Abstract
Objective
The aim of this study was to identify racial and ethnic disparities in patient portal offers, access, and use and to examine the role of providers in facilitating access to electronic health information (EHI) by offering patient portals and encouraging their use.
Materials and Methods
Using nationally representative survey data from 2019 and 2020 (N = 8028), we examined disparities in patients being offered access to a portal by their provider and differences in subsequent access and use. Using multivariable models, we estimated the effect of race and ethnicity on the likelihood of being offered, accessing or using a portal. Among those offered, we examined the relationship between provider encouragement and portal access; and for those who did not access their portal, we explored reasons for nonuse.
Results
Black and Hispanic individuals were offered and accessed patient portals at significantly lower rates than White individuals. Compared to Whites, Black and Hispanic individuals were 5.2 percentage-points less likely to be offered a portal (P < .05) and, among those offered, 7.9 percentage-points less likely to access their portal (P < .05). Black and Hispanic individuals who were offered and accessed a portal were 12 percentage-points more likely than Whites to use it to download or transmit information (P < .01). Individuals who were offered a portal and encouraged to use it were 21 percentage-points more likely to access it.
Discussion
Differences in patient portal access and use are likely driven by disparities in which groups of patients reported being offered a portal.
Conclusions
Providers play an important role in increasing access to EHI by facilitating access to patient portals.
Keywords: patient portals, electronic health information, health disparities
INTRODUCTION
Patient medical records are digitized across many healthcare settings.1,2 Federal policies have sought to increase patients’ access to their electronic health information (EHI), as studies have shown that patient engagement with EHI—such as through the use of patient portals (hereafter also referred to as “portals”)—can help patients make informed decisions about their health care, facilitate communication with healthcare providers, improve adherence to medications, and lead to better health outcomes.3–8 Starting in 2014, the Centers for Medicare & Medicaid Services (CMS) Electronic Health Record (EHR) Incentive Programs, supported by the Office of the National Coordinator for Health Information Technology (ONC) Health IT Certification program, required participating hospitals and eligible healthcare providers to adopt certified EHR technology with capabilities that enable patients to electronically view, download, and transmit their health information, which was largely implemented via patient portals.9–11
In 2019, 60% of office-based physicians and nearly all hospitals (97%) enabled patients to view their EHI using a patient portal.12,13 As of 2020, only about six in 10 individuals nationwide (57%) reported being offered access to a patient portal by their healthcare provider and 40% accessed their record at least once within the past year.14 This represents significant progress from 2014 when only 33% of individuals reported being offered access to a portal and 27% logged in to their account.15,16 While the overall increase in portal access is encouraging, a digital divide exists in the access and use of patient portals despite the enactment of policies aimed at increasing access to EHI.17 Early studies leveraging administrative and national survey data found that, in addition to differences in patient portal access and use—which may be driven in part by varying preferences for portal use—Black and Hispanic individuals were significantly less likely to report being offered access to EHI via a portal after adjusting for personal characteristics.18–24 Later studies found similar racial/ethnic disparities in the likelihood of patients reporting they were offered a portal, but no longer found significant differences in portal access and use among those who were offered access to their portal or encouraged by their healthcare provider to use it.25–27
In 2020, ONC published the Cures Act Final Rule (Cures Rule), which sought to advance patient access to EHI by calling on health IT developers to adopt standards-based application programming interfaces (APIs) that could enable patients to access their EHI using health apps via their smartphone or other methods.28 Since modern methods of accessing EHI require an individual to first have patient portal credentials, racial and ethnic disparities in portal offers and use have downstream implications for API-based app access.
Building on prior studies, we use the most recent nationally representative survey data to identify disparities in patient reports of being offered access to a patient portal by their healthcare provider (henceforth “offered” a portal). To understand the role that providers play in exacerbating disparities in patient access to EHI, we compare rates of patient-reported access and use among White, Black, and Hispanic individuals in the overall sample and among those who were offered a portal by their provider, and thus were given an opportunity to access and use it. To understand how providers can ameliorate disparities in patient access to EHI, we examine the role of patient-reported provider encouragement in increasing portal access among those who were offered a portal (henceforth “encouraged” to use a portal). Finally, for those who were offered but did not access their portal, we explore reasons for nonuse. Unlike previous studies, we apply inverse propensity score weighting to adjust for potential confounding factors. Given that health inequities are often the product of inequities in other parts of society, accounting for these factors allows us to isolate the unique effect of race and ethnicity on patient portal offers, access, and use. Our analysis goes beyond identifying disparities by shedding light on mechanisms through which disparities may occur—through initial offer rates and subsequent encouragement—and how they can be addressed.
OBJECTIVE
The overarching objective of this study is to identify racial and ethnic disparities in patient portal offers, access, and use. We explore five research questions:
Are there racial and ethnic disparities in the share of individuals who were offered, accessed, or used their patient portal to view test results, download or transmit information, and message with their provider?
What is the effect of race and ethnicity on the likelihood of being offered a patient portal?
What is the effect of race and ethnicity on the likelihood of accessing or using a patient portal among those offered a portal?
What is the effect of healthcare provider encouragement on the likelihood of accessing a portal among those offered? Does this effect vary by racial or ethnic group?
What are the reasons for not using a portal among those who were offered a portal but did not access it? Do reasons vary by racial or ethnic group?
MATERIALS AND METHODS
Data and study population
Data used for this study came from two cycles of the Health Information National Trends Survey (HINTS), a nationally representative survey of civilian, noninstitutionalized adults conducted by the National Cancer Institute that tracks individuals’ access and use of their health information. Data were collected prior to the Cures Act API provisions going into effect. HINTS 5 Cycle 3 (2019) was conducted from January to May 2019, yielding 5438 eligible questionnaires and a response rate of 30.3%. Cycle 4 (2020) was conducted from February to June 2020 yielding 3,865 eligible questionnaires and a response rate of 36.6%. We restricted our sample to respondents who had a healthcare visit in the past 12 months (N = 8028) to better identify racial and ethnic disparities in portal use among individuals with a recent interaction with the healthcare system, and thus had an opportunity to be offered a patient portal and use it. All analyses used survey weighting procedures with jackknife replicate weights to account for the complex survey design. See the HINTS website for additional information on survey design and weighting.29,30
Variables
Independent variables
For the descriptive analysis, race/ethnicity was defined as a categorical variable representing five mutually exclusive groups: Hispanic, non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, non-Hispanic other or multiple races (henceforth referred to as White, Black, Asian, and other or multiple races). For multivariate analyses, we narrowed our focus to examine disparities among Black and Hispanic respondents—the two groups with the lowest rates of patient portal access and use—relative to White respondents. Separate multivariate analyses were performed across three sub-populations of respondents (where White is the reference group): Black alone, Hispanic alone, and Black or Hispanic. We included this pooled sample in all analyses as a robustness check, particularly for stratified analyses where the sample size is small. All multivariate models controlled for gender, education, income, rurality, insurance status, chronic condition, having a regular healthcare provider, and number of internet access types.
Outcome variables
In this study, we examined several binary outcomes related to patients’ engagement with their online medical records via a patient portal. The first outcome indicates respondents who reported being offered access to their patient portal by a healthcare provider (ie, whether they were offered portal credentials needed to access their online medical record). The second indicates respondents who accessed their portal at least once in the last 12 months. Among those who accessed their portal, we examined use of a patient portal to view test results, download or transmit health information, and securely message with a provider. Our fourth outcome indicates whether any of a respondent’s healthcare providers ever encouraged them to use a patient portal, which we exclusively examined among those who were offered access to their portal. Finally, we explored a list of reasons for not using a portal among those who were offered a patient portal but did not access it (eg, preferring to speak to their healthcare provider directly, privacy and security concerns, having no way to access the website). More information on key measures and corresponding survey questions is provided in Supplementary Appendices SA and SB.
Statistical analysis
We reported national statistics on rates of individuals who were offered a patient portal by their healthcare provider and examined rates of patient portal access—overall and among those offered a portal—and use among those who were offered and accessed their portal. We then compared differences in unadjusted estimates among respondents identifying as Black, Hispanic, Asian, and other or multiple races relative to White. Next, we used a weighted linear probability model (LPM) to estimate the effect of identifying as Black or Hispanic, Black alone, and Hispanic alone on the likelihood of being offered, accessing, or using a patient portal. To adjust for potential confounding, we controlled for factors related to race and ethnicity and our outcomes of interest using inverse propensity score weighting. We followed the approach of Ye et al31 in defining the treatment or “risk-exposed” group as respondents who identified as Black or Hispanic, whereas the reference sample included those who identified as White. To validate the use of propensity score methods, we assumed conditional independence—that treatment assignment and potential outcomes are independent conditional on measured covariates—and checked for sufficient overlap, or common support, among observed characteristics in the risk-exposed and reference groups. If these two assumptions are met, propensity score methods enable unbiased estimates of treatment effects.
We took a similar approach in estimating the effect of provider encouragement on the likelihood of accessing a patient portal by first predicting the propensity to be encouraged to use a portal and then estimating the effect of encouragement on patient portal access (among those offered a portal). To examine whether the effect of provider encouragement varied by race/ethnicity, we included interaction terms between each racial/ethnic group and encouragement. We then re-estimated the effect of encouragement for each sub-group. Finally, we described reasons for not using a portal among those who were offered a patient portal but did not access it (overall and by race/ethnicity). More details on the statistical analysis and methodological assumptions can be found in Supplementary Appendix SB).
RESULTS
Descriptive analysis
Race/ethnicity, education, income, insurance status, having a regular provider, and access to the Internet were associated with being offered a patient portal (Table 1).
Table 1.
Sample characteristics for the overall study population and by those offered and not offered a patient portal, 2019–2020
| Offered a patient portalb |
||||
|---|---|---|---|---|
| All (N = 8028) (%) | Yes (61%, N = 4892) (%) | No (39%, N = 2993) (%) | Chi square | |
| Gender | ||||
| Female | 53 | 57 | 47 | χ2(1) = 75.14 |
| Male | 47 | 43 | 53 | P < .001 |
| Race/ethnicity | ||||
| Non-Hispanic White | 66 | 70 | 59 | |
| Non-Hispanic Black | 12 | 10 | 14 | χ2(4) = 131.76 |
| Non-Hispanic Asian | 5 | 5 | 5 | P < .001 |
| Non-Hispanic other or multiple races | 3 | 3 | 3 | |
| Hispanic | 14 | 11 | 19 | |
| Age (years) | ||||
| 18–34 | 23 | 23 | 24 | |
| 35–46 | 18 | 19 | 17 | χ2(3) = 22.50 |
| 47–64 | 36 | 38 | 34 | P = .07 |
| 65+ | 22 | 20 | 24 | |
| Education | ||||
| Less than high school | 7 | 3 | 11 | |
| High school grad | 2 | 18 | 28 | χ2(3) = 414.87 |
| Some college | 40 | 42 | 37 | P < .001 |
| College grad | 32 | 37 | 24 | |
| Income | ||||
| <$35,000 | 27 | 20 | 36 | |
| $35,000–$74,000 | 31 | 30 | 31 | χ2(2) = 262.16 |
| >$75,000 | 43 | 49 | 33 | P < .001 |
| Location | ||||
| Urban | 87 | 88 | 87 | χ2(1) = 3.06 |
| Rural | 13 | 12 | 13 | P = .33 |
| Insurance status | ||||
| Insured | 95 | 97 | 93 | χ2(1) = 73.43 |
| Uninsured | 5 | 3 | 7 | P < .001 |
| Chronic condition | ||||
| Yes | 62 | 64 | 60 | χ2(1) = 9.51 |
| No | 38 | 36 | 40 | P = .05 |
| Regular provider | ||||
| Yes | 72 | 78 | 61 | χ2(1) = 261.52 |
| No | 28 | 22 | 39 | P < .001 |
| Internet access typesa | ||||
| Broadband | 39 | 44 | 32 | χ2(1) = 126.01 P < .001 |
| Cellular | 60 | 66 | 52 | χ2(1) = 153.37 P < .001 |
| Wireless (Wi-Fi) | 73 | 79 | 63 | χ2(1) = 257.29 P < .001 |
| Dial-up | 2 | 1 | 3 | χ2(1) = 20.66 P = .01 |
| No internet access | 13 | 6 | 24 | χ2(1) = 501.55 P < .001 |
Note: Only includes respondents who had a healthcare visit in the past year. The last column reports results from a chi-square test of independence between respondent characteristics and being offered a patient portal
Internet access categories are not mutually exclusive.
Excludes 143 respondents who did not respond to the survey question about being offered a patient portal.
Table 2 reports unadjusted rates of individuals who were offered, accessed, or used a patient portal in 2019 and 2020. Compared to Whites, Black and Hispanic individuals were significantly less likely to be offered a patient portal by their healthcare provider (54% and 49%, respectively) and had significantly lower rates of patient portal access (overall and among those offered a portal). Rates of patient portal offers and access among individuals identifying as Asian and other or multiple races were similar to those observed for Whites with the exception of Asians being significantly more likely to access their patient portal once offered.
Table 2.
Percent of individuals who were offered, accessed, or used a patient portal in 2019–2020, stratified by race and ethnicity (unadjusted estimates)
| All (%) | White (%) | Black (%) | Hispanic (%) | Asian (%) | Other (%) | |
|---|---|---|---|---|---|---|
| Offered patient portal | 61 | 65 | 54*** | 49*** | 58 | 66 |
| Accessed patient portal | ||||||
| Overall | 45 | 49 | 36*** | 33*** | 50 | 44 |
| Among offered | 69 | 71 | 62** | 59** | 81** | 64 |
| Used patient portal (among offered and accessed) | ||||||
| View test results | 87 | 88 | 84 | 81 | 96*** | 85 |
| Download or transmit | 39 | 36 | 45** | 45 | 53** | 55 |
| Message HCP | 57 | 55 | 62 | 54 | 74*** | 70 |
Note: Only includes respondents who had a healthcare visit in the past year. Asterisks indicate statistically significant differences in race/ethnicity (with White as the reference category) and patient portal offers, access, and use.
P < .01,
P < .05.
Abbreviation: HCP: healthcare provider
Among individuals who were offered and accessed their patient portal, most used their portal for at least one purpose including to view test results (87%), download or transmit health information (39%), or message their healthcare provider (57%). While individuals identifying as Black, Hispanic, and other or multiple races reported slightly lower rates of portal use for viewing test results compared to Whites, they reported significantly higher rates of portal use to download or transmit information. Compared to White individuals, rates of portal use among Asians were higher across all functionalities.
Multivariable regression analysis
Patient portal offers
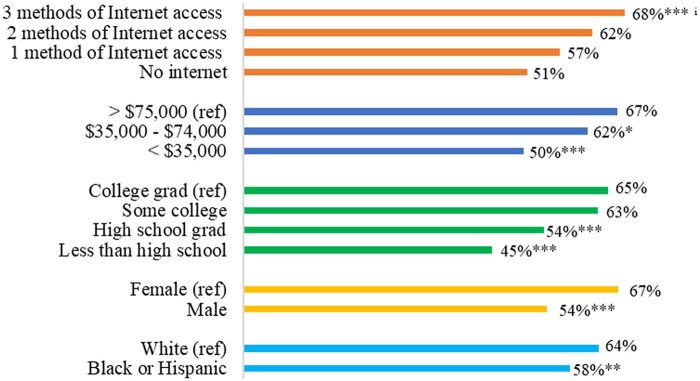
Table 3 reports adjusted estimates from separate weighted LPMs estimating the effect of race and ethnicity on the likelihood of being offered, accessing, or using a patient portal. The predicted probability of being offered a patient portal was significantly lower for Black and Hispanic individuals combined (58%) compared to White individuals (64%) (Figure 1). This corresponds to a 5.2 percentage-point reduction in the likelihood of being offered a patient portal (P < .05) for respondents who identified as Black or Hispanic (Table 3, panel A). When examined separately, compared to Whites, Black and Hispanic individuals were 5.3 and 5.4 (P < .05) percentage-points less likely to be offered a patient portal, respectively.
Table 3.
Marginal effects of race and ethnicity on the likelihood of being offered, accessing, or using a patient portal, 2019–2020 (adjusted estimates)
| Panel A: patient portal offers from HCP | |||
|---|---|---|---|
| Offered | |||
| Black or Hispanic (vs White) | −0.0524** (0.0221) | ||
| Black (vs White) | −0.0534 (0.0318) | ||
| Hispanic (vs White) | −0.0535** (0.0264) | ||
| Panel B: patient portal access | |||
|---|---|---|---|
| Accessed | Accessed (among offered) | ||
| Black or Hispanic (vs White) | −0.0717*** (0.0208) | −0.0792** (0.0332) | |
| Black (vs White) | −0.0715** (0.0299) | −0.0778 (0.0419) | |
| Hispanic (vs White) | −0.0637** (0.0288) | −0.0691 (0.0452) | |
| Panel C: patient portal use among those who were offered and accessed their portal | |||
|---|---|---|---|
| View test results | Download or transmit | Message HCP | |
| Black or Hispanic (vs White) | −0.0323 (0.0310) | 0.122*** (0.0367) | 0.0305 (0.0384) |
| Black (vs White) | −0.0135 (0.0355) | 0.129*** (0.0444) | 0.0573 (0.0499) |
| Hispanic (vs White) | −0.0277 (0.0345) | 0.135*** (0.0507) | 0.0263 (0.0455) |
Note: Panels A–C report marginal effects (ME) derived from separate weighted linear probability models that control for gender, education, income, rurality, insurance status, chronic condition, having a regular healthcare provider, and number of internet access types. The analytical weight is the survey weight interacted with the inverse of the propensity score. Standards errors (SE) are in parentheses. Reported estimates in each cell indicate the marginal effect of being in each risk-exposed group (ie, Black or Hispanic, Black only, or Hispanic only relative to White) on the likelihood of being offered a patient portal (panel A), accessing the portal (panel B), or using the portal to view test results, download or transmit information, and message with a healthcare provider (HCP) (panel C). All analyses control for respondent characteristics and were restricted to respondents who had a healthcare visit in the last year. Full regression output is available in the Appendix. Standard errors are in parentheses.
P < .01,
P < .05.
Figure 1.
Predicted probabilities of being offered a patient portal.
Note: Predicted probabilities correspond to the model presented in Supplementary Table SA1, column 1. Access types include broadband (such as DSL, cable, or FiOS), cellular network (eg, phone, 3G/4G), and/or wireless network (ie, Wi-Fi). iAn additional access type significantly increases the likelihood of being offered a patient portal by 5.8 percentage-points (P < .01). ***P < .01, **P < .05.
Males, individuals with a high school education or less, and those with annual household incomes below $75 000 had significantly lower predicted probabilities of being offered a patient portal compared to females, college-educated individuals, and those earning more than $75 000 (Figure 1). Conversely, individuals with internet access, insurance, a chronic condition or regular healthcare provider had significantly higher predicted probabilities of being offered a patient portal. On average, an additional internet access type increased the likelihood of being offered a patient portal by 5.8 percentage-points (P < .01) (Supplementary Table SA1).
Patient portal access
Identifying as Black or Hispanic was associated with a 7.2 percentage-point reduction in the likelihood of accessing a patient portal (P < .01) (Table 3, panel B). Separately, Black and Hispanic individuals were 7.2 and 6.4 percentage-points less likely to access their patient portal, respectively, compared to Whites (P < .05). Once we conditioned on being offered a patient portal, Black and Hispanic individuals combined were nearly 8 percentage-points less likely to access a patient portal (P < .05), however, individual estimates were no longer statistically significant.
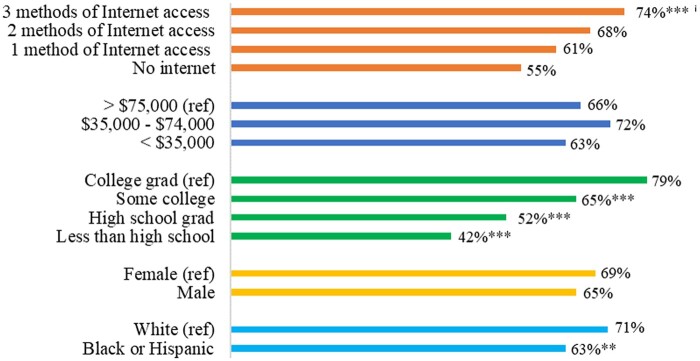
Individuals with less than a college degree had a significantly lower predicted probability of accessing a portal compared to those with a college degree regardless of receiving an offer (Figure 2). Internet access was also a significant predictor of patient portal access across analyses. On average, an additional internet access type increased the likelihood of accessing a patient portal among those offered by almost 6.5 percentage-points (P < .01). Having a regular provider was a significant predictor of patient portal access for Hispanic individuals, but not for Black individuals (Supplementary Table SA2).
Figure 2.
Predicted probabilities of accessing a patient portal (among offered).
Note: Predicted probabilities correspond to the model presented in Supplementary Table SA2, column 4. Access types include broadband (such as DSL, cable, or FiOS), cellular network (eg, phone, 3G/4G), and/or wireless network (ie, Wi-Fi). iAn additional access type significantly increases the likelihood of accessing a patient portal (among offered) by 6.5 percentage-points (P < .01). ***P < .01, **P < .05.
Patient portal use
Differences in patient portal use were examined among respondents who were offered and accessed a patient portal. While Black and Hispanic respondents were less likely than Whites to use their portal to view test results and more likely to message with their provider, these differences were not statistically significant. In contrast, Black and Hispanic respondents were 12 percentage-points more likely to use their patient portal to download or transmit information (P < .01) (Table 3, panel C). After accounting for patient portal offers and access, gender, education, and income were not strong predictors of portal use. Having more methods by which to access the Internet, however, was generally associated with increased usage. An additional method of accessing the Internet increased the likelihood of use by approximately 4 to 8 percentage-points (Supplementary Tables SA3–SA5).
Role of provider encouragement
Table 4 reports adjusted estimates from separate weighted LPMs estimating the effect encouragement on the likelihood of accessing a patient portal for the overall sample and stratified by race and ethnicity. Overall, individuals who were offered a patient portal and encouraged to use it by their healthcare provider were 21 percentage-points more likely to access their portal compared to those who were not encouraged (P < .01). Being offered and encouraged to use a patient portal by a healthcare provider was a strong predictor of patient portal access in the overall sample and across different racial and ethnic groups, however, the effect of encouragement was not statistically significant in the Black stratified sample. While the marginal effects of encouragement varied by race and ethnicity (columns 2–4), coefficients on the interaction terms between race/ethnicity and encouragement included in the overall sample (column 1) were not statistically significant, suggesting there were no meaningful differences in the effect of encouragement across racial/ethnic groups (Supplementary Table SA6).
Table 4.
Marginal effects of encouragement on the likelihood of accessing a patient portal (among those who were offered a patient portal), overall and stratified by race and ethnicity, 2020 (Adjusted estimates)
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Variables | All respondents | White | Black or Hispanic | Black | Hispanic |
| Encouraged | 0.214*** (0.0620) | 0.220*** (0.0597) | 0.206** (0.102) | 0.199 (0.134) | 0.260** (0.123) |
| Observations | 1792 | 1192 | 458 | 241 | 217 |
Note: Columns (1)–(5) report marginal effects derived from separate weighted linear probability models that control for gender, education, income, rurality, insurance status, chronic condition, having a regular healthcare provider, and number of internet access types. The analytical weight is the survey weight interacted with the inverse of the propensity score. Column (1) includes all respondents; this specification controlled for race/ethnicity as a categorical variable (White is the reference group) and included a set of interaction terms between race/ethnicity and encouragement (estimates on the interactions were not statistically significant). Columns (2)–(5) report results from analyses stratified by White, Black or Hispanic, Black, and Hispanic, respectively. All analyses were restricted to respondents who went to the doctor in the last year and those who reported being offered a patient portal by their healthcare provider. Standard errors are in parentheses.
P < .01,
P < .05.
All analyses were restricted to respondents who had a healthcare visit in the past year and who reported being offered a portal by their healthcare provider. Standard errors are in parentheses. Full regression output is available in the Supplementary Appendix.
Reasons for not using a portal
To understand whether there may be differences in the perceived utility of patient portals that contribute to disparities in access and use, we explored reasons for not using a patient portal among respondents who were offered a portal, but did not access or use it. Overall, preferences for speaking with a healthcare provider directly and perceived lack of need to access online medical records were the most common reasons provided for not accessing a patient portal among those offered (77% and 63%, respectively) (Table 5). Compared to Whites, Black individuals were significantly more likely to indicate they did not access their portal because they preferred to speak with their provider directly (91%, P < .01) or were concerned about the privacy or security of the website (33%, P < .05). There were no significant differences in reasons for not accessing a patient portal among Hispanic and White individuals.
Table 5.
Reasons for not accessing a patient portal among individuals who were offered a portal and had a healthcare visit in the past year, stratified by race and ethnicity
| Overall (%) | White (%) | Black (%) | Hispanic (%) | |
|---|---|---|---|---|
| Prefer to speak to your healthcare provider directly | 77 | 78 | 91*** | 63 |
| Did not have a need to use online medical record | 63 | 65 | 52 | 61 |
| Found it difficult to login | 27 | 27 | 23 | 28 |
| Concerned about the privacy or security of the website | 22 | 19 | 33** | 27 |
| Not comfortable or experienced with computers | 23 | 21 | 27 | 27 |
| Do not have a way to access the website | 14 | 14 | 16 | 15 |
| Don't have an online medical record | 12 | 12 | 12 | 13 |
| More than one online medical record | 11 | 11 | 5** | 9 |
Note: All analyses were restricted to respondents who went to the doctor in the last year and those who reported being offered a patient portal by their healthcare provider.
P < .01,
P < .05.
DISCUSSION
Consistent with earlier studies investigating disparities in patients’ engagement with their EHI via a patient portal,18–27 we found that in 2019 and 2020, Black and Hispanic individuals reported being offered and subsequently accessing patient portals at significantly lower rates than White individuals. In multivariable models, Black and Hispanic individuals were significantly less likely than Whites to report being offered a patient portal and to access it. However, once we conditioned on being offered a portal, differences in access were no longer significant in the nonpooled samples, which suggests differences in access may be driven by disparities in being offered a portal and points to the importance of healthcare providers offering portals to promote access. Encouragingly, we found little evidence of differences in patient portal use among individuals who reported they were offered and subsequently accessed their portal. Rates of portal use to view test results and message with providers were similar across racial/ethnic groups, whereas Black and Hispanic individuals were more likely than Whites to use their portal to download or transmit information.
Overall, our findings suggest that while there are varied reasons for not accessing a portal, providers’ lack of consistency in offering patients access to portals remains a limiting factor to broadening patient access and use of EHI. Given that EHR developers have largely chosen to authorize third-party health app connections to their IT systems32 using the patient portal credentials issued to individual patients,33 limited portal access may diminish patients’ ability to take advantage of modern tools to access and manage their health information. To reap the full benefits of polices aimed at increasing patient access to EHI, it is critical to foster practices that lead to equitable access and use.34 This includes encouraging the adoption of information-sharing best practices, addressing access-related barriers to use, and facilitating conversations that alleviate patient concerns around the privacy and security of EHI. Our findings also indicate that individuals who were offered a patient portal and encouraged to use it were significantly more likely to access their portal compared to those who were offered but not encouraged, which speaks to the importance of healthcare provider conversations around patient portal access and use.
Taken together, our findings indicate that providers can play an important role in promoting patient engagement with EHI via patient portals. However, as evidenced from prior analyses of hospital-level data,13 smaller practices and lower-resourced healthcare providers who serve disadvantaged populations may be less likely to have EHRs that possess certain patient engagement capabilities, and therefore less likely to offer patient portals or encourage their use. Given that access and use did not vary substantially by race and ethnicity once individuals were offered access to a patient portal, interventions that increase availability and awareness of patient engagement functions and incentivize providers to encourage the use of these features could be an important means to increasing access and use of EHI among diverse populations.
To date, interventions to address disparities in portal use have been limited. Efforts have largely focused on targeting patients rather than educating providers and health IT developers or implementing structural solutions that promote equitable access to EHI. Multi-pronged interventions that make it easier for patients to access their EHI and broaden access via organizational policies and provider incentives may be more effective at addressing disparities in portal use. For example, implementing a “universal access” policy requiring providers to offer patient portal enrollment is one strategy that could help increase patient portal offers and subsequent use.35
However, it is important to note that being encouraged to use a portal was not equally effective in increasing access in our study and, as evidenced by reasons for not using a patient portal, nor is it the only factor that influences individual decisions to access and use EHI. Thus, a one-size approach may not be effective in addressing underlying issues related to patient access. Effective interventions should aim to resolve specific barriers to access and use. In exploring reasons for not using a portal among those who were offered, Black individuals were significantly more likely than Whites to indicate they preferred to speak with their provider directly. They were also more likely to indicate other barriers to use—such as privacy or security concerns. These findings are consistent with prior qualitative research that identified fear of eroding personal relationships with providers and concerns related to the security and privacy of online information as barriers to portal use among Black or African American patients.36 These findings reinforce the importance of building patient-provider trust, which in turn, can help increase communication between patients and providers. However, achieving meaningful engagement may require employing community-based interventions that leverage trusted sources to address privacy and security concerns and communicate the benefits of having access to EHI. Using trusted sources to provide tangible examples of how patient portals and health apps can be used to message with providers, manage health conditions, and participate in healthcare decision-making may serve to increase access and use among hesitant populations.
Beyond issues related to patient-provider trust, low rates of patient portal offers and access among Hispanic populations may also stem from language barriers, which can diminish the utility of patient portals as well as hinder patient-provider conversations around access and use. Consequently, providers may be less likely to offer patient portals to individuals they perceive to have limited English proficiency (LEP). While several major EHR developers offer patient portals in Spanish, most do not have multilingual resources for a broad range of languages.37 Moreover, it is unclear whether providers are aware of these capabilities or feel equipped to convey this information to LEP patients. Resources to help providers communicate effectively with LEP patients could help reduce disparities in patient portal access and ultimately use. Furthermore, requiring multi-lingual portals to be uniformly available and offering patient educational materials in multiple languages may improve patient portal access and use among Hispanic individuals and LEP individuals more broadly.38,39
Given persistent racial and ethnic disparities in patients reporting being offered access to their medical records via a patient portal, policy efforts aimed at making it easier for patients to access their EHI should embrace the concept of health equity by design.34,40 For instance, given that Black and Hispanic portal users may be more likely to use mobile devices to access EHI,41,42 promoting access through mobile health apps could increase access to EHI through features that enable easy log-in access, real-time tracking, and simplified data display.43 However, as portal access currently remains a prerequisite for accessing one’s data through a health app since patient portal credentials are often required to authorize health apps to receive their EHI from within an EHR, eliminating racial and ethnic disparities in patient portal offers is critical to ensuring equitable access and use of health apps.
LIMITATIONS
One potential limitation of this study is our inability to capture unobserved preferences related to portal use—such as attitudinal barriers, general distrust for the healthcare system, or other factors that may influence access and use—and thus our propensity score estimates may produce biased results since we can only balance observed covariates.44 Another limitation of this study is the use of a cross-sectional, self-report survey to make inferences about provider behavior which may be subject to recall and nonresponse bias. For instance, our results may be biased if individuals with limited technology access or familiarity with health IT were less likely to recall being offered a patient portal by their provider. We aimed to mitigate this limitation by restricting the sample to individuals who had a healthcare visit in the past year and by controlling for characteristics—for example, internet access, having a regular provider or chronic condition—that may affect an individual’s recall or frequency of interaction with their healthcare provider and patient portal. Finally, we are limited in our ability to detect the full extent of potential racial/ethnic disparities in patient portal offers, access, and use by our use of a simplified categorization of race/ethnicity, which does not fully represent the diversity of races and ethnicities present in the United States.
CONCLUSION
In 2019 and 2020, Black and Hispanic individuals were less likely to report being offered a patient portal compared to their White counterparts. While there were significant differences in rates of patient portal access and use at the national level, race and ethnicity were not strong predictors of patient portal access and use in multivariable analyses once we conditioned on being offered a patient portal. Our findings suggest that differences in access and use are likely driven by disparities in whether a patient is offered a portal. Moreover, our findings indicate that provider encouragement significantly increased the likelihood of access and use among those offered a portal.
Our findings point to the role healthcare providers play in exacerbating and ameliorating racial and ethnic disparities in patients’ access and use of their EHI. These findings are somewhat encouraging because they indicate portal access and use can be influenced by tailored efforts that ensure patient portals are being offered consistently—regardless of race, ethnic origin, or native language—and incentivize healthcare providers to encourage their use. As ONC embarks on expanding access to EHI through health apps it is critical to monitor disparities in patient access to EHI, as well as assess the impact of interventions that engage specific populations of focus and policy efforts aimed at reducing disparities in patient portal access and use.
Supplementary Material
Contributor Information
Chelsea Richwine, Office of the National Coordinator for Health Information Technology, Office of Technology, Washington, District of Columbia, USA.
Christian Johnson, Office of the National Coordinator for Health Information Technology, Office of Technology, Washington, District of Columbia, USA.
Vaishali Patel, Office of the National Coordinator for Health Information Technology, Office of Technology, Washington, District of Columbia, USA.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
AUTHOR CONTRIBUTIONS
All authors contributed to the study concept and design, drafting, and critical editing of the manuscript. CR is responsible for the accuracy and final contents of the article.
SUPPLEMENTARY MATERIAL
Supplementary material is available at JAMIA Open online.
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
The data underlying this article are available on the Health Information National Trends website, which can be found here: https://hints.cancer.gov/data/download-data.aspx.
REFERENCES
- 1. Office of the National Coordinator for Health Information Technology. Office-Based Physician Electronic Health Record Adoption, Health IT Quick-Stat #50. https://www.healthit.gov/data/quickstats/office-based-physician-electronic-health-record-adoption. Accessed April 2022.
- 2. Office of the National Coordinator for Health Information Technology. Non-Federal Acute Care Hospital Electronic Health Record Adoption, Health IT Quick-Stat #47. https://www.healthit.gov/data/quickstats/non-federal-acute-care-hospital-electronic-health-record-adoption. Accessed April 2022.
- 3. U.S. Department of Health and Human Services. Health Information Privacy, February 2017. https://www.hhs.gov/hipaa/for-individuals/guidance-materials-for-consumers/index.html. Accessed May 2022.
- 4.21st Century Cures Act, Pub. L. No. 114-255, 130 Stat. 1033, Title IV, Sec 4006. December 13, 2016.
- 5. U.S. Department of Health and Human Services. HIPAA for Individuals: Get It. Check It. Use It, January 2020. https://www.hhs.gov/hipaa/for-individuals/right-to-access/index.html
- 6. Dendere R, Slade C, Burton-Jones A, Sullivan C, Staib A, Janda M.. Patient portals facilitating engagement with inpatient electronic medical records: a systematic review. J Med Internet Res 2019; 21 (4): e12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Epic Research. Shorter Hospital Stays Associated with Patient Portal Use, November 17, 2021. https://epicresearch.org/articles/shorter-hospital-stays-associated-with-patient-portal-use.
- 8. James J. Patient engagement. Health Affairs Health Policy Brief 2013; Feb 14: 1–6. doi: 10.1377/hpb20130214.898775. [DOI] [Google Scholar]
- 9. U.S. Department of Health and Human Services. Medicare and Medicaid Programs: Electronic Health Record Incentive Program – Stage 2, September 2012. https://www.govinfo.gov/content/pkg/FR-2012-09-04/pdf/2012-21050.pdf. [PubMed]
- 10. Office of the National Coordinator for Health Information Technology. Certification of Health IT. View, Download, and Transmit to 3rd Party. https://www.healthit.gov/test-method/view-download-and-transmit-3rd-party. Accessed May 2022.
- 11. Coelius RM. Get the Facts Regarding View, Download and Transmit 2014 Requirements, January 31, 2014. https://www.healthit.gov/buzz-blog/meaningful-use/view-download-transmit-facts
- 12. National Center for Health Statistics. 2019 National Electronic Health Records Survey Public Use File National Weighted Estimates, August 2021. https://www.cdc.gov/nchs/data/nehrs/2019NEHRS-PUF-weighted-estimates-508.pdf.
- 13. Johnson C, Pylypchuk Y. Use of Certified Health IT and Methods to Enable Interoperability by U.S. Non Federal Acute Care Hospitals, 2019. ONC Data Brief, No. 54. Washington, DC: Office of the National Coordinator for Health Information Technology; February 2021.
- 14. Westat. HINTS 5, Cycle 4 (2020) Dataset. https://hints.cancer.gov/data/download-data.aspx/. Accessed February 28, 2022.
- 15. Westat. HINTS 4, Cycle 4 (2014) Dataset. https://hints.cancer.gov/data/download-data.aspx. Accessed February 28, 2022.
- 16. Patel V, Johnson C. Trends in Individuals’ Access and Use of Online Medical Records and Technology for Health Needs: 2017-2018. ONC Data Brief, No. 48. Washington, DC: Office of the National Coordinator for Health Information Technology; May 2019. https://www.healthit.gov/sites/default/files/page/2019-05/Trends-in-Individuals-Access-Viewing-and-Use-of-Online-Medical-Records-and-Other-Technology-for-Health-Needs-2017-2018.pdf.
- 17. Otokiti A, Williams KS, Warsame L.. Impact of digital divide on the adoption of online patient portals for self-motivated patients. Healthc Inform Res 2020; 26 (3): 220–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ancker JS, Barrón Y, Rockoff ML, et al. Use of an electronic patient portal among disadvantaged populations. J Gen Intern Med 2011; 26 (10): 1117–23. Oct 1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Peacock S, Reddy A, Leveille SG, et al. Patient portals and personal health information online: perception, access, and use by US adults. J Am Med Inform Assoc 2017; 24 (e1): e173–e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gordon NP, Hornbrook MC.. Differences in access to and preferences for using patient portals and other eHealth technologies based on race, ethnicity, and age: a database and survey study of seniors in a large health plan. J Med Internet Res 2016; 18 (3): e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wallace LS, Angier H, Huguet N, et al. Patterns of electronic portal use among vulnerable patients in a nationwide practice-based research network: from the OCHIN practice-based research network (PBRN). J Am Board Fam Med 2016; 29 (5): 592–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Goel MS, Brown TL, Williams A, Hasnain-Wynia R, Thompson JA, Baker DW.. Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med 2011; 26 (10): 1112–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Roblin DW, Houston TK 2nd, Allison JJ, Joski PJ, Becker ER.. Disparities in use of a personal health record in a managed care organization. J Am Med Inform Assoc 2009; 16 (5): 683–9. [PMID: 19567790] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc 2011; 18 (3): 318–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Anthony DL, Campos-Castillo C, Lim PS.. Who isn’t using patient portals and why? Evidence and implications from a national sample of US adults. Health Aff (Millwood) 2018; 37 (12): 1948–54. [DOI] [PubMed] [Google Scholar]
- 26. Trivedi N, Patel V, Johnson C, Wen-Ying SC.. Barriers to accessing online medical records in the United States. Am J Manag Care 2021; 27 (1): 33–40. [DOI] [PubMed] [Google Scholar]
- 27. Shimoga SV, Lu YZ.. Role of provider encouragement on patient engagement via online portals. J Am Med Inform Assoc 2019; 26 (10): 968–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.21st Century Cures Act: Interoperability, Information Blocking, and the ONC Health IT Certification Program. 45 C.F.R. Parts 170 and 171. Proposed Rule; March 4, 2019.
- 29. Westat. HINTS 5 Cycle 1 Methodology Report; 2020. https://hints.cancer.gov/docs/methodologyreports/HINTS5_Cycle4_MethodologyReport.pdf. Accessed February 28, 2022.
- 30. Westat. HINTS 5 Cycle 2 Methodology Report; 2019. https://hints.cancer.gov/docs/Instruments/HINTS5_Cycle3_MethodologyReport.pdf. Accessed February 28, 2022.
- 31. Ye Y, Bond JC, Schmidt LA, Mulia N, Tam TW.. Toward a better understanding of when to apply propensity scoring: a comparison with conventional regression in ethnic disparities research. Ann Epidemiol 2012; 22 (10): 691–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Health Level Seven. SMART APP Launch Implementation Guide (v2.0.0: STU 2). http://www.hl7.org/fhir/smart-app-launch/. Accessed August 15, 2022.
- 33. Apple Registration Guide for Healthcare Organizations. Health App Data Share with Provider FAQ. https://support.apple.com/guide/healthregister/health-app-data-share-with-provider-faq-apd531bc6215/web. Accessed August 15, 2022.
- 34. Brewer LC, Fortuna KL, Jones C, et al. Back to the future: achieving health equity through health informatics and digital health. JMIR Mhealth Uhealth 2020; 8 (1): e14512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Grossman LV, Masterson Creber RM, Benda NC, Wright D, Vawdrey DK, Ancker JS.. Interventions to increase patient portal use in vulnerable populations: a systematic review. J Am Med Inform Assoc 2019; 26 (8–9): 855–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lyles CR, Allen JY, Poole D, Tieu L, Kanter MH, Garrido T.. “I want to keep the personal relationship with my doctor”: understanding barriers to portal use among African Americans and Latinos. J Med Internet Res 2016; 18 (10): e5910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Health Information Technology, Evaluation, and Quality Center. Multi-Lingual Patient Portal Status and Resources for Health Centers, December 2016. https://hiteqcenter.org/Resources/Electronic-Patient-Engagement/Patient-Portals/multi-lingual-patient-portal-status-and-resources-for-health-centers.
- 38. Ancker JS, Nosal S, Hauser D, Way C, Calman N.. Access policy and the digital divide in patient access to medical records. Health Policy Technol2017 2017; 6 (1): 3–11. [Google Scholar]
- 39. Tan-McGrory A, Schwamm LH, Kirwan C, Betancourt JR, Barreto EA.. Addressing virtual care disparities for patients with limited English proficiency. Am J Manag Care 2022; 28 (1): 36–40. [DOI] [PubMed] [Google Scholar]
- 40. Argentieri R, Mason TA, Hefcart J, Henry J. Embracing Health Equity by Design, February 22, 2022. https://www.healthit.gov/buzz-blog/health-it/embracing-health-equity-by-design
- 41. Chang E, Blondon K, Lyles C, Jordan L, Ralston J.. Racial/ethnic variation in devices used to access patient portals. Am J Manag Care 2018; 24 (1): e1–e8. [PubMed] [Google Scholar]
- 42. Ray R, Sewell AA, Gilbert KL, Roberts JD.. Missed opportunity? Leveraging mobile technology to reduce racial health disparities. J Health Polit Policy Law 2017; 42 (5): 901–24. [DOI] [PubMed] [Google Scholar]
- 43. Baldwin JL, Singh H, Sittig DF, Giardina TD.. Patient portals and health apps: Pitfalls, promises, and what one might learn from the other. Healthc (Amst) 2017; 5 (3): 81–5. Sep [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Goel MS, Brown TL, Williams A, Cooper AJ, Hasnain-Wynia R, Baker DW.. Patient reported barriers to enrolling in a patient portal. J Am Med Inform Assoc 2011; 18 (Supplement 1): i8–i12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available on the Health Information National Trends website, which can be found here: https://hints.cancer.gov/data/download-data.aspx.