Abstract
Among the novel mutations distinguishing SARS-CoV-2 from similar coronaviruses is a K403R substitution in the receptor-binding domain (RBD) of the viral spike (S) protein within its S1 region. This amino acid substitution occurs near the angiotensin-converting enzyme 2–binding interface and gives rise to a canonical RGD adhesion motif that is often found in native extracellular matrix proteins, including fibronectin. Here, the ability of recombinant S1-RBD to bind to cell surface integrins and trigger downstream signaling pathways was assessed and compared with RGD-containing, integrin-binding fragments of fibronectin. We determined that S1-RBD supported adhesion of fibronectin-null mouse embryonic fibroblasts as well as primary human small airway epithelial cells, while RBD-coated microparticles attached to epithelial monolayers in a cation-dependent manner. Cell adhesion to S1-RBD was RGD dependent and inhibited by blocking antibodies against αv and β3 but not α5 or β1 integrins. Similarly, we observed direct binding of S1-RBD to recombinant human αvβ3 and αvβ6 integrins, but not α5β1 integrins, using surface plasmon resonance. S1-RBD adhesion initiated cell spreading, focal adhesion formation, and actin stress fiber organization to a similar extent as fibronectin. Moreover, S1-RBD stimulated tyrosine phosphorylation of the adhesion mediators FAK, Src, and paxillin; triggered Akt activation; and supported cell proliferation. Thus, the RGD sequence of S1-RBD can function as an αv-selective integrin agonist. This study provides evidence that cell surface αv-containing integrins can respond functionally to spike protein and raises the possibility that S1-mediated dysregulation of extracellular matrix dynamics may contribute to the pathogenesis and/or post-acute sequelae of SARS-CoV-2 infection.
Keywords: SARS-CoV-2, Receptor binding domain, Fibronectin, Extracellular matrix protein, Integrin, Cell adhesion, Focal adhesions
Abbreviations: ACE2, angiotensin-converting enzyme 2; CoV, coronavirus; ECM, extracellular matrix; FAK, focal adhesion kinase; FN-null MEF, fibronectin-null mouse embryonic fibroblast; GST, glutathione S-transferase; RBD, receptor-binding domain; RGD, Arg-Gly-Asp; SAEC, small airway epithelial cell; SARS, severe acute respiratory syndrome; SPR, surface plasmon resonance
Coronaviruses (CoVs) are a diverse group of positive-stranded RNA viruses named for the distinctive crown-like protrusions on their surfaces. CoVs can infect a wide range of mammalian and avian species, causing mild to severe respiratory infections (1). At present, seven different CoVs are known to infect humans, four of which cause only mild disease (2). Within the past 20 years, three CoVs have emerged that are capable of causing more severe disease in humans: SARS-CoV-1, the cause of severe acute respiratory syndrome (SARS); MERS-CoV, the cause of Middle East respiratory syndrome (MERS); and SARS-CoV-2, the cause of COVID-19 (1). The most common symptoms of COVID-19 infection are fever, cough, shortness of breath, and fatigue (3), but disease progression varies widely with approximately 20% of nonvaccinated patients experiencing severe acute disease (4). Acute respiratory distress syndrome (5), as well as myocardial (6), renal (7), hepatic (8),and digestive (9) complications have all been reported. In addition, over half of patients with COVID-19, including those with mild, acute symptoms, exhibit a range of short and long-term post-acute sequelae that include pulmonary abnormalities, functional mobility impairment, fatigue, and joint pain (10, 11). The complex clinical manifestations of acute and post-acute COVID-19 suggest a dysregulated host response to infection that triggers immunoinflammatory, thrombotic, and parenchymal disorders (12), Yet, the pathophysiological mechanisms responsible for the diverse disease phenotypes remain largely unknown.
The extracellular matrix (ECM) glycoprotein, fibronectin, is an essential regulator of connective tissue homeostasis (13), epithelial morphogenesis (14), endothelial barrier maintenance (15, 16), local arteriolar tone (17, 18), and tissue repair (19). Fibronectin also serves a significant role in host–pathogen interactions, as fibronectin-binding and fibronectin-mimicking proteins have been identified across a broad spectrum of microbial pathogens (20). Compared with SARS-CoV-1, the spike (S)1 subunit of SARS-CoV-2 contains a novel mutation that mimics a bioactive sequence in fibronectin: a Lys (K) to Arg (R) mutation in the receptor-binding domain (RBD), resulting in the adhesive Arg-Gly-Asp (RGD) motif of fibronectin’s integrin-binding domain (21). In fibronectin, the RGD sequence is located in a short loop that extends from the tenth type III repeat (FNIII10) where it mediates adhesion for a variety of cell types, including epithelial cells, endothelial cells, and fibroblasts, via β1 and β3 integrins (22, 23). Ligation of cell surface integrins with the RGD sequence of fibronectin triggers a cascade of cell signaling events, including protein kinase C activation and Rho-mediated actomyosin contractility, that lead to changes in cell shape (24), focal adhesion composition (25, 26), and extracellular matrix assembly (27). Critically, activation of components of these adhesion-based signaling cascades has been associated with reduced endothelial and epithelial barrier function and increased prevalence of inflammatory diseases (28).
SARS-CoV-2 infects epithelial cells of both the respiratory (29) and gastrointestinal tracts (30) via S1-mediated recognition of angiotensin-converting enzyme 2 (ACE2) on host cell surfaces (31). Initial evaluation of interresidue distances within the crystal structure of SARS-CoV-2 spike in complex with ACE2 suggested that the RGD motif of S1 is located adjacent to, but not included within, the ACE2-binding surface (32). More recent analysis indicates that Arg403 of S1 is highly conserved across SARS-CoV-2 lineages and may facilitate viral engagement of human cells via an ionic interaction with residue Glu37 of ACE2 (33). Positive detection of S1-integrin binding via solid-phase ELISA assays has been reported by several independent groups for both α5β1 (34, 35) and αvβ3 (36) integrins. Viral infection studies further showed that cell-surface binding and viral uptake of SARS-CoV-2 can be inhibited by integrin antagonists, including the peptide inhibitors Cilengitide (36) and ATN-161 (34, 37), as well as by cell-permeable inhibitors of inside-out integrin signaling (38). Thus, converging evidence suggests that S1-integrin interactions occur during SARS-CoV-2 infection, although the specificity and selectivity for specific integrins, as well as the implications for SARS-CoV-2 infection and disease remain to be elucidated. In the present study, we investigated S1-integrin interactions using both primary human small airway epithelial cells, as well as fibronectin-null mouse embryonic fibroblasts (FN-null MEFs). FN-null MEFs do not produce fibronectin, laminin, or vitronectin (39, 40) and are cultured in the absence of serum, allowing for the characterization of S1 binding to cell surface receptors and the identification of intracellular signals triggered by S1-integrin engagement without interference from other adhesive ligands (40, 41, 42). Results of this study indicate that the RGD motif contained within S1 is a cryptic, low-affinity, αv integrin ligand that can mediate cell adhesion, spreading, and proliferation to a similar extent as native fibronectin. RBD-integrin engagement triggers canonical integrin-mediated signaling cascades, focal adhesion formation, and actin cytoskeletal organization, thus functioning as a classical αv integrin agonist.
Results
S1-RBD of SARS-CoV2 supports cell adhesion and proliferation via αvβ3 integrins
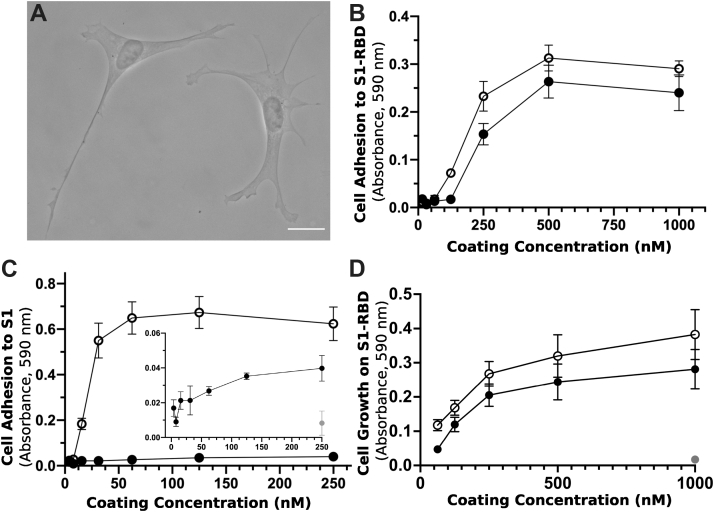
The integrin-binding RGD motif is contained within a variety of endogenous ECM glycoproteins (43) and is frequently expressed by microbial pathogens as a mechanism for attachment to host tissue (44). To begin to determine whether S1-RBD functionally interacts with cells, FN-null MEFs were seeded into wells coated with either S1-RBD or the RGD-containing module of fibronectin, FNIII10. At 4 h after seeding, cells adherent to S1-RBD exhibited robust adhesion and classical fibroblast morphology, characterized by extended membrane protrusions (Fig. 1A). Cell adhesion was dose dependent with respect to substrate coating concentration and comparable with adhesion on FNIII10 (Fig. 1B). Under these assay conditions, full-length S1 supported minimal cell attachment compared with the similarly sized fibronectin fragment, FNIII8-13 (Fig. 1C).
Figure 1.
S1-RBD supports cell adhesion and proliferation.A, FN-null MEFs (2.5 × 103 cells/cm2) were seeded onto coverslips precoated with S1-RBD (500 nM) and cultured for 4 h prior to fixation and phase-contrast imaging. The scale bar represents 20 μm. B, FN-null MEFs (1.9 × 105 cells/cm2) were seeded onto tissue culture plates precoated with the indicated concentration of S1-RBD (filled circles) or FNIII10 (open circles). Cells were cultured for 90 min, and relative cell number was determined by crystal violet staining. C, FN-null MEFs (1.9 × 105 cells/cm2) were seeded onto plates precoated with HN-tagged S1 (filled circles) or FNIII8-13 (open circles) for 90 min. Inset shows cell adhesion to S1 (filled circles) compared with bovine serum albumin–coated wells (gray circle). D, FN-null MEFs (2.3 × 103 cells/cm2) were seeded onto tissue culture plates precoated with the indicated concentration of S1-RBD (filled circles), FNIII10 (open circles), or GST (gray circle) and cultured for 4 days. Relative cell number was determined by crystal violet staining. Data are mean ± SEM; n ≥ 3 experiments performed in triplicate.
Ligation of integrins by RGD-containing agonists initiates cell signaling cascades that support cell proliferation (45). Thus, we next tested the ability of S1-RBD to support cell proliferation. To do so, FN-null MEFs were seeded at low density in defined, serum-free media onto tissue culture plates coated with S1-RBD, FNIII10, or the nonadhesive, protein purification tag, glutathione S-transferase (GST). After a 4-day incubation, relative cell number was quantified as a function of coating concentration. As shown in Figure 1D, cell number increased similarly with increasing coating density on S1-RBD- and FNIII10-coated wells. In contrast, cells seeded into GST-coated wells did not survive (Fig. 1D; 1 μM), indicating that cell proliferation in response to S1-RBD was specific and not due to the presence of endogenous or exogenously supplied adhesive proteins.
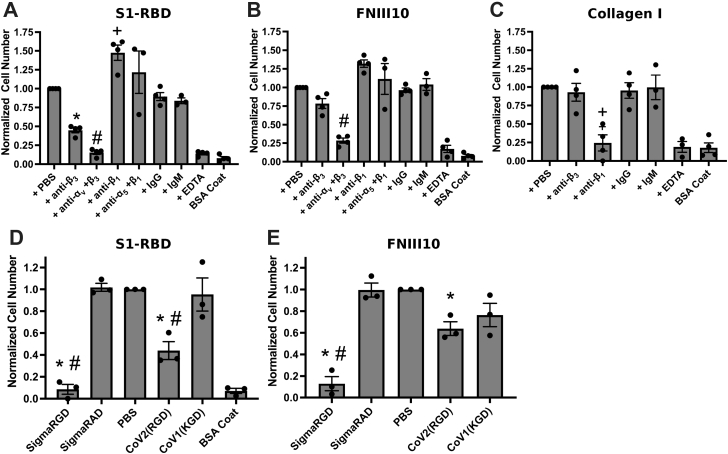
Integrins are heterodimeric receptors, whose ligand specificity is determined by the combination of alpha and beta subunits (43). FN-null MEFs express α1, α5, αv, β1, and β3 integrin subunits (40), of which both α5β1 and αvβ3 are RGD-binding integrins (43). To identify the integrin receptors mediating cell adhesion to S1-RBD, FN-null MEFs were preincubated with blocking antibodies directed against β1, β3, α5, or αv integrin subunits. Cell adhesion to S1-RBD was inhibited partially by antibodies against β3-integrin subunits and inhibited completely by either a combination of αv- and β3-blocking antibodies or EDTA (Fig. 2A). Similar results were obtained using the αvβ3-specific ligand, FNIII10 (46) (Fig. 2B). In contrast, cell adhesion to S1-RBD was not inhibited by either α5- or β1-blocking antibodies (Fig. 2A) under conditions that specifically inhibited adhesion to the β1-integrin ligand, collagen I (Fig. 2C). Rather, treatment of cells with anti-β1 antibodies significantly increased cell adhesion to S1-RBD (Fig. 2A). Finally, competitive inhibition assays were performed using short RGD-, RAD-, or KGD-containing peptides. Addition of soluble RGD peptides blocked cell adhesion to S1-RBD (Fig. 2D). In contrast, addition of control, RAD peptides had no effect on cell adhesion to S1-RBD (Fig. 2D). Furthermore, peptides derived from the RGD-containing region of SARS-CoV-2 partially inhibited cell adhesion to S1-RBD, whereas a peptide derived from the corresponding sequence of SARS-CoV-1, which contains a KGD rather than RGD motif, did not reduce adhesion to S1-RBD (Fig. 2D). Notably, SARS-CoV-2-derived peptides also partially inhibited cell adhesion to FNIII10 (Fig. 2E). Together, these data indicate that the RGD motif of S1-RBD ligates αvβ3 integrins in a cation-dependent manner.
Figure 2.
FN-null MEF adhesion to S1-RBD is mediated by αvβ3integrins and RGD. FN-null MEFs (5 × 105 cells/ml) were preincubated for 30 min with 50 μg/ml integrin-blocking antibodies (A–C) or 25 μM peptide (D–E) before seeding (9.4 × 104 cells/cm2) onto plates precoated with 250 nM S1-RBD (A and D), FNIII10 (B and E), or type I collagen (C). Relative cell number was determined by crystal violet staining. Data are mean ± SEM, normalized to corresponding vehicle (PBS) controls; n = 3 independent experiments performed in triplicate. One-way ANOVA, Bonferroni’s post hoc test: A–C ∗p < 0.05 versus PBS, IgG; +p < 0.05 versus PBS, IgM; #p < 0.05 versus PBS, anti-α5+β1; D–E ∗p < 0.05 versus PBS; #p < 0.05 versus corresponding negative control, RAD or KGD.
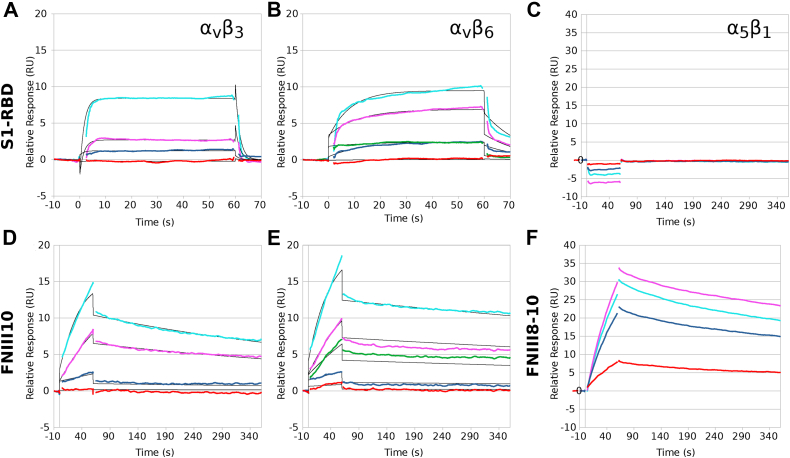
Surface plasmon resonance (SPR) was used next to study the kinetic parameters governing the binding of recombinant human integrins with immobilized S1-RBD. Representative response curves obtained from αvβ3, αvβ6, or α5β1 integrin binding to S1-RBD, FNIII10, or FNIII8-10 are shown in Figure 3. Experimental data were collected and globally fit using a 1:1 binding model. The fitted kinetic parameters, ka, kd, KD, and Rmax are shown in Table 1. The quality of each fit was evaluated by comparison with the experimentally measured Rmax and chi-squared values. Measurable binding of αvβ3 integrins to S1-RBD was observed (Fig. 3A). However, curve-fitting parameters indicated that the goodness of fit was not sufficient to perform kinetic analysis, suggesting that the KD of αvβ3 integrins binding to S1-RBD is greater than 500 nM (Table 1). Kinetic modeling of data obtained for αvβ6 integrin binding to S1-RBD provided a KD value of 230 nM (Fig. 3B and Table 1). In contrast, α5β1 integrins did not bind to S1-RBD (Fig. 3C), in agreement with results of cell adhesion assays (Fig. 2). Measured affinities of FNIII10 binding to αvβ3 (Fig. 3D) and αvβ6 (Fig. 3E) integrins were 21.8 nM and 6.6 nM, respectively (Table 1), which are similar to published values (47). Association rates for the interaction of αvβ6 integrins with S1-RBD and FNIII10 were similar (S1-RBD ka = 8.4 × 104 M−1s−1; FNIII10 ka = 7.1 × 104 M−1s−1). In contrast, the dissociation rate of αvβ6 integrins with S1-RBD was much larger than that observed with FNIII10 (S1-RBD kd = 236 × 10−4 s−1; FNIII10 kd = 6.0 ×10−4 s−1). Kinetic fits were not performed for the reaction of S1-RBD and α5β1 integrins, as binding was not observed (Fig. 3C) even at analyte concentrations substantially exceeding the KD of the interaction of FNIII8-10 with α5β1 integrins (47) and under reaction conditions in which α5β1 integrin binding to FNIII8-10 was observed (Fig. 3F). Together, these data indicate that S1-RBD is capable of binding directly to αv integrins through low-affinity interactions.
Figure 3.
Recombinant human integrins αvβ3and αvβ6, but not α5β1, bind to immobilized S1-RBD. Representative kinetic data for αvβ3 (A and D), αvβ6 (B and E), or α5β1 (C and F) binding to immobilized S1-RBD (A–C), FNIII10 (D–E), or FNIII8-10 (F). Data are presented as representative traces (bold colored lines) collected from one of two (α5β1, 100–1000 nM) or three (αvβ3, 5–450 nM and αvβ6, 5–500 nM) experiments and corresponding 1:1 binding fits (black lines).
Table 1.
Summary of kinetic and quality control parameters determined for the interaction of αv integrins with immobilized S1-RBD and FNIII10
| Ligand | Analyte | ka × 104 | kd × 10−4 | KD (nM) | Rmax fit (RU) | Rmax measured (RU) | Chi2 |
|---|---|---|---|---|---|---|---|
| S1-RBD | αvβ3 | - | - | >500 | - | - | - |
| S1-RBD | αvβ6 | 8.4 ± 1.8 | 236 ± 206 | 230 ± 180 | 6.9 ± 3.5 | 11.7 ± 0.7 | 0.1 ± 0.3 |
| FNIII10 | αvβ3 | 7.1 ± 1.4 | 15.0 ± 1.8 | 21.8 ± 1.6 | 12.8 ± 0.5 | 12.6 ± 0.4 | 0.06 ± 0.01 |
| FNIII10 | αvβ6 | 25.0 ± 18.8 | 6.0 ± 0.7 | 6.6 ± 3.1 | 16.6 ± 2.5 | 19.0 ± 2.3 | 0.16 ± 0.05 |
Data are presented as mean ± SEM for at least three independent experiments per integrin. Double-referenced experiments were performed simultaneously for S1-RBD and FNIII10 ligands in parallel flow cells.
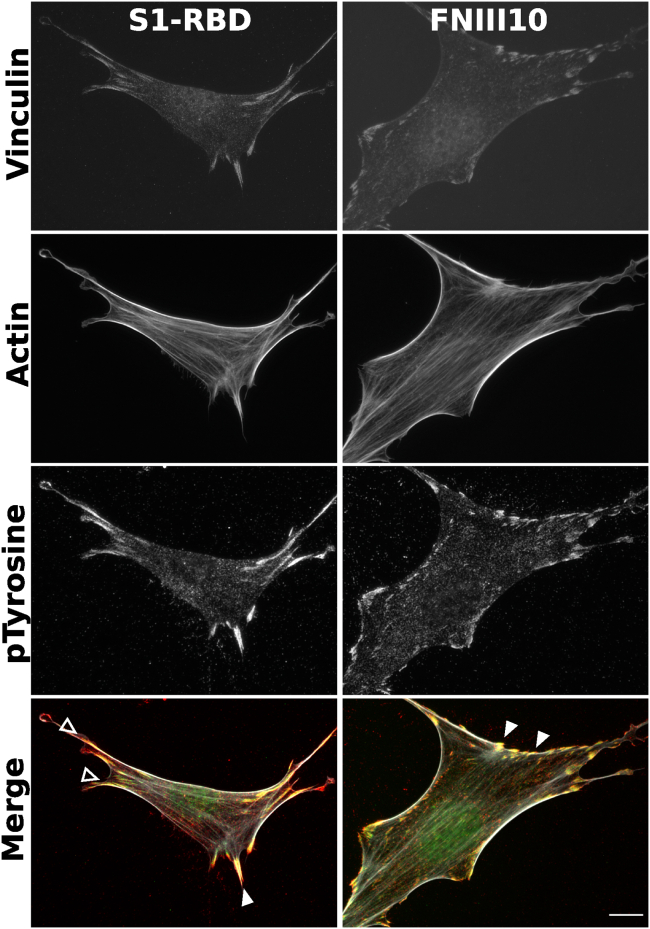
S1-RBD initiates focal adhesion formation and actin organization
Integrin ligation by endogenous ECM ligands triggers adhesion signaling cascades in which intracellular mediators are recruited to sites of integrin activation (45, 48). These protein complexes, known as focal adhesions, serve as central signaling hubs and functionally couple ECM-engaged integrins to the actin cytoskeleton (49). Notably, manipulation of focal adhesion signaling has been identified across a diverse spectrum of microbial pathogens, with the potential to influence multiple stages of cellular pathophysiology, including cell-surface attachment, invasion, and cell death (44). To determine whether engagement of αvβ3 integrins by S1-RBD supports focal adhesion formation and downstream signaling, FN-null MEFs adherent to S1-RBD were stained with the actin-binding protein phalloidin, together with antibodies against the focal adhesion adaptor vinculin, and a pan-specific phosphotyrosine antibody (50). Cells adherent to S1-RBD- or FNIII10-coated substrates were well spread and exhibited classical features of focal adhesions, including colocalized vinculin and phosphotyrosine staining, as well as actin stress fiber formation (Fig. 4). S1-RBD-adherent cells typically exhibited fewer, but larger, focal contacts than FNIII10-adherent cells.
Figure 4.
S1-RBD engagement initiates focal adhesion formation and actin organization. FN-null MEFs (2.5 × 103 cells/cm2) were seeded on coverslips coated with 500 nM S1-RBD (left) or FNIII10 (right). Cells were incubated for 4 h prior to fixation and immunofluorescent staining for vinculin (green), actin (TRITC-phalloidin, white), or phosphotyrosine (4G10, red). Arrowheads represent colocalization of vinculin and phosphotyrosine within focal adhesions (closed) and engagement with the actin cytoskeleton (open). Representative images shown from one of four independent experiments. The scale bar represents 10 μm.
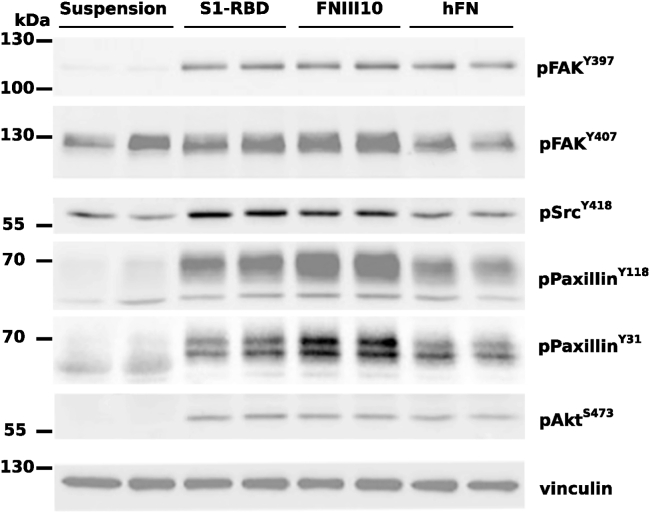
To identify proteins specifically phosphorylated by S1-RBD ligation, immunoblot analysis of whole-cell lysates was performed. Similar patterns of protein tyrosine phosphorylation were observed when lysates from attached S1-RBD- or FNIII10-adherent cells were probed with a pan-specific phosphotyrosine antibody (not shown). As such, immunoblots were next probed with phosphospecific antibodies against key components of adhesion signaling pathways (Fig. 5). These components included the early, adhesion-dependent autophosphorylation of focal adhesion kinase (FAK) at Y397 (51), which in turn enables recruitment and phosphorylation of Src at Y418 (52). Both FAK-Y397 and Src-Y418 were phosphorylated in response to S1-RBD ligation (Fig. 5). Moreover, the extent of FAK and Src phosphorylation was similar to that observed in either FNIII-10- or fibronectin-adherent cells (Fig. 5). FAK may be phosphorylated at additional tyrosine residues including Y407 (53), which was phosphorylated to a similar extent in both suspended and adherent cells (Fig. 5). S1-RBD triggered tyrosine phosphorylation of paxillin (Fig. 5), a central adaptor protein whose SH2 domains require phosphorylation at residues Y118 and Y31 for activation and cytoskeletal remodeling (54, 55). In addition, S1-RBD induced Akt phosphorylation at residue S473 to a similar extent as FNIII10- and fibronectin-adherent cells, implicating engagement of the prosurvival PI3K/Akt signaling axis (56, 57) and consistent with results demonstrating that S1-RBD ligation supports cell proliferation (Fig. 1D). Together, these data indicate that S1-RBD can trigger multiple aspects of adhesion-based signaling, including localization of vinculin to focal adhesions, phosphorylation of early adhesion signals FAK and Src, as well as activation of downstream adhesive effectors, including paxillin and Akt.
Figure 5.
Cell engagement with S1-RBD stimulates intracellular signaling. FN-null MEFs were either suspended in media or seeded at 3.5 × 105 cells/cm2 on wells precoated with 500 nM of S1-RBD or FNIII10, or 10 μg/ml of human plasma fibronectin (hFN) for 1 h. Cell lysates were analyzed by immunoblotting with the indicated phosphospecific antibodies or vinculin, as a loading control. Molecular mass markers are shown on the left.
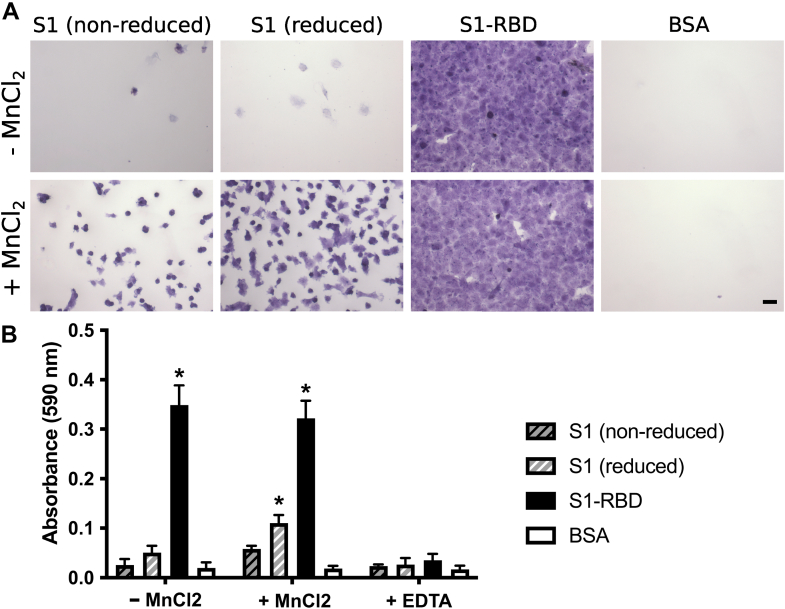
The data presented thus far indicate that the RGD sequence within S1-RBD is a functional, integrin-binding ligand that can mimic classical features and functions of native ECM ligands. In contrast, cells attached poorly to a larger fragment of S1 (Fig. 1C), which contains both the N-terminal domain and furin cleavage site in addition to RBD. Cryptic adhesive epitopes are a feature common to many native ECM proteins, including fibronectin (58) and thrombospondin (59). Thus, studies were conducted to explore conditions that might promote cell interactions with the larger S1 fragment. First, S1 was chemically reduced to alter its conformation. Cell adhesion to substrates precoated with either reduced or nonreduced S1 was then determined in the absence and presence of MnCl2, a potent activator of αvβ3 integrins (60). In the absence of MnCl2, few cells attached to S1, either in the nonreduced or reduced form (Fig. 6A, S1 - MnCl2). In contrast, in the presence of MnCl2, cells were visibly attached and well spread on substrates coated with either nonreduced or reduced S1, compared with bovine serum albumin (BSA)-coated wells (Fig. 6A, S1 + MnCl2). Cells attached and spread similarly on S1-RBD-coated substrates in the absence and presence of MnCl2 (Fig. 6A, S1-RBD ± MnCl2) indicating that integrin interaction with RBD did not require the high-affinity state.
Figure 6.
S1 contains a cryptic, Mn2+-sensitive adhesive epitope.A, FN-null MEFs (9.4 × 104 cells/cm2) were seeded on wells precoated with 250 nM reduced or nonreduced S1 protein, S1-RBD, or 1% bovine serum albumin (BSA). Cells were seeded for 1 h in the absence or presence of 1 mM MnCl2 or 10 mM EDTA. A, representative images of crystal violet–stained cells. The scale bar represents 100 μm. B, relative cell number presented as mean absorbance ± SEM, n = 3 independent experiments performed in triplicate. ∗p < 0.05 versus corresponding BSA control by two-way ANOVA with Bonferroni’s post hoc test.
Cell attachment to S1 was quantified using adhesion assays. In the presence of MnCl2, cell attachment to wells coated with reduced S1 was statistically increased versus BSA-coated wells (Fig. 6B; reduced S1 + MnCl2 versus BSA + MnCl2). Moreover, adhesion to reduced S1 was sensitive to the metal ion chelator, EDTA (Fig. 6B, reduced S1 ± EDTA). To determine whether increased cell adhesion to reduced S1 was due to changes in S1 protein conformation or increased substrate coating efficiency, ELISAs were performed on substrate-coated wells using anti-His antibodies. The relative coating density of reduced S1 was approximately double that of nonreduced S1 and S1-RBD (mean absorbances ± SD: reduced S1 = 1.56 ± 0.04; nonreduced S1 = 0.76 ± 0.01; S1-RBD = 0.95 ± 0.08). As such, the increase in cell adhesion observed with reduced S1 protein was likely due to an increase in coating density of the reduced S1 protein. There was no significant difference in protein density of wells coated with nonreduced S1 versus RBD. Together, these data indicate that, within the larger S1 fragment, the adhesive capacity of RBD is detectable but substantially reduced versus the RBD fragment.
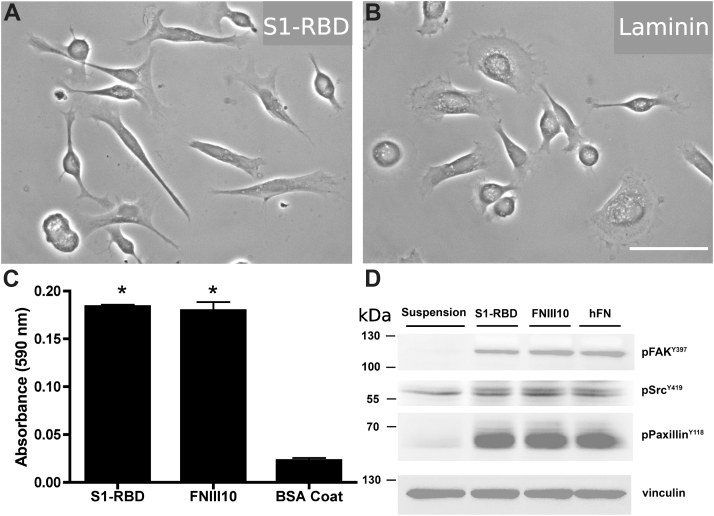
S1-RBD exhibits cation- and RGD-dependent binding to primary human small airway epithelial cell monolayers
We next sought to determine whether S1-RBD can mediate adhesion of human primary small airway epithelial cells (hSAECs). These primary cells are derived from the distal lung and are susceptible to SARS-CoV-2 infection (61, 62). hSAECs seeded in the presence of 1 mM MnCl2 attached and spread on S1-RBD-coated wells to a similar extent as that observed with laminin-coated wells (Fig. 7, A and B). hSAEC adhesion to S1-RBD was significantly increased compared with BSA-coated wells and was similar to that observed with wells coated with the αvβ3-ligand, FNIII10 (Fig. 7C). Furthermore, hSAECs adhesion to S1-RBD stimulated tyrosine phosphorylation of FAK, paxillin, and Src to a similar extent as FNIII10 and fibronectin (Fig. 7D). Thus, S1-RBD stimulates adhesion-mediated intracellular signaling pathways in human lung epithelial cells.
Figure 7.
S1-RBD supports cell adhesion and phosphotyrosine signaling in human small airway epithelial cells. hSAECs (6.7 × 104 cells/cm2) were seeded in the presence of 1 mM MnCl2 on wells precoated with S1-RBD, laminin, FNIII10, or 1% bovine serum albumin (BSA). Representative images of SAECs adherent of S1-RBD (A) or laminin (B) are shown. The scale bar represents 50 μm. C, cell adhesion after 2 h was determined by crystal violet staining. Data are presented as mean absorbance ± SEM. ∗p < 0.05 versus BSA by one-way ANOVA with Bonferroni’s posttest. D, cell lysates were obtained after 4 h of adhesion and analyzed by immunoblotting with the indicated phosphospecific antibodies. Vinculin was used as a loading control. Molecular mass markers are shown on the left. Control cells were maintained suspended in medium before lysing. SAEC, small airway epithelial cell.
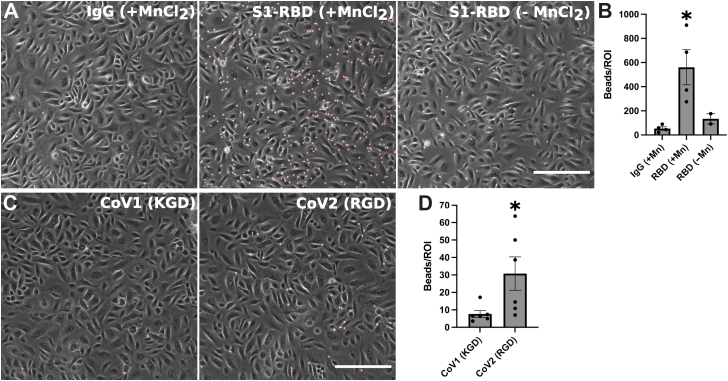
Thus far, the ability of S1-RBD to bind to integrins has been analyzed by presenting immobilized S1 fragments to nonadherent cells. To evaluate S1-RBD binding to cells that are already adherent and spread on native ECM substrates, assays were performed using either Fc-tagged RBD fragments immobilized on fluorescent protein G–coupled microbeads or biotin-tagged CoV 20-mer peptides immobilized on streptavidin-coupled microbeads. To begin, hSAEC monolayers were incubated with RBD- or IgG-immobilized beads. Following a 2-h incubation, limited binding of IgG-coupled beads to hSAEC monolayers was observed (Fig. 8A; IgG + MnCl2). In contrast, RBD-immobilized beads attached extensively to hSAECs in the presence but not the absence of MnCl2 (Fig. 8A). Quantification of the number of beads bound per imaging field indicated a significant increase in the number of RBD-beads bound versus IgG controls (Fig. 8B), demonstrating cation-dependent binding of S1-RBD to epithelial cell surfaces.
Figure 8.
S1-RBD-bound beads bind to SAEC monolayers in a cation- and RGD-dependent manner.A, laminin-adherent SAEC monolayers were treated with (A and B) IgG- or Fc-RBD-immobilized fluorescent microbeads in the presence or absence of 1 mM MnCl2 or (C and D) biotinylated CoV-2(RGD) or CoV-1(KGD) peptide-immobilized fluorescent microbeads in the presence of 1 mM MnCl2. Cells were incubated for 2 h at 4 °C. (A and C) representative phase images are shown; protein-immobilized beads are red. The scale bar represents 200 μm. (B and D) bead binding to SAEC monolayers was quantified as the mean for three independent regions of interest (ROIs) per well. Data are mean number of beads bound per 0.6 mm2 ROI ± SEM. In (B), n = 4 (+Mn) or n = 2 (−Mn) replicates per condition on two independent experimental days. ∗p < 0.05 versus IgG by one-way ANOVA with Bonferroni’s post hoc test. In (D), n = 6 replicates per condition on three independent experimental days. ∗p < 0.05 versus KGD by two-tailed t test. SAEC, small airway epithelial cell.
The role of the RGD motif in mediating RBD binding to epithelial cell surfaces was next assessed using CoV-derived peptides. A 20-mer, CoV-2 peptide encompassing the RGD motif was synthesized, and binding to epithelial cell surfaces was compared with the corresponding peptide of CoV-1, which contains a KGD sequence in place of RGD. The CoV-1 sequence was chosen expressly as a control for CoV-2 binding, as KGD is also an integrin-binding motif but with specificity for platelet αIIbβ3 integrins (63), which are not expressed by primary epithelial cells (64). Peptide-bound microbeads were incubated with laminin-adherent SAECs for 2 h, and unbound beads were removed by washing. As shown in Figure 8C, microbeads coated with RGD-containing CoV-2 peptides readily attached to epithelial cell surfaces, whereas beads coated with KGD-containing CoV-1 peptides did not. Quantification of the number of beads bound per imaging field indicated a significant increase in the number of CoV-2- versus CoV-1-beads bound per region of interest (Fig. 8D). The CoV-1- and CoV-2-derived peptides utilized in this study differ only in their integrin-binding sequences (IRGDE versus VKGDD for CoV-2 and CoV-1, respectively), thus providing additional evidence that mutation of the KGD sequence of CoV-1 to RGD conferred the RBD of CoV-2 with the capacity to interact with epithelial cell integrins.
Discussion
The identification of a conserved RGD motif within the SARS-CoV-2 spike protein generated substantial scientific interest (21, 33), and converging lines of experimental evidence suggest that integrin inhibition may be protective against SARS-CoV-2 binding and infection (34, 36, 37, 38, 65). To the best of our knowledge, the data presented in the present study are the first to demonstrate that the receptor-binding domain of SARS-CoV-2 spike protein functions as a classical integrin receptor agonist. S1-RBD supported cell adhesion (Fig. 1, A and B) and proliferation (Fig. 1D) to comparable extents as the RGD-containing fragment of the native ECM molecule fibronectin (FNIII10). This interaction was competitively inhibited by both αv integrin-blocking antibodies and RGD peptides (Fig. 2, A and D) and was also observed in an SPR model of direct S1-RBD-integrin binding (Fig. 3). Cells adherent to S1-RBD formed focal adhesions (Fig. 4), and key adhesion signaling mediators FAK, Src, Paxillin, and Akt were phosphorylated (Fig. 5). The present studies were conducted primarily in mouse embryonic fibroblasts, which do not express detectable levels of ACE2, and thus these results are unlikely to be complicated by potential interactions of S1-RBD with ACE2. As well, S1-RBD supported both cell attachment and adhesion-based signaling in primary human small airway epithelial cells (Fig. 7), while RBD-bound microbeads attached readily to SAEC monolayers (Fig. 8). Together, these results demonstrate that SARS-CoV-2 spike protein contains a functional adhesive epitope within the RBD that mediates αv integrin engagement via its RGD motif.
Of reports investigating integrin-spike interactions, α5β1 has been proposed as a receptor of interest, in part due to its functional association with ACE2 (66, 67), the ability of β1-selective integrin antagonists to reduce SARS-Co-V2 invasion (34, 37, 38), and observed α5β1 integrin-S1-RBD interactions by ELISA (34) and SPR (68) assays. Some reports have also implicated αvβ3 integrins in viral entry (36, 69), while others found no effects of integrin antagonists on viral invasion (33). In the present study, we compared effects of β1- and β3-integrin-blocking antibodies on cell attachment to RBD using a well-characterized fibroblast cell line that expresses both functional α5β1 and αvβ3 integrin receptors (40, 41). Notably, FN-null MEFs do not produce fibronectin, are cultured in the absence of serum, and do not deposit other endogenous matrix molecules, including RGD-containing thrombospondin and the α1/2β1 integrin ligand collagen, into their ECM (42). FN-null MEFs adhered to S1-RBD exclusively via αvβ3 integrins, with no contribution from α5β1 integrins (Fig. 2, A–C). This result was confirmed using recombinant integrins and SPR, which further indicated that the affinity of the epithelial integrin αvβ6 for S1-RBD was substantially higher than that of αvβ3 (Fig. 3 and Table 1). In contrast to previous reports (68), we found no detectable interaction between S1-RBD and α5β1 integrin using SPR. This intriguing finding may be due to differences in the SPR conditions, which in the present study, included the use of the nonionic detergent octyl glucoside (70) and MnCl2 (60, 71) to support functional activation of integrins within a purified protein system. While we did not test the integrin specificity of the larger S1 fragment in the present study, recent work by Park and colleagues (65) showed that an Fc-tagged S1 fragment could support αv-, α4-, or β1-mediated adhesion depending on cell type–specific integrin expression. Thus, the possibility remains that, like fibronectin (46, 47), synergistic sequences or conformational flexibility within the larger S1 domain may confer additional, dynamic integrin selectivity. The specificity and selectivity of spike and spike fragments may further be sensitive to modulators of integrin signaling, such as heparin sulfate proteoglycan coreceptors (72) or cell-surface proteases (73), both of which have been identified as factors regulating engagement of SARS-CoV-2 virions with host target cells (31, 33, 74, 75).
In contrast to the robust adhesive response observed on S1-RBD, cells seeded onto the larger S1 fragment of SARS-CoV-2 spike protein attached only weakly and exhibited limited spreading (Figs. 1C and 7B). Cell adhesion to S1 was partially rescued by chemical reduction of S1, which increased coating efficiency, and pretreatment of cells with Mn2+. One possible interpretation of these data is that the adhesive epitope contained within S1 is cryptic and thus only available to integrins under appropriate physical and chemical conditions. This hypothesis is further supported by molecular dynamics simulations suggesting that, in the absence of other interactions, the RGD site is unable to adopt the geometry necessary for high-affinity integrin ligation (76). Matricryptic epitopes have been identified in a number of native ECM proteins, including thrombospondin (59), which contains a cryptic RGD sequence whose exposure is regulated by cell-surface protein disulfide isomerases (77). Likewise, exposure of a self-association epitope in fibronectin (58) can be exposed by cell-derived mechanical force (78) and proteolytic fragmentation (58). Thus, the specific conformational requirements and activation steps enabling functional engagement of integrin receptors with SARS-CoV-2 spike in the context of established mechanisms of viral attachment and invasion represents an open question of substantial importance.
The intact, trimeric SARS-CoV-2 spike undergoes multiple conformational changes and molecular interactions during the viral invasion process (79), including conformational flexibility of the RBD domain (80, 81), as well as activation by cell-surface proteases TMPRSS2 (31) and Cathepsin L (33, 75). Separation of the RBD from the prefusion spike trimer during proteolytic activation may therefore be a critical activation step prior to integrin binding. Furthermore, the well-characterized, cell-surface spike receptor ACE2 (31, 33) and the more recently identified coreceptor heparin sulfate proteoglycans (74, 82) can associate laterally with integrins on human cell surfaces (66, 67, 83, 84). Thus, integrins and associated intracellular signaling partners are emerging as putative components of a larger molecular complex that is targeted during SARS-CoV-2 infection. Differences in baseline integrin expression and activation state between cell lines are also a likely contributing factor in conflicting reports on the integrin dependence and selectivity of SARS-CoV-2 infection (33, 34, 36, 37, 38, 69). Future elucidation of the conformational requirements and activation steps enabling functional engagement of integrin receptors with SARS-CoV-2 spike in the context of established mechanisms of viral attachment and invasion represents an open question of substantial importance.
The demonstration of an αv-specific integrin agonist functionality contained within S1-RBD protein opens multiple avenues that will be critical in expanding scientific understanding of SARS-CoV-2 and therapeutic options for a global population affected by the COVID-19 pandemic. The most immediate among these, the identification of anti-integrin therapeutics that are US Food and Drug Administration approved or in preclinical trials with potential efficacy against SARS-CoV-2 infection, is already underway (85). Integrins have been implicated in the pathophysiology of numerous respiratory viruses, including human cytomegalovirus (86), hantaviruses (87), and influenza (88), as either primary receptors or as major mediators of host response and disease severity, with the specific contributions of integrins in the context of COVID-19 disease yet to be elucidated (21, 89). Meanwhile, numerous questions remain unanswered regarding mechanisms underlying the differential susceptibility of vulnerable populations to severe manifestations of COVID-19 (3), as well as potential differences in infectivity, transmissibility, disease severity, and immune evasion associated with novel variants (https://covariants.org/) (90). Interrogating these open challenges in the context of integrin-spike interactions, including factors determining integrin selectivity and specificity, is a promising and yet unexplored avenue. For example, ACE2 cell surface expression levels alone do not sufficiently predict tissue susceptibility or disease severity (91). Thus, a combinatorial expression profile of ACE2, alongside αv integrin surface expression, may better predict cell tropism of SARS-CoV-2. Alternatively, fibronectin–integrin interactions play a key role in maintaining endothelial barrier function during sepsis (15, 16, 92, 93, 94, 95), which may be disrupted by competition from spike protein fragments during SARS-CoV-2-driven inflammation, a hypothesis that is supported by recent work in vascular endothelial cells (35). Variations in integrin expression and activation state are likewise associated with some of the key risk factors for severe complications of SARS-CoV-2 infection (3), including diabetes (96, 97), hypertension (98, 99, 100), and differing inflammatory responses (88, 101). As the global COVID-19 pandemic approaches a new, endemic stage, targeting the emerging spike-integrin signaling axis has the potential to become an essential tool in preventing or mitigating the most severe effects of the disease, particularly for vulnerable patients who are not fully protected by current preventative and therapeutic regimens.
Conclusions
The SARS-CoV-2 spike protein contains a novel RGD motif within its receptor-binding domain (S1-RBD). We demonstrate that S1-RBD is a functional integrin agonist with selectivity for αv integrins, specifically αvβ3 and αvβ6. In contrast, we found no evidence of S1-RBD engagement with α5β1 integrins in either cellular adhesion or SPR systems. S1-RBD-mediated cellular adhesion supported cell spreading and cytoskeletal engagement, focal adhesion formation, and stimulation of key intracellular signaling pathways associated with cytoskeletal organization and cell proliferation. Together, these data point to a functional role for αv integrins during attachment and invasion of SARS-CoV-2 and provide insight into critical open questions regarding COVID-19 pathophysiology, including mechanisms underlying variable disease severity, intersecting risk factors, and post-acute viral sequelae.
Experimental procedures
Reagents
Fibronectin was purified from outdated human plasma (American Red Cross) using gelatin-Sepharose (GE Life Sciences, now Cytiva) affinity chromatography (102). Type I collagen (rat tail) was purchased from Corning (354236). Unless otherwise indicated, chemicals were obtained from J.T. Baker or Sigma-Aldrich. GST-tagged FNIII10 and HN-tagged FNIII10-13 were produced and purified from Escherichia coli as described (46, 103). His-tagged S1 and S1-RBD of SARS-CoV-2 were purchased from Sino Biological (40591-V08H) and R&D Systems (10523-CV), respectively. Fc-tagged S1-RBD was from R&D Systems (10565-CV). Where indicated, S1 was reduced by successive 1-h treatments with 10 mM DTT and 30 mM N-ethyl maleimide (NEM) at 37 °C. Both reduced and nonreduced S1 were dialyzed into PBS prior to use. Integrin-blocking antibodies anti-α5 (clone 5H10-27), anti-αV (clone H9.2B8), anti-β1 (clone Ha2/5), and anti-β3 (clone 2C9.G2) and isotype controls were purchased from BD Biosciences. Antibodies for immunofluorescent staining were as follows: vinculin (clone VIN-11-5, Sigma or clone 42H89L44, Invitrogen); phosphotyrosine (clone 4G10, Sigma or PY20, BD Biosciences); phospho-FAK pY407 (polyclonal, Invitrogen #44650G); phospho-FAK pY397 (polyclonal, Biosource #44-624G); phospho-Src pY418 (polyclonal, Biosource #44-660); phospho-Paxillin pY118 (polyclonal, Invitrogen #44-722G); phospho-Paxillin pY31 (polyclonal, Invitrogen #44-720G); phospho-Akt pS473 (polyclonal, Cell Signaling #9271); TRITC-labeled phalloidin (Millipore, #90228). Alexa Fluor–conjugated secondary antibodies were from Molecular Probes. RGD-containing peptides derived from SARS-CoV-2 (ADSFVIRGDEVRQIAPGQTG) and KGD-containing peptides derived from SARS-CoV (ADSFVVKGDDVRQIAPGQTG) were produced with and without an N-terminal biotin-Ahx tag by Genscript. Integrin-blocking (GRGDSP, #SCP0157) and negative control (GRADSP, #SCP0156) peptides were purchased from Sigma. Recombinant human integrins αvβ3 (3050-AV), αvβ6 (3817-AV), and α5β1 (3230-A5) were from R&D Systems. Protein G–coated pink (PGFP-5058-5, 5.0–5.9 μm diameter) and streptavidin-coated Nile red (SVFP-6056-5, 5.0–7.9 μm diameter) fluorescent particles were purchased from Spherotech, Inc.
Cell culture
FN-null MEFs, derived previously from homozygous fibronectin knockout mouse embryos (40), were cultured under serum- and fibronectin-free conditions on collagen I–coated tissue culture flasks using a 1:1 mixture of Aim V (Invitrogen) and Corning SF Medium (Corning), as described (40). FN-null MEFs do not express vitronectin or laminin (39, 40) and in the absence of supplemental fibronectin are unable to assemble ECM fibrils of collagen I (104), thrombospondin (42), or fibrinogen (105). Adult human small airway epithelial cells (SAECs) were purchased from Lonza (CC-2547) and used between passages 6 and 8. SAECs were cultured in serum-free Small Airway Epithelial Growth Medium (Lonza CC-3118), according to manufacturer’s instructions. Cells were passaged at 70 to 80% confluence using ReagentPack subculture reagents (Lonza CC-5034). Neither FN-null MEFs nor SAECs expressed detectable levels of ACE2 protein by immunoblot analysis (data not shown).
Cell adhesion and proliferation assays
Cell adhesion assays were performed as described (41). Briefly, 96-well tissue culture plates were coated with S1-RBD (10–1000 nM), FNIII10 (10–1000 nM), GST (1000 nM), or S1 (7.8–250 nM) for 1 h at 37 °C. Relative protein coating concentrations were quantified by enzyme-linked immunoabsorbent assays (ELISA) using anti-His antibodies, as described (106). Cells were seeded on protein-coated wells (9.4 × 104 cells/cm2) in either AimV/SF medium (FN-null MEFs) or Small Airway Epithelial Basal Medium (CC-3119; Lonza) in the absence or presence of EDTA (10 mM), DTT (1 mM), or MnCl2 (1 mM) as indicated; MnCl2 was added 1 h after seeding. For integrin blocking studies, FN-null MEFs were preincubated with anti-integrin antibodies (50 μg/ml) or 25 μM peptide for 1 h prior to seeding. Integrin-blocking studies were performed using subsaturating protein coating concentrations to reduce the amount of antibody or peptide required to inhibit adhesion. Cells were then seeded into wells and incubated at 37 °C and either 8% (FN-null MEFs) or 5% (SAECs) CO2 for up to 2 h. Wells were washed with PBS to remove nonadherent cells, fixed with 1% paraformaldehyde, and stained with 0.5% crystal violet. The absorbance of crystal violet solubilized in 1% SDS was measured at 590 nm. Proliferation assays were performed by seeding FN-null MEFs (2.5 × 103 cells/cm2) on protein-coated 48-well plates. Cells were cultured for 4 days at 37 °C, 8% CO2 and then fixed and stained with crystal violet (41). In some experiments, images of adherent cells were obtained after crystal violet staining and before solubilization, using an IX70 inverted microscope (Olympus) equipped with a Micropublisher 3.3 RTV digital camera (Q Imaging).
Surface plasmon resonance
Kinetic studies of integrin–ligand interactions were performed using a BIAcore T200 instrument (Cytiva). Ligands (S1-RBD or FNIII10) were immobilized using amine-coupling chemistry according to the manufacturer’s instructions (BR-1000-50). Briefly, ligands diluted in 10 mM sodium acetate (pH 4.0, Cytiva) were immobilized on an EDC/NHS-activated CM5 chip (Cytiva) to a target level of 800 to 1000 RU. Excess amine-reactive groups were inactivated with 1 M ethanolamine (pH 8.5, Cytiva). Immobilization buffer was 10 mM Hepes buffer pH 7.4 containing 0.05% n-octyl-β-D-glucopyranoside (OGPS, Anatrace), 150 mM NaCl2, 2 mM MnCl2, 2 mM MgCl2, and 0.2 mM CaCl2. Lyophilized integrins were reconstituted with 50 mM Tris, pH 7.4 containing 25 mM OGPS, 1 mM DTT, 150 mM NaCl2, and divalent cations (αv integrins: 2 mM MnCl2, 2 mM MgCl2, and 0.5 mM CaCl2; α5β1 integrin: 2 mM MnCl2). Double-referenced binding experiments were performed in parallel flow cells for S1-RBD and the corresponding positive control (FNIII10 for αv integrins; FNIII8-10 for α5β1) (46) using a flow rate of 30 μl/min for 1 min with a dissociation time of 5 min. Surfaces were regenerated between injections using two 30-s injections of 20 mM EDTA and 1 M NaCl (47). Kinetic parameters were determined by fitting a 1:1 binding model with globally fit parameters for each collected data set using Biacore T200 Evaluation software (Version 3.2, GE). Owing to the large difference in dissociation rates between the two ligands, only the first 10 s of the dissociation curves were considered for S1-RBD data sets. Quality of fit was determined by agreement between measured and calculated Rmax and chi-squared values. Data sets not producing high-quality kinetic fit were excluded from calculation of kinetic parameters.
Immunofluorescence microscopy
Acid-washed glass coverslips were coated with saturating concentrations of protein (500 nM; S1-RBD or FNIII10) for 1 h at 37 °C. FN-null MEFs (2.5 × 103 cells/cm2) were seeded in AimV/SF media and incubated at 37 °C, 8% CO2 for 4 h. Cells were then fixed with 2% paraformaldehyde in PBS and processed for immunofluorescence microscopy as described (107). Cells were incubated with primary antibodies or TRITC-phalloidin diluted in PBS containing 0.1% Tween 20, 1% BSA, and 1 mM phenylmethylsulfonyl fluoride for 1 h at room temperature. Bound antibodies were detected with Alexa448-, Alexa549-, or Alexa647-labeled goat anti-rabbit or -mouse secondary antibodies and visualized using a BX60 fluorescence microscope (Olympus) equipped with an epifluorescent lamp (Lumen Dynamics) and an EXi Blue Fluorescence Camera (Q Imaging), acquired with QCapture software.
Immunoblot analysis
FN-null MEFs (3.4 × 104 cells/cm2) or SAECs (6.7 × 104 cells/cm2) were seeded on wells precoated with saturating concentrations of S1-RBD (500 nM), FNIII10 (500 nM), or fibronectin (10 μg/ml) and incubated at 37 °C for 1 h (FN-null MEFs) or 4 h (SAECs). Cells were lysed with 40 μl/cm2 SDS-RIPA buffer (50 mM Tris, 150 mM NaCl, 1 mM EDTA, 1% Triton X-100, 0.1% sodium dodecyl sulfate, 0.5% sodium deoxycholate, pH 7.6) containing 1 mM sodium orthovanadate, 1 mM phenylmethylsulfonyl fluoride, and 1× protease inhibitor cocktail (Sigma S8830). Cell lysates were analyzed by SDS-PAGE and immunoblotting (108). Immunoblots were blocked with either 5% nonfat milk or 3% BSA in Tris-buffered saline containing 0.1% Tween 20 (TBS-T). Membranes were incubated overnight at 4 °C with primary antibodies diluted in TBS-T. Vinculin was used as the protein loading control. Blots were then washed with TBS-T, incubated with horseradish peroxidase–conjugated secondary antibodies, and developed using SuperSignal West Pico Chemiluminescent Substrate (Thermo Scientific). Blots were imaged using a ChemiDoc imaging system (Bio-Rad).
Bead binding assay
Fc-RBD or mouse IgG (667 nM in PBS) was immobilized on Protein G fluorescent particles (5.0–5.9 μm diameter) according to the manufacturer’s instructions. Unbound protein G sites were blocked with 3% BSA. Biotin-labeled 20-mer peptides encompassing the RGD region of SARS-CoV-2 or corresponding KGD region of SARS-CoV-1 were immobilized on streptavidin fluorescent particles (5.0–7.9 μm diameter) according to the manufacturer’s instructions and blocked with 1% BSA. Ligand-bound beads were washed and resuspended in small airway epithelial media with or without 1 mM MnCl2 immediately prior to use. Glass coverslips were coated with 10 μg/ml laminin, and SAECs were seeded at a density of 5.4 × 104 cells/cm2. SAECs were allowed to adhere overnight in growth media and washed twice with basal media immediately prior to bead treatment. SAEC monolayers were incubated with 1 × 106 beads/cm2 beads for 2 h at 4 °C. Assays were performed at 4 °C to minimize nonspecific endocytosis of particles. Unbound beads were removed by gentle washing with basal media, and cells were fixed with 1% paraformaldehyde in PBS. hSAECs monolayers were visualized by low-power phase microscopy. Cell-bound beads were detected by fluorescence microscopy and counted using FIJI software (NIH, cell counter plugin). The extent of bead binding in each condition was quantified as the mean number of fluorescent beads in 3 to 6 independent regions of interest (0.6 mm2) per well.
Statistical analysis
Data are presented as mean ± standard error unless otherwise stated. Experiments were performed in duplicate or triplicate on a minimum of two independent days. All statistical analyses were performed using GraphPad Prism (version 9). Statistical differences between groups were identified by two-tailed t tests or one- and two-way ANOVAs as indicated, using Bonferroni’s posttest and a p-value threshold < 0.05.
Data availability
All data are contained within the article, with supplementary data available upon request (denise_hocking@urmc.rochester.edu).
Conflict of interest
The authors declare that they have no conflicts of interest with the contents of this article.
Acknowledgments
The authors thank the University of Rochester Structural Biology and Biophysics Facility for the use of the Biacore T200 System and Dr Jermaine L. Jenkins for technical assistance. This research was supported by National Institutes of Health grant R01 AG058746 and by a University Research Award from the University of Rochester. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author contributions
E. G. N. and D. C. H. conceptualization; E. G. N. and D. C. H. data curation; E. G. N. and X. S. P. formal analysis; E. G. N., X. S. P., and D. C. H. investigation; E. G. N. writing - original draft; E. G. N. and D. C. H. writing - review and editing; D. C. H. supervision; D. C. H. funding acquisition; D. C. H. methodology; D. C. H. project administration.
Reviewed by members of the JBC Editorial Board. Edited by Craig Cameron
References
- 1.Hu B., Guo H., Zhou P., Shi Z.-L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021;19:141–154. doi: 10.1038/s41579-020-00459-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yin Y., Wunderink R.G. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology. 2018;23:130–137. doi: 10.1111/resp.13196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yuki K., Fujiogi M., Koutsogiannaki S. COVID-19 pathophysiology: a review. Clin. Immunol. 2020;215:108427. doi: 10.1016/j.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bennett T.D., Moffitt R.A., Hajagos J.G., Amor B., Anand A., Bissell M.M., et al. Clinical characterization and prediciton of clinical severity of SARS-CoV-2 infection among US adults using data from the US National COVID Cohort Collaborative. JAMA Netw. Open. 2021;4:e2116901. doi: 10.1001/jamanetworkopen.2021.16901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 noval coronavirus in Wuhan, China. Lancet. 2020;395:P497–P506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zaim S., Chong J.H., Sankaranarayanan V., Harky A. COVID-10 and multiorgan response. Curr. Probl. Cardiol. 2020;45:100618. doi: 10.1016/j.cpcardiol.2020.100618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pei G., Zhang Z., Peng J., Liu L., Zhang C., Yu C., et al. Renal involvement and early prognosis in patients with COVID-19 pneumonia. J. Am. Soc. Nephrol. 2020;31:1157–1165. doi: 10.1681/ASN.2020030276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Y., Xiao S.-Y. Hepatic involvement in COVID-19 patients: pathology, pathogenesis, and clinical implications. J. Med. Virol. 2020;92:1491–1494. doi: 10.1002/jmv.25973. [DOI] [PubMed] [Google Scholar]
- 9.Pan L., Mu M., Yang P., Sun Y., Wang R., Yan J., et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am. J. Gastroenterol. 2020;115:766–773. doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Datta S.D., Talwar A., Lee J.T. A proposed framework and timeline of the spectrum of disease due to SARS-CoV-2 infection: illness beyond acute infection and public health implications. JAMA. 2020;324:2251–2252. doi: 10.1001/jama.2020.22717. [DOI] [PubMed] [Google Scholar]
- 11.Groff D., Sun A., Ssentongo A.E., Ba D.M., Parsons N., Poudel G.R., et al. Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection: a systematic review. JAMA Netw. Open. 2021;4:e2128568. doi: 10.1001/jamanetworkopen.2021.28568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Osuchowski M.F., Wingkler M.S., Skirecki T., Cajander S., Shankar-Hari M., Lachmann G., et al. The COVID-19 puzzle: deciphering pathophysiology and phenotypes of a new disease entity. Lancet Respir. Med. 2021;9:622–642. doi: 10.1016/S2213-2600(21)00218-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Humphrey J.D., Dufresne E.R., Schwartz M.A. Mechanotransduction and extracellular matrix homeostasis. Nat. Rev. Mol. Cell. Biol. 2014;15:802–812. doi: 10.1038/nrm3896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sakai T., Larsen M., Yamada K.M. Fibronectin requirement in branching morphogenesis. Nature. 2003;423:876–881. doi: 10.1038/nature01712. [DOI] [PubMed] [Google Scholar]
- 15.Wheatley E.M., McKeown-Longo P.J., Vincent P.A., Saba T.M. Incorporation of fibronectin into matrix decreases TNF-induced increase in endothelial monolayer permeability. Am. J. Physiol. Lung Cell. Mol. Physiol. 1993;265:L148–L157. doi: 10.1152/ajplung.1993.265.2.L148. [DOI] [PubMed] [Google Scholar]
- 16.Curtis T.M., McKeown-Longo P.J., Vincent P.A., Homan S.M., Wheatley E.M., Saba T.M. Fibronectin attenuates increased endothelial monolayer permeability after RGD peptide, anti-α5β1, or TNF-α exposure. Am. J. Physiol. 1995;269:L248–L260. doi: 10.1152/ajplung.1995.269.2.L248. [DOI] [PubMed] [Google Scholar]
- 17.Hocking D.C., Titus P.A., Sumagin R., Sarelius I.H. Extracellular matrix fibronectin mechanically couples skeletal muscle contraction with local vasodilation. Circ. Res. 2008;102:372–379. doi: 10.1161/CIRCRESAHA.107.158501. [DOI] [PubMed] [Google Scholar]
- 18.Sarelius I.H., Titus P.A., Maimon N., Okech W., Wilke-Mounts S.J., Brennan J.R., et al. Extracellular matrix fibronectin intitates endothelium-dependent arteriolar dilation via the heparin-binding matricryptic RWRPK sequence of the first type III repeat of fibrillar fibronectin. J. Physiol. 2016;594:687–697. doi: 10.1113/JP271478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sawicka K.M., Seeliger M., Musaev T., Macri L.K., Clark R.A.F. Fibronectin interaction and enhancement of growth factors: importance for wound healing. Adv. Wound Care. 2015;4:469–478. doi: 10.1089/wound.2014.0616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vaca D.J., Thibau A., Schütz M., Kraiczy P., Happonen L., Malmström J., et al. Interaction with the host: the role of fibronectin and extracellular matrix proteins in the adhesion of gram-negative bacteria. Med. Microbiol. Immunol. 2020;209:277–299. doi: 10.1007/s00430-019-00644-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mészáros B., Sámano-Sánchez H., Alvarado-Valverde J., Čalyševa J., Martínez-Pérez E., Alves R., et al. Short linear motif candidates in the cell entry system used by SARS-CoV-2 and their potential therapeutic implications. Sci. Signal. 2021;14:eabd0334. doi: 10.1126/scisignal.abd0334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruoslahti E., Pierschbacher M.D. New perspectives in cell adhesion: RGD and integrins. Science. 1987;238:491–497. doi: 10.1126/science.2821619. [DOI] [PubMed] [Google Scholar]
- 23.Pierschbacher M.D., Ruoslahti E. Cell attachement activity of fibronectin can be duplicated by small synthetic fragments of the molecule. Nature. 1984;309:30–33. doi: 10.1038/309030a0. [DOI] [PubMed] [Google Scholar]
- 24.Larsson C. Protein kinase C and the regulation of the actin cytoskeleton. Cell. Signal. 2006;18:276–284. doi: 10.1016/j.cellsig.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 25.Saoncella S., Echtermeyer F., Denhez F., Nowlen J.K., Mosher D.F., Robinson S.D., et al. Syndecan-4 signals cooperatively with integrins in a Rho-dependent manner in the assembly of focal adhesions and actin stress fibers. Proc. Natl. Acad. Sci. U. S. A. 1999;96:2805–2810. doi: 10.1073/pnas.96.6.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Longley R.L., Woods A., Fleetwood A., Cowling G.J., Gallagher J.T., Couchman J.R. Control of morphology, cytoskeleton and migration by syndecan-4. J. Cell Sci. 1999;112:3421–3431. doi: 10.1242/jcs.112.20.3421. [DOI] [PubMed] [Google Scholar]
- 27.Singh P., Carraher C., Schwarzbauer J.E. Assembly of fibronectin extracellular matrix. Annu. Rev. Cell. Dev. Biol. 2010;26:397–419. doi: 10.1146/annurev-cellbio-100109-104020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Citalán-Madrid A.F., Vargas-Robles H., García-Ponce A., Shibayama M., Betanzos A., Nava P., et al. Cortactin deficiency causes increased RhoA/ROCK1-dependent actomyosin contractility, intestinal epithelial barrier dysfunction, and disproportionately severe DSS-induced colitis. Mucosal Immunol. 2017;10:1237–1247. doi: 10.1038/mi.2016.136. [DOI] [PubMed] [Google Scholar]
- 29.Walls A.C., Park Y.-J., Tortorici M.A., Wall A., McGuire A.T., Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181:281–292. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lamers M., Beumer J., van der Vaart J., Knoops K., Pushchhof J., Breugem T.I., et al. SARS-CoV-2 productively infects human gut enterocytes. Science. 2020;369:50–54. doi: 10.1126/science.abc1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoffmann M., Kleine-Weber H., Schroeder S., Kruger N., Herrler T., Erichsen S., et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lan J., Ge J., Yu J., Shan S., Zhou H., Fan S., et al. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581:215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 33.Zech F., Schniertshauer D., Jung C., Herrmann A., Cordsmeier A., Xie Q., et al. Spike residue 403 affects binding of coronavirus spikes to human ACE2. Nat. Commun. 2021;12:6855. doi: 10.1038/s41467-021-27180-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Beddingfield B.J., Iwanaga N., Chapagain P.P., Zheng W., Roy C.J., Hu T.Y., et al. The integrin binding peptide ATN-161, as a novel therapy for SARS-CoV-2 infection. JACC Basic Transl. Sci. 2021;6:1–8. doi: 10.1016/j.jacbts.2020.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Robles J.P., Zamora M., Adan-Castro E., Siqueiros-Marquez L., de la Escalera G.M., Clapp C. The spike protein of SARS-CoV-2 induces endothelial inflammation through integrin a5B1 and NF-kB signaling. J. Biol. Chem. 2022;298:101695. doi: 10.1016/j.jbc.2022.101695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nader D., Fletcher N., Curley G.F., Kerrigan S.W. SARS-CoV-2 uses major endothelial integrin aVB3 to cause vascular dysregulation in vitro during COVID-19. PLoS One. 2021;16:e0253347. doi: 10.1371/journal.pone.0253347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Amruta N., Engler-Chiurazzi E.B., Murray-Brown E.C., Gressett T.E., Biose I.J., Chastain W.H., et al. In vivo protection from SARS-CoV-2 infection by ATN-161 in k18-hACE2 transgenic mice. Life Sci. 2021;284:119881. doi: 10.1016/j.lfs.2021.119881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Simons P., Rinaldi D.A., Bondu V., Kell A., Bradfute S., Lidke D.S., et al. Integrin activation is an essential component of SARS-CoV-2 infection. Sci. Rep. 2021;11:20398. doi: 10.1038/s41598-021-99893-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wojciechowski K., Chang C.H., Hocking D.C. Expression, production, and characterization of full-length vitronectin in Escherichia coli. Protein Expr. Purif. 2004;36:131–138. doi: 10.1016/j.pep.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 40.Sottile J., Hocking D.C., Swiatek P.J. Fibronectin matrix assembly enhances adhesion-dependent cell growth. J. Cell Sci. 1998;111:2933–2943. doi: 10.1242/jcs.111.19.2933. [DOI] [PubMed] [Google Scholar]
- 41.Roy D.C., Hocking D.C. Recombinant fibronectin matrix mimetics specify integrin adhesion and extracellular matrix assembly. Tissue Eng. Part A. 2013;19:558–570. doi: 10.1089/ten.tea.2012.0257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sottile J., Hocking D.C. Fibronectin polymerization regulates the composition and stability of extracellular matrix fibrils and cell-matrix adhesions. Mol. Biol. Cell. 2002;13:3546–3559. doi: 10.1091/mbc.E02-01-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Humphries J.D., Byron A., Humphries M.J. Integrin ligands at a glance. J. Cell Sci. 2006;119:3901–3903. doi: 10.1242/jcs.03098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Murphy K.N., Brinkworth A.J. Manipulation of focal adhesion signaling by pathogenic microbes. Int. J. Mol. Sci. 2021;22:1358. doi: 10.3390/ijms22031358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burridge K., Chrzanowska-Wodnicka M. Focal adhesions, contractility, and signaling. Annu. Rev. Cell. Dev. Biol. 1996;12:463–519. doi: 10.1146/annurev.cellbio.12.1.463. [DOI] [PubMed] [Google Scholar]
- 46.Farrar C.S., Rouin G.T., Miller B.L., Raeman C.H., Mooney N.A., Hocking D.C. A matricryptic conformation of the integrin-binding domain of fibronectin regulates platelet-derived growth factor-induced intracellular calcium release. Cells. 2019;8:1351. doi: 10.3390/cells8111351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brown A.C., Dysart M.M., Clarke K.C., Stabenfeldt S.E., Barker T.H. Integrin α3β1 binding to fibronectin Is dependent on the ninth type III repeat. J. Biol. Chem. 2015;290:25534–25547. doi: 10.1074/jbc.M115.656702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Harburger D.S., Calderwood D.A. Integrin signaling at a glance. J. Cell Sci. 2009;122:159–163. doi: 10.1242/jcs.018093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Burridge K. Focal adhesions: a personal perspective on a half century of progress. FEBS J. 2017;284:3355–3361. doi: 10.1111/febs.14195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Geiger B., Bershadsky A., Pankov R., Yamada K.M. Transmembrane extracellular matrix-cytoskeleton crosstalk. Nat. Rev. Mol. Cell. Biol. 2001;2:793–805. doi: 10.1038/35099066. [DOI] [PubMed] [Google Scholar]
- 51.Schaller M.D., Hildebrand J.D., Shannon J.D., Fox J.W., Vines R.R., Parsons J.T. Autophosphorylation of the focal adhesion kinase, pp125FAK, directs SH2-dependent binding of pp60Src. Mol. Cell. Biol. 1994;14:1680–1688. doi: 10.1128/mcb.14.3.1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cobb B.S., Schaller M.D., Leu T.-H., Parsons J.T. Stable association of pp60src and pp59fyn with the focal adhesion-associated protein tyrosine kinase, pp125FAK. Mol. Cell. Biol. 1994;14:147–155. doi: 10.1128/mcb.14.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Calalb M.B., Polte T.R., Hanks S.K. Tyrosine phosphorylation of focal adhesion kinase at sites in the catalytic domain regulates kinase activity: a role for src family kinases. Mol. Cell. Biol. 1995;15:954–963. doi: 10.1128/mcb.15.2.954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schaller M.D., Parsons J.T. pp125FAK-dependent tyrosine phosphorylation of paxillin creates a high-affinity binding site for Crk. Mol. Cell. Biol. 1995;15:2635–2645. doi: 10.1128/mcb.15.5.2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Turner C.E. Paxillin and focal adhesion signaling. Nat. Cell Biol. 2000;2:E231–E236. doi: 10.1038/35046659. [DOI] [PubMed] [Google Scholar]
- 56.Troussard A.A., Mawji N.M., Ong C., Mui A., St.-Arnaud R., Dedhar S. Conditional knock-out of integrin-linked kinase demonstrates an essential role in protein kinase B/Akt activation. J. Biol. Chem. 2003;278:22374–22378. doi: 10.1074/jbc.M303083200. [DOI] [PubMed] [Google Scholar]
- 57.Khwaja A., Rodriguez-Viciana P., Wennström S., Warne P.H., Downward J. Matrix adhesion and Ras transformation both activate a phosphoinositide 3-OH kinase and protein kinase B/Akt cellular survival pathway. EMBO J. 1997;16:2783–2793. doi: 10.1093/emboj/16.10.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hocking D.C., Sottile J., McKeown-Longo P.J. Fibronectin’s III-1 module contains a conformation-dependent binding site for the amino-terminal region of fibronectin. J. Biol. Chem. 1994;269:19183–19191. [PubMed] [Google Scholar]
- 59.Sun X., Skorstengaard K., Mosher D.F. Disulfides modulate RGD-inhibitable cell adhesive activity of thrombospondin. J. Cell Biol. 1992;118:693–701. doi: 10.1083/jcb.118.3.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cluzel C., Saltel F., Lussi J., Paulhe F., Imhof B.A., Wehrle-Haller B. The mechanisms and dynamics of αvβ3 integrin clustering in living cells. J. Cell Biol. 2005;171:383–392. doi: 10.1083/jcb.200503017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Posch W., Vosper J., Noureen A., Zaderer V., Witting C., Bertacchi G., et al. C5aR inhibition of nonimmune cells suppresses inflammation and maintains epithelial integrity in SARS-CoV-2-infected primary human airway epithelia. J. Allergy Clin. Immunol. 2021;147:2083–2097. doi: 10.1016/j.jaci.2021.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wettstein L., Weil T., Conzelmann C., Müller J.A., Groß R., Hirschenberger M., et al. Alpha-1 antitrypsin inhibits TMPRSS2 protease activity and SARS-CoV-2 infection. Nat. Commun. 2021;12:1726. doi: 10.1038/s41467-021-21972-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Scarborough R.M., Rose J.W., Hsu M.A., Phillips D.R., Fried V.A., Campbell A.M., et al. Barbourin. A GPIIb-IIIa-specific integrin antagonist from the venom of Sistrurus m. barbouri. J. Biol. Chem. 1991;266:9359–9362. [PubMed] [Google Scholar]
- 64.Huang J., Li X., Shi X., Zhu M., Wang J., Huang S., et al. Platelet integrin alphaIIbbeta3: signal transduction, regulation, and its therapeutic targeting. J. Hematol. Oncol. 2019;12:26. doi: 10.1186/s13045-019-0709-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Park E.J., Myint P.K., Gyasi A.M., Darkway S., Caidengbate S., Ito A., et al. The spike glycoprotein of SARS-CoV-2 binds to β1 integrins expressed on the surface of lung epithelial cells. Viruses. 2021;13:645. doi: 10.3390/v13040645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Clarke N.E., Fisher M.J., Porter K.E., Lambert D.W., Turner A.J. Angiotensin converting enzyme (ACE) and ACE2 bind integrins and ACE2 regulates integrin signaling. PLoS One. 2012;7:e34747. doi: 10.1371/journal.pone.0034747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lin Q., Keller R.S., Weaver B., Zisman L.S. Interaction of ACE2 and integrin β1 in failing human heart. Biochim. Biophys. Acta. 2004;1689:175–178. doi: 10.1016/j.bbadis.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 68.Liu J., Lu F., Chen Y., Plow E., Qin J. Integrin mediates cell entry of the SARS-CoV-2 virus independent of cellular receptor ACE2. J. Biol. Chem. 2022;298:101710. doi: 10.1016/j.jbc.2022.101710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bugatti A., Filippini F., Bardelli M., Zani A., Chiodelli P., Messali S., et al. SARS-CoV-2 infects human ACE2-negative endothelial cells through an αvβ3 integrin-mediated endocytosis even in the presence of vaccine-elicited neutralizing antibodies. Viruses. 2022;14:705. doi: 10.3390/v14040705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pytela R., Pierschbacher M.D., Argraves S., Suzuki S., Ruoslahti E. Arginine-glycine-aspartic acid adhesion receptors. Methods Enzymol. 1987;144:475–489. doi: 10.1016/0076-6879(87)44196-7. [DOI] [PubMed] [Google Scholar]
- 71.Mould A.P., Askari J.A., Barton S., Kline A.D., McEwan P.A., Craig S.E., et al. Integrin activation involves a conformational change in the α1 helix of the β subunit A-domain. J. Biol. Chem. 2002;277:19800–19805. doi: 10.1074/jbc.M201571200. [DOI] [PubMed] [Google Scholar]
- 72.Woods A. Syndecans: transmembrane modulators of adhesion and matrix assembly. J. Clin. Invest. 2001;107:935–941. doi: 10.1172/JCI12802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.van Hinsbergh V.W.M., Engelse M., Quax P.H.A. Pericellular proteases in angiogenesis and vasculogenesis. Arterioscler. Thromb. Vasc. Biol. 2006;26:716–728. doi: 10.1161/01.ATV.0000209518.58252.17. [DOI] [PubMed] [Google Scholar]
- 74.Clausen T.M., Sandoval D.R., Spliid C.B., Pihl J., Perrett H.R., Painter C.D., et al. SARS-CoV-2 infection depends on cellular heparan sulfate and ACE2. Cell. 2020;183:1043–1057. doi: 10.1016/j.cell.2020.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhao M.-M., Yang W.-L., Yang F.-Y., Zhang L., Huang W.-J., Hou W., et al. Cathepsin L plays a key role in SARS-CoV-2 infection in humans and humanized mice and is a promising target for new drug development. Signal. Transduct. Target. Ther. 2021;6:134. doi: 10.1038/s41392-021-00558-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Othman H., Messaoud H.B., Khamessi O., Ben-Mabrouk H., Ghedira K., Bharuthram A., et al. SARS-CoV-2 spike protein unlikely to bind to integrins via the Arg-Gly-Asp (RGD) motif of the receptor binding domain: evidence from structural analysis and microscale accelerated molecular dynamics. Front. Mol. Biosci. 2022;9:834857. doi: 10.3389/fmolb.2022.834857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hotchkiss K.A., Matthias L.J., Hogg P.J. Exposure of the cryptic Arg-Gly-Asp sequence in thrombospondin-1 by protein disulfide isomerase. Biochim. Biophys. Acta. 1998;1388:478–488. doi: 10.1016/s0167-4838(98)00211-8. [DOI] [PubMed] [Google Scholar]
- 78.Zhong C., Chrzanowska-Wodnicka M., Brown J., Shaub A., Belkin A., Burridge K. Rho-mediated contractility exposes a cryptic site in fibronectin and induces fibronectin matrix assembly. J. Cell Biol. 1998;141:539–551. doi: 10.1083/jcb.141.2.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wrapp D., Wang N., Corbett K.S., Goldsmith J.A., Hsieh C.-L., Abiona O., et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367:1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Turoňová B., Sikora M., Schürmann C., Hagen W.J., Welsch S., Blanc F.E., et al. In situ structural analysis of SARS-CoV-2 spike reveals flexibility mediated by three hinges. Science. 2020;379:203–208. doi: 10.1126/science.abd5223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ray D., Le L., Andricioaei I. Distant residues modulate conformational opening in SARS-CoV-2 spike protein. Proc. Natl. Acad. Sci. U. S. A. 2021;118:e21009. doi: 10.1073/pnas.2100943118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Liu L., Chopra P., Li X., Bouwman K.M., Tompkins S.M., Wolfert M.A., et al. Heparin sulfate proteoglycans as attachment factor for SARS-CoV-2. ACS Cent. Sci. 2021;7:1009–1018. doi: 10.1021/acscentsci.1c00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Couchman J.R., Woods A. Syndecan-4 and integrins: combinatorial signaling in cell adhesion. J. Cell Sci. 1999;112:3415–3420. doi: 10.1242/jcs.112.20.3415. [DOI] [PubMed] [Google Scholar]
- 84.Woods A., Couchman J.R. Syndecan 4 heparan sulfate proteoglycan is a selectively enriched and widewpread focal adhesion component. Mol. Biol. Cell. 1994;5:183–192. doi: 10.1091/mbc.5.2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Carvacho I., Piesche M. RGD-binding integrins and TGF-β in SARS-CoV-2 infections - novel targets to treat COVID-19 patients? Clin. Transl. Immunol. 2021;10:e1240. doi: 10.1002/cti2.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Feire A.L., Koss H., Compton T. Cellular integrins function as entry receptors for human cytomegalovirus via a highly conserved disintegrin-like domain. Proc. Natl. Acad. Sci. U. S. A. 2004;101:15470–15475. doi: 10.1073/pnas.0406821101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gavrilovskaya I.N., Brown E.J., Ginsberg M.H., Mackow E.R. Cellular entry of hantaviruses which cause hemorrhagic fever with renal syndrome is mediated by β3 integrins. J. Virol. 1999;73:3951–3959. doi: 10.1128/jvi.73.5.3951-3959.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Meliopoulos V.A., Van de Velde L.-A., Van de Velde N.C., Karlsson E.A., Neale G., Vogel P., et al. An epithelial integrin regulates the amplitude of protective lung interferon responses against multiple respiratory pathogens. PLoS Pathog. 2016;12:e1005804. doi: 10.1371/journal.ppat.1005804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yan S., Sun H., Bu X., Wan G. New strategy for COVID-10. An evolutionary role for RGD motif in SARS-CoV-2 and potential inhibitors for virus infection. Front. Pharmacol. 2020;11:912. doi: 10.3389/fphar.2020.00912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Harvey W.T., Carabelli A.M., Jackson B., Gupta R.K., Thomson E.C., Harrison E.M., et al. SARS-CoV-2 variants, spike mutations and immune escape. Nat. Rev. Microbiol. 2021;19:409–424. doi: 10.1038/s41579-021-00573-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Beyerstedt S., Casaro E.B., Rangel É.B. COVID-19: angiotensin-converting enzyme 2 (ACE2) expression and tissue susceptibility to SARS-CoV-2 infection. Eur. J. Clin. Microbiol. Infect. Dis. 2021;40:905–919. doi: 10.1007/s10096-020-04138-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cohler L.F., Saba T.M., Lewis E., Vincent P.A., Charash W.E. Plasma fibronectin therapy and lung protein clearance with bacteremia after surgery. J. Appl. Physiol. 1987;63:623–633. doi: 10.1152/jappl.1987.63.2.623. [DOI] [PubMed] [Google Scholar]
- 93.Curtis T.M., Rotundo R.F., Vincent P.A., McKeown-Longo P.J., Saba T.M. TNF-α-induced matrix Fn disruption and decreased endothelial integrity are independent of Fn proteolysis. Am. J. Physiol. Lung Cell. Mol. Physiol. 1998;275:L126–L138. doi: 10.1152/ajplung.1998.275.1.L126. [DOI] [PubMed] [Google Scholar]
- 94.Rotundo R.F., Curtis T.M., Shah M.D., Gao B., Mastrangelo A., LaFlamme S.E., et al. TNF-α disruption of lung endothelial integrity: reduced integrin mediated adhesion to fibronectin. Am. J. Physiol. Lung Cell. Mol. Physiol. 2002;282:L316–L329. doi: 10.1152/ajplung.00145.2000. [DOI] [PubMed] [Google Scholar]
- 95.Resnikoff M., Brien T., Vincent P.A., Rotundo R.F., Lewis E., McKeown-Longo P.J., et al. Lung matrix incorporation of plasma fibronectin reduces vascular permeability in postsurgical bacteremia. Am. J. Physiol. Lung Cell. Mol. Physiol. 1999;277:L749–L759. doi: 10.1152/ajplung.1999.277.4.L749. [DOI] [PubMed] [Google Scholar]
- 96.Roth T., Podestá F., Stepp M.A., Boeri D., Lorenzi M. Integrin overexpression induced by high glucose and by human diabetes: potential pathyway to cell dysfunction in diabetic microangiopathy. Proc. Natl. Acad. Sci. U. S. A. 1993;90:9640–9644. doi: 10.1073/pnas.90.20.9640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kitsiou P.V., Tzinia A.K., Stetler-Stevenson W.G., Michael A.F., Fan W.-W., Zhou B., et al. Glucose-induced changes in integrin and matrix related functions in cultured human glomerular epithelial cells. Am. J. Physiol. Ren. Physiol. 2003;284:F671–F679. doi: 10.1152/ajprenal.00266.2002. [DOI] [PubMed] [Google Scholar]
- 98.Kim C.H., Vaziri N.D. Hypertension promotes integrin expression and reactive oxygen species generation by circulating leukocytes. Kidney Int. 2005;67:1462–1470. doi: 10.1111/j.1523-1755.2005.00223.x. [DOI] [PubMed] [Google Scholar]
- 99.Burgess M.L., Terracio L., Hirozane T., Borg T.K. Differential integrin expression by cardiac fibroblast from hypertensive and exercise-trained rat hearts. Cardiovasc. Pathol. 2002;11:78–87. doi: 10.1016/s1054-8807(01)00104-1. [DOI] [PubMed] [Google Scholar]
- 100.Umesh A., Paudel O., Cao Y.-N., Myers A.C., Sham J.S. Alteration of pulmonary artery integrin levels in chronic hypoxia and monocrolatine-induced pulmonary hypertension. J. Vasc. Res. 2011;48:525–537. doi: 10.1159/000329593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Mezu-Ndubuisi O.J., Maheshwari A. The role of integrins in inflammation and angiogeneisis. Pediatr. Res. 2020;89:1619–1626. doi: 10.1038/s41390-020-01177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Akiyama S.K. Purification of fibronectin. Curr. Protoc. Cell Biol. 2013;60 doi: 10.1002/0471143030.cb1005s60. 10.15.11-10.15.13. [DOI] [PubMed] [Google Scholar]
- 103.Hocking D.C., Smith R.K., McKeown-Longo P.J. A novel role for the integrin-binding III10 module in fibronectin matrix assembly. J. Cell Biol. 1996;133:431–444. doi: 10.1083/jcb.133.2.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sottile J., Shi F., Rublyevska I., Chiang H.-Y., Lust J., Chandler J. Fibronectin-dependent collagen I deposition modulates the cell response to fibronectin. Am. J. Physiol. Cell Physiol. 2007;293:C1934–C1946. doi: 10.1152/ajpcell.00130.2007. [DOI] [PubMed] [Google Scholar]
- 105.Pereira M., Rybarczyk B.J., Odrljin T.M., Hocking D.C., Sottile J., Simpson-Haidaris P.J. The incorporation of fibrinogen into extracellular matrix is dependent on active assembly of a fibronectin matrix. J. Cell Sci. 2002;115:609–617. doi: 10.1242/jcs.115.3.609. [DOI] [PubMed] [Google Scholar]
- 106.Roy D.C., Wilke-Mounts S., Hocking D.C. Chimeric fibronectin matrix mimetic as a functional growth- and migration-promoting adhesive substrate. Biomaterials. 2011;32:2077–2087. doi: 10.1016/j.biomaterials.2010.11.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hocking D.C., Kowalski K. A cryptic fragment from fibronectin’s III1 module localizes to lipid rafts and stimulates cell growth and contractility. J. Cell Biol. 2002;158:175–184. doi: 10.1083/jcb.200112031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Gildner C.D., Roy D.C., Farrar C.S., Hocking D.C. Opposing effects of collagen I and vitronectin on fibronectin fibril structure and function. Matrix Biol. 2014;34:33–45. doi: 10.1016/j.matbio.2014.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are contained within the article, with supplementary data available upon request (denise_hocking@urmc.rochester.edu).