Abstract
Products of the intercellular adhesion (ica) operon in Staphylococcus aureus and Staphylococcus epidermidis synthesize a linear β-1,6-linked glucosaminylglycan. This extracellular polysaccharide mediates bacterial cell-cell adhesion and is required for biofilm formation, which is thought to increase the virulence of both pathogens in association with prosthetic biomedical implants. The environmental signal(s) that triggers ica gene product and polysaccharide expression is unknown. Here we demonstrate that anaerobic in vitro growth conditions lead to increased polysaccharide expression in both S. aureus and S. epidermidis, although the regulation is less stringent in S. epidermidis. Anaerobiosis also dramatically stimulates ica-specific mRNA expression in ica- and polysaccharide-positive strains of both S. aureus and S. epidermidis. These data suggest a mechanism whereby ica gene expression and polysaccharide production may act as a virulence factor in an anaerobic environment in vivo.
Staphylococci cause a wide range of diseases in animals and humans (17). The virulence of the two major opportunistic pathogens of this genus, Staphylococcus epidermidis and Staphylococcus aureus, is multifactorial and mediated, particularly in S. aureus, by a variety of extracellular toxins and surface structures (2). In general, bacterial virulence is thought to be regulated by environmental signals to which the bacteria respond via global gene regulators, thereby adapting their phenotypes accordingly (21). Thus, typical staphylococcal infections such as endocarditis, meningitis, osteomyelitis, postoperative wound infections, and chronic lung infections may each involve different sets of virulence factors due to different environmental conditions. Similarly, in vitro gene expression by bacterial pathogens may not necessarily reflect in vivo gene expression (13).
Recently, it was shown that S. aureus strains expressing capsular polysaccharide type 5 (CP5) in vitro but not in vivo produce another polysaccharide in infected airways of cystic fibrosis (CF) patients, consisting of poly-N-succinyl-β-1,6-glucosamine (PNSG) (20). PNSG is synthesized by products of the intercellular adhesion (ica) gene locus in S. aureus (7, 20), which was previously identified in S. epidermidis (12) and whose presence in other closely related species such as Staphylococcus auricularis and Staphylococcus capitis was inferred (7).
Products of the ica locus in S. epidermidis also produce the polysaccharide intercellular adhesin (PIA). PIA production leads to cell-cell adhesion and is required for biofilm formation (11). This polysaccharide was identified as a linear β-1,6-linked N-acetylglucosaminoglycan (18, 19). Antibodies raised against S. epidermidis PIA or S. aureus PNSG recognize both antigens. We use a polyclonal antibody raised against S. epidermidis PIA in this work; however, where the exact nature of the polysaccharide is not known, we use the term “PIA/PNSG” to refer to the polysaccharide(s) synthesized by gene products of the ica locus in either S. epidermidis or S. aureus.
The ica operon (icaADBC) consists of four open reading frames, with a putative regulatory gene (icaR) located upstream and in the opposite orientation. In an in vitro assay, it was shown that IcaA and IcaD together synthesize sugar oligomers using UDP-N-acetylglucosamine as a substrate. This N-acetylglucosaminyltransferase activity together with the activity of IcaC produces a product in vitro that is recognized by an antibody raised against S. epidermidis PIA (9). Isogenic mutants of wild-type biofilm-forming strains in which the ica locus has been mutated or deleted are no longer able to form a biofilm in vitro, demonstrating that the ica genes, and therefore PIA/PNSG production, are required for biofilm formation (7, 11, 12).
Biofilm formation is a major concern in nosocomial infections because it protects microorganisms from opsonophagocytosis and antibiotic agents, leading to chronic infection and sepsis, particularly in immunocompromised patients (6). The contribution of PIA/PNSG to the virulence of S. epidermidis has been repeatedly demonstrated (24–26, 31); however, the environmental signals which mediate PIA/PNSG expression are at present unknown.
Recently, we provided evidence that the partial pressure of oxygen in airway plugs of CF patients was <4% that of intraluminal air (D. Worlitzsch, K. C. Meyer, P. Birrer, and G. Döring, Pediatr. Pulmonol., abstr. A457, p. 333, 1998). Since we also observed PNSG expression in the S. aureus-infected CF lung (20), the objective of the present study was to investigate the impact of anaerobiosis on PIA/PNSG expression in S. epidermidis and S. aureus. Here we show that PIA/PNSG expression is indeed induced by anaerobic growth conditions and that ica gene transcription is regulated by environmental oxygen.
MATERIALS AND METHODS
Staphylococcal strains and plasmids.
The strains used in this study are listed in Table 1. The ica deletion mutant of S. aureus ATCC 35556 was described previously (7). The S. epidermidis O-47 ica deletion mutant was constructed in a similar manner, replacing the entire ica operon (icaR-icaC) with a tetracycline resistance cassette. The S. epidermidis strain ATCC 35984 (RP62A) ica locus and surrounding DNA were amplified using PCR and primers CG-28 (CCGGATCCATTGAATAATCATGAAATAATGTC) and SR-1 (CGGGATCCGAGAAAAATTTCATTTTAAAATAAAC) and cloned into the SmaI site of temperature-sensitive shuttle vector pBT5, a derivative of pBT2 lacking the EcoRI restriction site in the multiple cloning site (4), creating plasmid pSC1. The ica locus was deleted using pSC1, inverse PCR, and primers CG-7 (CTAGAGCTCTAGACCTTTCGTTAGTTAGGTTGT) and SR-2 (CGGAATTCACGCGTCACCTGTCATGTATCTCACTCC) and replaced with the tetracycline resistance cassette from pT181, amplified using primers tet-4 (CTCGAATTCGCCAGTCGATTTAACGGAC) and tet-5 (CTCGAATTCGAGTGGCAAAATGCTAGCCAC) and restriction enzyme EcoRI, creating plasmid pSC12. Primers were obtained from MWG-Biotech (Ebersberg, Germany). PCR amplifications were performed using a MiniCycler PTC-150 (MJ Research, Inc., Watertown, Mass.). Homologous recombination was performed using wild-type S. epidermidis strain O-47 containing plasmid pSC12. Bacteria were grown overnight in B medium (1% tryptone [Gibco BRL-Life Technologies GmbH, Eggenstein, Germany], 0.5% yeast extract [Gibco BRL], 0.5% NaCl, 0.1% K2HPO4, 0.1% glucose) at 30°C with 10 μg of chloramphenicol/ml, diluted 1:1,000, and grown again at 30°C with antibiotic selection; diluted 1:1,000 and grown at 41°C without antibiotic selection twice; and diluted 1:100 and plated on tryptic soy broth (TSB) (Gibco BRL) plates containing 2.5 μg of tetracycline/ml. Homologous recombination and plasmid curing of chloramphenicol-sensitive, tetracycline-resistant colonies were then confirmed with PCR and detection for loss of PIA/PNSG expression. The strain listed in Table 1 as ATCC 10832 is not the same as the strain with the same name used in our previous study (7). Strain SE05 was isolated in association with a central venous catheter removed from a patient in the intensive care unit of the University Hospital, Tübingen, Germany, in January 2000.
TABLE 1.
Strains used in this study
Aerobic and anaerobic growth.
Bacterial strains were cultured in either TSB supplemented with 0.25% glucose (TSB plus Glc) or CYPG medium (23) supplemented with 2% glucose (CYPG plus Glc) and supplemented when appropriate with tetracycline (10 μg/ml), chloramphenicol (10 μg/ml), or erythromycin (10 μg/ml). Bacteria were incubated with shaking under both aerobic and anaerobic conditions in 250-ml Erlenmeyer flasks containing 100 ml of TSB plus Glc. Anaerobic conditions were created by bubbling filtered helium gas through the medium for 10 min following inoculation. Flasks were then immediately sealed such that no air could enter the flask during incubation. The airtight seal consisted of a silicone stopper pierced with two glass pipettes, one of which (gas inlet) was submerged in the medium. Attached to the outside end of each glass pipette was a piece of flexible tubing that could be attached to the helium gas tank and clamped to seal the flask after gassing. Alternatively, overnight cultures of staphylococcal strains grown in CYPG plus Glc were harvested and diluted in CYPG plus Glc to an optical density at 600 nm (OD600) of 0.05 and incubated under aerobic conditions (with shaking) and anaerobic conditions (without shaking) in glass tubes or microtiter plates (Becton Dickinson, Heidelberg, Germany) for up to 96 h. For anaerobic growth, glass tubes were placed in an anaerobic jar with Anaerocult A (Merck Eurolab GmbH, Darmstadt, Germany), whereas polystyrol 96-well microtiter plates were sealed with adhesive tape. Anaerobiosis in both of our experimental systems was confirmed using Anaerotest test strips (Merck). PIA/PNSG production and biofilm formation were also tested under controlled (3% O2, 1% CO2, 96% N2) conditions in a shaking gassed BB6060 incubator (Heraeus, Stuttgart, Germany); however, these conditions were apparently not anaerobic enough, and little difference was seen from cultures incubated in the presence of ambient air. Bacterial growth was determined by measuring CFU on blood agar plates and/or determining OD578.
Detection of PIA/PNSG expression and biofilm formation in vitro.
Biofilm assays and semiquantitative PIA/PNSG detection using cell surface extracts were performed as described previously (7, 11, 12). Briefly, cell surface extracts were prepared by growing cells overnight (14 to 18 h) or to an OD578 of 2.0 in TSB plus Glc, the optical density was determined, and an equal number of cells (typically 2 to 4 ml) from each culture was resuspended in 50 μl of 0.5 M EDTA, pH 8.0. Cells were then incubated for 5 min at 100°C and centrifuged to pellet the cells, and 40 μl of the supernatant was incubated with 10 μl of 20-mg/ml proteinase K (Boehringer GmbH, Mannheim, Germany) for 30 min at 37°C to minimize nonspecific background. The extracts were then spotted onto a nitrocellulose membrane, and the membrane was dried, blocked with 3% bovine serum albumin, and incubated with an anti-S. epidermidis PIA antibody (diluted 1:5,000) (kind gift of D. Mack, Hamburg, Germany). Anti-PIA antibodies were detected using an alkaline phosphatase-conjugated anti-rabbit immunoglobulin (IgG) antibody (Boehringer) and the 4-nitroblue tetrazolium chloride–5-bromo-4-chloro-3-indolylphosphate (NBT/BCIP) color detection system (Boehringer).
Biofilm assays were performed as follows. Bacteria were grown overnight in TSB plus Glc. Cultures were then diluted 1:200 in fresh medium and incubated overnight in stationary U-bottomed-well polystyrol microtiter plates (Greiner Labortechnik, Frickenhausen, Germany) at 37°C. Microtiter wells were washed twice with phosphate-buffered saline (PBS) (7 mM Na2HPO4, 3 mM NaH2PO4, 130 mM NaCl, pH 7.4), dried in an inverted position, and stained with 0.1% safranin (Serva Feinbiochemica GmbH & Co. KG, Heidelberg, Germany).
PIA/PNSG expression in CYPG plus Glc was determined using indirect immunofluorescence microscopy. Briefly, liquid cultures were washed three times with PBS (pH 7.2) containing 0.05% Tween 20. Bacteria were harvested by centrifugation (5,000 × g) and resuspended in 5 ml of PBS. A drop of the suspension was transferred to a glass slide (Becton Dickinson). Samples on glass slides were fixed with 4% formaldehyde for 1 h at 4°C, and nonspecific binding sites were blocked with 5% human IgG (Sigma, Deisenhofen, Germany). Thereafter, slides were incubated with a rabbit antibody raised against S. epidermidis PIA (diluted 1:200) or a polyclonal rabbit antibody raised against S. aureus PNSG (diluted 1:50) (kind gift of G. Pier, Boston, Mass.) for 1 h at room temperature. After washing with PBS, bound antibody was detected with indocarbocyanin 3 (Cy3)-conjugated goat anti-rabbit IgG (Jackson Dianova, Hamburg, Germany) and analyzed using an Axioplan fluorescence microscope (Zeiss, Oberkochen, Germany) and a Kontron KS 300 imaging system (Kontron Electronic GmbH, Eching, Germany). Results obtained with both antibodies were identical. Data shown were obtained using the anti-PIA antibody only.
In order to observe biofilm formation over time as detected with the anti-PIA antibody, bacteria were grown in CYPG plus Glc in stationary microtiter plates and enzyme-linked immunosorbent assays (ELISAs) were performed. Briefly, microtiter plates were washed gently three times with PBS (pH 7.2), air dried, fixed with formaldehyde, and blocked with human IgG. The plates were incubated with rabbit anti-S. epidermidis PIA antibody for 2 h at 37°C, washed, and incubated with horseradish peroxidase-conjugated anti-rabbit IgG antibody (diluted 1:250) (Dako, Hamburg, Germany) for 2 h at 37°C, followed by an incubation with the substrate (Sigma). After 40 min, OD450s were measured using an ELISA plate reader (SLT Lab Instruments, Crailsheim, Germany). Each assay was performed in triplicate.
RNA extraction and detection.
S. aureus cultures were grown to an OD578 of 2.0 in TSB plus Glc. Generally, anaerobic cultures grown overnight (14 to 18 h) reached an OD578 of approximately 2.0, and aerobic cultures were grown for several hours until an OD578 of 2.0 was reached. Approximately 1010 cells were harvested by centrifugation and washed with 0.5 volume of cold 0.5 M EDTA. S. aureus cell pellets were then resuspended in 1 ml of 0.5-mg/ml lysostaphin (Sigma-Aldrich Chemie GmbH, Deisenhofen, Germany) and incubated for 3 min at 37°C. S. epidermidis cells were resuspended in cold 0.5 M EDTA and disrupted using glass beads and vortexing. RNA was then prepared using the RNeasy Midi kit (Qiagen GmbH, Hilden, Germany) as recommended by the manufacturer. RNA yield was measured by OD260, and the relative concentration between samples was confirmed by visual inspection of rRNA in samples run on an agarose gel and stained with ethidium bromide. Three micrograms of total RNA from each sample was then applied to a nylon membrane (Boehringer) using a dot blotting apparatus (Bio-Rad Laboratories, Munich, Germany). Filters were hybridized at 50°C using DIG (digoxigenin) Easy Hyb solution (Boehringer) and an ica-specific DNA probe. Filters were washed in 0.1× SSC (1× SSC is 0.15 M NaCl plus 0.015 M sodium citrate)–0.1% sodium dodecyl sulfate at 68°C and exposed to X-ray film after detection using the DIG luminescent detection kit (Boehringer). The DIG-labeled probes were made by using PCR, DIG-labeled nucleotide labeling mix (Boehringer), and the Expand Long Template PCR system (Boehringer) as recommended by the manufacturer. Amplified DNA included sequences within the coding regions from the beginning of icaA to the end of icaC and was amplified using primers SA9 (GTATTTATGTCTATTTACTGGATTGTCGGTTC) and SA6 (GTAGTGATATCGCTAGAAAGCCATTGT) for S. aureus and primers SE1 (GTCAATTTACTGGATAGTAGGATCGATTTAC) and SE2 (AGTTAGGCTGGTATTGGTCAAATTGTAACT) for S. epidermidis.
RESULTS
Construction of an ica deletion-replacement mutant in S. epidermidis.
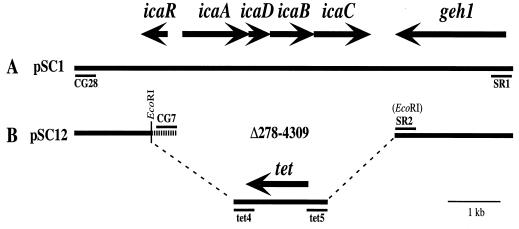
An ica deletion-replacement mutant was constructed in wild-type biofilm-forming S. aureus strain ATCC 35556 and was described previously (7). An S. epidermidis ica deletion-replacement mutant was constructed on a plasmid in a similar manner, replacing the entire ica operon (icaRADBC) with a tetracycline resistance cassette. The chromosomal copy of the ica operon was replaced by homologous recombination. A schematic representation of the cloning strategy is shown in Fig. 1 and described in more detail in Materials and Methods.
FIG. 1.
Schematic representation of cloning strategy used to construct the ica deletion-replacement mutant of S. epidermidis. A similar strategy was used to construct the ica deletion-replacement mutant of S. aureus, described in reference 7. (A) Plasmid pSC1. Sequences including and surrounding the ica locus are included in database entry U43366. Sequences including and surrounding the geh1 gene are included in database entry AF053006. PCR primers used to amplify cloned DNA are indicated (CG-28 and SR-1). (B) Plasmid pSC12, the deletion-replacement construct used for homologous recombination. Inverse PCR primers used to delete the ica locus (CG-7 and SR-2) and amplify the tetracycline resistance cassette (tet4 and tet5) are indicated. EcoRI restriction recognition sites contained within the sequences of primers SR-2, tet-4, and tet-5 and the EcoRI restriction site in the middle of icaR were used to insert the tetracycline resistance cassette. Deleted sequence numbers refer to database sequence U43366.
PIA/PNSG expression is increased in vitro under anaerobic growth conditions
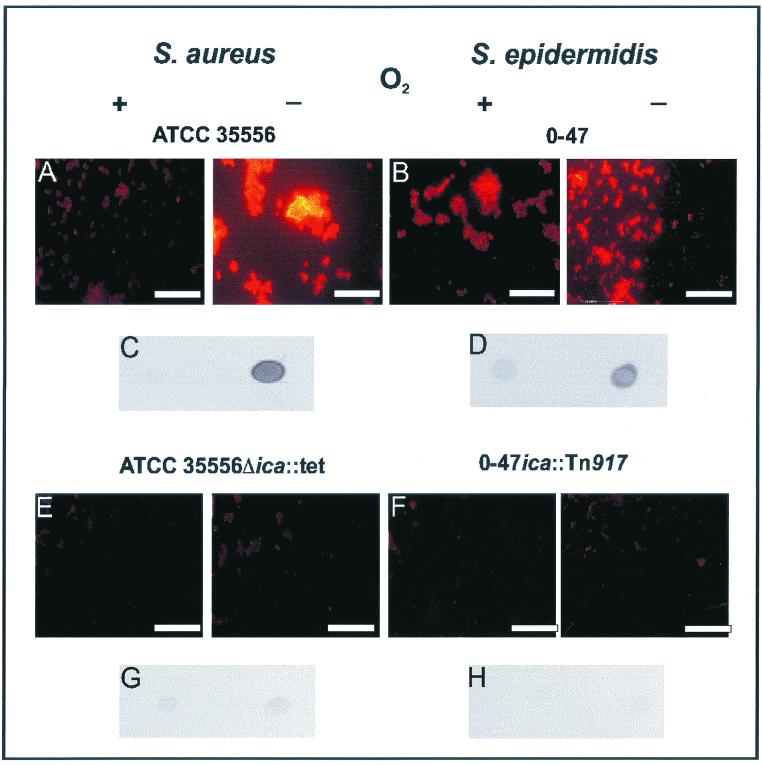
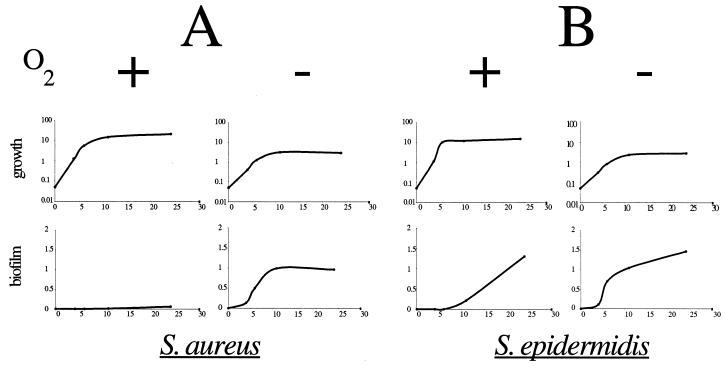
We tested a number of wild-type strains of S. aureus and S. epidermidis and isogenic deletion mutants lacking the ica gene locus for PIA/PNSG production and biofilm formation under aerobic and anaerobic growth conditions in liquid cultures and in polystyrene microtiter plates, respectively, using a polyclonal antibody raised against S. epidermidis PIA (7, 12). In contrast to aerobic growth conditions, anaerobiosis strongly stimulated PIA/PNSG production in ica-positive wild-type strains of S. aureus and S. epidermidis, whereas isogenic ica deletion mutant strains remained PIA/PNSG negative (Fig. 2). As shown in Fig. 2A, for S. aureus ATCC 35556 grown in CYPG medium supplemented with 2% glucose (CYPG plus Glc) for 96 h, PIA/PNSG expression was detectable only under anaerobic conditions. When cell surface extracts from bacteria grown overnight in TSB supplemented with 0.25% glucose (TSB plus Glc) were examined, PIA/PNSG expression was much stronger in cultures grown under anaerobic conditions (Fig. 2C). In contrast to S. aureus, S. epidermidis O-47 expressed PIA/PNSG under both aerobic and anaerobic conditions in CYPG plus Glc after 96 h; however, the expression was much stronger under anaerobic conditions (Fig. 2B). The difference between aerobic and anaerobic expression of PIA/PNSG in cell surface extracts was more dramatic after overnight growth in TSB plus Glc (Fig. 2D). Since PIA/PNSG is required for biofilm formation, we measured biofilm formation over time using an anti-PIA antibody during S. aureus and S. epidermidis growth. Biofilm was formed by S. aureus only under anaerobic conditions (Fig. 3A). In contrast to S. aureus, S. epidermidis produced biofilm under both aerobic and anaerobic conditions; however PIA/PNSG was detectable significantly earlier under anaerobic conditions (Fig. 3B). These data suggest that PIA/PNSG production in S. epidermidis is less stringently regulated by oxygen than in S. aureus and that the amount of PIA/PNSG produced under the aerobic conditions used in this in vitro system is sufficient to mediate biofilm formation.
FIG. 2.
Increased expression of PIA/PNSG under anaerobic conditions in S. aureus and S. epidermidis in vitro. The ica-positive S. aureus strain ATCC 35556 (A), an isogenic ica-deletion mutant (ATCC 35556Δica::tet) (E), the ica-positive S. epidermidis strain O-47 (B), and an isogenic ica transposon mutant (O-47ica::Tn917) (F) were grown under aerobic (+) and anaerobic (−) conditions for 96 h in CYPG plus Glc. PIA/PNSG expression was detected by indirect immunofluorescence using rabbit antibodies raised against S. epidermidis PIA and a Cy3-conjugated goat anti-rabbit IgG antibody. Magnifications for panels A, B, E, and F, ×1,000; bar = 10 μm. Cell surface extracts from S. aureus (C and G) and S. epidermidis (D and H) wild type and isogenic deletion mutants, grown overnight (14 to 18 h) under aerobic or anaerobic conditions in TSB plus Glc, were spotted on nitrocellulose filters, and PIA/PNSG was detected using the same anti-S. epidermidis PIA antibody used for panels A, B, E, and F.
FIG. 3.
Biofilm formation under aerobic and anaerobic conditions. The same S. aureus (A) and S. epidermidis (B) wild-type strains shown in Fig. 2 were grown under aerobic and anaerobic conditions in CYPG plus Glc for up to 24 h in microtiter plates, and biofilm formation was quantified using the S. epidermidis anti-PIA antibody. The growth rate of the strains was determined independently by measuring the OD600 in liquid culture.
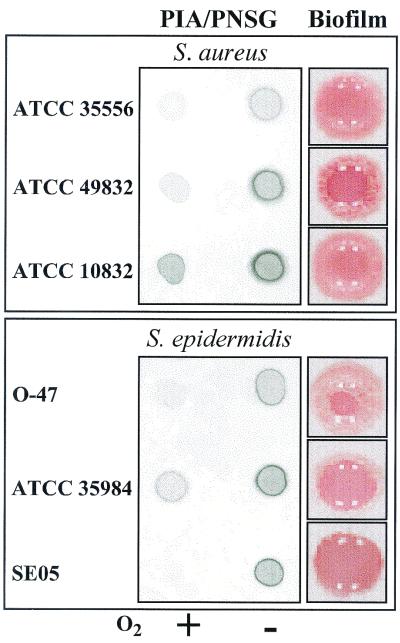
Increased PIA/PNSG expression under anaerobic conditions is a general phenomenon.
We examined PIA/PNSG expression in three representative strains from each species under aerobic and anaerobic conditions. Each of the six strains carries the ica locus (data not shown), expresses PIA/PNSG, and forms a strong in vitro biofilm. The results confirmed that PIA/PNSG production is stimulated by anaerobic growth conditions in multiple representatives of each species (Fig. 4). PIA/PNSG production seems to be very sensitive to the presence of oxygen. Experiments performed in an incubator with a controlled (3% oxygen) environment compared to parallel cultures grown in an incubator with ambient air showed only minimal differences in PIA/PNSG production. In addition, increased CO2 concentrations (1%) in the same experiments did not affect PIA/PNSG expression (data not shown).
FIG. 4.
PIA/PNSG expression is stimulated under anaerobic conditions in six S. aureus and S. epidermidis biofilm-forming strains. Three S. aureus and three S. epidermidis biofilm-forming strains were grown under both aerobic (+) and anaerobic (−) conditions to early stationary phase (14 to 18 h) in TSB plus Glc. PIA/PNSG expression (PIA/PNSG) was detected in cell surface extracts isolated from an equal number of cells from each strain using an antibody raised against S. epidermidis PIA. Biofilm formation in a microtiter plate well is shown for each strain (Biofilm). Adhering cells are stained with safranin (red color) to facilitate visualization of the biofilm.
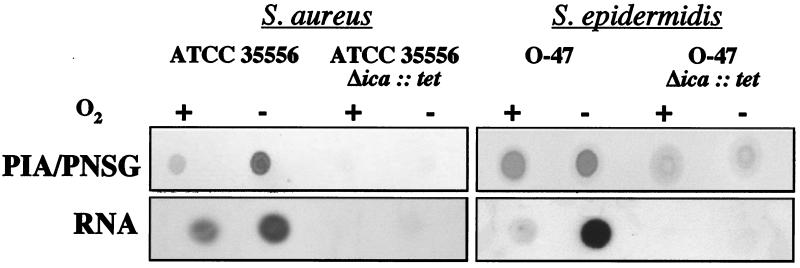
Increased PIA/PNSG expression levels reflect increased RNA levels under anaerobic conditions in vitro.
Total RNA was extracted from S. aureus strain ATCC 35556, S. epidermidis strain O-47, and their respective isogenic ica deletion mutants grown under both aerobic and anaerobic conditions. Low levels of ica-specific transcripts were detected in wild-type cells of both species grown under aerobic conditions; however, much stronger expression was detected in bacteria grown under anaerobic conditions. This increase was reflected in the expression of PIA/PNSG in cell surface extracts prepared from the same cultures (Fig. 5). The relative level of PIA/PNSG expression between aerobic and anaerobic conditions in this S. epidermidis strain was less dramatic under these conditions (both cultures were grown to an OD578 of 2) than when both cultures were allowed to grow to stationary phase (Fig. 2D). RNA levels, however, were dramatically different, suggesting a further layer of regulation of PIA/PNSG production.
FIG. 5.
Increased PIA/PNSG expression under anaerobic conditions correlates with ica operon transcript levels in S. aureus and S. epidermidis. Cell surface extracts from S. aureus ATCC 35556, S. epidermidis O-47, and their respective isogenic ica deletion mutants were grown to an OD578 of 2.0 under aerobic (+) or anaerobic (−) conditions in TSB plus Glc. Cell surface extracts from an equal number of cells from each strain were spotted onto a nitrocellulose filter, and PIA/PNSG was detected using a polyclonal anti-S. epidermidis PIA antibody (PIA/PNSG). RNA was extracted from cells from the same cultures, spotted onto a nylon filter, and hybridized with an ica-specific DNA probe (RNA).
DISCUSSION
Bacterial biofilm formation is of major concern in association with indwelling medical devices, since the biofilm provides bacteria with considerable resistance to host defenses and antimicrobial agents (6, 10). Single bacterial cells can be easily eliminated by macrophages or neutrophils in the healthy host; however, bacterial colonies enclosed in a self-produced polymeric sugar matrix are far more resistant to oxygen radicals and phagocytosis. Consequently, as has been shown using S. epidermidis in animal models, the virulence of S. epidermidis strains that produce polysaccharide is greater than that of polysaccharide-negative S. epidermidis strains (25, 26, 28). The self-produced extracellular polysaccharide that forms a matrix around the bacteria may impair the penetration of antimicrobial agents. Once a biofilm has formed, the low metabolic rate of the bacteria may also limit the effectiveness of antibiotics that require active cell division and active metabolism (15).
Until recently, little has been known about the ability of S. aureus to form a biofilm. Unlike clinical isolates of Pseudomonas aeruginosa from patients with CF (reviewed in reference 8), S. aureus produces very little PIA/PNSG in vitro on culture plates but produces predominantly polysaccharide microcapsules of type 5 or 8 (1, 14, 27, 29). Due to this in vitro phenotype, most investigators have thought that S. aureus would also express CP5 or CP8 during infections in animals or humans. Only recently was it shown that CP5 expression is in fact reduced in the lungs of CF patients (13) and that PNSG expression is increased (20). Apparently, PNSG production by S. aureus is not restricted to the airways of patients with CF, because the polysaccharide was also detected in a mouse renal infection model using immunoelectron microscopy and ELISA (20).
Altogether, although both S. epidermidis and S. aureus are now known to produce PIA/PNSG in vivo during human and animal infections, little is known about the environmental factor(s) that triggers this expression. Here, we provide evidence that at least one environmental stimulus responsible for increased PIA/PNSG expression is lack of oxygen. This notion is based on our findings showing that in vitro anaerobic growth conditions trigger increased ica gene transcription and PIA/PNSG expression by S. aureus and S. epidermidis strains that carry the ica gene locus as detected by RNA blotting and specific antibodies raised against S. epidermidis PIA. This does not mean that the strains tested produced no polysaccharide product under aerobic conditions; our data show that production is stimulated under anaerobic conditions, an increase that may be at least partially attributable to transcriptional regulation.
The anaerobic stimulation of extracellular polysaccharide has been confirmed using two different types of medium and three different methods for generating anaerobic conditions. Our assays measured ica transcription, PIA/PNSG production, and biofilm formation. Findings by Barker et al. (3), who showed that undefined coagulase-negative bacteria form biofilms only under aerobic conditions, may be explained by differences in the organisms tested and the assay(s) employed.
While some staphylococcal strains are able to form an in vitro biofilm, others are not (3, 7). We investigated approximately 17 S. epidermidis and 41 S. aureus strains in the course of this study and found that, for those strains that produce PIA/PNSG, PIA/PNSG production is stimulated by anaerobic conditions. PIA/PNSG production was observed in approximately the same proportion of strains as reported by McKenney et al. to produce PNSG (reference 20 and data not shown). This does not necessarily mean that apparently PIA/PNSG-negative strains produce no PIA/PNSG or PIA/PNSG-like product(s), however. Support for this idea stems from our observation that a few biofilm-positive strains transcribe ica-specific RNA but produce no detectable PIA/PNSG (data not shown). Although the ica locus appears to be transcribed in these strains, the encoded Ica proteins may not be translated or may contain mutations or truncations that render them unable to produce mature PIA/PNSG. This would imply that these strains are able to form in vitro biofilms in a PIA/PNSG-independent manner. This observation is also supported by the finding of Muller et al. (22) that a few S. epidermidis strains that are able to form a biofilm apparently produce no polysaccharide. Alternatively, it is possible that PIA/PNSG is modified, for example, (de)acetylated or (de)succinylated, in a manner such that our antibody(ies) no longer recognizes the antigen(s) produced by these strains. The fact that antibodies raised against S. epidermidis PIA or S. aureus PNSG detect both antigens implies that the chemical structures of PIA and PNSG are identical or very similar. A direct structural comparison has not been made to date, and the possibility of other, perhaps strain-specific, modifications to the glucosamine backbone cannot be eliminated. Nevertheless, immunological cross-reactivity was observed in animal experiments where animals actively immunized with the polysaccharide antigen were protected from a challenge with S. epidermidis (31) and S. aureus (20).
In summary, an anaerobic environment stimulates PIA/PNSG production in both S. aureus and S. epidermidis. Anaerobic environments may develop in localized infections and stimulate expression of this virulence factor by both pathogens in vivo. PIA/PNSG production and biofilm formation pose a considerable risk for the patient. The elucidation of the molecular mechanism(s) of biofilm formation may lead to better tools for clinical intervention in the future.
ACKNOWLEDGMENTS
We are grateful to Dietrich Mack, Hamburg, Germany, for a rabbit antibody against PIA and Gerald B. Pier for a rabbit antibody against PNSG. The technical assistance of Ulrike Pfitzner and Mulugeta Nega is gratefully acknowledged.
S.E.C. was supported in part by NRSA Postdoctoral Fellowship AI09626 from the National Institute of Allergy and Infectious Diseases. This project was supported in part by the German Bundesministerium für Bildung, Wissenschaft, Forschung und Technologie (DLR: 01KI9751/1).
REFERENCES
- 1.Albus A, Fournier J M, Wolz C, Boutonnier A, Ranke M, Hoiby N, Hochkeppel H, Döring G. Staphylococcus aureus capsular types and antibody response to lung infection in patients with cystic fibrosis. J Clin Microbiol. 1988;26:2505–2509. doi: 10.1128/jcm.26.12.2505-2509.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arvidson S. Extracellular enzymes from Staphylococcus aureus. In: Easmon C S F, Adlam C, editors. Staphylococci and staphylococcal infections. London, United Kingdom: Academic Press; 1983. pp. 745–808. [Google Scholar]
- 3.Barker L P, Simpson W A, Christensen G D. Differential production of slime under aerobic and anaerobic conditions. J Clin Microbiol. 1990;28:2578–2579. doi: 10.1128/jcm.28.11.2578-2579.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brückner R. Gene replacement in Staphylococcus carnosus and Staphylococcus xylosus. FEMS Microbiol Lett. 1997;151:1–8. doi: 10.1111/j.1574-6968.1997.tb10387.x. [DOI] [PubMed] [Google Scholar]
- 5.Christensen G D, Bisno A L, Parisi J T, McLaughlin B, Ester M G H, Luther R W. Nosocomial septicemia due to multiply-resistant Staphylococcus epidermidis. Ann Intern Med. 1982;96:1–10. doi: 10.7326/0003-4819-96-1-1. [DOI] [PubMed] [Google Scholar]
- 6.Costerton J W, Stewart P S, Greenberg E P. Bacterial biofilms: a common cause of persistent infections. Science. 1999;284:1318–1322. doi: 10.1126/science.284.5418.1318. [DOI] [PubMed] [Google Scholar]
- 7.Cramton S E, Gerke C, Schnell N F, Nichols W W, Götz F. The intercellular adhesion (ica) locus is present in Staphylococcus aureus and is required for biofilm formation. Infect Immun. 1999;67:5427–5433. doi: 10.1128/iai.67.10.5427-5433.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Döring G, Knight R, Bellon G. Immunology of cystic fibrosis. In: Hodson M E, Geddes G, editors. Cystic fibrosis. London, United Kingdom: Chapman and Hall; 1995. pp. 99–129. [Google Scholar]
- 9.Gerke C, Kraft A, Süßmuth R, Schweitzer O, Götz F. Characterization of the N-acetylglucosaminyltransferase activity involved in the biosynthesis of the Staphylococcus epidermidis polysaccharide intercellular adhesin (PIA) J Biol Chem. 1998;273:18586–18593. doi: 10.1074/jbc.273.29.18586. [DOI] [PubMed] [Google Scholar]
- 10.Götz F, Peters G. Colonization of medical devices by coagulase-negative staphylococci. In: Waldvogel F A, Bisno A L, editors. Infections associated with indwelling medical devices. 3rd ed. Washington, D.C.: ASM Press; 2000. pp. 55–88. [Google Scholar]
- 11.Heilmann C, Gerke C, Perdreau-Remington F, Götz F. Characterization of Tn917 insertion mutants of Staphylococcus epidermidis affected in biofilm formation. Infect Immun. 1996;64:277–282. doi: 10.1128/iai.64.1.277-282.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heilmann C, Schweitzer O, Gerke C, Vanittanakom N, Mack D, Götz F. Molecular basis of intercellular adhesion in the biofilm-forming Staphylococcus epidermidis. Mol Microbiol. 1996;20:1083–1091. doi: 10.1111/j.1365-2958.1996.tb02548.x. [DOI] [PubMed] [Google Scholar]
- 13.Herbert S, Worlitzsch D, Dassy B, Boutonnier A, Founier J M, Bellon G, Dalhoff A, Döring G. Regulation of Staphylococcus aureus capsular polysaccharide type 5: CO2 inhibition in vitro and in vivo. J Infect Dis. 1997;176:431–438. doi: 10.1086/514061. [DOI] [PubMed] [Google Scholar]
- 14.Hochkeppel H K, Broun D G, Vischer W, Imm A, Sutter S, Staeubli U, Guggenheim R, Kaplan E L, Boutonnier A, Fournier J M. Serotyping and electron microscopy studies of Staphylococcus aureus clinical isolates with monoclonal antibodies to capsular polysaccharide types 5 and 8. J Clin Microbiol. 1987;25:526–530. doi: 10.1128/jcm.25.3.526-530.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoyle B D, Costerton J W. Bacterial resistance to antibiotics: the role of biofilms. Prog Drug Res. 1991;37:91–105. doi: 10.1007/978-3-0348-7139-6_2. [DOI] [PubMed] [Google Scholar]
- 16.Iordanescu S, Surdeanu M. Two restriction and modification systems in Staphylococcus aureus NCTC 8325. J Gen Microbiol. 1976;96:277–281. doi: 10.1099/00221287-96-2-277. [DOI] [PubMed] [Google Scholar]
- 17.Lowy F D. Staphylococcus aureus infections. N Engl J Med. 1998;339:520–532. doi: 10.1056/NEJM199808203390806. [DOI] [PubMed] [Google Scholar]
- 18.Mack D, Fischer W, Krokotsch A, Leopold K, Hartmann R, Egge H, Laufs R. The intercellular adhesin involved in biofilm accumulation of Staphylococcus epidermidis is a linear β-1,6-linked glucosaminoglycan: purification and structural analysis. J Bacteriol. 1996;178:175–183. doi: 10.1128/jb.178.1.175-183.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mack D, Haeder M, Siemssen N, Laufs R. Association of biofilm production of coagulase-negative staphylococci with expression of a specific polysaccharide intercellular adhesin. J Infect Dis. 1996;174:881–884. doi: 10.1093/infdis/174.4.881. [DOI] [PubMed] [Google Scholar]
- 20.McKenney D, Pouliot K L, Wang Y, Murthy V, Ulrich M, Döring G, Lee J C, Goldmann D A, Pier G B. Broadly protective vaccine for Staphylococcus aureus based on an in vivo-expressed antigen. Science. 1999;284:1523–1527. doi: 10.1126/science.284.5419.1523. [DOI] [PubMed] [Google Scholar]
- 21.Mekalanos J J. Environmental signals controlling expression of virulence determinants in bacteria. J Bacteriol. 1992;174:1–7. doi: 10.1128/jb.174.1.1-7.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Muller E, Takeda S, Shiro H, Goldmann D, Pier G B. Occurrence of capsular polysaccharide/adhesin among clinical isolates of coagulase-negative staphylococci. J Infect Dis. 1993;168:1211–1218. doi: 10.1093/infdis/168.5.1211. [DOI] [PubMed] [Google Scholar]
- 23.Novick R P. Genetic systems in staphylococci. Methods Enzymol. 1991;204:587–636. doi: 10.1016/0076-6879(91)04029-n. [DOI] [PubMed] [Google Scholar]
- 24.Peters G, Locci R, Pulverer G. Microbial colonization of prosthetic devices. II. Scanning electron microscopy of naturally infected intravenous catheters. Zentbl Bakteriol Abt 1 Orig B. 1981;172:293–299. [PubMed] [Google Scholar]
- 25.Rupp E M, Ulphani J S, Fey P D, Bartscht K, Mack D. Characterization of the importance of polysaccharide intercellular adhesin/hemagglutinin of Staphylococcus epidermidis in the pathogenesis of biomaterial-based infection in a mouse foreign body infection model. Infect Immun. 1999;67:2627–2632. doi: 10.1128/iai.67.5.2627-2632.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rupp E M, Ulphani J S, Fey P D, Mack D. Characterization of Staphylococcus epidermidis polysaccharide intercellular adhesin/hemagglutinin in the pathogenesis of intravascular catheter-associated infection in a rat model. Infect Immun. 1999;67:2656–2659. doi: 10.1128/iai.67.5.2656-2659.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ryding U, Flock J I, Soderquist B, Christensson B. Expression of collagen-binding protein and types 5 and 8 capsular polysaccharide in clinical isolates of Staphylococcus aureus. J Infect Dis. 1997;176:1096–1099. doi: 10.1086/516520. [DOI] [PubMed] [Google Scholar]
- 28.Shiro H, Muller E, Gutierrez N, Boisot S, Grout M T T D, Goldmann D, Pier G B. Transposon mutants of Staphylococcus epidermidis deficient in elaboration of capsular polysaccharide/adhesin and slime are avirulent in a rabbit model of endocarditis. J Infect Dis. 1994;169:1042–1049. doi: 10.1093/infdis/169.5.1042. [DOI] [PubMed] [Google Scholar]
- 29.Sompolinsky D, Samra Z, Karakawa W W, Vann W F, Schneerson R, Malik Z. Encapsulation and capsular types in isolates of Staphylococcus aureus from different sources and relationship to phage types. J Clin Microbiol. 1985;22:828–834. doi: 10.1128/jcm.22.5.828-834.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sussenbach J S, Monfoort C H, Schiphof R, Stobberingh E E. A restriction endonuclease from Staphylococcus aureus. Nucleic Acids Res. 1976;3:3193–3202. doi: 10.1093/nar/3.11.3193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Takeda S, Pier G B, Kojima Y, Tojo M, Muller E, Tosteson T, Goldmann D A. Protection against endocarditis due to Staphylococcus epidermidis by immunization with capsular polysaccharide/adhesin. Circulation. 1991;84:2539–2546. doi: 10.1161/01.cir.84.6.2539. [DOI] [PubMed] [Google Scholar]