Abstract
Background
The prevention and treatment of eating disorders relies on an extensive body of research that includes various foci and methodologies. This scoping review identified relevant studies of eating disorders, body image, and disordered eating with New Zealand samples; charted the methodologies, sample characteristics, and findings reported; and identified several gaps that should be addressed by further research.
Methods
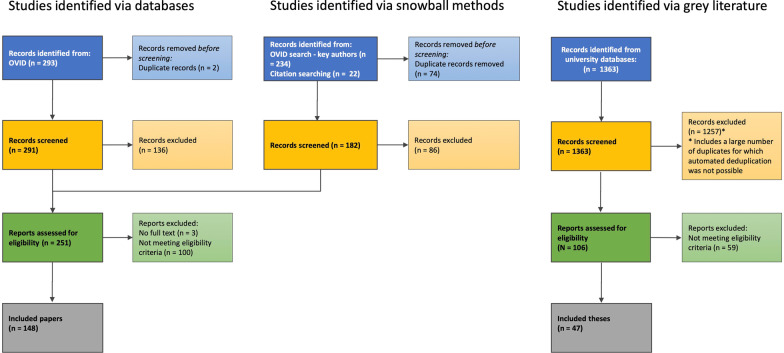
Using scoping review methodology, two databases were searched for studies examining eating disorders, disordered eating, or body image with New Zealand samples. Snowball methods were further used to identify additional relevant articles that did not appear in initial searches. Two independent reviewers screened the titles and abstracts of 473 records. Full text assessment of the remaining 251 records resulted in 148 peer-reviewed articles being identified as eligible for the final review. A search of institutional databases yielded 106 Masters and Doctoral theses for assessment, with a total of 47 theses being identified as eligible for the final review. The included studies were classified by methodology, and the extracted information included the study foci, data collected, sample size, demographic information, and key findings.
Results
The eligible studies examined a variety of eating disorder categories including binge-eating disorder, bulimia nervosa, and anorexia nervosa, in addition to disordered eating behaviours and body image in nonclinical or community samples. Methodologies included treatment trials, secondary analysis of existing datasets, non-treatment experimental interventions, cross-sectional observation, case-control studies, qualitative and mixed-methods studies, and case studies or series. Across all of the studies, questionnaire and interview data were most commonly utilised. A wide range of sample sizes were evident, and studies often reported all-female or mostly-female participants, with minimal inclusion of males and gender minorities. There was also an underrepresentation of minority ethnicities in many studies, highlighting the need for future research to increase diversity within samples.
Conclusion
This study provides a comprehensive and detailed overview of research into eating disorders and body image in New Zealand, while highlighting important considerations for both local and international research.
Keywords: Eating disorders, Anorexia nervosa, Bulimia nervosa, Binge eating disorder, Scoping review, New Zealand
Plain English summary
Research into eating disorders should include different methods, and should be relevant to people of different ages, gender identities, and ethnicities. We completed a scoping review of research into eating disorders, disordered eating, and body image in New Zealand samples. We searched academic databases for relevant articles, and then screened the articles for eligibility. We then hand-searched key articles, and searched databases again using the names of key authors. A total of 148 peer reviewed articles and 47 theses were eligible for the review, and from these we extracted data on the study method, sample characteristics, and the focus and results. A wide range of methods and sample sizes were reported, and the studies explored several different eating disorders, as well as disordered eating and body image in nonclinical samples. However, the studies often involved all or mostly female samples, few to no gender minority participants, and an underrepresentation of minority ethnicities. Funders should provide adequate time and financial resources to fund recruitment from historically under-represented groups, emphasising their involvement as active researchers. In addition, funders should consider financing the use of novel or underutilised methods to advance knowledge in this field.
Introduction
Eating disorders such as binge-eating disorder (BED), bulimia nervosa (BN), and anorexia nervosa (AN) are complex and potentially life-threatening psychiatric illnesses. Research in the New Zealand population suggests a lifetime prevalence of 1.9% for BED, 1–1.3% for BN, and 0.6% for AN [1, 2]. These disorders create a significant burden upon the lives of those affected, with many individuals facing prolonged periods of inpatient treatment or multiple relapses. Although research into eating disorders has made substantial progress in recent years, the limited success of available treatments underscores the need for a more complete picture of how to best understand and approach this cluster of disorders.
In addition to the more commonly acknowledged eating disorders noted above, there is a growing awareness surrounding those whose symptoms fall within the Diagnostic and Statistical Manual (DSM-5) [3] other specified feeding and eating disorders (OSFED) diagnostic category. These disorders include atypical or subthreshold forms of BN, AN, and purging disorder which previously were included in the DSM-IV eating disorder not otherwise specified (EDNOS) category, and the newly included night eating syndrome. Despite this group of disorders having been identified as being the most prevalent [4], research surrounding them is comparatively sparse.
At a sub-threshold level, eating disorder psychopathology is common in New Zealand, and has been reported in adolescents, university students, and middle-aged samples [5–7]. Disordered eating is often tightly intertwined with body dissatisfaction—a core symptom in the diagnostic criteria for AN and BN [3], which is also suggested to be relevant for BED [8]. Body dissatisfaction is regarded as a significant risk factor for the development of eating disorders [9, 10], with etiological models commonly citing the relationship between body dissatisfaction and subthreshold disordered eating. Body dissatisfaction can be seen as almost normative among young women and, increasingly, young men [11]. In light of this, our understanding of disordered eating can be supplemented by research into body dissatisfaction at both a clinical and subthreshold level.
Although many aspects of eating disorders, subthreshold disordered eating, and body dissatisfaction are studied extensively internationally, it is often unclear whether findings generalise to a New Zealand population. Moreover, even where such findings are applicable, there remains a need to understand these issues in a manner consistent with New Zealand’s unique sociocultural context [12, 13]. Achieving this requires a comprehensive body of research to be conducted within New Zealand, ideally with a range of study designs to ensure a detailed and broad understanding of these issues. Moreover, this research should adequately cover the range of issues pertaining to body image and eating disorders, and include samples that are representative of the population as a whole (such as Indigenous Māori and Pasifika populations). To this end, it is critical that local researchers are aware of what is available within the literature and what is lacking, thus informing the direction for future research and methodologies. However, we were unable to identify any comprehensive reviews of relevant studies involving New Zealand-based participants, thereby hindering progression of research into the issues at hand.
In an effort to bridge the gap between extant research and future projects, the present review scopes and synthesises the foci reported by studies examining eating disorders, disordered eating, and body image within studies that include New Zealand samples. This review was informed by scoping methodology outlined by the Preferred Reporting Items for Systematic Review and Meta-Analysis extension for Scoping Review (PRISMA-ScR) [14]. It involved: (a) the identification of relevant journal articles and theses; (b) charting the foci, methodologies, sample characteristics, and findings reported in the identified literature; and (c) a descriptive review of what was included, as well as gaps and areas which may be expanded upon.
Methods
Research question
The scoping review was informed by the research question: “To date, what are the methodologies and results reported by studies that have examined eating disorders, disordered eating, and body image in clinical and non-clinical samples in New Zealand?”.
Eligibility
Meeting initial eligibility criteria was dependent on (1) the full text being available, (2) some portion of the sample living in New Zealand during the research, (3) the article or thesis being available in English, (4) the record not being a duplicate, and (5) the topic or a part of the focus being within scope. The scope was informed by the overarching research question of this review, and research items needed to include an examination of eating disorders, disordered eating, or body image in New Zealand samples.
Included eating disorder diagnoses were BED, BN, and AN in addition to disorders in the Other Specified Feeding and Eating Disorder (OSFED) category (DSM-5) or the former Eating Disorder Not Otherwise Specified (EDNOS) category (DSM-IV-TR) [15]. Also included were studies where only symptoms of these disorders (e.g. binge eating, purging) were assessed. Not included were Avoidant/Restrictive Food Intake Disorder (ARFID), pica and rumination disorder; categories shifted to the eating disorders section of DSM-5 from the DSM-IV-TR Feeding and Eating Disorders of Early Childhood Section [3, 15]. Body image in the context of this review included perceptions of one’s own body shape and size, but excluded research items that focused only on concerns such as perceived facial flaws [16], which are often a feature of body dysmorphic disorder. Lastly, research on samples of clinicians working in eating disorder treatment were included, given that this adds considerably to knowledge surrounding eating disorders and their treatment in New Zealand.
Both qualitative and quantitative studies were deemed in scope, as were case studies and case series. International studies that included original data from one or more New Zealand participants were included; however, meta analyses and systematic reviews were not, given that relevant data were likely already published elsewhere. It was decided that conference abstracts would be excluded, given that the findings were either published elsewhere, or the abstracts did not include sufficient information to meet basic eligibility criteria. Lastly, any trials that were in progress but unpublished were also excluded, as it would not be possible to chart the findings of those studies.
Initial database search
To locate references for journal articles from a wide range of sources, relevant search terms were entered into Ovid (EMBASE, psychINFO). The search terms “eating disorder*.kw”, “anorexia nervosa.kw”, “bulimia nervosa.kw”, “binge eating disorder.kw”, “disordered eating.kw”, and “body image.kw” were combined using the “OR” function. This result was then combined with “new zealand.af” using the AND function, and the results were deduplicated. No additional search limitations were used in Ovid. The cut-off date for this and subsequent searches was set to 20 May, 2021.
Snowball searches
During the initial screen of records returned in Ovid, seven authors known to publish research within this scope frequently appeared as first authors. Publications from these authors were further searched in Ovid by entering the search terms “jordan jennifer.au”, “carter frances a.au”, “gendall kelly a.au”, “mcintosh virginia v w or mcintosh virginia violet williams or mcintosh virginia vw).au”, “bulik cynthia m.au”, “wilksch simon m or wilksch sm.au”, “latner janet d or latner jd.au”. These searches were combined using the OR function, and the result was then combined with “new zealand.af” using the AND function. The results were deduplicated within Ovid before being merged with the initial OVID search records, and the combined results were again deduplicated.
The citations within key papers were also hand-searched by two reviewers (HK and LC) for additional relevant publications within New Zealand. Key papers included relevant epidemiological studies and treatment trials known among New Zealand eating disorders researchers. Referenced papers were then located and screened using the same criteria and checklist. Furthermore, when papers reporting secondary analyses referred back to publications which described original study samples, those publications were identified and screened for inclusion.
Grey literature search
To locate Master’s and Doctoral theses, institutional research archives were searched for each of the University of Otago (OURArchive), University of Waikato (Research Commons), University of Canterbury (College of Science, College of Arts), Massey University (Massey Research Online), Auckland University of Technology (Open Repository), and Victoria University of Wellington (Open Access), and University of Auckland (ResearchSpace). A total of 29 potentially relevant theses, including 25 from the University of Auckland, were unavailable online or were only accessible only to staff and students at the relevant institutions. As such, full-text screening was unable to be completed for these records.
The terms “binge eating disorder”, “bulimia nervosa”, “anorexia nervosa”, and “body image” were entered into each university research archive and limited to thesis where possible. The terms “eating disorder” and “disordered eating” were also entered into the same archives. In some instances, these latter terms returned the same results as one of the initial four search terms, such as the results for “eating disorder” being the same as those for “binge eating disorder” in one database. In such cases, results were not added to the final number of records to be screened. In addition, when a very large number of unrelated results were returned for thesis search terms, the results for those terms were limited to “title contains”.
In some cases, the findings from grey literature had already been published in peer reviewed journals. To avoid overlap in these situations, the grey literature record was removed as a duplicate in favour of the published article. Further journal articles identified during this process were labelled as being found via snowball search.
Record screening and eligibility
Search results from OVID were exported into EndNote, and then entered into an Excel spreadsheet to be screened separately by two blind reviewers (HK and LC). The reviewers first pre-screened the titles and abstracts of each record for relevance. Journal articles that were eligible for full-text searching were then located where possible, and the reviewers filled out a checklist to determine whether predetermined eligibility criteria were met. Following blind review, authors HK and LC met to discuss a small number of cases where the decision to include or exclude a record was inconsistent. In these cases, the records were further assessed and a final decision was agreed upon for each, with a total of 10 papers being discussed and 7 of these being excluded from the review.
Data extraction and study classification
For each included research item, a range of data were extracted. The relevant population(s) or construct(s) of interest were identified, including any specific eating disorders being examined, disordered eating among nonclinical (NC) populations, or clinicians working within eating disorder treatment settings. The focus of each study was also briefly summarised, as were the key data collection instruments or measures. Gender and ages of participants were recorded as specified in the research article or thesis, however gender data were converted to percentages where applicable, and age ranges were favoured where available. Ethnicities were also recorded as specified, however for consistency, terms such as “Caucasian” and “New Zealand European” were recorded as “European” for the purposes of this review, and these data were also converted to percentages where applicable. The key findings were summarised based upon information within abstracts and full texts. Lastly, each study was categorised according to the primary methodology used, while those that analysed data from existing treatment trial and survey datasets were labelled as secondary analyses.
The scoping review has been registered on OSF (https://osf.io/c8jwn). No ethical approval was required for this review.
Results
Total records included
The total number of records identified and excluded at each step of the literature search are detailed in Fig. 1. A total of 195 records were included in the final review, with 148 journal articles and 47 theses (13 Doctoral, 34 Master’s) having met full eligibility criteria for the study. Journal articles were published between December 1978 and May 2021, while theses were completed between 1990 and 2021. The specific completion dates for two theses finalised in 2021 were unable to be verified, however the decision was made to include those in the review. The number of publications per year, in addition to the cumulative total of publications, is shown in Fig. 2.
Fig. 1.
PRISMA flowchart depicting record identification process and number of records included or removed at each stage
Fig. 2.
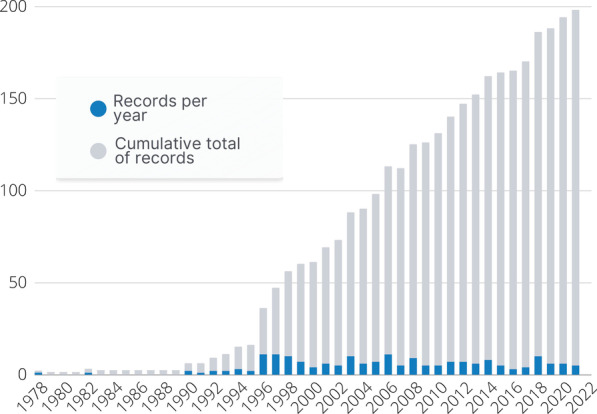
Number of included theses or journal articles published each year and cumulative totals
Study classifications
Study methodologies across the journal articles and theses fell into seven broad categories of treatment trials (18 records, Table 1), secondary analyses of existing datasets (50 records, Table 2), non-treatment experimental interventions (17 records, Table 3), cross-sectional research (63 records, Table 4), case control studies (9 records, Table 5), qualitative or mixed-methods (28 records, Table 6), or case studies and series (10 records, Table 7).
Table 1.
Treatment trials
| References | Population focus | Focus | Key data collected | Sample n | Gender | Age | Ethnicity | Summary findings |
|---|---|---|---|---|---|---|---|---|
| Babbott [59]* | Non-clinical (NC) | Non-concurrent multiple baseline: Trialling acceptance and commitment therapy for disordered eating | EAT-26, AAQ, SWLS, SA-45 | 17 | 12% M 88% F | 18–64 | 64.7% European, 5.9% Māori, 11.8% Indian, 11.8% Latin American, 5.9% South African | Significant decrease in eating pathology, but not general pathology |
| Bulik [18] | BN (BTS) | RCT: Results from end of RCT and follow-up at 6 and 12 months. Therapies were CBT + then randomisation to 1) exposure with response prevention to binges (B-ERP), 2) to purging (P-ERP) or 3) relaxation | Physiological, biological measures, self-report measures, SCID I and II, HDRS, GAF, EDI | 135 | F | 17–45 |
BTS sample 91% European 6% Maori, Pasifika, Asian |
All therapies were effective and did not differ on abstinence or binge purge frequency. B-ERP had advantage for other ED symptoms, and mood but this was not maintained over follow-up |
| Carter [60] | BN (BTS) | RCT: 3-year follow up of BTS | Structured interview of ED symptoms, EDI, HDRS, GAF | 135 (113 at follow up) | F | 17–45 | BTS sample | At the 3-year follow-up, 85% of the sample had no current diagnosis of bulimia nervosa. Failure to complete CBT was associated with inferior outcome. No differential effects were found for exposure versus nonexposure-based treatment |
| Carter [61] | AN (ATS) | RCT: long-term efficacy of three psychotherapies for AN (ATS) | SCID (DSM-IV). Global AN symptom status,, physical, cognitive and behavioural ED measures, EDE, EDI-2, GAF, HDRS | 43 | F | 17–40 |
ATS sample 100% European |
SSCM advantage over CBT and IPT during treatment was not sustained. All effective bus no significant differences among treatments at follow-up |
| Clyne [62] | BED | Single case design with multiple baseline evaluation: preliminary trial of a psychoeducational group programme of emotion regulation for treatment of BED | Daily Log of Eating and Emotions, BES, QEWP, DASS, PSS, The COPE, EIS, TAS-20, ATSS | 11 | F | 18–69 | 100% European | Reduced binge-eating, alexithymia, stress, and depression. Improvements in cognition. At 2/3 month follow up, all participants no longer met criteria for BED |
| Clyne [63] | BED | Non-randomised with waitlist control group: regulation of negative emotion as a possible BED treatment | QEWP, EDE, EDE-Q, BES, EES | 23 | F | 18–65 | 91.3% European, 4.3% Māori, 4.3% Other | Treatment outcomes comparable to existing therapies for BED |
| Davey [64]* | BN, AN, EDNOS, NC | Quasi-experimental (non-randomised) 2-group comparison: Efficacy of two pre-treatment interventions focused on motivation. Groups were motivation + education versus motivation alone | EDE-Q4, BDI-II, Dflex, MSOC, Change Continuum | 252 | 97% F, 3%M | 11–62 | 88.5% European, 4.8% Māori, 4.8% Asian, 0.8% Pasifika, 0.4% South American, 0.8% Middle Eastern | Improvements in motivational stage of change were observed in both groups, while improvements in patient readiness, confidence and importance to change as well as treatment attendance were identified in the pure Motivation Group |
| de Hoedt Norgrove [65]* | Emotional eaters | Multiple baseline design: Acceptance and commitment therapy (ACT) for emotional eating using a multiple baseline | Feedback questionnaire, MEAQ, valuing questionnaire, AAO, CES, GHQ, journal entries (e.g. frequency of unhealthy eating) | 8 |
6 F 2 M |
18–52 | 75% European, 12.5% European/Māori, 12.5% Māori/ Pasifika | Reduction in binge eating, associated with decreased experiential avoidance and cognitive inflexibility |
| McIntosh [17] | AN (ATS) | RCT: comparing efficacy of CBT versus IPT versus a control therapy (nonspecific supportive clinical management | Global AN symptom status, SCID for DSM-IV, EDE, HDRS, GAF, EDI-2 | 56 | F | 17–40 |
ATS sample 96% European |
Nonspecific supportive clinical management (subsequently called SSCM) superior in completers and intention to treat analyses |
| McIntosh [66] | BN (BTS) | RCT: Long-term follow up of participants from RCT for BN | SCID, Structured interview of ED symptoms, EDI, HDRS, GAF | 135 (109 at follow up) | F | 14–45 | BTS sample | Those in in SSCM group more likely to have a good outcome post-treatment, but no differences between groups at long-term (5 year) follow-up |
| McIntosh [19] | BED, BN (BEP) | RCT: efficacy of three therapies for binge eating: Standard CBT versus CBT augmented with schema therapy versus CBT with a focus on appetite | SCID-I and II, EDE-12, EDI-2, SCL-90-R | 56 | F | 16–65 | BEP sample | All groups improved but no significant differences between therapies |
| Mercier [67]* | BN | RCT: Tested intervention aiming to alter coping behaviours and cognitive processes in those with BN versus directly targeting clinical features. Wait-list control and follow-up design | General information questionnaire, DSSI-R, The Bulimia Test, Affectometer 2, BDI, RSES, STAI, TAI | 24 | F | 19.3–41.1 | Not stated | Decreased BN behaviours and cognitions following alternative intervention, little difference between intervention groups by 3 years |
| Roberts [68] | BN, AN | Single arm design: Efficacy and feedback on group cognitive remediation therapy | Dflex, Autism Quotient, EDE-Q, DASS-21, BMI, qualitative questionnaire | 28 |
96% F 4% M |
M 25.07 (SD 8.25) | Not stated | Intervention was effective and had positive qualitative feedback |
| Then [69]* | AN | Single arm design: Efficacy of metacognitive therapy modified for the treatment of A | BMI, EDE-Q, MCQ-30, TCQ | 12 | Not stated | M 22.17 (SD 5.17) | 1 NZE, 2 Māori, 3 Samoan, 4 Cook island, 5 Tongan, 6 Niuean, 7 Chinese, 8 Indian, 9 other | Mixed results but there were reductions in patients positive beliefs about worry, depressive symptoms, worries and rumination levels following metacognitive therapy |
| Wallis [70]* | BED | Quasi-experimental (non-randomised intervention) with control: Teaching emotional discrimination and management in a group programme for those with BED | EDI-2, MHO, BDI, BAI, EES, COPE, GHQ | 6 (BED n = 3, NC n = 3) | F | 25–47 | 83% European, 17% Māori | EDI-2, EES, BDI, BAI, and COPE results indicated positive results following the programme |
| Wilksch [71] | NC (MS -T) | RCT: Trialling online programs for efficacy in reducing risk of disordered eating in an Australasian sample | EDE-Q | 575 | F | 18–25 | 82.2% European, 8.8% Asian, other not stated | Media Smart Targeted program reduction in DE |
| Wilksch [72] |
BED, BN, AN, OSFED, NC (MS—T) |
RCT: Programme seeking to reduce risk of eating disorder diagnosis in NZ and Australia | EDE-Q | 316 (MS-T n = 122 (baseline ED diagnosis n = 90): CT = 194 (baseline ED diagnosis n = 130)) | F |
M 20.8 (SD 2.26) |
MS-T sample | At 12-month follow up MS-T participants were 75% less likely than controls to meet ED criteria, this finding was also significant amongst both non-treatment seekers and treatment seekers |
| Wilksch [73] | NC | RCT: An online 9-module eating disorder risk reduction program (Media Smart—Targeted (MS-T)) and control condition (positive body-image tips) | DASS-21, Mini International Neuropsychiatric Interview (dependence on alcohol, dependence on recreational drugs, high suicidality) | 316 | F | 18–25 | States most common is European and Asian | MS-T shows positive effect on eating disorder risk, as well as other mental health factors |
NC non-clinical, RCT randomised-controlled trial, EAT Eating Attitudes Questionnaire, AAQ Acceptance and Action Questionnaire, SWLS Satisfaction with Life Scale, SA-45 Symptom Assessment-45 Questionnaire, SCID Structured Clinical Interview for DSM Disorders, HDRS Hamilton Depression Rating Scale, GAF Global Assessment of Functioning Scale, EDI Eating Disorders Inventory, EDE Eating Disorder Examination, BES Binge Eating Scale, QEWP Questionnaire on Eating and Weight Patterns, COPE Coping Orientation to Problems Experienced Inventory, EI Emotional Intelligence, TAS-20 Toronto Alexithymia Scale, ATSS Activated Thoughts in Simulated Situations, EDE Eating Disorders Examination interview, EDE-Q Eating Disorder Examination Questionnaire, EES Emotional Empathy Scale, BDI Beck Depression Inventory, Dflex Detail and Flexibility Questionnaire, MSOC Motivational Stages of Change, MEAQ Multidimensional Experiential Avoidance Questionnaire, AAQ The Acceptance and Action Questionnaire, CES Compulsive Eating Scale, GHQ General Health Questionnaire, CSPRS-AN Collaborative Study Psychotherapy Rating Scale—Anorexia Nervosa, SCL-90-R Symptom Checklist-90-Revised, DSSI-R Delusions-Symptoms-State Inventory-Revised, RSES Rosenberg Self-Esteem Scale, STAI State Trait Anxiety Inventory, TAI Test Anxiety Inventory, DASS Depression Anxiety and Stress Scale, PSS Perceived Stress Scale, EIS Emotional Intelligence Scale, BMI body mass index, MCQ Metacognition Questionnaire, TCQ Thought Control Questionnaire, MHO Middlesex Hospital Questionnaire, COPE Coping Orientation to Problems Experienced
*Identifies that the record is a thesis
Table 2.
Secondary analyses
| References | Population focus | Focus | Key data collected | Sample n | Gender | Age | Ethnicity | Summary findings |
|---|---|---|---|---|---|---|---|---|
| Anderson [74] | BN (BTS) | Temperament and character ratings at the beginning of CBT intervention and one year later | TCI, HDRS, B-ERP, P-ERP | 135 (91 for this report) | F | 17–45 | BTS sample | Decreases in harm avoidance temperament and increase in self-directedness |
| Bourke [75] | BN (BTS) | Neuropsychological function in BN with comorbid psychological conditions | Diagnostic interviews, neuropsychological testing | 41 | F | 17–45 | BTS sample | Borderline personality disorder and MD together associated with impaired cognitive function |
| Bulik [76] | BN (BTS) | Examined BN sample with and without personality disorders, and self-directedness in predicting presence of personality disorders | SCID for DSM-III-R, HDRS, custom structured interview of BN symptoms, GAF | 76 | F | > 16 | BTS sample | 63% had 1or more personality disorder diagnoses, which were associated with greater depressive symptoms, laxative use, greater body dissatisfaction, worse global functioning, and lower self-directedness |
| Bulik [77] | BN (BTS) | Examining histories of anxiety disorders in those with BN | SCID I (DSM-III-R), age onset, Self-report ED symptoms | 114 | F | 17–45 | BTS sample | Anxiety disorders onset earlier than BN |
| Bulik [78] | BN (BTS) | Salivary reactivity to palatable food before, during, and after treatment | SCID (DSM-III-R), HDRS, Physiological responses | 31 | F | 18–40 | BTS sample | After treatment, salivation increased significantly (p = .002) over baseline after presentation of the same foods |
| Bulik [79] | BN (BTS) | Comparing onset of binge eating, dieting and BN in relation to clinical characteristics and personality traits | SCID modified, SCID II, HDRS, TCI | 108 | F | 17–45 | BTS sample | Dieting preceded binge eating in the majority of women with BN. In the minority of women where binge eating precedes dieting, markedly higher novelty seeking and lower harm avoidance are displayed |
| Bulik [80] | BN (BTS) | Comparing BN participants with/without comorbid alcohol dependence | SCID (DSM-III-R), HDRS, GAFS, EDI-2, TCI, BIS, Défense Style Questionnaire | 114 | F | 17–45 | BTS Sample | Women with comorbid BN and alcohol dependence have increased psychopathology, impulsivity and novelty seeking |
| Bulik [81] | BN, AN, MD | Comparing prevalence and ago of onset of adult and childhood anxiety disorders relative to primary diagnosis of BN, AN, MD and NC controls | Diagnostic Interview for Genetic Studies, SCID for DSM-III-R | 68 (AN), 116 (BN), 56 (MD), 98 (NC) | F | AN: M 31.3, BN: 26.0, MD: M 30.6, NC: M 35.5 | Not stated | Certain anxiety disorders (specific phobia, overanxious disorder) were non-specific risk factors for later affective and eating disorders, while others more specific (e.g. AN and antecedent OCD) |
| Bulik [82] | BN (BTS) | Predictors of successful BN treatment | SCID and SCID-II HDRS, GAFS, EDI-2, Bulimia Cognitive Distortions Scale TCI | 98 | F | 17–45 | BTS sample | Baseline symptomatology and personality factors predicted rapid and sustained treatment response |
| Bulik [83] | BN, AN (BTS, Christchurch Outcome of Depression Study, Sullivan et al. [84] study) | Personality traits and history of suicidal behaviour in BN, AN and MD | TCI |
269 (AN 70; BN 152; MDD 59) |
F | 22–39 | Not stated for AN or MDD sample but BN sample was part of the BTS sample | Suicide attempts are equally common in women with eating disorders and women with depression, and were associated with the temperament dimension of high persistence and the character dimensions of low self-directedness and high self-transcendence |
| Carter [85] | BN (BTS) | Examining changes in information processing speed following CBT | Stroop test performance, self-reported recent binge, vomiting, and other purging | 98 | F | 17–45 | BTS sample | Information processing speed not associated with change across BN treatment |
| Carter [86] | BN (BTS) | How performance on cue reactivity test predicted outcome of psychotherapy for BN | Clinician interview, EDI, HDRS, GAF, blood pressure, heart rate, salivation | 135 | F | 17–45 | BTS sample | Abstention during pre-treatment cue reactivity task was associated with better outcome at 6-month follow-up |
| Carter [87] | BN (BTS) | How CBT for BN changed cue reactivity and associations with self-report measures | Clinician interview, EDI, HDRS, GAF, blood pressure, heart rate, salivation | 135 | F | 17–45 | BTS sample | Association between favourable treatment outcome and low cue reactivity on self-report measures at posttreatment |
| Carter [88] | BN (BTS) | Evaluating specific hypotheses on the relationship of cue reactivity and outcome in BN women | Structured interview, EDI, HDRS, Axis V of DSM-III-R, self-report, physiological measures | 135 | F | 17–45 | BTS sample | Pre-treatment cue reactivity could not predict most effective treatment modality |
| Carter [89] | BN (BTS) | Whether having a child after BN treatment puts women at increased risk for ED or depression | SCID (DSM-III-R), life charts (key life events, e.g. pregnancy), menstrual + weight history, pregnancy/childbirth | 135 | F | 17–45 | BTS sample | Childbirth was not specifically associated with symptomatology following treatment for bulimia nervosa |
| Carter [90] | BN (BTS) | Factors related to childbirth reported at BN treatment follow-up | SCID, EDI, HDRS, BMI, GAF, BDI, SCL | 125 | F | 17–45 | BTS sample | Demographic variables and poor functioning following treatment predictive of non-conception |
| Carter [91] | BN (BTS) | Influence of pre-treatment weight across treatment and five-year follow-up |
Pre-treatment BMI, BMI at follow-up |
134 | F | 17–45 | BTS sample | Participants who were overweight at baseline gained more weight than those in low and normal weight groups |
| Carter [92] | BN (BTS) | 5-year follow-up of those who participated in BTS RCT for BN | SCID (DSM-III-R), EDI, HDRS, GAF, BMI | 80 | F | 17–45 at treatment | ATS sample | Five years after treatment, approximately one half of the participants had changed substantially in weight. Patients who gained weight were more likely to have been heavier and more dissatisfied with their body |
| Carter [93] | BN (BTS) | Testing whether able to assess cue reactivity with a self-report questionnaire | Adapted Situational Appetite Measure (SAM) | 135 (complete data for 82) | F | 17–45 | BTS sample | A self-report questionnaire provided useful information regarding cue reactivity among women treated for bulimia nervosa. Greater improvements in cue reactivity associated with favourable treatment outcomes |
| Carter [94] | BN (BTS, Christchurch Outcome of Depression Study, postpartum study [95]) | Sex frequency, enjoyment, and issues in women with AN, MD, or in postpartum period | Social Adjustment Scale | 76 (10 AN) | F | AN: 28.4 (SD 6.1) | Various samples | AN and MD groups more likely to have had sex in prior two weeks, but also more likely to report sexual problems, than postpartum group |
| Carter [96] | BN (BTS) | Relationship between weight suppression prior to treatment and treatment outcomes | BMI | 132 | F | 17–45 | BTS sample | Found that weight suppression did not predict treatment outcome but did predict weight gain |
| Carter [97] | AN (ATS) | Whether severity of weight suppression predicted total rate and amount of weight gain during AN recovery | BMI | 56 | F | 17–45 | BTS sample | Weight suppression was positively associated with total weight gain and rate of weight gain over treatment |
| Falloon [98]* | BED, BN (BEP) | Focused on how closely therapists in the BEP RCT adhered to each of three psychotherapies for binge eating | Collaborative Study Psychotherapy Rating Scale-Binge Eating (CSPRS-BE) | 112 participants, 4 therapists | F | M 35.3 (SD 12.6) | 67% NZ European, 17% other European, 9.8% Māori, 3.6% Asian, 2.7% other | Therapy modalities were distinguishable by raters blind to treatment |
| Gendall [99] | BN (BTS) | Comparing nutrient intake of women with BN regarding recommended dietary allowances, and to population sample | Food diaries |
50 (BN) 468 (Population sample) |
F |
BN:17–45 Population: 19–44 |
BTS sample | Food eaten outside of binges episodes associated with low iron, calcium and zinc, and overall energy intake. Overcompensation for this during binge episodes |
| Gendall [100] | BN (BTS), MD (Christchurch Outcome of Depression study) | Comparison of visceral protein and haematological status between BN and depression controls | SCID, HDRS, structured interview of recent BN symptomatology Bloodwork (visceral protein and haematological status) |
152 (BN) 68 (MD) |
F |
BN: 17–45 MD: 18–46 |
BTS and MD samples | BN and MD groups did not differ on visceral protein or haematological measures. Low prealbumin and albumin levels were associated with more frequent vomiting. High frequency of vomiting and alcohol abuse/dependence, may increase the risk of subclinical malnutrition |
| Gendall [101] | BN (BTS) | Factors association with BMI and weight change in BN, before, during, and after CBT treatment | HDRS, GAFS, EDI, physical measurements | 94 | F | 17–45 | BTS Sample | CBT is not usually accompanied by substantial weight gain |
| Gendall [102] | BN (BTS) | Menstrual cycle and associated factors in BN patients. How this changed across and after CBT treatment | Blood sampling, self-reported food/drink intake, BMI, SCID, GAFS, HDRS | 82 | F | 17–45 | BTS sample | Association between menstrual irregularity and indices of nutritional restriction, not reflected by energy intake or body weight |
| Gendall [103] | BN (BTS) | Blood lipid and glucose changes during and after CBT for BN (BTS) | Blood tests, BMI, SCID, HDRS | 135 | F | 17–45 | BTS sample | At 3-year follow up, plasma HDL-cholesterol increased and total cholesterol decreased significantly in the group as a whole |
| Gendall [104] | BN (BTS) | Thyroid hormone levels in women before and after CBT for BN | SCI for DSM-III-R, HDRS, BMI, blood samples (serum T4 and free T4) | 107 | F | 17–45 | BTS sample | Lower pre-treatment T4 associated with persisting ED at follow up |
| Gendall [105] | BN (BTS) | Childhood gastrointestinal (GI) issues and BN psychopathology | SCID, structured interview questions about childhood GI complaints | 135 | F | 17–45 | BTS sample | Individuals with childhood GI complaints and other risk factors for BN may be at greater risk of developing a more severe eating disorder at an earlier age |
| Gendall [106] | AN (ATS) | Factors associated with amenorrhea in AN | SCID (DSM-IV), HDRS, TCI, additional questions on eating/weight/treatment/menstrual status, food diary, physical measurements | 39 | F | 23.3 ± 6.2 | ATS sample | The use of exercise to control weight, low novelty seeking scores, and low systolic blood pressure were predictors of amenorrhea independent of body mass index |
| Jenkins [107]* | AN (ATS) | Whether motivation to recover is related to treatment outcome in those with anorexia nervosa | SCID for DSM-IV, Global AN status, motivation measures, including Motivational Interviewing Skills Code Version 2.0 Outcome Rating Scale | 53 | F | 18–45 | ATS sample | Higher levels of positive change talk (and lower levels of negative) did not associate with better treatment outcome. No significant difference in treatment outcome observed between participants with different positive/negative change talk ratios |
| Jordan [108] | AN (ATS) | Comparing history of anxiety and substance use disorders in those with AN and MDD | SCID for DSM-III-R |
90 (40 AN; 58 MDD) |
F | 18–40 |
AN: 98% European MDD: 93% European |
OCD elevated in AN compared to MDD sample |
| Jordan [109] |
AN (ATS) BN (BTS) |
Comparing lifetime comorbidities in participants with AN, BN, and major depressive disorder | SCID-P, SCID II, HDRS, GAF | 56 (AN), 132 (BN), 100 (MD) | F | 17–40 | AN: 96% European, BN 91% European, MD 94% European | AN had higher OCD, AN-BP and BN elevated Cluster B personality disorders; all samples elevated Cluster C personality disorders |
| Jordan [110] | AN (ATS) | Assessing the constructs measured by YBC-EDS | YBC-EDS, BMI, HDRS, EDE-12, EDI-2 | 56 | F | 17–40 | 100% European (96% NZ European, 4% European born outside NZ) | Measured severity, YBCEDS sensitive to change following treatment |
| Jordan [111] | AN (ATS) | Clinical characteristics of participants who prematurely terminate treatment | SCID, SCID II, TCI-293, GAF, HDRS, EDE-12, EDI-2 | 56 | F | 17–40 | Predominantly European | Lower self-transcendence scores associated with premature treatment termination |
| Jordan [112] | BN (BEP) | Comparing symptoms and comorbidities across BN-P, BN-NP, and BED groups | SCID for DSM-IV, MADRS, GAF, EDE, EDI-2 | 112 | F | > 16 | BEP sample | BN-NP sits between BN and BED but some distinct features |
| Jordan [113] | AN (ATS) | Process and other factors associated with treatment non-completion in AN | Treatment Credibility Scale, TCI, VTAS-R, VPPS, therapy alliance ratings | 56 | F | 17–40 | ATS sample | Predicted by treatment credibility, lower self-transcendence, and lower early therapy alliance |
| Lacey [114] | BN, AN, OSFED, EDNOS (PRIMHD) | Comparing clinical characteristics and health service use for EDs by Māori and non-Māori |
National health database PRIMHD data |
3,835 | F | 10+ | 7% Māori | Māori were under-represented in treatment services. Once in treatment, duration was comparable. Māori more likely to be treated for BED or EDNOS |
| McIntosh [115] | AN (ATS) | Relevance of BMI cut off in diagnosing AN | SCID for DSM-IV, EDE, HDRS, GAF, EDI-2, BIAQ, TFEQ, EAT, SCL-90, anthropometric and medical measures | 56 | F | 17–40 | ATS Sample | Little difference between strict versus lenient BMI groups |
| McIntosh [116] | AN (ATS) | Therapist adherence to three different psychotherapies in ATS RCT | CSPRS-AN |
56 (AN) 3 therapists |
FF therapists | AN: 17–40, not stated for therapists | ATS sample | Good adherence to therapy types, blind raters clearly distinguished therapies |
| McIntosh [117] | AN (ATS) | Assessing distinctiveness of three therapies and change over therapy in RCT for AN | CSPRS-AN (blind raters) | 53 | F | M 23.1 | ATS sample | Therapies distinguishable, subscale measures higher for corresponding therapies, both SSCM and CBT sessions rated significantly higher in the middle stage of therapy |
| Rowe [118] | BN (BTS) | Whether poorer treatment outcome for those with comorbid borderline personality disorder (BPD) and BN compared to other personality disorders (PD) or no personality disorder | SCID-I and II for DSM-III-R, CBSI, HDRS, GAF, EDI, TCI, EDI | 135 | F | 17–45 | 91% NZ European | Those with BN and BPD more impaired at pre-treatment for BN and comorbid BPD, but treatment outcome over 3 years of follow up was not poorer for this group |
| Rowe [119] | BN (BTS) | Impact of Avoidant personality disorder on BN treatment outcome over 3 years | SCID-I, SCID-II, CBSI, HDRS, GAF, self-report questionnaires including EDI | 134 | F | 17–45 | BTS sample | No impact on eating disorder symptoms, but worse depressive and psychosocial functioning at pre and post treatment |
| Rowe [120] | BN (BTS) | PD severity/number of PDs as a predictor of BN treatment outcome | SCID (DSM-III-R), CBSI, HDRS, GAF, EDI | 134 | F | 17–45 | BTS sample | More PDs did not impact outcome at 3 years |
| Rowe [121] | BN (BTS) | Personality dimensions as predictors of 5-year outcomes among BN women | SCID-I, SCID-II, GAF, EDI-2, TCI, personality reassessment, 12-month ED behaviours and mood disorders | 134 | F | 17–45 | BTS sample | No single personality measure predicted 5-year outcome, and so comprehensive personality assessment is desirable |
| Sullivan [122] | BN, AN (BTS) | Differences between those with BN with/without AN history | SCID, HDRS, GAFS, EDI-2, TCI, Defence Style Questionnaire | 114 | F | 17–45 | BTS sample | Some differences between those with and without prior AN, but not distinct groups |
| Sullivan [123] | BN, MD (BTS) | Comparing total serum cholesterol in women with BN versus depression versus population norms | SCID, HDRS, GAFS, structured interview to assess last 14 days ED behaviour, blood samples | 126 (AN), 57 (MD) | F | 17–45 | BTS sample | BN women had markedly higher total cholesterol than depressed women, and population norms |
| Surgenor [124] | AN (ATS) | Association between sense of control and variability of AN | SCID-P (DSM-III-R (with psychotic screen), EDI, Shapiro Control Inventory, additional information on ED history including anthropometric measures, menstrual status, and chronicity | 51 | F | M 23.4 (SD 6.4) | ATS sample | Adverse overall sense of control (along with reliance on specific means of gaining control) associated with more severe eating disturbance. Greater use of a negative-assertive style of gaining control associated with a longer time since first diagnosis, desire for control significantly associated with menstrual status |
| Talwar [125]* | Community sample | Correlates of disordered eating behaviours in a community sample of women | EDI-2, Rosenberg Self-Esteem Scale, BMI | 60 | F | 16–55 | 70.8% NZ European, 6.3% Māori | Dysfunctional eating attitudes and behaviours associated with higher perfectionism, lower self-esteem, and elevated body mass. Increased body dissatisfaction significantly predicted BN symptoms |
NC non-clinical, RCT randomised-controlled trial, MD major depression, TCI Temperament and Character Inventory, HDRS Hamilton Depression Rating Scale, B-ERP Binge—exposure to response prevention to binges, P-ERP Purge—exposure with response prevention to purging, SCID Structured Clinical Interview for DSM, GAF Global Assessment of Functioning, EDI Eating Disorder Inventory, BIS Behavioural Inhibition System, BCDS Bulimia Cognitive Distortions Scale, BMI body mass index, SAM Situational Appetite Measure, CSPRS-BE Collaborative Study Psychotherapy Rating Scale—Binge Eating, YBC-EDS Yale Brown Cornell Eating Disorders Scale, EDE Eating Disorders Examination, MADRS Montgomery and Asperg Depression Rating Scale, VTAS-R Revised Vanderbilt Therapeutic Alliance Scale, VPPS Vanderbilt Psychotherapy Process Scale, PRIMHD Programme for the Integration of Mental Health Data, BIAQ Body Image Avoidance Questionnaire, TFEQ Three Factor Eating Questionnaire, EAT Eating Attitudes Test, SCL Symptom Checklist, CSPRS-AN Collaborative Study Psychotherapy Rating Scale—Anorexia Nervosa, CBSI Comprehensive Bulimia Severity Index, SCID-P structured clinical interview for DSM with psychotic screen
*Identifies that the record is a thesis
Table 3.
Non-treatment experimental interventions
| References | Population focus | Focus | Key data collected | Sample n | Gender | Age | Ethnicity | Summary findings |
|---|---|---|---|---|---|---|---|---|
| Boyce [126] | NC | Whether media body ideal exposure alters mood and weight satisfaction among restrained eaters, and whether changes in either direction encourage intake of food | RS-CD, DIS, BMI, single-item weight satisfaction scale (10-point), single item hunger scale (7-point), computer task to assess implicit mood, food intake | 107 | F | 18–37 | 66% NZ European, 8% Chinese, 4% NZ European/Māori, 1% Māori, 21% other ethnicities | For restrained eaters, exposure to media images was associated with decreases in self-reported weight satisfaction and negative mood, but did not alter food intake |
| Boyce [127] | NC | Impact of advertent or inadvertent exposure to media or control images (four conditions) and subsequent weight satisfaction and eating among restrained eaters | RS-CD, DIS, single item weight satisfaction scale (10-point), visual analogue scale of hunger, food intake | 174 | F | M 20.43 (SD 6.29) | 79% NZ European, 5% Chinese, 5% NZ European/Māori, 2% Indian, 9% other ethnicities | Advertent (but not inadvertent) exposure to body ideal images triggered eating by restrained eaters. Neither media exposure condition impacted their weight satisfaction |
| Bulik [24] | BN, NC | Whether alcohol consumption differed between food deprivation and no food deprivation conditions | Behavioural | 5 | F | M 25.6 ± 5.6 | Not stated | More alcohol consumed in non-deprived condition |
| Bulik [128] | BN | Examining the reinforcing value of cigarettes and food after food deprivation in female smokers with and without BN | Behavioural | 10 (4 BN) | F | 18–33 | Not stated | Increase in reinforcing value of food, and time spent working for cigarettes after deprivation in control but not BN women |
| Bulik [129] | BN, NC | Effect of coffee in BN and controls during food deprivation and no deprivation | Likert scale ratings, game responses to earn coffee | 10 | F | BN: 32.0 ± 6.1, NC: 21.7 ± 3.8 | Not stated | Those with BN consumed more coffee in deprivation condition versus control group |
| Bulik [130] | BN (BTS) | Salivation at presentation of food in BN sample, restrained eaters, and unrestrained eaters | SCID for DSM-III-R | 57 (19 BN) | F | BN: 27·7 ± 5·8 | Part of BTS sample | BN woman displayed significantly lower salivary reactivity than restrained or unrestrained eaters |
| Carter [131] | BN | Examining cue reactivity methodology | SCID, self-report on urge to binge/purge, assessor evaluated urge to restrict, heart rate, blood pressure |
7 (BN) 13 (Control) |
F | BN: M 26, NCM 28 | Not stated | Recommendations for cue reactivity assessment procedure are given, emphasising standardisation of measures, and participant-specific cues |
| Carter [132] | BN | Evaluated body image assessment and cue reactivity in women with BN in response to a range of cues | Silhouette method for assessing body image, BDI, EDI, self-report |
7 (BN) 8 (NC) |
F | 18–40 | Not stated | BN women rated bodies as larger, and had lower body image satisfaction versus NC women. Body satisfaction ratings were not affected by cue presentation. High-risk food cues were sufficient to elicit urges to binge in BN women |
| Carter [133] | BN | Information processing speed and cue reactivity in BN woman in response to cues | Stroop colour-naming tasks, BDI, DRS, EDI, Self-report measures on low mood, urge to eat/binge, confidence to resist this | 13 (6 BN) | F | 18–40 | Not stated | Specific cue types, as well as the way they were presented affected speed of information processing suggesting a more complex relationship than was anticipated |
| Gendall [134] | Cravers | Effect of meal macronutrient composition on subsequent behaviour and mood | Appetite and mood ratings (60 mm VAS) pre and post-test meals | 9 | F | 38–46 | Not stated | Consumption of protein-rich meals increases susceptibility to craving sweet-tasting foods in vulnerable women |
| Gendall [135] | Cravers | Meal induced change in tryptophan in relation to craving and binge eating | Blood sample assays | 9 | F | 34.9–50.4 | Not stated | Reduced plasma tryp:LNAA ratio (induced via high protein meal) reduced urge to binge |
| Hickford [136] | NC | Comparing restrained and unrestrained eaters' cognitions | BDI, Restraint scale (short), SCID for ED modules of DSM-III-R | 10 | F | 18–40 | Not stated | No difference in frequency of food cognitions between groups |
| Latner [137] | BED, BN | Comparing food intake between those ingesting high-carbohydrate or high-protein supplements | EDE, BDI-II, PRIME-MD | 18 | F | 34.78 ± 9.80 | Not stated | Protein supplement led to less binge-eating |
| Latner [138] | BED, NC | Whether energy density of meals affects intake in BED and NC | Behavioural data, EDE, EAT, DASS, BMI |
30 (15 BED, 15 NC) |
F | M 27.0 (SD 8.25) | 63.3% European, 10% Māori, 6.7% Pasifika, 6.7% Asian, 6.7% Indian, 6.7% other | Energy intake significantly lower in the low-ED condition than high-ED condition. BED participants report lower satiation. Decreasing energy density of food consumed may help satiation disturbances |
| Latner [139]* | BED, NC | Effects of two different food volumes (same total calories) on subsequent appetite and intake | Ratings (VAS, 5-point scale) for appetite and eating, food diary, food intake | 30 (15 BED, 15 NC) | F | M 27.07 (SD 8.24) | Not stated | Decreases in hunger, desire to eat, and loss of control were observed following higher volume food preloads. BED participants displayed greater desire and excitement to eat than controls |
| Stock [140] | NC | Body image relationship with body functionality versus body control | Big Five Inventory, Iowa-Netherlands Comparison Scale (INCOM), VAS for body image measures, self-objectification questionnaire (SOQ), RSES, food choice questionnaire, VAS for mood | 131 | F | 18–35 | Not stated | No increase in body satisfaction, but and lower self-objectification over time in body functionality group. Higher neuroticism associated with lower body satisfaction. Body image group participants reported lower self-esteem |
| Walsh [141]* | BN, NC | Examining neuroendocrine and neuropsychological functioning in individuals with eating disorders | BDI, EAT, blood testing, subjective ratings of physical symptoms | Study 1: 15 (NC), Study 2: 12 (NC), Study 3: 20 (12 NC, 8 recovered BN) | F | 19–37 | Not stated | Trytophan-free amino acid drink administration did not impact mood or food intake. Moderate dieting associated with alterations in brain serotonin function in women |
NC non-clinical, RS-CD Restraint Scale—Concern for dieting subscale, DIS Dietary Intent Scale, BMI body mass index, SCID Structured Clinical Interview for DSM, DRS Disability Rating Scale, EDI Eating Disorder Inventory, VAS Visual Analogue Scale, BDI Beck Depression Inventory, EDE Eating Disorder Examination, EAT Eating Attitudes Test, DASS Depression Anxiety and Stress Scale, SOQ Self-Objectification Questionnaire, RSES Rosenberg Self Esteem Scale
*Identifies that the record is a thesis
Table 4.
Cross-sectional research
| References | Population focus | Focus | Data collected | Sample n | Gender | Age | Ethnicity | Summary findings |
|---|---|---|---|---|---|---|---|---|
| Baxter [142] | BN, AN (TRH) | Mental health conditions among Māori participants in Te Rau Hinengaro | CIDI for DSM-IV | 2595 |
60% F 40% M |
16+ | 100% Māori (only Māori participants from TRH) | ED lifetime prevalence of 0.7% AN and 2.4% BN |
| Bensley [143]* | NC (OSSLS2) | Body image among adolescents and association with different lifestyle behaviours | Otago Students Secondary School Lifestyle Survey (OSSLS2): Subscales from the Food, Feelings, Behaviours, and Body Image Questionnaire (FFBBQ), BMI, DQI | 681 |
56% F 44% M |
15–18 | 74% NZ European, 9% Māori, 1% Pasifika, 7% Asian, 8% other | Females had higher scores on all subscales (figure dissatisfaction, fear of weight gain, dietary restraint, and concern about eating and weight), as did those who were overweight and obese. High levels of body dissatisfaction not limited to those who were overweight and obese) |
| Blackmore [144]* | NC | Explored self-induced vomiting after drinking alcohol in relation to eating disorder pathology among university students | EAT-26, MAST, Drinking Habits Questionnaire, BULIT-R, CES-D, AUDIT | 261 |
59% F 38% M |
17–35 | Predominantly European | For females, alcohol-related self-induced vomiting was associated with eating disorder pathology |
| Boyes [145] | NC | Healthy and unhealthy dieting behaviours in university couples | Perceived Relationship Quality Components Scale, RSES, BDI-II, WCBS, additional Likert scales | 114 |
50% F 50% M |
15–57 | Predominantly European | More body satisfaction among F with higher SE and lower depressive symptoms. More depressive symptoms and relationship dissatisfaction for men associated with more dieting and BD in F partners. M dieted more when F partners higher SE and fewer depressive symptoms |
| Brewis [146] | NC | Body image in Samoan participants living in Samoa and New Zealand | BMI, custom questionnaires | 226 |
55% F 45% M |
25–55 | 100% Samoan | Body dissatisfaction and slim ideals common, weight loss attempts and body perceptions not different between those above versus below BMI of 27 |
| Bushnell (1990) [147] | Population sample (CPES) | Bulimia prevalence in Christchurch population sample, oversampled for younger women | Diagnostic Interview Schedule | 1498 |
66% F 34% M |
18–64 | 93% European | Widespread disordered eating behaviours/attitudes, cohort effect for younger women |
| Chan [148] | NC | Relationship between perfectionism and ED symptoms in Chinese immigrants, and the role of ethnic identity | EDI, PANAS, MEIM, MCSDS | 301 |
59% F 41% M |
M 22.37 | 100% reported Chinese ancestry | Relationship between ED symptomatology and perfectionism mediated by cultural identity. Strong sense of belonging and attachment to Chinese culture appears to be protective |
| Dameh [149]* | AN | Evaluating insight, as well as factors that may affect this, in participants meeting DSM-IV criteria for anorexia nervosa | Markova and Berrios Insight Scale (MBIS), SAI, EAT-26 | 18 | F | 17–43 | Not stated | Impaired insight in those with AN was associated with features of illness, ED/behaviours and history of abuse |
| Durso [150] | NC | Testing weight bias scale and associations between self-directed weight bias and other factors | Weight Bias Internalisation Scale | 198 (1 NZ participant) | Not specified for NZ | Not stated for NZ | Not stated for NZ | Scale had good internal consistency and linked to other factors related to body image and ED |
| Fear [151] | NC | Self-reported disordered eating/attitudes in female secondary school students | BMI, EDE-2, BMI | 363 | F |
M 14.9 (SD 0.4) |
77% European, 16% Māori, 3% Samoan, 4% other | Most students wished to be smaller size, high prevalence of ED behaviours |
| Foliaki [152] | Population sample | Prevalence of psychiatric disorders among Pasifika in New Zealand | CIDI | 2374 | 52% F, 48% M | 16 + | 100% Pasifika | 12-month prevalence 1.5%; lifetime ED prevalence 4.4% |
| Gendall [153] | NC | Exploring food cravings in young women within the community | DIGS, custom food craving questionnaire | 101 | F | 18–45 | 98% European | History of cravings common (58%) within this sample. Narrowing definition meant that fewer (28%) met criteria. Multiple core features more common for those with strong cravings |
| Gendall [154] | NC | Characteristics of individuals who reported cravings for food | DIGS, TCI, EDI | 101 | F | 23–46 | Not stated | Food cravings associated with alcohol abuse/dependence and also novelty seeking, high rates of ED symptoms |
| Gendall [155] | AN | Food cravings and intensity of craving in those with past history of AN and NC | DIGS, TFEQ, TCI | 101 | F | 35 ± 6 | Not stated | Greater proportion of those with previous AN reported strong and more intense cravings |
| Gendall [156] | NC | Can aspects of restrained eating be predicted using the Temperament and Character Inventory (TCI) | DIGS, TCI, TFEQ | 101 | F | 18–45 | Not stated | Low self-directedness related to higher TFEQ score, disinhibition, and hunger susceptibility. High self-transcendence related to higher TFEQ score and cognitive restraint |
| Gendall [157] | NC | Comparing those who crave food and binge eat versus those who crave and do not subsequently binge | Food | 223 | F | 18–46 | Not stated | Cravers who binged tended to have higher BMI, higher frequency of diagnosed BN, elevated dietary restraint, and lower self-directedness |
| Gibson [42] | NC | Body image scores for rugby union players | Body composition, custom version of Low Energy Availability Amongst New Zealand Athletes, EDI-3 | 26 | M | 19–28 | Not stated | High prevalence of disordered eating behaviours, disturbances in body image |
| Griffiths [28] | NC | Anabolic androgenic steroid use/contemplation and associations with factors including body dissatisfaction and ED symptoms in sexual minority men | Online survey: Self-report weight/height, sexuality, anabolic steroid use/consideration, MBAS-R, EDE-QS, BBQ |
1797 from Aus 514 from NZ |
99.1% M, 0.4% other (same sample in refs 24–26) |
18–78 years | Reported as Aus NZ and Non-Aus NZ | ED symptoms and dissatisfaction with muscularity and height more prevalent among those who use AAS, while dissatisfaction with body fat less common in this group |
| Griffiths [27] | NC (Griffiths et al. [28]sample) | Pornography use and body image, associated behaviours, and quality of life in sexual minority men | Online survey: self-reported weight and height, sexuality, MBAS-R, EDE-QS |
1797 from Aus 514 from NZ |
99.1% M, 0.4% other | 18–78 | Not stated for NZ | Increased pornography use was weakly associated with more body dissatisfaction and thoughts of anabolic steroids use |
| Griffiths [29] | NC (Griffiths et al. (2017) sample) [28] | Social media use and body image, ED symptoms, and steroid use contemplation in sexual minority men | Online survey: self-reported social media/dating use, height/weight, sexuality, use/thoughts of anabolic steroids, MBAS-R, EDE-QS |
1797 from Aus 514 from NZ |
99.1% M, 0.4% other | 18–78 | Not stated for NZ | Social media use positively associated with body dissatisfaction, ED symptoms, and thoughts of anabolic steroid use. Some associations strongest for image-centric platforms |
| Hechler [158] | Clinicians | Assess clinicians understanding of role of physical activity in AN—and describe assessment and management strategies | EDSCS (Eating disorder specialist/clinician survey) | 33 | Not stated | Not stated | Reported as Aus/NZ | The majority of specialists consider physical activity to be important in EDs, however those from an Asian background considered it to be minor in comparison to other nationalities |
| Hickman [159]* | BN, NC | Looking at relationships and associated attachments in those with and without BN, within a sample of university students | EDI, Close Relationship Scale, TFEQ, Relationship Satisfaction Scale | 123 (unclear how many with BN symptoms) | F | 18–40 | Not stated | More anxious attachment and dieting in participants with bulimia |
| Hudson [160]* | NC | Body dissatisfaction, BMI, esteem, eating attitudes | EDE, BSQ, RSES, BMI | 36 | F | 17–55 |
67% NZ European, 8% Māori, 25% Other |
Elevated BMI linked to higher body dissatisfaction |
| Jenkins [161]* | NC | Eating disorder symptomatology among females in NZ of Chinese and other ethnicities | EAT-40, Eating Disorder Belief Questionnaire, additional custom questions, Perceived Sociocultural Pressure Scale, SEED, ratings of body image figures | 116 | F | 18–47 | 34% Chinese, 5% Taiwan, 49% NZ European, 8% NZ Māori, 1% Pasifika, 3% Other Ethnicities | More body image dissatisfaction and fear of weight gain in Chinese group. Similar pressure to be thin between groups |
| Jospe [162] | NC (SWIFT) | Whether association between weight/diet monitoring influenced eating disorder symptoms | EDE-Q, self-reports of ED behaviours | 250 | 62% F, 68% M | < 18 | 176 European, 18 Māori, 7 Pasifika, 5 Asian | Self-monitoring did not increase ED symptoms |
| Kessler [1] | TRH (BED data not previously reported) | Assessing prevalence and correlates of binge eating disorder | Composite International Diagnostic Interview | 24124 (7312 NZ) | Not specified for NZ | > 18 | Not stated | Lifetime prevalence estimates of BED are higher than BN, fewer than half of lifetime BN or BED cases receive treatment |
| Kessler [26] | BED, BN (TRH) | Compared impairment and role attainment (e.g. employment) between BED and BN | CIDI, WHO-DAS | 7312 from NZ (not included in occupation and earnings assessment) | Not specified for NZ | 18–98 | Not stated | Effects on role attainments similar for BN and BED. F less likely to be currently married, M less likely to be currently employed. Both more higher odds of work disability and more days of work impairment |
| Kokaua [163]* | BN, AN | Includes prediction of eating disorder prevalence among Cook Islanders in New Zealand | NZMHS, MHINZ | How to report? | How to report? | 16+ | Cook Island | Any eating disorder 1.4% 12 months prevalence (unadjusted) or 1.1% adjusted. Ethnic differences in eating disorders even after adjustment |
| Latner [164] | BED, BN, AN | Comparing quality of life ratings in those with subjective versus objective binge eating | EDE-Q, SF-36, BDI-II | 53 | F | M 26.30 (SD 8.98) | 94% European, 2% Asian, 2% Māori, 2% Pasifika | Impaired quality of life for subjective binge episodes and compensatory behaviours. Also accounted for 27% of physical QoL variance |
| Latner [165] | NC | Associations between body checking/avoidance, quality of life (QoL) and disordered eating | BCQ, BIAQ, BMI, SF-36, EDE-Q, BDI-II | 214 | F |
M 26.3 (SD 8.98) |
86% European, 8% Asian, 52% Māori | Both body checking and avoidance associated with lower QoL and higher ED symptoms |
| Latner [166] | BED, BN, AN, EDNOS | QoL impairment due to features of EDs (e.g. eating concern, restraint, vomiting, excessive weight concerns) | EDE-Q, The Medical Outcomes Short-form Health Survey (SF-36), BDI-II |
53 ED 212 NC |
F | 17–65 | 88% European, 7% Asian, 5% Māori | More EDE-Q features, particularly shape/weight concerns, were predictive of poorer QoL |
| Lau [167]* | NC (SuNDiAL) | Desire to lose weight and methods of losing weight, including unhealthy weight loss methods, among adolescents | Weight attitudes and motivations for food choice questionnaire, custom questions about body image and weight loss intentions and methods | 370 | 66% F, 34%M | 15–18 | 72% European, 14% Māori, 13% Asian, 2% Pasifika | High prevalence of weight loss intentions. Weight loss methods more common in females |
| Leydon [168] | NC | Eating habits among jockeys | EAT, food diaries, menstrual status, DEXA scan, body composition, anthropometry | 20 |
70% F 30% M |
Not stated | Not stated | Osteopenia and weight control efforts common among sample of jockeys |
| Linardon [169] | NC, BED, BN | Participant views of digital interventions for treatment and prevention of eating disorders | Custom questionnaires | 722 (133 from Aus/NZ) |
95% F 5% M |
M 30.25 (SD 8.29) | 77.1% European, 0.4%% African American, 8.6% Hispanic, 10.4% Asian, 0.6% Pasifika Island, 2.9% other | Pros and cons identified, cons included concerns about privacy and accuracy of data |
| Lucassen [170] | NC (YHS) | Comparing body size, weight, nutrition, and activities in sexual and gender minorities (SGM to controls | Custom survey re weight control behaviours, BMI | 7769 |
56% F (incl. 312 S/GM females) 45% M (incl. 150 S/GM males) |
13–18 | 49% European, 20% Māori, 13% Pasifika, 12% Asian, 6% other | More issues with nutrition, unhealthy weight control, and inactivity among sexual and gender minorities |
| Madden [7] | NC | Association between intuitive eating and BMI, and eating behaviours among less intuitive eaters | Intuitive Eating Scale, BMI (self-reported weight/height), Rapid Assessment of Physical Activity, additional selected questions of menopausal status, binge-eating, food intake, and rate of eating | 2500 | F | 40–50 | 83% European, 11.4% Māori, 3.0% Pasifika, 85% Asian | Intuitive eating inversely associated with BMI. Partial mediation by binge-eating |
| Maguire [171] | AN | Ability to predict length of inpatient treatment Australasian clinical data | Clinical data | 154 | 98% F |
M 21.2 (SD 7.2) |
Not stated | Difficulty in predicting length of stay, with only two factors (length of stay, 2–3 previous admissions) independently contributing to this |
| McCabe [172] | NC | Three studies comparing body image of those within five different countries and cultures (Fijian, Indo-Fijian, Tongans living Tonga, New Zealand Tongan, European Australians) | Interviews and questionnaires about eating behaviours and physical activity, perceptual distortion task | Study 1: 240; Study 2: 3000; Study 3: 300 | 50% F, 50% M | 12–18 |
Study 1: 48 from each cultural group, Study 2: 600 from each cultural group, Study 3:100 from each Fijian cultural group and European Australians |
Body image, eating, and physical activity influenced by socio-cultural environment |
| McCabe [173] | NC (Pacific OPIC Project) | Environmental influences on body change strategies within different cultural groups | Body Image and Body Change Questionnaire | 4904 (461 NZ) | 48% F, 52% M (NZ 62% F, 38% M) | 12–18 | Tongan | Differing messages across and within cultural groups |
| Miller [174] | NC | Body perception in relation to media consumption and societal ideals | The Sociocultural Attitudes Towards Appearance Questionnaire, FRS, Media Time Use, INCOM | 181 |
66% F 34% M |
17–30 | 84% European, 7% Māori, 3% Asian, 2% other | Greater discrepancy between ideal and perceived current body figures for women. Greater thin ideal internalisation for women. Awareness and internalisation of thinness norms predicted body perceptions for women but not men |
| Moss [175]* | AN, EDNOS | Body dissatisfaction and associated factors in adolescents with eating disorders | EDI-3, CAPS, PSPS, DASS-21 |
40 (13 AN, 7 EDNOS) 20 NC |
F | M 15.75 (SD 1.52) |
ED: 80% European 10% Māori, 10% other CT: 90% European, 10% Māori, 0% other |
Higher maladaptive perfectionism and anxiety linked to BD, but didn’t interact as predictors of BD in ED group |
| Muir [176]* | AN, NC | Whether women with AN differed from low weight women without AN in recognising emotions | Performance on facial emotion recognition test (reaction speed and accuracy) | 33 | F | 18–55 | AN: 41.7% NZE, 8% Maori, 4 “other”. NC: 90.5% NZE, 2 British, 1 Russian | Shorter response time for AN group, no difference in accuracy measures |
| Mulgrew [177] | NC | Weight control behaviours and associated factors in young people | BAQ, MBAS-R, PHQ, modified WCBS, BMI, weight management questions | 1082 |
75% F 25% M |
18–30 | 79% NZEO | More weight control behaviours among females. Feelings of fatness a key predictor of weight control |
| Ngamanu [178]* | NC | Compared levels of body image dissatisfaction and eating pathology in Māori and Pakeha women, also examining whether the ethnic attachment of participants was associated with the body image | BMI, MEIM, FRS, EAT-26 | 100 | F | 18–50 + | 34% Pakeha, 66% Māori | Body image dissatisfaction and eating pathology did not differ between groups. Level of ethnic attachment also did not impact body image satisfaction |
| Browne [179] | BN, AN (TRH) | Lifetime prevalence/risk of psychiatric disorders in the New Zealand population | Survey | 12, 992 |
57% F 43% M |
16+ | 20% Māori, 17% Pasifika, 63% Other (Part 1), 22% Māori, 18% Pasifika, 60% Other (long-form sample) |
Any ED 1.7%CI 1.5, 2.1) LT prevalence AN 0.6 (CI 0.4,0.8): BN 1.3 (1.1,1.5): Females: 2.9 (CI 2.3,3.5); Males 0.5 (CI 0.3, 0.9) |
| O'Brien [6] | NC | Body image and self-esteem in physical education (PE) university students | Demographic questionnaires, self-reported BMI, BES, EAT-26, global self-esteem scale from the SDQIII | 228 | F |
PE 18: 34 ± 0.64, Psychology 18: 46 ± 0.78, Year 3 PE 21:.0 ± 1.18, Year 3 Psychology20: 9 ± 1.06 |
Not stated | Year 3 PE students had lower self-esteem and more disordered eating |
| O'Brien [180] | NC | Psychosocial characteristics among those in a weight loss programme | Custom questions on reasons, MBSRQ, single item self-esteem scale | 106 |
86% F 14% M |
M 41.9 (SD 10.8) |
Not stated | Key reasons for wanting to lose weight were mood, appearance, and health. Poorer self-image/self-esteem for those citing mood reasons |
| Overton [181] | Clinical | Comparing emotional experience of women with EDs to NC controls | EDI-2, YSQ-SI, DES-IV | 130 (30 ED) | F |
Cases: M 28.1 NC M 23.8 |
Not stated | Use of disordered eating behaviours to manipulate both positive and negative emotional states, should be recognised as an important maintenance factor |
| Reynolds [182] | Clinicians | Whether health professionals felt orthorexia should be recognised as an eating disorder | Custom online survey and qualitative text boxes | 52 |
96% F 4% M |
41.2 ± 11.9 | Not stated | Most clinicians (71%) felt that orthorexia should be recognised as a distinct ED |
| Robertson [183]* | NC | Associations between body image, self-esteem, and peer and romantic relationships | Body Image and Body Change Questionnaire, Physical Attractiveness Scale, Body Image Behaviour Scale, Social Physique Anxiety Scale, Physical Appearance Comparison Scale, RSES, Self-Description Questionnaire III, Perceived Relationship Quality Components Scale | 91 | 80% F, 20% M | 17–69 | Not stated | Positive relationship between body-image and self-esteem, and between body image and quality of romantic relationships. Positive relationship between self-esteem and relationships (peer and romantic). Body image predicted self-esteem and quality of peer-relationships Self-esteem predicted romantic relationship quality |
| Rodino [184] | Clinicians | Fertility specialists' knowledge and practices relating to eating disorder | Adapted online questionnaire | 106 | 51% F, 49% M | 25 + | Not stated | Knowledge around relevant symptoms of eating disorders, but uncertainty around ED detection. Many not satisfied with training in this area, or not confident in ability to recognise symptoms. Large majority indicated need for further education/guidelines |
| Rosewall [185] | NC | Risk factors for body dissatisfaction in girls | NZSEI, EAT-26, Stunkard Body Figure Drawings, EDI, CAPS, RSES, Sociocultural Influences on Body Image and Body Change Questionnaire (Perceived Pressure to Lose Weight subscale), PANAS, POTS | 231 | F | 14–18 | 73.7% NZ European, 10.3% Māori, 5.6% Asian, 2.6% Pasifika and 3% Other | Risk factors for higher levels of body dissatisfaction were perfectionism, perceived media pressure, and low self-esteem |
| Rosewall [186] | NC | Exploring moderations of association between body dissatisfaction and disordered eating behaviours | NZSEI, ChEAT, Collins Body Figure Perceptions, EDI, CAPS, RSE, PANAS-C, Sociocultural Influences and Body Change Questionnaire, POTS (weight-based teasing subscale) | 169 | F | 10–12 | 84.0% NZ European, 11% Māori, 6% Asian, 2% Pasifika, 1% Other | Body dissatisfaction and disordered eating association were moderated by personal (e.g. perfectionism, self-esteem) and environmental factors (e.g. teasing, perceived media pressure) |
| Rosewall [187] | NC | Psychopathology factors related to links between BMI and body dissatisfaction, and between body dissatisfaction and disordered eating | BMI, BSQ, BIA, BES, EAT-26, PAI | 186 | F | 18–40 | 78.9% NZ European, 13.3% Asian/part Asian, 3.0% Māori, 1.2% Pasifika Island 3.6% other | Reporting lower BD (than would be predicted by BMI), and less disordered eating (than would be predicted by BD) was linked to lower levels of anxiety/depression and higher mood stability |
| Shephard [188]* | NC | Influence of family experiences related to food and self-compassion on the association between appearance ideals and body dissatisfaction | SATAQ (Revised—Female Version), BSQ, family Experiences Related to Food Questionnaire (FERFQ), self-compassion scale (SCS) | 106 | F | 18–48 | 85.8% NZ European, 4.6% NZ European and 'another ethnicity', 3.8% Chinese, 1.9% Māori, 3.8% another ethnicity | Family food related experiences and self-compassion appear to be protective, moderating relationship between body dissatisfaction and thin ideal internalisation |
| Slater [189]* | NC | Energy intake, activity, and disordered eating behaviours in recreational athletes | EDI-3, LEAFQ | 170 |
64% F 36% M |
18–56 | Not stated | Low energy availability (LEA) common but no risk of ED for most of those with LEA |
| Strang [190]* | Restrained eaters | Responses to Stroop test words about food, weight, and shape by restrained eaters versus unrestrained eaters | Stroop test, RS, STAI, BDI | 55 (21 restrained eaters) | Only F after initial phase | Restrained: 24.33 (9.80), unrestrained: 21.85 (5.64) | Not stated | No group differences, but may have been due to minimal symptomatology in restrained eating group versus comparison groups |
| Talwar [12] | NC | Body image and body dissatisfaction among Māori and non-Māori participants | Multigroup Ethnic Identity Measure, BIA-G, BES | 45 | F |
Māori: M 19.8 (SD 1.2), European: M 19.0 (SD 1.2) |
50% Māori 50% European |
Lower concern about weight among Māori. Stronger Māori ethnic identity was associated with lower weight concern |
| Utter [5] | NC | Identifying 'red flag' behaviours for unhealthy weight loss | Youth'07 survey | 9107 |
46% F 56% M |
13–18 | Māori, European, Pasifika, Asian (% not stated in this paper) | Meal skipping and fasting are 'red flag' behaviours associated with poor mental wellbeing |
| Vallance [191] | NC | ED symptoms and health related quality of life | SF-36, EDE-Q, EDI-2, BSQ, BCQ, BIAQ, BDI-II, BSI | 214 | F | 17–65 | 85% European, 7.5% Asian, 6.1% Māori | DE and BD linked to lower quality of life |
| Vaňousová [192] | NC | Evaluating validity of the Eating Concerns (EAT) scale from the MPPI-3 | MPPI-3 (specifically EAT scale), EPSI, EDE-Q, EDDS, BES, BI_AAQ | 396 |
79% F 21% M |
17–51 | 91% European, 12% Maori, 8% Chinese, 4% Indian, 2% Pasifika (some participants more than one) | Scores from new MPPI-3 EAT scale seem promising as a screening measure for eating pathology |
| Wells [20] | BN, AN (TRH) | Prevalence and severity of different disorders, including eating disorders, within NZ. Oversampled for Māori and Pasifika | CIDI | Short form: 12, 992, long form: 7435 | 57% F, 43% M | 16+ | 20% Māori, 17% Pasifika, 63% Other (Part 1), 22% Māori, 18% Pasifika, 60% Other (long-form sample) | Any eating disorder 1.7% lifetime prevalence, 0.5% 12-month prevalence |
| Wells [193] | BN, AN (TRH) | Severity and interference with life for mental health conditions among NZ sample | CIDI, Sheehan Disability Scale | Part 1: 12,992, part 2: 7435 | 57% F, 43% M | 16+ | 20% Māori, 17% Pasifika, 63% Other (Part 1), 22% Māori, 18% Pasifika, 60% Other (long-form sample) | Prevalence for EDs 0.5% in last 12 months |
NC non-clinical, CIDI Composite International Diagnostic Interview, BMI body mass index, DQI Diet Quality Index, EAT Eating Attitudes Test, MAST Michigan Alcohol Screening Test, CES-D Centre for Epidemiologic Studies Depression Scale, AUDIT Alcohol Use Disorders Identification Test, RSE Rosenberg Self-Esteem Scale, BDI Beck Depression Inventory, WCBS Weight Control Behaviours Scale, EDI Eating Disorder Inventory, PANAS-C Positive and Negative Affect Scale for Children, MEIM Multigroup Ethnic Identity Measure, MCSDS Marlowe-Crowne Social Desirability Scale, SAI Spontaneity Assessment Inventory, WBIS Weight Bias Internalisation Scale, DIGS Diagnostic Interview for Genetic Studies, TCI Temperament and Character Inventory, TFEQ Three Factor Eating Questionnaire, LEANZA Low Energy Availability Amongst New Zealand Athletes, MBAS-R Revised Male Body Attitudes Scale, EDE-QS Eating Disorder Examination Questionnaire Short, BBQ Brunnsviken Brief Quality of Life Scale, EDSCS Eating Disorder Specialist/Clinician Survey, SDQIII Self-Description Questionnaire III, BSQ Body Shape Questionnaire, SEED Short Evaluation of Eating Disorders, NZMHS World Health Organisation Disability Assessment Schedule, New Zealand Mental Health Survey, MHINZ Mental Health Information New Zealand, SF-36 36 Item Short-Form Survey, BIAQ Body Image Avoidance Questionnaire, BCQ Body Checking Questionnaire, EDE Eating Disorders Examination, FRS Figure Rating Scale, INCOM Iowa-Netherlands Comparison Scale, CAPS Clinician Administered PTSD Scale for DSM, PSPS Perceived Sociocultural Pressure Scale, DASS Depression Anxiety and Stress Scale, BAQ Body Attitudes Questionnaire, PHQ Patient Health Questionnaire, BES Binge Eating Scale, MBSRQ Multidimensional Body-Self Relations Questionnaire, YSQ-SI Young Schema Questionnaire—Social Isolation, DES Differential Emotions Scale, PANAS Positive and Negative Affect Scale, CAPS Clinician Administered PTSD Scale, POTS The Perception of Teasing Scale, NZSEI New Zealand Socioeconomic Index, ChEAT Children’s Version of the Eating Attitudes Test, EDI-BD Eating Disorders Inventory—Body Dissatisfaction scale, BIA Body Image Assessment, PAI Personality Assessment Inventory, LEAFQ Low Energy Availability Questionnaire, STAI State-Trait Anxiety Inventory, BIA-G Group Administered Version of the Body Image Assessment, MMPI Minnesota Multiphasic Personality Inventory, EPSI Eating Pathology Symptoms Inventory, EDDS The Eating Disorder Diagnostic Scale, BI_AAQ Body Image—Acceptance and Action Questionnaire
*Identifies that the record is a thesis
Table 5.
Studies using case-control methodologies
| References | Population focus | Focus | Key data collected | Sample n | Gender | Age | Ethnicity | Summary findings |
|---|---|---|---|---|---|---|---|---|
| Archer [194]* | BN, AN | Exploring factors associated with AN and BN and how these may underlie dysfunctional cognitions seen in these disorders | EDI-2, BDI, MPS, Setting Conditions for Anorexia Scale, TPQ Harm Avoidance, PBI, FES | 135 | F | 18–44 | CT: 100% European. Not stated for other groups | Dysfunctional perfectionism (e.g. MPS concern over mistakes, personal standards, and parental criticism, and TPQ harm avoidance) a key personality characteristic in AN and BN |
| Bulik [195] | BN | Linking perceptions of family of origin in those with BN, BN and comorbid SUD, and NC | Diagnostic Interview Schedule version III-A, Family Environment Scale self-report, Semi-structured Family Environment Interview Q-Sort | 63 (33 BN) | F | Not stated | Not stated | BN with no substance use disorder: group mothers viewed as more neurotic. BN group fathers perceived as more seductive. Mother of BN with substance use disorder placed emphasis on weight/appearance/exercise |
| Bulik [196] | AN | Assessing predictors of BN in women with AN | Medical records, Diagnostic Interview for Genetic Studies (modified) | 69 | F | 23–72 | Not stated | Highest risk window for developing BN is within 2 years after onset of AN |
| Bulik [197] | AN | Examining fertility and reproductive history in women with AN versus NC group | Interviews about fertility and related history | 98(66 AN) | F | AN: M 32.4 (SD 8.0), NC: M 35.5 (SD 6.2) | Not stated | More miscarriages and caesareans in AN group |
| Bulik [198] | AN | Assessment of relevant factors (eating attitudes, parental bonding, personality) in those with a history of AN (full recovery, partial recovery, chronically ill) and NC | EDI, TFEQ, TCI, PBI, BMI | 168 (70 AN) | F | 23–45 | Above sample | Partially recovered and chronically ill groups reported more harm avoidance, and lower self-directedness and cooperativeness, compared with fully recovered and control groups. Lower parental care scores among chronically ill group |
| Fowler [199] | BED | Family factors and comorbid psychopathology in those with BED and CT with obesity | DIGS, FH-RDC, PBI, FES | 40 (20 BED, 20 CT) | F | M 38.8 (SD 9.8) | Not stated | BED associated with affective and anxiety disorders, and with family history of BED but not substance misuse. BED linked to “affectionless control” parenting style in the PBI, and numerous difficulties on the FES |
| Latner [200[] | BN | Association of psychopathology with objective and subjective bulimic episodes | EDE, TFEQ, EDI, DASS | 81 | F | M 28.11 |
81% European 10% Asian 7% NZ Māori 2% Pasifika |
Frequency of objective and subjective bulimic episodes correlated with general eating psychopathology measures, and with measures of depression, anxiety, and stress |
| Romans [201] | BN, AN | Experience of childhood sexual abuse (CSA) prior to developing ED | PSE, ICD-10, PBI, custom interview questions (CSA) | 477 | F | 18+ | Not stated | Higher rates of EDs among group who experienced CSA. ED risk factors among those with history of CSA were early paternal overcontrol and early puberty |
| Sullivan [84] | AN | Follow up of those with AN referred to eating disorders service within a 3-year period, an average of 12 years prior to the time of follow up | DIGS, GAF | 168 (70 AN) | F | AN M 32.4 (SD 7.8), comparison M 35.5 (SD 6.2) | AN: 98.6% European, comparison: 96.9% European | AN group persistence in low body weight, perfectionism, and cognitive restraint |
NC non-clinical, CT controls, EDI Eating Disorder Inventory, BDI Beck Depression Inventory, MPS Multidimensional Perfectionism Scale, TPQ Tridimensional Personality Questionnaire, PBI Parental Bonding Instrument, FES Family Environment Scale, FEI Family Environment Interview, DIGS Diagnostic Interview for Genetic Studies, SCID Structured Clinical Interview for DSM, TFEQ Three Factor Eating Questionnaire, TCI Temperament and Character Inventory, BMI body mass index, FH-RDC Family History—Research Diagnostic Criteria, DASS Depression Anxiety and Stress Scale, PSE Present State Examination, ICD International Classification of Diseases, GAF Global Assessment of Function
*Identifies that the record is a thesis
Table 6.
Qualitative and mixed-methods studies
| References | Population focus | Focus | Key data collected | Sample n | Gender | Age | Ethnicity | Summary findings |
|---|---|---|---|---|---|---|---|---|
| Allison [202]* | NC | Feminist approach exploring issues related to young women’s body perception and eating behaviours | Thematic analysis of journal entries | 15 | F | 14–16 | 10 European, 1 Samoan, 1 South American, 1 Irish-English, 1 Chinese-European-Eurasian, 1 not stated | Identified Western cultural influences on eating behaviours and body image |
| Barry [202]* | NC | Issues with eating, weight, and body image in women with type 1 diabetes and health professionals | Semi-structured interviews | 17 (12 with type 1 diabetes, 5 health professionals) | F | 16–25 | Not stated | Different perceptions of health professionals versus young women with Type 1 diabetes. Eating and weight related disturbance (including insulin omission) reported |
| Batenburg [203]* | AN | Experiences and opinions of those who had experienced and recovered from anorexia nervosa | Semi-structured interviews | 8 | F | 17–27 | 5 NZ European, 1 Māori/European, 1 Indian, 1 Belarusian | Model of AN aetiology developed, based on categories of perceived causes of relapse |
| Bellingham [204]* | AN | Parental perspective on experiences of having a child with AN | Semi-structured interviews | 12 | 50% M, 50% F | Not stated | Not stated | Identified three stages from parental accounts, termed the insidious, tenacious, and recovery stages |
| Carne [205]* | NC (OPIC Project) | Included examination participants' attitude toward own weight | PedsQL, AQoL, semi-structured interviews | Quantitative: 4429, qualitative: 36 (drawn from quantitative sample) | Quantitative: 48% F, 52% M, qualitative: 50% M, 50% F | 13–18 |
Quantitative: 59% Pasifika, 20% Māori, 11% European, 10% Asian Qualitative: 33.3% Māori, 33.3% European, 33.3% Pasifika |
Lower physical QOL linked to higher weight status, high QOL for those who were obese (relative to previous findings), sociocultural factors protective against internalised stigma, friendships related to perception of own weight |
| Chisholm [206]* | NC | Examined relationship between dieting and factors within romantic relationships in a sample of heterosexual couples | PRQC, AAQ, RSES, BDI-21, WCBS, EDI-2, WMSI, weight-loss support helpfulness, BMI, body satisfaction (Likert scale) | 88 | 50% F, 50% M | F: M 29.43, (SD 11.87), M: M 31.61 (SD 11.87) | Not stated | More disordered eating attitudes where lower perceived partner support. Higher levels of unhealthy dieting with lower self-esteem (mediated by disordered eating attitudes). Partner support appears protective for those with low self-esteem |
| Conder [207]* | NC | Explored body image and how this was constructed among women with intellectual disabilities | Semi-structured qualitative interviews | 25 | F | 21–65 | 88% NZE, 8% Māori, 4% Pasifika | Themes identified were 'beauty and the body', 'a fit and functional body' and 'a gendered body' |
| Easter [208]* | NC | Problematic behaviours among elite athletes. Includes topic of disordered eating | Semi-structured qualitative interviews | 10 | 50% F, 50% M | Early 20s to late 40s | 80% European/Pakeha, 10% Māori, 10% Other European | A number of behaviours reported, including disordered eating. Potential influences on this behaviour included comments/criticism from others, unrealistic sociocultural standards, and media influence |
| Gunn [209]* | BN, AN, EDNOS, self-diagnosed | Experiences of mothers who became pregnant after having recovered from an eating disorder | Qualitative interviews |
10 women with past ED, 8 without |
F | 27–46 | European | Reported healthy pregnancies among recovered women, no difficulties with infant feeding, no tendency for undue anxiety about weight gain |
| Hall [210] | AN | Family factors and their association with AN | Interviews with parents of those with AN | 50 (AN) | F | Not stated | European | Possible aetiological factors included socioeconomic status, and family factors such as a parental history of psychiatric and medical illness |
| Hammond [211]* | NC, ED | Examined body image appraisals, self-esteem, body related esteem, weight locus of control, and figure ratings in groups of women: normal weight, overweight, had ED or were body builders. Qualitative study examined self-esteem and experience of teasing | RSES, BES, WLOCS, figure rating scale, silhouette rating scale, qualitative interviews | 122 | F | Normal weight: M 31.14 (SD 10.40), overweight: M 38.84 (SD 12.50), ED: M 27.48 (SD 10.23), body builders: M 28.81 (SD 6.31) | 89% European, 3% Maori, 4% Pasifika, 3% Other | Positive description for normal and muscular, but not thin or overweight body types. Difference between groups regarding ideal figures. Self-esteem and body esteem did not correlate for body builders. ED reported feeling bigger compared to what they thought. Similar ratings for figures seen as likely to be attractive for males |
| Jones [43]* | NC | Body image dissatisfaction in males involved in weight training, and potential influences and impacts on wellbeing | Semi-structured interviews | 12 | M | 18–29 | 83.33% NZ European, 8.33% NZE/Māori, 8.33% Cook Island/Māori/Tahitian/Scottish | Weight training exercise related to both positive and negative body image/evaluation, observed sociocultural influences on body image Behavioural indications that participants were downplaying impact of body image dissatisfaction |
| Kleinbichler [212]* | AN, NC | Elaborating on knowledge surrounding metacognitive processes in AN, compared with dieting and non-dieting women | BMI, DASS, EAT-26, PSWQ, PBRS, NBRS, RRQ, TCQ, MCQ-30, EDE-Q4 | 131 | F | Non-diet: M 21.38, diet: M 23.44 (SD 8.06), AN: M 24.0 (SD 6.00) | 70% NZ European, 3% Māori, 5% Chinese, 2% Indian, 11% other, 8% multi-ethnicity | Maladaptive cognitive styles among those with AN, compared with dieting and non-dieting women. Evidence supports presence of cognitive attentional syndrome in those with AN |
| McClintock [213]* | NC | Influences on body image dissatisfaction/disturbance, examined in three different ways | Focus group data | Study 1: 23, Study 2: 190, Study 3: 33 | F | 14–18 | Study 1: 73.9% Pakeha, 17.4% Māori, 8.7% other minority cultures. Study 2: 74% Pakeha, 14.5% Māori, 2, 3% Pasifika, 6.9% Asian, 1.2% South African, 1.2% other minority. Study 72.7% Pakeha, 15.2% Māori, 3% Pasifika | Identified important role of social evaluation for influencing body image and unhealthy dieting behaviour, and interrelationships between sociocultural and interpersonal influences |
| Poulter [214] | NC | Explore perspectives of female undergraduate students with positive body image | Body image questions, BAS, BESAA, SATAQ, focus group | n = 139 for screening. N = 19 for focus analysis | F | 18–30 | Predominantly European | Themes included body positivity with age, mindfully engaging with media content, functional conceptualisation of the body, and role of religious and cultural identities. Women with positive body image utilise a body-protective filter, favouring body-positive information from environment |
| Schofield [215]* | NC | Low energy availability and associated factors (e.g. body image, nutrition) in athletes | Qualitative data, physiological data, food record |
Study 1: 15, Study 2: 11 |
Study 1 67% F, 33% M, Study 2: 64% F, 36% M | 22.8 ± 3.8 | European | Highlighted complex nature of LEA, risk impacted by sociocultural environment and type of sport |
| Snell [216] | Clinicians | Investigating the nurse experience in an ED inpatient service | Interview | 7 | Not stated | 30–50 | Not stated | Nurses have crucial role in ED unit with unique challenges, and therapeutic relationship with these professionals can help engage clients in treatment/recovery. At times felt that this important role was invisible |
| Stiles [217]* | BN, AN | Assessing which eating behaviours were perceived as being normal by clinicians, dieticians, and healthy women | EDE-Q, ONE, eating behaviour, ratings of eating behaviours shown in video (Likert scales), eating style questions, qualitative interview | 67 | F | 18–60 | Not stated | Key theme was flexibility (e.g. not having strict rules). Themes also eating in response to physiological hunger, meeting nutritional needs, eating in socially acceptable manner, eating for pleasure, and regular eating) |
| Surgenor [218] | AN | Identify how patients view their AN with respect to self | Semi-structured interview | 5 | F | 17–late 20s | Not stated | Patient's 'selves' have strategically different implications for therapeutic interventions. Individual therapy could be improved by establishing an authentic basis |
| Surgenor [219] | AN | Can treatment drop-out for AN be predicted from routine admission data collection? | BDI, EAT-26, EDI-2, RSES | 213 (treatment episodes) | F | Drop out: M 22.3, regular discharge: M 21.2 | Not stated | Lower BMI, AN purging subtype, and active fluid restriction make significant independent contributions to drop-out risk |
| Stanley [220]* | BN, AN | Risk and protective factors for those who were identified as being at-risk of negative life outcomes, and who had originally been interviewed as 12 years prior (when they were aged 11–12 years) | Semi-structured interview | 9 (1 AN and BN history) | 33.3% F, 66.6% M | 21–22 | 56% Māori, 33% Pasifika, 11% Pakeha | Identified protective factors for AN participant included intrapersonal ability (e.g. self-awareness) and external supports (e.g. family). Risk factors were self-identified aberrant cognitions, physical health, adoption, and secondary schooling |
| Swain-Campbell [221] | BN, AN, 'other EDs' | Satisfaction with specialist eating disorders services | Custom questionnaire (structured and open-ended questions) | 120 | 4% M | M 27 | 94% European | Overall high approval, but negative commentary on some aspects of treatment (e.g. being weighed, gaining weight, stopping purging as compensatory strategy) |
| Teevale [222]* | NC (OPIC) | Views about eating, physical activity, and body image in Pasifika Island adolescents and parents |
Study 1 Questionnaire Study 2 Qualitative individual interviews |
Study 14,215 Study 2 68 | Study 1 52% F, 48% M Study 2 68% F, 32% M (qualitative) | Study 1 12–20 Study 2 13–17 (qualitative) | Study 1 55.4% Pasifika, 20.2% Māori, 12.3% Asian, 12.1% European, Study 2: Pasifika | Socio-environmental influences (e.g. occupational type, health education) more relevant to health behaviours than socio-cultural factors. Qualitative study: Beliefs about eating, physical activity, and body image similar between obese and healthy-weight Pasifika participants |
| Thabrew [223] | AN | Exploring inpatient AN treatment experience | Semi-structured interview | 9 | F | 15–17 |
7 NZ European 2 Asian |
Themes identified included admission benefits (safe space, support from staff), stress (e.g. being re-fed, being away from supports and regular life), control/power (e.g. compulsory treatment), being heard, and comparison with others in treatment |
| Tozzi [224] | AN (Sullivan et al. [84] sample) | Subjective accounts of causes of AN and recovery | DIGS, open ended questions | 69 | F | M 32.3 (SD 7.8) | 98.6% European | Family dysfunction most commonly cited as causal, in addition to dieting/weight loss and stress. Factors contributing to recovery included relationships and maturation |
| Watterson [225]* | BN, AN, BED (COSTS) | Mixed methods study of factors associated with ED maintenance and recovery, and perceptions of what contributed to successful treatment and recovery | Qualitative interview, online survey based on existing surveys by BEAT charity and Butterfly Foundation | 358 (quantitative), 18 of whom also participated in qualitative interviews | F | 28.2 (SD 12.2) | 88.7% NZ European, 6% Māori, 1.1% Pasifika, 13.2% other (includes Chinese, European, Australian, Middle Eastern, and Indian) | Multiple causal factors endorsed across EDs, most frequent were low self-esteem, perfectionism and difficulty managing negative emotions. Need for control was higher for those with AN |
| Waugh [25] | BN, AN | Comparing children of those with current or past AN or BN on factors such as eating behaviours, health, development, and psychometric variables | EDI, Toddler Temperament Scale, maternal report and interviews, food diaries, videoed mealtimes | 20 mothers (10 cases, 10 NC controls) | F (Children: 5 M and 5 F per group) |
Cases M 30.1 (SD 3.1), NC M 30.8 (SD 3.6). Children 12–48 months |
Not stated | Difficulties in children of the ED group include low birth weight, difficulties with breast feeding, and non-interactive mealtimes |
| Webb [226]* | AN | Features of AN as indicated by those with current or past AN | Interviews available notes and documents | 7 | F | 18–35 | Not stated | Identifies issues relating to control/ self-concept, continued concerns around food/exercise, reluctance to develop sexual relationships, and concerns around relationships with others |
NC non-clinical, PedsQL Pediatric Quality of Life Inventory, AQoL Assessment of Quality of Life, PRQC Perceived Relationship Quality Components, AAQ Acceptance and Action Questionnaire, RSES Rosenberg Self-Esteem Scale, BDI Beck Depression Inventory, WCBS Weight Control Behaviours Scale, BMI body mass index, BES Binge Eating Scale, WLOCS Weight Locus of Control Scale, DASS Depression Anxiety and Stress Scale, EAT Eating Attitudes Test, PSWQ Penn State Worry Questionnaire, PBRS Positive Beliefs about Rumination Scale, NBRS Negative Beliefs about Rumination Scale, RRQ Rumination and Reflection Questionnaire, TCQ Thought Control Questionnaire, MCQ-30 Metacognitive Questionnaire 30, EDE Eating Disorder Examination, BAS Body Appreciation Scale, BESAA Body Esteem Scale for Adolescents and Adults, SATAQ Sociocultural Attitudes Towards Appearance Questionnaire, ONE Opinions on Normalised Eating, DIGS Diagnostic Interview for Genetic Studies, EDI Eating Disorders Inventory
*Identifies that the record is a thesis
Table 7.
Case studies and case series
| References | Population focus | Focus | Key data collected | Sample n | Gender | Age | Ethnicity | Summary findings |
|---|---|---|---|---|---|---|---|---|
| Bulik [227] | BN | BN participant who ate large quantities of bran as a method of simultaneously bingeing and purging | Case notes | 1 | F | 27 | European | Reported positive treatment outcome following CBT including exposure with response prevention |
| Bulik [228] | BN | Characteristics of a woman who self-induced a miscarriage through dietary restriction and exercise | SCID I and II, self-monitoring | 1 | F | 28 | Not stated | First account of intentional use of ED behaviours to cause a miscarriage. Commentary on patient’s perspective |
| Bulik [229] | BN, AN (ATS) | Case of participant who combined her ED symptoms with factitious presentations | Case notes, structured interview | 1 | F | Late 30s | Not stated | AN and BN true comorbid conditions with Munchausen's syndrome |
| Hall [230] |
Service data BN, AN, Atypical EDs |
Examined referral patterns to the eating disorder service in Wellington from 1977 to 1986 | Interviews about ED history, case record review | 343 | 96% F | 15–29 | Not stated | Rates of AN were stable but BN referrals increased from 6 to 44/100,000 per year |
| Hill [231] | AN | Case, treatment, and outcome of an elderly woman with AN | Case notes | 1 | F | 72 | Not stated | Onset following bereavement of husband, after nine ECT treatments the eating behaviour improved and depressive symptoms diminished |
| McKenzie [232] |
AN Service data |
Patterns of inpatient hospitalisation for AN patients admitted for the first time in 1980 and 1981 | Clinical data | 112 |
89% F 11% M |
20.2 ± 7.5 |
99% European 1% Māori |
Long admissions, secondary only to schizophrenia and organic conditions., with 45% readmission within 5 years |
| Scott [233]* | BN, AN | Own and family’s story in relation to author's experience with BN and AN | Conversations with family members | 1 (AN/BN) | F (author) | N/A | N/A | Author identifies growth following experience, AN/BN identified as something which defies logic, isolated author from others |
| Surgenor [234] | AN | Case of attempted suicide using nasogastric feeding tube during AN treatment | Case description | 1 | F | 33 | Not stated | Advised potential precautions around those with NG who are at risk of self-harm |
| Surgenor [235] | Atypical EDs | Case report on atypical eating disorder in transgendered woman | ED service assessment data, EDI-2 | 1 | Transgender | 25 | Fijian-Indian, European | Insight into the co-occurrence of an ED and transgenderism |
| Wu [236] | BN, AN (GBDS) | ED prevalence and disability-adjusted life years in different countries between 1990 and 2017 | Age standard rates (prevalence), disability-adjusted life years | Not stated for NZ | Not stated for NZ | 5–50 (age groups) | Not stated for NZ | High age-standardized rates of prevalence and disability and adjusted life-years of eating disorders in Australasia |
Structured Clinical Interview for DSM, EDI eating disorder inventory
*Identifies that the record is a thesis
Foci and wider studies
The groups examined included binge-eating disorder (BED), bulimia nervosa (BN), anorexia nervosa (AN), Eating Disorder Not Otherwise Specified (EDNOS) or Other Specified Feeding and Eating Disorders (OSFED), orthorexia, and disordered eating or body image among non-clinical (NC) groups. Many publications reported data on a range of variables from larger studies or datasets, including the Anorexia Treatment Study (ATS) [17]; Bulimia Treatment Study (BTS) [18]; the Binge Eating Psychotherapy study (BEP) [19]; Te Rau Hinengaro (TRH) [20]; The Costs of Eating Disorders in New Zealand (COSTS) study, the Survey of Nutrition, Dietary Assessment and Lifestyles (SuNDiAL), Youth Health Surveys [21], Programme for the Integration of Mental Health Data (PRIMHD), The Collaborative Psychiatric Epidemiology Surveys (CPES) [22], and the Global Burden of Disease Study (GBDS) [23].
Sample characteristics
A wide range of sample sizes existed within the quantitative research, with the smallest sample recorded at 5 participants [24] and the largest being 12,992 participants [20]. Within the qualitative research, the sample sizes ranged from 1 to 69 participants. The majority of publications reported all-female (137 studies) or mostly female (14 studies) participant groups. A small number focused on male participants, and on sexual minority individuals. The age range of participants was large, with the lowest age being 12 months [25] and the highest being 98 years [26]. Of the 123 studies that provided age ranges for their samples, seven included children under the age of 13 years, with two focusing specifically on children. Thirty-five included participants over 45 years, though none focused specifically on this age group. A total of 133 studies reported ethnicity data or included samples for which ethnicity was previously reported; ethnicity data were unavailable for the remaining 62 studies. Two of the records within the scope of this review focused primarily on eating disorders or body image among Māori—the Indigenous New Zealand minority population.
Types of data collected
The majority of studies used interviews or self-report measures. Data collection instruments that were commonly used to examine eating pathology included the Eating Disorder Inventory (EDI; 24 studies) [30], EDI-2 (19 studies), [31] EDI-3 (3 studies) [32], Eating Disorder Examination (EDE) [33] or the related questionnaire EDE-Q (29 studies) [34], and the Eating Attitudes Test (EAT-26 or EAT-40) [35] questionnaires (10 studies). Various versions of the Structured Clinical Interview for the Diagnostic and Statistical Manual (SCID) [36] were also used (35 studies). Other commonly identified instruments included the Beck Depression Inventory (BDI) [37] in 18 studies, Rosenberg Self Esteem Scale (RSES) [38] in 9 studies, Hamilton Depression Rating Scale (HDRS; 31 studies) [39], and the Temperament and Character Inventory (TCI) [40] in 14 studies. Among the qualitative studies, individual interviews were most common, while the use of focus groups was minimal. With the exception of physical measures such as weight and height, other physiological methods of data collection and analysis such as blood testing (8 studies), neuroimaging, genetic testing, and other biological assessments were less common.
Discussion
This scoping review identified studies that examined disordered eating and body image in clinical and non-clinical samples from New Zealand, and outlined the methodologies and results reported for each study. A large number of records were located and assessed, and these involved a wide range of methodologies and vastly different foci highlighting considerable progress in understanding disordered eating and body image within New Zealand.
Methodology Most of the literature identified in this review described quantitative research, however a smaller number of exploratory qualitative studies and case studies were also identified, with the majority being identified during grey literature searches. Longitudinal studies and follow up studies of eating disorder treatments, particularly those of five years or more, were also uncommon, which may be attributable to the high cost and attrition rates associated with this type of research. Studies included participants from both clinical samples and non-clinical samples; however, large clinical samples were uncommon, which is likely underpinned by limited funding for larger studies (given that New Zealand allocates a much smaller portion of its GDP to funding research, relative to other countries) [41]. In addition, the relatively small New Zealand population makes it difficult to recruit large samples of individuals with eating disorders, which are relatively low prevalence conditions. Self-report and interview measures were identified as being most frequently used, whereas the analysis of biological data such as blood samples, which can be helpful in understanding the impact of disordered eating, was uncommon. This may be attributable to the relative ease and affordability of survey and interview data, whereas other methods tend to require more financial and research infrastructure, resources, and expertise.
Sex and gender Although some of the studies included males or gender minorities, most focussed on samples that were predominantly or exclusively female. The identification of only two all-male samples [42, 43] is consistent with reports that less than 1% of all published eating disorder research focused specifically on males with these disorders [44, 45]. Several of the identified New Zealand studies of eating disorders excluded potential male participants, or excluded data provided by male survey respondents. This may be partly because the prevalence of these disorders, with the exception of BED, tends to be lower among males [46], leading to low recruitment numbers that generally preclude statistical analyses. The inclusion of male participants also necessitates adapting treatment packages or prevention strategies for these individuals, which provides further logistical challenges for researchers [47]. Although females may be an easier group to recruit from, differences in the presentation of eating disorders and body image concerns in males need to be examined further [48]. In addition, the consistently low recruitment of male participants perpetuates the notion that eating disorders primarily afflict females, while reducing the likelihood that men will come forward to participate in future research on eating disorders, or to seek treatment. There is also evidence to suggest differences in body image concerns, as well as eating disorder risk factors and presentation, among sexual minority and LGBTQIA + individuals [28]; however, very few of the identified studies explored these differences. As such, there is a need for context-specific information to assist healthcare providers in furthering their knowledge of the presentation and treatment options for men, gender minority, and LGBTQIA + individuals in New Zealand.
Age There was a tendency for studies to recruit adolescents and younger adults. This may be partly attributable to convenience, with university aged students being the most readily available population for non-clinical studies, while the higher prevalence of eating disorders among young people can make other age groups more difficult to sample from. We identified very few studies that included participants under the age of 13, which is of particular concern given reports that eating disorders are being increasingly identified among children [49]. Conversely, there were also fewer studies involving middle-aged or older participants, despite middle-age being associated with increased eating disorder risk for women in particular, in part related to the menopause transition [50, 51]. With increased knowledge surrounding the risk and development of eating and body image issues across different age groups in New Zealand, more targeted and effective prevention and treatment strategies may be established.
Ancestry Many studies did not report ethnicity data, and Māori and Pasifika peoples were typically under-represented where these data were available. The lack of Māori and Pasifika representation and inclusion marginalises these groups further, while the extent and ways they are impacted by eating disorders, disordered eating, and body image concerns remain unclear. A lack of research into eating disorders within Indigenous and minority ethnicity populations is common within international literature, which limits our understanding of how to best understand, detect, and approach the treatment of eating disorders among these groups [52]. The results of this review suggest that New Zealand is no exception to this pattern, despite the prevalence of anorexia nervosa and bulimia nervosa in Māori being similar to or higher than in the general population [53]. Food and rituals surrounding food are central to Māori and Pasifika cultures, and are important to consider when assessing and treating eating disorders in Māori and Pasifika participants [13]. It is important to assess all eating disorders in future studies, given subthreshold eating disorders and disordered eating have been found to be highly prevalent in Indigenous peoples in Australia, suggesting current diagnostic criteria may not adequately capture eating problems in underrepresented minority identity groups [54]. Therefore, future studies of eating disorders and related issues within New Zealand need to actively seek participation from Māori and Pasifika people, and explore these issues from a culturally inclusive viewpoint.
Strengths and limitations This review has a number of strengths. Firstly, it captures research spanning a 43-year timeframe, allowing for a thorough investigation into the nature of research on disordered eating and body image within New Zealand. Furthermore, the review has included not only peer-reviewed journal articles, but also grey literature in the form of Masters and Doctoral theses. The addition of postgraduate research has allowed for a pragmatic and inclusive examination of the work conducted using New Zealand based samples, whereas a traditional style of review may exclude valuable data present in grey literature. The present review also has several limitations, with one being that a portion of the relevant grey literature, was unavailable for screening. Some of these theses could have added to the breadth of research methodologies, participants, and foci reported in the review. Although all Medline records are indexed in Embase, it may have been beneficial to also include Medline in the search strategy, as the indexing is unique to each of these databases. In addition, although every attempt was made to pre-define which topics would be included or excluded in the search, there is still a chance of reviewer bias in choosing whether to include research that fit less clearly within the margins of the scope. This is a risk particularly with the inclusion of research on body image. For example, other reviewers might have included studies with questionnaire items that alluded to body image, e.g. “how I look” without specifying weight and shape. However, the involvement of two independent reviewers reduced the risk of bias, as any inconsistencies in the inclusion of records were carefully addressed.
Recommendations Given the data presented in this review, a number of recommendations have been formulated for New Zealand research in the area of eating disorders, disordered eating, and body image. Firstly, although studies of a short term and non-experimental nature are less time-consuming and cheaper, the relapsing nature of eating disorders indicates that more longitudinal studies and long-term psychotherapy follow-ups would be valuable. Future research will also benefit from utilising different assessment methods to better understand the mechanisms underlying eating disorders. These may include physiological methods such as neuroimaging, or other biometric or biological, and genomic and other—omic approaches [55–57]. This in turn would allow for a more complete physiological picture of eating disorders in New Zealand, and would aid local research in keeping pace with international research methods. A second recommendation is to include more studies of body image and eating behaviours among males and LGBTQIA + communities. As mentioned earlier, this would further contribute to an understanding of how to responsibly and appropriately approach eating disorders in these groups. Future research should also examine eating disorders and body image concerns before adolescence, and beyond the age of 45, to better address the needs of individuals affected at different life stages. Finally, the paucity of research using a representative proportion of Māori and Pasifika participants was of particular concern. Although it may be more difficult to recruit participants from ethnic minority groups, it is vitally important that researchers make every effort to do so. This should involve engaging these communities from the outset, rather than only studying them as research participants [58].
Funders should be aware of considerable need for eating disorders research to be able to better serve ill individuals and their families in New Zealand. Proposal requirements should require inclusion of men and minoritized gender and ethnic groups, even specifying a minimum percentage of males and individuals from minority ethnicity groups. Funding should be allocated and timed in a way that supports recruitment from more difficult to reach groups, such as providing budgets specifically for targeted advertising and allowing more time to focus on engaging with these participant communities. In addition, funded research should be encouraged to include these groups as active researchers, building capacity in these communities and enabling them to provide guidance throughout the study. Lastly, budgets should be sufficient to support controlled treatment trials, particularly for groups that have been understudied, and research involving techniques and methods that are novel or underutilised.
Conclusions This scoping review is the first comprehensive examination of research into disordered eating and body image conducted in New Zealand. By summarising the foci, methods, and results for each of these studies, the review has also highlighted many gaps and areas where further funding and research is needed, including more treatment trials and longitudinal research, more advanced methods of data collection and analysis, and the inclusion of more diverse sample groups. While it may be more difficult to recruit individuals from minority groups, the greater social connectivity provided by the internet may assist researchers in recruiting, surveying, or interviewing such groups with less difficulty than previously. This study has identified a considerable body of research, and provides important information to assist funders and researchers in benchmarking findings against samples from New Zealand.
Acknowledgements
Not applicable.
Author contributions
LC: conceptualisation, methodology, formal analysis, writing—original draft. HLK: methodology, formal analysis, writing—review and editing. MAP: writing—review and editing. MAK: writing—review and editing. CMB: writing—review and editing. JJ: conceptualisation, formal analysis, methodology, supervision, writing—review and editing. All authors read and approved the final manuscript.
Funding
All authors were supported in part by the Eating Disorders Genetics Initiative (EDGI) grant (NIMH R01MH120170). The funder has no input into this scoping review.
Availability of data and materials
All data generated during this study are included in this published article and were extracted from existing publications.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent or participation
Not applicable.
Competing interests
CM Bulik reports: Shire (grant recipient, Scientific Advisory Board member); Lundbeckfonden (grant recipient); Pearson (author, royalty recipient); Equip Health Inc. (Clinical Advisory Board).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiat. 2013;73(9):904–914. doi: 10.1016/j.biopsych.2012.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Browne M, Wells J, Scott K, McGee MA. Lifetime prevalence and projected lifetime risk of DSM-IV disorders in Te Rau Hinengaro: the New Zealand Mental Health Survey. Aust N Z J Psychiatry. 2006;40(10):865–874. doi: 10.1080/j.1440-1614.2006.01905.x. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-5: Fifth edition. Arlington, VA : American Psychiatric Association, [2013]; 2013.
- 4.Riesco N, Agüera Z, Granero R, Jiménez-Murcia S, Menchón JM, Fernández-Aranda F. Other specified feeding or eating disorders (OSFED): clinical heterogeneity and cognitive-behavioral therapy outcome. Eur Psychiatry. 2018;54:109–116. doi: 10.1016/j.eurpsy.2018.08.001. [DOI] [PubMed] [Google Scholar]
- 5.Utter J, Denny S, Robinson E, Ameratunga S, Crengle S. Identifying the ‘red flags’ for unhealthy weight control among adolescents: findings from an item response theory analysis of a national survey. Int J Behav Nutr Phys Act. 2012;9(1):99. doi: 10.1186/1479-5868-9-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O'Brien KS, Hunter JA. Body esteem and eating behaviours in female physical education students. Eat Weight Disord. 2006;11(2):e57–60. doi: 10.1007/BF03327761. [DOI] [PubMed] [Google Scholar]
- 7.Madden CEL, Leong SL, Gray A, Horwath CC. Eating in response to hunger and satiety signals is related to BMI in a nationwide sample of 1601 mid-age New Zealand women. Public Health Nutr. 2012;15(12):2272–2279. doi: 10.1017/S1368980012000882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grilo CM. Why no cognitive body image feature such as overvaluation of shape/weight in the binge eating disorder diagnosis? Int J Eat Disord. 2013;46(3):208–211. doi: 10.1002/eat.22082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stice E. Risk and maintenance factors for eating pathology: a meta-analytic review. Psychol Bull. 2002;128(5):825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- 10.Cooley E, Toray T. Body image and personality predictors of eating disorder symptoms during college years. Int J Eat Disord. 2001;30:28–36. doi: 10.1002/eat.1051. [DOI] [PubMed] [Google Scholar]
- 11.Purton T, Mond J, Cicero D, Wagner A, Stefano E, Rand-Giovannetti D, et al. Body dissatisfaction, internalized weight bias and quality of life in young men and women. Qual Life Res. 2019;28(7):1825–1833. doi: 10.1007/s11136-019-02140-w. [DOI] [PubMed] [Google Scholar]
- 12.Talwar R, Carter JD, Gleaves DH. New Zealand female body image: what roles do ethnicity and body mass play? N Z J Psychol. 2012;41:69. [Google Scholar]
- 13.Williams Z, De Bruyn K, Scott M. The challenges of treating eating disorders in Maori. J Eat Disord. 2015 doi: 10.1186/2050-2974-3-S1-O32. [DOI] [Google Scholar]
- 14.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 15.American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 16.Toh WL, Grace SA, Rossell SL, Castle DJ, Phillipou A. Body parts of clinical concern in anorexia nervosa versus body dysmorphic disorder: a cross-diagnostic comparison. Australas Psychiatry Bull R Aust N Z Col Psychiatrists. 2020;28(2):134–139. doi: 10.1177/1039856219839477. [DOI] [PubMed] [Google Scholar]
- 17.McIntosh VV, Jordan J, Carter FA, Luty SE, McKenzie JM, Bulik CM, et al. Three psychotherapies for anorexia nervosa: a randomized, controlled trial. Am J Psychiatry. 2005;162(4):741–747. doi: 10.1176/appi.ajp.162.4.741. [DOI] [PubMed] [Google Scholar]
- 18.Bulik CM, Sullivan PF, Carter FA, McIntosh VV, Joyce PR. The role of exposure with response prevention in the cognitive-behavioural therapy for bulimia nervosa. Psychol Med. 1998;28(3):611–623. doi: 10.1017/S0033291798006618. [DOI] [PubMed] [Google Scholar]
- 19.McIntosh VVW, Jordan J, Carter JD, Frampton CMA, McKenzie JM, Latner JD, et al. Psychotherapy for transdiagnostic binge eating: a randomized controlled trial of cognitive-behavioural therapy, appetite-focused cognitive-behavioural therapy, and schema therapy. Psychiatry Res. 2016;240:412–420. doi: 10.1016/j.psychres.2016.04.080. [DOI] [PubMed] [Google Scholar]
- 20.Wells JE, Oakley Browne MA, Scott KM, McGee MA, Baxter J, Kokaua J. Te Rau Hinengaro: the New Zealand Mental Health Survey: overview of methods and findings. Aust N Z J Psychiatry. 2006;40(10):835–844. doi: 10.1111/j.1440-1614.2006.01902.x. [DOI] [PubMed] [Google Scholar]
- 21.Fleming TM, Clark T, Denny S, Bullen P, Crengle S, Peiris-John R, et al. Stability and change in the mental health of New Zealand secondary school students 2007–2012: results from the national adolescent health surveys. Aust N Z J Psychiatry. 2014;48(5):472–480. doi: 10.1177/0004867413514489. [DOI] [PubMed] [Google Scholar]
- 22.Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the collaborative psychiatric epidemiology studies (CPES) Int J Methods Psychiatr Res. 2004;13(4):221–240. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lopez AD, Murray CC. The global burden of disease, 1990–2020. Nat Med. 1998;4(11):1241–1243. doi: 10.1038/3218. [DOI] [PubMed] [Google Scholar]
- 24.Bulik CM, Brinded EC. The effect of food deprivation on alcohol consumption in bulimic and control women. Addiction. 1993;88(11):1545–1551. doi: 10.1111/j.1360-0443.1993.tb03140.x. [DOI] [PubMed] [Google Scholar]
- 25.Waugh E, Bulik CM. Offspring of women with eating disorders. Int J Eat Disord. 1999;25(2):123–133. doi: 10.1002/(SICI)1098-108X(199903)25:2<123::AID-EAT1>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 26.Kessler RC, Shahly V, Hudson JI, Supina D, Berglund PA, Chiu WT, et al. A comparative analysis of role attainment and impairment in binge-eating disorder and bulimia nervosa: results from the WHO World Mental Health Surveys. Epidemiol Psychiatr Sci. 2014;23(1):27–41. doi: 10.1017/S2045796013000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Griffiths S, Mitchison D, Murray SB, Mond JM. Pornography use in sexual minority males: associations with body dissatisfaction, eating disorder symptoms, thoughts about using anabolic steroids and quality of life. Aust N Z J Psychiatry. 2018;52(4):339–348. doi: 10.1177/0004867417728807. [DOI] [PubMed] [Google Scholar]
- 28.Griffiths S, Murray SB, Dunn M, Blashill AJ. Anabolic steroid use among gay and bisexual men living in Australia and New Zealand: associations with demographics, body dissatisfaction, eating disorder psychopathology, and quality of life. Drug Alcohol Depend. 2017;181:170–176. doi: 10.1016/j.drugalcdep.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 29.Griffiths S, Murray SB, Krug I, McLean SA. The contribution of social media to body dissatisfaction, eating disorder symptoms, and anabolic steroid use among sexual minority men. Cyberpsychol Behav Soc Netw. 2018;21(3):149–156. doi: 10.1089/cyber.2017.0375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Garner DM, Olmstead MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. Int J Eat Disord. 1983;2(2):15–34. doi: 10.1002/1098-108X(198321)2:2<15::AID-EAT2260020203>3.0.CO;2-6. [DOI] [Google Scholar]
- 31.Garner D. Eating Disorder Inventory-2: Psychological Assessment Resources; 1991.
- 32.Garner D. EDI-3 Eating Disorder Inventory-3 Professional Manual. Lutz, FL: Psychological Assessment Resources. Inc[Google Scholar]. 2004.
- 33.Fairburn C, Cooper Z. The eating disorder examination. In: Fairburn CG, Wilson GT, editors. Binge eating: nature, assessment and treatment. New York: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- 34.Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? Int J Eat Disord. 1994;16(4):363–370. doi: 10.1002/1098-108X(199412)16:4<363::AID-EAT2260160405>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 35.Garner DM, Olmsted MP, Bohr Y, Garfinkel PE. The eating attitudes test: psychometric features and clinical correlates. Psychol Med. 1982;12(4):871–878. doi: 10.1017/S0033291700049163. [DOI] [PubMed] [Google Scholar]
- 36.Columbia Psychiatry. Structured Clinical Interview for DSM Disorders (SCID) [updated 2022]. Available from: https://www.columbiapsychiatry.org/research/research-areas/services-policy-and-law/structured-clinical-interview-dsm-disorders-scid.
- 37.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4(6):561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 38.Rosenberg M. Society and the adolescent self-image. Princeton: Princeton University Press; 2015. [Google Scholar]
- 39.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cloninger CR, Przybeck TR, Svrakic DM, Wetzel RD. The temperament and character inventory (TCI): a guide to its development and use. 1994.
- 41.The World Bank. Research and development expenditure (% of GDP)—New Zealand: the World Bank Group; 2022. Available from: https://data.worldbank.org/indicator/GB.XPD.RSDV.GD.ZS?locations=NZ.
- 42.Gibson C, Hindle C, McLay-Cooke R, Slater J, Brown R, Smith B, et al. Body Image Among Elite Rugby Union Players. J Strength Cond Res. 2019;33(8):2217–2222. doi: 10.1519/JSC.0000000000002312. [DOI] [PubMed] [Google Scholar]
- 43.Jones LNT. Body image dissatisfaction among men engaged in regular weight training activities: an exploratory analysis. New Zealand: University of Waikato; 2014. [Google Scholar]
- 44.Murray SB, Griffiths S, Mond JM. Evolving eating disorder psychopathology: conceptualising muscularity-oriented disordered eating. Br J Psychiatry. 2016;208(5):414–415. doi: 10.1192/bjp.bp.115.168427. [DOI] [PubMed] [Google Scholar]
- 45.Nagata JM, Murray SB, Bibbins-Domingo K, Garber AK, Mitchison D, Griffiths S. Predictors of muscularity-oriented disordered eating behaviors in U.S. young adults: a prospective cohort study. Int J Eat Disord. 2019;52(12):1380–1388. doi: 10.1002/eat.23094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biol Psychiat. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goldstein MA, Alinsky R, Medeiros C. Males with restrictive eating disorders: barriers to their care. J Adolesc Health. 2016;59(4):371–372. doi: 10.1016/j.jadohealth.2016.07.022. [DOI] [PubMed] [Google Scholar]
- 48.McCabe MP, Ricciardelli LA. Body image dissatisfaction among males across the lifespan: a review of past literature. J Psychosom Res. 2004;56(6):675–685. doi: 10.1016/S0022-3999(03)00129-6. [DOI] [PubMed] [Google Scholar]
- 49.Campbell K, Peebles R. Eating disorders in children and adolescents: state of the art review. Pediatrics. 2014;134(3):582–592. doi: 10.1542/peds.2014-0194. [DOI] [PubMed] [Google Scholar]
- 50.Baker JH, Eisenlohr-Moul T, Wu Y-K, Schiller CE, Bulik CM, Girdler SS. Ovarian hormones influence eating disorder symptom variability during the menopause transition: a pilot study. Eat Behav. 2019;35:101337. doi: 10.1016/j.eatbeh.2019.101337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Baker JH, Runfola CD. Eating disorders in midlife women: a perimenopausal eating disorder? Maturitas. 2016;85:112–116. doi: 10.1016/j.maturitas.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 52.Hay PJ, Carriage C. Eating disorder features in indigenous aboriginal and Torres Strait Islander Australian peoples. BMC Public Health. 2012;12(1):233. doi: 10.1186/1471-2458-12-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lacey C, Clark M, Manuel J, Pitama S, Cunningham R, Keelan K, et al. Is there systemic bias for Maori with eating disorders? A need for greater awareness in the healthcare system. N Zaland Med J. 2020;133(1514):71. [PubMed] [Google Scholar]
- 54.Burt A, Mannan H, Touyz S, Hay P. Prevalence of DSM-5 diagnostic threshold eating disorders and features amongst Aboriginal and Torres Strait islander peoples (First Australians) BMC Psychiatry. 2020;20(1):1–8. doi: 10.1186/s12888-020-02852-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bulik CM, Thornton LM, Parker R, Kennedy H, Baker JH, MacDermod C, et al. The eating disorders genetics initiative (EDGI): study protocol. BMC Psychiatry. 2021;21(1):234. doi: 10.1186/s12888-021-03212-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thornton LM, Munn-Chernoff MA, Baker JH, Juréus A, Parker R, Henders AK, et al. The anorexia nervosa genetics initiative (ANGI): overview and methods. Contemp Clin Trials. 2018;74:61–69. doi: 10.1016/j.cct.2018.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Watson HJ, Yilmaz Z, Thornton LM, Hübel C, Coleman JR, Gaspar HA, et al. Genome-wide association study identifies eight risk loci and implicates metabo-psychiatric origins for anorexia nervosa. Nat Genet. 2019;51(8):1207–1214. doi: 10.1038/s41588-019-0439-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.MacDermod C, Pettie MA, Carrino EA, Garcia SC, Padalecki S, Finch JE, et al. Recommendations to encourage participation of individuals from diverse backgrounds in psychiatric genetic studies. Am J Med Genet B Neuropsychiatr Genet. 2022;189(5):163–173. doi: 10.1002/ajmg.b.32906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Babbott KM. The effectiveness of an ACT based intervention in the management of disordered eating. New Zealand: The University of Waikato; 2018. [Google Scholar]
- 60.Carter FA, McIntosh VV, Joyce PR, Sullivan PF, Bulik CM. Role of exposure with response prevention in cognitive-behavioral therapy for bulimia nervosa: three-year follow-up results. Int J Eat Disord. 2003;33(2):127–135. doi: 10.1002/eat.10126. [DOI] [PubMed] [Google Scholar]
- 61.Carter FA, Jordan J, McIntosh VV, Luty SE, McKenzie JM, Frampton CM, et al. The long-term efficacy of three psychotherapies for anorexia nervosa: a randomized, controlled trial. Int J Eat Disord. 2011;44(7):647–654. doi: 10.1002/eat.20879. [DOI] [PubMed] [Google Scholar]
- 62.Clyne C, Blampied NM. Training in emotion regulation as a treatment for binge eating: a preliminary study. Behav Chang. 2004;21(4):269–281. doi: 10.1375/bech.21.4.269.66105. [DOI] [Google Scholar]
- 63.Clyne C, Latner JD, Gleaves DH, Blampied NM. Treatment of emotional dysregulation in full syndrome and subthreshold binge eating disorder. Eat Disord. 2010;18(5):408–424. doi: 10.1080/10640266.2010.511930. [DOI] [PubMed] [Google Scholar]
- 64.Davey MR. An evaluation of the pre-treatment motivation groups run by the south island eating disorders service. New Zealand: University of Canterbury; 2012. [Google Scholar]
- 65.de Hoedt Norgrove TC. Reflective Kai-tiakitanga: evaluation of a self-help acceptance and commitment therapy package for emotional eating behaviours. New Zealand: The University of Waikato; 2019. [Google Scholar]
- 66.McIntosh VV, Carter FA, Bulik CM, Frampton CM, Joyce PR. Five-year outcome of cognitive behavioral therapy and exposure with response prevention for bulimia nervosa. Psychol Med. 2011;41(5):1061–1071. doi: 10.1017/S0033291710001583. [DOI] [PubMed] [Google Scholar]
- 67.Mercier D. An alternative intervention for bulimia. New Zealand: University of Otago; 1990. [Google Scholar]
- 68.Roberts ME. Feasibility of group cognitive remediation therapy in an adult eating disorder day program in New Zealand. Eat Behav. 2018;30:1–4. doi: 10.1016/j.eatbeh.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 69.Then R. An open trial investigating the usefulness of metacognitive therapy for patients diagnosed with anorexia nervosa. New Zealand: University of Canterbury; 2020. [Google Scholar]
- 70.Wallis NJ. Treating binge eating disorder: a psychoeducational programme teaching emotional discrimination and management. New Zealand: University of Canterbury; 1998. [Google Scholar]
- 71.Wilksch SM, O'Shea A, Taylor CB, Wilfley D, Jacobi C, Wade TD. Online prevention of disordered eating in at-risk young-adult women: a two-country pragmatic randomized controlled trial. Psychol Med. 2018;48(12):2034–2044. doi: 10.1017/S0033291717003567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wilksch SM, O'Shea A, Wade TD. Media smart-targeted: diagnostic outcomes from a two-country pragmatic online eating disorder risk reduction trial for young adults. Int J Eat Disord. 2018;51(3):270–274. doi: 10.1002/eat.22825. [DOI] [PubMed] [Google Scholar]
- 73.Wilksch SM, O'Shea A, Wade TD. Depressive symptoms, alcohol and other drug use, and suicide risk: prevention and treatment effects from a two-country online eating disorder risk reduction trial. Int J Eat Disord. 2019;52(2):132–141. doi: 10.1002/eat.23005. [DOI] [PubMed] [Google Scholar]
- 74.Anderson CB, Joyce PR, Carter FA, McIntosh VV, Bulik CM. The effect of cognitive-behavioral therapy for bulimia nervosa on temperament and character as measured by the temperament and character inventory. Compr Psychiatry. 2002;43(3):182–188. doi: 10.1053/comp.2002.32359. [DOI] [PubMed] [Google Scholar]
- 75.Bourke CM, Porter RJ, Sullivan P, Bulik CM, Carter FA, McIntosh VV, et al. Neuropsychological function in bulimia with comorbid borderline personality disorder and depression. Acta Neuropsychiatr. 2006;18(3–4):162–167. doi: 10.1111/j.1601-5215.2006.00148.x. [DOI] [PubMed] [Google Scholar]
- 76.Bulik CM, Sullivan PF, Joyce PR, Carter FA. Temperament, character, and personality disorder in bulimia nervosa. J Nerv Ment Dis. 1995;183(9):593–598. doi: 10.1097/00005053-199509000-00006. [DOI] [PubMed] [Google Scholar]
- 77.Bulik CM, Sullivan PF, Carter FA, Joyce PR. Lifetime anxiety disorders in women with bulimia nervosa. Compr Psychiatry. 1996;37(5):368–374. doi: 10.1016/S0010-440X(96)90019-X. [DOI] [PubMed] [Google Scholar]
- 78.Bulik CM, Sullivan PF, Lawson RH, Carter FA. Salivary reactivity in women with bulimia nervosa across treatment. Biol Psychiatry. 1996;39(12):1009–1012. doi: 10.1016/0006-3223(95)00317-7. [DOI] [PubMed] [Google Scholar]
- 79.Bulik CM, Sullivan PF, Carter FA, Joyce PR. Initial manifestations of disordered eating behavior: dieting versus binging. Int J Eat Disord. 1997;22(2):195–201. doi: 10.1002/(SICI)1098-108X(199709)22:2<195::AID-EAT12>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 80.Bulik CM, Sullivan PF, Carter FA, Joyce PR. Lifetime comorbidity of alcohol dependence in women with bulimia nervosa. Addict Behav. 1997;22(4):437–446. doi: 10.1016/S0306-4603(96)00053-6. [DOI] [PubMed] [Google Scholar]
- 81.Bulik CM, Sullivan PF, Fear JL, Joyce PR. Eating disorders and antecedent anxiety disorders: a controlled study. Acta Psychiatr Scand. 1997;96(2):101–107. doi: 10.1111/j.1600-0447.1997.tb09913.x. [DOI] [PubMed] [Google Scholar]
- 82.Bulik CM, Sullivan PF, Carter FA, McIntosh VV, Joyce PR. Predictors of rapid and sustained response to cognitive-behavioral therapy for bulimia nervosa. Int J Eat Disord. 1999;26(2):137–144. doi: 10.1002/(SICI)1098-108X(199909)26:2<137::AID-EAT2>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 83.Bulik CM, Sullivan PF, Joyce PR. Temperament, character and suicide attempts in anorexia nervosa, bulimia nervosa and major depression. Acta Psychiatr Scand. 1999;100(1):27–32. doi: 10.1111/j.1600-0447.1999.tb10910.x. [DOI] [PubMed] [Google Scholar]
- 84.Sullivan PF, Bulik CM, Fear JL, Pickering A. Outcome of anorexia nervosa: a case-control study. Am J Psychiatry. 1998;155(7):939–946. doi: 10.1176/ajp.155.7.939. [DOI] [PubMed] [Google Scholar]
- 85.Carter FA, Bulik CM, McIntosh VV, Joyce PR. Changes on the stroop test following treatment: relation to word type, treatment condition, and treatment outcome among women with bulimia nervosa. Int J Eat Disord. 2000;28(4):349–355. doi: 10.1002/1098-108X(200012)28:4<349::AID-EAT1>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 86.Carter FA, McIntosh VV, Joyce PR, Bulik CM. Abstention during cue reactivity assessment is associated with better outcome among women with bulimia nervosa. Eat Behav. 2001;2(3):273–278. doi: 10.1016/S1471-0153(01)00034-4. [DOI] [PubMed] [Google Scholar]
- 87.Carter F, Bulik C, McIntosh V, Joyce P. Changes in cue reactivity following treatment for bulimia nervosa. Int J Eat Disord. 2001;29:336–344. doi: 10.1002/eat.1027. [DOI] [PubMed] [Google Scholar]
- 88.Carter FA, Bulik CM, McIntosh VV, Joyce PR. Cue reactivity as a predictor of outcome with bulimia nervosa. Int J Eat Disord. 2002;31(3):240–250. doi: 10.1002/eat.10041. [DOI] [PubMed] [Google Scholar]
- 89.Carter FA, McIntosh VV, Joyce PR, Frampton CM, Bulik CM. Bulimia nervosa, childbirth, and psychopathology. J Psychosom Res. 2003;55(4):357–361. doi: 10.1016/S0022-3999(02)00641-4. [DOI] [PubMed] [Google Scholar]
- 90.Carter FA, McIntosh VV, Frampton CM, Joyce PR, Bulik CM. Predictors of childbirth following treatment for bulimia nervosa. Int J Eat Disord. 2003;34(3):337–342. doi: 10.1002/eat.10218. [DOI] [PubMed] [Google Scholar]
- 91.Carter FA, McIntosh VVW, Joyce PR, Gendall KA, Bulik CM. Impact of pre-treatment weight on weight trajectory in women treated for bulimia nervosa. Eur Eat Disord Rev. 2004;12(6):387–391. doi: 10.1002/erv.600. [DOI] [Google Scholar]
- 92.Carter FA, McIntosh VV, Joyce PR, Gendall KA, Frampton CM, Bulik CM. Patterns of weight change after treatment for bulimia nervosa. Int J Eat Disord. 2004;36(1):12–21. doi: 10.1002/eat.20021. [DOI] [PubMed] [Google Scholar]
- 93.Carter FA, McIntosh VV, Joyce PR, Frampton CM, Bulik CM. Cue reactivity in bulimia nervosa: a useful self-report approach. Int J Eat Disord. 2006;39(8):694–699. doi: 10.1002/eat.20331. [DOI] [PubMed] [Google Scholar]
- 94.Carter FA, Carter JD, Luty SE, Jordan J, McIntosh VV, Bartram AF, et al. What is worse for your sex life: starving, being depressed, or a new baby? Int J Eat Disord. 2007;40(7):664–667. doi: 10.1002/eat.20394. [DOI] [PubMed] [Google Scholar]
- 95.Carter J, Mulder R, Bartram A, Darlow B. Infants in a neonatal intensive care unit: parental response. Arch Dis Child Fetal Neonatal Ed. 2005;90(2):F109–F113. doi: 10.1136/adc.2003.031641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Carter FA, McIntosh VV, Joyce PR, Bulik CM. Weight suppression predicts weight gain over treatment but not treatment completion or outcome in bulimia nervosa. J Abnorm Psychol. 2008;117(4):936–940. doi: 10.1037/a0013942. [DOI] [PubMed] [Google Scholar]
- 97.Carter FA, Boden JM, Jordan J, McIntosh VV, Bulik CM, Joyce PR. Weight suppression predicts total weight gain and rate of weight gain in outpatients with anorexia nervosa. Int J Eat Disord. 2015;48(7):912–918. doi: 10.1002/eat.22425. [DOI] [PubMed] [Google Scholar]
- 98.Falloon C. Therapist adherence in the treatment of transdiagnostic binge eating disorders. New Zealand: University of Canterbury; 2018. [Google Scholar]
- 99.Gendall KA, Sullivan PE, Joyce PR, Carter FA, Bulik CM. The nutrient intake of women with bulimia nervosa. Int J Eat Disord. 1997;21(2):115–127. doi: 10.1002/(SICI)1098-108X(199703)21:2<115::AID-EAT2>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 100.Gendall KA, Bulik CM, Joyce PR. Visceral protein and hematological status of women with bulimia nervosa and depressed controls. Physiol Behav. 1999;66(1):159–163. doi: 10.1016/S0031-9384(98)00236-4. [DOI] [PubMed] [Google Scholar]
- 101.Gendall KA, Bulik CM, Sullivan PF, Joyce PR, McIntosh VV, Carter FA. Body weight in bulimia nervosa. Eat Weight Disord. 1999;4(4):157–164. doi: 10.1007/BF03339730. [DOI] [PubMed] [Google Scholar]
- 102.Gendall KA, Bulik CM, Joyce PR, McIntosh VV, Carter FA. Menstrual cycle irregularity in bulimia nervosa. Associated factors and changes with treatment. J Psychosom Res. 2000;49(6):409–415. doi: 10.1016/S0022-3999(00)00188-4. [DOI] [PubMed] [Google Scholar]
- 103.Gendall KA, Joyce PR, Carter FA, McIntosh VV, Bulik CM. The effect of bulimia nervosa on plasma glucose and lipids. Physiol Behav. 2002;77(1):99–105. doi: 10.1016/S0031-9384(02)00829-6. [DOI] [PubMed] [Google Scholar]
- 104.Gendall KA, Joyce PR, Carter FA, McIntosh VV, Bulik CM. Thyroid indices and treatment outcome in bulimia nervosa. Acta Psychiatr Scand. 2003;108(3):190–195. doi: 10.1034/j.1600-0447.2003.00117.x. [DOI] [PubMed] [Google Scholar]
- 105.Gendall KA, Joyce PR, Carter FA, McIntosh VV, Bulik CM. Childhood gastrointestinal complaints in women with bulimia nervosa. Int J Eat Disord. 2005;37(3):256–260. doi: 10.1002/eat.20088. [DOI] [PubMed] [Google Scholar]
- 106.Gendall KA, Joyce PR, Carter FA, McIntosh VV, Jordan J, Bulik CM. The psychobiology and diagnostic significance of amenorrhea in patients with anorexia nervosa. Fertil Steril. 2006;85(5):1531–1535. doi: 10.1016/j.fertnstert.2005.10.048. [DOI] [PubMed] [Google Scholar]
- 107.Jenkins L. Motivation to change and anorexia nervosa: relation between expressions of motivation to change and outcome in psychotherapy. New Zealand: University of Canterbury; 2013. [Google Scholar]
- 108.Jordan J, Joyce PR, Carter FA, Horn J, McIntosh VV, Luty SE, et al. Anxiety and psychoactive substance use disorder comorbidity in anorexia nervosa or depression. Int J Eat Disord. 2003;34(2):211–219. doi: 10.1002/eat.10177. [DOI] [PubMed] [Google Scholar]
- 109.Jordan J, Joyce PR, Carter FA, Horn J, McIntosh VV, Luty SE, et al. Specific and nonspecific comorbidity in anorexia nervosa. Int J Eat Disord. 2008;41(1):47–56. doi: 10.1002/eat.20463. [DOI] [PubMed] [Google Scholar]
- 110.Jordan J, Joyce PR, Carter FA, McIntosh VV, Luty SE, McKenzie JM, et al. The Yale-Brown-Cornell eating disorder scale in women with anorexia nervosa: what is it measuring? Int J Eat Disord. 2009;42(3):267–274. doi: 10.1002/eat.20605. [DOI] [PubMed] [Google Scholar]
- 111.Jordan J, McIntosh VV, Carter FA, Joyce PR, Frampton CM, Luty SE, et al. Clinical characteristics associated with premature termination from outpatient psychotherapy for anorexia nervosa. Eur Eat Disord Rev. 2014;22(4):278–284. doi: 10.1002/erv.2296. [DOI] [PubMed] [Google Scholar]
- 112.Jordan J, McIntosh VV, Carter JD, Rowe S, Taylor K, Frampton CM, et al. Bulimia nervosa-nonpurging subtype: closer to the bulimia nervosa-purging subtype or to binge eating disorder? Int J Eat Disord. 2014;47(3):231–238. doi: 10.1002/eat.22218. [DOI] [PubMed] [Google Scholar]
- 113.Jordan J, McIntosh VVW, Carter FA, Joyce PR, Frampton CMA, Luty SE, et al. Predictors of premature termination from psychotherapy for anorexia nervosa: Low treatment credibility, early therapy alliance, and self-transcendence. Int J Eat Disord. 2017;50(8):979–983. doi: 10.1002/eat.22726. [DOI] [PubMed] [Google Scholar]
- 114.Lacey C, Cunningham R, Rijnberg V, Manuel J, Clark MTR, Keelan K, et al. Eating disorders in New Zealand: implications for Māori and health service delivery. Int J Eat Disord. 2020;53(12):1974–1982. doi: 10.1002/eat.23372. [DOI] [PubMed] [Google Scholar]
- 115.McIntosh VVW, Jordan J, Carter FA, McKenzie JM, Luty SE, Bulik CM, et al. Strict versus lenient weight criterion in anorexia nervosa. Eur Eat Disord Rev. 2004;12(1):51–60. doi: 10.1002/erv.557. [DOI] [Google Scholar]
- 116.McIntosh VVW, Jordan J, McKenzie JM, Luty SE, Carter FA, Carter JD, et al. Measuring therapist adherence in psychotherapy for anorexia nervosa: Scale adaptation, psychometric properties, and distinguishing psychotherapies. Psychother Res. 2005;15(3):339–344. doi: 10.1080/10503300500091124. [DOI] [PubMed] [Google Scholar]
- 117.McIntosh VV, Jordan J, Carter JD, Luty SE, Carter FA, McKenzie JM, et al. Assessing the distinctiveness of psychotherapies and examining change over treatment for anorexia nervosa with cognitive-behavior therapy, interpersonal psychotherapy, and specialist supportive clinical management. Int J Eat Disord. 2016;49(10):958–962. doi: 10.1002/eat.22555. [DOI] [PubMed] [Google Scholar]
- 118.Rowe SL, Jordan J, McIntosh VVW, Carter FA, Bulik CM, Joyce PR. Impact of Borderline Personality Disorder on Bulimia Nervosa. Aust N Z J Psychiatry. 2008;42(12):1021–1029. doi: 10.1080/00048670802512040. [DOI] [PubMed] [Google Scholar]
- 119.Rowe SL, Jordan J, McIntosh VVW, Carter FA, Frampton C, Bulik CM, et al. Does avoidant personality disorder impact on the outcome of treatment for bulimia nervosa? Int J Eat Disord. 2010;43(5):420–427. doi: 10.1002/eat.20716. [DOI] [PubMed] [Google Scholar]
- 120.Rowe SL, Jordan J, McIntosh VV, Carter FA, Frampton C, Bulik CM, et al. Complex personality disorder in bulimia nervosa. Compr Psychiatry. 2010;51(6):592–598. doi: 10.1016/j.comppsych.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 121.Rowe S, Jordan J, McIntosh V, Carter F, Frampton C, Bulik C, et al. Dimensional measures of personality as a predictor of outcome at 5-year follow-up in women with bulimia nervosa. Psychiatry Res. 2011;185(3):414–420. doi: 10.1016/j.psychres.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 122.Sullivan PF, Bulik CM, Carter FA, Gendall KA, Joyce PR. The significance of a prior history of anorexia in bulimia nervosa. Int J Eat Disord. 1996;20(3):253–261. doi: 10.1002/(SICI)1098-108X(199611)20:3<253::AID-EAT4>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 123.Sullivan PF, Gendall KA, Bulik CM, Carter FA, Joyce PR. Elevated total cholesterol in bulimia nervosa. Int J Eat Disord. 1998;23(4):425–432. doi: 10.1002/(SICI)1098-108X(199805)23:4<425::AID-EAT10>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 124.Surgenor LJ, Horn J, Hudson SM. Empirical scrutiny of a familiar narrative: sense of control in anorexia nervosa. Eur Eat Disord Rev. 2003;11(4):291–305. doi: 10.1002/erv.499. [DOI] [Google Scholar]
- 125.Talwar R. Correlates and predictors of dysfunctional eating attitudes and behaviours in a non-clinical New Zealand female sample. New Zealand: University of Canterbury; 2009. [Google Scholar]
- 126.Boyce JA, Kuijer RG, Gleaves DH. Positive fantasies or negative contrasts: the effect of media body ideals on restrained eaters’ mood, weight satisfaction, and food intake. Body Image. 2013;10(4):535–543. doi: 10.1016/j.bodyim.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 127.Boyce JA, Kuijer RG. Focusing on media body ideal images triggers food intake among restrained eaters: a test of restraint theory and the elaboration likelihood model. Eat Behav. 2014;15(2):262–270. doi: 10.1016/j.eatbeh.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 128.Bulik CM, Brinded EC. The effect of food deprivation on the reinforcing value of food and smoking in bulimic and control women. Physiol Behav. 1994;55(4):665–672. doi: 10.1016/0031-9384(94)90042-6. [DOI] [PubMed] [Google Scholar]
- 129.Bulik CM, Brinded EC, Lawson RH. The effect of short-term food deprivation on the reinforcing value of coffee in bulimic and control women. Behav Chang. 1995;12(2):63–68. doi: 10.1017/S0813483900004241. [DOI] [Google Scholar]
- 130.Bulik CM, Lawson RH, Carter FA. Salivary reactivity in restrained and unrestrained eaters and women with bulimia nervosa. Appetite. 1996;27(1):15–24. doi: 10.1006/appe.1996.0030. [DOI] [PubMed] [Google Scholar]
- 131.Carter FA, Bulik CM. Cue reactivity and bulimia nervosa: refining and standardising methodology. Behav Chang. 1996;13(2):98–111. doi: 10.1017/S0813483900003806. [DOI] [Google Scholar]
- 132.Carter FA, Bulik CM, Lawson RH, Sullivan PF, Wilson JS. Effect of mood and food cues on body image in women with bulimia and controls. Int J Eat Disord. 1996;20(1):65–76. doi: 10.1002/(SICI)1098-108X(199607)20:1<65::AID-EAT8>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 133.Carter FA, Bulik CM, Lawson RH, Sullivan PF, Wilson JS. Effect of mood and food cues on information processing in women with bulimia nervosa and controls. Behav Chang. 1997;14(2):113–120. doi: 10.1017/S0813483900003570. [DOI] [Google Scholar]
- 134.Gendall KA, Joyce PR, Abbott RM. The effects of meal composition on subsequent craving and binge eating. Addict Behav. 1999;24(3):305–315. doi: 10.1016/S0306-4603(98)00046-X. [DOI] [PubMed] [Google Scholar]
- 135.Gendall KA, Joyce PR. Meal-induced changes in tryptophan:LNAA ratio: effects on craving and binge eating. Eat Behav. 2000;1(1):53–62. doi: 10.1016/S1471-0153(00)00006-4. [DOI] [PubMed] [Google Scholar]
- 136.Hickford CA, Ward T, Bulik CM. Cognitions of restrained and unrestrained eaters under fasting and nonfasting conditions. Behav Res Ther. 1997;35(1):71–75. doi: 10.1016/S0005-7967(96)00056-3. [DOI] [PubMed] [Google Scholar]
- 137.Latner JD, Wilson GT. Binge eating and satiety in bulimia nervosa and binge eating disorder: effects of macronutrient intake. Int J Eat Disord. 2004;36(4):402–415. doi: 10.1002/eat.20060. [DOI] [PubMed] [Google Scholar]
- 138.Latner JD, Rosewall JK, Chisholm AM. Energy density effects on food intake, appetite ratings, and loss of control in women with binge eating disorder and weight-matched controls. Eat Behav. 2008;9(3):257–266. doi: 10.1016/j.eatbeh.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 139.Latner JD, Rosewall JK, Chisholm AM. Food volume effects on intake and appetite in women with binge-eating disorder and weight-matched controls. Int J Eat Disord. 2009;42(1):68–75. doi: 10.1002/eat.20570. [DOI] [PubMed] [Google Scholar]
- 140.Stock K. The relationship between focussing on body functionality and body satisfaction: the moderating role of neuroticism and social comparison orientation. New Zealand: University of Canterbury; 2018. [Google Scholar]
- 141.Walsh A. Serotonin and the eating disorders: the effects of dieting, acute plasma tryptophan depletion and mCPP administration on brain 5-HT function. New Zealand: University of Otago; 1994. [Google Scholar]
- 142.Baxter J, Kingi TK, Tapsell R, Durie M, McGee MA. Prevalence of mental disorders among Māori in Te Rau Hinengaro: the New Zealand Mental Health Survey. Aust N Z J Psychiatry. 2006;40(10):914–923. doi: 10.1080/j.1440-1614.2006.01911.x. [DOI] [PubMed] [Google Scholar]
- 143.Bensley R. Associations between aspects of body image and lifestyle behaviours and attitudes in Otago adolescents. New Zealand: University of Otago; 2017. [Google Scholar]
- 144.Blackmore NPI. Alcohol related vomiting in a New Zealand University sample: frequency, gender differences, and correlates. New Zealand: Univeristy of Canterbury; 2009. [Google Scholar]
- 145.Boyes AD, Fletcher GJ, Latner JD. Male and female body image and dieting in the context of intimate relationships. J Fam Psychol. 2007;21(4):764–768. doi: 10.1037/0893-3200.21.4.764. [DOI] [PubMed] [Google Scholar]
- 146.Brewis AA, McGarvey ST, Jones J, Swinburn BA. Perceptions of body size in Pacific Islanders. Int J Obes Relat Metab Disord. 1998;22(2):185–189. doi: 10.1038/sj.ijo.0800562. [DOI] [PubMed] [Google Scholar]
- 147.Bushnell JA, Wells JE, Hornblow AR, Oakley-Browne MA, Joyce P. Prevalence of three bulimia syndromes in the general population. Psychol Med. 1990;20(3):671–680. doi: 10.1017/S0033291700017190. [DOI] [PubMed] [Google Scholar]
- 148.Chan CKY, Glynn OR. Perfectionism and eating disorder symptomatology in Chinese immigrants: mediating and moderating effects of ethnic identity and acculturation. Psychol Health. 2006;21(1):49–63. doi: 10.1080/14768320500105312. [DOI] [Google Scholar]
- 149.Dameh M. Insight in anorexia nervosa. New Zealand: University of Otago; 2002. [Google Scholar]
- 150.Durso LE, Latner JD. Understanding self-directed stigma: development of the weight bias internalization scale. Obesity. 2008;16(Suppl 2):S80–S86. doi: 10.1038/oby.2008.448. [DOI] [PubMed] [Google Scholar]
- 151.Fear J, Bulik C, Sullivan P. The prevalence of disordered eating behaviours and attitudes in adolescent girls. N Z J Psychol. 1996;25:7–12. [Google Scholar]
- 152.Foliaki SA, Kokaua J, Schaaf D, Tukuitonga C. Twelve-month and lifetime prevalences of mental disorders and treatment contact among Pacific people in Te Rau Hinengaro: the New Zealand Mental Health Survey. Aust N Z J Psychiatry. 2006;40(10):924–934. doi: 10.1080/j.1440-1614.2006.01912.x. [DOI] [PubMed] [Google Scholar]
- 153.Gendall KA, Joyce PR, Sullivan PF. Impact of definition on prevalence of food cravings in a random sample of young women. Appetite. 1997;28(1):63–72. doi: 10.1006/appe.1996.0060. [DOI] [PubMed] [Google Scholar]
- 154.Gendall KA, Sullivan PF, Joyce PR, Fear JL, Bulik CM. Psychopathology and personality of young women who experience food cravings. Addict Behav. 1997;22(4):545–555. doi: 10.1016/S0306-4603(96)00060-3. [DOI] [PubMed] [Google Scholar]
- 155.Gendall KA, Sullivan PF, Joyce PR, Bulik CM. Food cravings in women with a history of anorexia nervosa. Int J Eat Disord. 1997;22(4):403–409. doi: 10.1002/(SICI)1098-108X(199712)22:4<403::AID-EAT5>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 156.Gendall KA, Joyce PR, Sullivan PF, Bulik CM. Personality and dimensions of dietary restraint. Int J Eat Disord. 1998;24(4):371–379. doi: 10.1002/(SICI)1098-108X(199812)24:4<371::AID-EAT4>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 157.Gendall KA, Joyce PR, Sullivan PF, Bulik CM. Food cravers: characteristics of those who binge. Int J Eat Disord. 1998;23(4):353–360. doi: 10.1002/(SICI)1098-108X(199805)23:4<353::AID-EAT2>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 158.Hechler T, Beumont P, Marks P, Touyz S. How do clinical specialists understand the role of physical activity in eating disorders? Eur Eat Disord Rev Prof J Eat Disord Assoc. 2005;13(2):125–132. doi: 10.1002/erv.630. [DOI] [Google Scholar]
- 159.Hickman K. Adult attachment, bulimia nervosa and relationship satisfaction. New Zealand: University of Canterbury; 1988. [Google Scholar]
- 160.Hudson CLF. The relationship of body image, body mass index, and self-esteem to eating attitudes in a normal sample. New Zealand: University of Canterbury; 2008. [Google Scholar]
- 161.Jenkins SL. Body image and eating attitudes: comparing Chinese females with other females living in New Zealand [Masters] Hamilton: University of Waikato; 2007. [Google Scholar]
- 162.Jospe M, Brown R, Williams S, Roy M, Meredith-Jones K, Taylor R. Self-monitoring has no adverse effect on disordered eating in adults seeking treatment for obesity. Obes Sci Pract. 2018 doi: 10.1002/osp4.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kokaua J. An Application Of Hierarchical Bayes Models To Estimated Prevalence Of Mental Disorder And Mental Health Service Use Among Cook Islanders In New Zealand: University of Otago; 2015.
- 164.Latner JD, Vallance JK, Buckett G. Health-related quality of life in women with eating disorders: association with subjective and objective binge eating. J Clin Psychol Med Settings. 2008;15(2):148–153. doi: 10.1007/s10880-008-9111-1. [DOI] [PubMed] [Google Scholar]
- 165.Latner JD, Mond JM, Vallance JK, Gleaves DH, Buckett G. Body checking and avoidance in women: associations with mental and physical health-related quality of life. Eat Behav. 2012;13(4):386–389. doi: 10.1016/j.eatbeh.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 166.Latner JD, Mond JM, Vallance JK, Gleaves DH, Buckett G. Quality of life impairment and the attitudinal and behavioral features of eating disorders. J Nerv Ment Dis. 2013;201(7):592–597. doi: 10.1097/NMD.0b013e3182982bbe. [DOI] [PubMed] [Google Scholar]
- 167.Lau C. Weight loss intentions and methods in New Zealand adolescents. New Zealand: University of Otago; 2021. [Google Scholar]
- 168.Leydon MA, Wall C. New Zealand jockeys' dietary habits and their potential impact on health. Int J Sport Nutr Exerc Metab. 2002;12(2):220–237. doi: 10.1123/ijsnem.12.2.220. [DOI] [PubMed] [Google Scholar]
- 169.Linardon J, Messer M, Lee S, Rosato J. Perspectives of e-health interventions for treating and preventing eating disorders: descriptive study of perceived advantages and barriers, help-seeking intentions, and preferred functionality. Eat Weight Disord. 2021;26(4):1097–1109. doi: 10.1007/s40519-020-01005-3. [DOI] [PubMed] [Google Scholar]
- 170.Lucassen MF, Guntupalli AM, Clark T, Fenaughty J, Denny S, Fleming T, et al. Body size and weight, and the nutrition and activity behaviours of sexual and gender minority youth: findings and implications from New Zealand. Public Health Nutr. 2019;22(13):2346–2356. doi: 10.1017/S1368980019001149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Maguire S, Surgenor LJ, Abraham S, Beumont P. An international collaborative database: its use in predicting length of stay for inpatient treatment of anorexia nervosa. Aust N Z J Psychiatry. 2003;37(6):741–747. doi: 10.1080/j.1440-1614.2003.01257.x. [DOI] [PubMed] [Google Scholar]
- 172.McCabe M, Mavoa H, Ricciardelli L, Schultz J, Waqa G, Fotu K. Socio-cultural agents and their impact on body image and body change strategies among adolescents in Fiji, Tonga, Tongans in New Zealand and Australia. Obes Rev Off J Int Assoc Study Obes. 2011;12(Suppl 2):61–67. doi: 10.1111/j.1467-789X.2011.00922.x. [DOI] [PubMed] [Google Scholar]
- 173.McCabe MP, Busija L, Fuller-Tyszkiewicz M, Ricciardelli L, Mellor D, Mussap A. Sociocultural influences on strategies to lose weight, gain weight, and increase muscles among ten cultural groups. Body Image. 2015;12:108–114. doi: 10.1016/j.bodyim.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 174.Miller E, Halberstadt J. Media consumption, body image and thin ideals in New Zealand men and women. N Z J Psychol. 2005;34:189. [Google Scholar]
- 175.Moss HJ. Body dissatisfaction in adolescents with eating disorders: associations with maladaptive perfectionism and anxiety. New Zealand: University of Canterbury; 2011. [Google Scholar]
- 176.Muir K. A comparison of the recognition of facial emotion in women of low body weight, both with and without anorexia nervosa. New Zealand: University of Canterbury; 2011. [Google Scholar]
- 177.Mulgrew KE, Kannis-Dymand L, Hughes E, Carter JD, Kaye S. Psychological factors associated with the use of weight management behaviours in young adults. J Health Psychol. 2016;24(3):337–350. doi: 10.1177/1359105316675210. [DOI] [PubMed] [Google Scholar]
- 178.Ngamanu RE. Body image attitudes amongst Māori and Pakeha females. New Zealand: The University of Waikato; 2006. [Google Scholar]
- 179.Oakley Browne MA, Wells JE, Scott KM, McGee MA. Lifetime prevalence and projected lifetime risk of DSM-IV disorders in Te Rau Hinengaro: the New Zealand Mental Health Survey. Aust N Z J Psychiatry. 2006;40(10):865–874. doi: 10.1080/j.1440-1614.2006.01905.x. [DOI] [PubMed] [Google Scholar]
- 180.O'Brien K, Venn BJ, Perry T, Green TJ, Aitken W, Bradshaw A, et al. Reasons for wanting to lose weight: different strokes for different folks. Eat Behav. 2007;8(1):132–135. doi: 10.1016/j.eatbeh.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 181.Overton A, Selway S, Strongman K, Houston M. Eating disorders—the regulation of positive as well as negative emotion experience. J Clin Psychol Med Settings. 2005;12(1):39–56. doi: 10.1007/s10880-005-0911-2. [DOI] [Google Scholar]
- 182.Reynolds R, McMahon S. Views of health professionals on the clinical recognition of orthorexia nervosa: a pilot study. Eat Weight Disord. 2020;25(4):1117–1124. doi: 10.1007/s40519-019-00701-z. [DOI] [PubMed] [Google Scholar]
- 183.Robertson RK. Body image, self-esteem, and interpersonal relationships in adulthood. New Zealand: Auckland University of Technology; 2009. [Google Scholar]
- 184.Rodino IS, Byrne SM, Sanders KA. Eating disorders in the context of preconception care: fertility specialists' knowledge, attitudes, and clinical practices. Fertil Steril. 2017;107(2):494–501. doi: 10.1016/j.fertnstert.2016.10.036. [DOI] [PubMed] [Google Scholar]
- 185.Rosewall JK, Gleaves DH, Latner JD. An examination of risk factors that moderate the body dissatisfaction-eating pathology relationship among New Zealand adolescent girls. J Eat Disord. 2018;6(1):38. doi: 10.1186/s40337-018-0225-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Rosewall JK, Gleaves DH, Latner JD. Moderators of the relationship between body dissatisfaction and eating pathology in preadolescent girls. J Early Adolesc. 2019;40(3):328–353. doi: 10.1177/0272431619837385. [DOI] [Google Scholar]
- 187.Rosewall JK, Gleaves DH, Latner JD. Psychopathology factors that affect the relationship between body size and body dissatisfaction and the relationship between body dissatisfaction and eating pathology. Front Psychol 2019;9. [DOI] [PMC free article] [PubMed]
- 188.Shephard SL. The sociocultural model of eating disorders in New Zealand women: family food-related experiences and self-compassion as moderators. New Zealand: University of Canterbury; 2012. [Google Scholar]
- 189.Slater J. Low energy availability in New Zealand recreational athletes. New Zealand: University of Otago; 2015. [Google Scholar]
- 190.Strang PM. A comparison of cognitive interference in restrained and unrestrained eaters using a modified Stroop task: a thesis presented in partial fulfilment of the requirements for the degree of Master of Arts in Psychology at Massey University [Masters] New Zealand: Massey University; 1996. [Google Scholar]
- 191.Vallance JK, Latner JD, Gleaves DH. The relationship between eating disorder psychopathology and health-related quality of life within a community sample. Qual Life Res. 2011;20(5):675–682. doi: 10.1007/s11136-010-9799-x. [DOI] [PubMed] [Google Scholar]
- 192.Vaňousová N, Brown TA, Sellbom M. Criterion and incremental validity of the MMPI-3 eating concerns scale in a university sample. J Clin Psychol Med Settings. 2021 doi: 10.1007/s10880-021-09772-6. [DOI] [PubMed] [Google Scholar]
- 193.Wells JE, Browne MA, Scott KM, McGee MA, Baxter J, Kokaua J. Prevalence, interference with life and severity of 12 month DSM-IV disorders in Te Rau Hinengaro: the New Zealand Mental Health Survey. Aust N Z J Psychiatry. 2006;40(10):845–854. doi: 10.1080/j.1440-1614.2006.01903.x. [DOI] [PubMed] [Google Scholar]
- 194.Archer AJ. Women with anorexia nervosa and bulimia nervosa: individual and family characteristics, with particular emphasis on perfectionism. New Zealand: University of Canterbury; 1996. [Google Scholar]
- 195.Bulik CM, Sullivan PF. Comorbidity of bulimia and substance abuse: perceptions of family of origin. Int J Eat Disord. 1993;13(1):49–56. doi: 10.1002/1098-108X(199301)13:1<49::AID-EAT2260130107>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 196.Bulik CM, Sullivan PF, Fear J, Pickering A. Predictors of the development of bulimia nervosa in women with anorexia nervosa. J Nerv Ment Dis. 1997;185(11):704–707. doi: 10.1097/00005053-199711000-00009. [DOI] [PubMed] [Google Scholar]
- 197.Bulik CM, Sullivan PF, Fear JL, Pickering A, Dawn A, McCullin M. Fertility and reproduction in women with anorexia nervosa: a controlled study. J Clin Psychiatry. 1999;60(2):130–135. doi: 10.4088/JCP.v60n0212. [DOI] [PubMed] [Google Scholar]
- 198.Bulik CM, Sullivan PF, Fear JL, Pickering A. Outcome of anorexia nervosa: eating attitudes, personality, and parental bonding. Int J Eat Disord. 2000;28(2):139–147. doi: 10.1002/1098-108X(200009)28:2<139::AID-EAT2>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 199.Fowler SJ, Bulik CM. Family environment and psychiatric history in women with binge-eating disorder and obese controls. Behav Chang. 1997;14(2):106–112. doi: 10.1017/S0813483900003569. [DOI] [Google Scholar]
- 200.Latner JD, Hildebrandt T, Rosewall JK, Chisholm AM, Hayashi K. Loss of control over eating reflects eating disturbances and general psychopathology. Behav Res Ther. 2007;45(9):2203–2211. doi: 10.1016/j.brat.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 201.Romans SE, Gendall KA, Martin JL, Mullen PE. Child sexual abuse and later disordered eating: a New Zealand epidemiological study. Int J Eat Disord. 2001;29(4):380–392. doi: 10.1002/eat.1034. [DOI] [PubMed] [Google Scholar]
- 202.Allison JE. An exploration of issues that might surround and affect young women's eating behaviours : a thesis presented in partial fulfilment of the requirements for the degree of Master of Arts in Nursing at Massey University [Masters]: Massey University; 2001.
- 203.Batenburg G. Perceived causes of initial development and relapses in anorexia nervosa: a comparison to theoretical models of aetiology. New Zealand: The University of Waikato; 2015. [Google Scholar]
- 204.Bellingham A. Parents battling their child's anorexia: what is it like for a parent to care for a child with an eating disorder? New Zealand: Massey University; 2012. [Google Scholar]
- 205.Carne SS. Aspects of adolescent obesity in New Zealand : quality of life, psychosocial factors and psychological theory. New Zealand: University of Auckland; 2008. [Google Scholar]
- 206.Chisholm AM. When and why does female dieting become pernicious? The role of individual differences and partner support in romantic relationships. New Zealand: University of Canterbury; 2008. [Google Scholar]
- 207.Conder JA. The body image of women with intellectual disability. New Zealand: University of Otago; 2014. [Google Scholar]
- 208.Easter CD. Perspectives and experiences of off-field problematic behaviour among elite New Zealand athletes. New Zealand: University of Waikato; 2014. [Google Scholar]
- 209.Gunn C. How women cope with pregnancy and early mothering after recovery from an eating disorder: a grounded theory of women's experience. New Zealand: Massey University; 2005. [Google Scholar]
- 210.Hall A. Family structure and relationships of 50 female anorexia nervosa patients. Aust N Z J Psychiatry. 1978;12(4):263–268. doi: 10.3109/00048677809159090. [DOI] [PubMed] [Google Scholar]
- 211.Hammond KM. A quantitative and qualitative analysis of women’s body image: comparisons between normal weight, overweight, eating disordered and body building women. New Zealand: University of Auckland; 1996. [Google Scholar]
- 212.Kleinbichler JK. The type and frequency of metacognitions in women dieting, not dieting, and with anorexia nervosa. New Zealand: University of Canterbury; 2013. [Google Scholar]
- 213.McClintock JM. The influence of sociocultural and interpersonal factors on body image disturbance and unhealthy dieting in female adolescents. New Zealand: The University of Waikato; 2003. [Google Scholar]
- 214.Poulter PI, Treharne GJ. "I'm actually pretty happy with how I am": a mixed-methods study of young women with positive body image. Psychol Health. 2020;36(6):649–668. doi: 10.1080/08870446.2020.1820008. [DOI] [PubMed] [Google Scholar]
- 215.Schofield KL. A mixed-method approach to low energy availability in elite track cyclists. New Zealand: The University of Waikato; 2021. [Google Scholar]
- 216.Snell L, Crowe M, Jordan J. Maintaining a therapeutic connection: nursing in an inpatient eating disorder unit. J Clin Nurs. 2010;19(3–4):351–358. doi: 10.1111/j.1365-2702.2009.03000.x. [DOI] [PubMed] [Google Scholar]
- 217.Stiles G. Normalised eating in the treatment of eating disorders. New Zealand: Massey University; 2014. [Google Scholar]
- 218.Surgenor LJ, Plumridge EW, Horn J. "Knowing one's self" anorexic: implications for therapeutic practice. Int J Eat Disord. 2003;33(1):22–32. doi: 10.1002/eat.10117. [DOI] [PubMed] [Google Scholar]
- 219.Surgenor LJ, Maguire S, Beumont PJV. Drop-out from inpatient treatment for anorexia nervosa: can risk factors be identified at point of admission? Eur Eat Disord Rev. 2004;12:94–100. doi: 10.1002/erv.539. [DOI] [Google Scholar]
- 220.Stanley PG. Risk and resilience: the role of risk and protective factors in the lives of young people over time. New Zealand: Auckland University of Technology; 2010. [Google Scholar]
- 221.Swain-Campbell NR, Surgenor LJ, Snell DL. An analysis of consumer perspectives following contact with an eating-disorders service. Aust N Z J Psychiatry. 2001;35(1):99–103. doi: 10.1046/j.1440-1614.2001.00855.x. [DOI] [PubMed] [Google Scholar]
- 222.Teevale T. Obesity in Pacific adolescents: a socio-cultural study in Auckland. New Zealand: University of Auckland; 2009. [Google Scholar]
- 223.Thabrew H, Mairs R, Taylor-Davies G. Young people's experiences of brief inpatient treatment for anorexia nervosa. J Paediatr Child Health. 2020;56(1):30–33. doi: 10.1111/jpc.14483. [DOI] [PubMed] [Google Scholar]
- 224.Tozzi F, Sullivan PF, Fear JL, McKenzie J, Bulik CM. Causes and recovery in anorexia nervosa: the patient's perspective. Int J Eat Disord. 2003;33(2):143–154. doi: 10.1002/eat.10120. [DOI] [PubMed] [Google Scholar]
- 225.Watterson R. Exploring the onset, maintenance, treatment and recovery of eating disorders from the perspective of New Zealand women with lived experience: a mixed methods approach. New Zealand: University of Canterbury; 2020. [Google Scholar]
- 226.Webb SB. Anorexia nervosa—its nature and treatment : a phenomenological investigation: a dissertation presented in partial fulfilment of the requirements for the degree of Master of Philosophy in Education at Massey University [Masters]: Massey University; 1982.
- 227.Bulik CM. “Abuse” of dietary fibre in a woman with bulimia nervosa. Behav Change. 1992;9(4):258–259. doi: 10.1017/S0813483900006197. [DOI] [Google Scholar]
- 228.Bulik CM, Carter FA, Sullivan PF. Self-induced abortion in a bulimic woman. Int J Eat Disord. 1994;15(3):297–299. doi: 10.1002/1098-108X(199404)15:3<297::AID-EAT2260150316>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 229.Bulik CM, Sullivan PF, Fear JL, Pickering A. A case of comorbid anorexia nervosa, bulimia nervosa, and Munchausen's syndrome. Int J Eat Disord. 1996;20(2):215–218. doi: 10.1002/(SICI)1098-108X(199609)20:2<215::AID-EAT14>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 230.Hall A, Hay PJ. Eating disorder patient referrals from a population region 1977–1986. Psychol Med. 1991;21(3):697–701. doi: 10.1017/S0033291700022339. [DOI] [PubMed] [Google Scholar]
- 231.Hill R, Haslett C, Kumar S. Anorexia nervosa in an elderly woman. Aust N Z J Psychiatry. 2001;35(2):246–248. doi: 10.1046/j.1440-1614.2001.00871.x. [DOI] [PubMed] [Google Scholar]
- 232.McKenzie JM, Joyce PR. Hospitalization for anorexia nervosa. Int J Eat Disord. 1992;11(3):235–241. doi: 10.1002/1098-108X(199204)11:3<235::AID-EAT2260110306>3.0.CO;2-T. [DOI] [Google Scholar]
- 233.Scott PL. Positioning and re-positioning of individual and family relationships in relation to anorexia/bulimia: an auto-ethnographical informed study [Doctor of Philosophy]. The University of Waikato, New Zealand 2010.
- 234.Surgenor LJ, Snell DL. Nasogastric tube as a means of attempted suicide: a case report. Eur Eat Disord Rev. 1998;6(3):212–215. doi: 10.1002/(SICI)1099-0968(199809)6:3<212::AID-ERV246>3.0.CO;2-2. [DOI] [Google Scholar]
- 235.Surgenor LJ, Fear JL. Eating disorder in a transgendered patient: a case report. Int J Eat Disord. 1998;24(4):449–452. doi: 10.1002/(SICI)1098-108X(199812)24:4<449::AID-EAT14>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 236.Wu J, Liu J, Li S, Ma H, Wang Y. Trends in the prevalence and disability-adjusted life years of eating disorders from 1990 to 2017: results from the Global Burden of Disease Study 2017. Epidemiol Psychiatr Sci. 2020;29:e191. doi: 10.1017/S2045796020001055. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated during this study are included in this published article and were extracted from existing publications.