Abstract
Transvenous laser-assisted lead extraction is successful, with a low procedural complication rate for a wide range of indications. Here, we report a case of right internal jugular triple-lumen central venous catheter fracture and subsequent embolism to the right pulmonary artery during laser lead extraction that was successfully retrieved with a gooseneck snare. (Level of Difficulty: Advanced.)
Key Words: central venous catheter, implantable cardioverter-defibrillator, laser lead extraction
Abbreviations and Acronyms: CVC, central venous catheter; ICD, implantable cardioverter-defibrillator; RV, right ventricle
Central Illustration

A 58-year-old man with a history of ventricular fibrillation requiring a single-chamber single-coil implantable cardioverter defibrillator (ICD) for secondary prevention was referred from an outside hospital for laser lead extraction because of ICD lead vegetation and methicillin-sensitive Staphylococcus aureus bacteremia.
Learning Objectives
-
•
To recognize catheter fracture as a potential complication in laser lead extraction procedures.
-
•
To understand treatment modalities for catheter fracture and embolism.
-
•
To avoid CVC placement in the path of pacemaker/ICD lead extraction.
Twenty-eight years before to this presentation, his initial ICD was implanted in the abdomen, with a lead tunneling to the right subclavian vein because the left subclavian vein was inaccessible. His right-sided lead and generator were abandoned because of low shock impedance in the lead and were replaced with a left pectoral transvenous single-chamber ICD. One year before this presentation, the abdominal generator was extracted after a motor vehicle accident, but the leads were abandoned.
He had initially presented to an outside hospital with pain, erythema, and drainage in the abdominal wound. He was found to have infection of the abdominal device pocket site, for which he underwent right-sided tunneled lead removal, wound debridement, and wound vacuum application by general surgery. Wound and blood cultures grew methicillin-sensitive S. aureus. A transesophageal echocardiogram revealed left-sided ICD lead vegetations in the right atrium. He was given cefazolin. A polyurethane 7-F 20-cm triple-lumen right internal jugular central venous catheter (CVC) was inserted secondary to poor access and need for prolonged antibiotic administration at the outside hospital (Figure 1). He was transferred to our center for consideration of laser lead extraction.
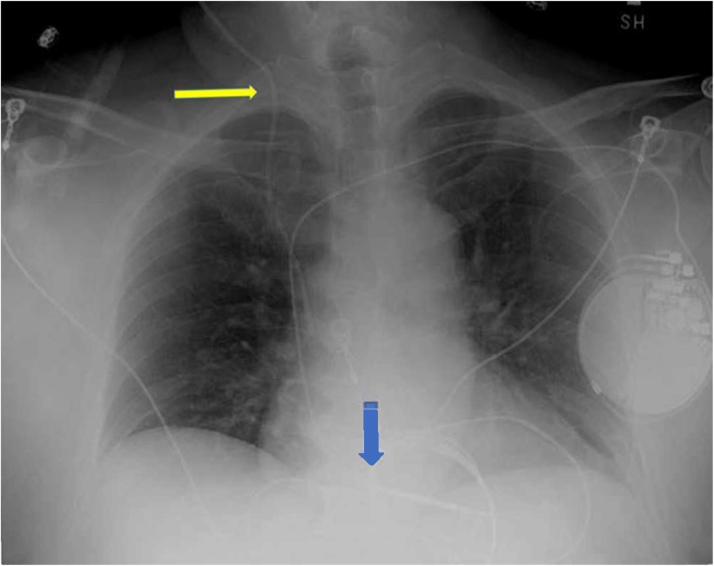
Figure 1.
Baseline Preoperative Chest X-Ray
Baseline preoperative chest x-ray with single-chamber implantable cardioverter-defibrillator (blue arrow) and right internal jugular central venous catheter (yellow arrow).
On presentation to our hospital, his initial vital signs were temperature of 37.1 °C, heart rate of 78 beats/min, respiratory rate of 18 breaths/min, blood pressure of 111/70 mm Hg, and oxygen saturation of 99%. He was in no acute distress; his lungs were clear to auscultation, and heart sounds were normal without a murmur detected. He had a right abdominal, linear, and transverse wound measuring 4 inches, and a wound vacuum was applied.
Medical History
The patient had a medical history of ventricular fibrillation, persistent atrial fibrillation, hypertension, and hyperlipidemia.
Differential Diagnosis
Based on the history, physical examination results, and work-up, the differential diagnosis in this case was ICD lead vegetation versus ICD lead thrombus.
Investigations
The decision was made after consultation with infectious disease and cardiothoracic surgery teams to proceed with laser lead extraction.
Management
Briefly, the patient was given local lidocaine anesthesia, and a horizontal incision was made over the left infraclavicular fossa. The ICD generator was identified and externalized from the pocket. The generator was disconnected from the right ventricle (RV) lead. Then, a clearing stylet was applied to the old RV lead, and an attempt to retract the fixation screw was made using a torquing tool. The clearing stylet was removed from the lead. A lead-locking device was applied to the tip of the old RV lead and deployed. Sutures were used to tie the insulation of the lead and to provide additional anchoring points.
A 16-F laser sheath was then applied over the old RV lead. Several applications of the laser were used to dissect the RV lead down to the proximal ICD coil. Despite multiple attempts, we could not advance the laser sheath further down the lead. It was also noticed at this juncture that a portion of the CVC placed in the right internal jugular vein fragmented during laser advancement and embolized to a distal branch of the right pulmonary artery (Figure 2, Video 1). We removed the fragmented CVC from the body to avoid further damage (Figures 3 and 4). A 6-F femoral venous sheath was used for medication and fluid administration from here on. At this time, we also decided to continue with lead extraction by switching to a 13-F mechanical rotating dilator sheath. Several applications of the mechanical tool were successful in freeing the lead to the tip. The lead was removed from the patient's body, and hemostasis was achieved in the pocket with manual pressure.
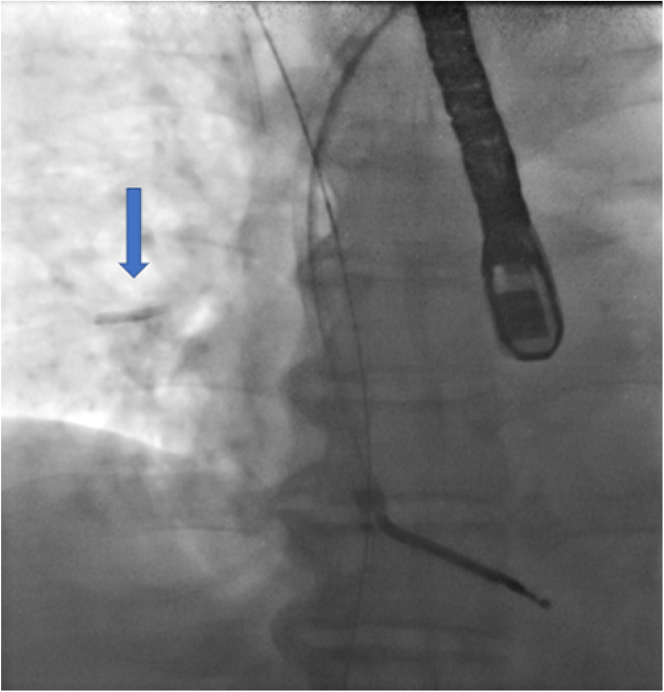
Figure 2.
Central Venous Catheter Fragment in Right Pulmonary Artery
Central venous catheter fragment in right pulmonary artery (blue arrow).
Figure 3.
Remaining Proximal Portion of Central Venous Catheter After Removal
Charring and burn marks are evident at the distal tip of the catheter (blue arrow).
Figure 4.
Distal Tip of Fractured Central Venous Catheter
Distal tip of fractured central venous catheter with burn marks (blue arrow).
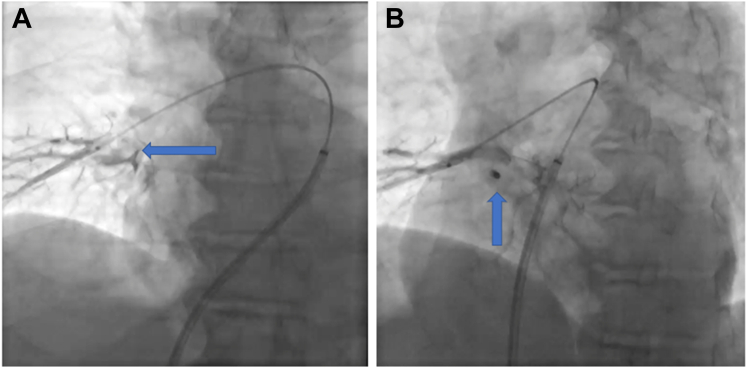
Next, it was decided to snare the fragmented portion of the CVC via right femoral vein access. A 6-F multipurpose catheter was advanced over a 260-cm 035 Glidewire to the right pulmonary artery using small injections of contrast material as a guide (Figures 5A and 5B, Videos 1 and 2). The guidewire was placed next to the fragmented CVC, and a 4-F snare catheter was advanced over it. Next, we exchanged the guidewire for a 10-mm gooseneck snare. Using orthogonal fluoroscopic views, we were able to successfully snare the fragmented portion (Figure 6, Video 3). Next, we removed the whole snare with the fragment en masse from the body (Figure 7). Hemostasis in the groin was achieved with manual compression.
Figure 5.
Angiography of Right Pulmonary Artery
(A, B) Angiography of right pulmonary artery localizing the position of catheter fragment.
Figure 6.
Fluoroscopy View of Embolized Catheter Tip
Fluoroscopy view of embolized catheter tip with snare (blue arrow).
Figure 7.
Fragmented End of Retrieved Catheter
Fragmented end of the catheter retrieved with snare tool (white arrow).
Discussion
To our knowledge, this is the first reported case of fracture of a CVC catheter and subsequent embolism during lead extraction using specifically excimer laser. The catheter tip was noted to fragment during advancement of the laser sheath, and embolization to the pulmonary artery was clearly witnessed during the case.
The 2017 Heart Rhythm Society expert consensus statement recommends complete device and lead extraction in patients with definite implantable electronic device infection evidenced by sepsis, valvular endocarditis, or lead endocarditis.1 Several techniques and tools are used in lead extraction such as traction, locking stylet, sheath and grasping devices, mechanical dilator sheaths, and laser extraction.2,3 Lead extraction can be challenging because of the fibrous adhesions between the lead and cardiovascular structures that develop over time. The application of a laser sheath over the lead during extraction helps release these adhesions by delivering a ring of laser light in pulses to the working section of the sheath. The PLEXES trial demonstrated a higher success rate in laser lead extraction (94%) compared with nonlaser lead extraction (64%).4 The rates of major complications from laser lead extraction range between 1.2% and 3.4%.4, 5, 6, 7 Major complications reported in the literature include right atrial tear and perforation, cardiac tamponade (1.2%), tricuspid laceration requiring surgical repair (0.6%), subclavian vein laceration (0.6%), and hypotension prompting surgical exploration (0.6%). Minor complications commonly seen include pocket hematoma (1.5%), discrete pericardial effusion (0.6%-0.7%), pneumothorax (0.6%-0.7%), pulmonary edema (0.6%), and transient low output state (0.6%).5 To the best of our knowledge, CVC fracture and embolism have been reported only once in the literature.6 In that case, the patient was incidentally found to have fracture and embolization of the peripherally inserted CVC after the procedure. In addition, the case report did use mechanical tools in addition to laser. Mechanical tools tend to have a higher propensity of causing damage to catheters as well as ipsilateral leads because of their rotating cutting blades. Our case is unique because the fragmentation and embolization clearly occurred during advancement of the laser sheath. Ultraviolet lasers in lead extraction use xenon-based excimer technology. They are unique because they facilitate photoablation by selectively binding scar tissue surrounding the cardiac pacemaker and ICD leads. This is achieved when an ultraviolet laser pulse hits tissue and is absorbed by the water molecule, which vaporizes it, resulting in breakage of molecule bonds and cell rupture. The laser does not interact with adjacent leads or other catheters because its properties affect tissue (photochemical, photomechanical, photothermal) that contain water to break molecular bonds. The tip temperature during laser pulse delivery is 108 °F. The polyurethane and silicone materials used in manufacturing CVCs are extremely resistant to this minor temperature change.
CVCs are widely used in clinical practice for resuscitation and administration of vasoactive medications, hemodialysis, chemotherapy, and prolonged parenteral nutrition and antibiotics.7 Fracture and embolization are among the rare and life-threatening complications of the CVC.8 The fractured fragment could potentially trigger a localized inflammatory response, which can lead to the creation of a thrombus and associated respiratory and hemodynamic complications. Most embolized catheter fragments can be removed percutaneously with a gooseneck snare, as we did in our patient. In rare cases, depending on the location of the catheter, fragment removal with a surgical thoracotomy might become necessary. In some instances, the catheter can be abandoned if the risks associated with an invasive extraction outweigh the benefits.9
The mechanism of the laser lead extraction–related CVC fracture is evident on inspection of the removed CVC. In our case, the burn marks and char formation at the catheter transection level indicate that injury was due to laser-induced damage instead of mechanical trauma or pinching (Figures 3 and 4). It is possible that the administration of medications and intravenous fluids at high rates through the triple lumen acted as an “accelerant” of sorts, resulting in damage and ultimate fracture. However, previous pulling tension and friction contributing to a partial tear that was completed by laser-induced damage is another possibility. Therefore, we advise extreme caution and immediate catheter integrity assessment with fluoroscopy with the use of laser technology in a vein occupied by a catheter. We also believe that if possible, avoiding intravenous lines ipsilateral to the side where the tools for lead extraction will need to be advanced can help prevent this complication. Finally, if laser lead extraction is anticipated, we recommend relocation of a CVC in the internal jugular vein to a more proximal position, or removal entirely from the neck with a replacement catheter placed in the femoral vein, at least until conclusion of the procedure.
Follow-Up
Another CVC was inserted, and the patient was discharged with intravenous antibiotics and a wearable cardioverter-defibrillator.
Conclusions
Laser lead extraction can result in not only venous or cardiac injury but also injury to intraluminal structures such as CVCs. We advise caution and vigilance to maintain the integrity of the CVC.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Anteroposterior angiography of right pulmonary artery localizing the position of catheter fragment.
Right anterior oblique angiography of right pulmonary artery localizing the position of catheter fragment.
Gooseneck snaring of catheter fragment in right pulmonary artery.
References
- 1.Kusumoto F.M., Schoenfeld M.H., Wilkoff B.L., et al. 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm. 2017;14:e503–e551. doi: 10.1016/j.hrthm.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Farooqi F.M., Talsania S., Hamid S., Rinaldi C.A. Extraction of cardiac rhythm devices: indications, techniques and outcomes for the removal of pacemaker and defibrillator leads. Int J Clin Pract. 2010;64:1140–1147. doi: 10.1111/j.1742-1241.2010.02338.x. [DOI] [PubMed] [Google Scholar]
- 3.Bahadır N., Canpolat U., Kaya E.B., et al. Comparison of acute and long-term outcomes of Evolution(®) and TightRail™ mechanical dilator sheaths during transvenous lead extraction. J Cardiovasc Electrophysiol. 2021;32:1395–1404. doi: 10.1111/jce.15006. [DOI] [PubMed] [Google Scholar]
- 4.Wilkoff B.L., Byrd C.L., Love C.J., et al. Pacemaker lead extraction with the laser sheath: Results of the pacing lead extraction with the excimer sheath (PLEXES) trial. J Am Coll Cardiol. 1999;33:1671–1676. doi: 10.1016/s0735-1097(99)00074-1. [DOI] [PubMed] [Google Scholar]
- 5.Sood N., Martin D.T., Lampert R., Curtis J.P., Parzynski C., Clancy J. Incidence and predictors of perioperative complications with transvenous lead extractions: Real-world experience with National Cardiovascular Data Registry. Circ Arrhythm Electrophysiol. 2018;11 doi: 10.1161/CIRCEP.116.004768. [DOI] [PubMed] [Google Scholar]
- 6.Rizkallah J., Sumner G., Sheldon R. Central venous catheter fracture during pacemaker lead extraction. HeartRhythm Case Rep. 2016;2:11–13. doi: 10.1016/j.hrcr.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rupp S.M., Apfelbaum J.L., Blitt C., et al. Practice guidelines for central venous access: A report by the American Society of Anesthesiologists task force on central venous access. Anesthesiology. 2012;116:539–573. doi: 10.1097/ALN.0b013e31823c9569. [DOI] [PubMed] [Google Scholar]
- 8.Surov A., Wienke A., Carter J.M., et al. Intravascular embolization of venous catheter---causes, clinical signs, and management: A systematic review. JPEN J Parenter Enteral Nutr. 2009;33:677–685. doi: 10.1177/0148607109335121. [DOI] [PubMed] [Google Scholar]
- 9.Kim O.K., Kim S.H., Kim J.B., et al. Transluminal removal of a fractured and embolized indwelling central venous catheter in the pulmonary artery. Korean J Intern Med. 2006;21:187–190. doi: 10.3904/kjim.2006.21.3.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Anteroposterior angiography of right pulmonary artery localizing the position of catheter fragment.
Right anterior oblique angiography of right pulmonary artery localizing the position of catheter fragment.
Gooseneck snaring of catheter fragment in right pulmonary artery.