Abstract
Background
The COVID-19 pandemic has posed unprecedented challenges for societies. Emerging data have indicated that the younger population are the most vulnerable group to the development of mental health problems during this pandemic. The present study aimed to examine the effects of the changes in health behaviors on mental health problems to identify an at-risk group among adolescents and young adults.
Methods
In the present cross-sectional study, secondary school students (N = 2556) ages 15–21 years participated in Hungary. A self-report questionnaire was developed to measure the changes in health behaviors. Mental health problems were measured by the Beck Hopelessness Scale and the 20-item UCLA Loneliness Scale.
Results
A significant proportion of the students showed moderate/severe hopelessness or high loneliness which were more pronounced among adolescent females. An at-risk group was identified among adolescents and young adults. Students who have a lower number of friends, spend less time in front of a screen, and feel lonely often/very often are more likely to have moderate/severe hopelessness with high loneliness.
Limitations
All data were collected online, and students completed the questionnaires voluntarily. Cross-sectional, non-preregistered study.
Conclusions
Loneliness and hopelessness were prevalent in the young population during the COVID-19 pandemic. The at-risk group of adolescents characterized by moderate/severe hopelessness with high loneliness highlights the need for follow-up mental health to avoid future poor mental and physical health. It is also recommended to develop effective interventions targeted to gender and age, with the promotion of resiliencies and buffers against vulnerabilities of negative life events.
Keywords: Loneliness, Hopelessness, Adolescents, Young adults, Risk group, COVID-19 pandemic
1. Background
The SARS-CoV-2 coronavirus pandemic (COVID-19) has overall health, social and economic consequences. The pandemic has disrupted normal daily routines worldwide including attendance teaching among children and adolescents, and across all age groups, depending on the degree of vulnerability (Mazza et al., 2020).
During the first wave of COVID-19, all schools were closed from March 16, 2020, until the end of the school year, June 15, 2020, in Hungary. Educational institutions were instructed to suspend in-person class attendance and switch to online e-learning and education. Then, during the second and third waves of the COVID-19, the secondary schools were closed again from 12 November 2020, and education was completely switched to online education until May 10, 2021 (Monostori, 2021). The government announced further strict community restrictions on November 10, 2020, which was extended until March 29, 2021. Under the measures introduced on 26 November 2020, a digital timetable has been introduced in secondary education from grade 9 in Hungary. Students were home-bound and digital class attendance was required between 8 a.m.–4 p.m. on school days (Ministry of Justice, 2020). Restaurants, and cultural and leisure establishments were closed, and gatherings were banned in general. There was also a night-time curfew between 8 p.m. until 5 a.m. In this term, individual outdoor activities were allowed considering the restrictions of gathering, and competitive athletes were not restricted in their activities.
The COVID-19 pandemic has posed unprecedented challenges for societies. Since the pandemic began, we are living under social restrictions to reduce the spread of the COVID-19 virus. Living under some community lockdowns for a longer or shorter period and learning in distance education or working in a home office have had negative effects on the daily routine, social contacts, and the normal way of life of the families. It is not surprising that this situation has led to the development of psychological problems or diseases such as low mood, insomnia, depression, post-traumatic stress disorder, anxiety, anger, irritability, and loneliness in a wide range of society. There are further factors that had increased the risk of the development of mental health problems during the pandemic in the population such as sociodemographic and occupational factors, pre-existing mental health problems, as well as a longer period of social isolation (Duan and Zhu, 2020; Morelli et al., 2020).
Vulnerable groups such as adolescents/young adults and older adults have anticipated that they would have a higher risk of the negative psychological impacts of COVID-19. There is a lot of study on adults and older adults on mental health consequences during lockdown and restrictions. However, emerging data have indicated that the younger population is the most vulnerable group to the development of mental health problems during this pandemic (McQuaid et al., 2021), especially with pre−/ existing psychopathological symptoms (Essau and de la Torre-Luque, 2021). Most of the studies demonstrated longitudinal deterioration in the mental health of the young population with increased depression and anxiety symptoms, psychological distress, negative affect, decreased mental well-being and increased loneliness (Loades et al., 2020; Rogers et al., 2021; Cooper et al., 2021; Ludwig-Walz et al., 2022; Cénat et al., 2022), especially for early and late adolescence (Kauhanen et al., 2022; Ludwig-Walz et al., 2022). Home isolation and social distancing (Loades et al., 2020), lack of prosocial/physical activity (Mittal et al., 2020), family stress and heightened concerns (Meade, 2021), increased screen time (Duan et al., 2020), etc. have contributed to adolescents' and young adults' mental health worldwide (Cao et al., 2020; McElroy et al., 2020; Zhou et al., 2020). Examining the global evolution of mental health problems during the COVID-19 pandemic, a spike was detected when social isolation, school closures and confinement occurred (Cénat et al., 2022).
The present study aims to examine the mental health status of adolescents and young adults during distance learning education in Hungary. In this study, we focused on the relationship between mental health, especially the level of loneliness and hopelessness, and changes in physical activity, screen time, self-rated health status, sleep time, and well-being. A further aim was to identify an at-risk group for mental health problems among adolescents and young adults who may currently face serious challenges in social life and education.
2. Methods and materials
2.1. Participants
In a cross-sectional study design, secondary school students (N = 2556) in 66 public education institutions in 37 cities were surveyed from nine regions in Hungary. A total of 48 students were excluded from the study sample because of missing data or lack of parental agreement. The age of secondary school-going students is between 15 and 21 years, depending on the form and type of education in Hungary.
2.2. Survey
A cross-sectional self-report questionnaire based on the Health Behavior of School-aged Children (HBSC) (hbsc, 2006) and the Youth Risk Behavior Survey (YRBSS) (Grunbaum et al., 2004) created by the Centers for Diseases Control (CDC) was developed. Some questions were modified during versus before the COVID-19 pandemic lockdown periods. Besides demographics (gender, age), body mass index (BMI) was calculated by weight and height, we used BMI Z scores during the analysis.
From the questionnaire, in the present study, we used the following variables related to mental health issues in adolescents and young adults: moderate-to-vigorous physical activity, screen time, self-rated health, sleep time, well-being, close friends, and self-rated loneliness evaluated before and during the distance learning period.
Moderate-to-Vigorous Physical Activity and Screen Time were measured on a 0–7-point scale. Moderate-to-Vigorous Physical Activity was assessed by sets of questions in pairs such as for aerobic exercise “On how many days per week did you exercise or participate in physical activity for at least 20 min that made you sweat and breathe hard, such as basketball, soccer, running, swimming laps, fast bicycling, fast dancing, or similar aerobic activities before distance learning period?” and “On how many days per week do you…during distance learning period?”. For muscle-strengthening with the question pairs “On how many days per week did you do exercises to strengthen or tone your muscles, such as push-ups, sit-ups, or weightlifting before distance learning period?” and “On how many days per week do you…during distance learning period?”. To measure spending time in front of a screen, we also used question pairs such as “On how many days per week did you spend time in front of a screen (television, notebook, smartphone) in the evenings before distance learning period?” and “On how many days per week do you…during distance learning period?”. Moderate-to-Vigorous Physical Activity and Screen Time were measured on a 0–7-point scale. The change (days/week) in these variables was calculated with days/week during distance education minus days/week before distance education (from −7 to +7 days = week, 0 means no changes). Based on the Moderate-to-Vigorous Physical Activity change, we used the no change, increased, and decreased aerobic exercise/muscle strengthening categories in models.
Self-rated health was assessed with the questions of “Would you say your health was/is…?” (excellent, good, fair/poor) before and during the distance learning period. Change in SH was examined on a contingency table, classified participants into no change, decreased or increased categories on self-rated health. Self-rated sleep duration was assessed with the questions of “How many hours did/do you sleep…?” (<7 h, between 7 and 8 h, 9 h, or >10 h) before and during the distance learning period. Similar to other variables, we classified participants into no change, decreased or increased categories on self-rated sleep duration. Change in well-being was evaluated with the statement of “I feel less well now, during the distance learning period than before the distance learning period” (agree, disagree, same). The number of close friends was measured with the question of “At present, how many close male and female friends do you have?”. Self-rated Loneliness was assessed with the question of “Do you feel lonely?” (no, sometimes, often, very often). No one answered with “no”. Thus, we examined the groups of sometimes versus often and very often lonely.
To measure mental health problems, i.e., problems in the affective-emotional aspects of mental health, we used the Beck Hopelessness Scale (BHS) (Beck and Steer, 1988; Beck et al., 1974; Perczel Forintos et al., 2001) which is a self-report measure of the three primary aspects of hopelessness: feeling about future, decreases in motivation, and expectations. The higher the total BHS score reflects higher levels of hopelessness. On the total BSH score, normal range (0–3), mild (4–8), moderate (9–14), and severe (>14) hopelessness categories can be determined (Beck and Steer, 1988; Perczel Forintos et al., 2001). For loneliness, the 20-item UCLA Loneliness Scale (UCLA-LS20) was used (Version 3) (Russell et al., 1978; Russell, 1996) to measure the unpleasant experience, when an individual perceives their social network as insufficient, i.e., a perceived discrepancy between the actual and the ideal/desired social networks/contacts (Peplau and Perman, 1979). On the total UCLA-LS 20 score, the following loneliness severity cut-offs were used: no/low (≤28), moderate (28–43), and high (>43) (Cacioppo and Patrick, 2008).
2.3. Procedure
The 15-min online survey was shared on a web page and was accessible for six weeks during the lockdown, distance learning period. Our research team was in touch with school principals and physical education teachers, who encouraged the students to complete the survey. The students completed the survey primarily during online physical education lessons. Information about the aims of the research was given online and parental consent was requested before completion, students were excluded who did not have parental consent or submitted a negative parental response. This research was non-preregistered, it was approved by the Ethical Committee of the Medical Research Council (TUKEB), Hungary, under ETK TUKEB ethical permission No. IV/3067- 3/2020/EKU.
2.4. Data analysis
Frequencies and percentages for categorical variables and means calculations with their corresponding standard deviations (SD) for continuous variables were reported. Gender and age differences were examined by independent samples t-test with Hedges' g effect size. Associations between age/ gender and categorical variables were examined by calculating Pearson's chi-square test (crosstabs) with Cramer's V effect size. Binary and multinomial logistic regression models were used to ascertain the effects of gender, age, BMI Z Score, change in aerobic exercise, muscle strengthening, screen time, self-rated health, self-rated sleep duration, the number of close friends, well-being and self-rated loneliness on the likelihood that participants have mental health problems. First, univariate logistic regression models were built for each of the independent variables (that were either dichotomized or scaled). Then, all variables were entered into a final multivariate logistic regression model. Univariate odds ratios (OR) and multivariate-adjusted odds ratios (aOR) with their corresponding 95 % confidence intervals (95 % CI) were reported. A multinomial logistic regression model was used to examine the association between mental health problems, loneliness and/or hopelessness, and the outcomes of interest. For the regression model, the p-value was calculated using a two-tailed Wald z-test. The level of significance was set a priori at 0.05. Statistical analysis and visualization were conducted using IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp. Released 2017. Armonk, NY, USA: IBM Corp).
3. Results
3.1. Characteristics of the sample
A total of 2508 secondary school students participated in the survey, 42.7 % males. We classified students based on their age into two groups, adolescents (n = 1413, min-maxage = 14-17 yr,) and young adults (n = 1095, min-maxage = 18–21 yr). Age showed a non-significant association with gender. BMI categories revealed a significant association with age and gender. A higher proportion of young adults and males was in the overweight/obese, and obese BMI categories. Characteristics of the sample, see in Table 1 .
Table 1.
Characteristics of the sample (N = 2508).
| Variables | Adolescents (n = 1413) | Young adults (n = 1095) | p [ES] | Males (n = 1072) | Females (n = 1436) | p [ES] |
|---|---|---|---|---|---|---|
| Gender, Male n (%) | 621(43.9) | 451(41.2) | 0.167a [0.03] |
N/A | N/A | N/A |
| Age, M ± SD | 16.3 ± 0.7 | 18.6 ± 0.6 | N/A | 17.3 ± 1.3 | 17.3 ± 1.3 | 0.798b |
| Weight (kg) | 63.3 ± 13.6 | 66.6 ± 14.5 | N/A | 71.4 ± 14.7 | 59.8 ± 11.3 | N/A |
| Height (cm) | 171.2 ± 9.3 | 171.9 ± 9.5 | N/A | 178.6 ± 7.7 | 166.2 ± 6.5 | N/A |
| BMI categories1, n (%) | ||||||
| Underweight | 89(6.3) | 40(3.7) | <0.001c [0.10] |
55(5.1) | 74(5.2) | < 0.001c [0.10] |
| Normal weight | 1146(81.1) | 856(78.2) | 817(76.2) | 1185(82.5) | ||
| Overweigth/obese** | 123(8.7) | 131(11.9) | 142(13.3) | 112(7.8) | ||
| Obese | 55(3.9) | 68(6.2) | 58(5.4) | 65(4.5) |
Notes. 1BMI categories based on BMI %ile for 2–19 yr, and on BMI score for ≥20 yr, ** ‘overweight/obese’ terminology based on: Barlow SE and the Expert Committee 2007, [ES]: effect size, a Fisher's exact test for association between gender and age-groups with [Phi], b Independent Samples T-Test for differences between males and females, c Pearson's chi-square test for association between gender/age-groups and BMI categories with [Cramer's V], N/A statistical analysis is not applicable.
3.2. Hopelessness and loneliness among adolescents and young adults during the distance learning period
In sum, nearly half of the students showed mild hopelessness (57.2 %, n = 1435) and moderate loneliness (59.8 %, n = 1500). Further nearly one-fifth were characterized by moderate/severe hopelessness (18 %, n = 451) and a quarter by high loneliness (24.9 %, n = 624). Among adolescents were significant differences in proportions by gender. Moderate/severe hopelessness and moderate/high loneliness showed higher proportions among adolescent females than males (Table 2 ).
Table 2.
Hopelessness and loneliness among adolescents and young adults by gender.
| Total sample (N = 2508) |
||||||
|---|---|---|---|---|---|---|
| Adolescents (n = 1413) |
Young adults (n = 1095) |
|||||
| Variables | Males (n = 621) | Females (n = 792) | p [ES] | Males (n = 451) | Females (n = 644) | p [ES] |
| Beck hopelessness scale, M ± SD | 5.5 ± 3.1 | 6.0 ± 3.5 | 0.004 [0.15]a | 5.9 ± 3.4 | 6.3 ± 3.5 | 0.070 [0.12]a |
| Normal range, n(%) | 172(27.8) | 205(25.9) | 0.047 [0.08]b | 103(22.8) | 142(22.0) | 0.461 [0.05]b |
| Mild | 353(56.8) | 448(56.6) | 269(59.7) | 364(56.7) | ||
| Moderate | 89(14.3) | 112(14.1) | 65(14.4) | 116(18.0) | ||
| Severe | 7(1.1) | 27(3.4) | 14(3.1) | 21(3.3) | ||
| UCLA Loneliness Scale, M ± SD | 35.9 ± 9.6 | 37.9 ± 10.1 | <0.001 [0.20]a | 37.4 ± 10.1 | 38.0 ± 9.6 | 0.376 [0.06]a |
| No/low, n(%) | 130(20.9) | 111(14.0) | 0.003 [0.09]b | 68,815.1 | 75(11.6) | 0.153 [0.06]b |
| Moderate | 344(55.4) | 485(61.2) | 263(58.3) | 408(63.4) | ||
| High | 147(23.7) | 196(24.8) | 120(26.6) | 161(25.0) | ||
Notes. [ES]: effect size.
Hedges's g.
Cramer's V.
There is a significant, positive moderate correlation between hopelessness and loneliness (rho(2506) = 0.458, p < 0.001) regardless of gender and age.
3.3. Univariate and multivariate analysis for hopelessness and loneliness
Binary logistic regression models were built to analyze the relationship between changes in physical activity (aerobic exercise/muscle strengthening), screen time, self-rated health, self-rated sleep duration, well-being, the number of close friends, and self-rated loneliness and hopelessness or loneliness adjusted by gender, age, and BMI.
In the final multivariate analysis for hopelessness and loneliness, less amount of time spent in front of a screen, a lower number of friends, and feeling lonely often/very often were an increase the likelihood of moderate/severe hopelessness or high loneliness. The model explained 15 % (Nagelkerke R2) of the variance of hopelessness, and correctly classified 83.6 % of cases. Table 3 showed the results of the models. The model of loneliness explained 27.4 % (Nagelkerke R2) of the variance, and correctly classified 80.7 % of cases. Table 3 showed the results of the models.
Table 3.
Univariate and multivariate analysis for hopelessness and loneliness.
| Hopelessness |
Loneliness |
|||
|---|---|---|---|---|
| Characteristics | Univariate |
Multivariate |
Univariate |
Multivariate |
| OR (95%CI) | aOR (95%CI) | OR (95%CI) | aOR (95%CI) | |
| Gender | ||||
| Male | Ref | Ref | Ref | Ref |
| Female | 1.2 [1.0–1.5] | 1.2 [0.9–1.5] | 1.0 [1.8–1.2] | 0.9 [0.7–1.1] |
| Age | ||||
| Adolescents | Ref | Ref | Ref | Ref |
| Young adults | 1.2 [1.0–1.5] | 1.2 [1.0–1.6] | 1.1 [0.9–1.3] | 1.2 [0.9–1.4] |
| BMI Zscore | 1.1 [1.0–1.3] | 1.1 [0.9–1.2] | 1.1 [1.0–1.2] | 1.1 [1.0–1.2] |
| Aerobic exercise | ||||
| No change | Ref | Ref | Ref | Ref |
| Decreased | 1.3 [1.0–1.6] | 1.1 [0.8–1.5] | 1.1 [0.8–1.3] | 0.9 [0.7–1.3] |
| Increased | 1.1 [0.8–1.6] | 0.9 [0.6–1.4] | 1.3 [0.9–1.7] | 0.9 [0.6–1.4] |
| Muscle strengthening | ||||
| No change | ref | ref | ref | ref |
| Decreased | 1.4 [1.1–1.8] | 1.2 [0.9–1.6] | 1.1 [0.9–1.3] | 0.9 [0.7–1.2] |
| Increased | 1.2 [0.9–1.6] | 1.1 [0.8–1.6] | 1.3 [1.0–1.6] | 1.2 [0.8–1.6] |
| Screen time | ||||
| No change | Ref | Ref | Ref | Ref |
| Decreased | 1.7 [1.1–2.8] | 2.1 [1.2–3.5] | 1.5 [1.1–2.0] | 1.9 [1.1–3.2] |
| Increased | 0.9 [0.8–1.1] | 0.9 [0.7–1.1] | 1.2 [0.9–1.5] | 0.8 [0.6–1.0] |
| Self-rated health status | ||||
| No change | Ref | Ref | Ref | Ref |
| Decreased | 1.4 [1.1–1.8] | 1.1 [0.8–1.5] | 1.5 [1.2–1.8] | 1.3 [1.0–1.7] |
| Increased | 1.1 [0.8–1.6] | 1.0 [0.7–1.6] | 1.5 [1.1–2.1] | 1.3 [0.9–1.9] |
| Self-rated sleep duration | ||||
| No change | Ref | Ref | Ref | Ref |
| Decreased | 1.5 [1.1–2.0] | 1.3 [0.9–1.8] | 1.2 [0.9–1.6] | 1.0 [0.7–1.4] |
| Increased | 1.2 [0.9–1.5] | 1.0 [0.7–1.6] | 1.0 [0.8–1.2] | 1.0 [0.8–1.3] |
| Number of close friends | 1.6 [1.6–1.7] | 1.7 [1.6–1.8] | 1.4 [1.4–1.5] | 1.5 [1.4–1.5] |
| Well-being | ||||
| No change | Ref | Ref | Ref | Ref |
| Decreased | 1.4 [1.1–1.7] | 1.1 [0.8–1.4] | 1.3 [1.1–1.6] | 1.1 [0.8–1.4] |
| Increased | 0.9 [0.7–1.3] | 1.0 [0.7–1.4] | 1.1 [0.9–1.4] | 1.0 [0.7–1.4] |
| Self-rated loneliness | ||||
| Sometimes | Ref | Ref | Ref | Ref |
| Often | 5.3 [4.0–7.1] | 4.4 [3.2–6.0] | 6.8 [5.1–9.0] | 6.5 [4.7–9.0] |
| Very often | 8.6 [5.9–12.7] | 6.5 [4.3–9.8] | 15.0 [9.6–23.3] | 13.9 [8.6–22.6] |
Notes. OR: odds ratio, aOR: multivariate-adjusted odds ratio, 95%CI: confidence interval, ref.: reference group.
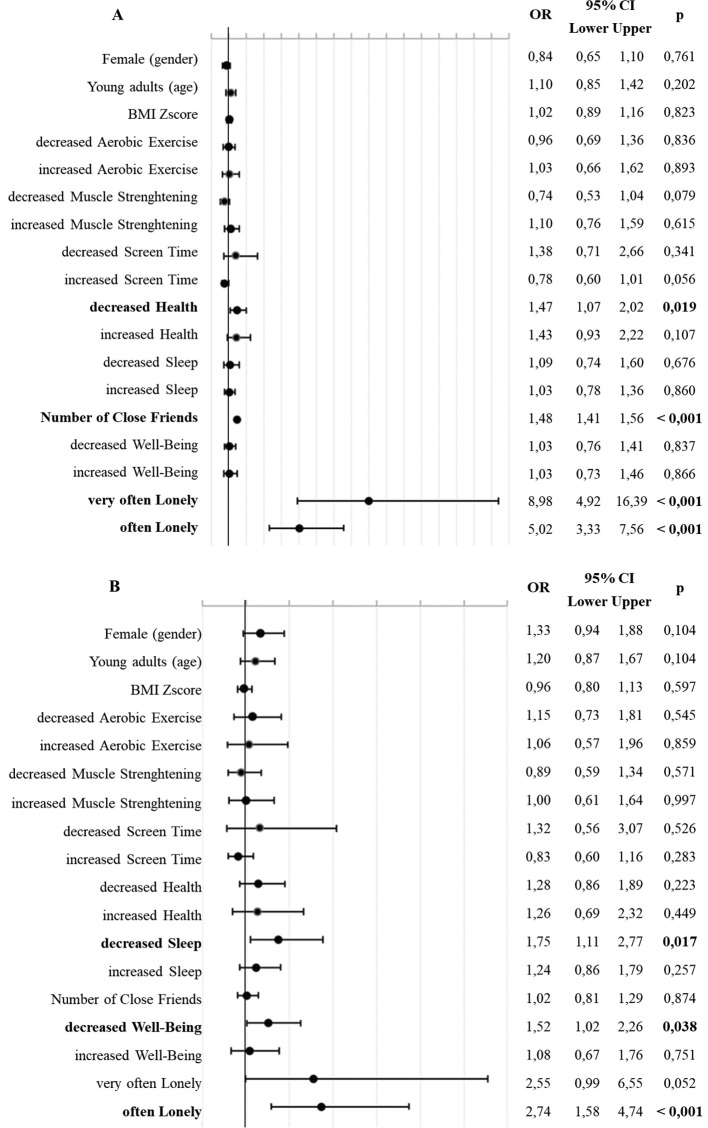
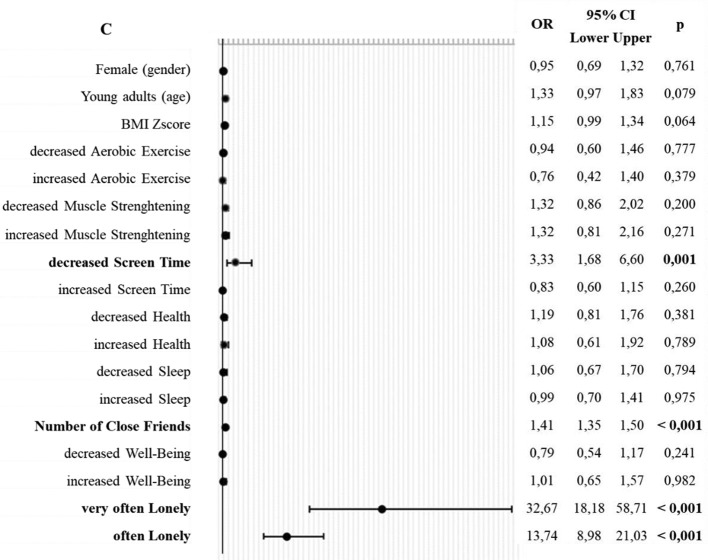
3.4. Multinomial logistic regression model for mental health risk
We classified participants into four categories according to the scores of hopelessness and loneliness. The first group (n = 1693, 67.5 %) can be considered ‘mentally healthy’ in the sense that it is characterized by no, low/moderate loneliness AND normal/mild hopelessness. The participants in the second group, the ‘hopelessness’ group, show moderate/severe hopelessness AND no, low/moderate loneliness (n = 191, 7.6 %). The third group was the ‘loneliness’ group including people characterized by high loneliness AND normal/mild hopelessness (n = 364, 14.5 %). Finally, people with high loneliness AND moderate/severe hopelessness form a group at particular risk for mental health problems.
A multinomial regression model was used to determine the effect of the outcomes of interest and mental health groups. Based on the result, a lower number of close friends, a decreased self-rated health status, and feeling lonely often/very often were associated with high loneliness. Decreased sleep duration, decreased well-being, and feeling lonely often were associated with moderate/severe hopelessness. Students who have a lower number of friends, spend less amount of time in front of a screen, and feel lonely often/very often are more likely to have moderate/severe hopelessness with high loneliness (Fig. 1 ).
Fig. 1.
Multinominal logistic regression model for mental health groups.
Notes. Reference group: ‘mentally healthy’; A: ‘loneliness’ group, B: ‘hopelessness’ group, C: ‘at-risk’ group, OR: odds ratio, 95 % CI: confidence interval, p: p-value, in bold: statistically significance.
The model explained 25.8 % (Nagelkerke R2) of the variance of mental health, and correctly classified 70.7 % of cases, with 39.3 % correct classification for the particular at-risk group characterized by moderate/severe hopelessness with high loneliness.
4. Discussion
In the present study, we examined the prevalence of loneliness and hopelessness in adolescents and young adults during distance learning education. In sum, more than half of the students reported mild hopelessness and moderate loneliness. Furthermore, a significant proportion of the students, nearly one-fifth and one-fourths showed moderate/severe hopelessness or high loneliness which were more pronounced among adolescent females. Finally, we identified an at-risk group in adolescents and young adults. Students who have a lower number of friends, spend less amount of time in front of a screen, and feel lonely often /very often are more likely to have moderate/ severe hopelessness with high loneliness.
Loneliness can be defined as a subjective experience of a perceived discrepancy between actual and desired social contacts (quantity and/or quality) (Perlman and Peplau, 1981). The level of loneliness was also significant before the covid-19 pandemic, it has already been recognised as a major public health concern (Leigh-Hunt et al., 2017; Cacioppo and Cacioppo, 2018; Jeste et al., 2020).
Social distancing and school closures resulted in an increased level of loneliness, especially with mental health consequences for adolescents/students and young adults (Killgore et al., 2020; Tull et al., 2020; Bu et al., 2020). Although loneliness remained relatively stable in the general population before and after the lockdown period, younger people reported a higher increase in and a higher level of loneliness (Niedzwiedz et al., 2021). Female young adults aged 18–30 years who had already a higher risk of being lonely experienced an increased level of loneliness during the pandemic (Bu et al., 2020). One-third of adolescents have reported a high level of loneliness, and almost half of young adults have been lonely during lockdown which might have detrimental consequences on mental health (Mental Health Foundation, 2021; Lee et al., 2020).
There are a few studies that examined the level of hopelessness during the pandemic and/or lockdown among the younger population. The earliest studies demonstrated an increased level of depression and anxiety (Racine et al., 2020; Marques de Miranda et al., 2020) in children and adolescents which is also supported by further studies. Adolescents or their parents have reported symptoms of internalizing disorders such as depression and anxiety, with increased levels in female adolescents compared to male peers (Duan and Zhu, 2020). Based on previous studies, perceived difficulties such as social isolation, confinement, and school closures resulted in mental health problems, particularly higher depressive symptoms and more loneliness compared to pre-pandemic baselines (Loades et al., 2020; Rogers et al., 2021; Ludwig-Walz et al., 2022). Furthermore, during the COVID-19 pandemic, a higher dose-response relationship was found when school closures occurred (Ludwig-Walz et al., 2022).
It can be assumed that there is a relationship between hopelessness and depression. On one hand, based on the hopelessness theory of depression (Abramson et al., 1989), negative life events could lead to hopelessness, through negative inferences, which may result in symptoms of depression. On the other hand, based on the interpersonal theories of depression (Hames et al., 2013), interpersonal stress which is related to relationship problems and social rejection may lead to depressive symptoms. There is no question that the COVID-19 pandemic represents a significant negative life event and interpersonal stress for everyone.
Adolescents and young adults during the COVID-19 pandemic, especially during distance learning education have faced many challenges such as the new norm of education and lack of optimal learning with cognitive vulnerabilities such as school performance and computer competence, and pre-existing vulnerabilities such as personality, family, and environmental characteristics. Many adolescents and young adults may have seen these challenges as negative life events that they cannot cope with or find difficult to cope with. Based on the results of the present study, a lower number of friends, feeling lonely often/very often and less amount of time spent in front of the screen result in an increase in the likelihood of moderate/severe hopelessness or high loneliness.
The pandemic causes significant changes in friendship and family dynamics among adolescents and young adults. They perceived social and emotional changes such as less support from friends and negative affect, which were associated with mental health problems and loneliness (Rogers et al., 2021; Cooper et al., 2021; Ludwig-Walz et al., 2022). For adolescents and young adults, the peer group is one of the most significant groups for supporting and developing identity (Meeus and Dekoviíc, 1995). Young adults who have fewer friends are at a greater risk for loneliness (Beutel et al., 2017; Shovestul et al., 2020). During the distance learning education period, there was limited access to social support from the peer group. It is worth highlighting that the size of the social network and quantity of social contacts might be more important than the quality (Nicolaisen and Thorsen, 2014) for this young population, which was significantly impaired by social distancing and isolation during the pandemic.
Finally, we found that spending less amount of time in front of the screening in the evening was associated with moderate/severe hopelessness and/or high loneliness. This result seems to contradict previous studies which demonstrated greater virtual contact, or a higher number of hours spent on social media is associated with increased loneliness (Rumas et al., 2021; Cauberghe et al., 2021) and depressive symptoms in adolescents (Murata et al., 2021). In sum, increasing time or no change in time in front of a screen was the most common among students but nearly a tenth of students spent lesser time in front of a screen. Based on this result, it can be assumed that students commonly use this ‘time in front of a screen to keep in contact with their friends. Thus, less time in front of the screen can be related to a higher level of social isolation from peers and lead to a higher level of hopelessness and loneliness. At the same time, it is uncertain if virtual social contact is beneficial during a pandemic when in-person contact is limited. Based on some evidence, virtual interaction does not have the same positive effects as in-person contact (Lee et al., 2011).
There is also some evidence that the pandemic had a greater negative impact on females than on males, possibly exacerbating the gender disparity in health behaviors, especially sedentary/ screen time and physical activity/ exercise that existed among adolescents and young adults before the pandemic (Sterdt et al., 2014). These findings point to the necessity for gender- and age-sensitive interventions. During a pandemic, it is needed for developing public health strategies by scientists, policymakers and professionals to intervene in health and risk behaviors, as well as minimize the health risks connected with changes in these behaviors. Indirect long-term health risks must be considered for adolescents and young adults when developing restrictive policies.
4.1. Limitations of the present study
There are some limitations of the present study. These include the fact that all data were collected online, and students completed the questionnaires voluntarily in a cross-sectional survey; thus, it is not possible to make any causal inferences. Besides selection bias, recall bias and memory inaccuracies may occur which are common biases in cross-sectional studies, and therefore it is possible that students under- or overestimated their measured status (health, physical activity, sleep, screen time, etc.). Further response bias may be caused by misinterpretation of questions, socially acceptable responses, consent responses or even extreme responses. However, during the period of distance learning imposed during the quarantine, self-report data collection was one of the most appropriate methods for the collection of data from a large number of participants. Another limitation is that it is difficult to measure in detail all aspects of students' lives in one study such as types and modalities of indirect social contacts such as text messaging or evaluate other protecting effects such as the closeness of parents. Finally, although there is an officially translated version of UCLA-LS20 in the Hungarian language (Csóka et al., 2007), and it is widely used in research and practice, UCLA-LS20 has not been validated yet in the Hungarian language.
5. Conclusions
In the present study, we demonstrated that the COVID-19 pandemic can be associated with significant mental health problems in adolescents and young adults. The identified at-risk group showed moderate/severe hopelessness with high loneliness. The consequences of this pandemic situation on mental health in this young population may be significant considering the fact that loneliness and hopelessness may be associated with future poor mental and physical health. Thus, there is a need for public health strategies to monitor mental and physical symptoms in one of the most vulnerable populations such as adolescents and young adults. For future studies, it is recommended to develop effective interventions targeted to gender and age with the promotion of resiliencies and buffers against vulnerabilities of negative life events.
Funding
Not applicable.
Ethics approval and consent to participate
The study was conducted with the approval of the Ethical Committee of the Medical Research Council (TUKEB), Hungary, under ETK TUKEB ethical permission No. IV/3067–3/2020/EKU.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
CRediT authorship contribution statement
All authors contributed to the conception of the study to the final draft of the manuscript. JT: analysing the data, interpreting the results, and writing the first manuscript, ZSK: collecting data, reviewing/editing of the manuscript, FI: Conceptualization, supervision of the study, reviewing/editing of the manuscript. All authors read and approved the final manuscript.
Conflict of interest
The authors have declared that they have no competing or potential conflicts of interest.
Acknowledgement
Not applicable.
References
- Abramson L.Y., Metalsky G.I., Alloy L.B. Hopelessness depression: a theory-based subtype of depression. Psychol. Rev. 1989;96:358–372. doi: 10.1037/0033-295X.96.2.358. [DOI] [Google Scholar]
- Beck A.T., Steer R.A. Psychological Corp; San Antonio, TX: 1988. Manual for the Beck Hopelessness Scale. [Google Scholar]
- Beck A.T., Weissman A., Lester D., Trexler L. The measurement of pessimism: the hopelessness scale. J. Consult. Clin. Psychol. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Beutel M.E., Klein E.M., Brähler E., Reiner I., Jünger C., Michal M., Wiltink J., Wild P.S., Münzel T., Lackner K.J., Tibubos A.N. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. 2017;17:97. doi: 10.1186/s12888-017-1262-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bu F., Steptoe A., Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020;186:31–34. doi: 10.1016/j.puhe.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J.T., Cacioppo S. The growing problem of loneliness. Lancet. 2018;391:426. doi: 10.1016/S0140-6736(18)30142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J.T., Patrick W. W.W. Norton & Company Inc; New York, NY: 2008. Loneliness: Human Nature And the Need for Social Connection. [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cauberghe V., Van Wesenbeeck I., De Jans S., Hudders L., Ponnet K. How adolescents use social media to cope with feelings of loneliness and anxiety during COVID-19 lockdown. Cyberpsychol. Behav. Soc. Netw. 2021;24:250–257. doi: 10.1089/cyber.2020.0478. [DOI] [PubMed] [Google Scholar]
- Cénat J.M., Farahi S.M.M.M., Dalexis R.D., Darius W.P., Bekarkhanechi F.M., Poisson H., Broussard C., Ukwu G., Auguste E., Nguyen D.D., Sehabi G., Furyk S.E., Gedeon A.P., Onesi O., El Aouame A.M., Khodabocus S.N., Shah M.S., Labelle P.R. The global evolution of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis of longitudinal studies. J. Affect. Disord. 2022;315:70–95. doi: 10.1016/j.jad.2022.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper K., Hards E., Moltrecht B., Reynolds S., Shum A., McElroy E., Loades M. Loneliness, social relationships, and mental health in adolescents during the COVID-19 pandemic. J. Affect. Disord. 2021;289:98–104. doi: 10.1016/j.jad.2021.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csóka Sz., Szabó G., Sáfrány E., Rochlitz R., Bódizs R. Kísérlet a felnőttkori kötődés mérésére – a kapcsolati kérdőív (Relationship Scale Questionnaire) magyar változata [An experiment to measure adult attachment - the Hungarian version of the Relationship Scale Questionnaire] Pszichológia. 2007;27(4):333–355. [Article in Hungarian] [Google Scholar]
- Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7:300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L., Shao X., Wang Y., Huang Y., Miao J., Yang X., Zhu G. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J. Affect. Disord. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essau C.A., de la Torre-Luque A. Adolescent psychopathological profiles and the outcome of the COVID-19 pandemic: longitudinal findings from the UK Millennium Cohort Study. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;110 doi: 10.1016/j.pnpbp.2021.110330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grunbaum J.A., Kann L., Kinchen S., Ross J., Hawkins J., Lowry R., Harris W.A., McManus T., Chyen D., Collins J. Youth risk behavior surveillance–United States, 2003. Morbidity and mortality weekly report. MMWR Surveill. Summ. 2004;53:1–96. [PubMed] [Google Scholar]
- Hames J.L., Hagan C.R., Joiner T.E. Interpersonal processes in depression. Annu. Rev. Clin. Psychol. 2013;9:355–377. doi: 10.1146/annurev-clinpsy-050212-185553. [DOI] [PubMed] [Google Scholar]
- hbsc Health behaviour in school-aged children. 2006. https://filer.uib.no/psyfa/HEMIL-senteret/HBSC/2006_Mandatory_Questionnaire.pdf Accessed 20 Oct 2020.
- Jeste D.V., Lee E.E., Cacioppo S. Battling the modern behavioral epidemic of loneliness: suggestions for research and interventions. JAMA Psychiatry. 2020;77:553–554. doi: 10.1001/jamapsychiatry.2020.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauhanen L., Wan Mohd Yunus W.M.A., Lempinen L., Peltonen K., Gyllenberg D., Mishina K., Gilbert S., Bastola K., Brown J.S.L., Sourander A. A systematic review of the mental health changes of children and young people before and during the COVID-19 pandemic. Eur. Child Adolesc. Psychiatry. 2022:1–19. doi: 10.1007/s00787-022-02060-0. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W., Cloonan S.A., Taylor E.C., Dailey N.S. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee P.S.N., Leung L., Lo V., Xiong C., Wu T. Internet communication versus face-to-face interaction in quality of life. Soc. Indic. Res. 2011;100:375–389. doi: 10.1007/s11205-010-9618-3. [DOI] [Google Scholar]
- Lee C.M., Cadigan J.M., Rhew I.C. Increases in loneliness among young adults during the COVID-19 pandemic and association with increases in mental health problems. J. Adolesc. Health. 2020;67:714–717. doi: 10.1016/j.jadohealth.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh-Hunt N., Bagguley D., Bash K., Turner V., Turnbull S., Valtorta N., Caan W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- Loades M.E., Chatburn E., Higson-Sweeney N., Reynolds S., Shafran R., Brigden A., Linney C., McManus M.N., Borwick C., Crawley E. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry. 2020;59:1218–1239.e3. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludwig-Walz H., Dannheim I., Pfadenhauer L.M., Fegert J.M., Bujard M. Increase of depression among children and adolescents after the onset of the COVID-19 pandemic in Europe: a systematic review and meta-analysis. Child Adolesc. Psychiatry Ment. Health. 2022;16:109. doi: 10.1186/s13034-022-00546-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques de Miranda D., da Silva Athanasio B., Sena Oliveira A.C., Simoes-E-Silva A.C. How is COVID-19 pandemic impacting mental health of children and adolescents? Int. J. Disaster Risk Reduct. 2020;51 doi: 10.1016/j.ijdrr.2020.101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health. 2020;17:3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy E., Patalay P., Moltrecht B., Shevlin M., Shum A., Creswell C., Waite P. Demographic and health factors associated with pandemic anxiety in the context of COVID-19. Br. J. Health Psychol. 2020;25:934–944. doi: 10.1111/bjhp.12470. [DOI] [PubMed] [Google Scholar]
- McQuaid R.J., Cox S., Ogunlana A., Jaworska N. The burden of loneliness: implications of the social determinants of health during COVID-19. Psychiatry Res. 2021;296 doi: 10.1016/j.psychres.2020.113648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade J. Mental health effects of the COVID-19 pandemic on children and adolescents: a review of the current research. Pediatr. Clin. N. Am. 2021;68:945–959. doi: 10.1016/j.pcl.2021.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meeus W., Dekoviíc M. Identity development, parental and peer support in adolescence: results of a national Dutch survey. Adolescence. 1995;30:931–944. [PubMed] [Google Scholar]
- Mental Health Foundation Loneliness during coronavirus. 2021. https://www.mentalhealth.org.uk/coronavirus/loneliness-during-coronavirus Accessed 15 Dec 2021.
- Ministry of Justice . Ministry of Justice, Hungary; 2020. Government Decree 484/2020 (10 Nov) on the Second Phase of Protective Measures Applicable during the Period of State of Danger.http://jogszabalykereso.mhk.hu/translated/doc/J2020R0484K_20210320_FIN.pdf Accessed 15 Dec 2021. [Google Scholar]
- Mittal V.A., Firth J., Kimhy D. Combating the dangers of sedentary activity on child and adolescent mental health during the time of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry. 2020;59:1197–1198. doi: 10.1016/j.jaac.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monostori J. Publications Office of the European Union; Luxembourg: 2021. The School Year 2020-2021 in Hungary During the Pandemic - Country Report. 2021, ISBN 978-92-76-38671-1. JRC125455. [DOI] [Google Scholar]
- Morelli M., Cattelino E., Baiocco R., Trumello C., Babore A., Candelori C., Chirumbolo A. Parents and children during the COVID-19 lockdown: the influence of parenting distress and parenting self-efficacy on children's emotional well-being. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.584645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murata S., Rezeppa T., Thoma B., Marengo L., Krancevich K., Chiyka E., Hayes B., Goodfriend E., Deal M., Zhong Y., Brummit B., Coury T., Riston S., Brent D.A., Melhem N.M. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress. Anxiety. 2021;38:233–246. doi: 10.1002/da.23120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolaisen M., Thorsen K. Who are lonely? Loneliness in different age groups (18–81 years old), using two measures of loneliness. Int. J. Aging Hum. Dev. 2014;78:229–257. doi: 10.2190/AG.78.3.b. [DOI] [PubMed] [Google Scholar]
- Niedzwiedz C.L., Green M.J., Benzeval M., Campbell D., Craig P., Demou E., Leyland A., Pearce A., Thomson R., Whitley E., Katikireddi S.V. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK Household Longitudinal Study. J. Epidemiol. Community Health. 2021;75:224–231. doi: 10.1136/jech-2020-215060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peplau L.A., Perman D. In: Love And Attraction: An International Conference. Cook M., Wilson G., editors. Pergamon; Oxford: 1979. Blueprint for a social psychological theory of loneliness; pp. 101–110. [Google Scholar]
- Perczel Forintos D., Sallai J., Rózsa S. A Beck-féle Reménytelenség Skála pszichometriai vizsgálata [Psychometric properties of Beck Hopelessness Scale] Psychiat. Hung. 2001;16:632–643. [Google Scholar]
- Perlman D., Peplau L.A. In: Personal Relationships: 3. Relationships in Disorder. Gilmour R., Duck S., editors. Academic Press; London: 1981. Toward a social psychology of loneliness; pp. 31–56. [Google Scholar]
- Racine N., Cooke J.E., Eirich R., Korczak D.J., McArthur B., Madigan S. Child and adolescent mental illness during COVID-19: a rapid review. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers A.A., Ha T., Ockey S. Adolescents' perceived socio-emotional impact of COVID-19 and implications for mental health: results from a U.S.-based mixed-methods study. J. Adolesc. Health. 2021;68:43–52. doi: 10.1016/j.jadohealth.2020.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumas R., Shamblaw A.L., Jagtap S., Best M.W. Predictors and consequences of loneliness during the COVID-19 pandemic. Psychiatry Res. 2021;300 doi: 10.1016/j.psychres.2021.113934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D.W. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J. Pers. Assess. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Russell D., Peplau L.A., Ferguson M.L. Developing a measure of loneliness. J. Pers. Assess. 1978;42:290–294. doi: 10.1207/s15327752jpa4203_11. [DOI] [PubMed] [Google Scholar]
- Shovestul B., Han J., Germine L., Dodell-Feder D. Risk factors for loneliness: the high relative importance of age versus other factors. PloS One. 2020;15 doi: 10.1371/journal.pone.0229087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterdt E., Liersch S., Walter U. Correlates of physical activity of children and adolescents: a systematic review of reviews. Health Educ. J. 2014;73:72–89. doi: 10.1177/0017896912469578. [DOI] [Google Scholar]
- Tull M.T., Edmonds K.A., Scamaldo K.M., Richmond J.R., Rose J.P., Gratz K.L. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S.J., Zhang L.G., Wang L.L., Guo Z.C., Wang J.Q., Chen J.C., Liu M., Chen X., Chen J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used during the current study are available from the corresponding author on reasonable request.