM, Rolighed L, Andersen TL, Heegaard AM. Innervation is higher above bone remodeling surfaces and in cortical pores in human bone: lessons from patients with primary hyperparathyroidism. Sci Rep. (2019) 9(1):5361. 10.1038/s41598-019-41779-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Nencini S, Ivanusic J. Mechanically sensitive aδ nociceptors that innervate bone marrow respond to changes in intra-osseous pressure. J Physiol. (2017) 595(13):4399–415. 10.1113/JP273877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Sottnik JL, Dai J, Zhang H, Campbell B, Keller ET. Tumor-induced pressure in the bone microenvironment causes osteocytes to promote the growth of prostate cancer bone metastases. Cancer Res. (2015) 75(11):2151–8. 10.1158/0008-5472.CAN-14-2493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Tomlinson RE, Li Z, Li Z, Minichiello L, Riddle RC, Venkatesan A, et al. NGF-TrkA signaling in sensory nerves is required for skeletal adaptation to mechanical loads in mice. Proc Natl Acad Sci U S A. (2017) 114(18):E3632–e41. 10.1073/pnas.1701054114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Tomlinson RE, Li Z, Zhang Q, Goh BC, Li Z, Thorek DLJ, et al. NGF-TrkA signaling by sensory nerves coordinates the vascularization and ossification of developing endochondral bone. Cell Rep. (2016) 16(10):2723–35. 10.1016/j.celrep.2016.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Jimenez-Andrade JM, Ghilardi JR, Castañeda-Corral G, Kuskowski MA, Mantyh PW. Preventive or late administration of anti-NGF therapy attenuates tumor-induced nerve sprouting, neuroma formation, and cancer pain. Pain. (2011) 152(11):2564–74. 10.1016/j.pain.2011.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Offley SC, Guo TZ, Wei T, Clark JD, Vogel H, Lindsey DP, et al. Capsaicin-sensitive sensory neurons contribute to the maintenance of trabecular bone integrity. J Bone Miner Res. (2005) 20(2):257–67. 10.1359/JBMR.041108 [DOI] [PubMed] [Google Scholar]
- 152.Cole JS, Patchell RA. Metastatic epidural spinal cord compression. Lancet Neurol. (2008) 7(5):459–66. 10.1016/S1474-4422(08)70089-9 [DOI] [PubMed] [Google Scholar]
- 153.Yu D, Thakor DK, Han I, Ropper AE, Haragopal H, Sidman RL, et al. Alleviation of chronic pain following rat spinal cord compression injury with multimodal actions of huperzine A. Proc Natl Acad Sci U S A. (2013) 110(8):E746–E55. 10.1073/pnas.1300083110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Peters CM, Ghilardi JR, Keyser CP, Kubota K, Lindsay TH, Luger NM, et al. Tumor-induced injury of primary afferent sensory nerve fibers in bone cancer pain. Exp Neurol. (2005) 193(1):85–100. 10.1016/j.expneurol.2004.11.028 [DOI] [PubMed] [Google Scholar]
- 155.Yanagisawa Y, Furue H, Kawamata T, Uta D, Yamamoto J, Furuse S, et al. Bone cancer induces a unique central sensitization through synaptic changes in a wide area of the spinal cord. Mol Pain. (2010) 6:38. 10.1186/1744-8069-6-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Urch EC, Donovan-Rodriguez T, Dickenson HA. Alterations in dorsal horn neurones in a rat model of cancer-induced bone pain. Pain. (2003) 106(3):347–56. 10.1016/j.pain.2003.08.002 [DOI] [PubMed] [Google Scholar]
- 157.Urch CE, Donovan-Rodriguez T, Gordon-Williams R, Bee LA, Dickenson AH. Efficacy of chronic morphine in a rat model of cancer-induced bone pain: behavior and in dorsal horn pathophysiology. J Pain. (2005) 6(12):837–45. 10.1016/j.jpain.2005.08.005 [DOI] [PubMed] [Google Scholar]
- 158.Donovan-Rodriguez T, Urch CE, Dickenson AH. Evidence of a role for descending serotonergic facilitation in a rat model of cancer-induced bone pain. Neurosci Lett. (2006) 393(2-3):237–42. 10.1016/j.neulet.2005.09.073 [DOI] [PubMed] [Google Scholar]
- 159.Zhang RX, Liu B, Li A, Wang L, Ren K, Qiao JT, et al. Interleukin 1beta facilitates bone cancer pain in rats by enhancing NMDA receptor NR-1 subunit phosphorylation. Neuroscience. (2008) 154(4):1533–8. 10.1016/j.neuroscience.2008.04.072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Gu X, Zhang J, Ma Z, Wang J, Zhou X, Jin Y, et al. The role of N-methyl-D-aspartate receptor subunit NR2B in spinal cord in cancer pain. Eur J Pain. (2010) 14(5):496–502. 10.1016/j.ejpain.2009.09.001 [DOI] [PubMed] [Google Scholar]
- 161.Sattler R, Tymianski M. Molecular mechanisms of glutamate receptor-mediated excitotoxic neuronal cell death. Mol Neurobiol. (2001) 24(1-3):107–29. 10.1385/MN:24:1-3:107 [DOI] [PubMed] [Google Scholar]
- 162.Vanderah TW, Laughlin T, Lashbrook JM, Nichols ML, Wilcox GL, Ossipov MH, et al. Single intrathecal injections of dynorphin A or des-tyr-dynorphins produce long-lasting allodynia in rats: blockade by MK-801 but not naloxone. Pain. (1996) 68(2-3):275–81. 10.1016/S0304-3959(96)03225-3 [DOI] [PubMed] [Google Scholar]
- 163.Quasthoff S, Hartung HP. Chemotherapy-induced peripheral neuropathy. J Neurol. (2002) 249(1):9–17. 10.1007/PL00007853 [DOI] [PubMed] [Google Scholar]
- 164.Wang Z, Sun H, Yakisich JS. Overcoming the blood-brain barrier for chemotherapy: limitations, challenges and rising problems. Anticancer Agents Med Chem. (2014) 14(8):1085–93. 10.2174/18715206113139990029 [DOI] [PubMed] [Google Scholar]
- 165.Seretny M, Currie GL, Sena ES, Ramnarine S, Grant R, MacLeod MR, et al. Incidence, prevalence, and predictors of chemotherapy-induced peripheral neuropathy: a systematic review and meta-analysis. Pain. (2014) 155(12):2461–70. 10.1016/j.pain.2014.09.020 [DOI] [PubMed] [Google Scholar]
- 166.Holmes J, Stanko J, Varchenko M, Ding H, Madden VJ, Bagnell CR, et al. Comparative neurotoxicity of oxaliplatin, cisplatin, and ormaplatin in a wistar rat model. Toxicol Sci. (1998) 46(2):342–51. 10.1006/toxs.1998.2558 [DOI] [PubMed] [Google Scholar]
- 167.Cavaletti G, Cavalletti E, Oggioni N, Sottani C, Minoia C, D'Incalci M, et al. Distribution of paclitaxel within the nervous system of the rat after repeated intravenous administration. Neurotoxicology. (2000) 21(3):389–93. PMID: [PubMed] [Google Scholar]
- 168.Cavaletti G, Tredici G, Petruccioli MG, Dondè E, Tredici P, Marmiroli P, et al. Effects of different schedules of oxaliplatin treatment on the peripheral nervous system of the rat. Eur J Cancer. (2001) 37(18):2457–63. 10.1016/S0959-8049(01)00300-8 [DOI] [PubMed] [Google Scholar]
- 169.Screnci D, McKeage MJ, Galettis P, Hambley TW, Palmer BD, Baguley BC. Relationships between hydrophobicity, reactivity, accumulation and peripheral nerve toxicity of a series of platinum drugs. Br J Cancer. (2000) 82(4):966–72. 10.1054/bjoc.1999.1026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Cliffer KD, Siuciak JA, Carson SR, Radley HE, Park JS, Lewis DR, et al. Physiological characterization of taxol-induced large-fiber sensory neuropathy in the rat. Ann Neurol. (1998) 43(1):46–55. 10.1002/ana.410430111 [DOI] [PubMed] [Google Scholar]
- 171.Fischer SJ, Podratz JL, Windebank AJ. Nerve growth factor rescue of cisplatin neurotoxicity is mediated through the high affinity receptor: studies in PC12 cells and p75 null mouse dorsal root ganglia. Neurosci Lett. (2001) 308(1):1–4. 10.1016/S0304-3940(01)01956-5 [DOI] [PubMed] [Google Scholar]
- 172.McDonald ES, Windebank AJ. Cisplatin-induced apoptosis of DRG neurons involves bax redistribution and cytochrome c release but not fas receptor signaling. Neurobiol Dis. (2002) 9(2):220–33. 10.1006/nbdi.2001.0468 [DOI] [PubMed] [Google Scholar]
- 173.Materazzi S, Fusi C, Benemei S, Pedretti P, Patacchini R, Nilius B, et al. TRPA1 and TRPV4 mediate paclitaxel-induced peripheral neuropathy in mice via a glutathione-sensitive mechanism. Pflugers Arch. (2012) 463(4):561–9. 10.1007/s00424-011-1071-x [DOI] [PubMed] [Google Scholar]
- 174.Nassini R, Gees M, Harrison S, De Siena G, Materazzi S, Moretto N, et al. Oxaliplatin elicits mechanical and cold allodynia in rodents via TRPA1 receptor stimulation. Pain. (2011) 152(7):1621–31. 10.1016/j.pain.2011.02.051 [DOI] [PubMed] [Google Scholar]
- 175.Nieto FR, Entrena JM, Cendán CM, Del Pozo E, Vela JM, Baeyens JM. Tetrodotoxin inhibits the development and expression of neuropathic pain induced by paclitaxel in mice. Pain. (2008) 137(3):520–31. 10.1016/j.pain.2007.10.012 [DOI] [PubMed] [Google Scholar]
- 176.Xiao W, Boroujerdi A, Bennett GJ, Luo ZD. Chemotherapy-evoked painful peripheral neuropathy: analgesic effects of gabapentin and effects on expression of the alpha-2-delta type-1 calcium channel subunit. Neuroscience. (2007) 144(2):714–20. 10.1016/j.neuroscience.2006.09.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Musatov A, Robinson NC. Susceptibility of mitochondrial electron-transport complexes to oxidative damage. Focus on cytochrome c oxidase. Free Radic Res. (2012) 46(11):1313–26. 10.3109/10715762.2012.717273 [DOI] [PubMed] [Google Scholar]
- 178.Luiz AP, MacDonald DI, Santana-Varela S, Millet Q, Sikandar S, Wood JN, et al. Cold sensing by NaV1.8-positive and NaV1.8-negative sensory neurons. Proc Natl Acad Sci U S A. (2019) 116(9):3811–6. 10.1073/pnas.1814545116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Peters CM, Jimenez-Andrade JM, Kuskowski MA, Ghilardi JR, Mantyh PW. An evolving cellular pathology occurs in dorsal root ganglia, peripheral nerve and spinal cord following intravenous administration of paclitaxel in the rat. Brain Res. (2007) 1168:46–59. 10.1016/j.brainres.2007.06.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Scuteri A, Nicolini G, Miloso M, Bossi M, Cavaletti G, Windebank AJ, et al. Paclitaxel toxicity in post-mitotic dorsal root ganglion (DRG) cells. Anticancer Res. (2006) 26(2a):1065–70. PMID: [PubMed] [Google Scholar]
- 181.Freelove R, Walling AD. Pancreatic cancer: diagnosis and management. Am Fam Physician. (2006) 73(3):485–92. PMID: [PubMed] [Google Scholar]
- 182.Moore JC, Adler DG. Celiac plexus neurolysis for pain relief in pancreatic cancer. J Support Oncol. (2009) 7(3):83–7, 90. PMID: [PubMed] [Google Scholar]
- 183.Pour PM, Bell RH, Batra SK. Neural invasion in the staging of pancreatic cancer. Pancreas. (2003) 26(4):322–5. 10.1097/00006676-200305000-00002 [DOI] [PubMed] [Google Scholar]
- 184.Jemal A, Clegg LX, Ward E, Ries LA, Wu X, Jamison PM, et al. Annual report to the nation on the status of cancer, 1975-2001, with a special feature regarding survival. Cancer. (2004) 101(1):3–27. 10.1002/cncr.20288 [DOI] [PubMed] [Google Scholar]
- 185.Seki H, Tanaka J-I, Sato Y, Kato Y, Umezawa A, Koyama K. Neural cell adhesion molecule (NCAM) and perineural invasion in bile duct cancer. J Surg Oncol. (1993) 53(2):78–83. 10.1002/jso.2930530205 [DOI] [PubMed] [Google Scholar]
- 186.Zhu Z, Friess H, di Mola FF, Zimmermann A, Graber HU, Korc M, et al. Nerve growth factor expression correlates with perineural invasion and pain in human pancreatic cancer. J Clin Oncol. (1999) 17(8):2419–28. 10.1200/JCO.1999.17.8.2419 [DOI] [PubMed] [Google Scholar]
- 187.di Mola FF, di Sebastiano P. Pain and pain generation in pancreatic cancer. Langenbeck's Arch Surg. (2008) 393(6):919–22. 10.1007/s00423-007-0277-z [DOI] [PubMed] [Google Scholar]
- 188.Hartel M, di Mola FF, Selvaggi F, Mascetta G, Wente MN, Felix K, et al. Vanilloids in pancreatic cancer: potential for chemotherapy and pain management. Gut. (2006) 55(4):519–28. 10.1136/gut.2005.073205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Sevcik MA, Jonas BM, Lindsay TH, Halvorson KG, Ghilardi JR, Kuskowski MA, et al. Endogenous opioids inhibit early-stage pancreatic pain in a mouse model of pancreatic cancer. Gastroenterology. (2006) 131(3):900–10. 10.1053/j.gastro.2006.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Porreca F, Ossipov MH, Gebhart GF. Chronic pain and medullary descending facilitation. Trends Neurosci. (2002) 25(6):319–25. 10.1016/S0166-2236(02)02157-4 [DOI] [PubMed] [Google Scholar]
- 191.Ren K, Dubner R. Descending modulation in persistent pain: an update. Pain. (2002) 100(1-2):1–6. 10.1016/S0304-3959(02)00368-8 [DOI] [PubMed] [Google Scholar]
- 192.Mantyh PW. Cancer pain and its impact on diagnosis, survival and quality of life. Nat Rev Neurosci. (2006) 7(10):797–809. 10.1038/nrn1914 [DOI] [PubMed] [Google Scholar]
- 193.Muralidharan A, Wyse BD, Smith MT. Optimization and characterization of a rat model of prostate cancer-induced bone pain using behavioral, pharmacological, radiological, histological and immunohistochemical methods. Pharmacol Biochem Behav. (2013) 106:33–46. 10.1016/j.pbb.2013.02.020 [DOI] [PubMed] [Google Scholar]
- 194.Shenoy P, Kuo A, Vetter I, Smith MT. Optimization and in vivo profiling of a refined rat model of walker 256 breast cancer cell-induced bone pain using behavioral, radiological, histological, immunohistochemical and pharmacological methods. Front Pharmacol. (2017) 8:442. 10.3389/fphar.2017.00442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Ceyhan GO, Michalski CW, Demir IE, Müller MW, Friess H. Pancreatic pain. Best Pract Res Clin Gastroenterol. (2008) 22(1):31–44. 10.1016/j.bpg.2007.10.016 [DOI] [PubMed] [Google Scholar]
- 196.Feng W, Teng R, Zhao Y, Gao J, Chu H. Epigenetic modulation of wnt signaling contributes to neuropathic pain in rats. Mol Med Rep. (2015) 12(3):4727–33. 10.3892/mmr.2015.3972 [DOI] [PubMed] [Google Scholar]
- 197.Quick ML, Mukherjee S, Rudick CN, Done JD, Schaeffer AJ, Thumbikat P. CCL2 and CCL3 are essential mediators of pelvic pain in experimental autoimmune prostatitis. Am J Physiol Regul Integr Comp Physiol. (2012) 303(6):R580–9. 10.1152/ajpregu.00240.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Pickering V, Jordan RC, Schmidt BL. Elevated salivary endothelin levels in oral cancer patients–a pilot study. Oral Oncol. (2007) 43(1):37–41. 10.1016/j.oraloncology.2005.12.027 [DOI] [PubMed] [Google Scholar]
- 199.Schmidt BL, Pickering V, Liu S, Quang P, Dolan J, Connelly ST, et al. Peripheral endothelin A receptor antagonism attenuates carcinoma-induced pain. Eur J Pain. (2007) 11(4):406–14. 10.1016/j.ejpain.2006.05.007 [DOI] [PubMed] [Google Scholar]
- 200.Ye Y, Dang D, Zhang J, Viet CT, Lam DK, Dolan JC, et al. Nerve growth factor links oral cancer progression, pain, and cachexiaanti-NGF as a therapy in head and neck cancer. Mol Cancer Ther. (2011) 10(9):1667–76. 10.1158/1535-7163.MCT-11-0123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Lam DK, Schmidt BL. Serine proteases and protease-activated receptor 2-dependent allodynia: a novel cancer pain pathway. Pain. (2010) 149(2):263–72. 10.1016/j.pain.2010.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Amadesi S, Cottrell GS, Divino L, Chapman K, Grady EF, Bautista F, et al. Protease-activated receptor 2 sensitizes TRPV1 by protein kinase cepsilon- and A-dependent mechanisms in rats and mice. J Physiol. (2006) 575(Pt 2):555–71. 10.1113/jphysiol.2006.111534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.McNicol E, Horowicz-Mehler N, Fisk RA, Bennett K, Gialeli-Goudas M, Chew PW, et al. Management of opioid side effects in cancer-related and chronic noncancer pain: a systematic review. J Pain. (2003) 4(5):231–56. 10.1016/S1526-5900(03)00556-X [DOI] [PubMed] [Google Scholar]
- 204.Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. (2015) 14(2):162–73. 10.1016/S1474-4422(14)70251-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Glaum SR, Miller RJ, Hammond DL. Inhibitory actions of delta 1-, delta 2-, and mu-opioid receptor agonists on excitatory transmission in lamina II neurons of adult rat spinal cord. J Neurosci. (1994) 14(8):4965–71. 10.1523/JNEUROSCI.14-08-04965.1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Trafton JA, Abbadie C, Marek K, Basbaum AI. Postsynaptic signaling via the [mu]-opioid receptor: responses of dorsal horn neurons to exogenous opioids and noxious stimulation. J Neurosci. (2000) 20(23):8578–84. 10.1523/JNEUROSCI.20-23-08578.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Yamamoto J, Kawamata T, Niiyama Y, Omote K, Namiki A. Down-regulation of mu opioid receptor expression within distinct subpopulations of dorsal root ganglion neurons in a murine model of bone cancer pain. Neuroscience. (2008) 151(3):843–53. 10.1016/j.neuroscience.2007.11.025 [DOI] [PubMed] [Google Scholar]
- 208.Zhu C, Tang J, Ding T, Chen L, Wang W, Mei XP, et al. Neuron-restrictive silencer factor-mediated downregulation of μ-opioid receptor contributes to the reduced morphine analgesia in bone cancer pain. Pain. (2017) 158(5):879–90. 10.1097/j.pain.0000000000000848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Yao P, Ding Y, Wang Z, Ma J, Hong T, Zhu Y, et al. Impacts of anti-nerve growth factor antibody on pain-related behaviors and expressions of opioid receptor in spinal dorsal horn and dorsal root ganglia of rats with cancer-induced bone pain. Mol Pain. (2016) 12:1744806916644928. 10.1177/1744806916644928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev. (2001) 27(3):165–76. 10.1053/ctrv.2000.0210 [DOI] [PubMed] [Google Scholar]
- 211.Luckman SP, Hughes DE, Coxon FP, Graham R, Russell G, Rogers MJ. Nitrogen-containing bisphosphonates inhibit the mevalonate pathway and prevent post-translational prenylation of GTP-binding proteins, including ras. J Bone Miner Res. (1998) 13(4):581–9. 10.1359/jbmr.1998.13.4.581 [DOI] [PubMed] [Google Scholar]
- 212.Frith JC, Mönkkönen J, Auriola S, Mönkkönen H, Rogers MJ. The molecular mechanism of action of the antiresorptive and antiinflammatory drug clodronate: evidence for the formation in vivo of a metabolite that inhibits bone resorption and causes osteoclast and macrophage apoptosis. Arthritis Rheum. (2001) 44(9):2201–10. [DOI] [PubMed] [Google Scholar]
- 213.Kostenuik PJ, Nguyen HQ, McCabe J, Warmington KS, Kurahara C, Sun N, et al. Denosumab, a fully human monoclonal antibody to RANKL, inhibits bone resorption and increases BMD in knock-in mice that express chimeric (murine/human) RANKL. J Bone Miner Res. (2009) 24(2):182–95. 10.1359/jbmr.081112 [DOI] [PubMed] [Google Scholar]
- 214.O'Brien W, Fissel BM, Maeda Y, Yan J, Ge X, Gravallese EM, et al. RANK-independent osteoclast formation and bone erosion in inflammatory arthritis. Arthritis Rheumatol. (2016) 68(12):2889–900. 10.1002/art.39837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Guedon JG, Longo G, Majuta LA, Thomspon ML, Fealk MN, Mantyh PW. Dissociation between the relief of skeletal pain behaviors and skin hypersensitivity in a model of bone cancer pain. Pain. (2016) 157(6):1239–47. 10.1097/j.pain.0000000000000514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Ghilardi JR, Freeman KT, Jimenez-Andrade JM, Mantyh WG, Bloom AP, Kuskowski MA, et al. Administration of a tropomyosin receptor kinase inhibitor attenuates sarcoma-induced nerve sprouting, neuroma formation and bone cancer pain. Mol Pain. (2010) 6:87. 10.1186/1744-8069-6-87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Mantyh WG, Jimenez-Andrade JM, Stake JI, Bloom AP, Kaczmarska MJ, Taylor RN, et al. Blockade of nerve sprouting and neuroma formation markedly attenuates the development of late stage cancer pain. Neuroscience. (2010) 171(2):588–98. 10.1016/j.neuroscience.2010.08.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.McCaffrey G, Thompson ML, Majuta L, Fealk MN, Chartier S, Longo G, et al. NGF blockade at early times during bone cancer development attenuates bone destruction and increases limb use. Cancer Res. (2014) 74(23):7014–23. 10.1158/0008-5472.CAN-14-1220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Koewler NJ, Freeman KT, Buus RJ, Herrera MB, Jimenez-Andrade JM, Ghilardi JR, et al. Effects of a monoclonal antibody raised against nerve growth factor on skeletal pain and bone healing after fracture of the C57BL/6J mouse femur. J Bone Miner Res. (2007) 22(11):1732–42. 10.1359/jbmr.070711 [DOI] [PubMed] [Google Scholar]
- 220.Shelton DL, Zeller J, Ho WH, Pons J, Rosenthal A. Nerve growth factor mediates hyperalgesia and cachexia in auto-immune arthritis. Pain. (2005) 116(1-2):8–16. 10.1016/j.pain.2005.03.039 [DOI] [PubMed] [Google Scholar]
- 221.Wise BL, Seidel MF, Lane NE. The evolution of nerve growth factor inhibition in clinical medicine. Nat Rev Rheumatol. (2021) 17(1):34–46. 10.1038/s41584-020-00528-4 [DOI] [PubMed] [Google Scholar]
- 222.Sopata M, Katz N, Carey W, Smith MD, Keller D, Verburg KM, et al. Efficacy and safety of tanezumab in the treatment of pain from bone metastases. Pain. (2015) 156(9):1703–13. 10.1097/j.pain.0000000000000211 [DOI] [PubMed] [Google Scholar]
- 223.Arai H, Hori S, Aramori I, Ohkubo H, Nakanishi S. Cloning and expression of a cDNA encoding an endothelin receptor. Nature. (1990) 348(6303):730–2. 10.1038/348730a0 [DOI] [PubMed] [Google Scholar]
- 224.Sakurai T, Yanagisawa M, Takuwa Y, Miyazaki H, Kimura S, Goto K, et al. Cloning of a cDNA encoding a non-isopeptide-selective subtype of the endothelin receptor. Nature. (1990) 348(6303):732–5. 10.1038/348732a0 [DOI] [PubMed] [Google Scholar]
- 225.Plant TD, Zöllner C, Kepura F, Mousa SS, Eichhorst J, Schaefer M, et al. Endothelin potentiates TRPV1 via ETA receptor-mediated activation of protein kinase C. Mol Pain. (2007) 3:35. 10.1186/1744-8069-3-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Zhou Z, Davar G, Strichartz G. Endothelin-1 (ET-1) selectively enhances the activation gating of slowly inactivating tetrodotoxin-resistant sodium currents in rat sensory neurons: a mechanism for the pain-inducing actions of ET-1. J Neurosci. (2002) 22(15):6325–30. 10.1523/JNEUROSCI.22-15-06325.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Gold MS, Levine JD, Correa AM. Modulation of TTX-R INa by PKC and PKA and their role in PGE2-induced sensitization of rat sensory neurons in vitro. J Neurosci. (1998) 18(24):10345–55. 10.1523/JNEUROSCI.18-24-10345.1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Dymshitz J, Vasko MR. Endothelin-1 enhances capsaicin-induced peptide release and cGMP accumulation in cultures of rat sensory neurons. Neurosci Lett. (1994) 167(1-2):128–32. 10.1016/0304-3940(94)91044-8 [DOI] [PubMed] [Google Scholar]
- 229.Zhou QL, Strichartz G, Davar G. Endothelin-1 activates ET(A) receptors to increase intracellular calcium in model sensory neurons. Neuroreport. (2001) 12(17):3853–7. 10.1097/00001756-200112040-00050 [DOI] [PubMed] [Google Scholar]
- 230.Nishimura T, Akasu T, Krier J. Endothelin modulates calcium channel current in neurones of rabbit pelvic parasympathetic ganglia. Br J Pharmacol. (1991) 103(1):1242–50. 10.1111/j.1476-5381.1991.tb12331.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Suzuki T. Endothelin-1-induced depolarization and hyperpolarization in submandibular ganglion neurons. Bull Tokyo Dent Coll. (2004) 45(3):189–92. 10.2209/tdcpublication.45.189 [DOI] [PubMed] [Google Scholar]
- 232.Yamamoto H, Kawamata T, Ninomiya T, Omote K, Namiki A. Endothelin-1 enhances capsaicin-evoked intracellular Ca2+ response via activation of endothelin a receptor in a protein kinase cepsilon-dependent manner in dorsal root ganglion neurons. Neuroscience. (2006) 137(3):949–60. 10.1016/j.neuroscience.2005.09.036 [DOI] [PubMed] [Google Scholar]
- 233.Pomonis JD, Rogers SD, Peters CM, Ghilardi JR, Mantyh PW. Expression and localization of endothelin receptors: implications for the involvement of peripheral glia in nociception. J Neurosci. (2001) 21(3):999–1006. 10.1523/JNEUROSCI.21-03-00999.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Koyama Y, Mizobata T, Yamamoto N, Hashimoto H, Matsuda T, Baba A. Endothelins stimulate expression of cyclooxygenase 2 in rat cultured astrocytes. J Neurochem. (1999) 73(3):1004–11. 10.1046/j.1471-4159.1999.0731004.x [DOI] [PubMed] [Google Scholar]
- 235.Khodorova A, Navarro B, Jouaville LS, Murphy JE, Rice FL, Mazurkiewicz JE, et al. Endothelin-B receptor activation triggers an endogenous analgesic cascade at sites of peripheral injury. Nat Med. (2003) 9(8):1055–61. 10.1038/nm885 [DOI] [PubMed] [Google Scholar]
- 236.Khodorova A, Montmayeur JP, Strichartz G. Endothelin receptors and pain. J Pain. (2009) 10(1):4–28. 10.1016/j.jpain.2008.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Yoneda T, Hiasa M, Nagata Y, Okui T, White FA. Acidic microenvironment and bone pain in cancer-colonized bone. Bonekey Rep. (2015) 4:690. 10.1038/bonekey.2015.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Vultaggio-Poma V, Sarti AC, Di Virgilio F. Extracellular ATP: a feasible target for cancer therapy. Cells. (2020) 9(11):2496. 10.3390/cells9112496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Sawynok J. Adenosine and ATP receptors. In: Stein C, editors. Analgesia. Berlin, Heidelberg: Springer Berlin Heidelberg; (2007). p. 309–28. [Google Scholar]
- 240.Jimenez-Andrade JM, Mantyh WG, Bloom AP, Xu H, Ferng AS, Dussor G, et al. A phenotypically restricted set of primary afferent nerve fibers innervate the bone versus skin: therapeutic opportunity for treating skeletal pain. Bone. (2010) 46(2):306–13. 10.1016/j.bone.2009.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Gilchrist LS, Cain DM, Harding-Rose C, Kov AN, Wendelschafer-Crabb G, Kennedy WR, et al. Re-organization of P2X3 receptor localization on epidermal nerve fibers in a murine model of cancer pain. Brain Res. (2005) 1044(2):197–205. 10.1016/j.brainres.2005.02.081 [DOI] [PubMed] [Google Scholar]
- 242.ter Laak MP, Hamers FP, Kirk CJ, Gispen WH. rhGGF2 protects against cisplatin-induced neuropathy in the rat. J Neurosci Res. (2000) 60(2):237–44. [DOI] [PubMed] [Google Scholar]