Dear Editor
On 9th December 2021, a COVID-19 outbreak was discovered in Xi'an and Zhengzhou in China, causing an overwhelming threat to the city's health care system. The support was requested throughout the National Health Commission of the People's Republic of China, and numerous healthcare workers (HCWs), including physicians and nurses, volunteered to assist the two cities. Notably, the prolonged pandemic has caused a heavy physical and psychological burden, affecting the economy, social life, and others as a massive challenge. The rapidly increasing number of patients quickly overdraw medical resources, resulting in a shortage of HCWs and devices all over the country. Recent studies (Eftekhar et al., 2021) show that HCWs often experience the occurrence and transformation of various negative emotions during the pandemic. Negative emotions in HCWs may impact their health and hinder the patient's daily care, with worse outcomes (Coifman et al., 2021). Studies have also examined the relationship between perceived stress and social support among HCWs concerning occupational stressors and psychosomatic symptoms (Zou et al., 2022). However, there are few studies on the psychosomatic symptoms of HCWs in the context of the pandemic. These conditions have impacted the pandemic itself and society, posing a severe threat to the population's health, especially the mental health and psychosomatic symptoms of HCWs.
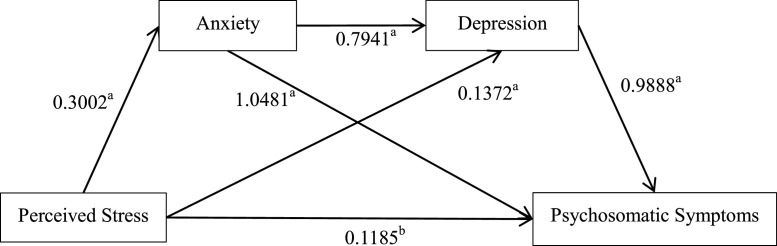
We recruited 344 HCWs. Psychosomatic Symptom Scale, the Chinese perceived stress scales, 7-item Generalized Anxiety Disorder Scale, and 9-item Patient Health Questionnaire were assessed. Forty-six cases were excluded due to invalid questionnaires and incomplete information. 288 HCWs, 32 males (11.11%) and 256 females (88.89%) , were included for further analysis. We found that 101 HCWs (35.07%) reported psychosomatic symptoms. HCWs with psychosomatic symptoms also exhibited higher perceived stress, more severe anxiety, and depressed mood (P < 0.001). Multiple linear regression analysis showed that anxiety, depression, and perceived stress were significant predictors of psychosomatic symptoms of HCWs, which explained 69.1% of the variance of psychosomatic symptoms. Correlation analysis revealed a significant correlation between the four variables of psychosomatic symptoms, anxiety, depression, and perceived stress among HCWs (P < 0.001). We observed a significant mediating effect of anxiety and depression on the association between perceived stress and psychosomatic symptoms (effect value = 0.236, Standard Error = 0.050, Bootstrap 95% CI = 0.147 to 0.341).
The study revealed that more than one-third of participants had psychosomatic symptoms and exhibited severer anxiety, depression, and perceived stress. Providing health and safety measures, psychological support, and improving safety and confidence is helpful to HCWs (Marinaci et al., 2021). Stress, anxiety, and depression were associated with psychosomatic burden in HCWs. Anxiety and depression mediated between perceived stress and psychosomatic symptoms. The chain intermediary analysis also shows that emotions such as anxiety and depression mediate between perceived stress and psychosomatic symptoms in HCWs. Health system personnel and policymakers should prioritize their mental health and implement appropriate interventions to reduce depression and anxiety (Ullah et al., 2022).
The main strengths of this study are that it provided a sketch of the psychosomatic symptoms of the HCW during the prolonged pandemic. We revealed that perceived stress among HCWs might lead to psychosomatic symptoms. Meanwhile, we provided implications for developing psychological prevention and intervention programs for other HCWs who suffer from psychosomatic problems during similar events. The study was cross-sectional, with a relatively small sample size. Future studies should include more participants from different regions for a more representative sample. Follow-up and active surveillance of psychosomatic symptoms in HCWs were essential to maintain their health, work efficiency, and life quality (Fig. 1 and Table 1 ).
Fig. 1.
Mediated effect of anxiety and depression in the relationship between perceived stress and psychosomatic symptoms in healthcare workers.
Note: aP <0.001, bP <0.05.
Table 1.
Demographics and assessments.
| Variables | Group with PSSS≥10 |
Group with PSSS<10 |
Z/X2 value |
P value |
|---|---|---|---|---|
| (n=101) | (n=187) | |||
| Gender (n, %) | 1.603b | 0.205 | ||
| Male | 8 (2.78) | 24 (8.33) | ||
| Female | 93 (32.29) | 163 (56.60) | ||
| Age [years, M (P25, P75)] | 31 (27.50, 35) | 32 (28, 37) | -1.504a | 0.133 |
| Occupation (n, %) | 0.995b | 0.319 | ||
| Physicians | 9 (3.13) | 24 (8.33) | ||
| Nurses | 92 (31.94) | 163 (56.60) | ||
| Education level (n, %) | 0.950b | 0.813 | ||
| College | 9 (3.13) | 14 (4.86) | ||
| Undergraduate | 80 (27.78) | 145 (50.35) | ||
| Master | 10 (3.47) | 21 (7.29) | ||
| Doctorate | 2 (0.69) | 7 (2.43) | ||
| Marital Status (n, %) | 1.093b | 0.579 | ||
| Unmarried | 31 (10.76) | 56 (19.44) | ||
| Married | 70 (24.31) | 129 (44.79) | ||
| Divorced | 0 | 2 (0.69) | ||
| CPSS [Scores, M (P25, P75)] | 28 (25, 31) | 17 (12, 23) | -9.556a | < 0.001 |
| GAD-7 [Scores, M (P25, P75)] | 7 (5.50, 10) | 1 (0, 3) | -11.448a | < 0.001 |
| PHQ-9 [Scores, M (P25, P75)] | 9 (7, 13) | 2 (0, 5) | -11.959a | < 0.001 |
a: Z value, b: X2 value, PSSS: Psychosomatic Symptom Scale, CPSS: Chinese Perceived Stress Scale, GAD-7: 7-item Generalized Anxiety Disorder Scale, PHQ-9: 9-item Patient Health Questionnaire.
Declaration of Competing Interest
None.
References
- Coifman KG, Disabato DD, Seah THS, Ostrowski-Delahanty S, Palmieri PA, Delahanty DL, Gunstad J. Boosting positive mood in medical and emergency personnel during the COVID-19 pandemic: preliminary evidence of efficacy, feasibility and acceptability of a novel online ambulatory intervention. Occup. Environ. Med. 2021 doi: 10.1136/oemed-2021-107427. oemed-2021-107427. [DOI] [PubMed] [Google Scholar]
- Eftekhar AM, Naserbakht M, Bernstein C, Alazmani-Noodeh F, Hakimi H, Ranjbar H. Healthcare providers experience of working during the COVID-19 pandemic: a qualitative study. Am. J. Infect. Control. 2021;49(5):547–554. doi: 10.1016/j.ajic.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marinaci T, Venuleo C, Gennaro A, Sammut G. Making sense of the COVID-19 pandemic: A qualitative longitudinal study investigating the first and second wave in Italy. Heliyon. 2021;7(9):e07891. doi: 10.1016/j.heliyon.2021.e07891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullah I, Khan KS, Ali I, Ullah AR, Mukhtar S, de Filippis R, Malik NI, Shalbafan M, Hassan Z, Asghar MS. Depression and anxiety among Pakistani healthcare workers amid COVID-19 pandemic: a qualitative study. Ann. Med. Surg. 2022;78(2012) doi: 10.1016/j.amsu.2022.103863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou Y, Lu Y, Zhou F, Liu X, Ngoubene-Atioky AJ, Xu K, Hong L, Shen G, Wu H, Cai Z, Liu Y, Chen L, Bao D. Three mental health symptoms of frontline medical staff associated with occupational stressors during the COVID-19 peak outbreak in China: the mediation of perceived stress and the moderation of social support. Front. Psychol. 2022;13 doi: 10.3389/fpsyg.2022.888000. [DOI] [PMC free article] [PubMed] [Google Scholar]